Getting Established on DMARD Therapy What are DMARDs?
advertisement
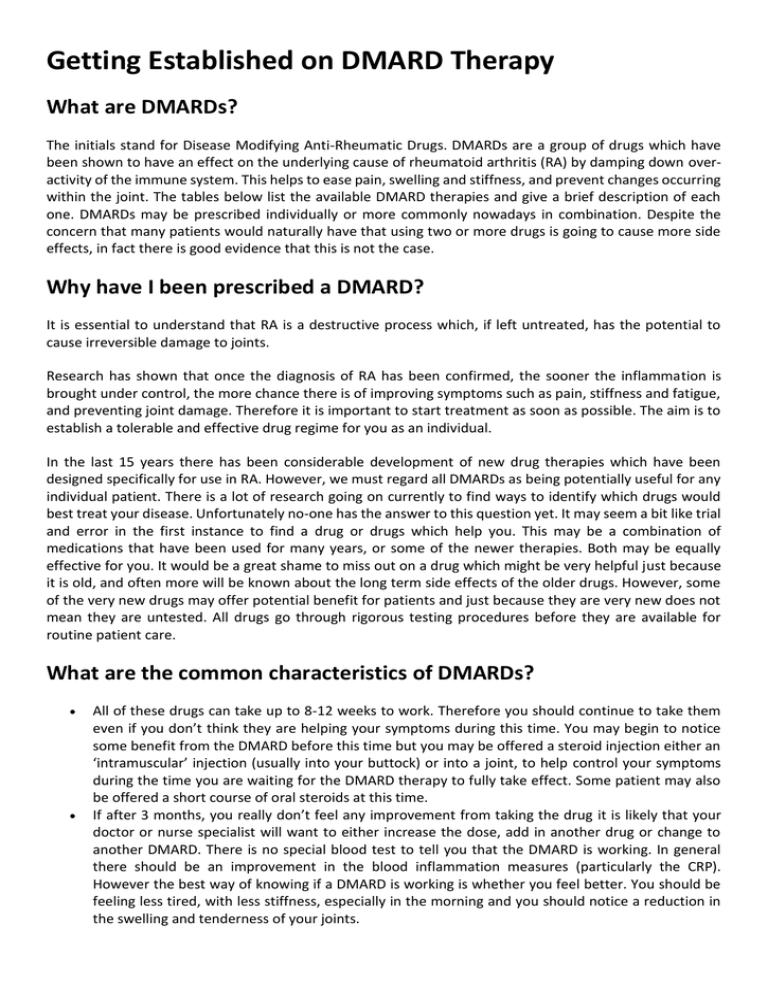
Getting Established on DMARD Therapy What are DMARDs? The initials stand for Disease Modifying Anti-Rheumatic Drugs. DMARDs are a group of drugs which have been shown to have an effect on the underlying cause of rheumatoid arthritis (RA) by damping down overactivity of the immune system. This helps to ease pain, swelling and stiffness, and prevent changes occurring within the joint. The tables below list the available DMARD therapies and give a brief description of each one. DMARDs may be prescribed individually or more commonly nowadays in combination. Despite the concern that many patients would naturally have that using two or more drugs is going to cause more side effects, in fact there is good evidence that this is not the case. Why have I been prescribed a DMARD? It is essential to understand that RA is a destructive process which, if left untreated, has the potential to cause irreversible damage to joints. Research has shown that once the diagnosis of RA has been confirmed, the sooner the inflammation is brought under control, the more chance there is of improving symptoms such as pain, stiffness and fatigue, and preventing joint damage. Therefore it is important to start treatment as soon as possible. The aim is to establish a tolerable and effective drug regime for you as an individual. In the last 15 years there has been considerable development of new drug therapies which have been designed specifically for use in RA. However, we must regard all DMARDs as being potentially useful for any individual patient. There is a lot of research going on currently to find ways to identify which drugs would best treat your disease. Unfortunately no-one has the answer to this question yet. It may seem a bit like trial and error in the first instance to find a drug or drugs which help you. This may be a combination of medications that have been used for many years, or some of the newer therapies. Both may be equally effective for you. It would be a great shame to miss out on a drug which might be very helpful just because it is old, and often more will be known about the long term side effects of the older drugs. However, some of the very new drugs may offer potential benefit for patients and just because they are very new does not mean they are untested. All drugs go through rigorous testing procedures before they are available for routine patient care. What are the common characteristics of DMARDs? All of these drugs can take up to 8-12 weeks to work. Therefore you should continue to take them even if you don’t think they are helping your symptoms during this time. You may begin to notice some benefit from the DMARD before this time but you may be offered a steroid injection either an ‘intramuscular’ injection (usually into your buttock) or into a joint, to help control your symptoms during the time you are waiting for the DMARD therapy to fully take effect. Some patient may also be offered a short course of oral steroids at this time. If after 3 months, you really don’t feel any improvement from taking the drug it is likely that your doctor or nurse specialist will want to either increase the dose, add in another drug or change to another DMARD. There is no special blood test to tell you that the DMARD is working. In general there should be an improvement in the blood inflammation measures (particularly the CRP). However the best way of knowing if a DMARD is working is whether you feel better. You should be feeling less tired, with less stiffness, especially in the morning and you should notice a reduction in the swelling and tenderness of your joints. Please bear in mind that if some of your joints have sustained damage as a result of having arthritis for some time, it may not be possible to improve them by using a DMARD. If many of your joints have improved, but one has not then that one joint may need to be treated in a different way from the other joints. Don’t feel that the DMARD is failing if it just fails to improve one joint whilst managing to improve other joints - that would be regarded as a success for the DMARD. With the exception of hydroxychloroquine, all of the standard DMARDs require you to have a blood test, usually at your GP surgery, on a regular basis (alternatively this may be done at the hospital depending on the local shared-care agreement). The reason for the blood test is firstly to help your GP and rheumatology team to assess that your disease is being well controlled, and secondly to make sure that the medication is not affecting your ability to fight infection, or having an adverse effect on your blood cells, liver or kidneys. Can I take any other medications with DMARDs? You can continue to take your usual medications for pain relief particularly in the first 8-12 weeks of treatment, unless your doctor advises against this. It is always a good idea to check that the prescriber is aware of your current medications whenever a new drug is prescribed or suggested (even if these are complementary or herbal remedies) to ensure that there are no potential adverse interactions. It is recommended that you have a vaccination against pneumonia (pneumovax) and an annual flu vaccination if possible when taking these medications. What happens if I can’t tolerate DMARD therapies or they do not control my RA? Your rheumatology team will assess your response to treatment on a regular basis, often monthly at first, with the frequency of appointment getting more spaced out as your disease is controlled. For some people, traditional DMARD therapies are not effective on their own in helping to control the inflammation. If you cannot tolerate DMARDs or despite being on a combination of treatment your disease remains active, you may be eligible to receive biologic therapy. Biologic therapies are often given in combination with DMARDs. Where can I get additional information about individual medications? It is important that you seek information from reputable sources. The information should be related to the condition you have, and relevant to the dose of medication you have been prescribed. Remember that many of these drugs are used to treat different conditions and, as such, may be used in larger doses which have the potential to alter the chance of you getting a side effect. Useful sources of information: Your rheumatology department / clinical nurse specialist ARUK website (www.arthritisresearchuk.org) Standard DMARD Methotrexate Comments This drug has been used in RA since the 1980s. It was originally established (Maxtrex) for use in cancer treatment (as early as the 1940s) and is still used for that purpose. However, in very small doses it can be very effective for the treatment of RA and childhood forms of arthritis. It is probably the most Standard DMARD Comments Typical dose: 7.5 - 25 mg once effective drug for RA we currently have and is typically the first or second a week (average dose 15- 20 choice DMARD treatment. It acts by suppressing the immune system and mg weekly). can slow down the progress of RA as well as making significant improvements in general well being by reducing the inflammation. Sulfasalazine has been available since the 1940s and is a combination drug Sulfasalazine (Salazopyrine) containing an anti-inflammatory compound and an antibiotic. It is unclear how it works but clearly it does work for a large number of patients with RA. It is also used for the treatment of inflammation of the bowel. Like Typical dose: 1.5 - 3 g/ day. methotrexate, it acts by suppressing the immune system. Hydroxychloroquine is a treatment for malaria but has been shown to damp down the immune system in a non-specific way. It has been available since the 70s and is used widely for the treatment of lupus (SLE) but is also an Hydroxychloroquine established drug for the treatment of mild RA. It is commonly used in (Plaquenil/ Quinoric) combination with other DMARDs. A rare, but serious side effect of hydroxychloroquine is an accumulation of the drug in the back of the eye, if Typical dose: 200-400 mg/ too much is given over too long a period of time. This can cause an day. interference with night-time vision and should be discussed carefully with your doctor before starting the treatment. It is recommended to have your eyes tested by an optician before starting treatment and then once a year. Leflunomide was introduced in 1999 specifically for treating RA. It has a particular effect on the lymphocytes which are an important set of cells Leflunomide (Arava) responsible for regulating parts of the immune system. It is likely to regulate the immune system by damping down the overactive lymphocytes. Typical dose: 10-20 mg/ day. Leflunomide may occasionally cause diarrhoea and can cause high blood pressure; therefore it is important to have your blood pressure checked when you attend your routine blood tests. Azathioprine is used to damp down the immune system by slowing down the rate of cell division amongst the inflammatory cells. Therefore it is known as a cytostatic drug. It has been widely prescribed since the 60s. Typical dose: calculated using Typical side effects can include sickness and diarrhoea. It can lower the white your weight (2cell count and platelet count, sometimes making you more prone to 2.5mg/kg/day). bruising, bleeding and infection. Azathioprine (Imuran) Penicillamine Typical dose: 1000mg/day. 500 Penicillamine was introduced in the 1970s and is not often used nowadays to treat patients with RA. Its mechanism of action is uncertain, it seems to damp down the immune system in a non-specific way. It must be taken as a single dose, not with food; otherwise it binds to the food, does not get – absorbed into your body, and therefore becomes ineffective. It can have a number of potential side effects including sickness and diarrhoea, and can also cause skin rashes. Routine blood and urine tests are important as it can cause a leak of protein through the kidney. Gold given by injection was originally introduced in the 1920s as a way of treating what was thought to be an infectious cause of arthritis. Since then it has been shown that gold is not a good anti-infection drug but Typical dose : 50mg/week – nevertheless, the drug does seem to have some value in treating RA when 50mg/month. given over a long period of time by repeated injection. Like other nonGold Injections (Myocrisin) Standard DMARD Comments specific DMARDs it damps down the immune system and seems to calm down RA. It has a number of side effects similar to penicillamine. It can cause skin rashes, nausea and diarrhoea. Routine blood testing is necessary to look for any reduction in the cell count and a urine check is required as it can cause a leak of protein through the kidney. Ciclosporin is an established treatment to suppress the immune system in patients who are about to undergo kidney or heart transplant. It was developed back in the 1970s and since then its effects on damping down the Ciclosporin immune system have also been used for the treatment of patients with RA. Common side effects include a rise in blood pressure, increased hair growth, Typical dose: 2.5–4 increased swelling of the gums and an increased risk of developing an mg/kg/day in two divided infection. There is also a risk of developing kidney disease while taking the doses. drug, including high blood pressure and interference with kidney function. The drug has to be monitored carefully, checking routine blood tests and blood pressure regularly. Biologic DMARDs Biological therapies are much more expensive than conventional treatments because they have to be manufactured in a special way. As a result there are certain criteria, determined by NICE (the National Institute for Health and Clinical Excellence,) that need to be met before a patient will be considered for biologic drugs. The NICE Guidelines state that to be eligible for biologic drugs patients must have previously failed on two conventional DMARDs, one of which must be methotrexate (unless there is a medical reason for not having it), and have high levels of persistent disease activity. The levels of disease activity are measured using a scale known as DAS (Disease Activity Score) which is calculated by combining a number of factors including the number of joints (out of 28) which are tender and/or swollen, and blood test results for inflammation levels. What are the common characteristics of biological therapies? In rheumatoid arthritis, biological therapies are designed to specifically attack cells or processes involved in causing the inflammation. Biological therapies are much more expensive than conventional treatments because they have to be manufactured in a special way. All biological therapies currently have to be given by injection, because they do not work if they are taken by mouth. Biological therapies have the potential to increase your risk of getting an infection (but probably no more so than conventional DMARDs). No routine blood monitoring is required whilst on biological therapies; however most patient have biological therapy in combination with other standard DMARDs which do require monitoring. In most cases, it is better for you to continue taking your conventional DMARD or DMARDs together with the new biologic therapy, even if the conventional DMARD or DMARD combination is not working. This is because the conventional DMARD can work together with the biologic therapy to give you even more help. For some biologic therapies, if you do not take a conventional DMARD or DMARD combination, your body’s immune system can develop antibodies to prevent the biologic therapy from working. All patients on biological therapies should be attending regular review with a member of the rheumatology team. Some patients receiving biologic therapies may be asked to consent to their details being recorded on the Biological register for the British Society for Rheumatology. This register helps to inform doctors across the country regarding the safety and efficacy of this group of drugs. The anti-TNFα treatments Inflammation is the body’s reaction to injury and is a necessary process for the repair of injury. A protein called tumour necrosis factor alpha (TNFα) promotes inflammation. In people with RA and some other inflammatory conditions, TNFα is overproduced in the body causing excess inflammation which has the potential to cause pain, tenderness and swelling of joints; and, if left unchecked, can damage bones, cartilage and tissue. The anti-TNF biologic treatments are man-made proteins that bind to TNFα and block the effects of excess TNFα, helping to reduce the inflammation that is caused by RA and subsequently slow or prevent destruction of joints. TNFα is important for normal health and it is not a good idea to block all TNFα in the body, otherwise patients are at risk of infection, particularly tuberculosis (TB). The other biologic drugs all target slightly different cells in the immune system. Biosimilars Several different biological drugs are currently being developed which have similar properties to existing biological agents. These are called biosimilars. Examples include Inflectra and remsima (similar to infliximab), benepali (similar to etanercept) or maball (similar to rituximab). Biosimilars are not exactly identical in structure to the original biological agent on which they are based. Before they can be used in clinical practice, they will already have been tested in clinical trials to show that they have a similar likelihood of helping and/or causing problems compared to the original treatment from which they were based. We expect that the biosimilar drugs will be cheaper. The first of these, inflectra, was approved for use in the UK in 2015. Anti-TNF DMARD Comments Infliximab (Remicade) Infliximab was the first anti-TNFα treatment to be established in RA, in (biosimilar names Inflectra and 2000. It has to be given by an intravenous infusion (a drip), so is usually given in hospital as a day patient. Initial doses of infliximab are given Remsima) more frequently to establish good control of the disease. The first 3 Typical dose: 3 mg/kg by doses are all given within an 8 week period, then every 8 weeks after intravenous infusion (drip) every that. 8 weeks. Etanercept (licensed in 2000) is given as an injection just under the skin, Etanercept (Enbrel) once or twice a week. Patients are usually taught how to inject themselves, using a syringe or an easy to use one-click pen. Sometimes (biosimilar name Benepali) patients can experience redness and soreness of the skin at the site of the injection. Typical dose: 50mg/week, either This can be avoided in most instances by varying the site of the injection as a single subcutaneous injection on each occasion over a cycle of 4-5 weeks (e.g. inject the outer side of (or as 2 injections on separate the left thigh on the first week, the inner side of the left thigh on the days of 25mg each.) second week then the stomach etc). Adalimumab (Humira) Adalimumab (licensed in 2003) is also given by injection under the skin every 2 weeks. Patients are usually taught how to inject themselves, Anti-TNF DMARD Comments Typical dose: 40 mg every 2 weeks using a syringe or an easy to use one-click pen. Sometimes patients can given by subcutaneous injection. experience redness and soreness of the skin at the site of the injection. This can be avoided in most instances by varying the site of the injection on each occasion over a cycle of 4-5 weeks (e.g. inject the outer side of the left thigh on the first week, the inner side of the left thigh on the second week then the stomach etc). Certolizumab-pegol was approved as a treatment for RA in 2009 and is given by injection every 2 weeks. It is currently only available in syringe Certolizumab-pegol (Cimzia) form and patients are usually taught how to inject themselves. Sometimes patients can experience redness and soreness of the skin at Typical dose: 2 x 200mg the site of the injection. This can be avoided in most instances by varying subcutaneous injection at weeks the site of the injection on each occasion over a cycle of 4-5 weeks (e.g. 0, 2 & 4 thereafter 200mg every 2 inject the outer side of the left thigh on the first week, the inner side of weeks. the left thigh on the second week then the stomach etc). It is a monoclonal antibody again binding to TNFα, but has a slightly different structure known as PEGylation. Golilmumab is the first monthly injectable anti-TNFα available to patients with RA, and has been available since 2009. Patients are usually taught how to inject themselves, using a syringe or an easy to use oneGolimumab (Simponi) click pen. Sometimes patients can experience redness and soreness of Typical dose: 50mg subcutaneous the skin at the site of the injection. This can be avoided in most instances by varying the site of the injection on each occasion over a cycle of 4-5 injection monthly. weeks (e.g. inject the outer side of the left thigh on the first week, the inner side of the left thigh on the second week then the stomach etc). Other biologic DMARDs Biologic DMARD Comments Rituximab is a treatment, given by infusion, designed to attack B-cells, which are an important part of the immune system involved in RA. Rituximab is (biosimilar name Maball) currently offered to patients who fail to improve with anti-TNFα therapy. It has a 50% chance of being Typical dose: Intravenous infusions of 1g on 2 effective, and appears to be relatively safe. It has occasions 14 days apart, then repeat no sooner been used in RA since 1998. than every 6 months if effective. Rituximab (Mabthera) This is a once-monthly intravenous infusion treatment, licensed for use in RA since 2009. As of Tocilizumab (RoActemra) 2014 it is also available as a subcutaneous injection Typical dose: 8mg/kg intravenous infusion monthly or (an injection under the skin). Tocilizumab can be 162mg subcutaneously every week (for all patients given when there has been an inadequate response regardless of weight). to one or more anti-TNFα treatments, or as a first biologic. It is a humanized monoclonal antibody against the interleukin-6 receptor (IL-6R). Interleukin 6 (IL-6) is a cytokine (protein that serves as a Biologic DMARD Comments messenger between cells) that plays an important role in immune response. Abatacept (Orencia) Typical dose: 500-1000mg (dependent on weight) at 0, 2 & 4 weeks then monthly intravenous infusions thereafter or 125mg subcutaneous injection every week (either alone or following an optional intravenous loading dose of 500-1000mg, calculated to be around 10mg per kg body weight). Abatacept (licensed in 2007) is an infusion that is given intravenously and followed with more doses 2 and 4 weeks later. Thereafter, infusions are given every 4 weeks. The dosage is adjusted according to the patient's weight. As of 2014 it is also available as a subcutaneous injection (an injection under the skin). Unlike other biologic drugs, abatacept does not block inflammatory proteins. Abatacept attaches to the surface of inflammatory cells (T cells) and blocks communication between these cells. By blocking this communication, abatacept lessens inflammation. Further Reading: NRAS 'Combination Therapy' NRAS 'What is RA?' NRAS 'Managing the pain of RA' References available on request Professor Raashid Luqmani DM FRCP FRCP(E), Professor of Rheumatology/Consultant Rheumatologist and Maureen Cox, Rheumatology Nurse Specialist. Rheumatology Department, Nuffield Orthopaedic Centre, Oxford Original article: 02/06/2006 Reviewed: 15/01/2016 Next review due: 15/01/2019