Neonatal and Infant Nutrition
advertisement

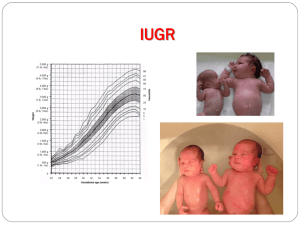
1 Abdulmahdi A. Hasan* *Ph,D, pediatric & psychiatric Mental Health Nursing Neonatal and Infant Nutrition Introduction What does ‘nutrition’ mean to you? The OED definition Nutrition (noun) 1. the process of taking in and assimilating nutrients. 2. the branch of science concerned with this process. DERIVATIVES nutritional adj. nutritionist noun. ORIGIN Latin, from nutrire ‘nourish’. • Textbook answer • Nelson’s Textbook of Paediatrics – achievement of satisfactory growth and avoidance of deficiency states. – Aims • To explore the knowledge base behind key competencies in nutrition for paediatricians • Reference: A Framework of Competences for Core Higher Specialist Training in Paediatrics (RCPCH, 2005.) • Objectives • By the end of this morning, you will – understand the effects of fetal growth restriction on short- and longterm health – understand the principles and importance of nutrition in the neonatal period including assessment of nutritional status – be able to make appropriate recommendations to address feeding problems and faltering growth • ‘Normal’ Nutrition • Fetal nutrition • Parenteral (mostly!) • Stores are laid late in gestation • At 28 weeks, a fetus has: – 20% of term calcium and phosphorus stores – 20% of term fat stores – About a quarter of term glycogen stores – Adaptation to nutrition after birth • Gut adaptation is regulated by – Endocrine factors – Intraluminal factors – Breast milk hormones and growth factors 2 • • • • • • • • • • • • • • • • • • • • • • • • • • • • – Bacteria Breast is best Feeding the term infant Breast feeding achieves – Nutrition – Immunological and antimicrobial protection – Passage of breast milk hormones and growth factors – Provision of digestive enzymes – Facilitation of mother-infant bonding Supplementing breast milk Should be unnecessary, but – Vitamin K levels are low – Vitamin D levels are low in areas of little sunlight – Iron levels are low (but very well absorbed) – Artificial Feeds Term formulas are broadly similar – May be whey or casein based – International agreed standards for constituents – Artificial feeding Practical considerations for making up feeds – Water softeners increase sodium content – Repeated or prolonged boiling can increase sodium content of water – Bottled water can contain high levels of carbon dioxide, sodium, nitrate and fluoride. Monitoring feeding Maternal sensation of engorgement and emptying Frequency of feeding Wet nappies Stools Jaundice Weight Normal output Support for breast feeding mothers Midwife Infant feeding specialist Breast feeding support groups National Childbirth Trust Nutrition for the preterm or sick baby From little acorns… The obstetric team ask you to talk to a mother who is being induced at 31 weeks gestation as she is ‘small for dates’. What further information would you like? Mrs Oak 28 year old primigravida 5’2, 80kg Smokes 5 cigarettes daily 3 • • • • • • • • • • • • • • • • • • • • • • Concerns about growth from 20 weeks Latest ‘dopplers’ show absent EDF Proteinuria and hypertension In groups, plan your chat How will you counsel the family? Consider particularly: – Risks of preterm delivery vs risk of continuing pregnancy – Short term risks – Approach to feeding – Long term outcome Short term risks of IUGR Obstetric – Intrauterine death – Intrapartum asphyxia – Short term risks of IUGR Paediatric – Hypoglycaemia – Necrotising enterocolitis – Increased risk of problems of prematurity – (hypothermia) – (polycythaemia) NEC and IUGR Case-control study (n=74) – at 30-36 weeks GA, birth weight <10th centile is a significant risk factor – OR 6 (1.3-26)1 Observational study (n= 69) – At 30-36 weeks 71% of cases were <10th centile2 • 1 Beeby and Jeffrey. 1991, ADC:67:432-5 • 2 McDonnell and Wilkinson. Sem Neonatol 1997 NEC and IUGR: Why? Pathogenesis of NEC requires – enteral feeding – gut ischaemia – bacterial infection Abnormal gut blood flow recognised in IUGR Ischaemic damage or reperfusion injury? Normal doppler flow in umbilical artery Absent end diastolic flow Reversed end-diastolic flow Abnormal dopplers and NEC In 9 of 14 studies, AREDF led to an increased risk of NEC OR 2.13 (95%CI 1.49 to 3.03) • Dorling J, Kempley S, Leaf A. Feeding growth restricted preterm infants with abnormal antenatal Doppler results. Arch. Dis. Child. Fetal Neonatal Ed. 2005; 90: F359-F363 4 • • • • • • • • • • • • • • • • • • • • • • • • • • • So how to feed? Delay start? Use non-nutritive feeds? Increase slowly? Use friendly bacteria? Cochrane review: early vs late feeding 72 babies in 2 studies Early feeders had – Fewer days parenteral nutrition – Fewer investigations for sepsis No difference in – NEC – Weight gain – Cochrane review: rapid vs slow increase 369 babies in 3 studies Rapid: 20 to 35 ml/kg/day Slow: 10 to 20 ml/kg/day Rapid group: – reached full enteral feeds and regained birthweight faster – No difference in NEC rate or length of stay Cochrane review: minimal enteral nutrition 380 babies in 8 studies 12 to 24 ml/kg/day for 5 to 10 days MEN group – Faster to full enteral feeds – Shorter length of stay – No difference in NEC Probiotics for preventing NEC Systematic review of 1393 VLBW infants treated with a variety of organisms Reduced risk of – NEC (RR 0·36, 95% CI 0·20–0·65) – Death (RR 0·47, 0·30–0·73) Achieved full feeds faster No difference in rates of sepsis – Deschpande et al, Lancet 2007 – Preventing NEC: what works? Feeding small or preterm infants: Choices Human milk – Mother’s own – Banked donor milk – Fortified Artificial – Term formula – Preterm formula Parenteral Nutrition Parenteral Nutrition 5 • • • Parenteral Nutrition If an infant can’t, won’t or shouldn’t be fed enterally What’s in the bag? – Fluid – Carbohydrate – Protein – Fat – Minerals and Trace Elements – Energy • Requirements – Basal metabolic rate – Physical activity – Specific dynamic action of food – Thermoregulation – Growth • Energy • Requirements kcal/kg/day – Basal metabolic rate 40 – Physical activity 4+ – Specific dynamic action of food (10%) – Thermoregulation variable – Growth 70 (To match in-utero growth of 15g/kg/day) • Protein • With glucose infusion alone, infants lose 1-2% of endogenous protein stores daily • 1g/kg/day gives protein balance • 2.5 to 3.5g/kg/day allows accretion – nb energy requirement • Safe to start soon after birth • Fat • Energy source • Essential fatty acid source (intralipid) • Cell uptake and utilisation of free fatty acids is deficient in preterm infants • Start at max 1g/kg/day, increasing gradually to 3g/kg/day (less if septic) • Benefits of PN • Earlier, faster weight gain • Avoidance of problems associated with enteral feeds • Risks of PN • Line associated sepsis • Line related complications (eg thrombosis) • Hyperammonaemia • Hyperchloraemic acidosis • Cholestatic jaundice • Trace element deficiency • Milk Feeds 6 • • • • • • • • Human milk advantages Protection from NEC Improved host defences Protection from allergy and eczema Faster tolerance of full enteral feeds Better developmental and intellectual outcome Human milk shortcomings if preterm Human milk may not provide enough – Protein – Energy – Sodium – Calcium, phosphorus and magnesium – Trace elements (Fe, Cu, Zn) – Vitamins (B2,B6,Folic acid, C,D,E,K) • Breast milk fortifiers • Improved – short term growth – nutrient retention – bone mineralisation • Concerns – trend towards increased NEC • Term vs preterm formulas • Term formulas do not provide for preterm protein, calcium, sodium and phosphate requirements, even at high volumes • Term formula (vs preterm formula) fed infants – Grow more slowly – Have lower developmental score and IQ at follow up • Feeding preterm infants: aim “To provide nutrient intakes that permit the rate of postnatal growth and the composition of weight gain to approximate that of a normal fetus of the same gestational age, without producing metabolic stress” American Academy of Pediatrics Committee on Nutrition • Evidence Based Nutrition • RA Ehrenkranz, Seminars in Perinatology 2007 (31): 48-55 • Post-Discharge Nutrition • Post discharge nutrition • Preterm infants tend to be small at discharge, and remain small into adolescence • Limited evidence for what rate of growth is optimal • The evidence • Comparison of ‘post-discharge’ formula with standard term formula – No consistent difference in growth parameters or body composition – Z-score reduces in both groups – Term formula needs supplementing with vitamins and iron to achieve targets • The evidence 7 • • • • • • • • • • • • • • • • • • • • • • • • Comparison of breast milk with term formula – Calcium and phosphate deficiency in breast milk fed infants in first year resolves by age two – Little difference in growth (although small numbers) Outcomes Catch-up Growth Enhanced nutritional intake sufficient to allow ‘catch-up’ growth improves long term neurodevelopmental outcome Body composition differences Compared to term infants, ex-preterm infants fed at 120 kcal/kg/day – Have more body fat – Have a different fat distribution The long range forecast with IUGR Does the in-utero environment or early feeding permanently change organ structure, function and metabolism? Developmental Origins theory Humans demonstrate ‘developmental plasticity’ in response to their environment Part of cardiovascular risk may be explained by in-utero and postnatal growth Developmental Origins theory Geographically, coronary heart disease correlates with past neonatal mortality In epidemiological studies, adult cardiovascular disease is associated with: – low birthweight – rapid early postnatal growth Is rapid catch-up growth bad? Postnatal weight gain is associated with BMI and waist circumference at 19 years IUGR infants are at increased risk of the metabolic syndrome Preterm infants fed breast milk rather than preterm formula – had lower BP at 13-16yrs – were less insulin resistant – had a better LDL:HDL ratio Nutrition Assessment How best to assess growth and nutrition? Weight – Reflects mass of lean tissue, fat, intra- and extra-cellular fluid compartments Length – More accurately reflects lean tissue mass Head circumference – Correlates well with overall growth and developmental achievement – Laboratory assessment TPN requires regular monitoring of acid base status, liver function, bone profile and electrolytes 8 • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • In enterally fed infants, monitoring albumin, transferrin, total protein, urea, alkaline phosphatase and phosphate may be useful Infant Feeding Task Read the GP referral letter In pairs: – Pick out the important aspects of the referral – Decide what further questions you’d like to ask the family – What sort of investigations (if any) might you consider? Faltering Growth ‘Failure to Thrive’ Term first used to describe delayed growth and development, – also called maternal deprivation syndrome. “A failure of expected growth and well being” Only growth can be objectively measured Crossing centiles? 5% of normal infants cross 2 intercentile spaces from birth to 6 weeks. 5% of normal infants cross 2 intercentile spaces from 6 weeks to 1 year. Infants regress to the mean Hence development of ‘thrive lines’ Causes and correlates Organic disease Abuse and Neglect Deprivation Undernutrition Causes and correlates Organic disease – <5%, usually suggestive symptoms and signs Abuse and Neglect – increased risk, but a small proportion Deprivation – may influence referral Undernutrition The Energy Balance Equation Undernutrition Most are underweight for height Fastest decline in weight gain when energy needs are highest Poor appetite Delayed progression to solid foods Limited range of foods Faltering Growth over time Consequences Lasting deficit in growth Lasting effects on appetite and feeding Low maternal self esteem Developmental delay at 1 year 9 • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • – 7-10 DQ points Small (not statistically significant) IQ difference at 8-9 years Management Few trials of intervention One RCT found health visitor led intervention useful One non randomised trial found dietary advice useful Management is therefore based on ‘accepted best practice’ – Screening or Case Finding? Up to 50% of children with FTT are never identified Recommendations for frequency of weighing suggest paying more attention to fewer weights. Growth Monitoring Primary or Secondary care? Common problem, often resolves with simple interventions Ill children or those losing weight need referral Home visitor assessment – Dietary history – Simple explanation and advice Second port of call should be dietician Strategies The Role of the Paediatrician Investigations (if necessary) should be completed promptly FBC, ferritin, U+Es, TFTs, TT glutaminase, MSU Chromosome analysis in girls CXR and sweat test in young infants or history of respiratory infections. Pathway of care If not improving? Nursery nurse involvement or nursery placement Help with other behavioural problems Treat illness in mother Social work input Almost never need food supplements or hospital admission Task One volunteer to play the part of Neil’s parent A second volunteer to be the registrar in clinic Others to observe and be prepared to give feedback at the end Question What are the agendas of the health professionals and the parent? How will you address the different priorities? Where will you take things from here? Feeding difficulties in ex-prems Feeding issues are common, especially in those born before 28 weeks Risk of – Disordered oral-motor functioning – Significant gastro-oesophageal reflux – Oral hypersensitivity 10 • • • • • • • • • • • • • • • • • • • • • • • • • • • – Neurological impairment affecting feeding Colic What is Colic? “excessive bursts of crying in an otherwise healthy infant not relieved by routine comfort” ‘Colic’ crying is said to be of higher amplitude, greater intensity, more frequent, and of longer duration Problems in Evaluation Poor case definition Few controlled studies Little evidence base for management or investigation The Classic Definition “crying lasting 3 or more hours per day, on more than 3 days a week, for at least 3 weeks and resolving around 3 months”. – Wassell, Pediatrics 1954 Study Results Quantifying colic – scoring scales – acoustic cry assessments No effect of sex, birth order, social class, ethnic origin. Vagal tone and cortisol levels are the same as in non-colicky babies The impact on parents Resistance to soothing causes anxiety Learned helplessness, causing anxiety and depression Stress can cause parental coping crises 10% of mothers experience a depressive disorder postnatally Temperament Some reports link excessive crying to later difficult behaviours – few studies only – based on maternal recall – possible that quality of care in later childhood is influenced by early patterns of behaviour Colic and difficulties with feeding 19 with colic v 24 without Assessment: – colic symptom checklist – neonatal oral assessment score – clinical feeding evaluation Outcomes Colic group showed: – more disorganised feeding behaviours, – less rhythmic nutritive and non-nutritive sucking, – more discomfort during feeds, – lower responsiveness during feeding interactions. • Miller-Loncar, Arch Dis Child 2004; 89 908-12 Organic causes of a ‘colicky’ baby 11 • • • • • • • • • • • • • • • • • • • • • • • • • • • congenital heart disease CNS abnormalities NAI fever eg UTIs maternal drug ingestion gastro-oesophageal reflux cows milk protein intolerance malabsorption gut dysmotility Gut hormones Motilin initiates migrating motor complexes Vagus stimulation increases number and force of contractions Raised motilin in 2 small studies of infantile colic Smokers have higher motilin levels Systematic review of treatment Lucassen et al, BMJ, 1998 50 complete studies, 27 controlled reviewed. Treatments for colic Results as effect size – Behavioural: (reducing stimulation) 0.48 – Dicycloverine: 0.46, but serious side effects – Hydrolysate milks: 0.22 – Herbal tea: 0.32 (single small study) – Low lactose and soya milks: no effect – Simethicone: no effect Treatments for colic Any Questions? Summary Optimal growth for neonates and infants requires careful thought about nutrition Interventions (or lack of them) may have long term consequences There is a limited evidence base to guide current practice Colic is common Feeding difficulties post SCBU are common