A 58 nW ECG ASIC With Motion-Tolerant Heartbeat Timing
advertisement
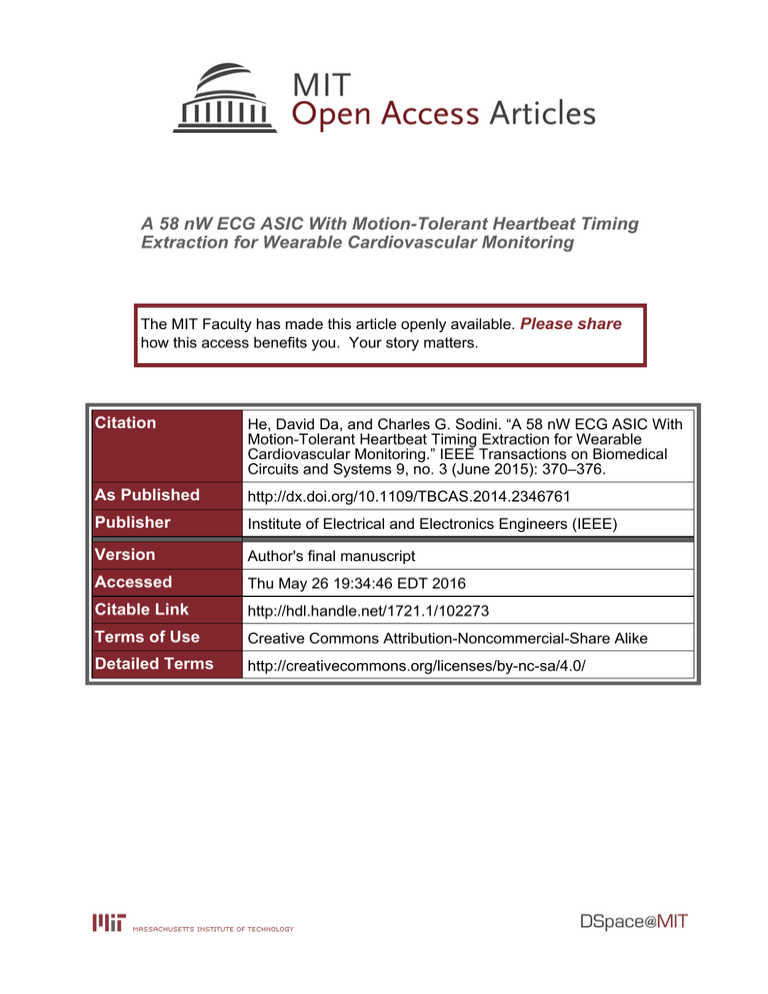
A 58 nW ECG ASIC With Motion-Tolerant Heartbeat Timing Extraction for Wearable Cardiovascular Monitoring The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation He, David Da, and Charles G. Sodini. “A 58 nW ECG ASIC With Motion-Tolerant Heartbeat Timing Extraction for Wearable Cardiovascular Monitoring.” IEEE Transactions on Biomedical Circuits and Systems 9, no. 3 (June 2015): 370–376. As Published http://dx.doi.org/10.1109/TBCAS.2014.2346761 Publisher Institute of Electrical and Electronics Engineers (IEEE) Version Author's final manuscript Accessed Thu May 26 19:34:46 EDT 2016 Citable Link http://hdl.handle.net/1721.1/102273 Terms of Use Creative Commons Attribution-Noncommercial-Share Alike Detailed Terms http://creativecommons.org/licenses/by-nc-sa/4.0/ IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS 1 A 58nW ECG ASIC with Motion-tolerant Heartbeat Timing Extraction for Wearable Cardiovascular Monitoring David Da He, and Charles G. Sodini, Fellow, IEEE Abstract—An ASIC for wearable cardiovascular monitoring is implemented using a topology that takes advantage of the electrocardiogram’s (ECG) waveform to replace the traditional ECG instrumentation amplifier, ADC, and signal processor with a single chip solution. The ASIC can extract heartbeat timings in the presence of baseline drift, muscle artifact, and signal clipping. The circuit can operate with ECGs ranging from the chest location to remote locations where the ECG magnitude is as low as 30µV . Besides heartbeat detection, a midpoint estimation method can accurately extract the ECG R-wave timing, enabling the calculations of heart rate variability. With 58nW of power consumption at 0.8V supply voltage and 0.76mm2 of active die area in standard 0.18µm CMOS technology, the ECG ASIC is sufficiently low power and compact to be suitable for long term and wearable cardiovascular monitoring applications under stringent battery and size constraints. Index Terms—Electrocardiogram, heart rate, motion artifacts, cardiovascular monitoring, wearable sensor. I. I NTRODUCTION ARDIOVASCULAR disease (CVD) affects 37% of the United States population and is the leading cause of death in the U.S. [1]. One type of CVD is cardiac arrhythmia, which is characterized by irregular heartbeat intervals. The most common form of cardiac arrhythmia is atrial fibrillation (AF) [2]. AF occurs when the atrium exhibits rapid and irregular contractions. AF is often undiagnosed, but increases the risk of stroke and heart failure by up to nine times [2]. Another example of arrhythmia is premature ventricular contraction (PVC). PVC’s can be the symptom of an underlying CVD such as cardiomyopathy. Both AF and PVC can be identified using continuous heartbeat timing monitoring [3]. The electrocardiogram (ECG) is a non-invasive surface measurement of the heart’s electrical potentials and is a primary tool for the assessment of cardiac health. Traditionally, the topology for an ECG heartbeat detection circuit consists of a low noise instrumentation amplifier (IA), an anti-alias filter, an ADC, and a digital processor [4] [5] [6]. This topology is shown in Fig. 1(a) along with a labeled ECG in Fig. 1(c). In this conventional topology, the IA amplifies the differential ECG signal with low noise op amps. The gain of the IA is set so that the amplified output is not saturated. After the anti-alias filter, the ADC uniformly quantizes the ECG signal, treating small features such as the ECG’s P-wave and large C D. He and C. G. Sodini are with the Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, 02139 USA (e-mail: david.he@alum.mit.edu; sodini@mit.edu). Manuscript received September 16, 2014. features such as the ECG’s R-wave with equal resolution. The ADC is usually implemented with a medium resolution SAR architecture to minimize power consumption. Finally, to detect heartbeats, the digitized ECG is processed using an algorithm to detect R-waves. Depending on the computational power available, such an algorithm ranges from simple thresholding to wavelet transforms. Even with a deep subthreshold digital processor such as in [6], the digital R-wave detection algorithm can consume three times higher power than the analog front end. The traditional topology is necessary for clinical ECG measurements, where multi-lead ECG signals are acquired with high fidelity in order to diagnose arrhythmias. These recordings are usually quantized with at least 12 bits to preserve P-wave details [7]. The American Heart Association recommends a sampling frequency of at least 150Sa/s to capture all features, while stating that a bandwidth of 1Hz to 30Hz generally produces a stable ECG without artifacts [8]. However, as mentioned, common arrhythmias can be detected with heartbeat timing monitoring where only the Rwave timing is needed. To take advantage of this fact, a new topology is presented that removes the need for the ADC and the signal processor to decrease the overall circuit’s complexity, power, and area. The demonstrated ASIC receives the ECG signal as an analog input and outputs a digital heartbeat signal, while being tolerant to signal interferers such as motion artifacts. This paper is organized into the following sections. Section II explains how the proposed topology operates. Section III discusses each circuit block in detail. In Section IV, measured results from both testbench and human subject tests are presented. Furthermore, a method to accurately extract Rwave timings from the ASIC output is validated using clinical data. II. P ROPOSED C IRCUIT T OPOLOGY The proposed topology is based on the fact that heartbeat detection relies on the ECG’s QRS complex, which has a higher frequency content and a greater magnitude than the adjacent ECG features. This circuit topology is shown in Fig. 1(b). In Fig. 1(b), the differential ECG signal is first amplified by a low noise programmable gain amplifier (PGA). The PGA’s output signal is split into two paths. The first path goes through the “QRS Amp,” which has a bandwidth that 1µ/5µ Cin = 12pF C M8 BIAS PGA 1µ/5µ+ out Ctank VDD VDD in ECG AV Rp IEEE TRANSACTIONS ON BIOMEDICALC CIRCUITS AND SYSTEMS Bank: f Electrodes VPGA + CVDD 20fF ~ 1.28pF Reset Cin preserves the QRS complex. The second path goes through Rp CV f Bank: CM the “Baseline Amp,” which an equal gain but a lower 20fF ~has 1.28pF Reset Gnd Vbaseline CM bandwidth to preserve only the low frequency drift caused by motion artifacts. VCM Then, a positive inline DC offset VCMadaptive threshold Gnd an VDC is added to VBaseline to create VBaseline+DC . A QRS complex (or heartbeat) occurs whenever VQRS > VBaseline+DC . This comparison is performed by a comparator, which consequently pulses a high DOU T when a heartbeat is detected. ECG Electrodes ECG Electrodes Processor for Heartbeat Processor Detection ADC IA Anti-alias IA ADC (a) ECG ECG PGA Electrodes PGA Electrodes VQRS QRS VQRS Amp VDC V V + + VDC V + Amp DOUT DOUT V Baseline Baseline Baseline+DC Baseline+DC BaselineBaseline Amp + Ground Ground Electrode Electrode (Optional) (Optional) Circuit gnd QRS Amp - CGnd 2 Vout M5 VDD M4 M6 rate range or when DOU T becomes irregularly spaced. Once M5 routine can be rerun to update detected,Cthe +-initial calibration V M4 M6 M3 Gnd VCDC . If the irregularCD OU T is caused by actual irregular RVDD Gnd waves, then the recalibration will be unable to complete, in which case Gnd arrhythmiaGnd can be implied. There are several advantages to thisVBaseline+DC topology in terms Φb 1 of circuit design. First, no signal processor or ADC is reC 2.9pF Φ reduces Φ significantly quired, which the device’s power and VDD Φb Φb C + V area. Second, a low voltage supply is possible because a 2.9pF clipped R-wave that exceeds the amplifier’s output range still Digital Outputs Φb Φ C Bank: heartbeat C Bank: Third, any comparator offset possesses information. 15fF ~ 155fF 40fF ~ 5.1pF is automatically compensated due to the VDC calibration. Fourth, amplifier linearity is unimportant because the signal VBaseline Gnd path is highly nonlinear. In terms of practical usage, this topology is tolerant to 40fF motion artifacts because the signal is QRS differentially Amp compared against its own baseline. Furthermore, no predefined 960fF subject-dependent parameters are needed. M3 Gnd VBaseline Gnd VDC CC = 1.9pF DC tank VDC DC Gnd 1µ/5µ 1µ/5µ VDD - - Gnd VQRS AV + VDD M7 VBIAS M8 III. C IRCUIT D ESIGN Microcontroller: Microcontroller: VDC calibration Circuit gnd CC = 560fF A. Programmable Gain Amplifier VDC calibration VPGA Vin_n M1 Vin_p M2 Baseline 40fF PGA’sAmp function is Vout VDD CC The to amplify the ECG directly from the M5 M4 M6 electrodes with960fFminimal circuit noise and M3power while having a range of gain to adapt to various ECG amplitudes. Fig. 2 Gnd Gnd A VBaseline shows the schematic +of the PGA, which consists of an op amp 15pF in the differenceC =configuration. (b) 1µ/5µ 1µ/5µ 0.8 Amp Outputs [V] Vin_p VDD Digital Outputs for Heartbeat Detection Anti-alias CC = 1.9pF + CVDC M1 - VDC M2 Vin_n R 0.6 V VQRS QRS V V VBaseline Baseline QRS Complex C V VBaseline+DC Baseline+DC 0.4 Cf Bank: 20fF ~ 1.28pF VCM 0.2 VDC 1µ/5µ VBIAS 1µ/5µ VDD M7 M8 - ECG Electrodes 1 VDD Rp > 10TΩ Cin = 12pF Q S 0 DOUT [Digital] T P Reset AV + Vin_n M1 VPGA Vin_p M2 Vout VDD Cin CC = 1.9pF Rp Cf Bank: M5 20fF ~ 1.28pF Reset M3 M4 M6 VCM 0 0 Gnd VCM 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 Gnd 2 Time [s] Fig. 2. The PGA schematic. (c) Fig. 1. a) The traditional topology for ECG heartbeat detection, b) the proposed topology with voltage nodes labeled, and c) an ECG waveform illustrating the QRS complex, baseline, baseline with VDC offset, and digital output. IA Processor for Heartbeat Detection ECG Electrodes PGA ADC Anti-alias Ground Electrode (Optional) QRS Amp Baseline Amp Circuit gnd Digital Outputs VQRS VBaseline VDC - + To correctly set VDC , it is incremented until the period between DOU T pulses is regular and is in the range of human beat-to-beat interval. As shown in Fig. 1(c), there is a wide range of valid VDC values since VDC can be set at any level between the R-wave and the next highest amplitude feature (usually the T-wave). Because respiration causes slight baseline modulation of the ECG, we use four respiratory cycles to complete the VDC calibration routine, which takes 20 seconds on average. This calibration is performed at the beginning of measurement by an external microcontroller that consumes 5µA at a clock frequency of 4kHz, which is powered off afterwards. During measurement, VDC may need to be recalibrated if the measurement condition changes significantly due to motion artifacts or muscle noise. The need to recalibrate VDC can be detected in real time when DOU T exceeds the human heart 1.8mm Sensing a biopotential such as the ECG creates several circuit requirements. First, because the ECG amplitudes vary between different body locations and different subjects by up + to two orders of magnitude, an adjustable gain is required. The gain of the PGA is set by Cin /Cf , where Cin = 12pF and Cf is implemented as a 6-bit binary weighted capacitor bank of 20f F to 1.28pF to adjust the PGA gain from 19dB to 56dB. Second, the AgCl electrode’s half-cell potential generates approximately 200mV of near-DC electrode offset voltage (EOV) which would saturate the amplifier if not removed. To filter this EOV, PMOS pseudo-resistors (Rp ) are used [9]. The Rp ’s are greater than 10T Ω but only occupy 10µm2 , thus enabling on-die sub-Hz high pass filters and effectively removing the EOV. The large Rp also allows the DC biasing of the amplifier inputs while maintaining a high input impedance, which is needed due to the capacitive Cin . Furthermore, because the input impedance is significantly larger than Relec ≈ 300kΩ, any differential voltage caused by unequal and varying Relec (such as during motion) is negligible. ECG Electrodes DOUT VBaseline+DC Microcontroller: VDC calibration Voltage Reference m PGA, QRS Amp, and Baseline Amp Current Reference VDC Comparator M3 + ΦCVDC - CVDD VBaseline+DC Vout_p M4 VDC VL VR M1 M2 SR Latch CGnd V QRS IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS 3 Gnd Φ Gnd It should be noted that the high impedance at the PGA input nodes leads to long start-up settling times. As a solution, reset switches shown in Fig. 2 are added to the PGA inputs to immediately shunt the input nodes to their final common-mode DC voltage VCM during start-up. The PGA’s op amp is a two-stage Miller-compensated op amp. This topology is chosen because of its compatibility with low voltage supply, wide output swing, and self-biasing. Due to the low frequency and bandwidth requirements of ECG signals (1Hz − 25Hz), the PGA can operate in deep subthreshold with 90nA of bias current. The low gm leads to a greater thermal noise spectral density, but the thermal noise contribution is limited because of the PGA’s low bandwidth. At this frequency, the dominant noise source is 1/f noise. Chopper modulation at the PGA inputs is a possible method to eliminate 1/f noise. However, chopper switches introduce a current path between the PGA inputs. If there is any input offset voltage, then an offset current would exist that can saturate the PGA through the high resistance feedback Rp . A solution is to use a GM − C servo-loop to provide a current path, but it consumes additional current [10]. Without chopping, the input 1/f noise can be designed to be within 1µVrms (0.5Hz − 50Hz) by appropriate transistor sizing, which is acceptable for ECG signals that are typically at 1mV . For these reasons, chopper modulation is not used. The input-referred 1/f noise spectral density for this op amp is shown in Equation (1), where (gm3 /gm1 )2 = 1 when in subthreshold [11]: 2 2 vif 2 · K1 gm3 2 · K3 sub = + (1) · 2 2 f ∆f W1 L1 Cox f gm1 W3 L3 Cox tank VDC DC VDD Gnd QRS Amp Gnd 40fF 1µ/5µ 1µ/5µ VTop 960fF - VTop Gnd VPGA VDD Flipb Baseline + V - DC Amp 40fF Vin_n M1 VBaseline Gnd M16 M15 VTop VBot M6 VDD + CC = 15pF M13 VL M14 M11 Vout_p C Bank: ~ 1.28pF Fig. 3. The QRS Amp and the20fFBaseline Amp schematic. V M9 M5 f CM 1 Rp > 10TΩ VR M12 M8 M7 Vout_n Reset Flipb M4 M3 AV Vout CC M5 Flipb Gnd Vin_p M2 DD 1µ/5µ 1µ/5µ 960fF VBot M8 ΦVb Reversed + - VDC CVDC VDD M7 VBIAS CC = 560fF CVDC VBot VQRS AV + VBaseline+DC V Vout_n M6 M10 VDD DD Gnd M7 V M8 Both and Baseline of CtankAmps have a Vfixed gain VDDC QRS = 12pF ECGF/40f F = 28dB,A thus resulting 960f in an overall gain V V M1 M2 Φ V Electrodes V range of 47dB to+ 84dB.+ At this overall gainV range and with V C C V V V VDC DC R Bank: VCDD = 0.8V , Cthe can be usedM5to measure - full dynamic CGndrange M3 VDD V Reset ECG signalsV at various wearable locations onΦ M4 the body M6 where Gnd V Gnd Gnd3mV the ECG ranges from approximately 30µV to . pp pp VBaseline Gnd Gnd 1µ/5µ BIAS 1µ/5µ DD in in_n V M3 in_p L DD R PGA in M2 M1 Baseline+DC p f M4 Vout_p out SR Latch CC = 1.9pF QRS 20fF ~ 1.28pF DD M16 M15 CM M13 VL M11 CM M14 M8 M7 Vout_n VR M12 Vout_p Vout_n DOUT + C. VDC Generator CVDC VDC M9 M6 M10 M5 - Gnd Processor for Heartbeat Detection Φb Φb Φb Ileak ADC IA Anti-aliasDD Φ VBaseline+DC . Gnd M4 VQRS QRS M1 Amp Ground Electrode (Optional) Vout_p The VDC M2 Baseline Amp Φ VBaseline Gnd QRS VDC - DOUT VBaseline+DC Gnd Circuit gnd - Φb Microcontroller: VDC calibration Φb Φb VDD VA Φb VM Φ VA Ileak Φb 1 R L ECG PGA Baseline+DC Electrodes Φ Digital Outputs to produce an adaptive threshold Φ V V SR Latch generator schematic V + is shown in Fig. 4. V M3 VB CVDC 2.9pF Φ Gnd Φ Φ+ - Ileak V B VDC Φ Φb VBaseline+DC V V 1 VTop Ctank VDD 2.9pF Bot CVDC + - VDC Flipb + V - InDC CVDC Out Top Φb CVDD Bank: 15fF ~ 155fF Φ VTop VTop Flipb VBot CGnd Bank: 40fF ~ 5.1pF VBot VTop VBot Flipb VBaseline C CVDC VDC + - VDC 1 Φb Gnd Reversed Flipb VDD QRS VTop VBot Amp 960fF Ctank Gnd VDD CVDD Gnd CVDC VPGA CVDC Gnd VBaseline+DC 1µ/5µ 1µ/5µ + - VDC CVDC CVDD VBaseline CGnd Gnd VDD + V - DC VQRSCVDC AV + + - VDC VBaseline 1 40fF M7 VBIAS CVDD CGnd CC = 560fF CGnd Vin_n M1 Gnd Gnd Baseline (a) + V Amp - 40fF (b) Φb CVDD CGnd in a) clock phase Φb and b) clock phase Φ. Fig. 5. The VDC generator M3 1µ/5µ 1µ/5µ VDD 960fF Φb Gnd Φb + VBaseline AV + V - DC Φ VDD CM5 tank M4 2.9pF Φb Gnd VBaseline+DC 1 Ctank Φ CVDC 2.9pF Vin_p M2 DC Gnd VBaseline+DC Ctank Flipb Fig. 4. The VDC generator schematic. B. QRS and Baseline Amplifiers Revers 1 Gnd + V - DC Ileak VM VA VA VB Φ The VDCV generator’s function CVDD CGnd is to add VDC to VBaseline ECG Electrodes VBot The PGA’s output is connected to the inputs of the QRS and Baseline Amps. The function of the QRS Amp is to amplify the ECG signal with a bandwidth that passes the QRS complex. Meanwhile, the Baseline Amp has the same gain but has a lower bandwidth that only passes the baseline signal. In Fig. 3, both amplifiers use identical two-stage Millercompensated op amps in the non-inverting configuration. The only difference is in the compensation capacitors (CC ). The 1 Gnd Baseline + According to Equation (1), several design choices are made to minimize 1/f noise. First, PMOS input transistors are used because they offer lower noise coefficients than NMOS transistors: K1 = Kp < Kn . Second, increasing W1 and L1 will reduce the noise contribution of the input transistors. However, excessive input transistor area will introduce significant parasitic capacitance at the drain of M2. This decreases the frequency of the second pole and lowers the phase margin. A dimension of 864µm/1.5µm (96 fingers of 9µm/1.5µm) is chosen so that M1 and M2’s 1/f noise contributes to 40% of total input noise. Third, increasing W3 and L3 will reduce the noise contribution of the mirror transistors. However, signal swing places an upper limit on W3 and process technology places an upper limit on L3 . A dimension of 100µm/20µm (8 fingers of 12.5µm/20µm) is chosen so that M3 and M4’s 1/f noise contributes to 20% of total input noise. VBaseline+DC Φ Miller multiplied CC and ba 0.5nA 1bias current create very C low while being 2.9pF area-efficient. For the QRS Φ Φ VDD corner frequencies Φ Φb b C 560f + F sets the Φ Amp, CC =2.9pF low passΦbcorner frequency at b V Ileak V VM For the B 25Hz, Φwhich passes theVQRS complex. Baseline Amp, b A Ileak VDD Φ Φ b CVCC =Bank: 15pF sets the low pass corner frequency at 1Hz, which C Bank: VB A ~ 155fF 15fF 40fF ~ 5.1pF Φ Φ only passes the baseline drift. Pseudo-resistors are usedOut to biasIn Φ the inverting node. V Gnd CVDD Bank: Φb Φ CGnd Bank: C IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS 4 CV DD is a 4-bit binary weighted capacitor bank of 15f F to 155f F , and CGnd is a 7-bit binary weighted capacitor bank of 40f F to 5.1pF . CV DD and CGnd values are selected during the initial VDC calibration by the microcontroller. Non-overlapping clock phases Φ and Φb are generated onchip at 2.0kHz by a clock generator. The clock frequency is chosen as a compromise between low power (favors lower frequency) and low charge leakage (favors higher frequency). During clock phase Φb (Fig. 5(a)), CV DD and CGnd are V respectively reset M15 M16 to VDD and ground. During the following clock phase Φ (Fig. 5(b)), CV DC is charged to a final voltage M13 M14 V V M11 M12 of VDC = VM7DD CV M8DD /(CV DD +CGnd ). During the following V V clock phase Φb , VVDC is added to VBaseline to produce D M6 M10 M9 M5 VBaseline+DC , while CV DD and CGnd are again reset. Ctank Gnd is present to reduce voltage ripples. With the selectable ranges V of CV DD and CGnd , VDC can be adjusted from 0% to 80% of V M3 M4 Φ VDD . This range covers most situations where the interferer V V SR Latch or noise occupies to 80% of VDD while having a lower M2 up V M1 V amplitude than the R-wave. Φ In consideration Gnd for long term at-home usage where the ECG electrodes are applied by the wearer, the VDC generator has the ability to generate negative VΦDC if the user accidentally Φb b Ileak V V Bby the two digital M reversesΦthe electrodes. This is symbolized b VA Ileak VDD blocks in Fig. 4 that can flip C during phase Φb . In the V VA VB Φ V DC Φ In then the Out case thatΦ the ECG is reversed and CV DC is flipped, M15 M16 Gnd heartbeat M13 occurs whenM14DOU T = 01 instead of DOU T = 1. V TheseV digital blocksM8are M11 M12 expanded in Fig. 6(a).Gnd M7 DD R L out_n out_p out_n OUT DD out_p L R QRS Baseline+DC Ileak by reducing the |VDS | of the switch closest to the capacitor. All switch and buffer transistors are minimally sized (PMOS: 400nm/180nm, NMOS: 220nm/180nm) to reduce the effect of charge injection. D. Comparator The comparator’s role is to output a digital pulse when a QRS complex has occurred, which is when VQRS > VBaseline+DC . A dynamic latched comparator based on [13] is used (Fig. 7). The dynamic topology is chosen because it consumes power only when latching. This topology offers the additional benefit of only using a single clock signal Φ, thus placing no requirements on Φb timing. M11 and M12 are added to reduce short circuit currents through M13-M16 when VL and VR are transitioning. This is important because short circuit currents of several nano-amps can be a significant portion of the overall power. VBaseline+DC contains switching transients from the VDC generator. However, these transients are designed to occur with Φb , which do not affect comparator accuracy because comparator latching occurs with Φ. VDD DD M15 M13 VL R L Vout_n M9 Vout_p VBot CVDC + - VDC VTop M11 M14 M8 M7 Vout_n Vout_n VTop M6 M10 M5 M16 M12 VR Vout_p Vout_n DOUT M9 DOUT M6 M10 M5 Gnd Flipb VDD + V - ΦDC CVDC VBaseline+DC M3 M4 VL VR M1 M2 Gnd Φb Vout_p Reversed SR Latch Flipb VQRS VDD Flipb Φ VBot Φ VTop VBaseline+DC VBot M3 Vout_p M4 VL VR M1 M2 SR Latch VQRS Gnd Φ (a) VBaseline+DC VDD Φb Ctank VA Ileak + CVDC VB- VDC VA CVDD CGnd Φ Gnd Gnd VBaseline 1 Φb Φb VM Gnd Ileak V B Fig. 7. The dynamic latched comparator with SR latch. The comparator is based on [13]. VDD Φ Φ Out Φb In 1 Gnd Gnd CVDC + V - DC (b) VBot Fig. 6. V The Top VDC generator’s internal circuit blocks: a) CV DC can be flipped during phase Φb in the case of reversed electrodes, and b) the low leakage Gnd Flipb capacitor discharge [12]. switch implementation to prevent Φb + VBaseline+DC +Φ Flipb CVDC V CVDC - VbDC 1 - DCthe switching Because frequency isReversed only 2.0kHz and VGnd Top C CVDD Ctank 2.9pF Φ Φ , a leakage current CV DC of only 5.8pA can reduce VDD = 2.9pF Φb Flipb Φb C + VDC by 1mV between V clock cycles. To reduce switch leakage, 2.9pF VBot stacked switches with aVTop push-pull buffer are implemented VBot Φ Φ based on [12]. The switch schematic is shown in Fig. 6(b) and b C Bank: C Bank: 15fF ~ 155fF 40fF4. ~ 5.1pF is used for all switches in Fig. The two stacked switches VBaseline+DC in Fig. 6(b) exponentially reduce1 the subthreshold Ileak by VBaseline Gnd Ctank VDD the decreasing |VGS | of the two switches. The push-pull buffer drives VM to the same voltage as VB , thus further decreasing VDC DC VDD CVDD Gnd QRS + CVDC Amp - VDC Out producesΦan input-referred comparator offset range of −13mV Gnd to 16mV . However, as mentioned in Section1II, no comparator offset compensation is needed due to the VDC calibration Gnd routine. The final output of the SR latch, DOU T , is a digital signal that pulses when a heartbeat is detected. VTop VBot VTop E. Peripheral Circuits Flipb All peripheral circuits and passive components are impleΦb current +on-chip. These circuits include mented a fast startup + CVDC V CVDC - VDC Reversed - DC reference for the amplifiers based on [14], a diode ladder voltage reference to generate the common-mode voltage for Flipb the PGA, and a clock generator that provides the 2.0kHz VBot non-overlapping clock signals for the VDC generator and the VTop VBot comparator. CGnd 1µ/5µ 1µ/5µ VBaseline Gnd VM 40fF 960fF Gnd Φb Ileak V B V A I M1-M4 gate lengths are set at 1µm to reduce geometry VDD leak VA VB mismatch. A Monte Carlo mismatch of 100 runs Φ simulation Φ Φb Gnd A V VDD V VDD 1 VBaseline+DC In Flipb 5 IV. M EASUREMENT R ESULTS The ASIC is fabricated using a standard TSMC 0.18µm 1P6M CMOS technology. The die area is 1.8mm × 1.8mm with an active area of 0.76mm2 as shown in Fig. 8. R Amp Outputs [V] 0.6 Total Gain 90 V VQRS QRS V VBaseline Baseline QRS Complex 80 V VBaseline+DC Baseline+DC Bandwidth 0.4 0.2 70 Q S 0 1 0 0 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 Total Gain [dB] DOUT [Digital] VDC T P 2 Time [s] 1.8mm 50 40 Voltage Reference PGA, QRS Amp, and Baseline Amp -6 10 60 Input-referred Noise 30 Current Reference Input-referred Noise [V/(Hz)1/2] 0.8 100 1.8mm 20 Comparator Clock Gen. VDC Gen. 10 -7 0 10 Config. Registers 1 10 Frequency [Hz] 2 10 10 3 10 Test Blocks Fig. 9. The measured PGA-QRS Amp signal path’s gain response and noise response. 0.8 Total Gain -7 10 0 1 10 10 3 10 2 10 Frequency [Hz] 10 VBaseline+DC VQRS 0.8 0.8 0.7 Amp Outputs [V] Amp Outputs [V] 0.7 0.6 0.6 A. Testbench Measurements The ECG’s amplification path goes through the PGA and then the QRS Amp. Fig. 9 shows the gain response and inputreferred noise response at the highest gain setting. In the gain response, the plot shows the sub-Hz high pass corner enabled by the PGA and QRS Amp’s pseudo-resistors, the low pass corner implemented by the QRS Amp’s low gm and large Cc , and the 40dB/dec falloff at higher frequencies due to the two poles from the PGA and the QRS Amp. In terms of noise response, 1/f characteristic below 10Hz √ the circuit exhibits a √ (or 1/ f when plotted as V / Hz). 0.5 0.4 0.3 0.5 0.4 0.3 0.2 0.2 0.1 0.1 [V] 0 0.8 OUT 0.8 D DOUT [V] 0 0 0.80 2 4 6 8 0 0.80 10 Time [s] 8 10 2 22 4 6 4 4 Time [s] 6 6 Time[s][s] Time 8 88 0.8 0 0 Amp Outputs [V] [V] Amp Outputs [V] OUT D 6 66 8 88 10 1010 VBaseline+DC VQRS 4 6 8 10 6 8 10 6 8 10 0.4 0.4 0.8 0.3 0.2 0 0.10 DOUT [V] 2 Time [s] Time[s][s] Time 2 4 Time [s] 0.8 0.8 0 0 0.7 10 Amp Outputs [V] Time [s] 2 4 Time [s] 0.6 0.5 0.4 0.3 0.2 0.1 0 2 4 0.80 0.8 0 0.8 2 4 6 8 10 6 8 10 0 0.8 000 00 0.7 2 22 4 6 4 4 Time [s] 6 6 Time[s][s] Time Time [s] 0.8 0 0 2 Time [s] 4 6 8 10 Time [s] VBaseline+DC VQRS 8 88 10 1010 0.6 0.5 0.4 TABLE I S IMULATED VS . MEASURED RESULTS FROM THE PGA-QRS A MP SIGNAL PATH . 0.3 0.2 0.1 0 2 4 6 8 0.8 0 0 10 2 4 Time [s] 6 8 10 Time [s] Parameter Programmable gain range Passband Unity-gain bandwidth Input-referred noise (in band) CMRR PSRR Current consumption (at 0.8 V) Simulated 47 dB – 84 dB Measured 47 dB – 88 dB 0.52 Hz – 51 Hz 6.4 kHz 0.99 µV rms 0.50 Hz – 22 Hz 2.9 kHz 2.7 µV rms 3mm x 3mm QFN-16 ECG ASIC ECG Electrode 2 ECG Electrode 1 1 VQRS VBaseline+DC VQRS 0.6 0.4 0.2 0 0.5 0 10 15 20 25 30 5 10 15 20 25 30 5 10 15 20 25 30 35 40 45 0.4 0.3 40 45 0.1 19 19.1 19.2 19 19.1 19.2 19 19.1 19.2 1 35 0.5 0.5 0 Midpoint Timing 1 1 Manual Estimated 0 Time [s] 0.6 0.5 0.2 5 1 0.5 VBaseline+DC 0.7 0.8 Amp Outputs [V] 0 0.6 0.8 0 0.5 0 0.7 0.4 4 44 DOUT [V] 0.1 2 22 DOUT [V] 0.3 10 8 0.3 0.8 0.2 0.7 0.1 0.6 0 0.5 0 0 000 0.8 0.80 0 0.7 10 1010 0.5 0.4 8 6 Time [s] 0.5 DOUT [V] 6 Time [s] 0.6 0.2 DOUT [V] 4 6 Time [s] 0.6 0.3 0.8 0.8 0.8 0.5 0.2 0.7 0.7 0.7 0.4 0.1 0.6 0.6 0.6 0.3 0.50 0.5 0.5 0.2 0.4 0.4 0.8 0.4 0.1 0.3 0.3 0.3 0 0.2 0.2 0.2 0 0.10 0.8 0.1 0.1 0 00 Amp Outputs [V] Amp Outputs [V] 0 0.8 000 00 0.7 2 4 R-waves [V] DAmp [V][V] Outputs Outputs Amp OUT Outputs [V] Amp [V][V] DOUT DOUT [V] DOUT 0.8 0.8 0.8 10 1010 2 [V] D OUT Amp Outputs [V] DOUT [V] [V][V] Outputs Amp Outputs Amp Amp [V] Outputs [V] Amp Outputs 0.5 0.4 8 88 4 0.6 0 [V][V] D DOUT DOUT [V] [V] DOUT OUT 0.6 0.3 0.8 0.8 0.8 0.2 0.7 0.7 0.7 0.1 0.6 0.6 0.6 0.50 0.5 0.5 0.4 0.4 0.4 0.8 0.3 0.3 0.3 0.2 0.2 0.2 0 0.10 0.1 0.1 0 00 4 6 4 4 Time [s] 6 6 Time[s][s] Time DOUT [V] Amp Outputs [V] 0.7 2 22 VBaseline+DC VQRS 0.6 0.6 0.3 0.8 0.5 0.5 0.5 0.2 0.7 0.4 0.4 0.4 0.1 0.6 0.3 0.3 0.3 0 0.5 0.2 0.2 0.2 0.4 0.1 0.8 0.1 0.1 0.30 00 0.2 0.800 0.1 0.8 0.8 Amp Outputs [V] 0 000 0.8 00 2 0.7 0.6 0.8 0.8 0.8 0.5 0.7 0.7 0.7 0.4 0.6 R-waves [V][V] Outputs Amp Outputs Amp Amp Outputs [V] [V][V] DOUT DOUT [V] DOUT 0.8 0.8 0.8 D D [V][V] [V][V] Outputs Amp OUT Outputs Amp [V] D DOUT Outputs [V] Amp [V]Outputs OUT Amp [V]Outputs [V] Amp OUT 0.7 0.8 0.8 0.8 0.7 0.7 0.7 0.6 0.6 0.6 0.5 0.5 0.5 0.4 0.4 0.4 0.3 0.3 0.3 0.2 0.2 0.2 0.1 0.1 0.1 0 00 35 40 45 0 Time [s] 78 dB 53 dB 92 nA 0.7 Table II lists the power consumption of each circuit block at VDD = 0.60.8V . 87% of the total power is allocated to the PGA due to bandwidth and thermal noise considerations. 0.5 circuits consume 8.6% of the total power. The The peripheral ECG ASIC’s 0.4 elimination of the ADC and the signal processor enables it to reduce power consumption. Another portion of the power0.3 saving is contributed by the PGA’s low bandwidth. A further source of power saving is the ECG ASIC’s low VDD , 0.2 which is enabled by its tolerance to signal clipping. 0.1 66 dB 61 dB 64 nA Table I compares the simulated and measured results from the PGA-QRS Amp signal path. Increasing the transistor bias currents did not appreciably decrease the input-referred noise, which indicates that the in-band noise is 1/f dominated as Fig. 9 indicates. Because of this, the actual PGA’s bias current is lowered compared to simulation, and the reduced low pass frequency of 22Hz remains sufficient to preserve the ECG’s QRS complex. The measured input-referred noise is greater than the simulated noise by 2.7 times, which is likely attributed to differences between the transistor model’s and the actual transistor’s 1/f characteristics. The measured level of noise is compatible with sensing the ECG, where the QRS amplitude is typically 1mVpp . 6 4 8 10 4 4 Time [s] 6 6 88 1010 Time[s][s] Time TABLE II S IMULATED0VS . MEASURED POWER CONSUMPTION OF EACH CIRCUIT BLOCK AT VDD = 0.8V . DOUT [V] Input-referred Noise 30 20 Circuit0.8 block PGA QRS Amp Baseline 0Amp 0.80 VDC generator Comparator Current0.7 reference Voltage reference 0.6 Clock 0.8 generator Total 0.8 0.8 D D [V][V] [V][V] Outputs Amp OUT Outputs Amp [V] D DOUT Outputs [V] Amp [V]Outputs OUT Amp [V]Outputs [V] Amp OUT Total Gain [dB] -6 10 50 40 Simulated Power (nW) 72.8 0.5 0.5 1.62 0.3 2.2 2.2 2.0 82.0 Measured Power (nW) 50.4 0.7 0.7 4 0.8 0.4 Time [s] 1.8 1.0 2.2 58.0 6 0.5 0.7 0.7 0.7 0.4 0.6 B. ECG Measurements 0.6 0.6 0.3 0.8 0.5 Fig. 10(a) to 10(d) show measured ECG and digital outputs 0.5 0.5 0.2 from various 0.7 0.4 wearable ECG scenarios to demonstrate the 0.4 0.4 ASIC’s robustness in the presence of baseline drift, muscle 0.1 0.6 0.3 attenuated signal. artifacts, and 0.3 0.3 0 In Fig. 10(a), 0.5 0.2 the at-rest chest ECG offers 1.8mVpp of stable signal. Here, 0.2VDC is set to 0.3V so that VBaseline+DC is 0.2 approximately 0.4 0.1 half of the VQRS amplitude. However, any VDC 0.8 0.1 0.1V and 0.65V would produce the correct 0.1 setting between 0.3 digital QRS 0output at DOU T . 00 In Fig. 0.2 10(b), the chest ECG contains significant baseline 0 drift due to motion. Despite the baseline drift, the same VDC 0.8 0 2 4 6 0.8 0.8 setting as0.1 in Fig. 10(a) results in a correct DOUTime fact, T . In[s] any VDC setting between 0.1V − 0.5V would be valid. This 0 demonstrates the ASIC’s tolerance to motion artifacts because its adaptive 0threshold VBaseline+DC tracks the 2 4 baseline drift.6 000 0.8 0 2 4 0 2 4 66 0.8 Time [s] 0.7 Time[s][s] Time [V] Bandwidth 60 OUT 80 70 Input-referred Noise [V/(Hz)1/2] 90 VQRS Amp Outputs [V] 100 Fig. 8. Die micrograph of the ECG ASIC with the circuit blocks labeled. ] 2 22 IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS VQRS 0.2 4 0.1 6 4 Time [s] [s] Time 6 4 444 6 666 10 10 8 8 888 10 10 10 10 Time [s] Time[s] [s] Time Time [s] 0 444 4Time [s] 2 22 2 2 2 8 6 66 6 4 Time 4Time [s][s] [s]6 6 Time TimeTime [s] [s] 2 22 4 6 4 4 Time [s] 6 6 Time[s][s] Time 0.8 (c) VBaseline+DC 10 VQRS 8 88 8 8 8 VBaseline+DC VQRS 8 88 10 1010 8 10 4 2 2 222 6 4 Time [s] [s] Time 8 6 4 6 444 Time [s] 666 Time[s] [s] Time Time [s] 10 10 8 4 2 8 888 6 4 8 6 4 0.6 6 2 22 2 2 2 0.5 0.5 0.4 0.4 8 88 8 8 8 0.8 0.8 2 4ECG4 Electrode62 6 TimeTime [s] [s] 2 15 20 25 30 40 20 25 30 35 15 20 25 30 R-waves 1 35 40 VQRS VBaseline+DC VQRS 8 10 DOUT [V] VQRS VBaseline+DC 0.4 O Amp Outp Amp 0.5 0.5 VBaseline+DC 0.7 0.6 0.5 0.4 0.3 0.2 5 10 15 20 25 30 35 40 0.1 45 19 19.1 19.2 1 0.5 0.5 Midpoint Timing VBaseline+DC 19 19.1 19.2 Midpoint Timing 19.2 20 25 30 35 40 0 45 19.1 19.2 19 19.1 19.2 19 19.1 19.2 1 Estimated 0 10 15 20 25 Time [s] 30 35 40 45 0 Time [s] 0.5 0 VQRS 0.4 15 Manual 5 19.1 Fig. 12. DOU T . VBaseline+DC 0.7 0.6 10 Time [s] VBaseline+DC 0.8 5 1 19 0.2 VBaseline+DC 6 0.6 0 0.5 45 Amp Outputs [V] 10 Amp Outputs [V] ECG Electrode 1 10 10 8 0.3 ECG Electrode 2 VQRS 8 4 0.8 10 ECG Electrode 1 4ECG Electrode62 Time [s] 2 1 0.4 3mm x 3mm0 19 40 45 QFN-16 ECG ASIC 1 Estimated Manual Time [s] 2 0.8 0.5 1 0 0 0.3 0.6 0.1 45 0 10 10 10 0.7 DOUT [V] 15 0.5 3mm x 3mm QFN-16 ECG ASIC 0.8 8 8 0.4 0 1 5 DOUT [V] 35 1 0 10 8 VBaseline+DC 1 10 6 6 0.2 0.2 5 4 4 Time [s] Time [s] 0.5 3mm x 3mm QFN-16 ECG ASIC 0.5 0 2 2 1 (d) 0.4 0.1 10 0.6 10 101010 10 10 0.3 0.3 0.2 0.2 10 0.8 0 00 0.70 0 0 10 VQRS 5 8 VQRS 0.2 0.3 6 Time [s] VBaseline+DC 4 6 44 4 Time [s] 6 6 6 4 Time 4Time [s][s] [s]6 6 Time TimeTime [s] [s] 0.6 0.4 4 Time [s] 0.8 0 10 3mm x 3mm While DOU T provides an approximate timing of the ECG QFN-16 ECG ASIC R-wave, an accurate ECG R-wave timing is necessary for several cardiovascular monitoring applications such as the ECG Electrode 2 calculation of heart rate variability for disease prediction. ECG Electrode 1 10 10 8 8 VQRS VQRS 0.5 2 Time [s] 0 0.8 0000.8 0 00 0 00 0.700.70 0.6 0.6 1 10 10 10 10 DOUT [V] [V][V] D DOUT OUT Amp Outputs [V] [V] Outputs Amp [V] DOUT 10 101010 TimeTime [s] [s] 2 ECG Electrode 1 VBaseline+DC VQRS 8 C. Recovering the ECG R-wave Timing from DOU T VBaseline+DC 8 88 8 6 Time [s] 0 2 Amp Outputs [V] 2 4 0.1 0 0 0 0 DOUT [V] Amp Outputs [V] 6 Time [s] 0 0.8 0000 000 0.7 10 10 10 10 4 2 [V] D OUT Outputs Amp [V][V] Outputs Amp DOUT [V][V] DOUT 10 10 0.1 0.1 0 0 2 10 10 0.8 0.8 Fig. 10. a) Measured chest ECG at rest (gain = 52dB), b) measured chest ECG with baseline drift due to motion artifacts (gain = 52dB), c) measured 0 muscle noise and signal clipping (gain = 64dB), and d) chest ECG with 0 2 4 6 8 measured head ECG with high gain due to attenuated Time [s]signal (gain = 84dB). 0.2 0.6 Estimation of the R-wave timing using the midpoint timing of 0.5 0.4 0.3 0.2 0.7 0.4 0.2 0.6 5 10 15 20 25 30 35 40 0.4 0.3 0.1 45 19 19.1 DOUT [V] 5 10 15 20 25 30 35 1 Manual 0 5 10 15 20 25 30 Time [s] 35 40 35 40 0.1 45 19 19.1 19.1 19.2 19.1 19.2 19.2 1 5 10 15 20 5 10 15 20 25 30 25 30 35 40 Midpoint Timing 0.5 0 45 19 19.1 19.2 19 19.1 19.2 1 Estimated Manual 0.5 0 35 40 0.5 45 0 Time [s] Time [s] 0 19 40 3mm 45 x 3mm 1 QFN-16 ECG ASIC Estimated 30 1 Midpoint Timing 0.5 25 3mm x 3mm QFN-16 ECG ASIC 0.5 19.2 1 R-waves 0 20 0.2 1 0.5 15 1 R-waves 0 10 0.5 0 0.5 5 DOUT [V] 0.6 DOUT [V] Amp Outputs [V] Amp Outputs [V] Although the R-wave’s peak is clipped in DOU T , the original R-wave timing can still be recovered with minimal error. As shown by Fig. 12, the R-wave timing can be estimated from the midpoint timing of DOU T pulses. This method is ECG Electrode 2 ECG Electrode 1 tested on normal chest ECG records from ten subjects totaling 2,304 heartbeats from the MIT-BIH PhysioNet database and V V Fig. 11. The wearable ASIC board at the head with wireless data transmission from our MIT clinical test (MIT IRB approval #1104004449). V V to a computer. Midpoint estimated R-wave timings are compared with manually annotated timings, the results of which are summarized In Fig. 10(c), pectoral muscle artifacts are present from in Table III. a rapid horizontal 90◦ arm movement. Also, an intentional high gain of 64dB increases the amplified ECG to 2.8Vpp , TABLE III C OMPARISON BETWEEN MIDPOINT- ESTIMATED R- WAVE TIMINGS AND which is beyond VDD = 0.8V and is clipped. To produce Midpoint Timing MANUALLY ANNOTATED R- WAVE TIMINGS FROM TEN SUBJECTS . the correct DOU T , VDC needs to be increased to 0.5V so that VBaseline+DC rises above VQRS ’s muscle artifacts and Estimated Manual amplified T-waves. The QRS complex’s clipping does not Subject Number Mean Stdev. Sampling of Beats R-wave R-wave Freq. matter because the beat information is still present. This Timing Timing [Hz] scenario is an example of a significant change of measurement Error [ms] Error [ms] condition leading to a new VDC setting. 1 250 0.91 1.6 250 To test the ASIC in the presence of an attenuated ECG 2 183 0.91 1.6 250 signal, we mount it at the head so that the ECG is measured 3 63 0.97 2.2 250 across the ear and the middle upper neck as shown in Fig. 11. 4 123 -1.70 1.6 250 The ECG at this location is in the range of 30µVpp − 40µVpp , 5 73 -2.40 1.8 250 6 467 -1.50 0.71 500 which is two orders of magnitude smaller than the standard 7 363 -1.00 0.71 500 chest ECG. This attenuation is due to the pattern of the ECG 8 357 -2.80 0.72 500 field lines at the head, which yield a very small potential 9 226 -0.88 0.72 500 difference when projected onto the lead. Because of this 10 199 -0.29 0.84 500 attenuation, the head ECG has a poor signal-to-noise ratio and Overall 2,304 -0.70 1.25 only R-waves are immediately visible [15]. 0 0.8 DOUT [V] 0.5 0 19 45 Time [s] ECG Electrode 2 ECG Electrode 1 1 VQRS VBaseline+DC 10 5 10 1 0.5 15 Amp Outputs [V] 20 25 30 35 40 20 25 30 35 40 19.2 Midpoint Timing 19 19.1 19.2 19 19.1 19.2 1 Manual 15 Estimated 20 25 30 35 40 45 0.5 0 0 5 10 15 20 0.5 0.4 0.3 0.2 25 30 35 40 0.1 45 19 19.1 19.2 19 19.1 19.2 19 19.1 19.2 1 DOUT [V] 1 0.5 0 0.6 Time [s] Time [s] DOUT [V] 10 19.1 0.5 0 45 0.2 5 19 1 0.4 Baseline+DC 0.7 Baseline+DC QRS 0.3 0.1 45 0.6 15 0 QRS 0.5 0.4 5 10 15 20 25 30 35 40 0.5 0 45 1 1 R-waves 0 0.6 0.2 DOUT [V] 5 1 0.8 R-waves 0 0.5 Amp Outputs [V] 0.4 0.2 VBaseline+DC 0.7 1 0.6 Amp Outputs [V] VQRS 0.8 R-waves 8 8 8 4 6 44 4 Time [s] 6 6 6 Time Time Time [s][s] [s] 8 8 2 0.8 attenuation, 0.2 0.80 0.8 00.8 0.8 0.8 0.8 101010 10 10 10 10 101010 10 10 VBaseline+DC 6 6 6 6 Time [s] Time [s] Amp Outputs [V] 0.3 4 4 0.1 0 0 VQRS 2 22 2 2 2 DOUT [V] 10 101010 0.4 (b) 6 0 R-waves 8 88 8 VBaseline+DC 8 8 88 8 8 8 VQRS 4 4 Time [s] Time [s] 0.1 10 0 Due0 to 0.3 0.8 0.8 0 0.2 0.70 0.7 0.1 0.6 0.6 0 0.5 0.5 0.4 0.8 0.4 0.3 0.3 0.2 0 0.2 0.10 Amp Outputs [V] 6 66 6 Time Time Time [s][s] [s] VQRS 6 VQRS Time [s] 4 6 2 4 6 2 2 2 [s] 4 46 66 6 4 4 4 Time 2 2 4 46 6 6 Time [s] Time [s][s] [s] Time Time [s] Time [s] Time TimeTime [s] [s] 2 2 0.5 0.8 0.4 DOUT [V] 1010 0.8 0 0.2 0.8 00 0 0.1 0.7 0 0.6 Amp Outputs [V] 88 Time [s] 4 0.2 DOUT [V] 0.5 444 4Time [s] 2 222 0 0.80 0 0.8 0.8 0.80 8 888 2 66 Time[s][s] Time 10 6 2 0 R-waves 2 V 8 Baseline+DC 10 V 6 QRS [V][V] D D [V][V] D [V] [V] D DDOUT OUT O Amp [V] Outputs Outputs Amp OUT [V] [V] Outputs Outputs Amp Amp [V] D [V] D D [V][V] Amp Outputs Outp Amp Amp OUT OUTOUT [V] Outputs Outputs Amp Amp [V] D[V] DOUT D[V] [V][V] [V] D DOUT [V][V] D OUT OUT Amp Amp [V]Outputs [V] Amp Amp [V][V] [V] Outputs Outputs Amp Amp OUT OUTOutputs [V][V]Outputs Outputs Outputs Amp Amp [V] [V] DOUT [V][V]Outputs [V] Amp Amp DOUT OUT OUT [V] Outputs [V] [V] D [V] [V] DAmp DD [V] Outputs [V] Outputs Outputs Outputs Amp Amp OUT OUT OUT Outputs[V][V] AmpOutputs Amp Outputs [V] OUT OUT Outputs Amp Amp [V] [V] DOUT Outputs[V][V] AmpOutputs Amp Outputs [V] Amp [V][V] D DOUT DOUT [V] [V] DOUT OUT Amp Outputs [V] 2 22 2 10 101010 10 10 8 R-waves 10 10 4 4 0.6 4(a) Time [s] 2 22 2 22 8 88 8 8 8 6 Time [s] R-waves 8 10 1010 0 0.8 000444 4Time [s] 666 6 0 40 Time 4Time [s][s] [s]6 6 Time [s] [s] 0.7 TimeTime 4 0.5 0.4 0.4 0.3 0.3 0.8 0.2 0.2 0.7 0.1 0.1 0.6 0 0 0.5 0.8 0.4 0.8 0.3 4 gain is 6increased 8to 84dB to 10 the the Time [s] sense the 30µVpp of ear ECG. At this high gain, a significant portion of the amplified output is noise and R-wave clipping is 0 8 10 2 2.7dB. 4 6 present, leading to an0 SNR of only However, with the Time [s] identical VDC setting as in Fig. 10(a) and 10(b), VBaseline+DC VBaseline+DC is able to rise above the noise and correctly capture the 8 10 heartbeats as shown by DOU T in Fig. 10(d). 88 1010 10 101010 VBaseline+DC VQRS 2 4 DOUT [V] 8 88 2 0.8 0.5 0.5 0.5 0.8 0 0.5 0.2 0.5 0 0.5 0.7 0.4 0.40.4 0.4 0.7 0.1 0.4 0.4 0.6 0.3 0.3 0.3 0.6 0 0.3 0.3 0.3 0.8 0.5 0.2 0.8 0.8 0.8 0.20.2 0.2 0.5 0.2 0.2 0.7 0.4 0.1 0.7 0.8 0.70.1 0.7 0.1 0.1 0.4 0.1 0.1 0.6 0.3 0 0.6 0.6 0.6 00 0 0.3 0.50 0 0.2 0.5 0.5 0.5 0 0.8 0.2 0 0.4 0.1 0.8 0.8 0.8 0.4 0.4 0.8 0.4 0.1 0.8 0.3 0 0.3 0.3 0.3 00 0.2 0000.2 0 0.2 0.8 0.2 00 00.8 00 0.8 0.10 0 0.8 0.10.1 0.7 0.1 0.7 0 0 0.6 0 00.6 0.8 0 0.50 0.5 0.8 0 0.8 0.8 0 0.8 0.7 0.4 0.4 0.6 0.3 0.3 0.8 0.8 0.8 0 0.8 0.5 0.8 0 0.2 0.7 0000.8 00.20 00.7 0.7 0.7 0.4 0.7 0.1 0.7 0.6 0.1 0.60.6 0.6 0.3 0.6 0 0.6 0.5 0 0.50.5 0.5 0.2 0.5 0.5 0.4 0.40.4 0.8 0.4 0.1 0.8 0.4 0.4 0.3 0.3 0.3 0 0.3 0.3 0.3 0.2 0.2 0.2 0 0.2 0.2 0 00.2 0.1 0.8 0.10.10 0.1 0.1 0 0.1 00 0 0 0 10 10 Baseline+DC QRS DOUT [V] 10 10 10 10 VBaseline+DC VQRS Amp Outputs [V] 8 888 2 22 2 2 2 DOUT [V] [V][V] Outputs Amp Outputs Amp Outputs Amp Amp [V][V] [V][V] [V] [V][V] [V] D DOUT DOUT D [V] [V] [V] DD DAmp DD [V] Outputs[V] AmpOutputs [V][V] Outputs Outputs OUT OUT Outputs Outputs [V] Amp Amp OUT [V] DD D [V] [V] [V] D DOUT D [V] Outputs Amp Outputs [V] OUT OUT OUT [V][V] Amp D D [V][V] Amp [V]Outputs [V]Outputs Outputs Amp [V] D OUT OUT OUTOutputs OUT OUT Outputs[V][V] Amp [V] [V][V] Amp Amp OUT OUT [V] Outputs Outputs Amp Amp [V] D Amp [V] DD [V] Outputs Outputs Amp Amp OUT OUT [V] Outputs Outputs Amp Amp [V] D DOUT[V][V] DAmp [V][V] D[V] DOUT DOUT [V]Outputs [V][V] OUT OUT [V] Amp Amp [V]Outputs D [V]Outputs [V] Outputs Amp Amp [V][V] [V][V] Outputs Outputs Amp OUT OUT Outputs Outputs Amp Amp Amp Amp [V] OUT OUT OUT [V] Amp [V] OutputsD[V] [V] Outputs [V] Outputs AmpOutputs Amp Outputs OUT 10 1010 DOUT [V] 8 88 Baseline+DC QRS 0.80 0.8 0 0.8 [V][V] D DOUT [V] [V] DD OUT [V] DOUT OUT OUT 10 1010 0.40.4 0.4 0.7 0.4 0.7 0.4 0.3 0.6 0.30.3 0.3 0.6 0.3 0.6 0.3 0.8 0.2 0.5 0.80.8 0.8 0.2 0.2 0.2 0.5 0.5 0.2 0.2 0.7 0.1 0.7 0.4 0.7 0.7 0.10.1 0.1 0.4 0.4 0.1 0.1 0.6 0 0.6 0.3 0.6 0.6 0 0 0.3 0 0.50 0.30 0.2 0.50.5 0.5 0.8 0.2 0.2 0.4 0.80.8 0.8 0.1 0.40.4 0.4 0.8 0.8 0.1 0.3 0.1 0.30.30 0.3 0 00 0.2 0000.2 0 0.2 0.8 0.2 00 00.8 00 0.100.80 0.8 0.8 0.10.1 0.7 0.1 0.7 0 0 0.6 0 00.6 0.8 0 0.5 0.8 0.8 000 0.8 0.5 0.8 0.70 0 0.80.8 0.8 0.4 0.7 0.7 0.7 0.4 0.6 0.3 0.6 0.6 0.8 0.6 0.3 0.8 0.8 0.8 0.5 0 0.8 0.8 0 0.2 0.5 0.7 0000.5 0.5 0.2 0 0 00.7 0.7 0.7 0.4 0.7 0.7 0.1 0.4 0.4 0.6 0.4 0.1 0.60.6 0.6 0.3 0.6 0.6 0 0.3 0.3 0.5 0.3 0 0.8 0.50.5 0.5 0.2 0.8 0.8 0.5 0.2 0.5 0.2 0.4 0.2 0.7 0.40.4 0.4 0.1 0.8 0.7 0.8 0.4 0.7 0.4 0.1 0.1 0.3 0.1 0.6 0.30.3 0.3 0 0.6 0.3 0.6 0.3 000 0.2 0.5 0.2 0.2 0.2 0.5 0.5 0 0.200.8 0.2 0.1 0.400 0.10.1 0.1 0.8 0.8 0.4 0.8 0.4 0.1 0.1 0 0.3 0 00.3 0 0 0.3 0 0.2 0 0.2 0.8 0.2 0000 0.8 0.80.8 0.8 0.1000 0.8 0.1 0.8 0.1 0.7 0 00 0.6 0 0.8 0.8 0000.8 0 00 00.5 00 0.8 0 0.700.8 0.7 0.4 0.6 0.6 0.3 0.8 0 0.5 0.8 0.8 0.8 0.5 0 00 0.2 0.7 00 0.4 0.7 0.7 0.7 0.4 0.1 0.6 0.3 0.6 0.6 0.6 0.3 0.50 0.2 0.5 0.5 0.5 0.2 0.4 0.1 0.4 0.4 0.8 0.4 0.1 0.3 0 0.3 0.3 0.3 0 0.2 0.2 0.2 0.2 0 0.1 0.8 0.80 0.1 0.1 0.1 0 000 10 3 10 2 10 [V][V] D DOUT [V] [V] DD OUT [V] D OUT OUT OUT DOUT[V][V] DOUT 1 10 Frequency [Hz] Amp Outputs [V] Input-referred Noise Input-referred Noise [V/(Hz)1/2] -6 10 Amp Outputs [V] [V] D OUT Output Amp Outp Amp Amp Output [V][V] Outputs Amp Outputs Amp Amp Outputs [V] Amp Outputs [V] Total Gain [dB] DOUT [V] [V][V] DOUT DOUT [V] DOUT DOUT [V] 0 10 0.5 0.8 0.50.5 0.5 0.8 0.5 0.8 0.5 0.4 0.7 R-waves 6 Bandwidth -7 10 Amp Outputs [V] 6 Total Gain 20 10 DOUT [V] 6 0.7 0.70.7 0.7 0.6 0.60.6 0.6 0.5 100 0.5 0.5 0.5 90 0.4 0.40.4 0.4 80 0.3 0.30.3 70 0.3 0.2 60 0.2 0.2 0.2 50 0.1 0.10.1 0.1 40 0 30 00 0 R-waves 6 0.5 0.7 0.4 0.50 0.70.7 0.7 0.4 0.6 0.3 0.5 0.5 0.60.6 0.6 0.3 0.2 0.8 0.5 0.2 0.50.5 0.5 0.4 0.2 0.7 0.4 0.1 0.40.4 0.4 0.4 0.8 0.1 0.4 0.6 0.3 0 0.3 0.1 0.8 0.3 0.3 0 0.3 0.5 0.2 0.20.2 0.2 IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS 0.8 0.3 0.4 0.3 0.1 0.8 0.10.1 0 0.1 0.3 0 0.2 00 0 0 0.2 2 4 6 8 0.80 0.2 0.2 0.800 0.8 2 4 Time [s] 6 8 0 0.8 0.1 0.80.8 0.8 0.7 Time [s] 2 4 6 8 0.10 0 0.80.8 0 0.6 0 0.80 2 6 0.8 8 10 0.8 0.1 V V V 4 V 0.1 0 0.8 0.8 0.8 0.8 0.8 0.8 0 0 0 2 4 6 8 10 0 2 4 6 8 0.5 0 0 0 0 0.80 00.80 0.80 00.80 [s] 0.7 0.7 22 2 44 4 8 8 8 Time 101010 22 2 44 4 66 6 88 8 Time [s] 6 6 6 0.8 0 Time [s] 0.7 0.7 0.7 0.7 0.7 0.7 Time[s][s] Time 0.4 Time [s] 0.7 0.7 0.7 0.7 Time [s] Time 0.6 0.6 Time Time [s][s] [s] 00 0.60.6 0.60.6 0.6 0.6 0.3 0.6 0.6 0.6 0.6 0 0.5 0 5 10 15 20 25 Time [s] 30 35 40 45 0.5 0 Time [s] 8 IEEE TRANSACTIONS ON BIOMEDICAL CIRCUITS AND SYSTEMS In all ten subjects, the standard deviation of R-wave timing error is less than the sampling period. This demonstrates that the R-wave midpoint estimation method can accurately recover the ECG peak timing information from DOU T . This enables the use of the ECG ASIC for applications beyond heartbeat detection, such as heart rate variability analysis, where accurate R-wave timing is necessary. V. C ONCLUSION An ECG ASIC for wearable heart monitoring is presented that takes advantage of the ECG’s characteristics to extract heartbeat timings in the presence of motion artifacts, muscle noise, signal clipping, and attenuated ECG signals as low as 30µV . Besides heartbeat detection, the R-wave timing is extracted using a midpoint estimation method. R-wave timings can be used for the calculation of predictive cardiovascular parameters such as heart rate variability. Implemented using a standard 0.18µm 1P6M CMOS technology, the ASIC consumes 58nW of power at 0.8V supply and occupies 0.76mm2 of active die area. The ECG ASIC has sufficiently low energy consumption for one year of continuous operation from a 0.7mAh thin-film battery, making it ideal for miniaturized and long term heartbeat monitoring in extremely battery constrained applications such as implantable pacemakers and defibrillators. Furthermore, the ECG ASIC’s power consumption is in range of energy harvesting power sources, thus making batteryless heartbeat monitoring a possibility. 7 [9] R. Harrison and C. Charles, “A low-power low-noise CMOS amplifier for neural recording applications,” Solid-State Circuits, IEEE Journal of, vol. 38, no. 6, pp. 958–965, 2003. [10] N. Verma et al., “A micro-power EEG acquisition SoC with integrated feature extraction processor for a chronic seizure detection system,” Solid-State Circuits, IEEE Journal of, vol. 45, no. 4, pp. 804–816, 2010. [11] D. Johns and K. Martin, Analog Integrated Circuit Design. New York, NY, USA: Wiley, 1996. [12] D. Daly and A. Chandrakasan, “A 6-bit, 0.2V to 0.9V highly digital flash ADC with comparator redundancy,” Solid-State Circuits, IEEE Journal of, vol. 44, no. 11, pp. 3030–3038, 2009. [13] M. Miyahara et al., “A low-noise self-calibrating dynamic comparator for high-speed ADCs,” in IEEE Asian Solid-State Circuits Conference, 2008, pp. 269–272. [14] S. Mandal, S. Arfin, and R. Sarpeshkar, “Fast startup CMOS current references,” in IEEE International Symposium on Circuits and Systems, 2006, p. 4. [15] D. He, E. Winokur, and C. Sodini, “The ear as a location for wearable vital signs monitoring,” in IEEE Engineering in Medicine and Biology Conference, 2010, pp. 6389–6392. David Da He received the B.A.Sc. degree in electrical engineering from the University of Toronto in 2005, and the S.M. and the Ph.D. degrees in electrical engineering from the Massachusetts Institute of Technology, in 2008 and 2013, respectively. Dr. He has worked on a variety of sensors, including a wearable vital signs monitor, an organic thin-film transistor temperature sensor, and industrial wireless condition monitoring sensors. He has served on the technical committee of the IEEE International Conference on Body Sensor Networks. Currently, Dr. He is a co-founder and the Chief Scientific Officer of Quanttus, where he works on new ways for wearable sensors, algorithms, and data insights to transform how we view personal health. ACKNOWLEDGMENT The authors would like to thank Professor Hae-Seung Lee (MIT), Tom O’Dwyer (Analog Devices), and Dr. Michael Coln (Analog Devices) for their valuable assistance. The chip fabrication was generously provided by TSMC. This work was funded by the MIT Medical Electronic Device Realization Center (MEDRC). R EFERENCES [1] P. Heidenreich et al., “Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association,” Circulation, vol. 123, pp. 933–944, 2011. [2] J. Waktare, “Atrial fibrillation,” Circulation, vol. 106, no. 1, pp. 14–16, 2002. [3] J. Chong, D. D. McManus, and K. H. Chon, “Arrhythmia discrimination using a smart phone,” in IEEE Body Sensor Networks Conference, 2013, pp. 223–226. [4] R. Yazicioglu et al., “A 30µW analog signal processor ASIC for biomedical signal monitoring,” in IEEE International Solid-State Circuits Conference Digest of Technical Papers, 2010, pp. 124–125. [5] S. Jocke et al., “A 2.6µW sub-threshold mixed-signal ECG SoC,” in VLSI Circuits, Symposium on, 2009, pp. 60–61. [6] D. Jeon et al., “An implantable 64nW ECG-monitoring mixed-signal SoC for arrhythmia diagnosis,” in IEEE International Solid-State Circuits Conference Digest of Technical Papers, 2014, pp. 416–417. [7] F. Censi et al., “On the resolution of ECG acquisition systems for the reliable analysis of the P-wave,” Physiological Measurement, vol. 33, p. 11, 2012. [8] J. Mason, E. Hancock, and L. Gettes, “Recommendations for the standardization and interpretation of the electrocardiogram. Part I: The electrocardiogram and its technology.” Circulation, vol. 115, pp. 1306– 1324, 2007. Charles G. Sodini received the B.S.E.E. degree from Purdue University, in 1974, and the M.S.E.E. and the Ph.D. degrees from the University of California, Berkeley, in 1981 and 1982, respectively. He was a member of the technical staff at HewlettPackard Laboratories from 1974 to 1982, where he worked on the design of MOS memory. He joined the faculty of the Massachusetts Institute of Technology, in 1983, where he is currently the LeBel Professor of Electrical Engineering. His research interests are focused on medical electronic systems for monitoring and imaging. These systems require state-of-the-art mixed signal integrated circuit and systems with extremely low energy dissipation. He is the co-founder of the Medical Electronic Device Realization Center at MIT. Along with Prof. Roger T. Howe, he is a co-author of an undergraduate text on integrated circuits and devices entitled ”Microelectronics: An Integrated Approach.” He also studied the Hong Kong/South China electronics industry in 1996-97 and has continued to study the globalization of the electronics industry. Dr. Sodini was a co-founder of SMaL Camera Technologies, a leader in imaging technology for consumer digital still cameras and machine vision cameras for automotive applications. He has served on a variety of IEEE Conference Committees, including the International Electron Device Meeting where he was the 1989 General Chairman. He has served on the IEEE Electron Device Society Administrative Committee and was president of the IEEE Solid-State Circuits Society from 2002-2004. He is currently the Chair of the Executive Committee for the VLSI Symposia and a Fellow of the IEEE.