Disclosures
advertisement

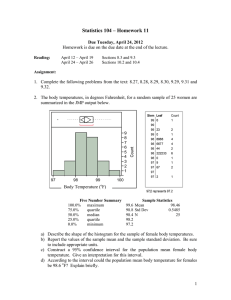
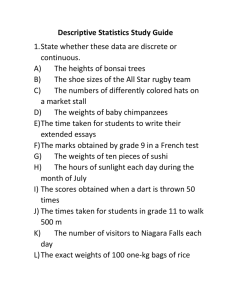
Disclosures • Dr Dr. Joynt has nothing to disclose disclose. • Dr. Orav has nothing to disclose. • Dr. Jha has provided consulting for UpToDate. UpToDate HARVARD SCHOOL OF PUBLIC HEALTH Does Volume Matter for Heart Failure? Evaluating quality, outcomes, and costs of care Karen E. Joynt, MD E. John Orav, PhD Ashish K. Jha, MD, MPH Background • Heart failure is common and costly: – Most frequent cause of hospitalizations – 1.4 million hospitalizations in 2007 – $17 billion in spending in 2007 • Heart failure outcomes remain poor: – At A 30 d days: 10% mortality, li 25% readmission d i i • Improving p g HF outcomes is a national priority Rosamond 2008, Hospital Compare 2009 National readmission rates 800 Numb ber of Hos spitals 700 600 500 400 600 h hospitals it l 1000 h hospitals it l 300 200 100 0 ≤5 7.5 10 12.5 15 17.5 20 22.5 25 27.5 30 32.5 35 37.5 40 42.5 45 47.5 ≥50 30-day readmission rate (%) Volume matters • For surgery and cardiac procedures procedures, higher volume leads to: • Better outcomes • Shorter length of stay • Lower costs • For medical illness,, the storyy is unclear: • Slight improvement? (HF, MI, PNA) • Worse care and outcomes? (PNA (PNA, COPD) Birkmeyer 2001, Birkmeyer 2002, Hannan 2003, Wu 2004, Jollis 1997, McGrath 2000, Hannan 2005, Thiemann 1999, Tu 2001, Lindenauer 2006, Ho 2008, Swisher 2000, Kuo 2001, Ross 2010 Specific Aims • To determine ifif, for heart failure failure, high volume hospitals: – Provide higher quality care – Have better outcomes – Have lower costs Methods • National Medicare data from 2006 and 2007 • Primary discharge diagnosis of HF • Exclusions: – Federal hospitals – Hospitals outside 50 states and Washington DC – Fewer than 25 discharges • Sample: – 4,009 hospitals – 699,109 patients Methods • Hospital characteristics: • American Hospital Association survey • Quality of care: • Hospital p Quality y Alliance HF score • Outcomes of care: • 30 30-day day risk risk-adjusted adjusted all all-cause cause mortality • 30-day risk-adjusted all-cause readmission • Costs C t off care: • Observed to predicted cost ratio Elixhauser 1998, Southern 2004, Jha 2009 Methods • Divided hospitals into quartiles by volume • Even number of hospitals in each quartile • Regression models for each outcome • Volume as the sole predictor p • Multivariate linear regression models for each outcome • Accounting for key hospital characteristics such as size teaching status size, status, and cardiac capability Results: hospitals by quartile Quartile 1 Quartile 4 Lowestt L volume Q til 2 Quartile Q til 3 Quartile Highest Hi h t volume Small (6-99) 82% 65% 20% 2% Med (100-399) 17% 33% 72% 65% Large (400+) 1% 2% 7% 33% P<0.001 for trend for each Results: hospitals by quartile Quartile 1 Quartile 4 Lowestt L volume Q til 2 Quartile Q til 3 Quartile Highest Hi h t volume For-profit 10% 19% 21% 12% Non-profit 52% 56% 64% 80% Public 38% 25% 15% 9% P<0.001 for trend for each Results: hospitals by quartile Quartile 1 Quartile 4 Lowestt L volume Q til 2 Quartile Q til 3 Quartile Highest Hi h t volume Urban 49% 71% 92% 100% Major teaching 1% 3% 6% 17% Cardiac intensive care 11% 22% 38% 67% P<0.001 for trend for each Results: patients by quartile Quartile 1 Quartile 4 Lowestt L volume Q til 2 Quartile Q til 3 Quartile Highest Hi h t volume 81 81 80 80 Male sex 40% 41% 43% 45% Minority 12% 12% 15% 15% Age P<0.001 for trend for each Results: patients by quartile Quartile 1 Quartile 4 Lowestt L volume Q til 2 Quartile Q til 3 Quartile Highest Hi h t volume Diabetes w/ comp 5% 5% 6% 6% Hypertension 52% 56% 58% 60% Renal failure 6% 8% 11% 13% P<0.001 for trend for each Volume and quality 100 87.1 HQ QA HF score, % complia ant 90 80 88 9 88.9 81.5 75.8 70 60 Quartile 1 Quartile 2 Quartile Qua t e3 Quartile 4 50 40 30 20 10 P<0.001 for trend 0 Hospital volume for HF Volume and mortality Risk-ad djusted 3 30-day m mortality rate, % 13 12 3 12.3 12 11 11.6 10.4 10 9.5 9 Quartile 1 Quartile 2 Quartile Qua t e3 Quartile 4 8 7 P<0.001 for trend 6 Hospital volume for HF Volume and readmission Risk-ad djusted 3 30-day re eadmission rate,, % 30 26.9 25 24.9 23.4 22.2 20 Quartile Q il 1 Quartile 2 Quartile 3 Quartile 4 P<0.001 for trend 15 Hospital volume for HF Volume and cost ratio Observed to o expecte ed cost rratio 1.1 1.05 1 0.97 0.94 0.94 0.9 Quartile 1 Quartile 2 Quartile Qua t e3 Quartile 4 P<0.001 for trend 0.8 Hospital volume for HF Multivariate analysis HQA HF score 30-day 30-day Cost ratio mortalityy readmission Q artile 1 (lowest Quartile (lo est volume) ol me) 78 3 78.3 11 9% 11.9% 25 5% 25.5% 0 96 0.96 Quartile 2 82.9 11.3% 24.4% 0.96 Quartile 3 86.4 10.4% 24.2% 0.98 Quartile 4 (highest volume) 86.4 9.8% 23.7% 1.01 Adjusted for patient characteristics, hospital beds, the presence of a CCU, ownership, teaching status, system membership, proportion Medicare, proportion Medicaid, urban location, and region. P<0.001 for trend for each. Summary • Hospitals with greater experience caring for HF patients – Provided higher quality care – Had better clinical outcomes • Do so at somewhat higher costs • These Th results l persisted i d even after f accounting g for hospital size, teaching g status, and the presence of a CCU Limitations • Administrative data for risk adjustment • Medicare patients only • We don’t know why volume is associated with better outcomes Implications • The volume volume-outcome outcome relationship appears to extend beyond surgical procedures • There is no free lunch • At least in the short run • This opens up two potential avenues for improving care for HF patients: • Regionalization of care • Partnerships between low and high volume institutions to share best practices Acknowledgements • Mentorship and collaboration: Ashish Jha • Statistical guidance: John Orav Quartiles by n of patients HQA HF 30-day 30-day score mortality readmission Cost ratio Quartile 1, n=2442 (low vol) 81.5 11.7% 25.6% 0.95 Quartile 2, n=804 88.0 10.2% 22.8% 1.0 Quartile 3 3, n=495 88 9 88.9 9 5% 9.5% 22 1% 22.1% 1 04 1.04 Quartile 4, 4 n n=268 268 (high vol) 89 2 89.2 9 1% 9.1% 22 1% 22.1% 1 09 1.09 P<0.001 for trend for each Volume and HQA score Volume and mortality Volume and readmission Volume and cost ratio Results: patients by quartile Quartile 1 Quartile 2 Quartile 3 Quartile 4 (25-78 (79-174 (175-361 (362-2839 discharges) discharges) discharges) discharges) Age 81 81 80 80 Female sex 60% 59% 57% 55% Non-white race 12% 12% 15% 15% Diabetes w/ comp 5% 5% 6% 6% Hypertension 52% 56% 58% 60% Renal failure 6% 8% 11% 13% Valvular disease 1% 2% 2% 3% P<0.001 for trend for each References • • • • • • • • • • • • Auerbach AD, Hilton JF, Maselli J, Pekow PS, Rothberg MB, Lindenauer PK. Shop for quality or volume? Volume, quality, and outcomes off coronary artery bypass surgery. Ann Intern Med. May 19 2009;150(10):696-704. ( ) Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. Sep 2001;130(3):415-422. Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. Med Apr 11 2002;346(15):1128 2002;346(15):1128-1137. 1137 Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. Jan 1998;36(1):8-27. Hannan EL, Wu C, Ryan TJ, et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted risk adjusted mortality rates? Circulation. Aug 19 2003;108(7):795-801. 2003;108(7):795 801. Hannan EL, Wu C, Walford G, et al. Volume-outcome relationships for percutaneous coronary interventions in the stent era. Circulation. Aug 23 2005;112(8):1171-1179. Ho V, Aloia T. Hospital volume, surgeon volume, and patient costs for cancer surgery. Med Care. Jul 2008;46(7):718-725. Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring efficiency: the association of hospital costs and quality of care. Health Aff (Millwood). May-Jun 2009;28(3):897-906. Jollis JG, Peterson ED, Nelson CL, et al. Relationship between physician and hospital coronary angioplasty volume and outcome in elderly patients. Circulation. Jun 3 1997;95(11):2485-2491. Kuo EY, Chang Y, Wright CD. Impact of hospital volume on clinical and economic outcomes for esophagectomy. Ann Thorac Surg. Oct 2001;72(4):1118-1124. Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD-9 and ICD-10 administrative databases. BMC Health Serv Res. 2008;8:12. Lindenauer PK, PK Behal R, R Murray CK CK, Nsa W, W Houck PM PM, Bratzler DW. DW Volume Volume, quality of care care, and outcome in pneumonia. Ann Intern Med. Feb 21 2006;144(4):262-269. References • • • • • • • • • • Lindenauer PK, Pekow P, Gao S, Crawford AS, Gutierrez B, Benjamin EM. Quality of care for patients hospitalized for f acute exacerbations off chronic obstructive pulmonary disease. Annals off internal medicine. 2006;144(12):894-903. McGrath PD, Wennberg DE, Dickens JD, Jr., et al. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA. Dec 27 2000;284(24):31393144. 3144 Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. Jan 29 2008;117(4):e25-146. g Y, Ko DT, Chen J, Drye y EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC, Ross JS, Normand SL, Wang Krumholz HM. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362(12):1110-1118. Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. Apr 2004;42(4):355-360. S i h SG Swisher SG, Deford D f d L, L M Merriman i KW KW, ett al. l Eff Effectt off operative ti volume l on morbidity, bidit mortality, t lit and d hospital h it l use after esophagectomy for cancer. J Thorac Cardiovasc Surg. Jun 2000;119(6):1126-1132. Thiemann DR, Coresh J, Oetgen WJ, Powe NR. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. May 27 1999;340(21):1640-1648. Tu JV, JV Austin PC PC, Chan BT BT. Relationship between annual volume of patients treated by admitting physician and mortality after acute myocardial infarction. Jama. Jun 27 2001;285(24):3116-3122. Ward MM. Hospital experience and mortality in patients with systemic lupus erythematosus: which patients benefit most from treatment at highly experienced hospitals? J Rheumatol. Jun 2002;29(6):1198-1206. Wu C,, Hannan EL,, Ryan y TJ,, et al. Is the impact p of hospital p and surgeon g volumes on the in-hospital p mortality y rate for coronary artery bypass graft surgery limited to patients at high risk? Circulation. Aug 17 2004;110(7):784-789.