Chronic Care Delivery
advertisement
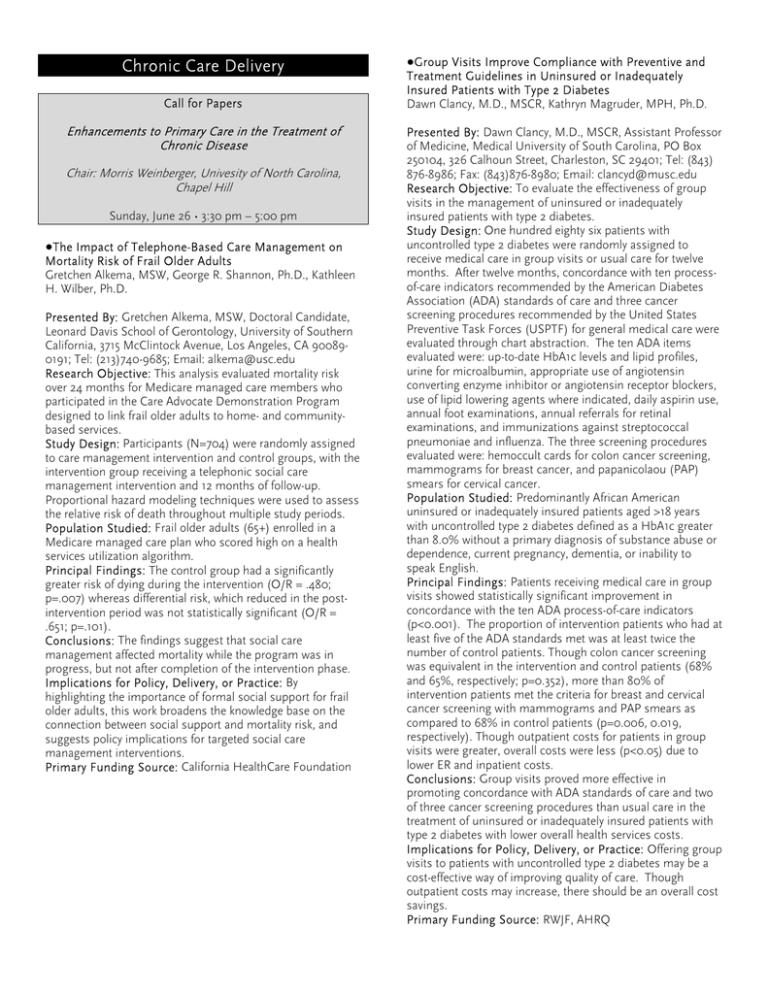
Chronic Care Delivery Call for Papers Enhancements to Primary Care in the Treatment of Chronic Disease Chair: Morris Weinberger, Univesity of North Carolina, Chapel Hill Sunday, June 26 • 3:30 pm – 5:00 pm ●The Impact of Telephone-Based Care Management on Mortality Risk of Frail Older Adults Gretchen Alkema, MSW, George R. Shannon, Ph.D., Kathleen H. Wilber, Ph.D. Presented By: Gretchen Alkema, MSW, Doctoral Candidate, Leonard Davis School of Gerontology, University of Southern California, 3715 McClintock Avenue, Los Angeles, CA 900890191; Tel: (213)740-9685; Email: alkema@usc.edu Research Objective: This analysis evaluated mortality risk over 24 months for Medicare managed care members who participated in the Care Advocate Demonstration Program designed to link frail older adults to home- and communitybased services. Study Design: Participants (N=704) were randomly assigned to care management intervention and control groups, with the intervention group receiving a telephonic social care management intervention and 12 months of follow-up. Proportional hazard modeling techniques were used to assess the relative risk of death throughout multiple study periods. Population Studied: Frail older adults (65+) enrolled in a Medicare managed care plan who scored high on a health services utilization algorithm. Principal Findings: The control group had a significantly greater risk of dying during the intervention (O/R = .480; p=.007) whereas differential risk, which reduced in the postintervention period was not statistically significant (O/R = .651; p=.101). Conclusions: The findings suggest that social care management affected mortality while the program was in progress, but not after completion of the intervention phase. Implications for Policy, Delivery, or Practice: By highlighting the importance of formal social support for frail older adults, this work broadens the knowledge base on the connection between social support and mortality risk, and suggests policy implications for targeted social care management interventions. Primary Funding Source: California HealthCare Foundation ●Group Visits Improve Compliance with Preventive and Treatment Guidelines in Uninsured or Inadequately Insured Patients with Type 2 Diabetes Dawn Clancy, M.D., MSCR, Kathryn Magruder, MPH, Ph.D. Presented By: Dawn Clancy, M.D., MSCR, Assistant Professor of Medicine, Medical University of South Carolina, PO Box 250104, 326 Calhoun Street, Charleston, SC 29401; Tel: (843) 876-8986; Fax: (843)876-8980; Email: clancyd@musc.edu Research Objective: To evaluate the effectiveness of group visits in the management of uninsured or inadequately insured patients with type 2 diabetes. Study Design: One hundred eighty six patients with uncontrolled type 2 diabetes were randomly assigned to receive medical care in group visits or usual care for twelve months. After twelve months, concordance with ten processof-care indicators recommended by the American Diabetes Association (ADA) standards of care and three cancer screening procedures recommended by the United States Preventive Task Forces (USPTF) for general medical care were evaluated through chart abstraction. The ten ADA items evaluated were: up-to-date HbA1c levels and lipid profiles, urine for microalbumin, appropriate use of angiotensin converting enzyme inhibitor or angiotensin receptor blockers, use of lipid lowering agents where indicated, daily aspirin use, annual foot examinations, annual referrals for retinal examinations, and immunizations against streptococcal pneumoniae and influenza. The three screening procedures evaluated were: hemoccult cards for colon cancer screening, mammograms for breast cancer, and papanicolaou (PAP) smears for cervical cancer. Population Studied: Predominantly African American uninsured or inadequately insured patients aged >18 years with uncontrolled type 2 diabetes defined as a HbA1c greater than 8.0% without a primary diagnosis of substance abuse or dependence, current pregnancy, dementia, or inability to speak English. Principal Findings: Patients receiving medical care in group visits showed statistically significant improvement in concordance with the ten ADA process-of-care indicators (p<0.001). The proportion of intervention patients who had at least five of the ADA standards met was at least twice the number of control patients. Though colon cancer screening was equivalent in the intervention and control patients (68% and 65%, respectively; p=0.352), more than 80% of intervention patients met the criteria for breast and cervical cancer screening with mammograms and PAP smears as compared to 68% in control patients (p=0.006, 0.019, respectively). Though outpatient costs for patients in group visits were greater, overall costs were less (p<0.05) due to lower ER and inpatient costs. Conclusions: Group visits proved more effective in promoting concordance with ADA standards of care and two of three cancer screening procedures than usual care in the treatment of uninsured or inadequately insured patients with type 2 diabetes with lower overall health services costs. Implications for Policy, Delivery, or Practice: Offering group visits to patients with uncontrolled type 2 diabetes may be a cost-effective way of improving quality of care. Though outpatient costs may increase, there should be an overall cost savings. Primary Funding Source: RWJF, AHRQ ●Assessment of Chronic Illness Care for Diabetes in Primary Care Clinics Amer Kaissi, Ph.D., Michael Parchman, M.D. Presented By: Amer Kaissi, Ph.D., Assistant Professor, Health Care Administration, Trinity University, One Trinity Place, # 58, San Antonio, TX 78212; Tel: (210)999-8132; Fax: (210)9998108; Email: amer.kaissi@trinity.edu Research Objective: The majority of care provided to patients with type 2 diabetes is provided in the primary care setting. The Chronic Illness Care model suggests that there are six structural dimensions of primary care teams that are important in improving the quality of diabetes care. The objective of this study is to assess the degree to which the six structural dimensions of the Chronic Illness Care model are implemented in primary care practices by comparing responses given by caregivers, administrative staff and an independent external observer, and to examine the relationship of these responses with selected quality of care process measures. Study Design: The “Assessment of Chronic Illness Survey” developed by Bonomi, Von Korff, Wagner and colleagues includes 25 questions that constitute 6 structural dimensions: organization, community linkages, self-management support, decision support, delivery system design, and clinical information systems. The wording of each question was modified slightly to be specific to the care of patients with type 2 diabetes. The quality measures included were percentage of patients in each clinic who had the following within the past 12 months: referral for dilated eye exam, foot exam, two blood pressure measurements, one HbA1c measurement, one urine micro albumin measurement, and one lipid measurement.Means of scores given by two groups of respondents and an external observer were compared using one-way Analysis of Variance (ANOVA). To determine which of these assessments were more related to actual quality measures, Spearman correlation coefficients were calculated. Population Studied: The survey was filled by 54 caregivers (physicians and nurses), 77 administrative staff (medical assistants, receptionists, office managers and other staff), and one external observer in 20 primary care clinics in the South Texas Ambulatory Research Network. Thirty patients in each clinic were included in the study and their charts were reviewed to assess the quality process measures. Principal Findings: Overall, administrative staff were more likely to rate their clinics higher on each structural dimension in the ACIC than caregivers or the external observer, with the differences being significant for three main dimensions: delivery system design F=3.064; P<0.05, clinical information systems F=8.301; P<0.05 and overall score that combines all six dimensions F=5.247; P<0.05. The observer’s assessment, and to a lesser degree the caregivers’ assessment were more consistently correlated with quality of care measures than the administrative staff assessments. For example, the observer’s assessment on four structural dimensions (community linkages, self-management support, decision support and clinical information systems) were statistically related to the percentage of patients with eye exam, while the caregiver’s assessment of only one dimension (decision support) and none of the administrative staff assessment were related to that same measure. Conclusions: Assessment of a primary care clinic’s structure seems to be more accurate when conducted by an external observer and by the caregivers that practice in the clinic, rather than by the administrative staff in the clinic. Administrative staff may tend to exaggerate the adequacy of the structures that are present in their clinics. Implications for Policy, Delivery, or Practice: The first step toward redesigning primary care practices in order to improve the quality of diabetes care is to accurately assess structures that are directly related to quality measures. This study suggests that a version of the ACIC tool that is tailored to diabetes management can be used to examine structural dimensions in primary care clinics, but may be more valid if completed by caregivers or an independent observer. The next step is to develop a profile of primary care clinics that provide higher quality of care. Primary Funding Source: AHRQ, Health Resource and Service Administration ●Care Management for Elders with Chronic Conditions in a Medicare Coordinated Care Demonstration Cheryl Schraeder, RN, Ph.D., FAAN Presented By: Cheryl Schraeder, RN, Ph.D., FAAN, Head, Health Systems Research Center, Carle Foundation, 307 East Oak #3, PO Box 718, Mahomet, IL 61853; Tel: (217)586-4164; Fax: (217)586-2174; Email: Cheryl.Schraeder@carle.com Research Objective: Does the Carle Medicare Coordinated Care Demonstration improve self-management behaviors, clinical health status, medication management for specified health conditions, patient satisfaction, service utilization and total Medicare cost of care compared to usual care? Study Design: A prospective, 48 month randomized clinical trial using an intent-to-treat approach. The Carle MCCD includes a multi-modial intervention provided by primary care teams (primary care physician, nurse partner and patient) and is based on core components of the Chronic Care Model: selfmanagement support, decision support, delivery system design, and clinical information systems. Population Studied: 1,948 Medicare beneficiaries (Treatment=980; Control=968) who enrolled in the Carle MCCD between April 2002 and April 2003 who self-reported a diagnosis of coronary artery disease, congestive heart failure, atrial fibrillation, diabetes, or chronic obstructive pulmonary disease and live in 11 counties in east-central Illinois or western Indiana. Principal Findings: There were no significant differences between the treatment and control groups in baseline characteristics, including demographics, health or functional status, targeted diagnoses, hospitalizations or ED visits, satisfaction, self-care behaviors or clinical health status measures. At the end of the first 12 months, based on a rolling enrollment period, there were significant differences between the treatment and control groups. The treatment group had higher scores in overall satisfaction with the health care they received (9.0 vs 8.7) and higher satisfaction with their nurse partner compared to their physicians' office nurses (9.3 vs 9.0). Treatment group patients with diabetes had higher rates of annual foot exams (52% vs 37%) and patients with congestive heart failure had higher rates of daily weighing (28% vs 17%). Treatment group patients had higher rates of LDL (78% vs 64%) and triglycerides testing (79% vs 65%) in accordance with the medical guidelines used in this study. Treatment group patients with diabetes had highher rates of HbA1c (81% vs 68%) and albuminuria testing (68% vs 34%). The treatment group also had higher rates of hypertension control (59% vs 45%). Conclusions: These outcome trends are continuing in the second evaluation period, 24 months after patient enrollment. We are in the process of acquiring the Medicare claims data through the end of 2003 to evaluate the economic impact of the intervention on Medicare costs. Implications for Policy, Delivery, or Practice: Early evaluation results suggest that an intervention composesd of primary care teams, using a combined case and disease management approach, can significantly impact the challenges older adults face in managing and living with multimorbid conditions. Primary Funding Source: CMS ●CCM Implementation and Patient Perceived Selfmanagement Support for Their Chronic Illness Shinyi Wu, Ph.D., Marjorie Pearson, Ph.D., Stephen Shortell, Ph.D., Jill Marsteller, Ph.D., Michael Lin, MS, Emmett Keeler, Ph.D. Presented By: Shinyi Wu, Ph.D., Associate Engineer, Health, RAND Corporation, 1776 Main Street, Santa Monica, CA 90401; Tel: (310)393-0411; Fax: (310)260-8155; Email: shinyi@rand.org Research Objective: Patient self-management is critical to managing chronic illnesses. The Chronic Care Model (CCM), a quality improvement (QI) framework, encourages organizations to make system changes and work with patients to support them in self-management. This study investigates whether patients report more self-management support with sites that do more to implement CCM. Study Design: An observational study conducted by the RAND/Berkeley Improving Chronic Illness Care Evaluation of chronic care collaboratives. The QI changes undertaken by participating organizations during the collaboratives were collected by interviews and progress reports. The data were then coded according to a hierarchical typology of CCM intervention strategies, and rated on their “depth”, i.e., likelihood of impact, using predefined rating criteria. Each organization received a summary rating for the overall changes made to implement the CCM and a sub rating for specific changes made to support patient self-management. Patients from the study organizations were surveyed 10 to 18 months after the collaboratives had begun. The telephone survey included questions on their perceptions of the selfmanagement support received from their healthcare providers in nine areas. OLS regressions were used to examine the relationships between patients’ ratings of their received selfmanagement support and the organizations’ implementation performance as defined by the overall and self-managementspecific implementation depth rating, controlling for average patient education, language, and disease type. Site variation in implementation depth was evaluated by one-sample t-tests. Population Studied: 1787 patients from 32 healthcare organizations that participated in one of three QI collaboratives to improve congestive heart failure, diabetes, or asthma care. Principal Findings: The organizations varied in the depth of overall CCM implementation (p<0.01) and the depth of changes to support patient self-management (p<0.01). Despite that, on average, in six of the nine areas patients perceived very good self-management support from providers (score 70 or higher in a 0-100 scale). The three areas that received lower ratings included proactive follow-up calls from providers (average score of 33), receipt of self-management plan copy (53), and appointment reminders (65). For these three areas, the intensity of changes an organization made in the area of self-management support was positively related to the levels of support perceived by patients (p< .10). In addition, patients from sites that had the best implementation of CCM overall not only were more likely to receive a proactive call but also were given greater confidence to control their disease (p <. 10). Sites that served a higher percentage of English speaking patients were rated higher. Conclusions: In general, patients reported good selfmanagement support from providers. Greater implementation of CCM changes, nevertheless, enhanced this critical factor of chronic illness care, especially in giving patients a written plan, appointment reminders, proactive follow-up calls, and overall confidence to control their disease. Implications for Policy, Delivery, or Practice: Successful implementation of CCM, specifically in the area of selfmanagement support, increases patients’ tools and confidence in managing their disease. . Organizations should be encouraged to intensify CCM change efforts to improve self-management support. Primary Funding Source: RWJF Call for Papers Organizational Factors & Tools for Improving Practice Chair: Shoshanna Sofaer, Baruch College Tuesday, June 28 • 8:30 am – 10:00 am ●Relationship Between the Chronic Care Model and Diabetes Outcomes Laurie Hurowitz, Ph.D., Benjamin Littenberg, M.D., Charles D. MacLean, M.D. Presented By: Laurie Hurowitz, Ph.D., Research Assistant Professor, General Internal Medicine, University of Vermont College of Medicine, 371 Pearl Street, Burlington, VT 05401; Tel: 802-847-7937; Email: laurie.hurowitz@uvm.edu Research Objective: As health care organizations consider improvement to better manage chronic illness, the Chronic Care Model has been promoted as a comprehensive model to guide change. Various components of the Chronic Care Model (CCM), such as use of clinical information systems and patient/provider reminders, provider education on clinical guidelines, and promotion of self-management techniques, are currently under study for their relationship to patient outcomes. To date, results have been mixed. However, few data exist on the efficacy and validity of the CCM, as a whole, and patient outcomes. The current study was designed to examine the relationship between glycemic control for patients diagnosed with diabetes and primary care practice organization across all components of the CCM. Study Design: This was a cross-sectional, observational study, using lab measures of glycemic control for adult patients diagnosed with diabetes at the baseline of a larger study on diabetes care, the Vermont Diabetes Information System (VDIS). Primary care practitioners (PCPs) responded to a standard survey measuring practice conformance with the CCM, the Assessment of Chronic Illness Care (ACIC). The instrument was modified to be specific to diabetes care. The ACIC survey, typically employed as a pre- and postassessment in quality improvement initiatives, includes 33 items, each on an 11-point scale. Higher scores are associated with greater conformance with the CCM. All analyses were conducted at the practice level. If more than one PCP responded to the survey, their scores were averaged to produce one practice level score. Glycosylated hemoglobin, as measured by the A1C assay, was used to assess glycemic control. A1C values were averaged at the practice level. Population Studied: Of the 118 PCPs in the 57 rural practices in Vermont and northern New York involved in the VDIS study, 47 PCPs in 28 practices completed surveys assessing practice conformance with the CCM. There were 3,701 patients with diabetes in these 28 practices. Principal Findings: A simple linear regression of the relationship between conformance with the CCM and average glycemic control showed that greater conformance with the CCM (higher scores) was associated with lower average A1C (coefficient = -0.088 p=.122, 95% CI -0.201, 0.025). Adjusting for age, gender, and panel size (number of patients with diabetes in a practice), the relationship between the total survey score and glycemic control had a coefficient of -0.091 (p=.055; 95% CI -0.184, 0.002). Conclusions: Greater conformance with the Chronic Care Model is related to better glycemic control among patients with diabetes. Implications for Policy, Delivery, or Practice: Absent controlled trials demonstrating the validity and efficacy of the CCM, these data are among the first to show a relationship between overall conformance with the CCM and patient outcomes. Primary Funding Source: No Funding ●Asthma Patients and the Patient-Clinician Relationship: A Qualitative Study of Continuity of Care Margaret Love, Ph.D., Sarah B. Wackerbarth, Ph.D., Renee V. Girdler, M.D., Arch G. Mainous, III, Ph.D., Dennis E. Doherty, M.D. Presented By: Margaret Love, Ph.D., Assistant Professor and Research Director, Family Practice and Community Medicine, University of Kentucky, K302 Kentucky Clinic, Lexington, KY 40536-0284; Tel: (859)323-6747; Fax: (859)323-6661; Email: mlove@email.uky.edu Research Objective: Previous research suggests that asthma patients value an ongoing relationship with their doctors or other health care professionals, seemingly more so than do patients without chronic illness or with certain other chronic illnesses. However, the reasons asthma patients value continuity of care have not been explicated. The aim of this study was to better understand asthma patients’ perceptions of their relationships with health care practitioners, particularly their reasons and priorities for continuity of care over time with the same practitioners. Study Design: In 2004 we conducted a qualitative focus group study. Participants also completed a brief survey about their asthma severity and demographic characteristics. Prompts for the audiotaped focus group discussions asked participants what they value in their relationships with health care professionals, why seeing the same clinician would be important to asthma patients, and how they develop and manage relationships with one or more clinicians. We used open coding of the focus group transcripts. Two researchers independently identified themes regarding what patients liked about their clinicians and relationships with them. Then the researchers discussed and consolidated the themes. Population Studied: Adult asthma patients were recruited through the University of Kentucky Family Medicine clinic, through the University of Kentucky Pulmonary Care clinic, and through flyers posted at community grocery stores, public libraries, and YMCAs. We conducted six focus groups with three to seven participants each. Of the 26 patients that participated, most were female, white, 41-60 years of age, and had health insurance. Principal Findings: Several themes emerged. Some themes addressed positive health outcomes resulting from care: clinician competence, successful diagnosis, and successful treatment. Other themes addressed the interpersonal process: the patient feels comfortable; the clinician talks, listens, and explains; and the clinician is straightforward. Many themes were about relationship qualities or information that can only be developed or acquired over time: the physician “knows me,” the patient trusts the clinician, the clinician trusts the patient, the clinician is reliable and can be depended on to help, the patient receives individualized care that takes disease history and preferences into account, and the physician cares about the patient. Also, patients wanted to avoid “starting over” each visit. Conclusions: Our results provide insight into what asthma patients find valuable about continuity of care with the same health care practitioner. Some of the patients’ concerns may be considered typical indices of high quality care (e.g., improved health outcomes) or of positive interpersonal interactions (e.g., listening). Their other concerns point to relationship qualities and knowledge that require a shared history (e.g., “knows me,” mutual trust, and avoid starting over). Implications for Policy, Delivery, or Practice: Better understanding of what asthma patients value about continuity can be used to develop practice systems that meet patients’ health care needs. Future research can evaluate whether improving the aspects of health care delivery that asthma patients value would improve their health care outcomes. In the context of the current health care environment, in which continuity of care with individual clinicians is diminishing, it will be important to develop strategies to meet chronically ill patients’ special concerns. Primary Funding Source: National Heart Lung and Blood Institute ●The Influence of Primary Care Practice Climate on Medical Services Costs and Quality of Care Douglas Roblin, Ph.D., David H. Howard, Ph.D., Edmund R. Becker, Ph.D., E. Kathleen Adams, Ph.D., Sheldon Greenfield, M.D. Presented By: Douglas Roblin, Ph.D., Research Scientist, Research Department, Kaiser Permanente Georgia, 3495 Piedmont Road NE, Building 9, Atlanta, GA 30305; Tel: (404) 364-4805; Fax: (404)364-7361; Email: Douglas.Roblin@KP.Org Research Objective: Improved teamwork among clinical staff has been cited as an opportunity for improving the quality and safety of health care delivery in the United States. Little is known, however, about: 1) whether primary care practices with higher levels of teamwork, collaboration, and care coordination (“practice climate”) are cost-saving or costgenerating compared with practices with lower levels, and 2) how differentials in service delivery costs are associated with variation in quality of care. We studied the influence of practice climate on medical services costs per member per month (PMPM) and diabetes quality of care among members empanelled to 16 semi-autonomous and self-directed adult medicine teams of the primary care delivery system in a group model managed care organization (MCO). Study Design: Member-level data (demographic, clinical, financial) were organized into 2 cross-sections (2000 and 2002). Intermediate outcomes (glycemic, lipid, and blood pressure control; ACEI and statin use) in the subsequent year (2001 and 2003) were obtained for members with diabetes. Practitioner and support staff surveys of practice climate were conducted in 2000 (N=183, 80% response rate) and 2002 (N=227, 91% response rate). Practice climate is a multidimensional construct, encompassing 7 subscales (e.g. delegation and collaboration, autonomy, and team ownership) with good reliability (Cronbach’s alpha > 0.80). Medical services costs PMPM were estimated as a function of team practice climate, controlling for member characteristics (age, gender, 7 major chronic diseases) using the 4-part modelling strategy of the RAND HIE. Diabetes quality of care was estimated as a function of average medical services costs PMPM per team (adults with diabetes), controlling for member characteristics. All models were estimated with fixed effects per team; and, standard errors were adjusted for clustering of members within team. Population Studied: 166,209 and 167,664 members, and 10,472 and 12,710 adults with diabetes, empanelled to the teams in 2000 and 2002, respectively. Principal Findings: Primary care and ancillary services costs PMPM were higher (p<0.05) on teams with more favorable perceptions of practice climate in both 2000 and 2002. On average, a member empanelled to a team with favorable practice climate (75th percentile) incurred $5-$6 more PMPM than a member empanelled to a with unfavorable practice climate (25th percentile). Acute and specialist care costs PMPM did not vary with practice climate. Teams with higher primary care and ancillary services costs PMPM per diabetes patient had greater likelihood of glycemic, lipid, or systolic blood pressure control (p<0.05) among their diabetes patients. For every 100 adults with diabetes, a team with $30 greater primary and ancillary services costs PMPM per diabetes patient achieved 7 more patients with glycemic control, 4 with lipid control, and 4 with blood pressure control. Conclusions: Primary care practices with higher levels of teamwork, collaboration, and coordination among practitioners and staff were associated with increased primary care and ancillary services costs PMPM and better intermediate outcomes among adults with diabetes. Implications for Policy, Delivery, or Practice: In the shortterm (1-2 years), an MCO that invests in enhancing primary care teamwork should not expect cost-savings because the better intermediate quality of care that obtains from improved teamwork may require increased services use (e.g. HbA1c tests for monitoring glycemic control). Primary Funding Source: AHRQ ●A Tale of Two Ownership Types: Implications for Organizational Resources, External Incentives, and the Implementation of the Chronic Care Model Margaret Wang, Ph.D., MPH, Stephen M. Shortell, Ph.D., MPH, Thomas G. Rundall, Ph.D. Presented By: Margaret Wang, Ph.D., MPH, Postdoctoral Research Fellow, UCLA/RAND Health Services Research Training Program, UCLA/RAND, 1776 Main Street, Santa Monica, CA 90401; Tel: (310)393-0411 x6077; Email: mcywang@berkeley.edu Research Objective: To compare freestanding physician organizations (Pos) with those affiliated with health systems or owned by hospitals on the availability of organizational resources; impact of external incentives on quality; and in turn their performance on chronic care management. Study Design: This study analyzed data collected by the National Study of Physician Organizations (NSPO), a crosssectional census survey (response rate = 70%) of Pos in the U.S. (September 2000 through September 2001). Multivariate regression analyses were performed to compare PO ownership types while adjusting for organizational and environmental characteristics. Population Studied: The studied population consisted of 1,104 Pos (67% medical groups and 33% IPAs) employing 20 or more physicians in the U.S., excluding single specialty Pos such as radiology, pathology, chiropractic, podiatry, ophthalmology, anesthesiology, emergency medicine, and/or imaging. Analyses were restricted to 966 Pos (58% freestanding physician-owned and 42% systemaffiliated/hospital-owned) reported treating at least one of the following chronic conditions: asthma, CHF, depression, or diabetes. Principal Findings: On the average, Pos adopted approximately four of the eleven items in the Chronic Care Management Index (CCMI), a composite measure reflecting the extent to which the Chronic Care Model (CCM) is implemented in Pos. System-affiliated/hospital-owned Pos implemented the CCM to a greater extent (i.e., about five items), compared to freestanding physician-owned Pos (i.e., about four items). In addition, Pos affiliated with health systems or owned by hospitals were found to have more sophisticated clinical information technology and offer more comprehensive case manager services to physicians, compared to Pos owned by physicians. PO receiving public recognition (e.g., blue ribbon awards) as an external incentive was found as a significant and robust factor positively associated with CCM implementation in all Pos, corresponding to a one-item increment in the CCMI. Subsample analyses revealed that the level of clinical information technology adoption and PO receiving better contracts as an external incentive for quality were both positively correlated with CCM implementation in the freestanding physicianowned PO sub-sample, but not in the systemaffiliated/hospital owned sub-sample, suggesting that these factors operate differently among these two PO ownership types. Conclusions: Results from this study indicate that Pos affiliated with health systems or owned by hospitals have implemented the CCM to a greater extent than Pos owned by physicians. Further analyses suggest that this difference is possibly due to system-affiliated/hospital-owned Pos having more organizational resources for chronic care management. Implications for Policy, Delivery, or Practice: This study provides important comparative evidence on the quality of chronic care management between system-affiliated/hospitalowned Pos and freestanding physician-owned Pos. These findings underscore the need to develop collaborative efforts between physician groups and health systems in order to facilitate synergistic use of resources for chronic care delivery. In addition, they highlight the importance for policy makers to consider using a mixture of resource-based (e.g., pay for performance) and institutional-based (e.g., blue ribbon awards) incentives to motivate improvement in chronic care delivery. Primary Funding Source: RWJF, Health Research and Education Trust Fellowship ●Factors Associated with Family Caregivers’ Experience of End of Life Care Anne Wilkinson, Ph.D., MS Presented By: Anne Wilkinson, Ph.D., MS, Senior Behavioral/Social Scientist, Health, RAND, 3720 Upton Street NW, Washington, DC 20016; Tel: (202) 895-2659; Fax: (202) 966-5410; Email: annew@rand.org Research Objective: Families and other informal caregivers are essential in meeting an individual’s physical and psychosocial needs and in accomplishing treatment goals. Caregivers face a wide spectrum of emotional, physical, and economic consequences as a result of their caregiving responsibilities, including caregiver burden. We describe the evidence base regarding care processes and interventions on end of life caregiver burden to inform a research agenda for palliative care. Study Design: As part of a systematic review of the end-of-life literature, we reviewed articles that evaluated caregiver burdens related to end-of-life care. Population Studied: We conducted a systematic review using Medline, Database of Reviews of Effects, the National Consensus Project bibliography, and recommendations of an international expert panel. We augmented our search with several systematic reviews from both Health Canada and National Institute for Clinical Excellence, United Kingdom. The searches were limited to published articles in the English language (1990-2004), involving adult human subjects. Principal Findings: From 24,423 total citations, we identified 18 systematic reviews, 23 intervention studies, and 134 observational reports addressing caregiver outcomes or concerns, excluding bereavement. The final report included 8 high-quality systematic reviews, 13 intervention studies, and 17 observational studies of caregiving to patients with cancer, dementia, and organ system failure. Outcomes included burden, stress, depression, anxiety, satisfaction (e.g., with care, life satisfaction, satisfaction with caregiving), caregiver morbidity and mortality, unmet needs, institutionalization, and place of death. Most articles involved interventions for caregivers to dementia patients or palliative care interventions for caregivers to advanced cancer patients. Dementia caregiver interventions showed small benefits for caregivers. Moderate positive effects were found for cancer patient caregivers using palliative care services, especially home care. However, the high levels of reported psychological morbidity and unmet need indicate that not all caregiver needs were being met. Families of younger, poorer, and more functionally dependent patients were the most likely to report losses in work hours, jobs, or the family’s savings. Caregivers to patients with substantial unmet needs were more likely to consider euthanasia or physician-assisted suicide, to have depressive symptoms or anxiety, and to report that caring for the patient interfered with their lives. Conclusions: This systematic review identified a large and diverse literature concerning caregiver burden. Interventions had little consistent effect on caregiver outcomes and most studies focused on dementia or cancer. Very few studies used RCT design, outcome measures differed widely across studies, and few studies examined palliative caregiving for nondementia, non-cancer deaths. Caregiver burden may be too multidimensional to be described in a single scale, improved by single component or short-term interventions, or generalizable across diverse populations. Implications for Policy, Delivery, or Practice: Informal caregiving will be a critical component of care for the increasing numbers of disabled elderly, yet research designs have been weak, interventions limited, and outcome assessment inadequate. Redesign of theoretical models, measurement tools, and intervention designs is a priority. Primary Funding Source: AHRQ, National Institute for Nursing Research Call for Papers Do Physicians Appropriately Intensify Care for Patients with Chronic Illnesses? Chair: R. Adams Dudley, University of California, San Francisco Tuesday, June 28 • 10:30 – 12:00 younger or with comorbid COPD. Presence of hypertension and diabetes increased the odds of initiation, but had no significant effect on persistence among initiators. Conclusions: For patients who start on beta-blocker and ACE inhibitor therapies, there is a significant decline in use over the course of two years. Implications for Policy, Delivery, or Practice: Quality improvement efforts have focused on prescription of betablockers upon hospital discharge for AMI. An important next step is to focus on long-term persistence on these therapies. Primary Funding Source: No funding source ●Refill Persistence with Beta-Blocker and ACE Inhibitor Therapy after Acute Myocardial Infarction Ayse Akincigil, Ph.D., John Bowblis, MA, Carrie Levin, Ph.D., Saira Jan, PharmD., Minalkumar A. Patel, M.D., Stephen Crystal, Ph.D. ●National Spending on Bariatric Surgery and Bariatric Medications Didem Bernard, Ph.D., William Encinosa, Ph.D., Claudia Steiner, M.D., MPH, Chi-Chang Chen, MS, Pharmacist Presented By: Ayse Akincigil, Ph.D., Assistant Research Professor, Institute for Health, Health Care Policy and Aging Research, Rutgers, The State University of New Jersey, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732) 9325348; Fax: (732) 932-8592; Email: aakincigil@ihhcpar.rutgers.edu Research Objective: In prevention of secondary heart attack, the importance of beta-blocker and ACE inhibitor therapy is greatly recognized. However, long-term adherence with this recommendation is not well described. Our objectives are to present rates and predictors of patient medication refill persistence with beta-blocker and ACE inhibitor therapy within the 24 months following an acute myocardial infarction (AMI). Study Design: A retrospective, observational study using linked medical and pharmacy claims from a large health plan. Population Studied: 1,624 subjects aged 18 or older with an inpatient claim for AMI (ICD-9-CM: 410.xx) between June 1, 2000 and May 31, 2001, continuously enrolled in the health plan throughout the 24 months following AMI. 23% were in point of service or HMO products; the remaining members were in indemnity products. Principal Findings: Among subjects with AMI and no counterindication for beta-blockers, 23% never filled an outpatient prescription for beta-blockers. Discontinuation is defined as failure to fill a subsequent prescription within 60 days after exhausting the days supplied from prior prescriptions. Among initiators, the discontinuation rate was 33% after a year, and 49% after 2 years (based on KaplanMeier estimates). Medication possession ratio (MPR) was calculated as the ratio of number of days supplied to number of days in the period. Persistence was defined as MPR > 0.75. Multivariate models predicting initiation and persistent use controlled for gender, age, income at zip-code level, plan type, number of hospitalization days for AMI, and presence of comorbid conditions. Odds of persistent beta-blocker use were higher for patients living in high income areas, and for those with chronic conditions that increase the risk of a secondary AMI (i.e., diabetes, hypertension, dyslipidemia, congestive heart failure, cerebrovascular and peripheral vascular disease). Number of hospitalized days for AMI had a positive effect on initiation, but not on long-term persistence. The ACE inhibitor initiation rate was 60%. Of those who initiated ACE inhibitor therapy, 30% discontinued therapy within the first year, and 48% within two years. Odds of persistent ACE inhibitor use were lower for patients aged 55 or Presented By: Didem Bernard, Ph.D., Economist, CFACT, AHRQ, 540 Gaither Road, Rockville, MD 20850; Tel: (301) 4271682; Email: dbernard@ahrq.gov Research Objective: Due to the growing epidemic of obesity, bariatric medicine is an emerging specialty of medicine dealing with methods of weight loss among the obese. Very little is known about the current use of bariatric surgery and bariatric medicines and the potential demand for these bariatric treatments. Study Design: We examine insurance claims for bariatric drugs and bariatric surgery among 5.1 million non-elderly people covered by 45 large employers across the U.S. in 2002. We also examine all inpatient discharges for bariatric surgery in 36 states from the 2002 HCUP State Inpatient Databases, representing 90% of all discharges from U.S. community hospitals. Population Studied: 5.1 million non-elderly people covered by 45 large employers across the U.S. in 2002 and all inpatient discharges for bariatric surgery in 36 states from the 2002 HCUP State Inpatient Databases. Principal Findings: In 2002, 76% of bariatric surgeries were covered by private insurance. Among the non-elderly population in the U.S. with private health insurance in 2002, there were 6.4 million morbidly obese adults clinically eligible for bariatric surgery. We estimate that 79,276 bariatric surgeries were performed on 78,336 adults (or 1.2% of those eligible for the surgery) at a total spending of $1.62 billion. Employers paid $1.56 billion of that expense. About 14% of the $1.62 billion was paid to surgeons. While 31% of those eligible for the surgery were men, only 16% of the surgeries were performed on men. Moreover, men had an inpatient death rate 7.75 times higher than women (0.80% vs 0.18%). In 2002, among a non-elderly sample of 5 million people with drug coverage under 45 large employers across the country (a 3.2% sample of all employer-sponsored health insurance with drug coverage in the U.S.), there were 1.14 million obese adults clinically eligible for bariatric drug therapy. We found that 22,119 adults (or 1.9% of those eligible) actually used insurance-covered, bariatric prescription drugs, at a total spending of $6.7 million, or $300 per user per year. Employers paid $6 million of that total expense. While 49% of those eligible were men, only 23% of those taking the bariatric medications were men. Conclusions: Less than 2% of the non-elderly adults with private insurance who were clinically eligible for bariatric treatments actually had bariatric drug use or bariatric surgery in 2002. Thus, future demand for bariatric treatments may be quite large. Implications for Policy, Delivery, or Practice: Due to the growing epidemic of obesity, not only Medicare but also employers are considering whether they should cover bariatric treatments. This study provides data on the cost and extent of utilization of bariatric surgery and medications among the privately insued population in 2002. Primary Funding Source: AHRQ ●The Impact of Adverse Events on Warfarin Prescribing in Atrial Fibrillation: a Matched-Pair Analysis Niteesh K. Choudhry, M.D. Presented By: Niteesh K. Choudhry, M.D., 1620 Tremont Street, Suite 3030, Boston, MA 02446; Tel: (617)278-0930; Email: choudhry@fas.harvard.edu Research Objective: Warfarin is received by only 30-60% of appropriate patients with atrial fibrillation (AF). Physicians’ experiences with warfarin-associated adverse events may be an important determinant of warfarin use. Some adverse events (i.e., major hemorrhage in an AF patient treated with warfarin) may be more influential than others (i.e., thromboembolic stroke in an AF patient who did not receive warfarin). Understanding the determinants of warfarin use may help improve the quality of care for patients with AF. Study Design: Using linked administrative data for 116,200 elderly patients with non-valvular non-transient AF, we identified 3921 who were hospitalized for major hemorrhage while on warfarin and 8720 hospitalized for thromboembolic strokes while not on warfarin. We identified the physicians responsible for the care of the patients that experienced adverse events and selected pairs of patients treated by that physician (one patient before and one patient after the adverse event (i.e., exposure). Using this paired analysis we compared the odds of warfarin receipt for pre- and post-exposure patients after adjusting for stroke and bleeding risk factors that also might influence warfarin use. We also evaluated a comparison outcome -- the odds of angiotensin converting enzyme (ACE) inhibitor prescriptions before and after exposure -- that should not have been influenced by warfarinassociated adverse events. Population Studied: Community dwelling elderly patients (aged 66 and older) in Ontario, Canada Principal Findings: For the 530 physician who were exposed to an adverse bleeding event and treated other AF patients during both the 90-day period before and the 90-day period after exposure, the odds of warfarin prescribing was 21% lower for post-exposure patients (adjusted OR 0.79, 95% CI: 0.621.00). Greater reductions in warfarin prescribing were found in analyses using patients for whom more time had elapsed between physician exposure and patient treatment. There were no statistically significant changes in warfarin prescribing after a physician had a patient experience a stroke while not on warfarin or in the use of ACE inhibitors by physicians who had patients with either bleeding events or strokes. Conclusions: These results suggest that a physician’s experience with warfarin-associated bleeding events can influence warfarin use. In contrast, adverse events that are likely associated with underuse of warfarin may not affect subsequent prescribing. Implications for Policy, Delivery, or Practice: Our findings highlight the need for strategies to modify physicians’ perceptions of the risks associated with warfarin use and to encourage warfarin prescribing for patients with AF. Primary Funding Source: Harvard Pilgrim Health Care Foundation and Canadian Institute for Health Research ●Evaluation of a Patient-Centered Care Coordination/Home-Telehealth Disease Management Program for Veterans with Diabetes Neale Chumbler, Ph.D., W. Bruce Vogel, Ph.D., Mischka Garel, MPH, Haijing Qin, MS, Rita Kobb, MS, ARNP, Patricia Ryan, MS, RN Presented By: Neale Chumbler, Ph.D., Research Health Scientist, Assistant Professor, Department of Health Services Research, Management and Policy, University of Florida, VA HSR&D/RR&D Rehabilitation Outcomes Research Center North Florida/South Georgia Veterans Health System, 1601 SW Archer Road (151B), Gainesville, FL 32608; Tel: (352)3761611 x4920; Fax: (352)271-4540; Email: neale.chumbler@med.va.gov Research Objective: To evaluate the effectiveness of a patient-centered care coordination/home-telehealth (CC/HT) program as an adjunct to treatment for veterans with diabetes. This program consists of a care coordinator (RN or ARNP) who uses disease management principles through the care continuum, manages treatment for veterans with diabetes, and equips the patient in self-management skills to reduce costly health services (e.g., hospitalizations). Study Design: This study evaluated a Department of Veterans Affairs (VA) CC/HT program in a Florida, Puerto Rico, and Georgia veteran population with diabetes. Care coordinators monitored patient responses through an in-home messaging device (called a Health Buddy). A total of 400 high-use veterans with diabetes (two or more all-cause hospitalizations or emergency department [ED] visits in the year prior to enrollment) were enrolled in one of four VA CC/HT programs. A matched comparison group of 400 veterans with diabetes who met the same inclusion criteria was randomly selected from VA administrative data. The matched comparison group was similar in age, facility site, marital status and service connected disability status. Propensity scores were applied to improve the balance between the treatment and comparison groups. Service use outcomes were measured at 12 months before and after enrollment. A difference-in-differences (DiD) approach was used in the multivariable statistical models to measure the treatment effect for patients in the programs. Population Studied: High service use veterans with diabetes. Principal Findings: One-year after enrollment, there was a significant difference between the treatment and comparison groups in the likelihood of one or more need-based primary care visits (p < .01), increasing in the treatment group by 7.3 percentage points (from 45.6% to 52.9%) and decreasing in the comparison group by 11.6 percentage points (from 40.8% to 29.2%). Need-based primary care clinic visits are newly scheduled visits that enable the veteran to be seen “just in time” rather than “just in case” (traditional care---seeing patients at regular intervals to catch problems). There was also a significant difference between groups in one or more emergency room visits (p < .0001); the comparison group increased by 49.3% and the treatment group showed a reduction of 17.4%, this finding may be the result of using inclusion criteria as an outcome variable. Conclusions: The Congressional Budget Office has indicated that regression to the mean can bias the kinds of simple prepost studies of disease management programs that have characterized the literature to date. The DiD design of the present work, however, avoids this pitfall. The rigor of our study design strengthens the finding that the CC/HT program was effective in increasing new, need-based primary care visits. The increase of such visits supports the notion of the “just in time” care approach, where the veterans’ health status was monitored and their clinical needs were met before their health deteriorates. Implications for Policy, Delivery, or Practice: Our results are consistent with the CC/HT program improving the quality of care for veterans through the incorporation of new patient education and telecommunications technologies that involve greater, more timely patient-clinician interaction. In this way, the program supports greater access to care and improved self-management for veterans with diabetes. Primary Funding Source: VA ●Progress in Reducing Cardiovascular Risk in Diabetes: Is it Enough? Monika M. Safford, M.D., Katharine A. Kirk, Ph.D., Catarina I. Kiefe, Ph.D., M.D. Presented By: Monika M. Safford, M.D., Associate Director, Deep South Center on Effectiveness, Medicine, Birmingham VA Medical Center and University of Alabama at Birmingham, 1717 11th Avenue South, MT643, Birmingham, AL 35294-4410; Tel: (205)934-6883; Fax: (205)934-7959; Email: msafford@uab.edu Research Objective: Hypertension (HTN) is a dominant cardiovascular risk factor, especially among people with diabetes (DM), at least as important as glycemic control. Yet, many individuals with DM have uncontrolled blood pressure (BP). National programs have recently emphasized cardiovascular risk factor control in DM, and the Veterans Administration (VA) has made HTN management and DM part of its nationwide performance measurement system. We studied nearly current patterns of BP medication management in a VA medical center. Study Design: We defined a retrospective DM cohort in 20012, and assessed HTN and BP medications at 2 observation periods: 2001-2 and 2003-4. We used the Veterans Health Information Systems and Technology Architecture (VISTA) for this study, an electronic medical record including all pharamcy, utilization and lab test results. Diagnostic codes and DM medications were used to define DM, and diagnostic codes and BP levels to define HTN. BP medication was “appropriately intensified” if dose was increased or a new BP medication class added after the last eligible primary care visit with SBP>=140mmHg (uncontrolled HTN). Separate logistic regressions for each observation period included age, sex, race/ethnicity, and SBP level. Population Studied: All DM patients cared for at a VA medical center in 2001-2. Principal Findings: The 6810 DM patients had mean (standard deviation) baseline age 64.7(10.8) years, 2.2% were women and 19.4% were African American. In 2001-2, 5190 patients had DM and HTN; in 2003-4, 3711 patients had DM and HTN, representing those who remained in care. Patients had many opportunities for management: the mean number of primary care visits was 6.1(3.7) in 2001-2 and 6.3(3.6) in 2003-4. The mean number of BP medications at last measure was 2.2(1.4) in 2001-2 and 2.7(1.9) in 2003-4. HTN control improved somewhat, but remained suboptimal: at last measure, 59.0% had uncontrolled HTN in 2001-2, and 50.6% in 2003-4. Of all the 2074 uncontrolled in 2001-2 who remained in care in 2003-4, 57.3% remained uncontrolled. BP management in those with uncontrolled HTN in the 2 assessment periods was more intense in 2003-4. For example, in 2001-2, 20.8% were on >2 BP medications, and 40.3% in 2003-4. Similarly, medications were intensified at only 33.7% of visits with uncontrolled HTN in 2001-2; this rose considerably but was still only 49.3% in 2003-4. In multivariable analysis, people of different ages, race/ethnicity or sex had generally similar patterns of medication intensification. Conclusions: Two thirds of intensification opportunities were missed in 2001-2. For those who remained in care, that proportion improved to half in 2003-4, and overall BP control improved modestly. Secular trends and the fact that the 20034 group represented a longer VA care period may have contributed to the improvement. Nevertheless, care fell considerably short of optimal in both observation periods. Implications for Policy, Delivery, or Practice: Efforts to improve HTN management in the very high risk group of persons with diabetes are bearing fruit. However, considerable room for improvement remains. Our data may also reflect a beneficial effect of remaining in care in a large healthcare system. Primary Funding Source: VA Related Posters Poster Session A Sunday, June 26 • 2:00 pm – 3:15 pm ●Utilization of Statin Therapy during the Two Years Following Acute Myocardial Infarction. Ayse Akincigil, Ph.D., John Bowblis, MA, Carrie Levin, Ph.D., Saira Jan, PharmD., Minalkumar A. Patel, M.D., Stephen Crystal, Ph.D. Presented By: Ayse Akincigil, Ph.D., Assistant Research Professor, Institute for Health, Health Care Policy and Aging Research, Rutgers, The State University of New Jersey, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732) 9325348; Email: aakincigil@ihhcpar.rutgers.edu Research Objective: Clinical trials have demonstrated the survival benefits of long term and regular use of statins. We describe rates and predictors of statin therapy utilization, including initiation, refill persistence and discontinuation within the 24 months following an acute myocardial infarction (AMI). Study Design: A retrospective, observational study using linked medical and pharmacy claims from a large health plan. Population Studied: 1,624 subjects aged 18 or older with an inpatient claim for AMI (ICD-9-CM: 410.xx) between June 1, 2000 and May 31, 2001, continuously enrolled in the health plan throughout the 24 months following AMI. 23% were members of point of service or HMO products; the remaining were in indemnity products. Principal Findings: Forty percent of patients initiated the therapy within the 30 days following AMI; 35% initiated after a delay of 30 days or more; and 25% did not fill any prescription for statins in the two-year follow up period. Discontinuation is defined as failure to fill a subsequent prescription within 60 days after exhausting the days supplied from prior prescriptions. Based on Kaplan-Meier estimates, discontinuation rates were 12% after 3 months, 30% after a year, and 46% after 2 years. Members of managed care products were more likely to initiate the therapy and to be persistent compared to members of indemnity plans. Patients between 45 and 75 years of age were more likely to initiate the therapy, and patients aged 55 or older were more likely to persist. Length of hospital stay for AMI significantly affected initiation and persistence rates. Odds of initiation increased by presence of dyslipidemia and the number of chronic conditions that increase the risk of a secondary AMI (i.e., diabetes, hypertension, congestive heart failure, cerebrovascular and peripheral vascular disease); odds of initiation decreased among patients living with renal disease. Conclusions: Lack of long-term adherence to statin therapy represents a source of missed opportunities for prevention of second AMIs. Younger patients and those in indemnity plans appear at particular risk for treatment dropout. Implications for Policy, Delivery, or Practice: Secondary prevention efforts need to focus not only on initiation but also adherence to statin therapy. Primary Funding Source: Other Population Studied: Community-dwelling beneficiaries who participated in the Medicare Current Beneficiary Survey during 2000-2002 and who were hospitalized and discharged home; n=1351, representing 2,883,726 persons after weighting. Principal Findings: Self-management ability was associated with significantly reduced length of stay ranging between 1.62.0 days, in a multivariate model that adjusted for age, gender, race, and self-reported health status. Unmet need was not associated with length of stay in similar models. Fifteen percent of the participants who were hospitalized were readmitted within 60 days of discharge; n=202. Participants who were readmitted were less likely to be married, more likely to live alone, and had a greater number of self-reported chronic conditions. Self-management was not associated with readmission, but having an unmet need and being unmarried increased the odds of readmission significantly; ORs=1.48 and 1.99, respectively, after adjustment for age, gender, race, selfreported health status, and length of stay of the initial admission. Conclusions: Improving older adults’ ability to self-manage their health conditions may decrease the duration of their stays in hospitals. Similarly, access to personal assistance for functional deficits after hospital discharge may decrease the likelihood of hospital readmissions. Implications for Policy, Delivery, or Practice: These findings could help health care providers target a vulnerable group of older adults for intensive discharge planning and postdischarge assistance to improve continuity of care. These data also suggest that self-management skills may be relevant to Medicare coverage policy. Primary Funding Source: RWJF ●The Effects of Self-Management and Home Help on Older Adults' Use of Hospitals. Alicia Arbaje, M.D., MPH, Jennifer Wolff, Ph.D., Neil Powe, M.D., MPH, MBA, Gerard Anderson, Ph.D., Chad Boult, M.D., MPH, MBA ●Development of a Nutrition Quality of Life Survey to Improve Patient-Centered, Chronic Nutrition Care Judith Barr, Sc.D., Gerald Schumacher, PharmD, Ph.D. Presented By: Alicia Arbaje, M.D., MPH, Robert Wood Johnson Clinical Scholar, Medicine, Johns Hopkins University, 600 North Wolfe Street, Carnegie 291, Baltimore, MD 21287; Tel: (410)614-4525; Fax: (410)614-9068; Email: aarbaje@jhmi.edu Research Objective: Older adults who transition from hospital to home may experience lapses in continuity of care and subsequent adverse events. Their ability to self-manage their health conditions and obtain help with their functional deficits may favorably affect their hospital utilization patterns and minimize the risk of discontinuity of care. We examined whether self-management skills and lack of help with functional deficits are associated with the length of stay and the likelihood of readmission among hospitalized communitydwelling Medicare beneficiaries. Study Design: Cohort study in which beneficiaries were interviewed at home and monitored through Medicare claims for hospital use during the following year. Measures include self-reported ability to manage one’s health conditions on a 4point scale, unmet need for functional deficits, that is, lack of personal assistance for difficulty with 6 ADLs and 6 IADLs, length of stay of first admission, and non-elective readmission within 60 days of hospital discharge. Presented By: Judith Barr, Sc.D., Director, NERCOA, National Education and Research Center for Outcomes Assessment, Northeastern University, 360 Huntington Avenue - 105DK, Boston, MA 02115; Tel: (617) 373-4188; Fax: (617) 373-2968; Email: j.barr@neu.edu Research Objective: To develop a Nutrition Quality of Life (NQOL)survey that can be used to improve patient-centered care by identifying patient-reported areas of concern and to target interventions to improve adherence to chronic nutritional therapy. Study Design: In Stage 1, we conducted 10 patient and 7 clinician focus groups in 6 geographically diverse US cities to identify physical, psychological, and social factors affecting NQOL following recommended dietary modifications. Each session was transcribed and read by the investigators and three content consultants. In Stage 2, we developed a 47-item survey, written at the 5th-6th grade level, that included 6 item clusters: food impact, self-image, self- efficacy, psychological, interpersonal, and physical. In Stage 3, we mailed the draft survey instrument to each of the focus group participants, asking the patients to complete the survey and asking both patients and clinicians to suggest improvements. Population Studied: The 65 patients in the focus groups of Stage 1 were 72/28% female/male; age range 18->65 years; 25/63/12% low/middle/high income; 66/22/11/1% Caucasian/African-American/Hispanic/other; and included 7 medical conditions that led to seeking medical nutrition therapy. The 46 dietitians in the focus groups were from outpatient, inpatient, military, public health, and home care practice sites. Principal Findings: 37 patients, responding to the survey in Stage 3, averaged 9 minutes to complete the instrument. Only one of the 47 items had more than two missing responses. Based on Stage 3 patient and clinician responses, the survey was modified to add 4 questions, and improve syntax and question order. A color format for visually scoring the survey was also developed. 81% of the patients and 71% of the clinicians said the survey would be helpful to assess the impact of dietary modifications on quality of life. Conclusions: Focus groups provide a forum for collection of valuable patient-reported concerns which can be used in the development of measures to support chronic care. Further work on the 51-item NQOL, version 1.4, will involve psychometric analyses based on larger population testing, and validity/reliability studies. Implications for Policy, Delivery, or Practice: Results from a survey to identify patient-centered concerns during long term nutritional therapy may assist care givers to target interventions to improve adherence to chronic dietary changes Primary Funding Source: American Dietetic Association Foundation ●Care Coordination using Information Sharing Systems for Children with Autism Spectrum Disorders Christine Burns, EdM, MBA, Susan Taylor Brown, Ph.D., MSW, Megan MacWilliams, Shawn Ryan Presented By: Christine Burns, EdM, MBA, Associate Director, Pediatrics, Strong Center for Developmental Disabilities, 601 Elmwood Avenue, Rochester, NY 14642; Tel: (585) 275-6681; Fax: (585) 275-3366; Email: Christine_Burns@urmc.rochester.edu Research Objective: Children with autism have special health care needs that require complex care provided by multiple specialists that typically continue throughout their lifetimes. Their care is often fragmented, and parents are challenged to be sure their children are receiving all the necessary care. Emerging electronic information sharing systems hold particular promise for improving the coordination of care of children with special needs. The purpose of this study was to identify the characteristics of care coordination programs, including family access to information, for children with Autism Spectrum Disorder within the University Centers for Excellence in Developmental Disabilities Education, Research, and Service (UCEDD) network. Study Design: A six-item telephone questionnaire was conducted surveying national interdisciplinary programs based in University Centers for Excellence in Developmental Disabilities that serve children with autism spectrum disorder who have special health care needs. Summary statistics for frequency were calculated for the total survey sample to describe comparisons between and among groups. Population Studied: Sixty-one University Centers for Excellence in Developmental Disabilities Education, Research, and Service serving individuals who have developmental disabilities. Principal Findings: Of the 41% UCEDDs providing services or supports for children with ASD 84% provide diagnosis/evaluation, 84% behavioral consultation, 88% educational consultation, 96% training for service providers, 88% training for parents, 72% parent support groups, 96% technical assistance and 72% research. These supports are provided in the Center and/or through collaboration with community programs. 72% reported involvement with care coordination for children with ASD. The number of disciplines providing services or supports to children with ASD ranged from 3 to 16. The majority of Centers involved 11 or more disciplines. The primary discipline was Speech Language Pathology followed by Psychology and OT. Respondents indicated that the primary method for information exchange was telephone followed by mail. Use of EIS by Centers included 64% Internet, 52% intranet, 20% VPN. EMRs are available in 32% of the Centers. Only 4% of Centers have intersystem access by community-based agencies and 0% allows direct access by parents. Conclusions: Considerable variability in implementation models for CC continues to exist. Patient and family participation is quite limited and must be improved to assure family-centered care. The majority of programs have fragmented care coordination models. Improvement of care coordination programs is needed to enhance health and functional outcomes of children with ASD. Implications for Policy, Delivery, or Practice: Models of care delivery must include effective care coordination that includes participation by consumers and families and utilizes efficient information exchange methodologies. Initiatives such as the Medical Home may be able to address these issues and improve family-centered care using EIS. There will be a need for TA for parents and care provides alike. Primary Funding Source: HRSA ●How do Practice Characteristics Relate to Diabetes Treatment Patterns Among Patients' Primary Care Providers? Catharine Burt, EdD, Jane E. Sisk, Ph.D. Presented By: Catharine Burt, EdD, Chief, Ambulatory Care Statistics Branch, CDC's National Center for Health Statistics, 3311 Toldeo Road, Hyattsville, MD 20782; Tel: (301)458-4126; Fax: (301)458-4032; Email: cburt@cdc.gov Research Objective: As the U.S. population ages and chronic disease management becomes increasingly important, policymakers are exploring methods to influence physicians’ management. This study analyzed whether selected characteristics of physicians’ practices influenced management of diabetes, a prevalent condition with growing evidence of appropriate management. Study Design: We examined whether management of diabetes by a patient’s primary-care provider was related to practice characteristics that might exert an influence through internal processes or external guidelines: number of physicians, type of practice (solo, single specialty group, multispecialty group), percentage of revenue from managed care, percentage of revenue from selected payers (Medicaid, Medicare, private insurance, other), and use of electronic medical records. Using logistic regression, we analyzed whether or not specific aspects of diabetes management, specified as dependent variables, were associated with these practice characteristics, with physician specialty and patient age, gender, and race as additional independent variables. We selected indicators recommended in evidence-based guidelines: for all diabetics - recording blood pressure, counseling for diet and nutrition, and counseling for exercise; for diabetics with hypertension – prescribing medications recommended by the Joint National Commission (JNC-VI). We also included for all diabetics - prescription of an angiotensin-converting-enzyme (ACE) inhibitor or angiotensin II-receptor blocker (ARB). The study involved a secondary analysis of encounter data from the 2001 and 2002 National Ambulatory Medical Care Survey, a national probability survey of office-based physicians with 65-70-% annual response rates. We specified each dependent variable as the percentage of visits with the specific aspects of management recoded, and used SUDAAN to account for the complex sample in determining statistical significance. Population Studied: Physician office visits (n=1,110) to primary care providers for adult patients (age = 18 years) with diabetes (ICD-9-CM code = 250 for any of three possible diagnoses). Principal Findings: Among visits by diabetics, 86.5% of the visits had recorded blood pressure, 38.1% had documented counseling for diet and nutrition, 18.4% for had exercise counseling recorded, and 21.3% had prescriptions for an ACEinhibitor or ARB. At visits by diabetics who were also hypertensive, 48.9% of the visits had prescriptions for JNC-VIrecommended medications. Regression results found few of the studied practice characteristics related to diabetes management. Physicians in practices with electronic medical records had higher odds of prescribing an ACE-inhibitor or ARB at all visits (p<.01). General and family practitioners had higher odds than cardiovascular specialists of documenting dietary counseling (p<.05) and exercise (p=.06). Conclusions: Management of diabetes varies little by organizational and financial characteristics of diabetic patients’ primary-care providers. Implications for Policy, Delivery, or Practice: In all practice settings, substantial room for improvement exists to improve evidence-based management regarding counseling for diet and exercise and prescribing appropriate medications for hypertension. Primary Funding Source: CDC ●Risk of Emergency Department Visits for Asthma: Frequent Symptoms or Delay in Care Neetu Chawla, MPH, Ying-Ying Meng, DrPH, Susan Babey, Ph.D., E. Richard Brown, Ph.D., Elizabeth Malcolm, M.D. MSHS, Yee Wei Lim, M.D., Ph.D. Presented By: Neetu Chawla, MPH, Research Associate, UCLA Center for Health Policy Research, 10911 Weyburn Avenue, Suite 300, Los Angeles, CA 90024; Tel: (310)7948362; Fax: (310)764-2686; Email: nchawla@ucla.edu Research Objective: To identify modifiable factors related to Emergency Department visits for asthma among a diverse non-elderly adult population in California. Study Design: This study used data from the 2001 California Health Interview Survey (CHIS). CHIS 2001 is a random-digit dial (RDD) telephone survey of 55,428 households drawn from every county in California and is the largest statewide health survey conducted in the United States. The sample was designed to provide estimates for California's overall population, its major racial and ethnic groups, and a number of ethnic subgroups. Logistic regression analyses were used to determine factors associated with emergency department (ED) visits for asthma. Factors studied include age, gender, race/ethnicity, education, English proficiency, insurance coverage, having a usual source of care, reasons for delaying asthma-related care, self-reported health status, frequency of asthma symptoms, rural/urban residence, and smoking status. Our analysis employs a framework based on the Anderson model of health care utilization. Population Studied: The population studied was 4,359 California adults, ages 18 to 64, who reported that they had been diagnosed with asthma and experienced asthma symptoms in the past year. Principal Findings: Overall 9.4% of adults with asthma reported visiting the ED due to asthma in the past year. We found that those with daily or weekly symptoms, with fair or poor health status, and who delayed care for asthma due to cost/insurance or other reasons were more likely to visit the ED for asthma. Stratification of the study population into those with daily/weekly symptoms and those with less frequent symptoms revealed that delay in care due to cost and health insurance coverage, delay in care for other reasons, and fair/poor health status remained significant for both groups. In addition, Latinos and women were more likely to visit the ED in the severe asthma group while Asians, African Americans, and the uninsured were more likely to visit the ED in the less severe group. Conclusions: To prevent ED visits for asthma, it is important to control asthma symptoms and reduce delays in receiving asthma care. In addition, racial and ethnic disparities exist in ED visits for asthma. Implications for Policy, Delivery, or Practice: ED utilization for asthma has been increasing, but our findings support the argument that this costly form of health care can be reduced. Two important factors, frequent asthma symptoms and delays in care for asthma, can be improved with effective interventions. Providers, patients and their family members could work in partnership to control asthma symptoms through more effective monitoring and medications. However, broader societal-level efforts are also needed, such as efforts to control asthma triggers (e.g., air pollution) and to improve health care coverage. Our findings also suggest that in addition to financial barriers, racial and ethnic minorities face other barriers to care, such as cultural or institutional barriers. Primary Funding Source: The California Endowment ●Sustainability of the Health Disparities Collaborative: Incentives, Assistance and Barriers Marshall Chin, M.D., MPH, Anne C. Kirchhoff, MPH, Jessica E. Graber, Ph.D., NORC-MWCNPresented By: Marshall Chin, M.D., MPH, Associate Professor, Department of Medicine, University of Chicago, 5841 South Maryland MC 2007, Chicago, IL 60637; Tel: (773)702-4769; Fax: (773)834-2238; Email: mchin@medicine.bsd.uchicago.edu Research Objective: Quality improvement (QI) collaboratives, typically using the Chronic Care Model (CCM), are increasingly used as a way to improve chronic illness care. In 1998, the Bureau of Primary Health Care (BPHC) started the Health Disparities Collaborative (HDC) to improve chronic disease management in community health centers (CHCs). Little is known, however, about the practical issues involved in sustaining QI programs over time and the help participants need for maintaining these programs. Therefore, we aimed to determine barriers to continued HDC success and to understand what incentives and assistance are needed to maintain improvements. Study Design: The first year of the HDC initiative includes learning sessions and conference calls where usually 10-20 teams at a time are trained in the CCM and rapid Plan-DoStudy-Act cycles to make changes focused on improving care. After the first year, CHCs concentrate on continuing and extending the improvements made in the initial year. In 2004, we conducted a mail survey of 1,519 administrators, providers, and staff from CHCs that had completed at least one year of the HDC by July 2003; 1,029 responded for a response rate of 68%. We report here on the initial 702 respondents. CHCs surveyed participated in the HDC on average approximately 3.5 years. Population Studied: We surveyed health center administrators, providers, and staff from 165 MidWest and West Central collaborative health centers. Of respondents, almost 20% were administrators (CEOs or Medical Directors), 66% were members of the QI teams, and 15% were other staff. Principal Findings: CHC administrators, providers and staff generally believe the HDC is successful (83%) and improves patient outcomes (88%) at their centers. However, CHC administrators note that the HDC leads to increased costs per patient (76%) and CHC costs (77%), but with no increased patient care reimbursement (79%) or grant acquisition (71%) to compensate for these costs. Respondents are somewhat concerned about burnout and inequitable workloads resulting from the HDC. Fifty-two percent of respondents believe that there is not sufficient funding or staff to run the HDC at their center. Also, they believe that sustaining the HDC would benefit from increased resources and assistance from BPHC and the CHC leadership for direct patient care, staff time for data entry and QI activities, and leadership support. Respondents deem personal incentives, such as receiving extra money for HDC work, somewhat less important than increases in system resources; however, 46% of participants who do not receive release time, indicate this is unacceptable. Conclusions: CHC personnel perceive the HDC to be worth the effort, but they also believe there are important financial and personnel barriers to maintaining improvements. Respondents indicate needing additional system support for patient care, data entry, QI, and leadership cooperation for sustaining the HDC. Implications for Policy, Delivery, or Practice: QI collaborative interventions, such as the HDC, are considered helpful by participants for improving care and patient outcomes; however, the sustainability of the HDC model and other QI collaborative programs may require increased resource support to maintain success over time. Primary Funding Source: AHRQ ●Productivity Enhancement for Primary Care Providers Using Care Management David Dorr, M.D., MS, Cherie P. Brunker, M.D., Adam Wilcox, Ph.D., Laurie Burns, PT, MS, Paul D. Clayton, Ph.D. Presented By: David Dorr, M.D., MS, Assistant Professor, Medical Informatics & Clinical Epidemiology, Oregon Health & Science University, 3181 SW Sam Jackson Park Road, Mailcode: BICC, Portland, OR 97219; Tel: (503) 494-4502; Fax: (503) 494-4551; Email: davedorr@gmail.com Research Objective: To determine the impact of a generalist care management system on the productivity of primary care providers. Study Design: A prospective cohort design was used to examine care management usage and productivity of primary care physicians (PCPs) over 24 months. Intermountain Health Care’s (IHC) generalist CM program consists of seven primary care clinics where specialized information system applications assist care managers and physicians in providing collaborative care for patients with one or more chronic illness or with psychosocial needs. Use of the system is voluntary and referrals are physician driven. Percent of patient visits who were care managed per physician per month was used to predict changes in work relative value units (wRVUs) generated over time. A mixed multivariable autocorrelation model was used to adjust for multiple levels of factors that might affect productivity, including time-based effects. Clinic level effects included clinic location (urban vs. rural), specialty mix, and team staffing levels. Patient panel effects included aspects of the patient population treated by the physician such as average case-mix as measured by the Chronic Disability Payment System (CDPS), average population age, percent married, and race. Physician factors examined included gender and age of physician, time in system, time since graduation, and specialty. Lag for time-based effects was determined with spatial autocorrelation. Continuous differences were tested with students' t and ANOVA, and model significance was tested with the likelihood ratio methods. Cost of the program was compared with revenue from productivity changes. Population Studied: 122 PCPs (53 internists; 69 family practitioners) within IHC over 24 months in 7 intervention and 23 control clinics. Principal Findings: The 122 primary care physicians saw 153,403 patients during 2,731 physician-months. In all, 4,898 (3.2%) patients were referred to CM. Unadjusted wRVUs were 377.9±104.3 for physicians with no/low CM use (67 control and 11 intervention physicians with <2% of visits with care managed patients) and 399.0±117.2 for those with higher care management use (44 physicians; >= 2% of visits), a 5% difference. Limiting the analysis to intervention physicians, low users had 332.5±144.9 wRVUs per month and higher users had 397.7±104.9 wRVUs (difference: 20%, p<.0001); this difference is strongest in physicians who adopted use during the study period. Specialty, average age (44.2), years in system (5.3), and gender (11% female) of physicians all influenced productivity at baseline and over time, as did percent of patient panel married (55.6%), Caucasian (93.2%), and average patient CDPS score (.79). Team staffing and clinic location also were significant predictors of productivity differences. After adjusting for these confounders, adjusted wRVUs were 318.00 ± 98.8 for low users and 398.8 ± 107.1 for high care management users. For physicians with access, adjusted wRVUs were 368.0±108.8 and 398.2±115.2 for low and high users (difference: 8%, p<.0001). Net cost of care managers from a physician only perspective was $11,643 per year. Conclusions: Productivity increases for physicians who made use of generalist care managers in our system were moderate but stable in a multivariable model. Net costs were reduced substantially in this limited perspective. Implications for Policy, Delivery, or Practice: Amount and accrual of benefits from CM programs have been hotly debated. When a generalist, information technology intensive program is used, provider productivity may increase and reduce net costs. However, assessment of productivity changes is challenging with many confounders. Primary Funding Source: John A. Hartford Foundation ●Drug Adherence and Physiologic Outcomes in Medicare Patients with Hypertension Vicki Fung, BA, Jie Huang, Ph.D, Richard Brand, Ph.D, Joseph Newhouse, Ph.D, Joseph Selby, M.D., MPH, John Hsu, M.D., MBA, MSCE Presented By: Vicki Fung, B.A, Analyst, Division of Research, Kaiser Permanente, 2000 Broadway, Oakland, CA 94612; Tel: (510)-891-3527; Fax: (510)-891-3606; Email: Vicki.Fung@kp.org Research Objective: The recent Medicare Modernization Act of 2003 (MMA) aims to help Medicare patients pay for chronic prescription drugs, such as blood pressure (BP) drugs. Clinical studies suggest that regular use of BP drugs decreases the risk of adverse cardiovascular events, but patients might have limited adherence to therapy. We examined levels of adherence to BP drugs, patient and insurance characteristics associated with lower adherence, and the association between adherence and physiologic outcomes in a Medicare population. Study Design: Using a large integrated delivery system’s (IDS) automated clinical databases, we determined adherence by calculating the proportion of days covered (PDC) by BP medications (i.e. angiotensin converting enzyme-inhibitors, angiotensin receptor blockers, beta blockers, calcium channel blockers, or diuretics) in 2003. We considered PDC = 0.8 as “adherent.” We used multiple logistic regression models to assess patient and insurance characteristics associated with lower adherence. We used logistic regression models to assess the association between adherence and elevated systolic blood pressure levels (SBP = 140mmHg) using the last measurement of the year in 2003. Population Studied: All subjects were members of the IDS who were 65+ years old with Medicare insurance, and had a diagnosis of hypertension and used a BP drug in 2002. The 85,099 subjects were an average age of 75.2 years old and were predominantly female (61.9%) and of white race/ethnicity (73.4%). In 2003, all subjects had at least some prescription drug coverage: 79.3% had a $1,000 annual drug benefit cap, and all subjects had a $10 generic and $20-35 brand drug copayment. 92.4% of subjects had at least one SBP measurement in 2003. Principal Findings: In 2003, 84.1% of subjects were adherent to any BP drug. In multivariate models, subjects with a benefit cap, who were male, had a higher comorbidity level, and were of non-white race/ethnicity were less likely to be adherent to BP drugs in 2003. Among all subjects, 37.9% had elevated SBP levels in 2003. After adjusting for covariates, adherence to BP medications was significantly associated with lower odds of elevated SBP levels (OR=0.87, 95% CI: 0.840.91). Conclusions: Over one in three Medicare patients in this sample had elevated systolic blood pressure levels. Moreover, many patients were not adherent to BP medications throughout the year. Adherence was associated with favorable clinical outcomes, as measured by non-elevated SBP levels. Implications for Policy, Delivery, or Practice: Despite the presence of relatively generous prescription drug coverage, many hypertensive Medicare patients in this study had elevated SBP and were not adherent to their drug regimen. Drug adherence was significantly associated with non-elevated blood pressure levels. These findings are particularly concerning given the clinical trial evidence indicating the value of lowering blood pressure for reducing adverse cardiovascular events. More research is needed to assess drug use, adherence, and clinical effects. Primary Funding Source: AHRQ ●Measuring the Quality of Follow-up Pharmacotherapy Management of Chronic Obstructive Pulmonary Disease (COPD) Exacerbations. Min Gayles Kim, MPH, Fernando Martinez, M.D., Russ Mardon, Ph.D., Phil Renner, MBA Presented By: Min Gayles Kim, MPH, Senior Health Care Analyst, Quality Measurement, National Committee for Quality Assurance, 2000 L Street NW Suite 500, Washington, DC 20036; Tel: (202)955-1731; Fax: (202)955-3599; Email: gayles@ncqa.org Research Objective: To explore the potential for a performance measure to assess the timely follow-up pharmacotherapy management of COPD exacerbations. Effective management of COPD exacerbations to shorten recovery and prevent relapse can have a large impact to reduce the economic and social burden and prevent worsening health status. Study Design: Observational study conducted in five health plans. Utilization of emergency department (ED) and inpatient services with a principal discharge diagnosis of COPD served as proxy for moderate to severe COPD exacerbations. Two indicators assessing the timely pharmacotherapy dispensing were measured: dispensing of systemic corticosteroids within 7 days and bronchodilator dispensing within 21 days of discharge from ED or inpatient visit. Pre-existing prescriptions for steroids and bronchodilators were included. Population Studied: Five health plans participated in the study and were asked to provide patient data and claims data (e.g. spirometry testing) from administrative data systems for the entire eligible population. In addition, each plan was asked to review medical records for a sample of 150 patients in the eligible population. The enrollments of these plans included commercial, Medicare, and Medicaid product lines across several geographical regions of the U.S., and ranged in size from 52,000 to over 820,000 members. Principal Findings: Plan-specific frequency of patients with an exacerbation ranged from 0.27 per 1000 to 1.35 per 1000 commercial plan members (avg: 0.65), and ranged from 7.56 per 1000 to 20.21 per 1000 Medicare members. Overall, 43% of plan enrollees who were discharged home from an ED or hospital visit received systemic corticosteroids within 7 days, and 54% received a bronchodilator within 21 days. Planspecific rates ranged from 26% to 52% for steroid use and 29% to 55% for bronchodilator use. Steroid and bronchodilator use rates were notably lower in the Medicare population compared to commercial (36% vs. 47% steroid; 45% vs. 53% bronchodilator). There was no difference in usage rates between men and women. 87% of all steroid prescriptions were for prednisone, and 75% of bronchodilator prescriptions were for Albuterol. Conclusions: Despite guideline recommendations for shortterm use of systemic corticosteroids to reduce rate of relapse and improve symptom management in moderate to severe exacerbations, this study shows considerable room for improvement. Similarly, bronchodilator therapy, which is a key COPD therapy because of its capacity to alleviate symptoms, decrease exacerbations, and improve health status, was underutilized. Steroid and bronchodilator use was much lower in the Medicare population reflecting possible disparity of care in the older population. Implications for Policy, Delivery, or Practice: Performance measures for appropriate follow-up pharmacotherapy of COPD exacerbations can be an important method for encouraging physicians to manage COPD effectively thereby decreasing the frequency of exacerbations by reducing the rate of relapse and improving symptom management. Primary Funding Source: Supported in part by educational grant from Boehringer-Ingelheim & Pfizer ●Robustness of Diabetes Self-Management Russell E. Glasgow, Ph.D., Lisa A. Strycker, MA, Diane K. King, MS, OTR, Deborah J. Toobert, Ph.D., Alanna Kulchak Rahm, MS, Marleah Jex, MPH Presented By: Russell E. Glasgow, Ph.D., Senior Scientist, Clinical Research Unit, Kaiser Permanente Colorado, 335 Road Runner Lane, Penrose, CO 81240; Tel: (719) 372-3165; Fax: (719) 372-6395; Email: russg@ris.net Research Objective: To evaluate the "robustness" or generalization of effects from a computer-assisted diabetes self-management program on reach, implementation, and efficacy attributable to a variety of factors below. Study Design: RCT with stringent attention control condition. Analyses were conducted of interaction or moderator effects due to health plan, counselor, and variety of patient characteristics. Population Studied: 217 adult type 2 primary care diabetes patients from both fee-for-service and HMO healthcare settings. Principal Findings: 41% patient participation, variable adoption by physicians (76% HMO vs 18% non-HMO), excellent implementation, and improvements in both dietary and physical activity outcomes. Few significant interactions between treatment condition and patient characteristics, type of healthcare plan, or counselor experience. Conclusions: Patients and (HMO) physicians were willing to participate in this self-management intervention. Interventionists from a variety of backgrounds delivered the program successfully, and the results appear robust across a variety of patient and delivery characteristics. Implications for Policy, Delivery, or Practice: This intervention applies generalizable across a variety of factors related to public health and potential moderator variables. More such research is needed to inform practice and policy concerning the conditions under which chronic care programs are and are not effective. Primary Funding Source: NIDDK ●Patient Assessment of Chronic Illness Care: Application in Diabetes Sample Russell E. Glasgow, Ph.D., Candace C. Nelson, MA, Holly Whitesides, BS, Diane K. King, MS, OTR, Barbara L. McCray Presented By: Russell E. Glasgow, Ph.D., Senior Scientist, Clinical Research Unit, Kaiser Permanente Colorado, 335 Road Runner Lane, Penrose, CO 81240; Tel: (719)372-3165; Fax: (719)372-6395; Email: russg@ris.net Research Objective: To evaluate the characteristics and usefulness of the Patient Assessment of Chronic Illness Care (PACIC) survey among a sample of 355 type 2 diabetes patients participating in a care improvement project. The PACIC is designed to assess patient reports of the extent to which they received care congruent with the Chronic Care Model and can also be scored to produce subscales reflecting the 5 As of behavioral counseling. Study Design: Patient survey administration. Analyses of the relationship of the PACIC to HEDIS-like measures of quality of care received, measures of physical activity and eating behaviors, and to a variety of patient characteristics. Population Studied: 355 adult type 2 primary care patients of 52 physicians throughout Colorado. Respondent characteristics generally matched those from BRFSS data from Colorado for diabetes patients(e.g., 47% female, average age = 63, 42% had family incomes < $30,000. Principal Findings: 1. These results generally replicated those of an initial validation study on the PACIC, but with a much larger diabetes sample. 2. The category of Chronic Care Model congruent care reported most often was patient activation activities. PACIC subscale activities reported to occur least frequently were related to follow-up and coordination of care. 3. The new 5 As scoring for receipt of behavioral counseling found that Agree activities were reported most often and Arranging follow-up and community resources the least often. 4. The PACIC summary scores were significantly related to both patient physical activity levels (r = .16, p <. 01) and to receipt of HEDIS- related quality of diabetes care (r = .21-.27, p <. 001). In contrast, and encouraging, very few patient characteristics were significantly related to any of the PACIC scale scores. Conclusions: The PACIC appears to be a useful patient report instrument that produces adequate variability and relates to some patient outcomes such as level of physical activity and quality of diabetes care received. The new items and 5 As scoring for receipt of behavioral counseling also appears to be useful. Implications for Policy, Delivery, or Practice: The PACIC scale offers promise as a practical way to assess patient perceptions of receipt of primary care reflective of both Chronic Care Model and USPSTF 5 As behavior change counseling activities. It is recoimmended for use in intervention studies to assess its sensitivity to change and to evaluate quality improvement innovations. Primary Funding Source: AHRQ ●Secondary Prevention Lipid Clinic: A Multidisciplinary Approach Anthony Greisinger, Ph.D., Ali Mortazavi, M.D., Kim Birtcher, Ph.D., Haroonur Rashid, M.D., Madjid Tehrane, M.D., Oscar Wehmanen, MS Presented By: Anthony Greisinger, Ph.D., Vice President for Research and Development, Kelsey Research Foundation, 7800 Fannin Street, Suite 209, Houston, TX 77054; Tel: (713) 442-1214; Fax: (713) 442-1229; Email: ajgreisinger@kelseyseybold.com Research Objective: Numerous studies have demonstrated that lipid clinics have outperformed usual care models in improving patient outcomes related to achieving LDL goals, increasing compliance with medication regimens, and reducing costs. We developed and evaluated the impact of a secondary prevention lipid clinic (SPLC) in improving treatment outcomes (total cholesterol <200, HDL >40, LDL <100, and triglycerides <150) for patients with a history of cardiovascular and cerebrovascular disease (CV disease). Study Design: Our multidisciplinary team approach includes cardiologists, a pharmacist, nurses, and a registered dietician. This approach uses a protocol based on the National Cholesterol Education Project (NCEP) guidelines that provides individualized patient and family education to promote appropriate lifestyle changes (e.g., cholesterol reduction, diet/weight management, exercise, medications, and tobacco cessation). Patients with a history of CV disease from a large multi-specialty medical organization were referred by a physician or through self-referral to the SPLC and followed prospectively. At the initial clinic visit, a pharmacist obtained patients’ histories and baseline measures of height, weight, dietary and exercise habits, and tobacco use. Customized verbal and written instructions about diet, exercise, tobacco cessation, and medications were provided to each patient. Cholesterol goals were discussed and patients’ commitments to making the recommended lifestyle changes were obtained. A cardiologist reviewed all treatment plans before discussions with the patient. At subsequent clinic visits, weight changes and compliance with exercise, medication, and tobacco cessation commitments were reviewed, revised as necessary, and discussed with patients. Patients’ progress was monitored at all subsequent clinic visits and clinical data were entered in a database specifically designed for the SPLC. Population Studied: Patients with a history of CV disease were identified and treated at a large multi-specialty medical organization. The organization has 21 clinics and more than 300 physicians serving the greater Houston, Texas metropolitan area. Principal Findings: Since the inception of the SPLC in October 2001, 1,286 patients have been enrolled, with 28% of these patients enrolled for 2 or more years. Data analyses (October 2001 through December 2004) show significant improvement in patient attainment of NCEP-recommended goals for cholesterol management. Baseline data collected at the initiation of the SPLC showed that 65.6% of patients had total cholesterol <200mg/dl, 50% had LDL <100mg/dl, 56.9% with HDL >40mg/dl, and 45.9% with triglycerides <150mg/dl. In December 2004, 88% of enrolled patients achieved total cholesterol of <200mg/dl, 71% were at goal for LDL <100mg/dl, 79.5% were at goal for HDL >40mg/dl, and 65.9% were at goal for triglycerides <150mg/dl. Conclusions: Multidisciplinary lipid clinics can assist patients in attaining NCEP-recommended goals for cholesterol management and address modifiable risk factors to prevent future cardiovascular events. Implications for Policy, Delivery, or Practice: These findings provide additional support for the effectiveness of multidisciplinary lipid clinics in improving patient outcomes and the quality of care. Future studies are needed to examine adherence to lipid clinics over time, the cost-effectiveness of these programs, and whether lipid clinics reduce the risk of future CV events. Primary Funding Source: Kelsey Research Foundation ●The Costs of Implementing the Health Disparities Collobarative to Improve Diabetes Care: a Community Health Center Perspective Elbert Huang, M.D., MPH, Sydney E.S. Brown, AB, James X. Zhang, Ph.D., NORC Presented By: Elbert Huang, M.D., MPH, Assistant Professor of Medicine, Section of General Internal Medicine, University of Chicago, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637; Tel: (773) 834-9143; Fax: (773) 834-2238; Email: ehuang@medicine.bsd.uchicago.edu Research Objective: The Health Disparities Collaboratives (HDC) is a national effort sponsored by the Bureau of Primary Health Care (BPHC) to improve the quality of chronic illness care in federally-qualified community health centers (CHCs). The HDC includes training of CHC teams in implementing the Chronic Care Model and techniques of rapid quality improvement (QI). Teams then use these new skills to develop QI projects. The HDC has been found to improve diabetes care. As the HDC is disseminated, it is crucial to understand the resources that are required to implement such a program. We evaluate the costs of implementing the Diabetes HDC program over time. Study Design: We adopted a case study approach. Data sources included: 1) a survey of center leadership in order to obtain details regarding the time commitment of providers and non-providers for HDC activities such as data collection, data entry, team meetings, and conferences; 2) comprehensive billing data for one center to calculate the value of provider time; 3) and annual Uniform Data System reports for descriptions of center clinical activity (i.e. unique patients seen). We used these data to estimate our main outcomes of interest: 1) the time commitment of providers and non-providers to Diabetes HDC activities (HDC hours per week, % provider time) and 2) the costs of implementing the Diabetes HDC (Program costs in $/unique patient seen/year) over time. Population Studied: Four Midwestern CHCs with consistent computerized financial records and involvement in the Diabetes HDC for at least 3 years. Principal Findings: The CHCs included two from Ohio (Ohio 1 and Ohio 2), one from Indiana, and one from Missouri. The number of unique patients seen annually per CHC ranged from 5729 to 28,451 in year one. All centers had growth in the number of patients seen. For Ohio 1 and the Indiana center, total HDC hours declined over time (Ohio 1: 24.8 hours/week to 18.6 over 5 years; Indiana: 48.9 hours/week to 23.3 over 4 years). Similarly, the costs of the HDC declined (Ohio 1: $3.57/patient/year to $2.22; Indiana: $10.52/patient/year to $2.43). In contrast, hours devoted to the HDC increased for Ohio 2 and the Missouri center. HDC costs declined for Ohio 2 ($15.40/patient/year to $11.15) but costs remained higher than any other center. HDC costs for the Missouri center rose ($2.88/patient/year to $4.51). The initial percentage of HDC time from providers varied by center, but generally declined. Conclusions: The CHCs developed distinctive strategies for implementing the Diabetes HDC that led to varied program costs. The overall time commitment and the percentage of time devoted by providers were important determinants of program costs. The costs of the HDC per patient declined for 3 out of 4 centers. Implications for Policy, Delivery, or Practice: This study provides the BPHC and CHCs with estimates of the initial and follow-up costs of implementing the Diabetes HDC. Further study to identify the most cost-effective approaches to implementing the HDC at the center level may help guide future funding mechanisms of federal QI programs. Primary Funding Source: AHRQ ●Identifying Medicare-Enrolled Veterans with Multiple Chronic Conditions – Using Medicare, or VA or Both? Michael Johnson, Ph.D., Margaret Byrne, Ph.D., Jennifer Hasche, MS, Nora Osemene, PharmD, Laura Petersen, M.D., MPH, Raji Sundaravaradan, BS, Iris Wei, DrPH, Robert Morgan, Ph.D. Presented By: Michael Johnson, Ph.D., Assistant Professor of Medicine, Houston Center for Quality of Care and Utilization Studies, Baylor College of Medicine, 2002 Holcombe Boulevard, Houston, TX 77030; Tel: (713)794-8608; Fax: (713)748-7359; Email: mjohnson@bcm.tmc.edu Research Objective: As the U.S. population ages and healthcare costs continue to escalate, there is increasing emphasis on studying elderly individuals with multiple chronic conditions. Elderly veterans are a unique population with dual eligibility for care from the VA and Medicare systems. Co-use of VA and Medicare services has implications for both quality and costs of care. Our objective was to identify Medicareenrolled veterans with multiple chronic diseases from both systems of care. We chose to identify enrollees with diabetes mellitus (DM), ischemic heart disease (IHD), or chronic heart failure (CHF), as these are prevalent, comorbid chronic conditions with a large burden of healthcare use and cost. Study Design: A retrospective cohort study. Population Studied: VA utilization records and Medicare claims records for over 5 million unique veterans enrolled in Medicare fee-for-service plans were separately searched for at least one occurrence of ICD-9-CM diagnosis codes indicating any of the 3 conditions for calendar years 1999-2002. Principal Findings: A total of 3,226,922 enrollees (63.4%) were identified as having at least one of these conditions. Of these individuals, 52.7% had DM, 74.8% had IHD and 39.4% had CHF. Among the DM group, 57.0% were identified in VA records, 74.9% were identified in Medicare claims, and 42.5% were found in both sources of records. Similarly, among the IHD group 54.3% were in VA, 74.7% in Medicare, and 38.8% were in both; among CHF, these percentages were 37.9%, 79.2% and 21.6% respectively. Of the DM patients identified in Medicare only (n=731,676 or 43% of all DM), 13.3% (n=97,415) were also found in either CHF or IHD cohorts identified in the VA. In other words, over 97,000 patients were found to have DM in Medicare records, but not in the VA, where they were found to have CHF or IHD. Eleven percent of IHD patients identified in Medicare only were in a non-IHD VA cohort, and 32.1% of CHF patients identified in Medicare were in a non-CHF VA cohort. Conclusions: The prevalence of these chronic diseases in isolation or in combination differs depending on which healthcare system is searched. These findings suggest that coding differences alone do not explain the variation in identification of these conditions. Substantial numbers of patients with a given chronic disease may not seek treatment in both healthcare systems for that condition, though they may receive other care in both systems. Thus, providers in the VA may be unaware their patients have certain conditions, or Medicare providers may be unaware their patients use the VA. If providers are aware, this information is not being captured in the administrative databases. Implications for Policy, Delivery, or Practice: Further research is needed to examine determinants in variation in coding or use patterns leading to differential ascertainment of disease conditions across the Medicare and VA systems. Researchers should use caution in determining disease cohorts based on either system alone. Primary Funding Source: VA ●Characteristics and Predictors of Multiple Complicated Transitions Thirty Days after Hospitalization for Acute Stroke Amy Kind, M.D., Maureen Smith, M.D., MPH, Ph.D., Jennifer Frytak, Ph.D., Michael Finch, Ph.D. Presented By: Amy Kind, M.D., Geriatric Fellow, Geriatrics, Univeristy of Wisconsin and William S. Middleton VA Hospital - GRECC, 2500 Overlook Terrace, William S. Middleton VA Hospital - GRECC, Madison, WI 53705; Tel: (608)280-7000; Fax: (608)280-7291; Email: ajh.kind@hosp.wisc.edu Research Objective: In our current system of compartmentalized healthcare, patients with complex health conditions like acute stroke often require care across multiple settings with numerous care transitions. Some of these patients will undergo “complicated” transitions, i.e. transitions from lower to higher care levels such as from home to the hospital. Patients who undergo multiple complicated transitions within a short time period indicate a potential failure of the health care system and represent a potential target for improved quality of care. The objective of this analysis is to define the characteristics and predictors of patients with multiple complicated transitions in the thirty days after hospitalization for acute stroke. Study Design: This study utilized Medicare claims and enrollment data from 11 regions in the United States. “Complicated transition” was defined as movement from a less intense to a more intense care setting (i.e., lower to higher level of care) with hospital being the highest on the care spectrum, then emergency room (ER), skilled nursing facility (SNF)/rehabilitation center/nursing home, home with home health care, and home without home health care (the lowest). Multivariable logistic regression was used to analyze the relationship between multiple complicated transitions and explanatory variables including socio-demographics, comorbidities, stroke severity, and HMO membership. Population Studied: Medicare beneficiaries aged 65 years and older discharged with acute ischemic stroke during 19982000, including 4,816 Medicare health maintenance organizations (HMO) patients from 422 hospitals and 39,283 Medicare fee-for-service (FFS) patients from the same hospitals. This analysis was restricted to 8,100 patients who had at least one complicated transition. Principal Findings: Among stroke patients with complicated transitions over the initial thirty days after hospital discharge, 84% experienced only one complicated transition while 16% (n = 1,266) experienced more than one complicated transition (1,087 patients experienced two complicated transitions, 156 experienced three, and 23 experienced four or more). The majority of complicated transitions (93%) involved ER visits or hospital readmissions. When compared to those with a single complicated transition, patients with multiple complicated transitions (>1) were more apt to be African American (Odds Ratio (OR) = 1.44, 95% Confidence Interval (CI) = 1.18-1.76), have a history of fluid or electrolyte disorder such as dehydration in the year prior to or during the index hospitalization (OR = 1.28, 95% CI = 1.12-1.47) and experience residual neurological deficits on discharge (OR = 1.27, 95% CI = 1.08-1.50). Conclusions: A significant number of stroke patients experience multiple complicated transitions thirty days after index hospitalization. This population could be distinguished from patients undergoing a single complicated transition by several socio-demographic and clinical factors available at the time of hospital discharge. Implications for Policy, Delivery, or Practice: The distinguishing factors in this population are remarkable for their potential to be influenced by socioeconomic and environmental pressures. This may point to a potential breakdown in our post-stroke system of health care for vulnerable populations. Further investigation should focus on the role that socioeconomic and environmental factors play in patients with multiple complicated transitions. Primary Funding Source: NIA ●Improving Primary Prevention for People with Chronic Disabling Conditions: Focus Group and Internet Poll Findings Thilo Kroll, Ph.D., Melinda T. Neri, BA, Gwyn C. Jones, Ph.D., Matthew E. Kehn, BA, Sally Michaels, BA, Marcie Goldstein, MA Presented By: Thilo Kroll, Ph.D., Senior Research Associate, Research Division, NRH Center for Health and Disability Research, 102 Irving Street, NW, Washington, DC 20010; Tel: (202) 877-1031; Email: thilo.kroll@medstar.net Research Objective: There is increasing evidence that people with chronic disabling conditions are less likely to receive primary preventive care services recommended by the U.S. Preventive Service Task Force than the general population. They are also at greater risks for an earlier onset of secondary conditions such as cardiovascular disease. This study’s objective was to determine the experiences of people with chronic disabling conditions with accessing and utilizing primary preventive services. Further, we sought community input for the development of strategies that could enhance access to these services. Study Design: The study combines in-depth focus groups with a national consumer poll. We conducted five focus groups with 36 adults (20 male, 16 female; Mdn ‘age’=46 years) with various chronic disabling conditions. Interview questions focused on experiences with primary preventive services, barriers to receiving timely and correct services, strategies to improve the service experience, and to address unmet information needs among health care professionals and consumers. We further conducted an Internet poll between August and November 2004 with n=518 (335 female; 183 male) adults from diverse racial/ethnic backgrounds with various self-reported conditions (e.g. spinal cord injury, cerebral palsy, post-polio, arthritis, diabetes) from 47 U.S. states and the District of Columbia. The research team worked with independent living specialists throughout the study. Population Studied: People with chronic disabling conditions. The largest subgroups were people with spinal cord injury, multiple sclerosis, cerebral palsy and stroke. Principal Findings: Focus group respondents reported several environmental, provider-side and personal barriers compromising primary preventive service access and utilization. Primary barriers include inaccessible provider facilities, equipment and procedures; insufficient support during appointments, lack of provider knowledge about the need for primary prevention, inappropriate professional behavior towards individuals with communication and mobility impairments, lack of reliable transportation to and from providers, and personal motivation to seek preventive care services. Suggested strategies involved careful planning for physician appointments, improved scheduling techniques, disability awareness education for primary care providers, and advice on practical assistance needs during appointments. Results from the Internet poll show that one-third (34.7%) reported negative experiences in the receipt or primary preventive services; while nearly three quarter (71.2%) of the respondents said they believed they are receiving correct services. There were no significant differences with regard to age, gender, race/ethnicity. The only significant difference was found for race/ethnicity with regard to perceived correct services. Significant more Non-Caucasian participants reported that they did not receive correct services. One-third of all respondents said that they had not received a routine physical exam, about half said they had not had a diabetes or cholesterol test. Only 42% of the men over age 51 had received a prostate exam; while only around half of the female respondents over age 51 had received a mammogram, pap smear or breast exam. Conclusions: Adults with chronic disabling conditions face multiple environmental and personal barriers in their access to primary preventive services. Based on our findings we will develop information resources for disabled consumers and health care professionals. Implications for Policy, Delivery, or Practice: Primary care providers need to become more knowledgeable about access barriers and adapt clinical practice to better address the primary prevention needs of people with chronic disabling conditions. Primary Funding Source: CDC ●Evaluating Best Practice Patterns Using Commercial Insurance Claims Data Sylvia Kuo, Ph.D, Susan Miller, MBA, Ph.D, Jim Burrill, M.D. Presented By: Sylvia Kuo, Ph.D, Investigator, Center for Gerontology and Health Care Research, Brown University, Box G-STZ, Providence, RI 02912; Tel: (401) 863-2060; Fax: (401) 863-9219; Email: Sylvia_Kuo@brown.edu Research Objective: With the decline of managed care, insurers are increasingly interested in promulgating evidencebased practices to improve the quality of care and reduce unnecessary health care utilization among their beneficiaries. Blue Cross & Blue Shield of Rhode Island (BCBSRI) covers approximately 80 percent of the commercial market in the state of Rhode Island. Through an analysis of BCBSRI’s claims data, our objective was to examine deviations from acute coronary symptom (ACS) best practices by describing the extent to which recommended coronary procedures were performed as well as by documenting the rate of duplicate procedures. (word count = 487) Study Design: Using BCBSRI claims data, rates of coronary procedures performed within 4 weeks from the initial onset of coronary symptoms as well as the rate of duplicate procedures were calculated among a cohort of all commercially insured adults. Procedures examined included coronary artery bypass grafts (CABGs), angioplasties (PTCAs), cardiac catheterizations and angiographies, stress echocardiograms, nuclear stress tests, stress EKGs, and echocardiograms. ICD9, CPT and HCPCS codes identified ACS diagnoses and associated coronary procedures. Procedure rates were also stratified by patient and provider characteristics. Population Studied: The population was a cohort of all adults enrolled in BCBSRI commercial products who experienced coronary symptoms for the first time between July 1 and December 31, 2003. A first-time experience was defined as not having had a previous claim associated with coronary symptoms or treatment procedures in the year preceding the study period; individuals also had to be continuously enrolled at BCBSRI for this period. During the last half of 2003, a total of 1,570 subscribers experienced initial coronary symptoms. Principal Findings: There was some duplication for the noninvasive diagnostic stress tests (about 5 percent of 720 who had initial test), and none for CABGs and PTCAs. However, 12 percent (2 of 17) of adults who had an angioplasty in the 4 week period had initially received a cardiac catheterization at a hospital without revascularization capabilities, while 40 percent (2 of 5) receiving a CABG had also undergone a prior catheterization. The majority of duplication in the stress tests occurred within the first 7 days of the initial test; duplicate tests were performed by the same physicians and concentrated among a small number of physicians. Conclusions: Although little duplication of coronary procedures is evident among BCBSRI enrollees, there may be unnecessary use of invasive services, particularly in receiving cardiac catheterization at one location but treatment at another. The concentration of duplicate stress tests among a few physicians illustrates variations in physician practice patterns, which suggest deviations from best practices. However, these findings should be confirmed using a larger cohort of BCBSRI enrollees. Implications for Policy, Delivery, or Practice: Inefficiencies due to the duplication of invasive procedures may not be problematic for insurers although further research should be conducted. However, the concentration of duplicate stress testing among a few physicians may suggest the practice of defensive medicine and variations in physician practice patterns rather than problems with poor initial test quality or inadequate information sharing across providers. Primary Funding Source: Blue Cross & Blue Shield of Rhode Island ●Achieving NCEP Goals in Patients with Diabetes: Results from the VDIS Trial Charles MacLean, MDCM, Amanda Kennedy, PharmD, Benjamin Littenberg, M.D., Richard G Pinckney, M.D., MPH, Phillip Ades, M.D. Presented By: Charles MacLean, MDCM, Associate Professor, Primary Care Internal Medicine, University of Vermont College of Medicine, 371 Pearl Street, Burlington, VT 05401; Tel: (802)847-8268; Fax: (802)847-0319; Email: charles.maclean@vtmednet.org Research Objective: Cholesterol management is essential in the preventive care of patients with diabetes. Recently, the National Cholesterol Education Program (NCEP) released a report providing updated treatment recommendations. It includes an optional LDL goal of <70 mg/dL for patients who are at very high risk for coronary heart disease (CHD). It is unknown how feasible this may be for very high risk patients with diabetes. Our goal is to assess the feasibility of attaining both the standard and the new optional LDL goals using currently available medications. Study Design: We performed a cross sectional analysis of laboratory data from the Vermont Diabetes Information System (VDIS), a large randomized trial of a decision support system for patients with diabetes. Medication lists were obtained by direct observation during a home interview. Patients were categorized into high and very high risk CHD status, based on NCEP criteria. For patients not at LDL goal we estimated the changes in therapy necessary to achieve goals, based on best evidence regarding medication effectiveness from the literature. We used optimistic assumptions regarding adherence and tolerability of medications. Population Studied: Adults with diabetes enrolled in the Vermont Diabetes Information System (VDIS),under care by a primary care provider in 47 practices in Vermont and northern New York (N=650). Principal Findings: The median age of the subjects was 66 years (range 25-93), the median duration of diabetes was 7.4 years (SD 10.1), and the mean A1C 7.1% (SD 1.3). Of the entire cohort, 49.4% (321/650) had an LDL < 100 mg/dL. 29.4% (191/650) of patients were at very high risk for CHD and, according to the NCEP, have an optional LDL goal of < 70 mg/dL. Only 15.7% (30/191) of very high risk patients had an LDL < 70 mg/dL. Of high risk patients, 17/459 (3.7%) would require more than two lipid-lowering drugs to achieve an LDL < 100 mg/dL. In the very high risk group, we estimate one quarter (50/191; 26.2%) of patients would require at least three drugs to reach an LDL < 70mg/dL. Conclusions: In many patients with diabetes at very high CHD risk, it will be difficult to attain an LDL goal of < 70 mg/dL. Approximately one quarter of patients will require more than two lipid lowering drugs at maximal doses to attain this goal, even assuming 100% tolerability of and adherence to lipid therapy. Implications for Policy, Delivery, or Practice: Given that three-drug lipid lowering therapy has not been tested in clinical trials, the latest recommendations from the NCEP regarding lipid lowering therapy for patients with diabetes may be overly aggressive. Primary Funding Source: National Institute of Diabetes, Digestive and Kidney Diseases ●Evaluation of an Interactive Voice Recognition (IVR) Disease Management Intervention on Outcomes of Care for Adults with Persistent Asthma David Mosen, Ph.D., MPH, William Vollmer, Ph.D., Elizabeth O'Connor, MS, Dawn Peters, Ph.D., Michael Kirshner, DDS, MPH, Sonia Buist, M.D. Presented By: David Mosen, Ph.D., MPH, Program Evaluation Consultant, Care Management Institute, Kaiser Permanente, 500 NE Multnomah, Suite 240, Portland, OR 97236; Tel: (503)813-3827; Fax: (503)813-2428; Email: david.mosen@kp.org Research Objective: Interactive Voice Recognition (IVR) technologies offer a cost-effective method to deliver automated, low intensity outreach for persistent asthmatics. This technology can be used to not only provide useful asthma health education, but can alert health providers when a patient’s asthma is poorly controlled. Despite these apparent benefits, little research has evaluated the impact of such interventions on outcomes of care. The primary objective of this study is to evaluate the impact of an IVR Disease Management Intervention on medication use, asthma-related hospital and emergency department (ED) utilization, asthma control, quality of life assessment (QOL), and satisfaction with care. Study Design: Using an intent-to-treat study design, we randomized 6948 adults with persistent asthma to receive usual care (UC, n = 3367) or an asthma outreach program (AOP, n = 3581). The AOP consisted of 3 calls spaced evenly over 11 months. Computerized calls were made using IVR technology. Each call lasted 5-10 minutes and asked about recent acute care, patterns of medication use, and current asthma control, followed by tailored feedback. Calls were documented in the medical record, and high risk patients were flagged for further follow-up. Random sample of the identified population completed surveys at baseline and follow-up to assess asthma control, QOL, and satisfaction with care. Electronic medical data were obtained for all and used to assess asthma related medication use and Hospital/ED utilization. Appropriate bivariate statistical tests (e.g. chisquare, t-tests) were used to assess differences in outcomes of care between the UC and AOP groups. Population Studied: Adults with asthma enrolled in large staff model HMO located in the Pacific Northwest. Principal Findings: A total of 47% of AOP participants completed >=1 call. Those responding were significantly likely to: be older and female, report worse QOL, and have used more inhaled corticosteriods during the baseline year. Overall, we found no significant (p < .05) differences at followup between UC and AOP for key study outcomes. However at follow-up, the subset of AOP patients who completed calls, compared to UC, use significantly more controller medications, and reported significantly better QOL on symptom and emotional scales and significantly greater satisfaction with their asthma care, and tended (p=.11) to report fewer asthma control problems. Conclusions: Although we did not find a difference in outcomes using the original intent-to-treat design, post hoc analysis of actual AOP users suggests a possible benefit in asthma-related health outcomes for the AOP intervention, among those respondents that completed 1 or more calls. Implications for Policy, Delivery, or Practice: Further research is needed to evaluate the effectiveness of IVR technologies as a medium to provide health education and modify behavior change among persistent asthmatics. Such research will provide needed information to health providers on how to best modify these strategies to improve their effectiveness. Primary Funding Source: CDC ●Localizing Cancer: Community-Based Approaches Toward Cancer Control in Georgia Christopher Parker, MBBS, MPH, Karen Minyard, Ph.D. Presented By: Christopher Parker, MBBS, MPH, Research Associate II, Georgia Health Policy Center, 14 Marietta Street, Atlanta, GA 30303; Tel: (404)463-9346; Fax: (404)651-3147; Email: chrisparker@gsu.edu Research Objective: A review and assessment of the progress of a regional statewide initiative designed to allow for greater cancer control at the local level. Study Design: Qualitative program metanalysis and case studies utilizing document review, interviews and focus group sessions. Population Studied: Participants in nine statewide regional coalitions (N~1500) Leadership representatives (N=36) Principal Findings: 1) There was unprecedented collaboration. The success in building these hitherto unachievable local coalitions strengthened the local health care sectors and paved the way for inter-regional synergism to be formalized. 2) The groups demonstrated significant overlap in regional thinking and program design. Many anticipated that the greatest return on investment would likely be seen from programs designed to address cancer prevention, early detection and the management of access to treatment. 3) Data acquisition was invaluable in the planning stages. Community specific information unearthed the depth of issues related to cancer control facing each region. This has resulted in a greater sense of a moral duty and ethical obligation to move toward implementation. 4) The regional programs perceived themselves to be the ideal vehicles by which ‘the science is taken to the people, and the people are taken to the science’. 5) Most regions have limited research capacity. The capacity for bench research is limited given the lower educational levels of rural Georgia and the relative paucity of tertiary academic institutions in many of the regions. 6) Business involvement is an untapped potential. To date most regions have reported only the polite involvement of the business community in their planning. Conclusions: In Georgia, cancer control has a real potential to catalyze and engage local community collaborations for the greater good of the state’s health care system. The collaborations will nonetheless need tangible state and business support to effectively implement these programs. Implications for Policy, Delivery, or Practice: No other state has previously attempted to “regionalize or localize” cancer care and control in this way. Georgia’s experiment may provide lessons for other interested states and policy makers may consider these local collaborations as yet another prong in the attack against cancer, that is a powerful adjunct to the more research-oriented, and academic Centers of Excellence. These local initiatives represent significant opportunities for public-private partnerships that may well realize the resources necessary to reduce the economic burden of cancer on local communities and eventually states. Primary Funding Source: Georgia Cancer Coalition ●Initial Non-Traumatic Lower Extremity Amputations Among Veterans with Diabetes Usha Sambamoorthi, Ph.D., Chin-lin Tseng, Dr.Ph., Mangala Rajan, MBA, Patricia Findley, Dr.Ph., Leonard Pogach, M.D., MBA Presented By: Usha Sambamoorthi, Ph.D., Health Scientist, Center for Healthcare Knowledge Management, Department Of Veterans Affairs, NJ Health Care System, 385 Tremont Avenue, East Orange, NJ 07018; Tel: (973) 676-1000 x1512; Fax: (973) 395 - 7111; Email: ushasambamoorthi@gmail.com Research Objective: Non-traumatic lower extremity amputations (LEA) occur at a markedly higher rate among persons with diabetes. The objective of the study was to identify initial (ILEA) and describe correlates of ILEA among veterans with diagnosed diabetes. Study Design: Secondary data analyses of merged Veteran Health Administration (VHA) and Medicare claims data for the fiscal years 1997 through 2000. ILEAs in FY 2000 were identified using a two-step algorithm. In the first step, amputations were identified using a comprehensive list of status post-amputation codes and lower limb prosthetic codes in addition to the actual procedure codes indicating amputations. In the second step we initiated a backward search of claims (look-back) to ensure that the observed amputation is indeed an ILEA. To measure the extent of leftcensoring bias due to varying length of look-back period, we estimated ILEAs by restricting the look-back period to 12, 18, 24 months and all years (between 3 and 10 years) of available prior data. Population Studied: Veterans using VHA facilities and diagnosed with diabetes during FY 1997-1998. There were 436,080 VHA patients with diabetes in FY 2000. Principal Findings: Overall, 2% (n = 9,617) had an LEA in FY 2000. ILEA estimates varied based on the look-back period and the use of post-amputation codes and lower limb prosthetic codes. ILEAs ranged from were from 4.6 per 1000 for the complete look-back period and 5.4 per 1000 for 12 months look-back period. Non-use of post-amputation and prosthetic codes increased these estimates to 8.4 per 1000 and 13.8 per 1000 respectively. Multiple logistic regressions revealed significant gender, race/ethnicity, age, foot-risk factors (such as peripheral vascular disease, and ulceration) and comorbid effects on the odds of having an ILEA. Veterans who used both Medicare and VHA systems were more likely to have an ILEA. However, this association was not consistent across different look-back periods. Conclusions: ILEA can be effectively identified using administrative data. Using status post-amputation codes and lower limb prosthetic codes in addition to actual procedure codes considerably reduces the estimate (~62%). However, the precision of ILEA estimates varied minimally as the lookback period increased. Implications for Policy, Delivery, or Practice: These findings highlight the usefulness of administrative data in identifying individuals with ILEAs. Accurate identification of ILEAs is critical to devise appropriate targeted interventions to reduce amputations among individuals with diabetes. Primary Funding Source: VA ●Practice Systems for Improving the Quality of Care for Chronically Ill Persons Sarah Scholle, Dr.PH., MPH, Greg Pawlson, M.D., MPH, Leif Solberg, M.D., Sarah Shih, MPH, Steve Asche, MA, Merry Jo Thoele, MPH Presented By: Sarah Scholle, Dr.PH., MPH, Assistant VP, Research and Analysis, NCQA, 2000 L Street, NW Suite 500, Washington, DC 20036; Tel: (202)955-1726; Fax: (202)9553599; Email: scholle@ncqa.org Research Objective: To perform feasibility, reliability, and validity testing on the Practice Systems Assessment Survey (PSAS), a self-report survey developed by the National Committee for Quality Assurance to measure the presence, scope, and function of organized systems in office practice. A widely cited reason for poor performance in ambulatory care is the finding that physician office systems and processes are not optimally designed to address the care of persons with chronic diseases or preventive needs. The goal of this instrument is to provide a relatively simple way to identify such systems for quality improvement, public accountability, and pay-for-performance. Study Design: The PSAS was developed with input from an expert panel and assesses key components of practice systems identified in the Chronic Care Model: continuity of care, clinical information systems, systematic monitoring, clinician reminders, performance tracking and feedback, quality improvement, care management, and patient education and support. After pretesting and subsequent refinements of items, a stratified sample of clinical personnel was surveyed. Trained nurse reviewers conducted on-site audits to verify the presence and use of the practice systems addressed in the survey. The surveys were compared to audit data in order to determine which staff position could provide the most accurate information about each section of the PSAS. Population Studied: Eleven medical groups in Minnesota, including primary and multi-specialty groups located in metropolitan and non-metropolitan areas. Principal Findings: A total of 328 surveys were completed by varying personnel in participating medical groups. Response rates by medical group ranged from 61% to 94% with a mean of 76%. Among the 11 groups, one had a fully integrated electronic medical record (EMR), three had EMRs with freestanding systems, six had paper records supplemented with electronic systems, and one had only paper-based records. Agreement between the audit and the survey responses on the functional capacity of the electronic systems varied by function and was highest for the most commone functions. For example, agreement was high (89.2% to 98.6%) regarding the ability of electronic systems to do scheduling, medication order entry, and alerts on drug-drug interactions. Agreement was lower for functions such as laboratory order entry and ability to search for patients based on diagnosis, with nurses having better agreement with the audit than physicians. Further analyses will assess interrater reliability and validity for the remaining PSAS domains. Conclusions: The degree of agreement on the capability of information systems varies by medical personnel and the type of system. Additional analyses and findings will report which respondents most accurately reflect local reality on other systems such as care management, quality improvement and performance monitoring. Implications for Policy, Delivery, or Practice: Information from this study will identify which medical personnel can most accurately report on the presence and function of practice systems relevant to quality care for patients with chronic conditions. The PSAS could help identify which systems should be targeted for improvement and potentially serve as a standardized metric for assessing and benchmarking office systems for public accountability and pay-for-performance efforts. Primary Funding Source: RWJF ●Internet-based, Personalized, Patient Activation Feedback to Improve Hypertension Guideline Adherence Does not Harm Patient Perceptions of Care Christopher Sciamanna, M.D., MPH, Edgar R. Miller, M.D., Ph.D, Michael Manocchia, Ph.D, Sarah Mui, B.S., Anthony N. Sciamanna, B.S., Christopher J. Pignatelli, B.S. Presented By: Christopher Sciamanna, M.D., MPH, Associate Professor, Health Policy, Jefferson Medical College, 1015 Walnut Street, Suite 115, Philadelphia, PA 19107; Tel: (215)9554376; Fax: (561)892-0511; Email: chris.sciamanna@jefferson.edu Research Objective: To improve blood pressure control rates, we developed a patient activation website to provide computer-tailored hypertension feedback. The website asks questions and provides feedback that highlights areas where their care adheres to guidelines and areas where their care does not, and encourages patients to ask questions during doctor visits that would lead to changes in their hypertension care. Study Design: The study was designed as a randomized controlled trial with a delayed treatment control, to measure the effect of using the website on a patients’ perception of the quality of their high blood pressure care. Population Studied: Subjects (121) with a history of hypertension and with access to the Internet were recruited to use the website and to answer questions about their health and health care before or after using the website. Principal Findings: The mean age of participants was 46.8 years and the mean duration of high blood pressure was 8.2 years. On average, participants received 8 corrective feedback paragraphs, which recommended a change to their care. Most participants rated the website as “excellent” or “very good”. Satisfaction with hypertension care was generally high, scoring a 3.8 out of 5. Subjects who answered the satisfaction with hypertension care questions before (59) and those who answered the questions after (62) using the website had similar responses with no significant differences in overall care or in any of the 4 dimensions of satisfaction with hypertension care or with their hypertension provider. Conclusions: Though our web-based, patient activation program identified gaps in the quality of hypertension care, the feedback did not adversely effect patient’s perceptions of the quality of their hypertension care. Implications for Policy, Delivery, or Practice: Concerns that providing physician-specific performance data to patients will harm the doctor-patient relationship may be overestimated. Primary Funding Source: NHLBI ●Effects of a Website Designed to Improve Patientprovider Interactions for the Management of Migraines. Christopher Sciamanna, M.D., MPH, Robert A.Nicholson, Ph.D., Jennifer H. Lofland, Ph.D., Michael Manocchia, Ph.D., Sarah Mui, BS, Christine W. Hartmann, Ph.D. Presented By: Christopher Sciamanna, M.D., MPH, Associate Professor, Health Policy, Jefferson Medical College, 1015 Walnut Street, Suite 115, Philadelphia, PA 19107; Tel: (215)9554376; Fax: (561)892-0511; Email: chris.sciamanna@jefferson.edu Research Objective: To improve migraine care, we developed a patient activation website to provide computer-tailored migraine feedback. The website asks questions and provides feedback that highlights areas where their care adheres to guidelines and areas where their care does not, and encourages patients to ask questions during doctor visits that would lead to changes in their migraine care. Study Design: This study was conducted to examine the effect of using the program on care that patients with migraine report receiving during a visit with their migraine care provider. Fifty-three migraine patients from a managed care organization were recruited and randomized to use the website before a doctor visit or to a delayed treatment control condition. Population Studied: Managed Care Organization patients with at least two visits coded for headache or migraine in the previous year. Principal Findings: Overall, the mean age was 42.0 years, most patients were female (86.5%), all were white, and 58.5% saw a headache specialist during their visit. Most (75.0%) reported having headaches at least once per week and 48.1% rated their headaches as “severe”. After the intervention, satisfaction with the visit was generally high (3.9 out of 5.0) and a mean of 5.0 topics were discussed during the visits. These differences were only significantly, however, for the report of discussing “whether you had migraine headaches or some other type of headache” (89.3% v. 54.5%; p < 0.01) and “whether or not there may be a more serious cause of your headaches” (50.0% v. 13.6%; p < 0.01). Among patients in the intervention condition, most (78.6%) printed the feedback from the website, though far fewer (28.6%) brought the feedback during their visit. Most (64.3%) reported asking questions that were suggested by the website. Conclusions: The patient activation website led to significant differences in migraine-related topics addressed during visits. Future studies are planned to understand the effects of the intervention on migraine-related outcomes. Implications for Policy, Delivery, or Practice: Patient activation interventions hold promise for improving the quality of care for chronic medical conditions. Primary Funding Source: NHLBI, NIAMS ●Reliance on VA/Medicare by Dually Eligible Veterans with Diabetes Yujing Shen, Ph.D., Mangala Rajan, MBA, Donald Miller, Sc.D., Steven Crystal, Ph.D., Leonard Pogach, M.D., MBA Presented By: Yujing Shen, Ph.D., Assistant Research Professor, Institute for Health, Health Care Policy and Aging Research, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732)932-8148; Fax: (732)932-6872; Email: yshen@ihhcpar.rutgers.edu Research Objective: Many older U.S. veterans are eligible for health care from both the Veterans Administration (VA) and from other providers with Medicare coverage. In order to better understand what influences choice for health services, we assessed reliance on VA and Medicare care by dually eligible veterans with diabetes and explored the factors associated with their reliance. Study Design: This is a cross-sectional analysis using data from the 1999 VA Diabetes Epidemiology Cohort (DEpiC) which includes VA and Medicare medical encounter files and the 1999 Large Health Survey of Veterans. We studied patients with Medicare fee for service in 1999. We identified those with inpatient care in VA only as VA reliant, those with inpatient care in Medicare only as Medicare reliant, and those with both VA and Medicare inpatient care as dual reliant. For those with outpatient but no inpatient, we grouped them into VA, Medicare and dual reliant also based on the source of their outpatient care. For multivariate analysis, we integrated both inpatient and outpatient groups together. Logistic regression was used to test the association between reliance on VA/Medicare (VA, dual, and Medicare reliant) and a number of factors including veterans' VA eligibility (priority) status, health status (by SF 36), travel distance to the closest VA and non-VA hospitals, and age, sex, race, education, and marital status. Population Studied: VA-Medicare dually eligible veterans with diabetes who had Medicare fee-for-service coverage in 1999 (N=90,193). Principal Findings: Overall, 13.9% used VA inpatient care only, 16.1% used Medicare inpatient only, 3.5% used both system for inpatient care, and 66.6% had no inpatient care (30.3% had VA outpatient only, 2% had Medicare outpatient only, 34.1% had outpatient care in both system). Those who were more likely to be VA reliant were: 50%+ service connected-disabled (VA priority 1) or catastrophically disabled (VA priority 4), younger age, smoker, non-white, less educated, unmarried, worse physical health status. Travel distance to VA or non-VA hospitals affected their use of care. For example, 10 extra miles of traveling to VA hospital decreased the chance of being VA reliant by 9% while 10 extra miles of traveling to non-VA hospitals decreased the chance of being Medicare reliant by 9%. Conclusions: Slightly more dually eligible VA patients with diabetes relied on Medicare for inpatient care, but the vast majority relied on either VA or both systems for outpatient care. Many factors in addition to access to traveling distance to care were associated with reliance on VA/Medicare care. Implications for Policy, Delivery, or Practice: Given that care is split between both systems in those with dual eligibility, strategies for care coordination across systems should be developed. Primary Funding Source: VA ●Barriers and Adaptations of Rural Diabetes Management Programs Anne Skinner, BS, RHIA, J. Patrick Hart, Ph.D., Roslyn Fraser, BA Presented By: Anne Skinner, BS, RHIA, Health Data Analyst, Preventive and Societal Medicine, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Tel: (402) 559-8221; Fax: (402) 559-7259; Email: askinner@unmc.edu Research Objective: To inform the development of appropriate policy and programmatic responses to the widespread need for diabetes care management in rural settings. This objective addresses the high proportion of diabetes cases combined with lack of resources that exists in rural areas. Study Design: An initial list of agencies, foundations, and associations involved in chronic disease management was compiled through discussions with key policy and practitioner informants. The list led to an internet search of websites and publications to identify, review, and describe rural chronic disease management initiatives throughout the United States. Next, we conducted interviews of representatives of diabetes programs at the national, state, and local levels across the five major diabetes initiatives in a geographically stratified sample of six states. We asked questions dealing with organizational and program characteristics, partnerships, barriers, effectiveness of the program, and considerations made for rural facilities. Interviews were transcribed and analyzed using NVivo software. Population Studied: National, state, and local level diabetes management programs across five major diabetes initiatives: CDC Diabetes Prevention and Control Programs, Health Disparities Collaboratives, Quality Improvement Organizations, Certified Rural Health Clinics, and the Office of Rural Health Policy Outreach and Network Programs. Principal Findings: At the time of this submission, interviews are complete and analysis is scheduled to be finished by February 1st. Preliminary findings indicate that several barriers to successful diabetes management programs are inherent in rural communities. Barriers include travel distances and isolation, low health literacy, cultural and linguistic diversity, lack of data registry management resources, time demands of collaborative activities, absence of locally controlled media, and challenges of integrated technology. Important adaptations that contribute to the success of diabetes management programs in rural areas include the development of formal and informal networks and collaborative efforts to overcome the isolation of the rural setting. Appropriate communications through the use of multicultural literature, media that cater to many literacy levels, and the hiring of bilingual and culturally competent staff have also shown to increase the effectiveness of programs as well as increase patient satisfaction. A systematic approach through the implementation of an electronic disease management system combined with data sharing also appears to improve process and outcome measures. Conclusions: In rural settings where high proportions of chronic disease exist in combination with few resources, additional basic support and locally appropriate adaptations create successful chronic disease programs. Implications for Policy, Delivery, or Practice: Our goal is to produce and disseminate findings on the policy implications of the relationship between current approaches to diabetes care management and their appropriateness, effectiveness, affordability and sustainability in rural service delivery settings. Primary Funding Source: Office of Rural Health Policy (ORHP) ●Nephrologists Care Reduced One-Year Mortality for Diabetic Patients with Chronic Kidney Diseases Chin-Lin Tseng, Dr.PH., Anjali Tiwari, M.D., MS, Elizabeth Kern, M.D., Donald Miller, Sc.D., Leonard Pogach, M.D., MBA Presented By: Chin-Lin Tseng, DrPH, Health Research Scientist; Assistant Professor, Center of Health Care Knowledge and Management, New Jersey Health Care systemEast Orange VA Medical Center; University of Medicine and Dentistry of New Jersey, 385 Tremont Avenue; #129, East Orange, NJ 07018; Tel: (973)676-1000 x2028; Fax: (973)3957114; Email: tseng@njneuromed.org Research Objective: There has been scant information available regarding the quality of care provided to patients with chronic kidney diseases in the US. Our objective was to evaluate the provision of nephrology specialist care among diabetic veterans with chronic kidney diseases (CKD) and its association with mortality when age, gender, race, medical and psychiatric comorbidities, and ACEI/ARB/statin usage are controlled for. Study Design: This study was a retrospective study. We used the 4 variable MDRD formula to determine eGFR (adjusted for age, sex, race, and creatinine levels). Multiple logistic regression was used to assess the impact of nephrologists care on one-year dialysis free mortality while controlling for age, gender, race, ACEI/ARB/statin medication, medical and psychiatric comorbidities. Population Studied: We used the Diabetes Epidemiology Cohort (DEPIC) dataset from our prior work to identify 561,088 veterans with diabetes in Fiscal year (FY) 1999 without a diagnosis of end stage renal disease or dialysis in FY 1997 or 1998 and were alive as of 9/30/1998. A total of 263,730 (64.73%) diabetic veterans could definitely be classified into one of the five stages according to K/DOQI criteria. Death outcome was obtained within 365 days from the initial eGFR during the study period. Further removal of 1,356 veterans who had dialysis prior to death during the follow-up resulted in 261,507 veterans. Principal Findings: The percentages of diabetic veterans by CKD stages were 21.5% (CKD 1), 47.5% (CKD 2), 28.7% (CKD 3), 2.2% (CKD 4), and 0.2% (CKD 5), respectively. The overall one year mortality rate in the study population was 3.6%. About 6.4% of the entire CKD population had at least one nephrologist visit after their initial eGFR during the study period. The percentages of nephrologist visit markedly increased at the more severe/later CKD stages: 1.1% (CKD 1), 1.9% (CKD 2), 13.5% (CKD 3), 54.8% (CKD 4), and 59.9% (CKD 5). Our multiple logistic regression models showed that older age, men, non-white racial groups, and more comorbidities were all significantly (p<0.001) associated with greater odds of death. Having nephrologist visits, on the other hand, reduced the odds of death, but only for patients in the later CKD stages. For patients in CKD stage 3, the odds ratio (OR) was 0.62 (95% confidence interval (CI)=(0.56, 0.69)). For patients in CKD stage 4 and 5 combined, the odds ratio was 0.39 (95% CI=(0.33, 0.47)). The results were similar when ACEI/ARB/statin usage was controlled for. Conclusions: A low percentage of diabetic veterans with CKD had any nephrologist visit after their initial eGFR. Nephrology specialist care was associated with reduced one year mortality among diabetic veterans with chronic kidney diseases, especially for patients in devastating CKD stages. Implications for Policy, Delivery, or Practice: Our data suggest compliance with roposed “quality of care measures” according to the K/DOQI and VA-DOD Guidelines needs to be improved for diabetic veterans with chronic kidney diseases. The health care systems need to make efforts in delivering nephrology specialist care to patients with chronic kidney diseases and patients are encouraged to seek such specialist care. Primary Funding Source: VA ●Decreased Mental Health Functioning is Associated with Increased Risk of Amputations Among Veterans with Diabetes Chin-Lin Tseng, Dr.PH., Mangala Rajan, MBA, Anjali Tiwari, M.D., Leonard Pogach, M.D., MBA Presented By: Chin-Lin Tseng, Dr.PH., Health Research Scientist; Assistant Professor, Center of Health Care Knowledge and Management, New Jersey Health Care System-EAst Orange VA Medical Center; University of Medicine and Dentistry of New Jersey, 385 Tremont Avenue, #129, East Orange, NJ 07018; Tel: (973)676-1000 x2028; Fax: (973)395-7114; Email: tseng@njneuromed.org Research Objective: Among individuals with diabetes, a lower extremity amputations (LEA) is often a catastrophic complication leading to poor quality of life, higher mortality rates, more hearth care costs. Whether adverse mental health is associated with increased risk of lower extremity amputations (LEAs) has not been well defined. Our objective was to evaluate the association between self reported mental health functioning upon risk of LEAs in veterans with diabetes using patient level administrative data as well as the 1999 Large Veterans Health Survey data (LVHS). Study Design: This study was a retrospective longitudinal cohort design. The outcomes were amputations in FY2000. Minor (toe or transmetarsal) or major (transtibial or transfemoral) amputations were determined from hospital discharges using the highest-level amputation. Mental Component Summary (MCS) from SF36 questions available from LVHS was used as a measure of mental health functioning. Other independent variables included selfreported demographics, foot risk factors(peripheral vascular disease, infections, ulcers and deformities), medical comorbidities, health behaviors (smoking and alcohol drinking), social support (being married, not living alone, and someone available to take to see a doctor) and physical component score (PCS) from SF36. All independent variables as measured in FY1999 were entered into a multinomial (polytomous) logistic regression model; variables with pvalues less than 0.05 were removed from the model. We reported odds ratios (OR’s) and 95% confidence intervals (CI’s). Population Studied: We analyzed 305, 218 veteran clinical users with diabetes who were dually enrolled in Medicare feefor service in fiscal year (FY) 1999 and FY2000 alive at the end of FY2000. A total of 97,652 completed the LVHS. We limited our analyses to those that had no recorded amputations in FY1998 or FY1999; it resulted in 96,242 veterans with diabetes for the statistical analysis. Principal Findings: Of the study cohort 96,242 diabetic veterans, 98.5% were men and the average age was 69.3 (±8.5) years old. There were 346 (3.6 per1000) minor and 366 major (3.8 per 1000) amputations in FY2000. The average MCS score was 43.4 (±13.4). MCS was significantly related to major amputations with decreased mental functioning per five points related to 7% increase in the risk of major amputations (Odds ratio=1.07, 95% confidence interval=(1.03, 1.11)), but was not related to risk of minor amputations. All independent variables except for foot deformity and having someone to take to the doctor were significantly associated with LEAs. Conclusions: Decreased mental health functioning was associated with a higher risk of amputations, especially major amputations in veterans with diabetes when age, race, foot risk factors, medical comorbidities, social support, and physical functioning were controlled for. Implications for Policy, Delivery, or Practice: Individuals with foot risk factors and lower mental health functioning may be candidates for foot care coordination programs that incorporate physical and mental health assessment and care. Mechanisms through which mental health affects amputation outcomes will need further study. Primary Funding Source: VA ●Glycemic Control and Labor Market Participation Kaan Tunceli, Cathy J. Bradley, Jennifer Elston-Lafata, Manel Pladevall, Allen Goodman, George Divine, Deneil M. Kolk, Hugo Xi, Kemeng Li Presented By: Kaan Tunceli, Ph.D., Research Scientist, Center for Health Services Research, Henry Ford Health Systems, 1 Ford Place, Suite 3A, Detroit, MI 48202; Tel: 313-874-5485; Fax: 313-874-1883; Email: ktuncel1@hfhs.org Research Objective: To examine the effect of glycemic control measured by HbA1c on labor market outcomes among patients with diabetes aged 30-64. Study Design: We used automated data sources available within a large multi-specialty medical group, to identify eligible study participants with diabetes and their glycemic control status in 2003. Data from a telephone survey administered to a random sub-sample of 423 eligible patients stratified by glycemic control level was used to solicit information regarding employment status, working hours, and absenteeism in 2004. Glycemic control was defined by average HbA1c during 12 months prior to interview date and classified into five categories (< 7%, 7-7.9%, 8-8.9%, 9-9.9%, • 10%). We estimated the effect of glycemic control on the probability of working using a multivariable probit model (N=415). Among those who are working, we estimate the effect of diabetes on usual weekly hours worked, and work-loss hours in the last week using multivariable ordinary least squares regressions (N=210). Age, gender, race, marital status, education, comorbidities, body mass index (BMI), and insulin usage were controlled. Population Studied: Study participants were drawn from the patients of a non-profit large multi-specialty salaried medical group providing care to the residents in southeastern Michigan, including Detroit and its surrounding metropolitan area. Patients with diabetes were identified according to their hospital discharge diagnosis, outpatient encounters, prescription drugs dispensed, and outpatient laboratory results in 2003. In addition, we restricted the sample to patients who were aged 30-64 at the time of the interview and who had at least one HbA1c test result during the one year before the interview. Principal Findings: The interview participation rate was 57.9%, with a lower rate (50.6%) among those with HbA1c • 10. No HbA1c category was statistically associated with employment status cross-sectionally. Among those who work, relative to patients with HbA1c < 7, patients with 9% • HbA1c < 10% and patients with HbA1c • 10% had 4.8 (p < 0.05) and 4.3 (p < 0.10) more work-loss hours per week respectively. HbA1c levels were not significantly associated with usual weekly hours worked. Conclusions: There might not be a systematic relationship between glycemic control and employment when observed cross-sectionally. It seems that poor glycemic control among employees with diabetes increases absenteeism, and thereby leads to productivity losses. Our analyses suggest that interventions designed to improve glycemic control are likely to yield labor economic benefits in addition to preserving health status and quality of life of individuals with diabetes. Future research is needed to explore the effect of changes in glycemic control on employment and productivity losses longitudinally. Implications for Policy, Delivery, or Practice: Information on the effect of glycemic control on labor market outcomes will be useful for evaluating the cost-effectiveness of interventions aimed toward glycemic control among patients with diabetes. Primary Funding Source: Wayne State University ●Development and Preliminary Evaluation of a Computerized Adaptive Assessment for Asthma (ASTHMA-CAT) Diane Turner-Bowker, Ph.D., Renee N. Saris-Baglama, Ph.D., Milena D. Anatchkova, Ph.D., David Mosen, Ph.D., MPH, John E. Ware, Jr., Ph.D. Presented By: Diane Turner-Bowker, Ph.D., Senior Scientist, Director of Grants & Research Administration, QualityMetric Incorporated, 640 George Washington Highway, Lincoln, RI 02865; Tel: (401)334-8800 x230; Fax: (401)334-8801; Email: dtbowker@qualitymetric.com Research Objective: To develop and field test a prototype patient-based system for assessing asthma impact and control (ASTHMA-CAT) that combines asthma-specific and generic health-related quality of life (HRQOL) measures in a single administration, and that yields user-friendly aggregate reports likely to enhance care management and improve decision-making. Study Design: The ASTHMA-CAT system was programmed for administration via the Internet and included: (a) either the DYNHA Asthma Impact Survey (AIS) [a dynamic survey which uses item response theory (IRT) models and computerized adaptive testing (CAT) methods to provide practical and precise measurement at the individual patient level] or a static, full-length Asthma Impact Survey (AIS); (b) the Asthma Control Test (ACT), a static short-form measure of asthma control; (c) the SF-8 Health Survey, a static short-form generic health status measure; (d) a socio-demographic survey; and (e) a patient User’s Evaluation Survey. This new short, yet comprehensive Internet-based dynamic health assessment was then pilot tested in a small sample of clinician-diagnosed asthma sufferers to evaluate the feasibility, efficiency, and accuracy of the ASTHMA-CAT. Participants were randomly assigned to complete either the dynamic AIS (n=55) or a fulllength static AIS (n=59). All participants completed the ACT, SF-8, socio-demographic and User’s Evaluation Survey. Finally, a prototype aggregate (or group-level) report was developed and evaluated by clinician providers in disease management. Population Studied: Participants were 114 adults with current asthma randomly sampled from a population of 10,000 adult members with chronic disease in Kaiser Permanente’s (KP) Care Management Institute (CMI). The sample was drawn from 16 metropolitan statistical areas (MSA) across six regions: Northern California (6 MSAs), Southern California (6 MSAs), Colorado (1 MSA), Georgia (1 MSA), Hawaii (1 MSA), and the Northwest (1 MSA). The final working sample was primarily comprised of White, non-Hispanic, educated women with mild to moderate asthma, reporting an average age of 45 years. Principal Findings: Response burden, measurement precision, discriminant validity, and users’ evaluation of the dynamic and static full-length Asthma Impact Surveys (AIS) were compared using t-test and ANOVA. The dynamic AIS was completed in significantly less time (M=50.4 seconds) than the static full-length AIS (M=387.4 seconds) [t(112)=-9.84, p=.00]; and achieved equally precise score estimation [t(109)=1.18, p=.24] with substantially fewer items (M=5 items) than the full-length survey. The dynamic AIS discriminated those with mild (M=40.0), moderate (M=52.0) and severe (M=66.1) asthma [F(2,51)=29.17, p=.00]. The dynamic AIS was also significantly easier to complete than the static fulllength survey [t(104)=2.10, p=.04]. 100% of those who took the dynamic AIS indicated that the survey was appropriate in length, compared with 67.8% of those who took the full-length static survey. Generally, very positive feedback was gained from providers regarding the format, relevance, and usefulness of the prototype aggregate report in asthma care evaluation and planning. Conclusions: ASTHMA-CAT is a comprehensive, yet efficient measurement system for adults with asthma. Implications for Policy, Delivery, or Practice: Enhancing the accessibility and interpretability of HRQOL tools and other patient-based assessments will make asthma management more effective in meeting patient care needs. Primary Funding Source: NIH: National Heart, Lung, and Blood Institute ●Primary Care Provider Concerns about Treatment of Chronic Pain Carole Upshur, EdD, Judith Savageau, MPH, Roger Luckmann, M.D. Presented By: Carole Upshur, EdD, Professor, Family Medicine and Community Health, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, MA 01655; Tel: (508)334-7267; Fax: (508)856-1212; Email: carole.upshur@umassmed.edu Research Objective: To identify the scope, concerns and barriers to chronic pain treatment by primary care providers in community-based health centers serving a diverse population in terms of ethnicity and socioeconomic status. Study Design: Survey of all PCPs at 6 federally qualified community health centers and two primary care clinics who had a primary care patient panel Population Studied: Primary care providers, including attendings, residents and nurse practitioners. Principal Findings: The overall response was n=111, or 62.3%. The mean percent of reported patients on the PCP’s schedule from a randomly selected week with a current chronic pain compliant was 37.5%. Providers ranked patient factors, such as lack of self-management, psychological issues, lack of compliance, and occupation as the four highest as barriers to achieving adequate pain management; and ranked such provider and health care system factors as difficulties coordinating care among multiple chronic conditions, lack of evidence based guidelines, time for careful diagnosis, lack of tracking systems, and difficulties assessing patients as less frequent barriers than patient factors. PCPs also reported they were only minimally likely to prescribe opioids for chronic pain Fear of the patient becoming addicted, and fear of the patient selling the opioids were ranked as the highest concerns, with uncertainty about the appropriateness of opioid use ranked third, followed by patients becoming a target for illegal drug users, and worries about side effects. Ranked last was worries about safety. Worriers about law enforcement oversight were surprisingly ranked 6th. Providers report moderate use of some patient centered-care techniques, however provision of patient education materials is ranked last among 12 options for assisting patients to manage their pain. Finally, providers ranked their satisfaction with treating their patients with chronic pain as quite low, M= 1.9 (SD=.81) on a scale where 0=not at all satisfied and 4= very satisfied. In addition, overall rankings of the level of pain management education received in medical or professional school, post graduate medical education, continuing education or on the job experience were extremely low. On a scale of 0=insufficient, 1=adequate, 2=good and 3= very good, the mean ranking was .5 (SD=.8), for medical school,.35 (SD=.67), for post-graduate medical education .7 (SD=.84), and for continuing education .9 (SD=.82). Conclusions: Patients with chronic pain complaints represent a large proportion of primary care visits in a typical week. Providers report overall insufficient training on chronic pain management throughout their educational experiences and very low levels of satisfaction in their ability to treat these patients. At the same time, they tend to identify patient barriers as more troublesome than provider or health care practice structures in adequately addressing patient pain complaints or in prescribing opioids. They do not use some common patient-centered interventions, such as educational materials very frequently. Implications for Policy, Delivery, or Practice: Provider training on managing chronic pain needs to be improved dramatically, including how to appropriately use opioid therapy and how to engage in more patient-centered care. In addition, practice delivery systems using chronic care models need to be developed for chronic pain patients similar to other chronic conditions. Primary Funding Source: AHRQ ●Implementing a Chronic Care Model for Depression Management in an Adult Medicaid Population Carole Upshur, EdD, Linda Weinreb, M.D., Presented By: Carole Upshur, Ed.D., Professor, Family Medicine and Community Health, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, MA 01655; Tel: (508)334-7267; Fax: (508)856-1212; Email: carole.upshur@umassmed.edu Research Objective: To implement a chronic care model of management for adults with depression insured by Massachusetts Medicaid managed care programs, measure outcomes, and identify systems and economic barriers to sustainability. Study Design: A longitudinal, nonexperimental design in six primary care practices. Practices systematically screened all MassHealth adults in their patient panels for depression using the PHQ-9 instrument and implemented chronic care management for major depression. Population Studied: Adults ages 18-64 enrolled in four managed care plans in the Massachusetts Medicaid program. Principal Findings: A total of 1025 adults were screened. The sample included 49% white, 38% Latino, 9% Black, and 5% other, with a mean age of 41 years, 75% female. A mean rate of 30.8% achieved screening scores indicating possible major depression, while an additional 17.2% had moderate depressive symptoms. 30.1% of patients entered care management, which consisted of periodic supportive phone calls and visits with either a nurse or social worker. 59% of patients remained in active care management for 6 months. Patients referred to care management had high rates of comorbid medical illness (60% had one or more of hypertension, diabetes, asthma etc.), and comorbid psychiatric symptoms (e.g. panic, anxiety, history of physical or sexual abuse) at baseline. Mean care manager telephone contacts (3.8),and in -person visits (1.6) over the 6 months were modest, while significant clinically improvement was found in 39% of cases at follow up (PHQ-9 <10 points or 50% improvement). Analysis revealed that Hispanic ethnicity, lack of prior depression treatment, absence of bipolar or psychotic symptoms, and absence of tobacco use explained outcome scores at 6 months. In addition, preliminary analyses of health care utilization, independent of absolute level of care management, calculated in PMPM units one year prior to enrollment in care management and one year after referral to care management, revealed significant decreases in acute primary care visits, significant increases in behavioral health office visits, and a trend to increased antidepressant medication prescribing. Rates of hospitalization were extremely low in both periods and not significantly different. Conclusions: Chronic care approaches to identification and management of depression can be successfully implemented in primary care practices serving Medicaid adults. The prevalence of major depression is high, approximately 6 times the level in the general population, and is accompanied by multiple medical and psychiatric comorbidity. Nevertheless, a relatively modest level of care management support over a period of 6 months assisted in helping a large percentage of the patients achieving clinically significant relief of their depression symptoms. At the same time, implementation of a chronic illness management intervention in this sample is associated with redistribution, rather than overall increases, in health care utilization. Implications for Policy, Delivery, or Practice: Major depression rates are extremely high among Medicaid-insured adults and it is often unrecognized or under treated, in part because symptoms of depression are confused with natural reactions to difficult life circumstances. There is potential for significant reduction in morbidity and more appropriate health and behavioral health care utilization. Primary Funding Source: RWJF ●Risk Indices for Adverse Outcomes After Surgery For Small Bowel Obstruction Katherine Virgo, Ph.D., MBA, Julie A. Margenthaler, M.D., Walter E. Longo, M.D., Frank E. Johnson, M.D., Tracy L. Schifftner, MS, William G. Henderson, Ph.D. Presented By: Katherine Virgo, Ph.D., MBA, Professor, Surgery, Saint Louis University & St. Louis VAMC, 3635 Vista at Grand Boulevard, Saint Louis, MO 63110-0250; Tel: (314) 289-7023; Fax: (314) 289-7038; Email: virgoks@slu.edu Research Objective: The study objectives were to identify risk factors for adverse outcomes following surgical treatment of small bowel obstruction (SBO) and develop an easy-to-use tool for clinicians to improve patient care. Study Design: Using prospectively collected data, independent variables examined included 68 pre-surgical and 12 intra-operative clinical risk factors; dependent variables were 21 specific adverse outcomes including death. Stepwise logistic regression analysis was used to construct models predicting 30-day morbidity and mortality rates and to derive risk index values. Patients were then divided into risk classes. Population Studied: The Veterans Affairs (VA) National Surgical Quality Improvement Program (NSQIP) contains prospectively collected and extensively validated data on >1,000,000 patients. All patients undergoing either adhesiolysis only or small bowel resection with anastomosis for SBO from 1991-2002 were selected for study. Principal Findings: Of the 2,002 patients identified, 1,650 underwent adhesiolysis only and 352 underwent small bowel resection. The adhesiolysis only group had a significantly lower frequency of three co-morbid conditions (alcohol use, disseminated cancer, weight loss; p<0.05); those undergoing small bowel resection had a lower frequency of congestive heart failure (p<0.05), but the groups were otherwise comparable. Thirty-seven percent of patients undergoing adhesiolysis only and 47% of patients undergoing small bowel resection had >1 complications (p<0.001). Pneumonia, prolonged ileus, failure to wean from the ventilator, unplanned intubation, superficial wound infection, urinary tract infection (UTI), systemic sepsis, and wound dehiscence were among the most frequently reported complications for both groups. The overall 30-day mortality rate was 7.7%. The mortality rate associated with small bowel resection did not differ significantly from the mortality rate for adhesiolysis only. The odds of death were highest for patients who had infected wounds, American Society of Anesthesiologists (ASA) class 4 or 5, age 80+, dyspnea at rest, and dirty wounds. Totally dependent functional health status, age 80+, dirty wounds, history of congestive heart failure (CHF), cerebrovascular accident (CVA) with neurological deficit, history of chronic obstructive pulmonary disease (COPD), and ASA class 4 or 5 were associated with a greater risk of complications. Morbidity rates ranged from 22%, among patients with 0-7 risk points, to 62% for those with 19+ risk points. Mortality rates ranged from 2%, among patients with 0-12 risk points, to 28% for those with 31+ risk points. Conclusions: Morbidity and mortality rates after surgery for SBO in VA hospitals are comparable to those in other large published series. In the current study, the morbidity rate, but not the mortality rate, was significantly higher in patients who required small bowel resection compared to those requiring adhesiolysis only (p<0.001). The risk indices presented here provide an easy-to-use tool for clinicians to predict outcomes for patients undergoing surgery for SBO. Implications for Policy, Delivery, or Practice: The calculated postoperative risk indices for 30-day morbidity and mortality may be useful in targeting peri-operative testing and supportive care to high-risk patients. While it is true that some patient risk factors are not modifiable, such as steroid use, health status, disseminated cancer, and chronic obstructive pulmonary disease, many of the preoperative and intraoperative factors identified by the NSQIP may be altered. Preoperative fluid resuscitation in patients with high serum creatinine levels, platelet and fresh frozen plasma transfusions for patients with low platelet levels or prolonged prothrombin times, and prevention of intra-operative wound contamination are some of the factors identified as important in preventing morbidity and mortality. Primary Funding Source: VA ●Complications from Affective Psychosis: What Are the Implications of Different Patterns Across Diverse Ethnicities? Elmer Washington, M.D., MPH, Jay J. Shen, Ph.D. Presented By: Elmer Washington, M.D., MPH, Medical Director, Aunt Martha’s Youth Service Center, 233 West Joe Orr Road, Chicago Heights, IL 60411; Tel: (708) 709-7610; Fax: (708) 747-3497; Email: ewashington@auntmarthas.org Research Objective: To evaluate patterns of care for affective psychosis across diverse ethnicities over time and to determine potential environmental effects on patterns of care and severity of disease. Study Design: Comorbidities across all populations were evaluated and included personality disorders and all medical conditions that may have an impact on the clinical outcomes. In addition, complicating conditions; defined as complications resulting potentially from inadequate access to timely care; were evaluated. These conditions included overdose or medication error resulting from carelessness (codes 960969), drug or alcohol abuse or dependence (codes 303 - 305), suicide attempt or self inflicted injury (E950-E959), homicide or injury inflicted upon another (E960-E969), legal intervention contributing to an injury (E970-E978), and physiologic malfunctioning caused by a mental disorder (306). Discharges with the diagnostic code 296 for all categories of affective psychosis were abstracted and analyzed for differences in comorbidities and complicating conditions across diverse ethnicities. Population Studied: Data was obtained on patients admitted with a diagnosis of affective psychosis to hospitals that participated in the National Inpatient Sample during 1995, 1997, 1999, 2000, and 2001. Sample sizes were 73,745 in 1995, 85,840 in 1997, 83,105 in 1999, 91,551 in 2000, and 95,260 in 2001. Ethnicities included white (79.3%), African American (13.8%), Hispanic (5.9%), and Asian-Pacific Islander (.9%) Principal Findings: White patients were older with higher risk of having comorbid conditions (RR ranging from 1.02 to 1.19) compared to the other minority groups. Compared to both African Americans and whites, Hispanics and Asians had lower risk of experiencing complicating conditions (RRs ranging from 0.77 to 0.89 for Hispanics and from 0.43 to 0.69 for Asians). Conclusions: Further research is needed to determine the factors underlying lower risk of complicating conditions among Asians and Hispanics. Several hypotheses including levels of group cohesion, the role of extended family, and various culturally based explanations merit further investigation. Implications for Policy, Delivery, or Practice: Public policy should encourage formation of support systems in areas where unemployment levels increase significantly given the existing body of research demonstrating the effectiveness of such systems. Primary Funding Source: AHRQ ●Recurrences of Non-Specific Occupational Low Back Injuries: Relative Contributions to Related Costs and Work Disability Radoslaw Wasiak, Ph.D., JaeYoung Kim, M.D., Ph.D., Glenn Pransky, M.D. Presented By: Radoslaw Wasiak, Ph.D., Research Scientist, Center for Disability Research, Liberty Mutual Research Institute for Safety, 71 Frankland Road, Hopkinton, MA 01748; Tel: (508)497-0242; Fax: (508)435-8136; Email: radoslaw.wasiak@libertymutual.com Research Objective: Previous studies have not measured the proportion of care-seeking and work disability that are associated with recurrences in claims for work-related LBI. The objective of this study was to examine whether recurrences, defined as repeated episodes of work disability or medical care, substantially contribute to total medical and indemnity costs and total duration of work disability. Study Design: Retrospective analysis of detailed workers’ compensation (WC) claims data for non-specific low back injuries (LBI) in a single jurisdiction. Three years of detailed follow-up data, starting at the beginning of the first episode were collected. Previously-validated definitions of recurrence were used to identify new episodes of care and new episodes of lost work time (work disability). Total duration of work disability, total medical costs, and total indemnity costs were investigated. For individuals with recurrences, outcome variables were separated into first-episode and recurrent period duration and costs. Population Studied: All persons with new lost-time claims for non-specific LBI reported in New Hampshire to a large WC provider from 1996 to 1999 were selected (N=1867). Principal Findings: The rate of recurrent work disability was 17.2% and the rate of recurrent care seeking was 33.9%. Individuals with recurrence had significantly higher total length of work disability and higher medical and indemnity costs. For those with recurrent work disability, 69% of total lost time from work, 71% of associated indemnity costs, and 84% of total medical costs occurred during the recurrent period. For those with recurrence of care, the respective values were 48%, 47%, and 42%. Conclusions: Recurrence of LBI contributes substantially to the total burden of work-related non-specific LBI, through both additional care-seeking and work disability. Results support the contention that non-specific LBI is episodic in nature. Although individuals may learn to live with their conditions, ongoing care and time away from work occur in a substantial proportion in work-related LBI. Implications for Policy, Delivery, or Practice: The study findings indicate that prevention of repeated episodes may lead to substantial cost savings and increase the rate of sustained return to work. Primary Funding Source: No Funding Source ●Dispersion of Care and Cardiovascular Outcomes; Does More Matter? Brook Watts, M.D., David Litaker, M.D., Ph.D. Presented By: Brook Watts, M.D., Quality Scholar, Education, Louis Stokes Cleveland VA Medical Center, 10701 East Boulevard, Cleveland, OH 44106; Tel: (216)791-3800 x4110; Email: wattsbrook@yahoo.com Research Objective: Dispersion of care (DOC) is viewed as a potential barrier to delivery of coordinated, comprehensive primary care. DOC has become even more salient given recent mandatory restrictions on the workweek of resident physicians. Disruptions introduced by these restrictions may result in unanticipated and/or undesirable effects on patient care, especially in the long-term risk management of chronic diseases. The purpose of this study was to examine the relationship of DOC to cardiovascular treatment outcomes in VA patients assigned a resident as their primary care provider. Study Design: In this retrospective cohort study, we assessed whether patients had attained nationally recommended riskfactor specific treatment goals for blood lipids, blood pressure (<140/90 or <130/80 in diabetics), and glycemic control (hemoglobin A1C <7%). We also assessed presence of poor blood pressure control (=160/100). DOC was determined using system-assigned numbers to identify the provider at each visit in the 12 months preceding the lipid profile. An established index of DOC was dichotomized to reflect either complete continuity vs. some degree of DOC. Multivariable logistic regression adjusted for patient demographics, clinical characteristics, and the nesting of patients within resident practices to assess the independent association of DOC with each outcome. Population Studied: Using the clinical database at the study site we identified 473 patients with a lipid profile obtained between January 2003 and October 2004 whose PCP was a 1st, 2nd, or 3rd year resident. Principal Findings: Of the 473 patients, 363 patients (76.7%) had DOC (range 2-5 providers). Although the DOC group included more women (5.8% vs. 0.9%; p=.04) and had more PCP visits (mean 3.3 +/-1.3 vs. mean 2.4 +/-0.63; p<.01), no other significant differences in patients’ age, cardiovascular disease, hypertension (HTN), disease burden, current tobacco abuse, and diabetes mellitus (DM) were present. Attainment of LDL goal was similar in the two groups (65.8% vs. 64.6%; p=.80), yet adequate blood pressure control in those with HTN or DM was lower in the DOC group (42.6% vs. 56.7%; p=.01) and the proportion of patients with poor blood pressure control (=160/100) was greater (14.6% vs. 6.4%; p=.02). In 148 DM patients, significantly fewer patients in the DOC group achieved desirable glycemic control (44.6% vs. 71.4%; p=.01). Using multivariate models, DOC remained associated with less frequent attainment of appropriate HTN control (OR 0.51; CI 0.30-0.87), an increased likelihood of having poor HTN control (OR 2.52; CI 1.11-5.75), and a lower likelihood of glycemic control in DM patients (OR 0.33; CI .12.93). We found no significant association between DOC and lipid control. Conclusions: The association between DOC and treatment outcomes does not appear uniform and may more negatively affect outcomes such as HTN and glycemic control that involve complex management and a greater familiarity with a patient’s comorbidities, medical history, and compliance. Implications for Policy, Delivery, or Practice: In residents’ clinics where DOC is common, developing systems to coordinate efforts at risk factor management may be useful. Our data also suggest that caution is needed when selecting outcomes to examine the impact of continuity on patient care. Primary Funding Source: VA ●Linking Provider Attitudes and Self-Efficacy to Secondary Cardiovascular Prevention Brook Watts, M.D., David Litaker, M.D. Presented By: Brook Watts, M.D., Quality Scholar, Education, Louis Stokes Cleveland VA Medical Center, 10701 East Boulevard, Cleveland, OH 44106; Tel: 216-791-3800 x4110; Email: wattsbrook@yahoo.com Research Objective: Patients with modifiable cardiovascular (CVD) risk factors may benefit from preventive care, yet health care providers frequently fail to provide this important service consistently. Conceptual models have identified provider attitudes and self-efficacy as potentially important barriers to provision of preventive care. The purpose of this study was to examine the association of these provider characteristics to CVD risk factor management and outcomes in high-risk patients. Study Design: In this cross-sectional study, data on provider attitudes and self-efficacy were measured using a standardized instrument and were linked with patient-level laboratory and pharmacy data to evaluate the association with the following CVD prevention process measures: lipid screening and treatment for dyslipidemia. We also examined the association between provider attitudes, self-efficacy, and self-report of services delivered with patients’ attainment of risk-adjusted nationally recommended treatment goals for low density lipoprotein (LDL). Multi-level models adjusted for the following covariates: 1) patients– age, gender, number of visits, and count of medical illnesses/health burden, and 2) providers– age, gender, and professional status (i.e., physician trainee, staff physician, non-physician provider). Population Studied: Thirty-seven primary care providers at various levels of professional training at a large VA outpatient clinic and 522 patients, each of whom had been seen at least twice in 2003 by a provider in our survey group and who had a diagnosis of coronary heart disease (CHD) or CHD equivalent condition and no contraindication to lipid-lowering therapy. Principal Findings: Of the 37 providers in our sample, 25 (67.6%) were interns or residents, 6 (16.2%) were staff physicians, and 6 (16.2%) were advanced practice nurses or pharmacists. The importance of CVD prevention was reported as high or very high by 32 providers (88.9%) and individual self-efficacy in CVD prevention was reported as high or very high by 15 providers (40.5%). Of the 522 high-risk patients identified, 361 (69.2%) had lipid screening during the study period; among screened patients, 202 (56.0%) were at the recommended treatment goal. Multi-level models showed no significant association between provider self-efficacy or selfreported service delivery in this area and process or outcomes related to CVD prevention. Conclusions: Although nearly all providers in our sample agreed with the importance of CVD risk factor management, we identified many missed opportunities for secondary CVD prevention. Favorable provider attitudes and high self-efficacy alone may be necessary, but they do not appear to be sufficient in guaranteeing delivery of recommended care or achievement of desirable outcomes. Implications for Policy, Delivery, or Practice: Factors other than attitudes and self-efficacy may be better targets for interventions to improve preventive CVD care. Systems which address outcome expectations, goals, facilitators and impediments may be necessary. Primary Funding Source: VA ●The Impact of Visit Interval on Blood Pressure Control and Management Mark Weiner, M.D., BJ Turner, M.D., Craig A. Umscheid, M.D., Christopher Hollenbeak, Ph.D., Yi-Ting Lin, MS, Simon Tang, MPH, Suchin Virabhak, Ph.D. Presented By: Mark Weiner, M.D., Assistant Professor, Division of General Internal Medicine, University of Pennsylvania, 423 Guardian Drive -- Room 1116, Philadelphia, PA 19104; Tel: (215) 898-5721; Fax: (215) 573-8779; Email: mweiner@mail.med.upenn.edu Research Objective: The appropriate interval in which to follow-up a patient with hypertension (HTN) has little support from empiric data. This study examines the association between the time interval since the prior visit for a patient with HTN and blood pressure (BP) control and physicians' management decisions regarding patients presenting with elevated BP. Study Design: We studied a retrospective cohort of hypertension (HTN) patients aged >= 18 with at least three visits from 1/1/03 to 8/01/04 in one of 8 primary care practices in Philadelphia urban and suburban settings. Clinical, laboratory, pharmacology and health care data came from electronic medical records and administrative billing data. The dependent variable was a finding of appropriate management for each visit. Management was appropriate if BP was normal or, if high, the dose of a current BP med was increased, a new BP med was started, or a med was renewed if expired >1 month. Since the unit of analysis was the visit, random effects multiple logistic regression was used to adjust for clustering of patients. Population Studied: HTN was defined using hierarchical criteria: 1) a prescribed BP medication (med); 2) ICD-9-CM diagnosis of HTN and >=1 visit with a high BP defined as systolic BP (SBP) >= 140 or diastolic BP (DBP) >= 90; or 3) high BP on >=2 visits. For each prescribed BP med, we determined the daily dose and duration of treatment. High BP based on JNC VI for patients without diabetes was SBP>=140 and DBP>=90 and for patients with diabetes, a more stringent threshold of SBP>=130 or DBP>=85 was set. Patients with diabetes (DM) were identified from diagnosis codes or HbA1C >7. Patients with and without DM were analyzed separately. Principal Findings: In 22,472 visits made by 3,597 HTN patients with DM, BP was controlled in 43%. In 48,718 visits of 10,086 patients without DM, BP control was achieved in 61%. Adjusting for demographic, clinical, and health care factors and using a visit interval of < 3 months as the reference, the adjusted odds ratio (AOR) of having uncontrolled BP was 1.10 (CI 1.04-1.16) for an visit interval of 6-9 months, 1.18 (CI 1.101.27) for an interval of 9-12 months and 1.25 (CI 1.17-1.33) for an interval over one year. In the DM patients, the associations were even stronger: AOR 1.11 (CI 1.02-1.22), AOR 1.38 (CI 1.211.58) and AOR 1.36 (CI 1.19-1.55). Inappropriate management was less likely (AORs ranging from 10 to 20% lower, p < 0.05) for longer visit intervals versus <3 months. Conclusions: Longer intervals between visits of patients with HTN, especially over 6 months, are associated with a greater risk of presenting to the visit with uncontrolled HTN. Physicians were more likely to modify HTN treatment in patients seen less frequently. Implications for Policy, Delivery, or Practice: Physicians are reacting appropriately to the elevated blood pressure readings that are associated with longer visit intervals. However, a more preventative and proactive strategy would set visit intervals of no more than 3-6 months for patients with HTN, especially those who also have DM. Primary Funding Source: Pfizer ●Identification of Subgroups of Medicare Beneficiaries with Diabetes: Segmentation to Inform Targeted Outreach and Tailored Education Strategies Sunyna S. Williams, Ph.D. Presented By: Sunyna S. Williams, Ph.D., Social Science Research Analyst, Office of Research, Development, and Information, Centers for Medicare & Medicaid Services, 7500 Security Boulevard/Mail Stop: C3-20-17, Baltimore, MD 21244; Tel: (410)786-2097; Email: sunyna.williams@cms.hhs.gov Research Objective: The purpose of this research was to identify subgroups or segments of Medicare beneficiaries with diabetes, to inform the development of targeted outreach and tailored education strategies. Study Design: This research involved secondary data analysis of the 2001 Medicare Current Beneficiary Survey (MCBS) Access File Community Questionnaire. The MCBS is an ongoing household panel survey conducted by the Centers for Medicare & Medicaid Services (CMS), of a representative national sample of Medicare beneficiaries. The Access File includes data on beneficiaries continuously enrolled for the year. The Community Questionnaire is administered by faceto-face interview with community-dwelling beneficiaries or their designated proxies, and assesses a wide range of healthrelated variables. The data files include a sample weight variable and variables to permit adjustment for the complex cluster sample design. Segmentation was achieved by conducting k-means cluster analysis on four knowledge and attitudes variables—global perceived knowledge about the Medicare program, self care self-efficacy composite, health information-seeking composite, and satisfaction with information received regarding health problems. Comparisons were conducted among the cluster segments, using chisquare (for categorical variables) and univariate general linear model with sequential sidak to control for Type I error (for continuous variables). Population Studied: Of the 15,246 in the community sample, 2,814 (19%) reported ever having been told by a doctor that he or she had diabetes. Of that diabetic subsample, 2,495 (90%) were self-respondents to the interview. The analytic sample is those 2,495 diabetic self-respondents. This sample is 15% disabled and under 65 years, 55% female, 72% white, and 77% overweight or obese. Principal Findings: The four-cluster solution was selected based on interpretability, separation, and distribution. Savvy beneficiaries (42%) are highest on all four knowledge and attitudes clustering variables. They are also the most educated, the healthiest, the least likely to have only basic Medicare fee-for-service, and engage in the most healthful and preventive behavior. Passive beneficiaries (23%) are lowest on self-efficacy and information-seeking, and moderate on knowledge and satisfaction. They are also the most likely to have only basic Medicare fee-for-service and engage in the least healthful and preventive behavior. Uninformed beneficiaries (29%) are lowest on knowledge, and moderate on the remaining clustering variables. They are also the least educated. Dissatisfied beneficiaries (6%) are lowest on satisfaction, and moderate on the remaining clustering variables. They are also the youngest, the most overweight and obese, the most depressed, the most likely to smoke, and the least satisfied with their healthcare. Additional analyses showed that, for tailoring purposes, those in the four segments can be identified using three single screening items. Conclusions: These analyses identified four segments of Medicare beneficiaries with diabetes that vary with regard to a range of health-related variables. Implications for Policy, Delivery, or Practice: These findings can be used to promote informed healthcare and self care decision-making among Medicare beneficiaries with diabetes. Outreach targeted to the different segments should consider differences in education and health status. For tailoring purposes, those in the four segments can be identified using the screening items. Education tailored for the different segments should also consider differences in knowledge, attitudes, and health behavior. Primary Funding Source: CMS ●Understanding Global Transition Ratings Kathleen Wyrwich, Ph.D., Vicki M. Tardino, MA Presented By: Kathleen Wyrwich, Ph.D., Assistant Professor, Research Methodology & Health Services Research, Saint Louis University, 3750 Lindell Boulevard, Room 230, St. Louis, MO 63108; Tel: (314)977-8192; Fax: (314)977-1616; Email: wyrwichk@slu.edu Research Objective: Several methods currently used for determining meaningful or important change in health-related quality of life (HRQoL) are based on patients' responses to global transition assessments. It can be empirically demonstrated that patients' responses to these gold standards for change do not adequately incorporate the prior condition, yet these transition items play an influential role in patient-clinician communications and cannot be disregarded. This follow-up study queried patients to better understand how they ascertained their transition assessments Study Design: We used face-to-face cognitive interviews to obtain qualitative clues for understanding patient reports of HRQoL changes over time. Interview transcripts were coded using the components of the Rapkin-Schwarz HRQoL Model. Population Studied: Prior to their qualitative interviews, the 41 chronic disease patients in this study had completed one year of enrollment in a clinical study with bi-monthly HRQoL telephone interviews that included the SF-36 and a diseasespecific (asthma, COPD, or heart disease) HRQoL instrument, as well as global transition assessments for each instrument's domains. Principal Findings: Patients' explanations for determining global transition assessments in HRQoL domains often focused on current mobility and fatigue patterns, physicians' statements about their conditions, comparisons of their current states with the prior health conditions, and strong personal convictions that reflected a resistance to voicing any emotional changes. Patients also expressed primary health concerns, like back pain, that were not related to the chronic conditions (asthma, COPD or heart disease) under investigatio Conclusions: Quantitative studies that incorporate GT assessments to anchor the interpretations of HRQoL changes should also consider additional relevant items identified by this qualitative investigation to inform researchers of the potential framework that patients use to assess and report their transitions. Implications for Policy, Delivery, or Practice: In addition, patient-clinician communications that incorporate global transition assessments to anchor the interpretations of HRQoL changes should also consider additional relevant questions identified by this qualitative investigation to understand the process each patient uses to appraise and report changes in HRQoL. Primary Funding Source: AHRQ ●The Effect of Evidence-Based Cardiac Medication Use on Hospital Readmission Zhou Yang, Ph.D., MPH Ade Olomu, M.D., William Corser, Ph.D., David Rovner, M.D., David Sheps, M.D., MPH, Margaret HolmesRover, Ph.D. Presented By: Zhou Yang, Ph.D., MPH, Assistant Professor, Health Services Research, Management and Policy, University of Florida, 101 South Newell Drive, Room 4141, Gainesville, FL 32610-0195; Tel: (352)273-6081; Fax: (352)273-6075; Email: zyang@phhp.ufl.edu Research Objective: The importance of outpatient cardiac medication use for patients has been widely recognized, and is a primary focus of quality improvement. While previous research has suggested that hospital discharge is a critical time to promote the initial and continued use of cardiac medications for Acute Coronary Syndrome (ACS) patients, little research has investigated the effects of ongoing outpatient drug use patterns after hospital discharge. Our objective was to analyze patterns of outpatient cardiac medication use after initial hospitalization for ACS, and investigate the impact on the probability of subsequent hospital readmissions. Study Design: This is an observational study using secondary data. Chart reviews are merged with data from post hospitalization surveys about health care utilization and health outcomes conducted at 3 time points: immediately after discharge, 3 months, and 8 months after discharge. We conducted a descriptive analysis to examine the dynamic feature of post-acute ACS patient care, particularly changing patterns of outpatient prescription drug use, post-discharge hospital readmissions, and Emergency Department (ED) visits. Series of multivariable logistic regression models were used to estimate the association between post ACS medication use and hospital readmission and ED visits by the 3 and 8 months telephone surveys. Population Studied: 433 patients prospectively identified with ACS in five mid-Michigan community hospitals during the period January 2002 to April 2003 Principal Findings: Most changes to medication regimens use occurred within 3 months after discharge, with fewer changes in the subsequent 5 months. Taking Beta-Blockers (odds ratio, 0.46 [95% CI, 0.21 to 0.99]) or AngiotensinConverting Enzyme Inhibitors (ACEI) (odds ratio, 0.31 [95% CI, 0.13 to 0.77]) significantly reduced the probability of hospital readmission within 3 months after discharge (P<0.05). Higher adherence to ACEI after discharge contributed to even lower hospital readmission rate (odds ratio, 0.55 [95% CI, 0.34-0.89], p<0.1). Re-hospitalized within 3 months after discharge was a strong predictor of later hospital readmission up to 8 months after discharge (odds ratio 0.74 [95% CI 0.73 to 1.74] p<0.05) Conclusions: In addition to the prescription of effective discharge medications, timely and appropriate medication adjustment in outpatient settings appears to improve health outcomes in ACS patients. Implications for Policy, Delivery, or Practice: Time interval shortly after discharge could be a good opportunity to initiate and promote drug therapy for post ACS patients, which indicates the important role of outpatient care physicians. More research, especially longitudinal studies are expected to be conducted at outpatient clinical settings to investigate the effect of physician-patients relationships on continuity of health care as well as subsequent health outcomes of post ACS patients. Primary Funding Source: AHRQ