Creating Caring Communities: Putting Mental Health on the Agenda Dr. James Irvine
advertisement

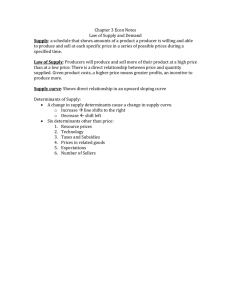
Creating Caring Communities: Putting Mental Health on the Agenda Dr. James Irvine Health Promotion Summer School Prairie Region Health Promotion Research Unit Mental Health Promotion: Identity, Culture and Power August 2005 Mental Health a state of balance between physical, mental, cultural, spiritual and other personal factors, and between the self, others and the environment Sartorius Positive Mental Health A value in its own right; contributes to the individual’s well-being and quality of life; and also contributes to society and the economy by increasing social functioning and social capital. Jané-Llopis E, Barry M, Hosman C, Patel V. Why the interest in mental health promotion? Why the interest from ‘health’? Why the interest from other sectors? Increasing interest in population’s mental health Increasing awareness of mental disorders being common & disabling Economic consequences clearer Links between physical & mental health better appreciated Links between education, labour, justice, etc & mental health more understood Increasing recognition of the link needed between economic & social development Mental Illness Impact Neuropsychiatric disorders account for 13% of Global Burden of Disease; (Moodle and Jenkins) Predictions that by 2020, depression will be the 2nd leading cause of disability in the world; Poor mental health also contributes to poor physical health; One in four persons will develop a mental or behavioural disorder throughout their lifetime. Prevalence ~10% of adults (WHO) Mental Illness Impact 20% of adolescents under the age 18 suffer from developmental, emotional or behavioural problems; 1 in 8 has a mental disorder; from poor communities this increases to 1 in 5. Economic costs substantial 30-40% of workplace sickness absence is attributable to mental disorders (Jenkins) Socio-economic & Life Stress Impact on Physical Health Social Risk Factors Adverse childhood experiences (ACE) Lower childhood socio-economic status Leads to increased: Cardiovascular risk Lipids (cholesterol) Insulin resistance Obesity Dong M et al Circulation 2004; Lawlor, Ebrahim, Smith. BMJ 2002 Mental health status is associated with risk behaviours at all stages of the life cycle. Young people with depression and low selfesteem are linked with smoking, binge drinking, eating disorders and unsafe sex. Vicious circle Links between physical health and mental health are bidirectional Malnourishment in infants – increased risk of cognitive and motor deficits Heart disease and cancer can increase risk of depression Mood disorders can lead to increased risk of injuries, poor physical and role function Learned helplessness, hopelessness and depression associated with decreased immunologic activity and increased risk of tumor growth and infections. Many of the interventions designed to improve mental health will also promote physical health and vice versa. (when mental health promotion is thought of in a broader sense than previously understood) Promoting mental health has the potential to reduce a whole range of risk behaviours and their consequences such as loss of productivity, crime, drop-out from school, disrupted family relationships (Moodle and Jenkins) Similarities in the conditions for different health and social outcomes Same risk factors (low attachment to one’s community, school, family and workplace; parental alcohol and drug use; family conflict; inconsistent parenting; marital instability) and Absence of protective factors Can result in increased crime, drop out from school, increased risk of alcohol abuse, sexual activity, depression and suicide, drug addition What we spend on policing and courts and jails is not available to be spent on affordable housing, school systems, or income security. Feather Mental Well-Being: the foundation of a healthy individual, family & community The Health of the Population Prerequisites peace shelter education food income stable ecosystem sustainable resources social justice and equity Determinants child development working conditions education choices and coping income and social status physical environments health services social support network Social, environmental & economic determinants of mental health Risk Factors Isolation / alienation Lack of education, transport, housing Neighourhood disorganization Peer rejection Poor social circumstances Poor nutrition Poverty Racial injustice / discrimination Violence Work stress Unemployment Access to drugs / alcohol Displacement War Protective Factors Empowerment Positive interpersonal interactions Social participation Social responsibility / tolerance Social services Social support / community network Cultural integration Williams, Saxena, McQueen Societal or community-level characteristics: Culture, Language, Cohesion, Control Aboriginal Youth Suicide by Cultural Continuity Factors Cultural Continuity Factors Cultural Facilities Health Education Land Claims Self-Government 0 Yes No 20 40 60 80 100 120 Suicide Rate / 100,000 Source: Chandler & Lalonde, 1998 140 160 Post-Traumatic Stress Response Popular explanations of health inequities of the Aboriginal communities are limited (its more than health behaviours, more than socio-economic), The enduring impact of colonization and loss of culture are identified as critical health issues – concepts of historical and intergenerational trauma need to be recognized Mental health and social problems linked to social and cultural disruption over the lifespan and across generations Mitchell, Maracle Post-Traumatic Stress Response arises from external trauma and terrifying experiences that break a person’s sense of predictability, vulnerability, and control. Mentally: negative beliefs about themselves and the world, Emotionally: cycles of denial and anxiety Physically: sleep disturbances, anxiety, nightmares, flashbacks Behaviourally: avoidance, isolation, drinking, drugging, increasingly aggressive. PTSR is a useful model for understanding and addressing health inequities: Provides a social / historical context for what has been incorrectly viewed as individual/cultural weaknesses, or illness, Confirms holistic understanding of well-being and cultural renewal Compassionately validates stress responses as appropriate human reaction to trauma; Offers access to proven psycho-educational and therapeutic approaches Points to use of group/community models for collective mourning, support and healing. Mental Health Promotion Enhances positive mental health Contributes to the reduction of risk behaviours such as tobacco, alcohol, and drug misuse, unsafe sex Reduction of social and economic problems such as drop out from school, crime, absenteeism from work and intimate partner violence Reduction of rates, severity of, mortality from physical and mental illness. How do we approach mental health promotion? Poverty Sexual Activity Drugs Diet Smoking Education Unemployment Social Supports Early Childhood Development Principles of Health Promotion Health education Policy analysis Community development and organization Health advocacy Legislation World Health Organization (1984) Ottawa Charter for Health Promotion Building Healthy Public Policy Creating supportive environments Strengthening community action Developing personal skills Reorienting health services World Health Organization (1986) Key Population Health Promotion Ideas Meaningful participation Meaningful Participation Participation by local people is recognized as having the greatest and most sustainable impact when solving local problems and setting local norms Multi-sector collaboration and partnerships The health sector has to pick up the pieces resulting from poor mental health, but it has little effect on the determinants of mental wellbeing Expand the traditional view about who ‘owns’ mental health promotion, and who actually does, or can, promote mental health in most populations. Moodle/Jenkins Finding ways to shift emphasis from a sector-by-sector approach to a broader and more cohesive problem approach Community as the focus! Partnerships Within communities Between communities Within health organizations Mental health promotion & health promotion Treatment and promotion services Between health organizations With other sectors Conditions for success: Intersectoral action for Population Health Seek shared values and interest; alignment of purpose; common vision Ensure political support Engage key partners Ensure horizontal and vertical linking Invest in alliance building Focus on concrete objectives and visible results Ensure leadership, accountability and rewards are shared among partners Build stable teams of people skilled transformative action adapted from FPT Adv C on PH Housing Good housing acts as a mitigating factor against the negative effects of low SE status on health and well-being (Dunn, 2002). Community focus versus jurisdictional “if jurisdiction is your starting point, you’re not going to solve anything…Start from a community issues standpoint, set aside jurisdictional and policy issues, and commit some resources to it. You’ll see things happen” (Hanselmann, Gibbins) Intersectoral partnerships Individuals and organizations in business and industry, housing, local gov’t, sports, recreation, arts and culture, education, and justice already are promoting and in some cases demoting mental health May not be aware of the effect they have on mental health and can be further encouraged to either expand their health promoting work, or reduce the health damaging effects of their work Challenge is to work out how to create effective partnerships with these indiv and organizations. Take action on a variety of determinants Multiple Strategies Multiple Levels Reduce individual, socio-economic, and environmental risk factors, and Promote protective factors Supportive environments to reduce inequities & remove barriers Making healthy choices, easier choices. Creating supportive environments Policy Economic development Social action Community schools Early childhood supports Creating Supportive Environments High/Scope Perry Preschool Project Targeted 3-4 year old children from impoverished backgrounds Cost $1000 per child Cost-benefit - $7,000 to $8,000 per child Barnett WS. AJ Orthopsych 1993 Government Healthy Public Policy The way services are provided Environmental policy Policy on housing, transportation, etc Economic policy Taxation policy Social policy Healthy Policy is also for you & I School boards Recreation centers First Nations Band councils Municipal governments Committees and organizations Families Workplaces Capacity building and empowering practices Capacity building Increased awareness & knowledge Skill development Knowing how to access resources Developing social networks Learning from others Actions that focus on the health of the population Focus upstream on taking action earlier Evidence based decision making Not only doing things right, but the right things. The delivery of mental health promotion programs in an empowering, collaborative and participatory manner is central to mental health promotion activity. (Barry M) Four crucial settings for intervention Home, School, Workplace, and Community. Jané-Llopis/Barry MM Home During the first period of life, there is more development in mental, social, and physical functioning than in any other period across the lifespan UNICEF, 2002 School Enormous potential – no other setting where such a large proportion of children can be reached WHO “Child-friendly schools” promotes sound psychosocial environment; encourages tolerance and equality between genders, ethinic, religious and social groups. Promotes active involvement and co-op; avoids use of physical punishment; does not tolerate bullying. Supporting and nurturing environment; providing education which responds to the reality of the children’s lives. Establishes connections between school and family life, encourages creativity as well as academic abilities, and promotes self-esteem and self-confidence of children. Workplace Unemployment Work stress Noise, overload, time pressures Repetitive tasks Interpersonal conflicts Job insecurity Low sense of control Balance with personal life Community Change is more likely to come about when the people it affects are involved in the change process. Participation by local people is recognized as having the greatest and most sustainable impact when solving local problems and setting local norms Support Multi-outcome interventions One of remaining problems is the categorical approach to mental, social, educational, behavioural and legal problems. Many of these problems have commonalities that can be addressed simultaneously and that impact on many areas of functioning. Addressing the determinants Partner - Who can we work with, to do it better together? Advocate - What needs to be done at policy legislative level? Cheerlead - Enable - Mitigate - Encouraging and not getting in the way. What we do directly to change the determinants Picking up some of the pieces, so it isn’t worse Solutions? Will be found in:.. thinking, planning and working... across sectors and levels of government from multiple perspectives, including social, psychological, justice, education, and economic, from prevention and promotion through to treatment and care, using the expertise of many disciplines and engaging communities as partners in potential solutions. David’s Population Health Traps Macro Avoidance Micro Paralysis Many Small Steps “Almost anything you do will seem insignificant, but it is very important that you do it anyway” Mahatma Ghandi Why would a small group of dedicated individuals believe that by working together we can change the world? Because throughout history, it is the only thing that ever has. Other sources of further information: Moodle R and Jenkins R. Mental health promotion. I’m from the government and you want me to invest in mental health promotion. Well why should I? Promotion and Education 2005; S-2:37-41. Jané-Llopis E, Barry M, Hosman C, Patel V. Mental health promotion works: a review. Promotion and Education; 2005; ProQuest Nursing Journals, supplement 2: 9-25 Sask Health. Supporting mental well-being and decreased substance use and abuse. 2005 McCubbin M, Labonte R, Sullivan R, Dallaire B. Mental health is our collective wealth – a discussion paper. Submitted to Federal/Provincial/Territorial Advisory Network on Mental Health. Accessed online: http://www.spheru.ca/www/html/Reports/Reports_other.htm Dr. James Irvine Professor, Dept of Family Medicine, U of S Medical Health Officer, Population Health Unit, Northern Health Authorities 2nd Box 6000 Floor, Lac La Ronge Indian Band Office, LaRonge, Sk S0J 1L0 James.Irvine@mcrrha.sk.ca