Accountable Care Organizations: Lessons from current practice Julie Bynum, MD MPH Assistant Professor
advertisement

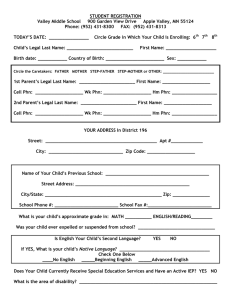
Accountable Care Organizations: Lessons from current practice Julie Bynum, MD MPH Assistant Professor Dartmouth Medical School Goals • Describe brief history & current concept • Describe development of our “experimental model” of an ACO • Discuss potential uses through evaluation of current data Vol 13, Issue 4, 43-57 Vol 13, Issue 5, 46-64 Variations in quality and spending The Dartmouth Atlas What is organizational accountability? Levels of decision-making and potential strategic levers Research priorities (biology vs. clinical practice) Coverage policy Performance measurement / Public reporting Payment system reform Recruitment / practice location decisions Capital investment (hospital, outpatient) Organizational structure (hospital, MD group) Process management (QI, IT adoption) Specialty certification Graduate Medical Education Continuing medical education HIT for care and decision-support Policy Environment (e.g. payment system) Local Organizational Context (e.g. capacity - culture) Physician - Patient Encounter What can be done? Levels of decision-making -- and potential strategic levers Where do these levers exist? • In Washington, DC • In State capitols Policy Environment (e.g. payment system) Where do these levers exist? • integrated health systems or managed care • FFS more challenging Local Organizational Context (e.g. capacity - culture) Where do these levers exist? • In hospitals • In clinics • In nursing homes • In home health agencies Physician - Patient Encounter Accountable Care Organizations Current measures Future measures should Focus largely on individual accountability (setting or clinician) for technical quality Focus on shared accountability for quality (broadly defined) and costs. Will do little to address: • Prevention / population health • Care fragmentation, silos • Provider-dominated decisions • Capacity and costs Including measures of: • Disease burden, outcomes • Integration & coordination • Informed patient choice • Longitudinal resource use Three components of ACO infrastructure • Local Accountability for Cost, Quality, and Capacity • Shared Savings • Performance Measurement ACOs - a few characteristics are essential 1 Can provide or manage continuum of care as a real or virtually integrated delivery system 2 Are of a sufficient size to support comprehensive performance measurement 3 Capable of internally distributing shared savings payments Accountable Care Organizations “experimental model” Physician-Hospital Networks Physicians and beneficiaries make naturally occurring groups centered around hospitals. Surgeons Primary care specialists Hospital Other specialties Medical sub-specialists Linking Beneficiaries and Primary Care MD PCP PCP Hospital PCP PCP Virtual Physician-Hospital Network PCP Medical sub-specialists PCP Surgeons Other specialties PCP Hospital PCP Virtual Physician-Hospital Network Cohort of Linked Medicare Beneficiaries Medical sub-specialists PCP PCP Surgeons Other specialties Hospital Physician-Hospital Network PCP PCP Bynum, Health Services Research, 2007 Concentration of Care: Physician Visits Reliance on PHN for Physician Visits Number of Medicare Beneficiaries in Network Percent of Total Beneficiaries Number of Local Networks Percent of E&M Visits Within PHN Under 5,000 21.9% 2616 61.6 5,000 -10,000 26.4% 941 70.4 10,000 –15,000 21.1% 422 72.6 15,000 + 31.6% 376 73.8 Concentration of Care: Costs Percentage of Costs within PHN physicians and hospital Number of Medicare Beneficiaries in Network Percent of Physician costs (RVU) in PHN Percent of Total costs (RVU+DRG) in PHN Under 5,000 43.8 45.8 5,000 -10,000 62.9 63.2 10,000 –15,000 66.9 66.9 15,000 + 69.2 69.0 Concentration of Care: Hospital Stays Percentage of Hospitalizations occur at PHN hospital Number of Medicare Beneficiaries in Network Percent of Medical Hospitalizations in PHN Percent of Surgical Hospitalizations in PHN Under 5,000 61.5 18.9 5,000 -10,000 65.7 46.2 10,000 –15,000 66.1 54.4 15,000 + 65.3 59.8 Surgical hospitalizations to primary hospital and most commonly used Hospital for high DRG hospital stays Most of their care from a single identifiable providers grouped around a hospital Bynum, Health Services Research, 2007 Concentration of Work: Physician Percentage Physician’s billing accounted for by linked cohort Number of Medicare Beneficiaries in Network Percent of Patients billed who are in PHN by Specialty Primary Care Medical Specialty Surgeons Other Under 5,000 85% 48% 48% 30% 5,000 -10,000 85% 54% 49% 38% 10,000 – 15,000 84% 55% 49% 42% 15,000 + 84% 56% 50% 43% Concentration of Work: Hospital Percentage Hospital admits and costs accounted for by linked cohort Number of Medicare Beneficiaries in Network Percent of all Medical Hospital stays at hospital by linked cohort Percent of all Surgical Hospital stays at hospital by linked cohort Percent of Hospital Costs at hospital by linked cohort Under 5,000 71.1 64.0 69.2 5,000 -10,000 67.5 59.2 62.7 10,000 –15,000 66.5 57.6 60.6 15,000 + 65.9 55.9 58.7 Health Policy Research Current Studies using PHN • Racial disparities in ambulatory diabetes care • Surgical rates defining signature & efficiency • Care fragmentation across clinicians and setting Unifying feature of these studies is need for a defined population Health Policy Implications • Current Medicare markets beneficiaries concentrate care in virtual networks ◦ Especially if large hospital with broad services ◦ If not, it is possible to determine referral hospital • Population-basis and size allow measurement of outcomes and costs • With measureable performance for populations comes potential for accountability Acknowledgments NIA PO1 Co-investigators Team Dan Gottlieb Jon Skinner Don Carmichael Elliott Fisher Kathy Stroffolino Stephanie Tomlin Dartmouth Atlas team Julie Lewis Jack Wennberg Yunjie Song David Goodman Jason Sutherland Weiping Zhou Collaborators Brookings Institute