Prospective association of Intimate Partner Violence (IPV) with receipt of
advertisement

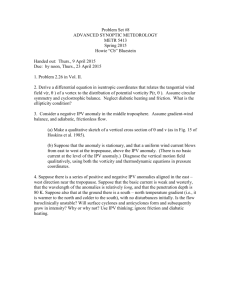
Prospective association of Intimate Partner Violence (IPV) with receipt of clinical li i l preventive i services i iin women off reproductive p age g Jennifer McCall-Hosenfeld, MD, MSc Pennsylvania State University College of Medicine Departments of Medicine and Public Health Sciences AcademyHealth A d H lh Annual Research Meeting 2010 Boston, MA 06.27.2010 Acknowledgements g Cynthia H. Chuang, MD, MSc NIH NICHD K23 HD051634 Carol S S. Weisman Weisman, PhD NIH ORWH BIRCWH 5 K12 HD05582-03 CePAWHS: PA Dept. of Health 4100020719 IPV survivors mayy need increased attention to preventive services. National consensus guidelines recommend safety planning. IPV is associated with increased risk for sexually transmitted infections (STIs) (STIs), unintended pregnancy, and substance abuse. Primar care pro Primary providers iders sho should ld approach counseling and screening for these issues among IPV survivors i with ith heightened h i ht d attention. Unclear if IPV survivors gget recommended preventive services in primary care. IPV often undetected in primary care settings. Gi Given llack k off d detection, t ti d do IPV survivors i receive appropriate services? Objective: to determine whether exposure to IPV predicts receipt of clinical preventive services. services Demographic factors. Population p under studyy The Central Pennsylvania Women´s Women s Health Study a longitudinal survey off a population-based sample of women of reproductive age. women ages 18-45 residing in a 28-county region of Central Pennsylvania. interviews conducted in 2004-2005. follow-up interviews were conducted two years later (n=1,420). Independent p variable - IPV Affirmative response to anyy of eight g items assessing physical and sexual partner violence exposure p in the p past 12 months. Threats of hitting, throwing Throwing objects Pushing, grabbing, shoving, slapping Kicking biting, Kicking, biting hitting Beaten up Choked Forced sex Threats with weapon Dependent p variables – clinical preventive services counseling for safety and violence concerns tests for STIs including g HIV counseling for STIs pap testing t ti blood p pressure testing g counseling for smoking or tobacco use counseling for alcohol or drug use birth control counseling Statistical methods Bivariate a ate a analysis. a ys s Multivariable models investigated the independent contribution of IPV to receipt of each of the services. Logistic regression. Controlled for age, g , educational status,, poverty, and continuous health insurance coverage in the past 12 months months. Results IPV=5% N=1420 Results – demographics g p IPV No IPV 70% 60% 50% 40% 30% 20% 10% 0% p=0.26 p<0 001 p<0.001 p<0.001 p=0 p 0.04 04 Results – p preventive services 100% 90% 80% 70% p<0.001 60% p=0.02 50% 40% 30% 20% 10% 0% p=0.01 p=0.05 IPV No IPV Results – p preventive services IPV No IPV NS 100% NS 90% 80% 70% p<0.001 60% p=0.02 50% NS 40% 30% 20% 10% 0% p=0.01 p=0.05 NS Multivariable results - IPV Odds of receipt of preventive services for women with IPV compared to women without IPV Controlling for age, education, poverty, and insurance gaps Counseling safety/violence counseling STI/HIV tests STI counseling STI counseling pap testing blood pressure test smoking/tobacco counseling* alcohol/drug counseling** birth control counselingg aOR 2.4 2.4 15 1.5 1.5 2.6 1.6 1.4 1.0 95% confidence 95% confidence intervals 1.3 4.7 1.4 4.2 07 0.7 30 3.0 0.7 3.3 0.6 11.1 1.0 2.6 0.7 2.7 0.6 1.7 *results similar when controlling for smoking **results results similar when controlling for binge drinking and drug use similar when controlling for binge drinking and drug use Multivariable results – insurance gaps g p Odds of receipt of preventive services for women with insurance gaps compared to women without insurance gaps Controlling for age, education, poverty, and IPV Counseling safety/violence counseling STI/HIV tests STI STI counseling li pap testing blood pressure test smoking/tobacco counseling* alcohol/drug counseling** birth control counseling birth control counseling aOR 0.6 1.3 10 1.0 0.4 0.4 1.0 0.8 0.9 *results similar when controlling for smoking **results similar when controlling for binge drinking **results similar when controlling for binge drinking 95% confidence 95% confidence intervals 0.3 1.0 0.9 1.8 06 0.6 16 1.6 0.3 0.5 0.2 0.7 0.8 1.4 0.5 1.3 0.6 1.3 Conclusions Increased odds of reporting safety and violence counseling among women with IPV. Overall rate of safety counseling among women g y low. with IPV ((20%)) is alarmingly Other key services for such as substance abuse or contraceptive counseling may be overlooked. Lack of continuous health insurance reduced odds of several services including safety counseling. Limitations Self-reported recollection of preventive counseling. Unclear how often services should be offered. offered Discussing a factor with a doctor does not mean that appropriate co counseling nseling occ occurred rred No data on IPV detection. Implications p Healthcare providers should improve rates of providing safety counseling to IPV survivors. Better evidence and improved guidelines for identification of and response to IPV needed. I Importance t off continuous ti health h lth insurance i coverage for the provision of appropriate primary healthcare. Thank you y Questions? Email: jsm31@psu.edu j @p