Neurology 2015 UCL Institute of Neurology Presented by the March 26-27 2015
advertisement
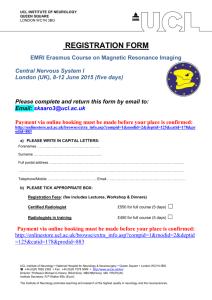
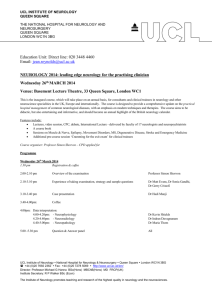
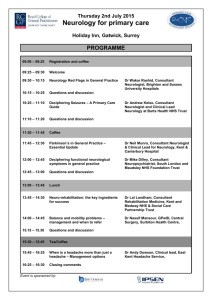
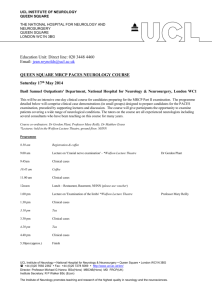
Neurology 2015 Leading-Edge Neurology for the Practising Clinician Presented by the UCL Institute of Neurology March 26-27 2015 Logan Hall, Institute of Education 20 Bedford Way, London WC1H 0AL Download course book at: www.tiny.cc/neur15book or scan the barcode with your smartphone 2015 Neurology UCL Institute of Neurology London March 26-27 InstituteAofANeurologyADirector ProfessoróMichaelóGóHanna A special thanks to Dr Suraj Rajan, MSc, MD for his work on the title logo for Neurology 2015 InstituteASecretary MróRobertóWalkeró Editors Mr Daniel CotfasóLó MróDavidóBlundred Neurology 2015 Lead Organiser ProfessoróSimonóShorvon This meeting is sponsored by the Pharmaceutical Industry with the presence of exhibition stands. There has been no Pharmaceutical Industry input to the scientific content of the meeting. TheóeditorsóareógratefulótoótheóQueenóSquareóLibrary:óWellcome Images, UCL Images Store and theóMedicalóIllustration Departmentóforósupplyingómanyóofó theóimagesóincludedóinóthisóbookletMóAllórightsóreservedM óóóóó óóóóóó óóóóóóóQ&B5:óUCLóInstituteóofóNeurology:óLondon UCLBInstituteBofBNeurologyBUCLBInstituteBofBNeurologyB|BNationalBHospitalBforBNeurologyB/BNeurosurgeryB|B B QueenBSquare2BBLondonBWCxNB8BGB|Bwww6ucl6ac6uk9io nBBBBBBB B BBBBB)55B4F(:FB769:B:86:B|BFax:)55B4F(:FB7:78B5F69B ChairAofANeurology ProfessoróMaryóReilly Director,ANHNN ProfessoróJohnóDuncan HeadAofAEducationAUnitA DróCarolineóSelaió HeadAofATeachingAandALearningASupportAA Mr David Blundredó SeniorAUnitAAdministratorAA MissóJeanóReynolds ó WELCOME TO NEUROLOGY 2015: Leading-edge Neurology for the Practising Clinician March 2015 Dear Colleagues, On behalf of the Executive Committee of UCL Institute of Neurology, it is a pleasure to welcome you to the Neurology 2015 course The aim of the course is to provide an update on the practical hospital management of common neurological diseases, with an emphasis on modern techniques and therapies. Its purpose is to be didactic, but also entertaining and informative. This programme book contains abstracts of the talks and also additional material provided by the speakers. The paper version also includes reprinted (with permission) full-text article. We hope the course will prove instructive, and we are keen to have feedback, so please do not hesitate to contact the organisers with any comments or suggestions. It is an annual event and your comments will be very helpful for planning for the future. Many people have been involved in assisting with the organization. Particular thanks go to Daniel Cotfas, David Blundred and Jean Reynolds in the Education Unit at the UCL Institute of Neurology for their contribution to the logistical aspects and the production of this programme. A special thanks go to all the speakers and presenters. We would also like to gratefully acknowledge the support of our sponsors (listed at the end of the programme book) which has made this conference possible. We have also added a selection of historical photographs as a visual survey of the history of Queen Square. These are kindly provided by the Department of Medical Illustration, the Queen Square Archives, Wellcome Images, UCL Image Store, Suraj Rajan, Barney Bryson, Bernadett Kalmar, David Werring, Kim Chisholm, Marija Sajic and Ken Smith. With best wishes, Simon Shorvon (On behalf of the UCL Institute of Neurology Executive Committee) Neurology 2015 Programme Thursday 26 – Friday 27 March 2015 Venue: Logan Hall, Institute of Education, Bedford Way, London Thursday, the 26th of March, 2015 Time Title Speaker Welcome Professor M Hanna 8.45 – 11.00 8.45 Topic 1: Leading edge therapy in acute neurology Chair: Professor S Shorvon What's new in Guillain Barré? Dr R Howard 9.30 The modern treatment of meningitis in hospital practice Advances in therapy of acute seizures and status epilepticus Coffee Break Dr S Farmer Nobel lecture: Membrane fusion and its implications for neurology Video Session: Eye movements and their disorders Professor J Rothman 8.00 – 8.40 8.40 10.15 11.00 – 11.30 11.30 12.05 – 12.45 12.45 – 13.45 13.45 – 16.00 13.45 Registration and coffee Professor S Shorvon Dr G Plant Lunch Topic 2: Clinical approach to neuromuscular disease Approach to diagnosis and management of peripheral neuropathy Approach to diagnosis and management of muscle disease Approach to diagnosis and management of diseases of the neuro-muscular junction Tea Break Chair: Professor D Kullmann Topic 3: Advanced therapy of headache and Parkinson’s Disease Management of migraine and other chronic headache syndromes Chair: Dr M Matharu 17.10 A pragmatic approach to treatment issues in early and late Parkinson’s Disease Professor K Bhatia 17.50 Reception 14.30 15.15 16.00 – 16.30 16.30 – 17.50 16.30 Professor M Reilly Professor M Hanna Professor D Kullmann Dr M Matharu Neurology 2015 Programme Thursday 26 – Friday 27 March 2015 Venue: Logan Hall, Institute of Education, Bedford Way, London Friday, the 27th of March, 2015 Time 8.00 – 8.45 8.45 – 11.00 8.45 9.30 10.15 Title Speaker Topic 4: Where decisions about therapy are difficult Chair: Dr J Chataway Balancing risk in the drug treatment of multiple sclerosis The place of surgery, chemotherapy and radiotherapy in the management of glioma Modern treatment of aneurysms and AVM Dr J Chataway Coffee Dr J Rees Miss J Grieve 11.00 – 11.30 11.30 – 12.05 Coffee Queen Square Town Hall meeting: Commissioning in Neurology Professor S Shorvon (chair), Dr C Mummery, Prof G Venables 12.05 CPC Dr M Lunn 12.45 – 13.45 13.45 – 16.00 13.45 Lunch 14.30 15.15 Topic 5: Neuropsychiatry and dementia Chair: Professor E Joyce Assessing dementia in clinical practice Professor M Rossor Neuropsychiatric disorders in Parkinson’s Disease and their management Prion disease - public health, CJD and therapy Professor E Joyce 16.00 – 16.30 16.30 – 17.50 16.30 Tea 17.10 Professor J Collinge Topic 6: Advances in Stroke Chair: Dr D Werring Advances and challenges in Stroke Dr D Werring Optimal management of TIA and stroke secondary to carotid atherosclerosis Professor M Brown What’s new in Guillain Barré? THURSDAY – 8:45AM by Dr Robin Howard Guillain Barré syndrome (GBS) remains an important neurological cause of severe, prolonged and often permanent disability and carries a significant mortality. It is increasingly recognised that GBS is a descriptive term for a group of acute immune demyelinating neuropathies that share overlapping sensory, motor and autonomic clinical features and characteristic laboratory and electrophysiological abnormalities. Over recent years there have been considerable advances in understanding the pathogenesis of acute demyelinating neuropathy which carries considerable implications for management. Whilst there are proven and effective treatments to reduce the effects of acute GBS, residual deficits are common and effective management encompasses both short-term immuno-modulation and longer term intensive care and rehabilitation. Dr Robin Howard Consultant Neurologist Senior Lecturer UCL Institute of Neurology Dr Howard is Consultant Neurologist at the National Hospital, Queen Square and St. Thomas’ Hospital, and Senior Lecturer at The Institute of Neurology, University College and King’s College. He qualified from Cambridge University and the Middlesex Hospital in 1980, undertook training in Oxford and London and was appointed to his present post in 1992. He is Head of Service for a large general neurological practice at St. Thomas’ and neurologist to 3 intensive care units. His major specialty interests are intensive care neurology and neuromuscular diseases including myasthenia gravis, motor neurone disease, post-polio syndrome and sleep disorders. Selected Publications ‒ Wakerley BR, Yuki N. Mimic and chameleons in Guillain Barre and Miller Fisher Syndromes. Pract Neurol 2014;0:1–10. ‒ Robin S Howard, S Veronica Tan, Werner J Z’Graggen. Weakness on the intensive care unit. Pract Neurol 2008; 8: 280–295 For more information visit: www.tiny.cc/rhoward or scan the QR code robin.howard@ucl.ac.uk THURSDAY – 9:30AM The modern treatment of meningitis in hospital practice by Dr Simon Farmer Bacterial Meningitis has a world wide incidence of between 1 and 4 per 100,000 of the population with a mortality of 35%. A significant number of survivors are left with serious neurological sequelae of the disease. With vaccination, improved nutrition and public health its incidence in developed countries is falling but it remains in modern hospital practice a serious cause of neurological mortality and morbidity, especially in immune suppressed patients. Rapid diagnosis and treatment of the meningitis is the main determinant of outcome. The strategies for rapid diagnosis and intensive treatment will be reviewed. Dr Farmer qualified from Bristol University in 1986. He trained in neurology and general medicine at the Royal London Hospital, NHNN and at St Mary’s Hospital, London. He was appointed consultant neurologist between St Mary’s Hospital and the National Hospital in 1996, and is on the staff of King Edward VII Hospital in London. His dominant neurological practice is general neurology. He covered acute in patient neurology at St Mary’s Hospital and at the National Hospital. He consulted on HIV positive patients and on immune suppressed patients at St Mary’s. He also provided neurology input to the paediatric meningitis unit at St Mary’s Hospital. He is a principal investigator at the Institute of Neurology and Associate Clinical Director for Neurology at NHNN. He has published over 100 articles in clinical and basic neuroscience and has contributed to several neurology text books Selected Publications ‒ Karen Edmond, Andrew Clark, Viola S Korczak, Colin Sanderson, Ulla K Griffiths, Igor Rudan. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. Lancet Infect Dis 2010; 10: 317–28 ‒ Natalie G Martin, Manish Sadarangani, Andrew J Pollard, Michael J Goldacre. Hospital admission rates for meningitis and septicaemia caused by Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae in children in England over five decades: a population-based observational study. Lancet Infect Dis 2014; 14 ‒ Russell M Viner, Robert Booy, Helen Johnson, W John Edmunds, Lee Hudson, Helen Bedford, Ed Kaczmarski, Kaukab Rajput, Mary Ramsay, Deborah Christie. Outcomes of invasive meningococcal serogroup B disease in children and adolescents (MOSAIC): a casecontrol study. Lancet Neurol 2012; 11: 774–83 Dr Simon Farmer PhD FRCP Consultant Neurologist and Associate Clinical Director National Hospital for Neurology & Neurosurgery (NHNN) For more information visit: www.tiny.cc/sfarmer or scan the QR code simon.farmer@uclh.nhs.uk THURSDAY - 10:15AM Advances in therapy of acute seizures and status epilepticus by Professor Simon Shorvon In recent years, there have been significant advances in the treatment of acute seizures and status, and these will be reviewed in this talk. In acute seizures and the early phase of status epilepticus, new buccal, intramuscular and intra-nasal therapies have been developed and have replaced the use of intravenous or rectal therapies in out-of-hospital settings. The advantages and characteristics of these are now well established and will be discussed. At the other end of the spectrum, the concept of super-refractory status epilepticus has been recently established, referring to status which does not respond to initial anaesthetic therapy in the ITU setting. This is a not uncommon clinical situation, with high morbidity and mortality. Therapy is empirical and unsatisfactory. This is also the subject of a global audit. The talk will focus on these points. Simon Shorvon was appointed Consultant Neurologist at the National Hospital for Neurology and Neurosurgery, Queen Square, London in 1983. He has held various posts including the Chair in Clinical Neurology, Head of the Department of Clinical Neurology, Head of the Epilepsy Research Group and is also Clinical Sub-Dean at the Institute of Neurology. He is Chairman of the Medical Committee at the National Hospital Queen Square, Harveian Librarian at the Royal College of Physicians and until 2014, President of the British Branch of the International League Against Epilepsy (ILAE). He served as a member of the international Executive Committee of the ILAE for 16 years, previously as ILAE Vice-President and as co-Editor-in-Chief of EPILEPSIA. He is recipient of lifetime achievement awards for work in epilepsy including 2008 European Epileptology Award, 2010 Lennox Prize of the American Epilepsy Society and the TS Shrinivasan award. Status epilepticus is one of his interests and he has written a monograph on the subject and organises the biannual status epilepticus colloquia, the next one of which is in London in April 2015. Selected Publications ‒ Anderson GD, Saneto RP. Current oral and non-oral routes of antiepileptic drug delivery. Adv Drug Deliv Rev. 2012 ;64(10):911-8. ‒ Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011 Oct;134(Pt 10):2802-18. Professor Simon Shorvon Consultant Neurologist Professor of Clinical Neurology UCL Institute of Neurology For more information visit: www.tiny.cc/sshorvon or scan the QR code s.shorvon@ucl.ac.uk THURSDAY – 11:30AM Nobel lecture: Membrane fusion and its implications for neurology by Professor James Rothman Information is passed between nerve cells and synaptic connections by neurotransmitters, which must be released synchronously with electrical activity. Synchronous release is due to just three proteins. SNARE proteins fuse the synaptic vesicles which store neuro-transmitters at nerve endings with the nearby nerve surface membrane. Complexin acts as a clamp to block SNAREs half-way through the fusion process by cross-linking them. The calcium ion sensor Synaptotagmin reverses the clamp and facilitates fusion but only when it binds calcium, which enters the presynaptic nerve in response to the electrical signal, synchronizing release to electrical action potentials. Recent results provide a structural biochemical basis for this vital physiological process. Professor Rothman, the Wallace Professor of the Biomedical Sciences at Yale University, is one of the world's most distinguished biochemists and cell biologists. He is Chairman of the Yale School of Medicine’s Department of Cell Biology and is the Director and founder of the Nanobiology Institute at Yale, and is a research professor at UCL. Professor James Rothman Visiting Research Professor UCL Institute of Neurology He is renowned for discovering the molecular machinery responsible for transfer of materials among compartments within cells. In so doing, he provided a unified conceptual framework for understanding such diverse and important processes as the release of insulin into the blood, communication between nerve cells in the brain, and the entry of viruses to infect cells. Numerous kinds of tiny membrane-enveloped vesicles ferry packets of enclosed cargo. Each type of vesicle must somehow deliver its specialized cargo to the correct destination among the maze of distinct compartments that comprise the cytoplasm of a complex animal cell. The delivery process, termed membrane fusion, is fundamental for physiology and medicine, as pathology in this process can cause metabolic, neuropsychiatric and other diseases. He has received numerous awards and honors in recognition of his work, notably the Nobel prize for Physiology or Medicine (2013). He is a member of the National Academy of Sciences (1993) and its Institute of Medicine (1995), and a Fellow of the American Academy of Arts and Sciences (1994). Selected Publications ‒ http://www.nobelprize.org/nobel_prizes/medicine/laureates/2013/roth man-lecture.html For more information visit: www.tiny.cc/jrothman or scan the QR code james.rothman@ucl.ac.uk THURSDAY – 12:05PM Video session: Eye movements and their disorders by Dr Gordon Plant Disorders of the central nervous system often cause abnormalities of eye movements. I will present a system for assessing such disorders at the bedside (excluding disorders of the III, IV and VI nerves and nystagmus). The patient is first of all asked to fix on a distant target and the eyes observed for stability of fixation – are there saccadic intrusions or nystagmus? An accommodative target is then introduced and near fixation examined to test the vergence system and the near response. Fixation should then be held with the eyes in various eccentric gaze positions to examine for nystagmus. The patient is then asked to follow the same target to examine smooth pursuit in the four cardinal directions (vertical, up and down; horizontal, left and right). A second target is now introduced and the patient instructed to look from one target to the other thus generating saccadic eye movements, again in the four cardinal directions. It may be useful to examine saccades of larger and smaller amplitude. The optokinetic drum may be used as an additional means of examining smooth pursuit and saccades. Lastly the oculocephalic reflex, the head thrust test and change in the orientation of the head in relation to gravity should be used to test the integrity of the vestibular influence on the ocular motor system. Dr Plant trained at Cambridge and St Thomas’, and further trained in Neurology at Queen Square attending clinics at Moorfields throughout to obtain experience in Ophthalmology. After a year as an MRC Travelling Fellow in San Francisco at the Smith Kettlewell Eye Research Institute and UCSF he took up, in 1991, his present post as Consultant Neurologist at Queen Square, Moorfields and St Thomas’. A Fellow of the Royal College of Physicians and Royal College of Ophthalmologists, Senior Lecturer at UCL and Visiting Professor at City University in London and Wills Eye Institute in Philadelphia. He is editor-in-chief of Neuro-Ophthalmology, founder of the UK Neuro-Ophthalmology Special Interest Group and a past President of the Clinical Neurosciences section of the Royal Society of Medicine. He has given numerous named lectures and published over 300 peer reviewed research papers. His clinical and research interests encompass most areas of the Neurology of Vision. He is particularly interested in promoting research and training in Medical Ophthalmology. Selected Publications ‒ Pau D, Al Zubidi N, Yalamanchili S, Plant GT, Lee AG. Optic neuritis. Eye (Lond). 2011 Jul; 25(7):833-42. doi:10.1038/eye.2011.81. Dr Gordon Plant Consultant Neurologist Senior Lecturer UCL Institute of Neurology For more information visit: www.tiny.cc/gplant or scan the QR code gordon.plant@uclh.nhs.uk THURSDAY – 1:45PM Approach to diagnosis and management of peripheral neuropathy by Professor Mary Reilly The diagnosis of a peripheral neuropathy relies heavily on a detailed clinical examination whereas the diagnosis of the cause of the neuropathy is refined by both the history and the examination. Slowly progressive longstanding length dependent neuropathies suggest a hereditary cause such as Charcot Marie Tooth disease (CMT) whereas a more rapid progression of a patchy neuropathy often points to an inflammatory cause such as chronic inflammatory polyradiculoneuropathy (CIDP) or, if painful, vasculitis. Nerve conduction studies and EMG are essential diagnostically especially in the classification of neuropathies into demyelinating or axonal, clarifying the presence and degree of motor and / or sensory involvement and in ascertaining various patterns. As with any disease the initial diagnostic aim is not to miss a treatable cause and a wide range of blood tests are used depending on the diagnostic suspicion. Skin biopsies for epidermal nerve fiber density are increasingly used in the diagnosis of small fiber neuropathy and the use of nerve and muscle imaging with both MRI and ultrasound is increasing. Therapies will be reviewed and range from symptomatic therapies e.g. pain relief, orthosis etc to immunotherapy and chemotherapy for inflammatory and myelodysplastic associated neuropathies. Professor Mary Reilly Consultant Neurologist Professor of Clinical Neurology UCL Institute of Neurology Mary M. Reilly was appointed a consultant neurologist at Queen Square in 1998 and a Professor of Clinical Neurology at UCL in 2010. Since 1998, she is head of the peripheral nerve services in the National Hospital for Neurology and Neurosurgery and has an active research program in genetic neuropathies. She is co-director of the MRC Centre for Neuromuscular Diseases in Queen Square, a past president of the British Peripheral Nerve Society, president elect of the international Peripheral Nerve Society and a council member of the Association of British Neurologists. She received her FRCP in 2002 and her FRCPI in 2003. Selected Publications ‒ Neligan A, Reilly MM, Lunn MP. CIDP: mimics and chameleons. Practical Neurol. 2014 Jul 17. ‒ Rossor AM, Polke JM, Houlden H, Reilly MM. Clinical implications of genetic advances in Charcot-Marie-Tooth disease. Nat Rev Neurol. 2013 Oct;9(10):562-71. For more information visit: www.tiny.cc/mreilly or scan the QR code m.reilly@ucl.ac.uk THURSDAY – 2:30PM Approach to diagnosis and management of muscle disease by Professor Michael Hanna Muscle diseases impair mobility and not infrequently cause serious cardiorespiratory complications. Their age of onset and severity is extremely wide; ranging from neonatal death, through young onset severe life-long disability to late onset mild phenotypes. About 90 000 people in the UK have one of the diverse group of genetic or acquired conditions which make up the primary muscle diseases. A great many more patients have muscle weakness due to complications of drugs or systemic diseases such as cancer. The important acquired muscle diseases include the inflammatory myopathies which are treatable and so the diagnosis must not be missed (or over diagnosed), as well as the drug-induced myopathies. There is also an important large number of primary genetic muscle diseases including dystrophies, congenital myopathies, metabolic disorders (including mitochondrial) and channelopathies. Some of the most rapid molecular and post-genomic advances in neurology have occurred in the field of muscle disease resulting in an advanced understanding of molecular pathophysiology. This understanding has led to an increasing number of experimental clinical trials targeting specific disease mechanisms. It seems most likely that there will be translation of these advances into new treatments in clinical practice in the next few years. Professor Michael Hanna is Director of the UCL Institute of Neurology. He is Professor of Clinical Neurology and Consultant Neurologist specialising in neuromuscular diseases at the National Hospital Queen Square. He is Director of the MRC Centre for translational research in neuromuscular diseases, which was established in 2008 and renewed in 2013. This joint London- Newcastle MRC Centre links basic science advances to clinical trials in patients with a range of neuromuscular diseases. He also leads the Queen Square Centre provision of a nationally commissioned highly specialised clinical and genetic diagnostic service for mitochondrial diseases and muscle channelopathies. Selected Publications ‒ Merrison AF, Hanna MG. The bare essentials: muscle disease. Pract Neurol. 2009 :54-65. PMID: 19151243. ‒ Rahman S, Hanna MG. Diagnosis and therapy in neuromuscular disorders: diagnosis and new treatments in mitochondrial diseases. J Neurol Neurosurg Psychiatry. 2009;80(9):943-53 Professor Michael Hanna Consultant Neurologist Professor of Clinical Neurology UCL Institute of Neurology For more information visit: www.tiny.cc/mhanna or scan the QR code m.hanna@ucl.ac.uk THURSDAY – 3:15PM Approach to diagnosis and management of diseases of the neuro-muscular junction by Professor Dimitri Kullmann Myasthenia gravis is an under-recognised cause of neuromuscular weakness, especially in the elderly. Seronegative myasthenia can present diagnostic challenges. Although most cases of myasthenia can be managed with anticholinesterase medication and immunosuppression, some refractory cases require intravenous immunoglobulin, plasma exchange or monoclonal antibody treatment. This talk will also discuss the role of thymectomy, and the diagnosis and management of Lambert-Eaton myasthenic syndrome, botulism and congenital myasthenic disorders. Dimitri Kullmann has a research interest in fundamental mechanisms of synaptic transmission, circuit neuroscience and gene therapy for epilepsy. He specializes clinically in myasthenia and neuro-critical care at the National Hospital for Neurology and Neurosurgery. He established his own laboratory at the Institute of Neurology in 1992, and has held an MRC Senior Clinical Fellowship, was Head of the Department of Clinical and Experimental Epilepsy, and is a Fellow of the Academy of Medical Sciences. Since 2014 he has been the editor in chief of Brain. Professor Dimitri Kullman, FMedSci Consultant Neurologist Professor of Neurology UCL Institute of Neurology Selected Publications ‒ Spillane J, Beeson DJ, Kullmann DM. Myasthenia and related disorders of the neuromuscular junction. J Neurol Neurosurg Psychiatry. 2010 Aug;81(8):850-7. ‒ Spillane, J., Sidle, K. C., Kullmann, D. M., Christofi, G., & Howard, R. S. (2013). Myasthenia gravis and neuromyelitis optica: A causal link. Multiple Sclerosis and Related Disorders, 2 (3), 233-237. doi:10.1016/j.msard.2013.01.003 ‒ Schapira, A. H. (2004). Disease of muscle and the neuromuscular junction. Clinical Neurology, 130-153. For more information visit: www.tiny.cc/dkullmann or scan the QR code d.kullmann@ucl.ac.uk THURSDAY – 4:30PM Management of migraine and other chronic headache syndromes by Dr Manjit Matharu Chronic daily headache (CDH) is a major worldwide health problem that affects 3–5% of the population and results in substantial disability. Besides migraine, several other primary headaches can cause CDH including tension-type headache, new daily persistent headache and the trigeminal autonomic cephalalgias. The management of these headaches involves addressing lifestyle factors and treatment with acute and preventive medical treatments. Recent advances are leading to the introduction of new therapies for these headache disorders. Advances in the management of headache disorders have meant that a substantial proportion of patients can be effectively treated with medical treatments. However, a significant minority of these patients are intractable to conventional medical treatments. While a substantial proportion of patients can be effectively treated with medical treatments, a significant minority of these patients are intractable to conventional medical treatments. Neurostimulation therapies that entail non-invasive and invasive peripheral or central nervous system targets are emerging as very promising approaches. Dr Manjit Matharu Consultant Neurologist Senior Lecturer UCL Institute of Neurology Dr Matharu is a Senior Lecturer at the Institute of Neurology and Honorary Consultant Neurologist at the National Hospital for Neurology and Neurosurgery, Queen square, London, UK. He is the Academic and Clinical lead of the Headache Group. His major research interests include interventional therapies for intractable headaches, trigeminal autonomic cephalalgias, and functional imaging in primary headaches. He is a member of the education subcommittee of the International Headache Society, and the Headache and Pain Subcommittee of The Association of British Neurologists (ABN). He was a member of the National Institute for Health and Clinical Excellence (NICE) guideline development group (GDG) for Headache Disorders. Selected Publications ‒ Nagy AJ, Rapoport AM. Update on future headache treatments. Neurol Sci. 2013 May;34 Suppl 1:S101-8. ‒ Miller S, Matharu M. Trigeminal autonomic cephalalgias: beyond the conventional treatments. Curr Pain Headache Rep. 2014 Aug;18(8):438 ‒ Lambru, G. and M. S. Matharu (2014). "Peripheral neurostimulation in primary headaches." Neurol Sci 35 Suppl 1: 77-81. For more information visit: www.tiny.cc/mmatharu or scan the QR code manjit.matharu@ucl.ac.uk THURSDAY – 5:10PM A pragmatic approach to treatment issues in early and late Parkinson’s Disease by Professor Kailash Bhatia Parkinson’s Disease is an evolving condition with a number of motor and non-motor features both related to the disease progression and also to dopaminergic drug treatments. A number of different drugs are available for treating the symptoms of Parkinson’s Disease. Hence clinicians require an outline of different strategies for the management of these motor and non-motor symptoms. In this regard we will consider the use of symptomatic dopaminergic drugs including the question of dopamine agonists versus levodopa. In addition we will look at the use of Mao-B inhibitors, COMT inhibitors and Amantidine. The management of levodopa induced dyskinesia and fluctuations will be discussed as well as issues regarding the use of duodopa and deep brain stimulation surgery for advanced PD. Finally it’s crucial also to consider the management of cognitive and neuropsychiatric features in the setting of PD. Kailash Bhatia is a Professor of Clinical Neurology at the UCL Institute of Neurology, and Honorary Consultant Neurologist at the affiliated National Hospital at Queen Square. He obtained his basic medical degree and neurology training in Mumbai, India and further training in neurogenetics and movement disorders with the late Professor’s Anita Harding and David Marsden. He is a Fellow of the Royal College of Physicians and corresponding Fellow of the American Academy of Neurology. His main research interest is in movement disorders, merging clinical, electrophysiological, and genetic methods to study the pathophysiology of conditions like dystonia and Parkinson’s Disease. Professor Bhatia has over 480 publications including 380 peer reviewed papers. He has been an Associate Editor of the Movement Disorders Journal and is the current editor of Movement Disorders Clinical Practice Journal. He is a grant reviewer for Telethon, Inserm France, UK PD society and a medical advisor to the UK Dystonia society. He serves the scientific board of the Bachman Strauss trust and is on the Executive Committee of The International Parkinson’s Disease and Movement Disorders Society. Selected Publications ‒ Massano J, Bhatia K. Clinical approach to Parkinson's Disease: features, diagnosis and principles of management. Cold Spring Harb Perspect Med 2012;2:a008870 Professor Kailash Bhatia, MD, DM, FRCP Consultant Neurologist Professor of Clinical Neurology UCL Institute of Neurology For more information visit: www.tiny.cc/kbhatia or scan the QR code k.bhatia@ucl.ac.uk FRIDAY – 8:45AM Balancing risk in the drug treatment of multiple sclerosis by Dr Jeremy Chataway There has not been a more exciting time to be involved in the management of multiple sclerosis (MS). Over the last 20 years has come an increasing number of agents (disease modifying treatments: DMT) which can reduce the attack rate in relapsing-remitting MS (RRMS). These range from first line (beta-interferons/copaxone) which reduce the rate by 30%; to oral agents (e.g. fingolimod) which can reduce it by 50%: to monoclonal antibodies (e.g. alemtuzumab) which can reduce it by nearly 80%. However with the increase in potency has come the increase in rare, but serious side-effects. These range from Progressive Multifocal Leukoencephalopathy (PML) to significant thyroid dysfunction to cardiac dysrthythmias. The debate now, is not whether to use an agent, but whether an escalation or induction approach is optimal. This talk will examine these issues. Dr Jeremy Chataway, MA, PhD, FRCP Consultant Neurologist Honorary Senior Lecturer UCL Institute of Neurology Dr Chataway is the clinical lead of the MS group at NHNN (about 3000 patients) and was a member of the 2014 MS NICE panel. He has a particular interest in clinical trial design and was the Chief Investigator (CI) of the recently reported MS-STAT trial in secondary progressive MS, using high dose simvastatin; and is the CI of the recruiting MS-SMART trial. He sits on the UK MS Society Grant Review Panel for Care and Services Research and UK MS Society Clinical Trials Network Steering Group; and works with the Comprehensive Clinical Trials Unit. He is keen to facilitate both trial design and implementation. Selected Publications ‒ Multiple Sclerosis: Current and Emerging Disease-Modifying Therapies and Treatment Strategies: Dean M. Wingerchuk, Jonathan L. Carter: Mayo Clinic Proceedings. Volume 89, Issue 2, February 2014, Pages 225–240 ‒ The new therapeutic landscape in multiple sclerosis: exciting times and new perspectives: Hartung, Hans-Peter; Kieseier, Bernd C. Current Opinion in Neurology: June 2014 - Volume 27 - Issue 3 - p 243–245 For more information visit: www.tiny.cc/jchataway or scan the QR code j.chataway@ucl.ac.uk FRIDAY –9:30AM The place of surgery, chemotherapy and radiotherapy in the management of glioma by Dr Jeremy Rees Gliomas represent the most common primary intracranial brain tumour and, with few exceptions, remain incurable. However, improvements in the safety and delivery of modern treatments have extended the quality of patients’ lives and, in some cases, their survival. Surgery, radiotherapy, and chemotherapy still form the cornerstone of management of glioma, and technical advances in these treatments have led to improvements in morbidity and survival, particularly over the last decade. In line with other areas of oncology, there is increasing use of combination therapies, particularly concomitant chemoradiation to improve survival. Targeted biological agents, gene therapy, and immunotherapy are under active investigation but have still not been widely taken up clinically because of the lack of proven benefit over and above standard therapies. There are some exciting new treatments, currently being evaluated, which offer hope for much better survival in malignant glioma Dr Jeremy Rees Consultant Neurologist Honorary Senior Lecturer UCL Institute of Neurology Dr Jeremy Rees qualified in 1988 from University College and Middlesex Medical School with distinctions in Medicine, Surgery and Therapeutics. After postgraduate training, including a period at Memorial Sloan Kettering Hospital, New York, in 1999 he was appointed as Honorary Senior lecturer in Neuro-oncology and Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. He specializes in the management of low-grade brain tumours and neurological complications of cancer. He has been the Clinical Lead for the Brain Tumour Unit at NHNN and is the Pathway Director for Brain Cancer at London Cancer, an Integrated Cancer System. He has carried out extensive research into multimodality imaging of Low Grade Gliomas, has edited a textbook on Neurooncology, and written numerous peer-reviewed research papers and chapters on Brain Tumours. Selected Publications ‒ Rees JH. Diagnosis and treatment in neuro-oncology: an oncological Perspective. The British Journal of Radiology, 84 (2011), S82–S89 ‒ Bradley D, Rees J. Updates in the management of high-grade glioma.. J Neurol. 2014 ; 261:651-4 For more information visit: www.tiny.cc/jrees or scan the QR code jeremy.rees@ucl.ac.uk Modern treatment of aneurysms and AVM FRIDAY – 10:15AM by Ms Joan Grieve Aneurysms most commonly present following a subarachnoid haemorrhage, or rarely a focal neurological deficit. Arteriovenous malformations may present with subarachnoid or intracerebral haemorrhage, epilepsy or progressive focal deficit. With the advent of MRI, many aneurysms and arteriovenous malformations are also now discovered coincidentally. Advances in treatment modalities are occurring more rapidly than advances in our knowledge of the natural history of these lesions, especially if presenting prior to haemorrhage. This means that decision-making regarding optimal management can be extremely difficult and requires a multidisciplinary approach. There has been a progressive shift from open surgical procedures to endovascular approaches as the technology to deal with more complex lesions has evolved and developed. This has also been driven by patient choice as well as perceived benefits to health economics. The treatment modalities available for management of these lesions and the patient, clinical and radiological factors considered when planning their treatment will be discussed. Ms Joan Grieve Consultant Neurosurgeon National Hospital for Neurology and Neurosurgery Joan Grieve has been a Consultant Neurosurgeon at the National Hospital for Neurology and Neurosurgery since 2002. She has a particular interest in vascular and pituitary subspecialties. She trained at St George's Medical School and undertook her neurosurgical training at Atkinson Morley's Hospital, Great Ormond Street Hospital for Children and The National Hospital for Neurology and Neurosurgery, obtaining FRCS(SN) in 2000. She was successful in being awarded an MD in 2004 entitled 'Novel Structural and Functional Imaging Techniques in Cerebral Arteriovenous Malformations' following 2 years of research at Queen Square. Selected Publications ‒ Advances in endovascular approaches to cerebral aneurysms. Dumont TM1, Eller JL, Mokin M, Sorkin GC, Levy EI. Neurosurgery. 2014 Feb;74 Suppl 1:S17-31. ‒ Contrast-enhanced magnetic resonance angiography in intracranial giant aneurysms. H.R.Jäger, H.Ellamushi, E.A.Moore, J.P.Grieve, W.Taylor, N.D.Kitchen. American Journal of Neuroradiology 2000; 21: 1900-1907. For more information visit: www.tiny.cc/jgrieve or scan the QR code joan.grieve@uclh.nhs.uk Clinicopathological conference (CPC) Presented by: Dr Michael Lunn, Dr Rahul Phadke and others Discussant: Dr Jeremy Rees, National Hospital for Neurology and Neurosurgery History 59 year old man was admitted to NHNN for investigation. He gave a nine month history of left foot beginning with tripping. This was associated with some abnormal sensation in the 2nd-4th toes of L foot, as if they had been immersed for hours in water. There were some intermittent spasms and cramps of the left leg which also steadily became weaker. Over the following months there was progressive weakness of the left foot requiring an AFO. In the 2/12 prior to admission, fasciculation was described in upper and lower limbs. There was difficulty climbing stairs and rising from chairs in the month prior to admission. For several weeks he had had urgency of urine with less than 5 minutes notice to pass water, and had had several incontinence episodes per week. His hearing, speech and swallowing were normal. He was emotionally normal with normal cognitive function. There was no relevant past medical history, no family history, no relevant travel history, medical or social exposure and he had a normal diet. Examination CNs normal: Eye examination was normal, JJ negative, no facial weakness, tongue normal. No muscle wasting in the limbs Bilateral deltoid and trapezius fasciculation were seen but there was normal strength. Brisk reflexes including pectoralis and trapezius jerks. Abdominal jerks absent. Spastic paraparesis with asymmetric L>R proximal and distal weakness. Brisk knee and ankle jerks, L extensor plantar response and normal vibration, JPS and pinprick sensation. No cerebellar signs. General physical examination was normal: weight normal, cardiovascularly normal, skin normal, testes normal. Investigations NCS: Sural SNAPs 6uV and 3 uV. Motor – median DML 4.3ms, amp 6.8mV, CV 47ms-1 F 34ms, ulnar DML 3.2ms, amp 11.1mV, CV 47ms-1 F 36ms, peroneal (EDB) DML 5.0ms, amp 2.0mV, CV 33ms-1 F 63ms. EMG evidence for non-lengthdependent denervation affecting 2 body regions. MRI brain and spine showed some atrophy Other investigations were performed to reach a diagnosis. Clinicopathological conference (CPC) FRIDAY – 12:05AM by Dr Michael Lunn Dr Michael Lunn is a Consultant Neurologist, Clinical Lead in Neuroimmunology and Honorary Senior Lecturer at the National Hospital for Neurology, Queen Square. His clinical and research interests are in the inflammatory neuropathies, particularly Guillain-Barré syndrome, CIDP, POEMS syndrome and other paraproteinaemic neuropathies. He also has an interest in clinical trials, in outcome measures used for measurement in clinical trials of neuropathic diseases and evidence synthesis and meta-analysis to improve future trial design and extract more information from trials with inadequate designs which together can suggest or confirm more significant clinical effects of therapy. Dr Michael Lunn Consultant Neurologist National Hospital for Neurology and Neurosurgery His out-patient practice as part of the Peripheral Nerve Service in the MRC Centre for Neuromuscular Disease at the National Hospital covers all inflammatory neuropathies with multidisciplinary support from neurophysiologists and nurse specialists. He works closely with the ITU team at the National Hospital Dr Lunn has published original papers, reviews and book chapters on aspects of inflammatory peripheral neuropathies, cited over 1100 times since 2009 and with an H-Index now at 20. He is Coordinating Editor of the Cochrane Neuromuscular Disease Group, managing, performing and publishing reviews of evidence based practice across the whole field of neuromuscular disease. For more information visit: www.tiny.cc/mlunn or scan the QR code michael.lunn@ucl.ac.uk Assessing dementia in clinical practice Assessing patients with cognitive impairment can be a major challenge in a busy neurology clinic. Not only can it be time consuming to assess the different domains of cognitive function but since cognition is very sensitive to ill health it is necessary to ensure that systemic determinants of dementia or co-morbidities worsening dementia are not missed. A structured approach is important. History from a family or friend is essential and the examination can start while the history is being taken by careful observation of the patient and informant. The broad categories of delirium, subcortical dementia and cortical dementia, whilst imprecise, can provide a useful framework as can the concept of ‘dementia plus’, i.e. cognitive impairment in the setting of additional neurological deficits. A structured approach will be discussed with illustrative videos. FRIDAY – 1:45PM by Professor Martin Rossor Professor Martin Rossor Consultant Neurologist Professor of Clinical Neurology UCL Institute of Neurology Martin Rossor trained in Neurology at the National Hospital, Queen Square and undertook research into the neurochemistry of degenerative dementia at the MRC Neurochemical Pharmacology Unit, Cambridge. He is a Professor of Clinical Neurology at the National Hospital for Neurology and Neurosurgery, and established a specialist cognitive disorders clinic which acts as a tertiary referral service for young onset and rare dementias. Clinical research interests are in the degenerative dementias and particularly in familial disease. He was editor of the Journal of Neurology, Neurosurgery & Psychiatry, and President of the Association of British Neurologists. Martin is the NIHR National Director for Dementia Research , Director of the NIHR Queen Square Dementia Biomedical Research Unit and a NIHR Senior Investigator. Selected Publications ‒ Martin N Rossor, Nick C Fox, Catherine J Mummery, Jonathan M Schott, Jason D Warren. Diagnosis of young-onset dementia. Lancet neurology 2010 9: 793-806. For more information visit: www.tiny.cc/mrossor or scan the QR code m.rossor@ucl.ac.uk FRIDAY – 2:30PM Neuropsychiatric disorders in Parkinson’s Disease and their management by Professor Eileen Joyce It is increasingly recognised that Parkinson's Disease is more than a movement disorder. Neuropsychiatric manifestations are a prominent aspect of the syndrome in both the early and late phases of the disease. These include: mood and anxiety disorders; cognitive impairment and dementia; psychosis and iatrogenic impulse control disorders. These symptom clusters and their timing can be explained by the spread of neuropathology throughout the brain. Alpha-synuclein is deposited early in brain stem serotonergic and noradrenergic nuclei and thereafter midbrain dopamine cell bodies, not only in the substantia nigra motor nucleus but also in the ventral tegmental area. This is followed by forebrain involvement of basal cholinergic nuclei and limbic and association cortex. The progressive pathology of Parkinson's Disease perturbates neural systems known to be dysfunctional in psychiatric disorders thus explaining symptom development. Understanding the underlying neuropathology of Parkinson's Disease informs treatment strategies. Professor Eileen Joyce Consultant Neuropsychiatrist Professor of Psychiatry UCL Institute of Neurology Eileen Joyce is Professor of Neuropsychiatry at the UCL Institute of Neurology and Honorary Consultant Neuropsychiatrist at the National Hospital for Neurology and Neurosurgery. Professor Joyce received a degree in psychology from the University of Cambridge where she also completed her PhD in dopamine psychopharmacology with Susan Iversen. She went on to study medicine at Cambridge and trained in psychiatry at the Maudsley Hospital. She spent her higher clinical and research training in the neuropsychiatry department of Professor Alwyn Lishman which was followed by a period of time as a research associate at The National Institute on Alcohol Abuse and Alcoholism, USA. She returned to the UK in 1991 to take up a senior lectureship at Imperial College and remained there until 2005 when she moved to University College London. Selected Publications ‒ Gallagher DA, Schrag A. (2012) Psychosis, apathy, depression and anxiety in Parkinson's Disease, Neurobiology of Disease 46: 581–589. For more information visit: www.tiny.cc/ejoyce or scan the QR code e.joyce@ucl.ac.uk Prion disease - public health, CJD and therapy John Collinge is Professor of Neurology and Head of the Department of Neurodegenerative Disease at the UCL Institute of Neurology, and Director of the MRC Prion Unit. He also directs the NHS National Prion Clinic at the adjacent National Hospital for Neurology and Neurosurgery. Professor Collinge trained in medicine at the University of Bristol and in neurology at St Mary’s Hospital and the National Hospital for Neurology and Neurosurgery in London. He is committed to highly multidisciplinary research and the seamless integration of basic laboratory and clinical research. He established the MRC Prion Unit at Imperial College in 1998 where he held the positions of Wellcome Senior Clinical Fellow and then Wellcome Principal Clinical Fellow. His laboratory demonstrated in 1996 that the new human prion disease, variant CJD, was caused by the same prion strain as that causing BSE in cattle and has been responsible for a number of key advances in the field. Professor Collinge has served on numerous Government advisory committees on prion disease at a national, European Union and international level. He is committed to public communication of the Unit’s research and gives many media interviews. He is a Founder Fellow of the Academy of Medical Sciences, a Fellow of the Royal Society and was awarded a CBE for services to medical research. Selected Publications ‒ Lloyd SE, Mead S, Collinge J. Genetics of prion diseases. Curr Opin Genet Dev. 2013 Jun;23(3):345-51. ‒ Thompson A, MacKay A, Rudge P, Lukic A, Porter MC, Lowe J, Collinge J, Mead S. Behavioral and psychiatric symptoms in prion disease. Am J Psychiatry. 2014 Mar 1;171(3):265-74. FRIDAY – 3:15PM by Professor John Collinge Professor John Collinge Professor of Neurology MRC Prion Unit Director UCL Institute of Neurology For more information visit: www.tiny.cc/jcollinge or scan the QR code j.collinge@prion.ucl.ac.uk Advances and challenges in stroke The outlook for treating stroke has changed dramatically in recent years. Major changes in routine care include intravenous thrombolysis for ischaemic stroke and reconfiguration of stroke services to provide high quality specialist hyperacute care. The range of patients who benefit from thrombolysis has extended with evidence from recent trials and pooled analyses. Although initial studies were neutral, evidence is now emerging to support endovascular therapy for selected patients with acute ischaemic stroke. In the field of intracerebral haemorrhage, hyperacute blood pressure reduction has recently been shown to be safe and to result in improved outcomes. In the field of secondary stroke prevention, notable recent advances include the widespread use of non-vitamin K anticoagulants to prevent ischaemic stroke in non-valvular atrial fibrillation. This lecture will briefly outline selected recent advances in stroke care, as well as some challenges for future research. David Werring is a Reader in Clinical Neurology and Honorary Consultant Neurologist at UCL Institute of Neurology, Queen Square, and the National Hospital for Neurology and Neurosurgery (NHNN), University College Hospitals (UCH) NHS Foundation Trust. At UCH he has been involved in developing a new hyperacute stroke service and outpatient services for patients with cerebral haemorrhage. Dr Werring is leading a research program in stroke, with a particular interest in neuroimaging and small vessel disease, especially intracerebral haemorrhage and cerebral amyloid angiopathy. He is Chief Investigator for the CROMIS-2 (Clinical Relevance of Microbleeds in Stroke) study (www.ucl.ac.uk/cromis-2), and for studies of new imaging biomarkers and treatments for cerebral amyloid angiopathy. He is Stroke specialty clinical lead for the NIHR North Thames Clinical Research Network, and member of the faculty of the European Stroke Organisation Conference. FRIDAY – 4:30PM by Dr David Werring Dr David Werring Consultant Neurologist Reader in Clinical Neurology UCL Institute of Neurology Selected Publications ‒ Charidimou A, Gang Q, Werring DJ. Sporadic cerebral amyloid angiopathy revisited: recent insights into pathophysiology and clinical spectrum. J Neurol Neurosurg Psychiatry. 2012 Feb;83(2):124-37. ‒ Greenberg SM, Al-Shahi Salman R, Biessels GJ, van Buchem M, Cordonnier C, Lee JM, Montaner J,Schneider JA, Smith EE, Vernooij M, Werring DJ. Outcome markers for clinical trials in cerebral amyloid angiopathy. Lancet Neurol. 2014 Apr;13(4):419-28. For more information visit: www.tiny.cc/dwerring or scan the QR code d.werring@ucl.ac.uk FRIDAY – 5:10PM Optimal management of TIA and stroke secondary to carotid atherosclerosis by Professor Martin Brown The randomised trials, ECST and NASCET, established the benefit of carotid endarterectomy (CEA) for symptomatic carotid stenosis many years ago. A risk prediction model based on ECST can be used to select patients likely to benefit from CEA. Carotid artery stenting (CAS) has been developed as alternative to CEA, but recent trials have shown higher procedural non-disabling stroke risk with CAS vs CEA. However, in patients younger than age of 70 and in patients with less than the average number of white matter lesions, the risks of stroke are similar. Long-term follow up has shown similar functional outcomes after CAS and CEA. Medical therapy has improved since these trials leading to a decline in the risks of recurrent stroke and the need to repeat old trials with modern technology. Future selection of patients for revascularisation will incorporate plaque imaging to identify high and low risk patients. Professor Martin Brown, MD, FRCP Consultant Neurologist Professor of Stroke Medicine UCL Institute of Neurology Martin M Brown qualified in Medicine from Cambridge University and the Middlesex Hospital Medical School. In 1999, he was appointed as the foundation Professor of Stroke Medicine at the UCL Institute of Neurology. He is also Consultant Neurologist at University College Hospital and the National Hospital for Neurology and Neurosurgery, Queen Square. His main research contribution has been the organization of large multicenter clinical trials aimed at improving the prevention of stroke, particularly from carotid artery narrowing caused by atherosclerosis. He is a past President of the British Association of Stroke Physicians and was the Clinical Director of the Thames Stroke Research Network from 2006 to 2014. Selected Publications - Bonati LH, Dobson J, Featherstone RL, et al. Long-term outcomes after stenting versus endarterectomy for treatment of symptomatic carotid stenosis: the International Carotid Stenting Study (ICSS) randomised trial. Lancet Published Online October 14, 2014. For more information visit: www.tiny.cc/mbrown or scan the QR code martin.brown@ucl.ac.uk NEUROLOGY 2015: Leading-edge Neurology for the Practising Clinician All articles printed with permission from the journals of Practical Neurology, Brain, Current opinion in Neurology, Neurology, Neurosurgery & Psychiatry, Cold Spring Harbor Perspectives in Medicine, Mayo Clinic Proceedings, The British Journal of Radiology, Neurosurgery, Neurological Sciences, Lancet Neurology, Lancet Infectious Diseases, Royal Society of Medicine, Neurobiology of Disease, Current Opinion in Genetics & Development. A very special thank you to all of our Sponsors: Sponsors Platinum • Allergan Ltd • Eisai Europe Ltd Gold • ElectroCore LLC • Genzyme Therapeutics Ltd • Novartis Pharmaceuticals UK Limited • Delta Surgical Limited • Lundbeck Ltd • Teva UK Ltd A very special thank you to all of our Sponsors: UCL INSTITUTE OF NEUROLOGY FACULTY OF BRAIN SCIENCES UCL Institute of Neurology MSc / MRes / Diploma Programmes The UCL Institute of Neurology offers a range of world-class taught and research 1-or 2-year MSc / MRes / Diploma programmes designed to deliver cutting edge knowledge and research skills to our students. Programmes include: ‒ Advanced Neuroimaging* ‒ Brain & Mind Sciences ‒ Brain Sciences ‒ Neuromuscular Disease ‒ Translational Neurology ‒ Stroke Medicine ‒ Neurology for Clinical Trainees ‒ Clinical Neuroscience & Clinical Neurology* * Distance learning available CT perfusion - acute stroke Courtesy Dr David Werring T2*-weighted MRI - cerebral haemorrhage Clinicians in training at the Leonard Wolfson Experimental Centre These full-time courses at the Institute of Neurology comprise: Courtesy Dr David Werring Apply today for SEPTEMBER 2015! ─ Increase your knowledge ─ Increase employability ─ Learn research skills ‒ Workshops, presentations, group-work ─ Start a research career ‒ A supervised research project providing the opportunity to work with international leaders and experts ─ Build networks for the future ─ PGCert & PGDip available for CPD for Allied Health Professionals ‒ Taught modules with between 60 to 100 lectures from clinical and research experts in clinical neurosciences For more information visit: www.ucl.ac.uk/ion/education/ or scan the barcode with your phone Contact us at: ion.educationunit@ucl.ac.uk Facebook.com/groups/UCLIoNEd & Twitter: @UCLIoNEd