PAY-FOR-PERFORMANCE IN TAIWAN OUTLINE OF PRESENTATION May Tsung-Mei Cheng
advertisement

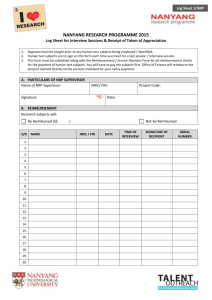
PAY-FOR-PERFORMANCE IN TAIWAN OUTLINE OF PRESENTATION May Tsung-Mei Cheng International Forum Princeton University I. QUICK OVERVIEW OF TAIWAN’S HEALTH SYSTEM II. OVERVIEW OF TAIWAN’S P4P PROGRAMS III. HOW P4P PROGRAMS IN TAIWAN WORK Academy Health Annual Research Meeting 2006 IV. FUNDING FOR P4P PROGRAMS IV. CONCLUDING OBSERVATIONS Seattle, Washington June 25-27, 2006 OVERVIEW OF TAIWAN’S HEALTH CARE SYSTEM I. QUICK OVERVIEW OF TAIWAN’S HEALTH SYSTEM • A single-payer system, “National Health Insurance” (NHI), established in 1995 and administered by the central government’s Bureau of National Health Insurance (BNHI) under the Department of Health (DOH). • Covers 99% of Taiwan’s population of 22.3 million; enrollment is mandatory • Comprehensive benefits: in- and outpatient care, drugs, dental, vision, traditional Chinese medicine, etc. • Smart Card (IC-Card) is used for accessing care in 100% of cases OVERVIEW OF TAIWAN’S HEALTH CARE SYSTEM OVERVIEW OF TAIWAN’S HEALTH CARE SYSTEM • NHI accounts for 56.55% of that total • Delivery system: private sector dominance (97% doctors in private practice; 84.8% hospitals private) • Out of pocket payments: 32% (by way of comparison, it is 30% in Canada) • Global budget: 4 sectors -- hospital, primary care, dental, traditional Chinese medicine • NHI is financed from 3 sources: households (38%), employers (35%) and government (27%) • Payment of providers is primarily FFS, some DRGs, case payment, capitation, and P4P • The premium structure is very complex. Roughly speaking, households pay a premium of 4.55% of income. • Patients have complete freedom to choose providers; co-pay varies by level of providers • Taiwan’s total NHE is 6.17% GDP (2004) • 100% electronic claim submission • No waiting lines like in the UK or in Canada • Satisfaction rate among citizenry is high: 70s% 1 GENESIS OF P4P INTIATIVES IN TAIWAN • NHI Law made no special provision re quality; emphasis was on access and coverage. II. OVERVIEW OF TAIWAN’S P4P SYSTEM • Even so, Taiwan’s BNHI has engaged in a number of quality improvement initiatives, of which P4P is one. • Several pilot programs began in late 2001. • In January 2006, two additional programs were initiated. 5 PILOT P4P PROGRAMS + 2 TRIAL PROGRAMS A. The “Original 5”: Implementation began late 2001 9 9 9 • • Asthma (based on process measures) Diabetes (based on process measures) Breast cancer (based on outcome measures) Cervical cancer Tuberculosis III. HOW P4P PROGRAMS IN TAIWAN WORK B. New - January 1, 2006: Trial period 1 yr. • Hypertension • Depression Voluntary participation by primary care physicians, hospitals, or clinics and other care facilities. To participate in the program, providers must adopt the following quality assurance measures: – Meet formal qualification/certification requirements for participating medical personnel (physicians, nurses, dieticians), hospitals and clinics. – Follow treatment guidelines such as the widely accepted guidelines for DM care developed by the U.S. based ADA. – Establish case-based Electronic Medical Record (EMR) and medical record management systems. Reporting: claims data, supplemented by selfreported performance data on the outcome and process parts, using a special webpage outside of regular claims filing channel. ILLUSTRATIONS: - Breast Cancer - Diabetes - Asthma 2 Breast Cancer – Starting date: November 1, 2001 – Outcome-based payment, contingent upon yearend total survival and disease-free survival – Provider participation: 3 medical centers, 5 hospitals, 2 regional hospitals for a combined total of 200 professional medical personnel committed to the program – 2,381 new patients covered in the program in 2004 = 44.34% of all BRAC patients in Taiwan EXTRA PAYMENTS FOR BREAST CANCER P4P Outcome-based bonus payments on top of regular case-based payment: – 1% of regular case payment at 1st yr. survival – 2% “ “ “ “ “ 2nd yr. “ – 5% “ “ “ “ “ 5th yr. “ Diabetes Mellitus (DM) Breast Cancer • Starting date: November 1, 2001 RESULTS: • 4th leading cause of death in Taiwan (2003) – The sole P4P program among the 5 that bases payment on outcomes, the BRAC P4P met 100% target goals for 5-year total survival and disease-free survival. – Patient satisfaction extremely high. • Accounting for 11.5% of NHI spending • Quality of care remained poor due to the fragmented care under the FFS payment system • Previous government attempts to improve the quality of care yielded mediocre results, thought to be due to lack of structural support and financial incentive to providers to deliver appropriate care. Diabetes Mellitus (DM) Diabetes Mellitus (DM) • Using disease management team care model, chronic care services are delivered by certified DM physicians, nurses, and dietitians 4 x/yr. Provider participation: • Required services include and tests for HbA1C, urine micro-albumin, eye exam, BP and LDL check, foot care, and patient counseling Hospitals/Clinics 2002 Cases 2003 2004 159 313 464 32,267 80,207 125,530 9/2005 596 143,148 • % DM patients enrolled in DM-P4P program: 2004 17.3% 2005 19.7% 3 Diabetes Mellitus (DM) EXTRA PAYMENTS FOR DIABETES P4P Complex process-based bonus scheme: – – – – – 1845 points for initial visit for new patient 875 points for each repeat visit (up to 3x/yr.) 2245 points for annual evaluation visit 200 points for drug refill prescription Eye exam separate payment NOTE: 1 POINT = NT$ 1 = US$ 0.03 Other medical services and drugs for DM patients enrolled in the program are paid under the traditional FFS payment scheme. Asthma • Provider participation: Cases A. Process indicators: Showed improvements across the board in 2004 over previous studies B. Outcomes indicators: HbA1c Systolic BP Diastolic BP LDL Pre-trial* 22.1 44.5 24.2 14.1 Post-trial** 16.1 40.4 22.5 13.6 % Change - 27.0 % - 9.2 % - 7.0 % - 3.5 % * ‘Pre-trial’ column: Numbers refer to % of DM patients in the experimental group whose biological and metabolic conditions were not well-controlled before entering trial ** ‘Post-trial’ column: Numbers refer to % of patients whose biologic and metabolic conditions remain not well-controlled after trial began. EXTRA PAYMENTS FOR ASTHMA P4P • Starting date: November 1, 2001; beginning in January 2004 payments increased also for care for co-morbidities of asthma patients Hospitals/clinics RESULTS: 2002 2003 2004 110 320 982 7,229 31,344 106,353 9/2005 1,252 148,831 1st Year: – – – – NT$ 500 ‘management fee’ for new patients NT$ 200 for 2nd visit NT$ 200 for 3rd visit NT$ 900 for year-end (4th) visit 2nd Year: – 4 visits @ NT$ 200, 200, 200, and 900 for ea. visit NOTE: NT$ 100 = US$ 3.05 Asthma RESULTS After 2 yrs. of follow up: – No apparent difference in frequency of outpatient visits – Cost for outpatient care: ↑ 16.27% – “ for TOTAL care: ↑ 9.17% – Frequency of emergency visits: ↓ 39.94% – Cost for emergency care: ↓ 30.90% – Frequency of hospitalization: ↓ 46.31% – Cost of inpatient care: ↓ 44% – Length of stay: ↓ 51.74% IV. FUNDING FOR P4P PROGRAMS 4 HOW MUCH IS COMMITTED TO “PERFORMANCE PAYMENTS”? • Beginning in 2006, funds for bonus payments are made available through a special, ear-marked budget line item titled “Other Budgets” within the NHI’s overall global budget. • Therefore, the P4P system is not budget-neutral. • Instead, performance payments are made in addition to the regular FFS payments for services rendered. IV. CONCLUDING OBSERVATIONS Total funding for P4P committed in 2006, by source of funding: GB for primary care NT$ 356 ml. Hospital GB NT$ 725 ml. Other sources NT$ 69 ml. TOTAL $ COMMITTED: NT$ 1,166 ml. At this time, total P4P spending under Taiwan’s NHI is between .3% and .4% of total NHI spending, but it is slated to grow in the future. It would appear that, based on the results of the P4P programs currently being adopted in Taiwan, financial incentives do play an important role in the delivery of better quality care and better outcomes. This is a conclusion the authors of a national DM study also reached. Of course, the “results” shown here may also be driven by other factors, e.g.: – guideline-based disease management helped guide/change provider behavior. – Coordinated efforts from other DOH agencies to promote better process and outcome, e.g., the Bureau of Health Promotion in the DOH actively works with the BNHI to improve DM care. To my knowledge, a full-fledged statistical analysis of Taiwan’s P4P programs controlling for possibly confounding factors has not yet been undertaken. Finally, whatever one may think of single-payer health insurance systems, Taiwan’s single payer system is an ideal platform for P4P programs, because that system embodies an information infrastructure that yields comprehensive and up-to-date information on the care actually delivered to patients. It allows Taiwan to base its P4P system more heavily on claims data, rather than on the less reliable, selfreported performance data now so widely used for P4P throughout the world. Of course, to the extent that claims for payment may be fraudulent or miscoded, such data are no more reliable than self-reported performance data. 5 All P4P systems, around the world, should operate on Ronald Reagan’s famous maxim: TRUST, BUT VERIFY. 6