Causal Effect of Managed Care on Health Care Quality: Guideline Discontinuities
advertisement
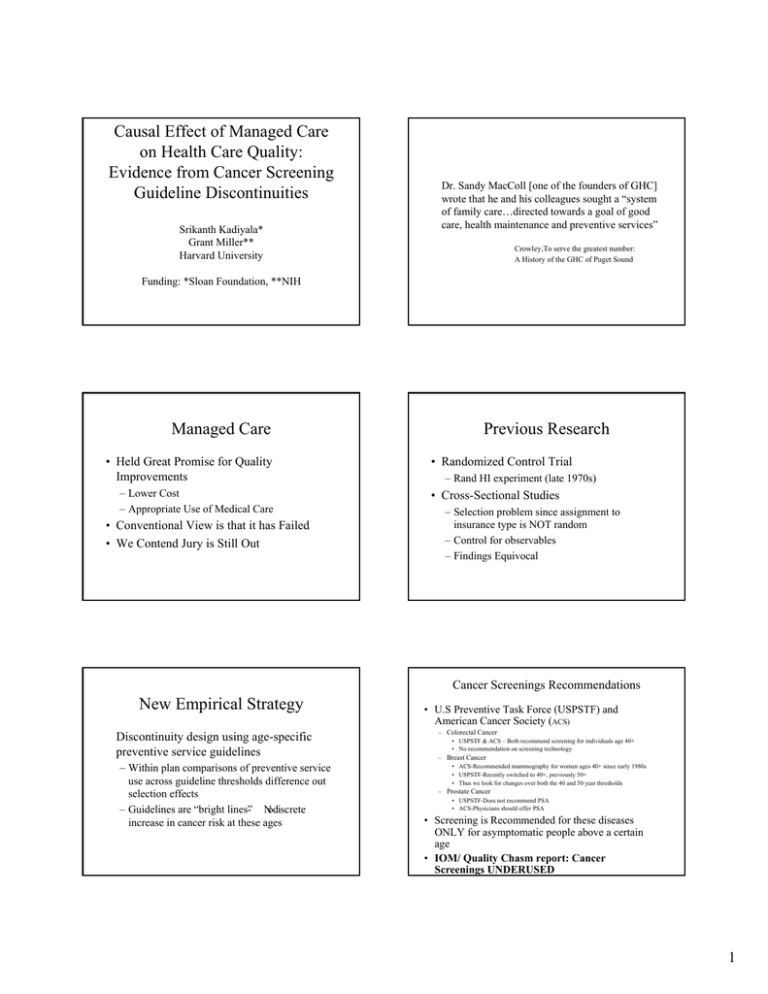
Causal Effect of Managed Care on Health Care Quality: Evidence from Cancer Screening Guideline Discontinuities Srikanth Kadiyala* Grant Miller** Harvard University Dr. Sandy MacColl [one of the founders of GHC] wrote that he and his colleagues sought a “system of family care…directed towards a goal of good care, health maintenance and preventive services” Crowley,To serve the greatest number: A History of the GHC of Puget Sound Funding: *Sloan Foundation, **NIH Managed Care • Held Great Promise for Quality Improvements – Lower Cost – Appropriate Use of Medical Care • Conventional View is that it has Failed • We Contend Jury is Still Out Previous Research • Randomized Control Trial – Rand HI experiment (late 1970s) • Cross-Sectional Studies – Selection problem since assignment to insurance type is NOT random – Control for observables – Findings Equivocal Cancer Screenings Recommendations New Empirical Strategy Discontinuity design using age-specific preventive service guidelines – Within plan comparisons of preventive service use across guideline thresholds difference out selection effects – Guidelines are “bright lines”- Nodiscrete increase in cancer risk at these ages • U.S Preventive Task Force (USPSTF) and American Cancer Society (ACS) – Colorectal Cancer • USPSTF & ACS – Both recommend screening for individuals age 40+ • No recommendation on screening technology – Breast Cancer • ACS-Recommended mammography for women ages 40+ since early 1980s • USPSTF-Recently switched to 40+, previously 50+ • Thus we look for changes over both the 40 and 50 year thresholds – Prostate Cancer • USPSTF-Does not recommend PSA • ACS-Physicians should offer PSA • Screening is Recommended for these diseases ONLY for asymptomatic people above a certain age • IOM/ Quality Chasm report: Cancer Screenings UNDERUSED 1 Natural Experiment Framework Managed Care Preguideline Regression Discontinuity Preguideline Post Guideline FFS Managed Care FFS Post Guideline Post Guideline Post Guideline 49 49 49 A 49 B E B F 50 50 C 50 D G 50 D H H Difference-In-Difference-In-Difference = [ (D-B)-(C-A) ] – [(H-F)-(G-E)] •Diff.-In-Diff.=[(D-B)] – [(H-F)] -This assumes that [(G-E)-(C-A)] is zero, which is a plausible assumption Data Colorectal Cancer: Any Screening in Last Year by Plan and Age • National Health Interview Survey(NHIS): • National Sample of Individuals • Breast Cancer (N=6807,Years 1998-2000) • Colorectal Cancer (N=3426,Year 2000) • Prostate Cancer(N=1543,Year 2000) • Insurance Plan Types • Group/Staff Models, IPA, POS, PPO, Fee-ForService(FFS) • Rich Set of Covariates – Income, Education, Race, Region, Marital Status • Also MarketScan Data 1997-2001(these results not reported) Breast Cancer: Mammogram Use in Last Year by Plan and Age 50 45 40 35 30 25 20 15 10 5 0 F 40 35 30 25 All Group/Staff IPA FFS 20 15 10 5 0 45-47 48-49 50-51 52-54 NHIS Data-Year 2000 Breast Cancer: Mammogram Use in Last Year by Plan and Age 60 50 All Group/Staff IPA FFS 40 All Group/Staff IPA FFS 30 20 10 0 35-37 38-39 40-41 NHIS Data: 1998-2000 42-44 45-47 48-49 50-51 52-54 NHIS Data: 1998-2000 2 Regression Discontinuity Estimate using Colorectal Cancer: Means by Plan and Age Group Prostate Cancer PSA Test Use in Last Year by Plan and Age 45 Plan 40 35 30 All Group/Staff IPA FFS 25 20 15 10 5 0 45-47 48-49 50-51 52-54 NHIS DATA: Year 2000 Regression Estimates of Screening Use Plan Colorectal Mam.(35-44) Mam.(45-54) PSA GHMO -.092(.027) -.086(.042) .05(.05) -.079(.07) IHMO -.008(.021) -.055(.021) .069(.026) -.054(.036) PPO -.021(.023) -.06 (.024) .034(.030) -.01(.044) POS .001(.032) -.039(.027) .017(.034) -.038(.047) GHMO*AGRP .24(.075) .124(.065) -.012(.07) .07(.11) IHMO*AGRP .022(.029) .087(.026) -.014(.03) -.007(.048) PPO*AGRP .035(.033) .103(.03) .001(.036) .075(.065) POS*AGRP -.032(.04) .078(.037) .025(.045) -.011(.07) N 3426 6807 5629 1543 Standard Errors in parantheses. Bold indicates point estimate is significant at the 5% level. Italics means significant at the 10% level. Regression models adjust for age,sex,race, education, income,marital status, region and time where appropriate. Interpretation of Results • Change in Use across Age thresholds generally larger in Managed Care Plans – Large statistically significant differences for Colorectal and Breast Cancer screenings – No Statistically Significant differences for Prostate Cancer Screening – Strongest Results for the Group/Staff Managed Care Models GHMO (N=171) Ages45-49 Ages50-54 Diff.-In-Diff . Relative to FFS 2.3% 36% [+33.7%] - [12.9%] = +20.8% (.017) (.07) IHMO (N=1369) 12% (.014) 21% (.018) [+9%] – [+12.9%] = - 3.9% PPO (N=745) 11% (.018) 22% (.022) [+11%] – [+12.9] = -1.9% FFS (N=619) 8.8% (.017) 21.7% (.027) +12.9% POS (N=520) 13.6% (.029) 17% (.027) [+3.4%] – [+12.9] = +9.5% Results from Cross-Section Regressions Plan Colorectal Mam (35-44) GHMO .019 (.04) -.02 (.036) IHMO .003 (.02) -.009 (.02) PPO -.005 (.02) -.006 (.02) POS -.012 (.027) .003 (.02) N 3426 6807 Standard Errors in parantheses. Bold indicates point estimate is significant at the 5% level. Regression models adjust for age,sex,race, education, income,marital status, region and time where appropriate. Supply or Demand • Survey data indicates individuals don’t know the right age cutoffs • We know whether people were offered screening services in the 2000 NHIS data – Using the same framework as above we find large statistically significant changes in Offer rates across the relevant age thresholds • This indicates that supply side responses drive changes in use over the age thresholds. 3 Future Work • How does Managed Care do it? – Plan Characteristics • Health Effects • Other treatments with Age Thresholds – Ex. Cholesterol Screening 4