Spatial Analysis of Healthcare Markets: Separating the Signal Admission Rates
advertisement
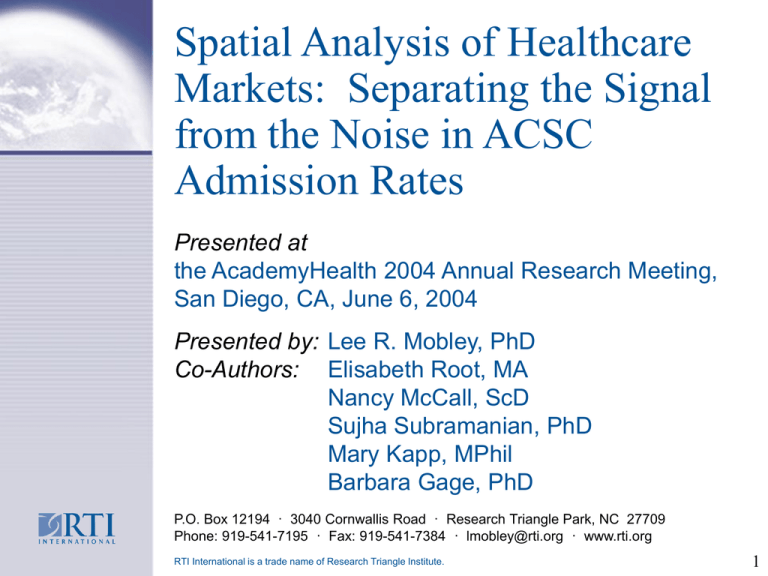
Spatial Analysis of Healthcare
Markets: Separating the Signal
from the Noise in ACSC
Admission Rates
Presented at
the AcademyHealth 2004 Annual Research Meeting,
San Diego, CA, June 6, 2004
Presented by: Lee R. Mobley, PhD
Co-Authors: Elisabeth Root, MA
Nancy McCall, ScD
Sujha Subramanian, PhD
Mary Kapp, MPhil
Barbara Gage, PhD
P.O. Box 12194 · 3040 Cornwallis Road · Research Triangle Park, NC 27709
Phone: 919-541-7195 · Fax: 919-541-7384 · lmobley@rti.org · www.rti.org
RTI International is a trade name of Research Triangle Institute.
1
Overview
This paper examines the association between
geographic or market-level supply and demand
factors and market-level rates of three ambulatory
care sensitive conditions (ACSCs):
chronic obstructive pulmonary disease (COPD)
congestive heart failure (CHF), and
lower limb peripheral vascular diseases (PVD)
Study Population: Medicare FFS beneficiaries over
two time periods: mid nineties and latter nineties.
Markets Definition: 306 Hospital Referral Regions
from the Dartmouth Atlas Project
2
Spatial Market Analysis:
Motivation
In the previous market-level analysis, we found
that Census division effects were significant
even after controlling for demographic and
disease severity factors, which suggests that
there may be important characteristics of places
that are omitted in the analysis.
Market-specific factors that impact access or
continuity of care may be important variables to
examine in explaining ACSC admission rates.
Medicare policy changes in the latter nineties
may have impacted these market-specific
effects.
3
CHF Rates in HRRs,
1995–1997
CHF_EARLY
0.014 - 0.024
0.024 - 0.032
0.032 - 0.051
NO_HRR
4
CHF Rates in HRRs,
1998–2000
CHF_LATE
0.014 - 0.024
0.024 - 0.032
0.032 - 0.056
NO_HRR
5
COPD Rates in HRRs,
1995–1997
COPD_EARLY
0.005 - 0.014
0.014 - 0.02
0.02 - 0.038
NO_HRR
6
COPD Rates in HRRs,
1998–2000
COPD_LATE
0.006 - 0.014
0.014 - 0.02
0.02 - 0.04
NO_HRR
7
PVD Rates in HRRs,
1995–1997
PVD_EARLY
0 - 0.002
0.002 - 0.003
0.003 - 0.008
NO_HRR
8
PVD Rates in HRRs,
1998–2000
PVD_LATE
0 - 0.002
0.002 - 0.003
0.003 - 0.007
NO_HRR
9
Access and Utilization
Access to care and utilization of health
services is impacted by many factors:
Population characteristics
Health system characteristics
Local area market characteristics
Our conceptual model combines these three
elements to show the pathways to realized
demand (actual utilization)
10
Methods:
Conceptual Model of Access
(Khan and Bhardwaj, 1994; WHO, 2000)
X1: Characteristics of Health Care
System
Place Specific Variables
•(Supply/Attraction)
•-Number/Location of Facilities
•-Number/Location of Nurses
•-HMO Penetration
Potential Access
X2: Characteristics of Health Care
System
Person-specific Variables
•Age, gender
•Race, ethnicity
•Education
•Morbidity
•Income, Poverty
X3: Barriers/Facilitators
(Intervening Factors)
•Transportation systems
•Traffic congestion
•Distance to facilities
•Climate
•Safety
Utilization of Health
Care Services
11
Methods: Empirical Challenge
The intervening factors that may be so
important in determining elderly utilization are
difficult to measure (proxy: population density).
Other important missing variables are practice
patterns and/or health behaviors that may vary
significantly from place to place, yet may be
similar in local regions (spillovers).
The empirical challenge is to find a model
specification that accounts for these missing
variables so that their omission does not impart
bias on other parameters of interest.
12
Methods
Three ACSCs were examined: PVD, COPD,
CHF; 3-year rates were constructed for 1995–
1997 and 1998–2000 (ACSC admission/all
beneficiaries in 1,000s).
We combined inpatient and ER/observation bed
stays.
Beneficiary and county-level data were
aggregated to HRRs, yielding 306 observations
in an early period and 306 in a late period.
SpaceStat software was used to estimate a
spillovers spatial regression model
13
Methods
Primary Data Sources for explanatory variables
CMS Enrollment Data File and claims Files
CMS Provider of Service (OSCAR) file
CMS Medicare Managed Care Penetration file
AMA Physician Masterfile
AHA County Hospital File
US Census of Populations
Interstudy
AARP
14
Methods
Sociodemographic Characteristics
Proportion of elderly in poverty (1989,1999)
Proportion of county that are elderly
Proportion of sample Black
Proportion of sample male
Proportion of sample >80
Proportion of sample dual enrolled
Proportion of sample who died
Proportion of elderly with supplemental insurance
15
Methods
Health Status Characteristics
Median PIP-DCG score
Proportion of sample with ESRD
Proportion of sample with diabetes
16
Methods
Market Characteristics
M+C Penetration
Proportion of population in private HMOs
Home health visits per Medicare insured
Medicare admissions to SNFs
Hospital inpatient occupancy of staffed beds
Number of non-Federal practicing MDs
Number of FTE, hospital-based RNs
Number of SNFs
Number of HHAs
Number of Hospices
Number of Rural Health Clinics
17
Methods
Market Characteristics
Number of hospitals with outreach programs
Number of hospitals with assisted living programs
Number of hospitals with rehabilitation programs
Number of hospitals with transportation
Number of hospitals with home health services
18
Methods
Access Proxies
Proportion of the population who said they didn’t
visit a physician due to cost
Proportion of the population who reported
problems accessing a primary care provider
19
Methods
We estimate the ecological model on data
from two separate cross sections to assess
whether factor effects changed over a time
We indirectly examine the influence of SNF
and HH payment reforms on the market rate
of ACSC hospitalizations
20
Empirical Findings
Beneficiary characteristics explain most of
the market-level variation in ACSC
admissions.
Poverty among the elderly has become an
increasingly important predictor of all three
ACSCs over time — the large, positive
association with COPD and CHF increases
(doubles in magnitude) over time.
The mean proportion of the elderly in
poverty declined nationally between
1989 and 1999.
21
Empirical Findings:
Demographic Factors
Places with higher proportions of the oldest-old
have lower COPD rates (and increasingly so over
time) and lower CHF rates (and diminishing over
time)
Places with higher proportions of beneficiaries who
died had higher COPD and CHF rates, fairly stable
over time.
Places with higher proportions of black beneficiaries
had lower PVD and COPD rates
Places with greater proportions of diabetics and
ESRD had higher PVD rates and more home health
visits per beneficiary (magnitude doubled over time)
22
Empirical Findings:
Market Factors
Places with more SNFs exhibit higher COPD and
CHF admit rates – but stable over time.
No association between number of HHAs and ACSC
admit rates but number of HHA visits positively
associated with PVD hospitalizations and
increasingly so over time.
Places with more hospital-based rehabilitation
programs have lower CHF and COPD rates – smaller
effect over time.
Managed care penetration of Medicare market has
no change in effect over time for CHF and PVD and
modest negative effect for COPD in later period
23
Other Factors
Inpatient hospital occupancy rate was positively
associated with PVD rates in the early period,
and negatively associated with CHF rates in the
later period.
Places with higher HMO penetration in the
private market show lower PVD and COPD
hospitalization rates in the early period.
Places with higher proportions of the elderly
holding supplemental insurances show lower
COPD hospitalization rates in the early period
and higher CHF rates in the later period.
24
Other Factors
Places where higher proportions of the
population ‘didn’t visit a doctor because of cost’
showed positive association with COPD rates
in the later period.
The numbers of physicians and registered
nurses, and the statewide measure of
physician shortage, were surprisingly
insignificant in these models.
Other supply variables such as hospital
services and other post-acute care services
were also surprisingly silent.
25
Empirical Findings:
Spatial Spillovers
Spatial Lag Model: Ri = jI wijRj + Xi + ui
Is the measure of strength of spatial spillovers
The estimate of is 0.164 for PVD, >0.50 for
COPD, and >0.40 for CHF
For PVD, spillovers are local (2 closest HRRs)
while for COPD and CHF, spillovers are regional
(6 closest HRRs)
Given the spatial clustering observed in COPD
and CHF, geographically-targeted interventions
may be possible.
26
CHF & COPD Rates ('98–'00) and Elderly in
Poverty (1999)
27
Change in CHF & COPD Rates ('95–'97) to
('98–'00), and Change in Elderly Poverty Rate
28