Acknowledgements Racial Differences in the Impact of HMO Coverage of Diabetes Blood Glucose
advertisement
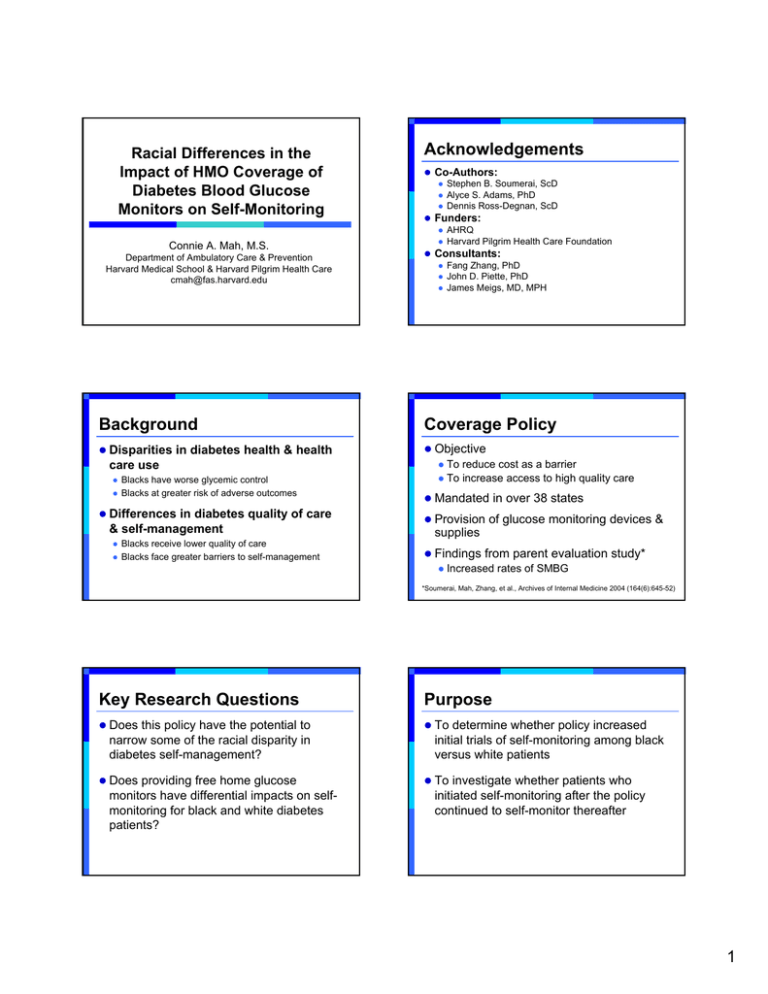
Racial Differences in the Impact of HMO Coverage of Diabetes Blood Glucose Monitors on Self-Monitoring Connie A. Mah, M.S. Department of Ambulatory Care & Prevention Harvard Medical School & Harvard Pilgrim Health Care cmah@fas.harvard.edu Acknowledgements z Co-Authors: z Stephen B. Soumerai, ScD z Alyce S. Adams, PhD z Dennis Ross-Degnan, ScD z Funders: z AHRQ z Harvard Pilgrim Health Care Foundation z Consultants: z Fang Zhang, PhD z John D. Piette, PhD z James Meigs, MD, MPH Background Coverage Policy z Disparities in diabetes health & health z Objective z To reduce cost as a barrier z To increase access to high quality care care use z z Blacks have worse glycemic control Blacks at greater risk of adverse outcomes z Differences in diabetes quality of care & self-management z z Blacks receive lower quality of care Blacks face greater barriers to self-management z Mandated in over 38 states z Provision of glucose monitoring devices & supplies z Findings from parent evaluation study* z Increased rates of SMBG *Soumerai, Mah, Zhang, et al., Archives of Internal Medicine 2004 (164(6):645-52) Key Research Questions Purpose z Does this policy have the potential to z To determine whether policy increased narrow some of the racial disparity in diabetes self-management? z Does providing free home glucose monitors have differential impacts on selfmonitoring for black and white diabetes patients? initial trials of self-monitoring among black versus white patients z To investigate whether patients who initiated self-monitoring after the policy continued to self-monitor thereafter 1 Research Design & Setting HPHC Coverage Policy z Research Design z Start of Implementation: Oct 1,1993 z Longitudinal, retrospective cohort analysis z Study Setting z z Harvard Vanguard Medical Associates (HVMA) Harvard Pilgrim Health Care (HPHC) Study Cohort z Objective z To motivate diabetes patients to start monitoring their blood glucose z Policy Benefits z Provision of glucose monitoring devices z Self-management training & education z Lower copay for up to 3 months’ supply of test strips (≤$5/script) HVMA Data Sources (1992-1996) Race Identification z Definition of Diabetes: ≥ 1 hospital discharge Dx; or ≥ 2 outpatient Dx; or z ≥ 1 insulin or oral sulfonylurea Rx z HbA1c Lab Results Ambulatory Medical Records z z Black or White race only Clinical Encounters PATIENT STUDY ID z Continuous enrollment (1992-1996) Pharmacy Claims Dispensed Test Strips Drug Therapy Membership/ Enrollment z N=2,275 adult patients Demographic Info Days Enrolled Census File Home Address (linked by census block group) Key Measures Main Analytical Methods z Main independent measure z Race (black v. white) z Outcome measures z Incidence of SMBG (≥1 strip) z Discontinuation of SMBG (>180 days w/out strips) z Kaplan-Meier & Log-Rank Tests z Covariates z Fixed (age, sex, census-derived median HH income & educational level, drug type, BMI, HbA1c test, primary health site) z TimeTime-Varying (mean HbA1c values in prior month, # MD visits per month) z z Cumulative rates of initiation of SMBG Cumulative rates of discontinuation of SMBG z Extended Segmented Cox Models Adjusting for patient-level fixed & time-varying covariates z Relative (hazard) rates of initiation of SMBG (blacks relative to whites) z 2 Pre-Policy Patient Differences Any Insulin Black White (n=264) (n=613) Oral Sulfonylurea Only Black White (n=250) (n=739) Female 63.3% 50.4% 57.6% 44.0% Mean Age 52±12 52±14 53±11 60±11 Mean BMI 32.7±7.1 30.5±7.5 32.0±6.3 32.1±7.2 Mean HbA1c 9.5±1.7 9.0±1.4 9.1±1.9 8.1±1.4 % Any SMBG 64.8% 77.8% 34.0% 30.8% Initiation of SMBG Bold denote p<0.05 Any Pre-Policy Oral Treatment (N=904) Any Pre-Policy Insulin Treatment (N=567) 0.8 phase-in 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0 0 Est. Haz Ratio 95% CI 1.09 0.84,1.40 1.35* 1.05,1.72 Pre-Policy Difference 1 (Black vs. White) Post-Policy Difference (Black vs. White) phase-in Controlling for age, glycemic control, time-dependent drug use, and timedependent number of physician visits Apr-95 Dec-94 Aug-94 Apr-94 Dec-93 Aug-93 Apr-93 Dec-92 Aug-92 Apr-92 Apr-95 Dec-94 Aug-94 Apr-94 Dec-93 Aug-93 Apr-93 Dec-92 Aug-92 Apr-92 Censoring at first insulin use or never initiated SMBG * p <0.05 Black White Post-Policy SMBG Initiators Discontinuation of SMBG % SMBG Discontinuation % with SMBG 1 100 90 80 70 60 50 40 30 20 10 0 Black (n=59) White (n=134) 6 Months 12 Months 18 Months Months since SMBG Initiation p<0.05 Discontinuation = >180 days without test strip use 3 Summary Limitations z Trials of self-monitoring in post-policy z Missing race data Î increase in SMBG Î greater for blacks on oral therapy z Persistence after initiation of SMBG in post-policy Î short-lived z Important unmeasured factors Socio-cultural factors (attitudes, perceptions, cultural beliefs/values) z Duration of illness z Intensity of medication use z z Single HMO Take Home Points z Coverage is effective in engaging patients in SMBG particularly blacks z Sustainability must be addressed z Additional interventions may be necessary to improve long-term adherence and clinical outcomes 4