N A ZSBT GUIDELINES FOR PRETRANSFUSION
advertisement

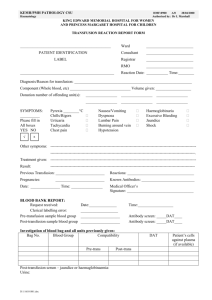
AUSTRALIAN & NEW ZEALAND SOCIETY OF BLOOD TRANSFUSION INC. AN ZSBT Australian & New Zealand Society of Blood Transfusion Inc GUIDELINES FOR PRETRANSFUSION TESTING 4th Edition 2002 Prepared by Scientific Subcommittee of the Australian & New Zealand Society of Blood Transfusion Inc 1 Copyright© by The Australian & New Zealand Society of Blood Transfusion Inc. Apart from any fair dealing for the use of private study, research, criticism, or review as permitted under the Copyright Act, no part of this book may be transmitted or reproduced in any form, electronic or mechanical, or by any information storage and retrieval system, without the written permission of the Publishers. Published in Australia by: Australian & New Zealand Society of Blood Transfusion Inc. 145 Macquarie Street Sydney NSW 2000 AUSTRALIA ISBN No: 0 9577262 3 6 1st Edition 2nd Edition 3rd Edition 1987 1993 1999 2 GUIDELINES FOR PRETRANSFUSION TESTING 4th Edition Prepared by Scientific Subcommittee of the Australian & New Zealand Society of Blood Transfusion Inc 145 Macquarie Street, Sydney NSW 2000 3 Scientific Subcommittee Membership Chairman Graeme Woodfield New Zealand Vice Chairman Ken Davis South Australia Members Andrew Francis South Australia Chris Hogan Victoria Pam Hudson New South Wales Trevor Roper Western Australia Peter Russell Queensland 4 Foreword The ANZSBT Council takes great pleasure in publishing the Fourth Edition of the Guidelines for Pretransfusion Testing. The ANZSBT issues its documents as Guidelines rather than as prescriptive Standards. This edition represents a further revision of the Guidelines and the incorporation of new material including further coverage of electronic crossmatching, increasing the stringency of sample labelling as well as addressing some of the recommendations from the recently published NHMRC/ASBT Clinical Practice Guidelines. Again a group of ANZSBT members from Australia and New Zealand has undertaken the task of revising the Pretransfusion Guidelines with energy and enthusiasm. The general membership has also been actively consulted for changes to be incorporated into this edition. As always there has been much debate and discussion resulting. Whilst, as in the past, it is impossible to incorporate every single submission and point of view, this document again represents a consensus of views as far as this has been possible to achieve. Previous editions of the Guidelines have been widely accepted and we are confident that this new edition will once again prove to be extremely valuable to the medical and scientific community. Mark Dean President Australian & New Zealand Society of Blood Transfusion November 2002 5 CONTENTS PAGE NO. INTRODUCTION i TERMINOLOGY ii SECTION A PRETRANSFUSION PROTOCOLS 1-7 A1 A 1.1 A 1.2 A 1.3 A 1.4 A 1.5 A 1.6 A 1.7 Recommended Pretransfusion Protocols ABO and Rh (D) Grouping Antibody Screening Group and Screen Crossmatching Sample validity Computer Crossmatch Remote Release of Blood 1 1 1 2 2 2 3 4 A2 Selection of Red Cell Products for Transfusion 4 A3 Emergency Transfusion 5 A4 Massive Transfusion 5 A5 Transfusion Recommendations in Pregnancy 6 A.6 Pretransfusion Testing in the Newborn 6 A7 Autologous Transfusion 6 A8 Selection of Non Red Cell Products 7 SECTION B. COLLECTION, LABELLING AND RECORD REQUIREMENTS 8-11 B1 B 1.1 B 1.2 B 1.3 Request Forms & Sample Collection Request Forms Samples Sample Collection & Labelling 8 8 9 9 B2 Pretransfusion Testing Records 10 B3 Transfusion Records 10 B4 Laboratory Records 11 SECTION C. PRINCIPLES OF TECHNICAL PROCEDURES FOR PRETRANSFUSION TESTING C1 C 1.1 C 1.2 C 1.3 C 1.4 C 1.5 C 1.6 C 1.7 C 1.8 Reagents ABO Grouping Reagents Rh(D) Typing Reagents Other Typing Reagents Antiglobulin Reagents Enzyme Preparations Low Ionic Strength (LIS) Solutions Isotonic Saline Reagent Red Cells 12-17 12 12 12 12 12 13 13 13 13 i C2 C 2.1 C 2.2 C 2.3 C 2.4 Tube Techniques General Indirect Antiglobulin Test (IAT) Enzyme Techniques for Antibody Detection Manual Polybrene Techniques 13 13 13 14 14 C3 C 3.1 C 3.2 C 3.3 Microplate Techniques General Liquid Phase Solid Phase 15 15 15 16 C4 Microcolumn Techniques (MCT) 16 C5 Other Techniques 17 SECTION D INVESTIGATION OF TRANSFUSION REACTIONS SECTION E QUALITY ASSURANCE 18 19-23 E1 Personnel 19 E2 Training records 20 E3 Register of Non-Conformances 20 E4 Reagents 20 E5 Equipment 20 E6 Protocols 21 E7 Internal Quality Assurance Programs 21 E8 External Quality Assurance Programs 21 E9 Computer Validation 22 E 10 E 10.1 E 10.2 E 10.3 E 10.4 Blood Products Refrigeration and Freezers Storage Requirements Transport Handling and Administration 22 22 22 22 22 SECTION F 1. 2. 3. APPENDICES 24-27 Abbreviations Maximum Blood Order Schedule (MBOS) Bibliography 24 25 27 ii Introduction The aim of this document is to provide guidelines for pretransfusion testing and safe transfusion practice. This requires: 1. Adequate documentation and accurate identification systems to minimise clerical errors and patient mis-identification. 2. Determination of the recipient ABO and Rh(D) group and the performance of an antibody screen to detect clinically significant red cell antibodies. 3. Adherence to the stringent requirements necessary for the use of computers and computer software in transfusion laboratory practice. 4. Suitable quality control programs for reagents, techniques, equipment and personnel. 5. Selection and provision of compatible blood and blood products. 6. Appropriate storage and handling of blood and blood products. 7. Appropriate investigation of adverse effects of transfusion. 8. Appropriate retention of records, data and documentation as required by national regulatory bodies. This document shall be used in conjunction with the requirements of national accreditation authorities, the national blood services and other regulatory bodies. i Terminology Standards Australia and virtually all national standards bodies around the world including the American Association of Blood Banks (AABB) are following the rules set down by the international standards bodies International Organisation for Standardisation (ISO) and International Electrotechnical Commission (IEC) for the use of the terms "shall" and "should". Although the recommendations in the Guidelines for Pretransfusion Testing are primarily educative, the Scientific Subcommittee has used the Standards Australia definition of these terms for consistency with current international usage. The term "shall" indicates a mandatory requirement, however this does not imply a mandatory legal requirement in an Australian Standard. The term "should" implies a recommendation where guidance is intended and does not preclude other acceptable practices. The term "may” is used to indicate an acceptable alternative or addition to the prescribed practice. ii SECTION A PRETRANSFUSION PROTOCOLS A1 RECOMMENDED PRETRANSFUSION PROTOCOL Pretransfusion testing (compatibility testing) shall consist of an ABO and Rh(D) Group and Antibody Screen and a Crossmatch where necessary (see A 1.4). A 1.1 ABO and Rh(D) Grouping A 1.1.1 The ABO and Rh(D) groups shall be determined on every patient sample used for pretransfusion testing . A 1.1.2 The ABO group shall be determined by testing the red cells with anti-A and anti-B [plus anti AB if desired] reagents and the serum or plasma against A1 and B red cells. Infants less than 4 months of age do not require a serum or plasma group. A 1.1.3 All anomalies in the ABO group should be resolved prior to selection of blood for crossmatching. Group O red blood cells shall be issued when the patient's ABO group cannot be determined prior to transfusion. A 1.1.4 The Rh(D) group shall be determined using an anti-D reagent. Where specified, an Rh(D) control recommended by the manufacturer shall be used in parallel with every test. When testing potential blood product recipients, the test for weak D antigen is not required. However testing for weak D shall be performed on previously untested bone marrow, stem cell and other donors [eg., directed, granulocyte]. A 1.1.5 The patient's ABO and Rh(D) group shall be confirmed before blood is transfused by either: comparing the current findings with those recorded for previous samples or, performing a second test either on the same sample by resampling on a separate occasion to the first test, or on a second current sample. If possible the second test should be performed by a second scientist/technologist who has no prior knowledge of the result. A 1.1.6 The ABO group of all units and the Rh(D) group of units labelled as Rh(D) Negative shall be confirmed by the laboratory undertaking the pretransfusion testing. Confirmatory weak D antigen testing is not required. A 1.2 Antibody Screening A 1.2.1 Techniques used for antibody screening shall be those that are capable of detecting clinically significant red cell antibodies reactive by haemolysis and/or haemagglutination at 37oC. These shall include a 37oC incubation phase and an indirect antiglobulin test although alternative test methods and temperatures may be substituted if the method has been appropriately validated and documented. 1 A 1.2.2 Reagent red cells shall consist of at least two group O red cells [NOT POOLED] and should express the following antigens: C, c, D, E, e, M, N, S, s, K, k, Fya, Fyb, Jka, Jkb. Where possible, one cell should be of the probable R1R1 genotype (CDe phenotype) and the other of the probable R2R2 genotype (cDE phenotype). Where appropriate, additional antigens may be included to reflect the antigenic profile of the local population. A 1.2.3 Where an immediate spin or other abbreviated crossmatch procedure is used reagent red cells shall demonstrate homozygous expression of Jka,Jkb,Fya,Fyb, in addition to the requirements of section A1.2.2. A 1.2.4 If an antibody screening test is positive, antibody identification shall be performed using a reagent red cell panel employing at least the method(s) by which the antibody was detected. Wherever possible, it should be demonstrated that the patient's red cells lack the corresponding antigen. Referral to a Reference Laboratory may be necessary for definitive or confirmatory identification. A 1.2.5 In patients with nonspecific antibodies [autoantibodies] reactive at 37oC, additional tests should be performed which allow the detection of coexisting alloantibodies. Differential alloabsorption may be required for patients transfused within the previous three months. A 1.3 Group and Screen These tests shall be performed on the patient sample within 7 days of collection except as noted in A 1.5.1. A 1.3.1 A Group and Screen (G&S) protocol consists of an ABO and Rh(D) group and an antibody screen on the patient's serum/plasma. Serum/plasma is retained for crossmatching if blood is required at a later stage (see A 1.4). A 1.3.2 In circumstances where the likelihood of blood use is minimal a G&S protocol is recommended in the first instance. If blood is required following a G&S, crossmatched blood should be available for infusion into the patient within 10 minutes of the request. A Group and Screen protocol may be used in conjunction with a Maximum Blood Order Schedule (MBOS), however each laboratory will need to assess the requirements for each surgical procedure in the hospitals it serves, using the crossmatch: transfusion (CT) ratio or MBOS as a guide [see Appendix 2. A 1.4 Crossmatching A 1.4.1 If no clinically significant red cell antibodies are detected in the antibody screen and there is no known history of clinically significant antibodies, the crossmatch may consist of an immediate spin technique only or another procedure capable of detecting ABO incompatibility [eg., computer crossmatch, see A1.6]. NB [Where an immediate spin ABO crossmatch is performed, the cells taken from each donor segment for testing shall be washed prior to performance of the test]. A 1.4.2 In cases where clinically significant antibodies are present or where there is a history of clinically significant antibodies, antigen negative blood should be crossmatched (see A 2.2) by an indirect antiglobulin test or validated equivalent (see A 1.2.1). A 1.5 Sample validity A 1.5.1 Pretransfusion testing and transfusion of a patient who is pregnant or who has been pregnant or transfused in the past three months shall be completed within 72 hours of the sample being collected, unless an extension of this period is approved by the officer-in-charge of the laboratory. 2 A 1.5.2 Compatibility testing may be performed on a sample collected in advance of elective surgery. This is permitted provided that the sample has been tested and stored in the laboratory at -200C for up to 1 month. The requirements of A 1.5.1 shall apply and be validated and documented by the requestor. A 1.5.3 Samples from patients to whom blood has been transfused should be retained for at least 7 days post transfusion for the purpose of investigation of reported transfusion reactions. A 1.5.4 Once a transfusion is commenced, units not transfused within 72 hours shall be subjected to pretransfusion testing on a new sample from the patient. A 1.6 Computer Crossmatching The SSC has been asked to look at preparing guidelines for computer crossmatching. In this regard the SSC feels that there is adequate and pertinent international literature in this area and strongly endorses the BCSH Guidelines [2000] in this area. [see Appendix 3, reference 13]. A 1.6.1 Where comprehensive validated electronic data management is in place (see E 9) a computer crossmatch may be used where the requirements of A 1.1 and 1.2 are met, and when clinically significant antibodies are not currently detectable and where there is no history of clinically significant antibodies. A 1.6.2 Features of the software shall ensure that: (i) group specific blood is not released electronically unless: there is a current Group and Screen sample [see A 1.5] that has been tested and results recorded (ii) group specific blood not be released on historical records (iii) group O Rh(D) negative or group O Rh(D) positive blood is only released in an emergency situation where there is no current Group and Screen (iv) release of blood for patients with special requirements (eg autologous, CMV antibody negative, irradiated), is precluded by messages informing the user if these requirements are not met (v) a mechanism exists to ensure the correct pack is labelled for a specific patient (vi) a unique pack label is generated during the release and that the software checks to ensure that the group of the labelled pack is compatible with the patient group (vii) a transfusion record is produced with the released pack to maintain documentation of the transfusion. A 1.6.3 Software used for computerised pre-transfusion testing shall be validated prior to implementation. Validation may take the form of a checklist showing that the appropriate responses were generated by the program under a series of challenges. A cross-tabulation of all ABO and Rh types of donor versus recipient combination is mandatory. In addition, a separate cross-tabulation shall be performed for each blood product type that would be crossmatched eg whole blood, red blood cells, etc. All validation shall be documented indicating the version of the software, date, and person performing the validation. This validation shall include an independent check of the whole documentation by a senior member of the transfusion laboratory staff who has an in depth knowledge of the software package concerned. A 1.6.4 Re-validation shall be performed after any software modification impacting on the electronic release of blood. A computer crossmatch is prohibited until this validation is complete. A 1.6.5 Only authorised staff with an appropriate security level, ie. staff under the direction of the senior scientist who is responsible for pretransfusion testing, may modify the software modules or algorithms relating to the blood transfusion software. A 1.6.6 All transactions shall be logged and traceable to an individual staff member. The audit trail shall include a record of the time and date stamping. Random access to the database to make changes is prohibited. 3 A 1.7 Remote Release of Blood A 1.7.1 The computer program for ‘Remote Release’ of blood shall be validated to ensure patient safety is maintained. A 1.7.2 All software shall be securely protected from either deliberate or accidental alteration or tampering. A 1.7.3 All users shall be trained, with regular training reviews and shall have individual passwords with designated levels of access to the program. A 1.7.4 Features of the software shall ensure that: (i) all requirements for computer crossmatching have been met (ii) any patient with a history of a clinically significant antibody detected at any time is excluded from remote release, with appropriate explanatory messages A 1.7.5 The parent laboratory shall be notified in ‘real time’ when remote release occurs, enabling the maintenance of stock levels. Different systems perform remote release in varying manners and notification processes may also vary. A2 SELECTION OF RED CELL PRODUCTS FOR TRANSFUSION A 2.1 Red Blood Cell products should be of the same ABO and Rh(D) type as the patient whenever possible. A 2.2 Selection where the antibody screen is positive: (i) where there is current or historical evidence of a clinically significant red cell antibody, blood should be selected which is negative for the relevant antigen. Where possible antigen typing should be confirmed by the laboratory performing the pretransfusion testing. (ii) when transfusion is unavoidable, serologically incompatible blood may be given after consultation with the responsible medical officer and the officer in charge of the laboratory (iii) for patients with antibodies to A1, P1, Lea, Leb, M or N reactive at room temperature but not at 37oC, the blood selected need not be antigen negative. (iv) in some circumstances certain antibodies reactive at 37oC may not be considered clinically significant. Serologically incompatible blood can be given with the permission of the responsible medical officer and the officer-in-charge of the laboratory Specificity Clinical significance Selection of units Rh antibodies (reactive by IAT) Yes Antigen negative Kell antibodies Yes Antigen negative Duffy antibodies Yes Antigen negative Kidd antibodies Yes Antigen negative Anti-S, -s Yes Antigen negative Anti-A1, -P1, -N Rarely IAT crossmatch compatible 37’C Anti-M Rarely IAT crossmatch compatible 37’C Anti-M reactive at 37’C Sometimes Antigen negative Anti-Lea, Anti –Le a+b Rarely IAT crossmatch compatible 37’C Anti –Le b No Not clinically significant and can be ignored High titre low-avidity antibodies (HTLA) Unlikely Antibodies against low/high frequency antigens Depends on specificity Local laboratory policy or seek advice from State Red Cell Reference Laboratory or equivalent Local laboratory policy or seek advice from State Red Cell Reference Laboratory or equivalent 4 A3 EMERGENCY TRANSFUSION In an emergency, standard pretransfusion testing should be applied. A 3.1 It is dangerous to issue blood for resuscitation on the basis of an historical blood group: • red cells issued for resuscitation shall be group O, • plasma issued for replacement shall be group AB [see A 8.1] until an adequately identified sample has been received and the historical group confirmed. A 3.2 If there is insufficient time to complete full compatibility testing, ABO and Rh(D) compatible red cells [preferably group specific] may be issued, provided the patient’s ABO and Rh(D) blood group can be classified as ‘typed twice’ as per A 1.1.5. If A 1.1.5 cannot be fulfilled then Group O Rh(D) negative [or O Rh(D) positive] red blood cells shall be issued. Where stocks of Rh(D) negative blood are limited, criteria for the issue of Rh(D) positive blood should be developed by the officer-in-charge of the laboratory. Pretransfusion testing shall be completed as soon as possible. A 3.3 If a patient of undetermined group receives Group O red cells, transfusion with group specific blood should commence as soon as possible. Change over from group O blood should be determined by local protocols, however determination of the absence of anti-A or B by IAT is recommended prior to such change over. A 3.4 Blood issued prior to the completion of pretransfusion testing shall be CLEARLY LABELLED eg. - "UNCROSSMATCHED BLOOD" or “EMERGENCY ISSUE - COMPATIBILITY TESTING NOT COMPLETED”. A 3.5 If the antibody screen is positive or the crossmatch is incompatible, inform the treating medical officer and the officer-in-charge of the laboratory. If blood is still required immediately, blood should be issued according to protocols developed by the laboratory for this situation. A suggested protocol is as follows: (i) indicate that this finding may delay the issue of compatible blood, but may not prevent the issue of incompatible blood (ii) crossmatch an excess of potential units and issue those which are crossmatch compatible (iii) as soon as possible, proceed with antibody identification. Once the antibody specificity is determined, crossmatch antigen negative blood (iv) determine if the apparent crossmatch compatible units are negative for the specific antigen if possible (see A 1.2.4) (v) once compatible blood is available, retrieve any untransfused units that have been issued as “uncrossmatched” or “incompatible” A4 MASSIVE TRANSFUSION Replacement of the patient’s total blood volume (70 mL/kg] within 24 hours A 4.1 The freshest available red blood cells should be selected, dependent on availability and in accordance with protocols developed by the laboratory. A 4.2 The management of patients with clinically significant red cell antibodies, for whom blood is not available, is discussed in A 2.2, A 3.5. A 4.3 Monitoring of coagulation parameters may assist in determining the requirement for other blood products. A 4.5 After transfusion of ten units of red cells in an adult, group specific issue may be used without crossmatching. 5 A5 TRANSFUSION RECOMMENDATIONS IN PREGNANCY A 5.1 CMV antibody negative blood or leucodepleted products should be used for pregnant women who require transfusion regardless of CMV antibody status [see Appendix 3, reference 15]. CMV infection (primary and re-infection) at any time during the pregnancy can cause congenital abnormalities. A 5.2 Blood for intrauterine transfusions where alloimmunisation is present shall be: (i) CMV antibody negative or leucodepleted (see Appendix 3, reference 5) (ii) irradiated (see Appendix 3, reference 5) (iii) group compatible with mother and foetus (iv) compatible with maternal blood group antibody Most alloimmunised women undergoing intrauterine top-up transfusion for foetal anaemia are antibody responders with a high likelihood of further antigen sensitisation. It is therefore recommended to select cells for transfusion which match the Rh, Kell, Duffy, Kidd, and S status of the mother. A6 A7 PRE TRANSFUSION TESTING IN THE NEWBORN (DURING FIRST FOUR MONTHS OF LIFE) A 6.1 An initial neonatal pre transfusion sample shall be tested in order to determine the ABO and Rh(D) group [see A 1.1]. In determining the ABO group only the red cell group need be performed. A 6.2 An antibody screen on maternal serum/plasma collected at delivery or at the time of neonatal admission should be performed where possible to detect clinically significant antibodies. If maternal serum/plasma is not available then neonatal serum/plasma shall be used A 6.3 If the initial antibody screen is negative, it is unnecessary to crossmatch donor red cells for the initial or subsequent transfusions. Repeat testing may be omitted for the remainder of any one hospital admission in the first four months of life A 6.4 If clinically significant antibodies are identified, donor units for transfusion that do not express the corresponding antigen, should be selected. Such units should be crossmatched using either maternal or neonatal serum/plasma (see 1.4.2). When the antibody is no longer demonstrable in the neonate's serum, provision of antigen negative blood may be discontinued. A 6.5 Following the transfusion of ABO compatible but not group specific blood further transfusions should be continued with group compatible blood. Transfusion of ABO specific blood may recommence once infused anti-A and/or anti-B antibodies are no longer detectable by the indirect antiglobulin test. Tests for anti-A shall use A1 cells. No subsequent crossmatching is then necessary during the remainder of any one hospital admission in the first four months of life (however compliance with A 6.2 – A 6.4 is required). A 6.6 For immunocompromised or low birth weight (<1,500 g) infants, blood products that contain cellular elements shall be CMV antibody negative or leucocyte depleted and irradiated (see Appendix 3, reference 5). AUTOLOGOUS TRANSFUSION (It is strongly recommended that reference be made to ASBT Autologous Guidelines, 2002, before undertaking an autologous collection program) A 7.1 Autologous units shall be clearly labelled to distinguish them from allogeneic (homologous) units and stored in a separate designated area. 6 A8 A 7.2 Pretransfusion records for autologous transfusion shall be as for allogeneic transfusion (see B 2). A 7.3 Pretransfusion testing [as per A 1] shall be performed on a pretransfusion sample of the patient's blood, collected independently from the autologous unit collection as for allogeneic transfusion. A 7.4 A compatibility label shall be attached to the autologous unit (see B 2.2.) SELECTION OF NON RED CELL PRODUCTS A 8.1 Fresh frozen plasma and cryoprecipitate should be ABO compatible with the recipient's red cells. Pretransfusion testing is not required. As a general guideline refer to the following: Recommended ABO group for plasma products Patients ABO blood group ABO group of plasma to issue Unknown [request patient sample for baseline G&S] O A B AB Issue AB if urgent O or A or B or AB A or AB B or AB AB (A if AB unobtainable) Individual units of different blood groups shall not be pooled. A 8.2 Platelet concentrates in order of preference should be: (i) Patient's own ABO, Rh(D) group, If this is not possible, a decision on whether to give antigen or plasma incompatible platelets may be of importance depending on the patient diagnosis/therapy: (ii) ABO, Rh(D) antigen compatible [but plasma incompatible], or (iii) ABO, Rh(D) antigen incompatible Requirements for HLA compatibility may take precedence over ABO typing. Individual units of different ABO blood groups shall not be pooled. Matching for Rh(D) type is desirable [as platelet products may contain small or minimal numbers of red cells], but may be less important than ABO matching. Platelets do not carry Rh antigens. A 8.3 The administration of Rh(D) immunoglobulin should be considered for Rh(D) negative patients, especially premenopausal females, when platelet concentrates from Rh(D) Positive donors are transfused. A 8.4 Buffy coats and granulocyte concentrates shall be irradiated and ABO and Rh(D) compatible. Pretransfusion testing is required due to the large number of red blood cells normally present in these products. Consideration shall be given to the CMV status of the recipient. 7 SECTION B REQUEST FORMS, SAMPLE COLLECTION, SAMPLE LABELLING AND RECORD REQUIREMENTS This is an area of transfusion practice that is crucial to safety and quality outcomes. Morbidity and mortality still occurs due to failures in correct patient identification at the time of sample collection, prescription of the wrong product, or infusion to the wrong patient. The then ASBT in conjunction with the NHMRC in October 2001 released clinical transfusion practice guidelines that have a direct bearing on aspects of pretransfusion testing, particularly in regard to documentation of the transfusion process. The retention of all laboratory records relating to transfusion practice detailed in this document shall comply with the requirements of national accreditation authorities or regulatory bodies. Electronic request ordering is now being encompassed by various hospital / laboratory information systems. These requests shall comply with the requirements of B 1.1. Telephone requests: There shall be a policy for documenting telephone requests for blood products. The use of a telephone request pad or other evidential means that provide data on such requests is recommended. Such requests shall be stored according to regulatory requirements. B1 REQUEST FORMS & SAMPLE COLLECTION B 1.1 Request forms It is recommended that request forms for transfusion be formulated for this purpose alone. They should be so designed as to alert the user to the need for considerable caution in identifying patients and ensuring that the pretransfusion samples are collected from the correct patient. These request forms should summarise the clinical recommendations of the NHMRC/ASBT guidelines and be able to collect standardised data items. Clinical and laboratory indications for blood components should be accurately recorded on these request forms and in the patient’s medical record. B 1.1.1 A formal request is required for pretransfusion testing which may be handwritten or in electronic form. B 1.1.2 The request shall clearly identify the patient and include in legible form: (i) (ii) (iii) (iv) (v) (vi) patient surname, given name(s) in full, and hospital record number and/or date of birth (see also B1.3.2) date and time of collection name of requesting physician and signature details of the request ie. Type of blood product, group and screen date and time required signature of the collector to confirm the correct labelling of the sample at the time of collection. The collector shall also sign a statement on the request form as follows: “I certify that the blood specimen(s) accompanying this request was drawn from the patient named above and I established the identity of this patient by direct inquiry and/or by inspection of wrist band, and immediately upon the blood being drawn I labelled the specimen(s)". (Amendment 25 February 2004) 8 Experience has shown that many errors occur in documentation when labelling samples and completing forms. It is suggested that where practical a second person verifies that correct patient identification and recording of correct patient details have been accurately performed. In emergency situations, where the patient's identity is unknown, an alternative reliable documented method of identification shall be substituted and be reliably linked to the patient's name once available. B 1.1.3 Other information should include clinical diagnosis and indication for transfusion, previous transfusion history, known red cell antibodies, pregnancies and gender [see introductory paragraph above]. B 1.1.4 For patients with a valid group and screen, a verbal request may be accepted to order blood dependent on local rules or other legislation, eg, a signed form to follow. B 1.2 Samples B 1.2.1 Either serum or EDTA plasma may be used for pretransfusion testing. SST samples shall not be used [due to the potential for the gel to adsorb antibodies resulting in possible false negative results in antibody detection]. B 1.2.2 Grossly haemolysed samples may indicate a problem with collection or transport. B 1.2.3 An EDTA sample is recommended for direct antiglobulin tests. B 1.3 Sample Collection & Labelling B 1.3.1 The patient's identity shall be positively confirmed* at the time of sample collection. *Patient identity shall be confirmed by asking the patient [if conscious and rational] to state their surname, given name(s), and date of birth and by checking the identity label securely fastened to the patient. B 1.3.2 Following collection and before leaving the patient, the tube(s) containing the sample(s) shall be legibly labelled with: (i) (ii) (iii) patient's surname, given name(s) in full, and hospital record number or date of birth. For unidentified patient see Section B1.1 date and time of collection the signature or initials of the collector shall appear on the sample tube, See qualifying statement in B 1.1.2 above. It is strongly recommended that addressograph labels should NOT be used, but if used they must conform to (i) to (iii) and B 1.1.2 applies. Samples that do not conform to these labelling requirements SHALL be discarded. If blood is required urgently under these circumstances refer to A 3. B 1.3.3 The request form and sample tube shall carry identical patient identification information. The request form and sample label shall be checked on receipt in the laboratory and, in case of discrepancy or doubt, a clear, documented protocol approved by the officer-in-charge of the laboratory shall be applied. Unlabelled samples shall be discarded. 9 B2 PRETRANSFUSION TESTING RECORDS B 2.1 B 2.2 B 2.3 B3 A pretransfusion testing record shall be completed for each patient on whom a pretransfusion sample is received and when blood is allocated by the testing laboratory and shall contain the following information: Recipient Surname and given name(s) in full Hospital record number or date of birth Date [and time] of collection of sample ABO/Rh(D) blood group Antibody screen result if performed Results of tests and their interpretation Donation Donation number ABO/Rh(D) blood group Compatibility testing result Identity of person performing the compatibility testing Date of compatibility testing A compatibility label carrying the details below shall be securely attached to each unit once pretransfusion testing is completed and the unit is allocated to the patient. Recipient Surname and given name(s) in full, Hospital record number or date of birth, ABO/Rh(D) blood group Donation Donation number ABO/Rh(D) blood group Statement of compatibility A clerical check on patient identity, the unit, and the compatibility label shall be made at the time of issue of blood from the laboratory. TRANSFUSION RECORDS There shall be a written order for the blood product, which should include a documented reason for the order. B 3.1 Transfusion of any blood product shall not commence until the following has been checked and found to be correct by two appropriate staff at the patient's bedside: (i) patient's surname, given name(s), medical record number or date of birth on both the patient's identification band and the unit compatibility label (ii) donation number, blood group and component type against the patient blood group and the unit compatibility label (iii) statement of compatibility (iv) expiry date of the unit has not been exceeded (v) expiry date of the cross match has not been exceeded B 3.2 A record shall be completed at the time of transfusion of each unit and remain a permanent part of the patient's medical record. It shall contain details of: RECIPIENT Surname, given name(s) in full Medical record number or date of birth ABO/Rh(D) group 10 DONATION B4 Donation number of each unit Identity of the person placing the unit of blood into the IV line and checking the compatibility record (initial and surname) Identity of the second person responsible for checking the transfusion at the bedside (initial and surname) Time and date each unit commenced and completed Details of untoward reaction to transfusion LABORATORY RECORDS B 4.1 Each laboratory shall have systems in place to identify adverse events or reactions to transfusion. The appropriate authority/manufacturer should be notified where indicated. B 4.2 The following information shall be recorded by the laboratory performing pretransfusion testing and maintained for a period as designated by the appropriate authority (see Appendix 3, reference 9): (i) donation or batch number and description of all blood components and manufactured blood products handled by the laboratory (ii) ABO/Rh(D) group if relevant (iii) the fate of the component or blood product (issued, expired, transferred) (iv) recipient's surname, given name(s) in full, medical record number or date of birth B 4.3 The laboratory shall ensure that systems are in place to trace every blood component or manufactured blood product issued. 11 SECTION C PRINCIPLES OF TECHNICAL PROCEDURES FOR PRETRANSFUSION TESTING A consistently high standard of pretransfusion testing depends on close attention to detail and quality assurance of the laboratory functions involved. In this section, recommendations are made concerning important points in the technical performance of pretransfusion testing. For further details regarding methodology, refer to the attached list of suggested references (see Appendix 3, Reference 1,2,3,4). The techniques specified for each laboratory shall be readily available in a procedure manual and be strictly followed. C1 REAGENTS Laboratories shall have a procedure in place to ensure that grouping reagents perform according to the manufacturer’s stated specificity. All reagents should be stored and used in accordance with the manufacturer's instructions. Reagents shall not be used beyond the manufacturer’s assigned expiry date except as specified in E 4.5. Reagents used by other methods need to be validated and documented. [see section E 4]. In-house reagents shall undergo appropriate quality control procedures. C 1.1 ABO Grouping Reagents A system shall be in place to confirm the specificity of ABO grouping reagents. ABO grouping reagents shall be confirmed against A2 and B cells. A1 and B cells are required for reverse grouping. C 1.2 Rh(D) Typing Reagents Rh(D) typing reagents shall be checked by the manufacturer's recommended procedure against cells with heterophenotypic Rh(D) expression (eg. R1r or R0r) and negative cells (rr). [Monoclonal Rh(D) typing reagents for routine determination of Rh(D) status should not detect DVI ]. C 1.3 Other Typing Reagents Positive and negative controls shall be used with typing reagents other than ABO & Rh(D) reagents in parallel with the unknown sample(s) or batches. Positive control cells with the weakest available antigen expression should be used (see Appendix 3, Reference 2). C 1.4 Antiglobulin Reagents Each batch of reagent shall be tested and validated prior to use, in parallel with the current acceptable batch of reagent, to confirm efficacy of the anti-IgG component, by using native sera or plasma containing weak IgG antibodies of various specificities by the routine antiglobulin methods in use. Antibodies of the Duffy and Kidd systems best challenge the antiglobulin reagents and would be suitable if available. Laboratories without access to suitable antibodies should obtain these from external sources. Antiglobulin reagent used for direct antiglobulin testing shall contain anti- IgG and anti-C3d. 12 C 1.5 Enzyme Preparations In-house reagents require careful standardisation to ensure that they are potent enough to permit detection of weak antibodies but not so sensitive as to give false positive reactions (see Appendix 3, Reference 2). Enzyme preparations should be tested for activity using antibodies known to be weakly reactive by enzyme techniques. C 1.6 Low Ionic Strength (LIS) Solutions C 1.6.1 LIS solutions (LISS) must be buffered to pH 6.7 with a final osmolality of 0.033 mOsm/L and conductivity of 3.6-3.7 mMho. C 1.6.2 LISS and LIS Additive solutions should be used according to the manufacturer's recommendations. C 1.7 Isotonic Saline Isotonic saline should have a pH between 6.8 and 7.2 and be buffered, unless the manufacturer of a reagent indicates otherwise ( eg. suspensions for typing by some monoclonal antibodies to MNS and Le system antigens). C 1.8 Reagent Red Cells C 1.8.1 Reagent red cells prepared in-house should be washed and diluted to the appropriate concentration prior to storage. C 1.8.2 All reagent red cells shall be stored according to the manufacturer's instructions. C2 TUBE TECHNIQUES C 2.1 General C 2.1.1 A 3% v/v cell suspension is recommended for tube tests except where otherwise indicated. C 2.1.2 All tubes shall be clearly labelled to indicate the source of cells and serum, and technique when appropriate. C 2.1.3 Serum or plasma should be added first, before adding cells, if this is acceptable for the method used. Each tube should be examined to ensure serum or plasma is present. C 2.1.4 All haemagglutination reactions should be graded or scored to indicate reaction strength. Negative reactions should be written "neg" or "0" not "-". Haemolysis should be recorded as such. Results should be written down immediately and not memorised, and interpretation should only proceed after all results have been recorded (see Appendix 3, Reference 3). C 2.2 Indirect Antiglobulin Test (IAT) C 2.2.1 A minimum serum:cell ratio of 40:1 is recommended (ie. 2 vol. serum: 1 vol. 3-5% v/v cell suspension for normal ionic strength IAT). A positive control comprising a weakly reacting antibody shall be used in all IAT techniques. 13 For LISS suspension techniques, equal volumes of serum or plasma and LISS suspended cells shall be used to maintain low ionic strength conditions. A test system using 2 vol. serum: 2 vol. 2% v/v LISS cell suspension maintains low ionic strength and meets the requirements for a minimum serum:cell ratio of 40:1 (see also C 1.6.2). C 2.2.2 A 30 minute minimum incubation time is adequate for normal ionic strength IAT, and 10 minute minimum and 30 minute maximum incubation time for LIS techniques. If plastic tubes or dry heating blocks are used for this procedure, a minimum 15 minute incubation time is required for LIS techniques to ensure adequate exposure at 37°C C 2.2.3 The indirect antiglobulin test should be observed for agglutination or haemolysis following incubation of cells and serum or plasma at 37oC, just prior to washing and addition of antiglobulin reagent. (If PEG is used this step shall be omitted). C 2.2.4 An auto control is not obligatory for the antiglobulin test. C 2.2.5 Standardised volumes shall be used for all dispensing steps when performing the low ionic IATs to ensure the correct ionic strength of the reaction mixture. C 2.2.6 Reading test reactions in test tubes shall be performed one tube at a time using a rolling or tilting action to ensure reliable observation of weak agglutination. C 2.2.7 Negative antiglobulin tests shall be validated by adding cells known to be weakly sensitised with IgG to each negative test, centrifuged and observed for weak mixed field agglutination. C 2.2.8 Wash solutions shall be buffered (see C 1.7) C 2.3 Enzyme Techniques for Antibody Detection C 2.3.1 Two stage techniques are preferred and should be conducted at 37oC. C 2.3.2 Serum and cells may be prewarmed to 37oC before mixing to avoid interference from clinically insignificant cold antibodies. C 2.3.3 A positive control reagent comprising a mixture of antibodies (eg. D and c antibodies) or soya bean lectin should be added to each negative test. C 2.3.4 Enzyme methods cannot be used to the exclusion of other tests as the enzymes destroy some antigens of the MNS and Fy systems. A number of antigens in other blood group systems may also be adversely affected by enzyme treatment. C 2.4 Manual Polybrene Techniques C 2.4.1 A negative control, comprising ABO compatible, serologically inert sera should be set up with each set of tests. C 2.4.2 A positive control comprising an antibody known to react weakly by the polybrene procedure should be set up with the first set of tests performed each day (or each shift) and whenever any of the reagents are replaced. C 2.4.3 If the technique is extended to the antiglobulin phase, monospecific anti-IgG shall be used. 14 C3 MICROPLATE TECHNIQUES Microplates provide an efficient means of batch processing samples for blood grouping and antibody screening. They may also be convenient when using cell panels for antibody identification. Liquid or solid phase techniques may be used. C 3.1 General C 3.1.1 Microplate techniques permit the use of diluted reagents for some applications. If diluted, adequate sensitivity and specificity of the reagents shall be confirmed and evaluation data documented and archived as per appropriate regulatory bodies (eg NPAAC requirements). C 3.1.2 Automated readers may be used to record agglutination reactions or solid phase results in microplates. Validation of the machine interpretation of results shall be established before routine use. C 3.1.3 Sample identification When processing samples from more than one patient on one plate, the letter/number code for each test well or row of wells as appropriate shall be recorded against the respective patient identification information. Automated equipment may facilitate this requirement. C 3.1.4 Wash buffers for the antiglobulin phase Bovine serum albumin (0.2%) and Tween (0.1%) should be included in wash buffers used for antiglobulin procedures to avoid non specific adherence of red cells to the well surface. C 3.1.5 Cell suspensions 0.2%-0.5% cell suspensions are required for all solid phase microplate applications. C 3.1.6 Centrifugation The optimum centrifugation conditions shall be determined for the specific equipment to be used. For end point reading of test results the aim should be to provide adequate packing of cells without requiring vigorous resuspension. Programmable centrifuges are recommended. C 3.2 Liquid phase Generally, the principles applying to tube techniques apply to microplate methods, however, some additional considerations apply:C 3.2.1 Type of plates Rigid or flexible polystyrene plates may be used but shall be "unactivated". Microplates or well strips treated to provide efficient protein binding for solid phase ELISA procedures should not be used. The plates shall have letter and number identification provided for each well. Non-specific binding can be avoided by use of a blocking agent (see C 3.1.4). C 3.2.2 Microplate Shakers These are recommended for all mixing stages of the techniques applied and are essential for standardisation of end stage cell resuspension immediately prior to reading results (except IAT see 3.2.3). The speed and time of operation should be established to provide the minimum agitation required to completely resuspend the cell button. 15 C 3.2.3 Antiglobulin Techniques A "streaming" technique is recommended for reading IAT which provides greater sensitivity using either U or V wells. A 0.2 - 0.5% cell suspension should be used (see Appendix 3, Reference 4), for liquid phase grouping and antibody screening methods). C 3.3 Solid phase The technical requirements for solid phase microplate techniques are different from those applying to liquid phase tests. Commercial solid phase blood grouping and antibody screening kits shall be used according to the manufacturer’s instructions. C 3.3.1 Type of plate Microplates should be U shaped rigid polystyrene "activated" for application of solid phase ELISA techniques. Strip wells in 1 x 8 or 2 x 8 format are also available. Carriers for the strips shall have letter/number coding to identify wells. C 3.3.2 Establishing solid phase reactant The concentration of antibody to be bound to the well surface either as the reactant or as a binding agent for a reactant should be in the range 2-20 ug/mL. C 4 MICROCOLUMN TECHNIQUES (MCT) C 4.1 MCT should be used according to the manufacturer's instructions. Any variations shall be validated. C 4.2 MCT using an AHG cassette/card is capable of detecting both IgG and IgM antibodies in a single procedure, therefore an additional 37°C technique is not required. C 4.3 All precautions relating to reagents used for blood group, antibody screening and crossmatch procedures apply (see C 1). C 4.4 All QC procedures for blood group, antibody screen and crossmatch procedures apply (see E 4). C 4.5 A weak IgG antibody control shall be used at least once per day in the AHG procedure. C 4.6 Each batch of AHG cassettes/cards shall be tested and validated prior to use. Test antisera should cover a range of reaction strengths to confirm adequate sensitivity. C 4.7 The following technical considerations are critical to the MCT (i) (ii) (iii) (iv) (v) red cell concentration shall be standardised volumetric pipettes shall be used the incubator and centrifuge for MCT cassettes/cards shall meet manufacturer specifications a technique shall be in place to confirm addition of patient serum or plasma the order of addition of reagents shall be that specified by the manufacturer unless otherwise validated Note : Use of antiglobulin control cells is unreliable following this technique and shall not be used. 16 C5 OTHER TECHNIQUES The use of other techniques is not precluded by these guidelines but all other methods should undergo a rigorous, controlled evaluation to demonstrate their sensitivity and reliability compared with the recognised, standard methods. Results of the evaluation shall be documented and archived according to requirements of appropriate regulatory authorities. These techniques, if introduced into routine use, shall be subject to ongoing adequate and appropriate quality control (see E). 17 SECTION D INVESTIGATION OF TRANSFUSION REACTIONS All transfusion reactions considered potentially haemolytic or due to bacterial contamination shall be reported immediately to the laboratory that performed the pretransfusion testing. Significant adverse reactions to transfusion including suspected disease transmission should be reported to the appropriate regulatory authorities. D1 Possible haemolytic transfusion reactions should normally be investigated prior to further transfusion, and it is recommended that the following protocol is used. D 1.1 Patient identification and donor unit compatibility label shall be rechecked at the bedside. D 1.2 The following should be sent immediately to the laboratory accompanied by a request form giving full clinical signs and symptoms of the reaction: (i) the blood pack, IV administration set and empty packs from previously transfused units (ii) EDTA, clotted and other samples, as necessary, be collected immediately post-reaction and from the opposite arm to the blood infusion site. (iii) the first sample of urine collected post transfusion D2 The investigations shall include: (i) a check on the identity of the patient on the pack label, the donor blood and the pretransfusion testing records (ii) visual examination of the patient's post-transfusion serum/plasma for haemoglobinaemia (iii) repeat ABO and Rh(D) typing and antibody screen on: the pretransfusion patient sample a post-transfusion patient sample (iv) repeat ABO and Rh(D) typing on the unit being transfused at the time of the reaction, and any previously transfused units when available (v) a direct antiglobulin test (DAT) on red cells obtained from the patient before and after transfusion (a negative DAT post-transfusion does not exclude a severe haemolytic transfusion reaction) (vi) an antiglobulin crossmatch of all red cell units given against: pretransfusion patient serum or plasma post-transfusion patient serum or plasma D3 It may be difficult clinically to distinguish a haemolytic or simple febrile nonhaemolytic transfusion reaction from that due to bacterial contamination. If the above tests are inconclusive further testing may be indicated, as follows: (i) determination of plasma haemoglobin, serum bilirubin and haptoglobin levels (ii) determination of urinary haemoglobin and urobilinogen (iii) samples of blood remaining in packs or tubing from transfusions given prior to the reaction should be sent to a microbiological laboratory for Gram stain and culture under appropriate conditions [ie, media, temperature and atmosphere]. (iv) blood cultures should be taken from the patient (v) observation of the contents of the original pack (following centrifugation if necessary) for pretransfusion haemolysis due to incorrect storage D4 Screening for HLA, platelet, and neutrophil antibodies may be indicated in the event of nonhaemolytic transfusion reactions. If the reaction is severe with pulmonary involvement and Transfusion Related Acute Lung Injury (TRALI) is suspected, plasma from the donor packs should be screened for HLA and neutrophil antibodies. D5 In suspected anaphylactoid reactions the possibility of the involvement of antibodies to plasma proteins, particularly IgA, should be considered. 18 SECTION E QUALITY ASSURANCE In Australia quality processes are now fully incorporated into NATA / RCPA accreditation under the requirements of AS ISO/IEC 17025 [1999]. All laboratories that perform pretransfusion testing shall participate in a quality assurance (QA) program that is designed to ensure accurate and consistent performance in all aspects of the laboratory's work practices from collection of samples to the final release of blood for transfusion. The QA program shall become an integral part of the workload of the laboratory and not be seen as an adjunct. It is recommended that one staff member should be designated as the Quality Assurance Officer, who is responsible for ensuring that all aspects of the QA program are fully understood and performed regularly. The Stephen Review [2001] in to the blood sector recommended the establishment of hospital transfusion committees “to implement and oversee quality assurance”. Hospital Transfusion Committees (HTC). The provision of safe and effective transfusion practice requires multidisciplinary collaboration. The HTC can help with areas covered by these guidelines, as follows: • • • • • • • E1 disseminating national or local guidelines within the institution developing local policies and protocols for blood use and collection auditing use and wastage, and developing related performance indicators risk management communication with internal and external bodies about quality assurance matters training of medical & nursing staff and phlebotomists in generating requests and collection and labelling of samples supporting haematologists and transfusion laboratory staff in enforcing policies relating to nonlaboratory aspects of transfusion practice, eg., documentation of transfusion, identification of patients, collection of samples for transfusion, and correct prescription of blood products PERSONNEL It is important that all personnel shall have a clear understanding of their role and responsibility within the laboratory and that their standard of performance be subject to regular review. E 1.1 All new personnel shall participate in an orientation program and be fully aware of all aspects of the laboratory. E 1.2 All personnel shall have an accurate job description detailing their position in a chain of command, the person to whom they report and the duties that they may perform with and without supervision. E 1.3 Staff shall be made fully aware of all health & safety requirements of the laboratory and of the institution. E 1.4 Regular proficiency testing of all laboratory staff shall be assessed by participation in both external QA [and where possible] by participation in an internal QA program/s. E 1.5 All staff should participate in continuing education programs to ensure a high level of current knowledge. 19 E2 TRAINING RECORDS Laboratories shall have • a training program for new staff and an on-going assessment program (other than internal and external QA programs) for all staff. • all training records and assessment records retained as per accreditation requirements • staff assessed as being competent to carry out the tasks they are doing. E3 REGISTER OF NON-CONFORMANCES Each laboratory shall have a system in place to record incidents, discrepancies, ‘near-misses’ that had, or had the potential to have an adverse impact on the patient. The system shall include a review and correction process. E4 E5 REAGENTS E 4.1 The laboratory shall maintain records of all quality control performed on reagents, including date of testing, batch number and expiry and the identity of the individual(s) performing the tests (see Appendix 3, Reference 9). E 4.2 Prior to use, the identity of any reagent shall be checked and confirmation obtained that it: i) is of normal appearance ii) has not passed its stated expiry date E 4.3 Reagents which are in routine use should be tested at the start of each working day [see C 1]. E 4.4 Reagents that are not in daily use should be subjected to quality control in parallel with each batch of tests. E 4.5 Use of rare reagents beyond their expiry date may be appropriate providing positive and negative controls are set up in parallel and perform satisfactorily. EQUIPMENT E 5.1 All laboratory equipment shall be subjected to regular maintenance programs to ensure reliability. Equipment shall be monitored in accordance with national accreditation guidelines and records kept. E 5.2 Refrigerators and deep freeze cabinets used to store blood products shall conform to the national standard (see Appendix 3, Reference 8). E 5.3 Waterbaths and heat blocks shall be cleaned regularly. The temperature shall be recorded daily. Water baths incorporating a stirrer or recirculating device are recommended. E 5.4 Centrifuges shall be maintained according to the manufacturer's recommendations and maintenance records kept. E 5.5 Automated cell washers used for washing antiglobulin tests shall be reserved for that purpose only. The washing of whole blood samples may cause contamination of the head and injection ports and these cell washers shall not be used for this purpose. E 5.6 For automated cell washers: (i) ensure that the saline supply is adequate at the start of each cycle (ii) check the saline delivery volume and residual saline volume following decant (iii) subject each cell washer to weekly replicate testing (see Appendix 3, Reference 3) 20 (iv) On a monthly basis, flush all pump tubes with 1% v/v sodium hypochlorite solution or other suitable agent. Ensure all traces of cleaning agent are removed before reusing E 5.7 E6 E7 E8 Check the accuracy and precision of all fixed volume pipettes and diluters regularly in accordance with national accreditation standards. PROTOCOLS E 6.1 A methods and procedures manual shall be available within the laboratory. All methods undertaken within the laboratory shall be clearly described and each one shall include: (i) title of method (ii) date introduced (or amended) (iii) step by step procedure (iv) standards and controls (v) references for method (vi) author/authoriser E 6.2 The methods and procedures manual shall be reviewed at least annually. The review date and all amendments made must be recorded. E 6.3. Procedures (such as investigation of transfusion reactions) which contain a number of methods shall be included in the manual and cross referenced to the methods. E 6.4 Instructions for the issue of blood and blood products under routine and emergency conditions shall be included in the manual. INTERNAL QUALITY ASSURANCE PROGRAMS E 7.1 All staff shall participate in regular (preferably quarterly) internal quality assurance programs, such as the inclusion of quality assurance samples into the routine workload. The results of such QA programs shall be reviewed. E 7.2 Any staff member failing to achieve satisfactory results shall be given further training. Repeated failure should be cause for withdrawal of that staff member from crossmatching and issue of donor blood until further training has been undertaken and performance deemed to be satisfactory by the person in charge of the transfusion laboratory has been achieved. E 7.3 Replicate testing, using weakly sensitised red cells or a weak antibody is the recommended means of assuring that weak reactions can be detected. The provision of mixed cell populations is also recommended. E 7.4 Records shall be kept of all internal quality assurance programs including the date performed, results obtained and the identity of the staff performing the tests E 7.5 Evidence of review and action taken shall be documented. EXTERNAL QUALITY ASSURANCE PROGRAMS E 8.1 All laboratories shall participate in recognised external quality assurance programs in areas appropriate to their range of methods. E 8.2 All staff shall participate in external QA programs on a rotational basis. E 8.3 Records of the results obtained and the identity of staff performing the testing together with the external organiser's reports shall be archived. E 8.4 Evidence of review and action taken shall be documented. 21 E9 COMPUTER VALIDATION (see also A 1.6) E 9.1 Irrespective of the source and prior manufacturer tests, the software shall be validated to ensure that it performs accurately in the environment in which it is to be used. Validation should include: (i) destructive tests of individual modules (ii) integrated tests of the complete system using correct and incorrect data designed to test all logic paths Validation documentation shall be archived. E 10 E 10.1 E 9.2 All changes to software shall be documented and fully validated before implementation. E 9.3 It is desirable to introduce new or modified software in parallel to the existing manual or computer system. BLOOD PRODUCTS Refrigerators and Freezers (i) refrigerators and freezers for storage of blood components shall comply with national standards (see Appendix 3, Reference 8). (ii) refrigerators and freezers shall have a temperature recording device which shall be checked at least daily. Charts should be kept for at least 1 year (see Appendix 3, Reference 8). (iii) refrigerators and freezers shall have an alarm system that complies with national standards. (iv) the alarm function of temperature recording devices shall be checked for both high and low temperature limits (see Appendix 3, Reference 8). E 10.2 Storage requirements Blood components shall be stored at monitored temperatures optimal for their function and safety. (i) whole blood and red blood cells, 2-6oC (ii) platelets, 20-24oC with gentle agitation (iii) fresh frozen plasma, below -25oC (iv) cryoprecipitate, below -25oC (v) manufactured blood products as per manufacturer’s instructions E 10.3 Transport Blood products shall be transported within their storage specification temperature for the duration of transit as per national standards. This can be done by continuous monitoring [eg, data loggers] or by using other validated procedures. E 10.4 Handling and administration Some practices are necessary for reasons of microbiological safety rather than product performance. (i) Fresh frozen plasma shall be placed in a sealed bag designed to exclude water and avoid contamination of the outlet port and thawed at 30-37oC. If not infused immediately it shall be stored between 2 and 8oC for up to 24 hrs. 22 If stored at these temperatures for more than 24 hrs it shall not be used as a source of labile clotting factors but shall be relabelled and may be used as “Thawed Plasma” for up to five days. It shall not be refrozen, provided that it is not used as a source of FVIII or FV. [see Appendix 3, reference 10] (ii) Cryoprecipitate shall be placed in a sealed bag as in E 10.4 (i) and thawed at 30-37oC. Thawed cryoprecipitate may be pooled (see A 8.1). If not infused immediately it shall be stored between 20 and 24oC and used within 6 hours. It shall not be refrozen (see Appendix 3, Reference 10). (iii) Red cell products which have been exposed to ambient or higher temperatures for longer than 30 minutes shall not be returned to stock and be labelled accordingly. (iv) If platelet concentrates are pooled locally (see A 8.2) then administration shall commence within 4 hours of pooling (see Appendix 3, Reference 12). This pooling shall be performed under aseptic conditions. (v) Manufactured blood products shall be administered as described in the product information sheet. 23 SECTION F APPENDICES APPENDIX 1 ABBREVIATIONS AHG antihuman globulin CMV cytomegalovirus CSL CSL Ltd CT crossmatch:transfusion DAT direct antiglobulin test G&S group and screen GVHD graft versus host disease HLA Human leucocyte antigen IAT indirect antiglobulin test LIS low ionic strength LISS low ionic strength solution MBOS maximum blood order schedule MCT microcolumn techniques PEG polyethylene glycol QA quality assurance QC quality control SST serum separator tubes v/v volume/volume vol volume 24 APPENDIX 2 MAXIMUM BLOOD ORDER SCHEDULE (MBOS) This MBOS is intended as a guide. Each laboratory will need to assess the usual requirements for each procedure in the hospitals that they serve in conjunction with the surgeons performing the procedures. The crossmatch:transfusion (CT) ratio is a useful guide. Normally, those procedures with a CT ratio of greater than 2 can be considered as potential candidates for a group and hold protocol. Specialised surgical procedures eg. cardiac, hepatic, neurosurgery usually employ standard protocols developed in consultation with the laboratory. GENERAL SURGERY: ABDOMINO-PERINEAL RESECTION AMPUTATION : BELOW KNEE : ABOVE KNEE ANTERIOR RESECTION 2 G&S G&S 2 APPENDICECTOMY NIL APRONECTOMY/LIPECTOMY BOWEL RESECTION BREAST SURGERY :LUMPECTOMY :SIMPLE MASTECTOMY :RADICAL MASTECTOMY BURNS DEBRIDEMENT CHOLECYSTECTOMY COLECTOMY(formation or closure) GASTRECTOMY GASTRIC STAPLING HAEMORRHOIDECTOMY HIATUS HERNIA REPAIR :TRANSTHORACIC :ABDOMINAL INCISIONAL HERNIA REPAIR LAPAROTOMY G&S LUMBAR SYMPATHECTOMY PANCREATECTOMY PAROTIDECTOMY SPLENECTOMY THYROIDECTOMY VAGOTOMY and DRAINAGE VARICOSE VEINS STRIPPING G&S 2 G&S G&S G&S INDIVIDUAL ASSESSMENT G&S G&S 2 G&S NIL 2 G&S NIL G&S 2 G&S 2 G&S G&S NIL ETHMOIDECTOMY MASTOIDECTOMY RHINOPLASTY G&S TONSILLECTOMY TRACHOESTOMY NIL G&S G&S G&S GYNAECOLOGICAL SURGERY CAESAREAN COLPOSUSPENSION CONE BIOPSY NIL G&S G&S 25 D&C ECTOPIC HYSTERECTOMY LAPAROSCOPY MYOMECTOMY OVARIANCYSTECTOMY TERMINATION OF PREGNANCY TUBAL LIGATION VAGINAL REPAIR VULVECTOMY G&S NIL G&S G&S NIL G&S G&S G&S NIL G&S ORTHOPAEDIC SURGERY ARTHROSCOPY ARTHROTOMY NIL FEMORAL NAIL REMOVAL FRACTURES :FEMUR HARRINGTON'S RODS HIP REPLACEMENT KNEE REPLACEMENT LAMINECTOMY MENISECTOMY PUTTI-PLATT SPINAL FUSION SYNOVECTOMY (KNEE) NIL NIL 2 4 3 G&S G&S NIL G&S 2 G&S THORACIC SURGERY LOBECTOMY PLEURECTOMY PNEUMONECTOMY THYMECTOMY 2 2 4 2 UROLOGICAL SURGERY CYSTOSCOPY/OTOMY CYSTECTOMY 4 NEPHRECTOMY NEPHROLITHOTOMY PROSTATECTOMY (OPEN) PYELOLITHOTOMY TRANSURETHRAL RESECTION OF PROSTATE. URETEROLITHOTOMY NIL G&S G&S 2 G&S G&S G&S VASCULAR SURGERY AORTIC ANEURYSM - ELECTIVE AORTO-FEMORAL BYPASS GRAFT AORTO-ILIAC BYPASS GRAFT AV SHUNT CAROTID ENDARTERECTOMY FEMORO-POPLITEAL BYPASS GRAFT ILIO-FEMORAL BYPASS GRAFT SYMPATHECTOMY LUMBAR 4 4 4 NIL G&S 2 4 G&S 26 APPENDIX 3 BIBLIOGRAPHY 1. Issitt PD and Anstee, D: Applied Blood Group Serology (4th Ed.), Miami; Montgomery Scientific Publications 1998 2. American Association of Blood Banks: Technical Manual (12th Ed., 13th Ed, 14th Ed.), Bethesda; 1996, 1999, 2002 3. Judd WJ: Methods in Immunohaematology (2nd Ed), Miami; Montgomery Scientific Publications 1994 4. British Society for Haematology and British Blood Transfusion Society BCSH Blood Transfusion Task Force: Guidelines for microplate techniques in liquid phase blood grouping and antibody screening. Clinical Laboratory Haematology, 12:437-460, 1990 5. Australasian Society of Blood Transfusion: Leucodepletion/Irradiation Guidelines. Topics in Transfusion Medicine, Vol 3 No 2, 1996 6. Moroff, G and Luban, NLC: Prevention of transfusion-associated graft-versus-host disease. Transfusion, 32:102-103, 1992 7. British Council for Standardisation in Haematology Blood Transfusion Task Force: Guidelines for pretransfusion compatibility procedures in blood transfusion laboratories. Transfusion Medicine 6: 273-283, 1996 8. Standards Australia: Medical refrigeration equipment for storage of blood and blood products and containers for transport of blood and blood products. Australian Standard AS 3864-1997 9. Retention of Laboratory Records and Diagnostic Material. National Pathology Accreditation Advisory Council, 1998 10. American Association of Blood Banks: AABB STANDARDS (21st Ed.), 2002 11. Commonwealth Dept of Human Services and Health, Blood and Blood Components/Therapeutic Goods Administration: Australian Code of Good Manufacturing Practice for Therapeutic Goods (2nd Ed.), Canberra: Australian Govt. Pub. Service, 1995 12. Minimum standards for the collection, processing and quality assurance of blood and medicines derived from human blood and plasma. New Zealand Blood Service, 1998 13. British Council for Standardisation in Haematology Blood Transfusion Task Force: Guidelines for blood bank computing. Transfusion Medicine 10: 307-314, 2000. 14. Clinical Practice Guidelines [Red Cells, Platelets, Fresh Frozen Plasma, Cryoprecipitate], NHMRC / ASBT, October 2001. 15. Boppana.SB. et al. Intrauterine transmission of cytomegalovirus to infants of women with preconceptional immunity. N Eng J Med, 2001, May 3;344 (18): 1366-71. 16. Transfusion Reactions 2nd Ed, Mark A Popovsky, American Association of Blood Banks, 2002. 17. Maxwell EL, Metz J, Haeusler MN, Savoia HF. Use of red blood cell transfusions in surgery. ANZ J. Surg.2002; 72: 561-566. 27