Urban/Rural Differences in Survival Among Medicare Beneficiaries with Breast Cancer
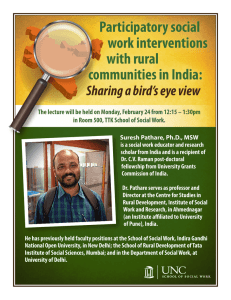
advertisement
Urban/Rural Differences in Survival
Among Medicare Beneficiaries with
Breast Cancer
Melony E.S. Sorbero, Ph.D.
RAND Corporation
Funded by Health Resources and Services Administration Office
of Rural Health Policy
Lisa R. Shugarman, Ph.D.
Haijun Tian, Ph.D.
Arvind Jain, M.S.
J. Scott Ashwood, M.A.
Background – Breast Cancer
• High incidence of breast cancer
– Most common cancer type in women
– Probability of diagnosis increases with age
• Second leading cause of cancer death in women
• American Cancer Society estimates for 2007
– 178,480 women will be diagnosed with invasive
breast cancer
– 40,460 will die
Sorbero 3 6-3-07
Background – Rural Health
• Rural areas are characterized by:
•
•
•
•
– Lower population density
– Large distances between individuals and
communities
– Large distances from urban centers
Experience challenges recruiting and retaining
providers
Hospitals and other facilities not capable of providing
all services
Populations in rural areas travel further and wait
longer for outpatient care
Rural elders more likely to be poor and near poor than
urban elders
Sorbero 4 6-3-07
Objectives
• To examine urban/rural differences in survival
among women age 65 and older who have been
diagnosed with breast cancer
• Survival differences may exist due to
– Urban/rural socioeconomic differences
– Lower local supply of cancer services and
providers in rural areas
Sorbero 5 6-3-07
Methods - Data
• Three data sources
– Surveillance, Epidemiology, and End Result
(SEER) Data (1995-1999)
• 14 cancer registries representing 26% US
population
– Linked Medicare administrative data (claims and
enrollment database) (1994-2003)
– Area Resource File (selected years for supply
variables)
Sorbero 6 6-3-07
Methods - Sample
• Inclusion criteria
– Breast cancer was the first diagnosed cancer
– Female
– Continuously enrolled in both Medicare Part A & B
for 1-year before diagnosis through 8 months after
diagnosis
• Exclusion criteria
– Enrolled in managed care (N=12,843)
– Eligible for Medicare for ESRD diagnosis or
disability (N=16,326)
– Breast cancer diagnosed via autopsy or death
certificate (N=47)
• N=32,626
Sorbero 7 6-3-07
Methods – Defining Urban/Rural
• County-based definitions create a single label for
counties with hetergeneous population densities
• 1990 Rural-Urban Commuting Area (RUCA) Codes
– Based on Census Bureau’s definitions of
urbanized areas and urban places (population
density and commuting patterns)
– Acknowledges great variation across rural areas
– Developed based on census tract and crosswalked to zip code
• Four categories created: Urban, Large Rural, Small
Rural, and Isolated Rural communities
Sorbero 8 6-3-07
Methods – Survival Analysis
• Cox proportional hazard models
– Hi(t) = 0(t ) exp{j1xi1... jkxik}
– Parametric tests of proportional hazards
assumption
• Overall survival time in months
– Date of diagnosis (mid-point of month) to
date of death
– Survivors censored at end of study period
Sorbero 9 6-3-07
Methods – Survival Analysis
• Variables entered into model in stages
– RUCA codes and demographic variables
• Age, gender, race, marital status, number of comorbidities
– Breast cancer variables
• Year of diagnosis, stage, ER and PR status
– Sociodemographic and supply variables
• 15% + of population not speaking English well, median
household income, and Medicaid status
• HPSA Residence, number of radiation oncologists and
number of hospital oncology services per 10,000 population
65+
Sorbero 10 6-3-07
Results – Sample Characteristics
Whole
Sample
Urban
Large Rural
Small Rural
Isolated
Rural
Mean Age**
76.0 (6.9)
75.9 (6.8)
75.8 (7.0)
76.7 (7.1)
76.7 (7.2)
% Married**
43.9
43.2
47.1
47.0
48.6
% Black**
6.3
7.5
0.6
0.1
0.1
% Medicaid
11.5
11.7
10.8
11.1
10.4
Mean Comorbidity*
1.8 (1.7)
1.8 (1.7)
1.6 (1.5)
1.5 (1.5)
1.6 (1.5)
Mean
Survival**
65.4 (26.4)
65.6 (26.5)
64.4 (26.2)
64.1 (26.0)
64.5 (26.6)
Variable
** p<0.01; * p<0.05
Sorbero 11 6-3-07
Results – Sample Characteristics
Whole
Sample
Urban
Large Rural
Small Rural
Isolated
Rural
In situ
13.6
14.2
10.8
10.2
11.0
1
46.8
46.6
48.4
47.0
47.7
2
29.0
28.7
29.7
31.1
31.1
3
5.0
5.0
5.2
5.8
4.5
4
3.3
3.3
3.6
3.3
2.6
Unstaged
2.3
2.2
2.3
2.7
3.2
ER positive
(%)**
59.3
58.4
62.6
65.6
63.4
PR positive
(%)**
49.1
48.0
53.8
56.4
54.9
Variable
Stage (%) **
** p<0.01; * p<0.05
Sorbero 12 6-3-07
Results – Sample Characteristics
Whole
Sample
Urban
Large Rural
Small Rural
Isolated
Rural
Not speaking
English well (%)**
14.8
16.5
10.8
3.0
3.6
Median income
<30,000 (%)**
33.0
23.8
65.3
92.3
84.1
HPSA (%)**
78.9
82.4
58.9
60.6
63.9
Mean N radiation
oncologists.**
1.3 (1.1)
1.5 (1.1)
0.4 (0.6)
0.2 (0.5)
0.1 (0.4)
Mean N hospitalbased oncology
services**
0.8 (0.8)
0.7 (0.3)
1.0 (0.9)
1.8 (1.8)
1.8 (2.2)
Variable
** p<0.01; * p<0.05
Sorbero 13 6-3-07
Multivariate Results
RUCA +
Demographic
+ Breast
Cancer
+ SES &
Supply
Variable
Hazard Ratio
Hazard Ratio Hazard Ratio
Urban
Referent
Referent
Referent
Large Rural
1.19****
1.13**
1.06
Small Rural
1.13***
1.06
0.95
Isolated
1.07
1.04
0.92
**** p<.0001; *** p<.001; ** p<.01
Sorbero 14 6-3-07
Multivariate Results - Supply
Full Model
Variable
Hazard Ratio
HPSA County
1.06*
Radiation Oncologists - Middle Tertile
0.99
Radiation Oncologists - Highest Tertile
1.05
Hospitals-based Oncology Services –
Middle Tertile
0.90***
Hospitals-based Oncology Services –
Highest Tertile
0.96
**** p<.0001; *** p<.001; ** p<.01; * p<.05
Sorbero 15 6-3-07
Summary
• Rural residence defined by RUCA categories not
consistently associated with mortality following a
breast cancer diagnosis
• Controlling for demographics, higher mortality in
large rural and small rural categories
• Residing in county with partial or whole HPSA
designation associated with increased mortality,
while increased supply of hospital-based oncology
services associated with decreased mortality
Sorbero 16 6-3-07
Limitations
• Measures of supply based on county not RUCA
codes
• Hospital-based oncology services a proxy for all
such providers
• Did not examine disease-free survival
• Findings may not be generalizable to Medicare
beneficiaries enrolled in managed care or nonelderly
Sorbero 17 6-3-07
Conclusions
• Women with breast cancer in rural areas experience
greater mortality
• Individual and regional socioeconomic factors
associated with risk of mortality
• Some evidence provider supply associated with
mortality in elderly breast cancer patients
• Policies should be developed to address provider
shortages in both rural and urban areas
Sorbero 18 6-3-07