Academic Program Review SUMMARY*
advertisement
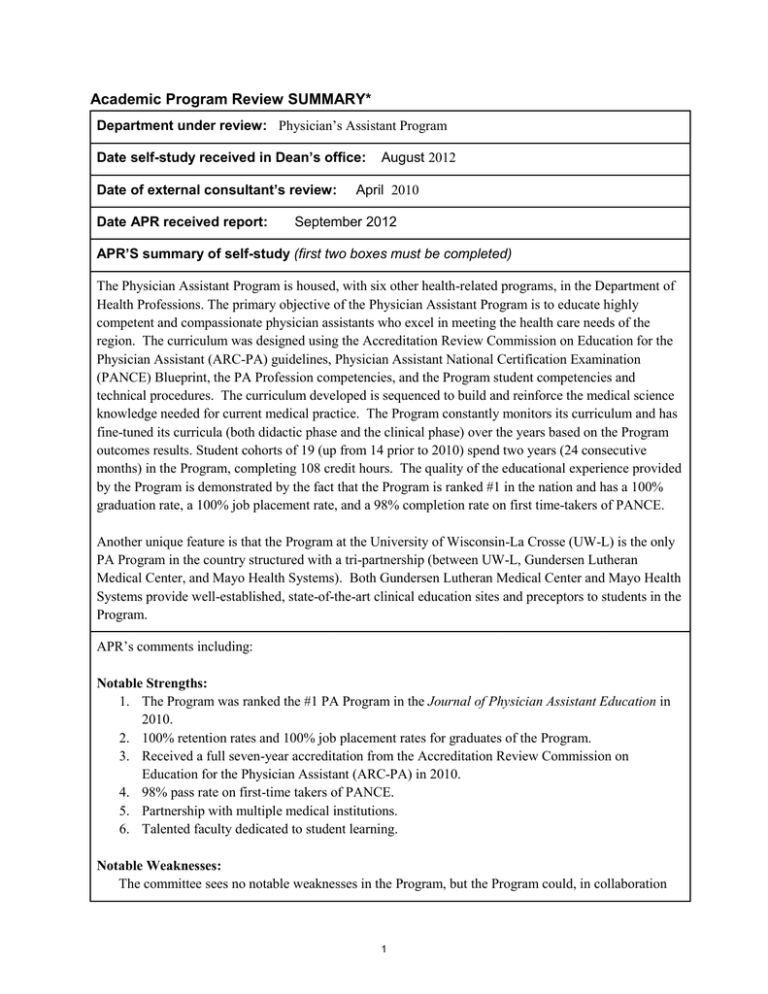
Academic Program Review SUMMARY* Department under review: Physician’s Assistant Program Date self-study received in Dean’s office: Date of external consultant’s review: Date APR received report: August 2012 April 2010 September 2012 APR’S summary of self-study (first two boxes must be completed) The Physician Assistant Program is housed, with six other health-related programs, in the Department of Health Professions. The primary objective of the Physician Assistant Program is to educate highly competent and compassionate physician assistants who excel in meeting the health care needs of the region. The curriculum was designed using the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA) guidelines, Physician Assistant National Certification Examination (PANCE) Blueprint, the PA Profession competencies, and the Program student competencies and technical procedures. The curriculum developed is sequenced to build and reinforce the medical science knowledge needed for current medical practice. The Program constantly monitors its curriculum and has fine-tuned its curricula (both didactic phase and the clinical phase) over the years based on the Program outcomes results. Student cohorts of 19 (up from 14 prior to 2010) spend two years (24 consecutive months) in the Program, completing 108 credit hours. The quality of the educational experience provided by the Program is demonstrated by the fact that the Program is ranked #1 in the nation and has a 100% graduation rate, a 100% job placement rate, and a 98% completion rate on first time-takers of PANCE. Another unique feature is that the Program at the University of Wisconsin-La Crosse (UW-L) is the only PA Program in the country structured with a tri-partnership (between UW-L, Gundersen Lutheran Medical Center, and Mayo Health Systems). Both Gundersen Lutheran Medical Center and Mayo Health Systems provide well-established, state-of-the-art clinical education sites and preceptors to students in the Program. APR’s comments including: Notable Strengths: 1. The Program was ranked the #1 PA Program in the Journal of Physician Assistant Education in 2010. 2. 100% retention rates and 100% job placement rates for graduates of the Program. 3. Received a full seven-year accreditation from the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA) in 2010. 4. 98% pass rate on first-time takers of PANCE. 5. Partnership with multiple medical institutions. 6. Talented faculty dedicated to student learning. Notable Weaknesses: The committee sees no notable weaknesses in the Program, but the Program could, in collaboration 1 with other health programs in the department, develop an interdisciplinary course for its students in the healthcare field which can strengthen its current curriculum. Self-Study: Purposes The primary objective of the faculty and academic staff of the Physician Assistant Program is to provide a high-quality education to students in the Program and to prepare excellent physician assistants who are grounded in professional ethics, cultural sensitivity, and the use of evidence-based medicine. Self-Study: Curriculum Like any other PA program in the nation, the UW-L Physician Assistant Program has to maintain national accreditation by the Accreditation Review Commission on Education for the Physician Assistant (ARCPA). In order to maintain the national accreditation, the Program must constantly monitor and fine-tune its curriculum to ensure that certain educational standards are met. The curriculum developed is rigorous, up-to-date, and is sequenced to build and reinforce the medical science knowledge needed for current evolving medical practice and to achieve the competencies needed for the physician assistant. A total of 108 credit hours are required to complete the 24-month curriculum, with 58 credit hours the first 12 months and 50 credit hours the second 12 months. The first 12 months of the curriculum (the didactic phase) is delivered primarily on the UW-L campus in La Crosse, Wisconsin. The second 12 months of the curriculum (the clinical phase) of the Program consists of clinical preceptorships primarily located at Gundersen Lutheran Medical Center in La Crosse, Mayo Clinic in Rochester, and their affiliated healthcare facilities. The clinical phase of the Program consists of eleven (11) 4-week rotations; each clinical rotation is 4 credit hours, for a total of 44 credit hours of clinical instruction. The students return to campus one day a month at the end of each clinical rotation and for a week-long summative evaluation at the end of the clinical year in order to earn an additional 6 credits in a Capstone course. Typical of other Physician Assistant programs in the country, the UWL program is accredited by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA). The Program was successfully reaccredited for a period of seven years in 2010. Self-Study: Assessment of Student Learning & Degree of Program Success The primary way in which the Program’s success is measured is by assessing “enabling competencies” in the following areas: Medical Knowledge, Interpersonal and Communication Skills, Patient Care, Professionalism, Evidence-Based Practice, and Understanding of Healthcare Systems. Direct measures include competency assessment, employment rates, performance on PANCE and Physician Assistant Clinical Knowledge Rating Assessment Test (PACKRAT) examinations, completion of Capstone project, clinical preceptor evaluations and summative examination. Indirect measures include formal interviews with student class cohorts, employer evaluations of graduates and retention of 2 students within the Program. Five outcome indicators were evaluated from 2006-2009. These included: graduation rate, PANCE results, employment location, graduate satisfaction, and supervising physician feedback. Since that time, the Program revamped its program evaluation plan to include more specific measurement criteria for each of the student learning outcomes adapted from the Competencies for the PA Profession, and these revised criteria are reflected in the 2010 and 2011 assessment (discussed below). 100% of the class of 2008 and 2009 graduated, took and passed the Physician Assistant National Certification Examination (PANCE) on the first or second attempt (only one student had to take the test a second time). On almost all national measures, students performed above the national average; the one subscore that was 1% below the national mean (hematology) in 2009 prompted the Program to revise that course. Since revision, this subscore has reached the national mean. 100% of the class of 2008 and all but one of the graduates of the Class of 2009 are employed: 100% of the Class of 2010 and Class of 2011 are employed (these combined figures lead the Program to report 100% employment rates in its self-study). All students admitted to classes graduating in 2008, 2009 and 2010 have been retained. Graduate surveys were distributed to members of the Classes of 2006 through 2009 (and their employing physicians) in 2010 (a total of 51 surveys were sent out). Response rate was 44% for alumni and 28% for employers. Of the 20 questions asked, the employers rated graduates favorably in all but one area, training regarding medical billing and coding. As a result of this feedback, specific education related to billing and coding has been added to the curriculum. As a result of focus group feedback and comments from students at the end of their education (gathered in 2010), the Program made changes to the curriculum in the following areas: 1. Radiologic diagnostic education 2. Increased attention to diagnostic testing for each clinical discipline 3. Revision of the behavioral medicine curriculum and integration throughout the didactic year 4. Wider scope of topics in medical ethics 5. Revision of the clinical epidemiology course with emphasis on interpretation of the medical literature and evidence-based practice. 6. Expanded focus of the healthcare systems course with study of multiple integrated delivery models of care. In 2010 and 2011, the Program assessed its success based on 20 specific goals for student performance within the areas of medical knowledge, interpersonal and communication skills, patient care, evidencebased practice, employment data, and knowledge of the healthcare industry. Evidence for success came from direct measures such as scores on national exams and grades in specific courses, and indirect measures such as surveys of students and employers. The Program met or exceeded its benchmark goals in 16 of the 20 measures and provided explanations and plans of action for the other four (because the Program is small, two of the four unmet goals related to the performance of only one or two students, and 3 the Program felt no need to make overall changes based on that data). One benchmark was unmet because survey data was still pending; the remaining unmet benchmark related to treatment planning has been addressed by the revision of a particular first-year course to offer students more clinical practice prior to their clinical year. Self-Study: Previous Academic Program Review and New Program Initiatives In 2004, the APR Committee expressed eight programmatic recommendations. Our current responses to each of these recommendations follow the respective entries below. Recommendation #1 - The PA Program should be provided a full time program assistant. Currently the Program does not have a dedicated full-time program assistant. The Health Professions Department with six programs share 3.92 FTE Academic Department Associates (Departmental decision); the PA Program is satisfied with the shared associate. Recommendation #2 – The PA faculty are encouraged to seek funding from various sources so that certifications and insurances may be maintained and research skills knowledge may be kept current. New student fees implemented in 2010 have been used to help faculty in professional development. However, these funds cannot be used to maintain certification or licensure of faculty members. Recommendation #3 – With regard to the preclinical year, the PA Program should reduce the length of the basic science curriculum, reducing redundancy while better building on students’ undergraduate prerequisite preparation. The current curriculum used is in compliance with ARC-PA standard, and the Program does not have the freedom to change the curriculum. Recommendation #4 – With regard to the preclinical year, the PA Program should work to integrate clinical preparatory sciences, building cohesive courses. This has been accomplished through course revisions. Recommendation #5 – With regard to the clinical year, the PA Program should work to enhance curricular flexibility to allow more experiences in tertiary care settings. This has been accomplished. Students may choose from selective and elective rotations (clinical) at tertiary care settings. Recommendation #6 – With regard to the clinical year, the PA Program should work to develop a schedule format that synchronizes students’ experiences with other learners on the clinical services. 4 This has been accomplished with help from the clinical partners. Recommendation #7 – With regard to the clinical year, the PA Program should work to strengthen preparation for inpatient practice and research skills. The curriculum during the didactic year has been modified to strengthen preparation of students for clinical experience by including more instruction and practice in clinical problem-solving and research. Recommendation #8 – Maintain a more regular alumni newsletter, as it may be a tool for recruitment and funding opportunities. The Program is planning to establish a biannual newsletter in near future. Self-Study: Personnel The Physician Assistant Program consists of 4.0 FTE core faculty members, including a full-time program director, a full-time clinical coordinator, and 2.0 FTE additional core faculty members. The PA Program is fully staffed in accordance with the ARC-PA standards. In addition to the core faculty, the PA Program is supported by 3.92 FTE administrative assistants who share responsibilities amongst the six programs housed in the Health Professions Department. The faculty and staff have ample funding and flexible schedules to take part in professional development activities. There is a budget line for professional development activities in the Program budget. Supported professional development activities include participation in national and state professional meetings, CME conferences, and seminars (in-person or on-line). Professional development activities are identified by each Core Faculty annually on their professional development plan. Self-Study: Support for Achieving Academic Program Goals (Resources) The PA Program is housed in the Health Sciences Center. Each year the Program admits 19 students and, currently, the facilities and equipment are adequate to its needs, with adequate office and classroom space, sufficient hardware, software, and instructional equipment. All of this is paid for by differential tuition and program fees paid by students in the Health Professions Department. External Reviewer Recommendations APR’s Comments on External Reviewer (if applicable). The ARC-PA Accreditation team visited the Program on April 29-30, 2010 and listed four citations (noncompliance) in its findings. The first two requirements have been successfully met by the Program. The third requirement (support for faculty to maintain their NCCPA certification status) cannot be satisfied 5 because of how university funding may and may not be used. The fourth requirement listed in the report is no longer required by ARC-PA. The APR committee suggests that if it is necessary for faculty members to maintain their NCCPA certification for accreditation purposes, then the university should consider finding a way to fund this since the PA Program is prohibited from implementing additional program fees to create a pool of money for this purpose. Department’s Response to the Reviewer Recommendations APR’s Comments on the Department’s Response (if applicable). The program has been able to rectify most of the concerns cited by the ARC-PA and the previous APR. Dean’s Letter APR’s Comments on Dean’s Letter (if applicable) The Dean agrees that the Program is excellent. APR’s Recommendations (must be completed) Recommendations: 1. 2. 3. 4. Maintain accreditation status and 100% graduation and placement rates. Develop an annual or biannual newsletter for alumni. Investigate funding mechanisms for supporting certification and licensure of faculty. Develop interdisciplinary course with other health-related programs. No serious areas to address – review in seven years. □ Some areas to address – review in seven years. □ Some areas to address – Department should submit short report on progress to Faculty Senate/ Provost’s Office in three years. * APR’s report to faculty senate will consist of this completed form in electronic form. 6