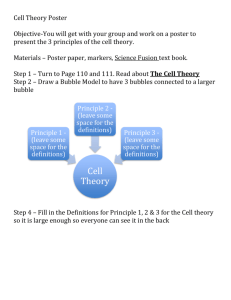
Poster Abstracts
advertisement

Poster Abstracts (in alphabetical order by presenters last name) Quality of Chronic Kidney Disease Care in Primary Care Adrienne Allen, M.D., John Forman, M.D; E. John Orav, Ph.D.; David Bates, M.D.; Bradley Denker, M.D.; Thomas Sequist, M.D. Presented by: Adrienne Allen, M.D., General Medicine Fellow, Division of General Medicine, Brigham and Women's Hospital, 1620 Tremont Street, Boston, MA 02120; Phone: (617) 525-7541; Email: aallen0@partners.org Research Objective: To evaluate the quality of chronic kidney disease(CKD) care for cardiovascular risk reduction, prevention of metabolic bone disease, and drug safety at a large multi-site group practice and to identify predictors of high quality CKD care. Study Design: We used electronic medical record data to identify patients with stages 3 or 4 CKD, defined as two recent estimated glomerular filtration rates (eGFR) between 15 and 60, separated by 90 days. We evaluated the quality of CKD care for cardiovascular risk reduction, prevention of metabolic bone disease, and drug safety (Table) for the 12 month period prior to July 2009. Drug safety was examined via electronic prescription rates of potentially inappropriate medications (NSAIDs, glyburide, metformin, nitrofurantoin) within the last 12 months. Primary care physician (PCP) awareness was measured by documentation of CKD on the electronic problem list, and nephrology comanagement was defined as a nephrology visit within the past 12 months. We fit hierarchical logistic regression models to identify predictors of appropriate CKD care after adjusting for patient age, sex, income, education level and insurance; presence of diabetes or hypertension; and clustering within clinics and PCPs. Population Studied: Primary care patients with chronic kidney disease in the metro-Boston area. Principal Findings: Among 11,760 patients treated by 166 PCPs across 15 clinics, 66% had hypertension and 29% had diabetes. PCP awareness of CKD was low (24%), and only 10% were co-managed with nephrology. Most patients were not receiving appropriate CKD care. Blood pressure control was achieved in 54% of patients; only 13% were screened for metabolic bone disease. Twenty percent had been prescribed one or more inappropriate drug within the year. Patients co-managed with nephrology were less likely to be prescribed an inappropriate drug (OR 0.77; 95% CI 0.64-0.93). PCP awareness and nephrology comanagement were consistently associated with improved effectiveness in microalbumin measurement, ACE/ARB use, and screening for metabolic bone disease. Conclusions: Significant gaps in quality of CKD care exist. These might be addressed by increasing primary care physician awareness of CKD, addressing knowledge deficits, and encouraging comanagement with nephrology. Implications for Policy, Delivery or Practice: To improve quality of CKD care, practices should consider using alerts for patients with stage 3 or 4 CKD as well as early nephrology referral. Funding Source(s): NRSA #T32HP10251-02 Poster Number: 1 Targeted Services to Improve Mental Health in the Context of Substance Abuse Treatment: Outcomes for Women with a History of Intimate Partner Violence Christina Andrews, M.S.W.; Jeanne Marsh, Ph.D. Presented by: Christina Andrews, M.S.W., Doctoral Candidate, School of Social Service Administration, University of Chicago, 969 E. 60th Street, Chicago, IL 60637; Phone: (773) 308-5123; Email: cmandrews@uchicago.edu Research Objective: Intimate partner abuse is a widespread phenomenon among women in substance abuse treatment. While prevalence estimates in the general population range from 13% to 30%, rates for women in substance abuse treatment are approximated to be much higher, spanning from 25% to 57%. Moreover, women who enter treatment with a history of intimate partner violence are more likely to develop mental health disorders stemming from abuse and trauma. Despite these statistics, little is known about the mental health services provided to this group of women. The present study responds to this gap in the literature by examining targeted services to address mental health for women with and without a history of intimate partner violence in substance abuse treatment. Study Design: Generalized linear mixed modeling was used to assess the association between receipt of mental health services and change in mental health distress from pre- to post-treatment. Interaction variables were used to test for moderating effects of intimate partner violence. Descriptive comparisons were made using chisquare tests for categorical variables, and analysis of variance (ANOVA) for continuous variables. Population Studied: The study uses data from the National Treatment Improvement Evaluation Study (NTIES), a prospective, cohort study of substance abuse treatment facilities and clients. The analytic sample consists of 1,123 women from 58 treatment facilities. Missing values were specified for these comparisons. Principal Findings: Women with a history of intimate partner violence (IPV+) had higher average levels of mental health distress than women without such a history (IPV-) at pre-treatment (p <.001) and post-treatment (p <.001). However, IPV+ women made greater reductions in mental health distress from pre-treatment to post-treatment (p <.001). IPV+ women were significantly more likely than IPV- women to receive mental health services (89% v. 67%, p <.001). Yet, receipt of mental health services was associated with similar improvement in mental health for all women who received them (p =.010); no interaction between mental health service receipt and IPV status was found (p =.601). Conclusions: In this sample, women with a history of intimate partner violence entered treatment with high levels of mental health distress, and the vast majority received mental health services. Over the course of treatment, women with a history of intimate partner violence made greater reductions in mental health distress than women without such a history. Receipt of mental health services is likely to have played a role in their improvement—receipt of such services was associated with significant reductions in mental health distress for all women who received them. Implications for Policy, Delivery or Practice: The study findings suggest that women with a history of intimate partner violence are more likely than women without such a history to need, use and benefit from mental health services within the context of substance abuse treatment. To assist women with a history of intimate partner violence to recover from addiction, providers should strive to offer mental health services in tandem with substance abuse treatment. Funding Source(s): NIDA Poster Number: 2 The Non-Physician Clinician Workforce of Nebraska Bettye Apenteng, B.Sc.; Keith Mueller, Ph.D.; Preethy Nayar, Ph.D. Presented by: Bettye Apenteng, B.Sc., Student, Health Services Research and Administration, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198; Phone: (206) 291-3132; Email: bapenten@unmc.edu Research Objective: To examine the demographic characteristics and practice location of nurse practitioners (NPs) and physician assistants (PAs) practicing in the state of Nebraska in 2008. Study Design: The study is a cross-sectional descriptive analysis of the 2008 University Of Nebraska Medical Center’s Health Profession Tracking Service survey data on nurse practitioners and physician assistants in Nebraska (N = 1175). Health Professional Shortage Area (HPSA) designations and the 2003 Federal Office of Management and Budget definition of metropolitan counties were used to characterize practice location and rural/urban location of practice. Population Studied: All Non Physician Clinicians (NPCs) or mid-level providers (Physician Assistants and Nurse Practitioners) actively practicing in the state of Nebraska in 2008. Principal Findings: Physician assistants and nurse practitioners in Nebraska are predominantly female and Caucasian with 66.5% of mid-level providers practicing in urban areas. Despite the fact that training programs for mid-level providers were originally inspired by the need to fill in gaps in primary care delivery, only 48.9% of Nebraska’s mid-level providers are in primary care. Of those who opt for specialty care, only 10.6% take up practice in mental health. A higher proportion of NPs are females, compared to PAs (92.6% vs. 61.0%). PAs in Nebraska are younger than NPs, (42yrs vs. 47yrs) and this is true for both primary care and specialty care, except for mental health. Among mental health mid-level professionals, there is no difference in the average age between the two professions. Psychiatric mid-level providers tend to be older than other mid-level providers (53yrs vs. 44yrs). Among primary care mid-level providers, a higher proportion of PAs than NPs practice in a non-metro location (? = 0.005). Also, a higher proportion of male mid-level providers practice in a non-metro area compared to female mid-level providers ((? = 0.01). In specialties other than primary care however, no association is seen between gender, license type and practice location. Over half of psychiatric mid-level providers (54.7%) practice in federally designated mental health HPSAs. Only 14.8% of Nebraska’s primary care mid-level providers practice in HPSA designated single counties, geographic areas, rural clinics, health centers and clinics serving special populations. These providers however, serve 39 of the 51 designated HPSA counties in Nebraska. Conclusions: There is a shift in interest, away from primary to specialty care as well as the preference for urban practice, this could serve as a threat to effectively addressing primary care and mental health access issues in underserved and rural areas. Implications for Policy, Delivery or Practice: Assessment of the demographic characteristics and practice location of NPCs as presented is crucial in workforce planning. The willingness of PAs and males to practice in rural areas should be factored into strategies for the recruitment and retention of health care professionals to rural areas. Policy should also address the lack of an adequately sized and aging mental health workforce. Poster Number: 3 Medicare Advantage Extra Payments in 2010 Grace Arnold, B.A.; Brian Biles, M.D., M.P.H. Presented by: Grace Arnold, B.A., Research Assistant, Department of Health Policy, George Washington University, 2021 K Street, NW, Suite 800, Washington, DC 20036; Phone: (202) 9944203; Email: gca@gwmail.gwu.edu Research Objective: Over the past decade, Medicare Advantage (MA) payment policy has shifted from one which encourages private plans in areas where they can provide benefits more efficiently than fee-for-service (FFS) Medicare to one which encourages plans in all areas of the country. In order to encourage plans in all areas of the country to participate in the MA program, plans in some areas are paid more than Medicare FFS costs. President Obama and Congressional leaders have argued that this is wasteful spending and eliminating these overpayments to MA plans was a major source of Medicare savings to make health reform legislation deficit neutral. We quantified overpayments to Medicare private plans in 2010 by geographic area and legacy benchmark category. Study Design: County-level payment benchmarks, enrollment and penetration data were downloaded from the Center for Medicare and Medicaid services website in November, 2009. Enrollees in Medicare "cost" and private fee-for-service (PFFS) plans were not included in the analysis. County-level payments were calculated by applying MedPAC's analysis of average bids in relation to FFS costs to county-level benchmark data in order to estimate bids. Seventy-five percent of the difference between the benchmark and the estimated bid was added to the bid to account for the Medicare rebate in the final payment figure. Average payments for geographic areas are enrollee-weighted. Population Studied: Medicare Advantage plan enrollees and Medicare beneficiaries Principal Findings: Nearly 10 million Medicare beneficiaries in the US participate in the MA program in 2010. Nationally, Medicare will pay plans more than $7 billion and an average of 110% more than local FFS costs in 2010. Counties that are paid at the legacy urban floor are home to 43% of MA enrollees and will receive 54% of the total national overpayments. Plans in these counties are paid an average of 114% of local FFS costs. Counties paid at the legacy floor of 100% of 2004 FFS costs will receive 28% of over payments and are home to 33% of plan enrollees. Plans in these counties are over paid an average of 108% of local FFS costs. Counties paid at the legacy blend benchmark are paid an average of 118% of FFS costs and those receiving a minimum payment update are paid at 116% of FFS costs. Conclusions: Medicare Advantage plans continued to receive payments in excess of Medicare FFS costs in 2010. The amount and distribution of extra payments varied with geographic area and county benchmark type. Implications for Policy, Delivery or Practice: If health reform legislation is enacted, the elimination of overpayments will have a significant impact on the MA program. This analysis will provide a baseline against which the effects of health reform will be measured. Funding Source(s): CWF Poster Number: 4 Why Do Individuals Receive Acupuncture: A Cross Sectional Analysis Based on U.S. Adult Sample? Shamly Austin, M.H.A., Ph.D ; Zo Ramamonjiarivelo, M.B.A.; Richard Shewchuk, Ph.D. Presented by: Shamly Austin, M.H.A., Ph.D. Candidate/Graduate Research Assistant, Department of Health Services Administration, University of Alabama at Birmingham, 1320 11th Ave South, Birmingham, AL 35205; Phone: (225) 252-8650; Email: shamly@uab.edu Research Objective: Over the years, the use of complementary and alternative medicine (CAM) has increased in the U.S from 36% in 2002 to 38.3% in 2006. Acupuncture is considered as a type of CAM with its origin in the traditional Chinese medicine. An estimated 3.1 million adults used acupuncture in 2007. Previously no studies analyzed the reasons for the use of CAM. Our study examines the reasons for the utilization of acupuncture services among U.S adults. Study Design: A cross sectional analysis was done based on 2007 National Health Interview Survey. The analysis includes 1,532 U.S adults who have reported the use of acupuncture services in their lifetime. The variables were recent visits measured as “saw a provider for acupuncture during the last 12 months”, reasons for the use of acupuncture, and socio-demographic variables including age, race/ethnicity, sex, education, and income. Univariate and bivariate analyses were performed to analyze the reasons for utilization of acupuncture services. Population Studied: Non-institutionalized U.S civilian population >=18 years, who reported the use of acupuncture services. Principal Findings: Of the 23,393 adults who completed the survey on alternative health questionnaire, 6.5% (n=1,532) reported use of acupuncture in their lifetime. Of these 1,532 individuals, 22.5% (n=344) reported recent use of acupuncture services, 64 % were females, 38% resided in the West, and 27% in the South, 65% were Whites, 14 % Hispanics, and 11% Asians, 78% were <65 years old, 45% were married, 43% had > high school education. 47% reported arthritis and body pain as the specific health condition for which they used acupuncture. The major reason for use was recommendations from family and friends (21%). This was followed by the belief that conventional medical treatment was of no help (20%), and another 20% used it for general health/wellness, 12% used it as it was recommended by their health care provider, and another 11.8% used it to enhance energy level. 10.4% used it to enhance immune function, and 4.6% felt that conventional medical treatment was too expensive. Additional analysis was done to determine whether reasons for acupuncture use were different for both sexes. Female responses indicated that the major reason for acupuncture use was that conventional medical treatment was of no help to them in curing illness (20%), and another 20% were recommended by their family/friends, followed by 19.5% reporting general health and wellness as the reason for use. Among men, the major reason for use was recommendation from family/ friends (24.5%), followed by general health/wellness (21.6%), and 19.6% used it as conventional medical treatment was of no help to them. Conclusions: The major reason for acupuncture use was recommendations from family/friends followed by the reason that conventional medicine was of little help. Implications for Policy, Delivery or Practice: The study helps to understand the reasons for emerging migration of individuals from conventional medicine to CAM and may be helpful for health insurers to make decisions on expansion of coverage to CAM users. Poster Number: 5 Physician Self-Referral of MRI and Care for Patients with Low Back Pain Jacqueline Baras, M.D., M.S.; Laurence Baker, Ph.D. Presented by: Jacqueline Baras, M.D., M.S., Medical Student, School of Medicine, Stanford University, 1070 Mercedes Avenue Apartment #11, Los Altos, CA 94022; Phone: (727) 742-8229; Email: jbaras@stanford.edu Research Objective: Physician self-referral of advanced imaging such as magnetic resonance imaging (MRI) is increasingly common. While selfreferral offers convenience and better continuity of care for patients, such arrangements produce strong financial incentives for physicians to order MRI scans that may not be necessary or appropriate. Additional scans may influence treatment patterns and total costs of care, but the size of the impact is uncertain. This paper investigates the relationship between physician selfreferral, use of MRI, receipt of surgery, and total spending for patients with low back pain. Study Design: Panel data difference-in-difference analysis, comparing changes in treatment patterns of self-referring physicians before and after they begin self-referring to changes in treatment patterns of non-self-referring physicians over the same time period. We use claims from a 20% sample of traditional Medicare beneficiaries to identify nonradiologist physicians who see low back pain patients and appear to begin self-referral arrangements for MRI between 1999 and 2005, as well as their patients who have a new episode of low back pain care during this time. We also identify episodes of low back pain treatment with physicians who never self-refer for MRI. For each episode, we track use of MRI, use of back surgery, and total Medicare spending associated with low back care claims, including all Medicare payments for physician, inpatient, and outpatient claims. We use regression analysis to identify changes in use of MRI, use of surgery, and spending for episodes before and after physicians begin self-referring, using episodes with non-self-referring doctors to control for overall time trends. The regressions also adjust for an array of demographic and socioeconomic covariates and include month, year, and physician fixed effects. Population Studied: 487,234 ninety-day episodes of care for low back pain among fee-for-service Medicare patients over age 65, associated with 79,971 physicians. Principal Findings: Physicians ordered more MRI scans for their patients with low back pain once they began to engage in self-referral of MRI. The unadjusted average of MRI procedures billed within 90 days increased from 11.4 per 100 episodes before self-referral to 16.3 per 100 episodes with self-referral; non-self-referring physicians ordered MRI considerably less often, at an average of 7.0 MRI scans per 100 episodes. These additional scans are statistically significantly associated with increases in surgery receipt and low backassociated spending. After stratification on physician specialty, the effect of self-referral of MRI was strongest among orthopedic surgeons and weakest among primary care physicians. Conclusions: Non-radiologist physicians who participate in self-referral arrangements of MRI appear to change their practice patterns and order more MRI scans for patients with low back pain. These increases in MRI use lead to increases in surgery receipt and total low back-related spending, but the strength of this effect varies widely across physician specialty. Implications for Policy, Delivery or Practice: Initiatives aimed at strengthening prohibitions on physician self-referral have the potential to influence overuse of care and spending, particularly if they address self-referral among subgroups of physicians and patients. Funding Source(s): Stanford University, California HealthCare Foundation Poster Number: 6 Qualitative Research and Racial Disparities in Screening Behaviors: Understanding Barriers and Facilitators of Colorectal Cancer Screening Arden Morris, M.D., M.P.H.; Elizabeth Becker, M.P.H.; Heather Elliott, B.A.; Gwen Alexander, Ph.D.; Derek Griffith, Ph.D. Presented by: Elizabeth Becker, M.P.H., Doctoral Student, Health Behavior/Health Education, University of Michigan School of Public Health, 1415 University Heights, Ann Arbor, MI 48109; Phone: (612) 590-1431; Email: eabecker@umich.edu Research Objective: Relative to Whites, African Americans with colorectal cancer experience a 20% higher cancer-specific mortality rate; however, even among patients with medical insurance, African Americans are less likely than Whites to undergo colorectal cancer screening. Traditional theoretical models of the risk-screening relationship may miss patients who delay or avoid screening for colorectal cancer in spite of their clinical status as high risk. Our objective was to understand racial differences in decision making factors around colorectal cancer from the patient’s perspective, and to create a new framework for understanding how African Americans make decisions regarding colorectal cancer screening. Study Design: Using trained race-concordant interviewers, we conducted semi-structured interviews with a convenience sample of 29 individual African American and White patients who had undergone colorectal cancer surgery. Population Studied: White and African American colorectal cancer surgery patients at a major urban hospital. Principal Findings: Thematic analysis of the data suggested a wide range of influences on patients’ screening behaviors. While some patients were proactive in the face of increased risk, others were not, despite high levels of social support and adequate insurance and access to care. Patients exhibited a wide range of patterns of interactions among relevant factors including social support, medical insurance, access to care and disease risk. These patterns differ from those established in the literature and that have informed screening interventions to date. For example, in contrast to established beliefs, some patients equated disease presence with illness, and failed to follow screening guidelines because they felt healthy. Others report delays in screening due to the burdens of other medical conditions, fearing both the screening procedure itself as well as facing yet another disease. Conclusions: Patient accounts of their decision making processes surrounding screening behaviors vary dramatically, suggesting the need for a multifaceted approach to screening promotion. Traditional models of decision making may not be adequate to capture the broad range of factors involved, as revealed by the qualitative data in this study. Neither risk, social support, access to care nor insurance has as strong of an influence on decision making as what the literature suggests. Using these data, we propose an alternative model of screening behavior in both low and high risk individuals accounting for variation within and between racial groups as well as commonalities across the study population. Patient accounts of their own decision making behaviors offer a unique lens through which to examine this process, and can help institutions and practitioners tailor their screening promotion messages. Implications for Policy, Delivery or Practice: To effectively address health and health care disparities, we need to understand underlying mechanisms of decision making and behavior. Utilizing qualitative research methods can help shed light on the ‘black box’ of decision making processes that patients undergo as they consider the burdens and benefits of colorectal cancer screening. Funding Source(s): American Cancer Society Poster Number: 7 Relation of Health Insurance to Weight Status Jean Bernhardt, Ph.D., M.S.N. Presented by: Jean Bernhardt, Ph.D., M.S.N., M.H.S.A., Student, University of Massachusetts; Phone: (978) 465-3989; Email: jbernhardt@partners.org Research Objective: The major purpose of this study was to examine the relationship of health insurance to weight status in 19-26 year olds using body mass index (BMI) as the surrogate measure of body weight. It was hypothesized that having health insurance would predict lower BMI. The study was conceptualized within an adapted social-ecological framework with eM.P.H.asis on the interactions of individuals and their environments. Study Design: This secondary data analysis study included data from 3804 young adults in the 2004 Medical Expenditure Panel Survey. Multivariate logistic regression analyses (using STATA 8.0) tested a non-recursive causal/path analytic model and structural equations to explain the likelihood of being obese (BMI=>30kg/m2). Youths’ race, gender, and education, along with parental education and obesity, were primary explanatory variables. Being on a restricted diet was considered a response to being obese. Sensitivity analysis was conducted on causal effects of BMIs >35 kg/m2. Population Studied: 19-26 year old young adults with private or public health insurance Principal Findings: Being Black (OR 1.90, CI 1.46, 2.48), having a high school diploma or less (OR 2.07, CI 1.40, 3.07), with at least one obese parent (OR 1.99, CI 1.36, 2.92), all significantly increased the probability of being obese. Physical activity (OR 0.59, CI 0.47, 0.73) reduced obesity likelihoods but was less common in females and minorities. Private insurance was associated with lower BMIs yet was statistically insignificant (OR 0.82, 0.63, 1.05) whereas young adults on public insurance (OR 1.40, CI 1.01, 1.95) had higher BMIs, suggesting unobserved differences in socioeconomic status related to type of insurance. However, at BMIs greater than or equal to 35 kg/m2, private insurance (OR 0.57, CI 0.38, 0.86) was negatively associated and statistically significant at influencing lower BMI levels. Conclusions: Insurance is a complex measure which reflected unmeasured characteristics associated with the type of insurance individuals had. Most importantly, having insurance did not offset unmeasured factors that contributed to being obese for those with public insurance. Implications for Policy, Delivery or Practice: Targeting health education to mitigate obesity, prevent future intergenerational transfer of obesity, and address the factors associated with obesity and public insurance in young adults may be effective. Understanding the relationship of health insurance to weight status in young adults has the potential to inform and guide public and health policy decisionmaking related to the utility of insurance to address the epidemic of obesity and support clinical interventions. Poster Number: 8 The Hidden Beneficiaries: Population Characteristics, Health Care Cost, and Health Care Access for the Five Subpopulations Within Medicare Liz Blodgett, M.H.P.A. Presented by: Liz Blodgett, M.H.P.A., Graduate Research Assistant, Health Policy and Administration, Washington State University, PO Box 1495, Spokane, WA 99210; Phone: (509) 9533667; Email: lizblodgett@wsu.edu Research Objective: The objective of this study is to assess variation in population characteristics, healthcare cost, and healthcare access for Medicare beneficiaries in 2007 divided both by eligibility and age. Study Design: This study was a secondary data analysis of the Medicare Current Beneficiary Survey 2007 Access to Care database. Beneficiaries were sorted into one of five groups by entitlement and age: end-stage renal disease-eligible beneficiaries under 65, ESRD over 65, Social Security Disability Insurance-eligible beneficiaries under 65, formerly SSDI-eligible beneficiaries over 65, and retirees. Group classification served as the independent variable.Dependent variables were derived from the MCBS Access to Care Codebook and grouped into four major areas: population characteristics, health and disability status, coverage and access, and cost. Population Studied: Full-year Medicare beneficiaries interviewed in the 2007 Medicare Current Beneficiary Survey. Principal Findings: The groups were found to differ significantly (p<.001) on population measures including race/ethnicity, income level, education level, and urban vs. rural residence; health and disability status measures including number of chronic conditions, number of ADLs, self-rated health status, rates of diagnoses for mental disorders and depression, and BMI; coverage and access measures including rates of dual eligibility, enrollment in Medicare HMOs and Medicare Part D, and rates of reporting trouble accessing healthcare or delaying care due to cost; and annual healthcare expenditures. This study found that former SSDI beneficiaries over age 65 - like younger SSDI beneficiaries - are sicker, poorer, and more likely to experience cost and access problems than retirees. These results suggest that Medicare population comparisons based on age or eligibility alone are overlooking major subpopulation differences. Conclusions about ESRD beneficiaries both under and over age 65 were limited due to small sample size. However, these beneficiaries have high rates of comorbidity, poor self-rated health, and the highest healthcare costs of any Medicare subpopulation. For example, ESRD beneficiaries had significantly higher annual levels of inpatient reimbursement than SSDI beneficiaries of any age or retirees; on average, $21,991 for ESRD under 65 and $10,291 for ESRD over 65 as compared to $2,239 for SSDI under 65, $3,233 for SSDI over 65, and $2,179 for retirees. Conclusions: In differentiating Medicare subpopulations, researchers and policymakers traditionally contrast younger and older beneficiaries. This division neglects the fact that younger beneficiaries become older beneficiaries and remain within the program. When subsumed into the category of older beneficiaries, the cost and use patterns of these sicker, poorer beneficiaries may actually obscure the true degree of difference between retirees and younger SSDI beneficiaries. Implications for Policy, Delivery or Practice: The health and population characteristics of SSDI beneficiaries over age 65 make them more reliant on Medicare than retirees, and therefore more vulnerable to policy changes that restrict or reduce coverage. As healthcare reform affecting Medicare is enacted, policymakers should consider the needs of these beneficiaries carefully. Medicare beneficiaries with ESRD are typically removed from comparisons entirely, due to their relatively small numbers. However, the exceptionally high cost of this subpopulation suggests that they have a disproportionate impact on Medicare relative to their population size. Funding Source(s): National Institute on Disability and Rehabilitation Research Poster Number: 9 Making Sense of Online Patient Conversations Karen Born, B.A., M.Sc.; Carlos Rizo, M.D.; Neil Seeman, L.L.B., M.P.H. Presented by: Karen Born, B.A., M.Sc., Ph.D. student, Health Policy, Management and Evaluation, University of Toronto, 155 College Street West Suite 425, Toronto, M5T3M6; Canada; Phone: (416) 710-2018; Email: karen.born@utoronto.ca Research Objective: To listen to patients' stories online to complement current approaches to gathering patient satisfaction data. Understand how listening to patients' stories through online social media can be part of the quality improvement process of health care organizations. Test the implementation of best practices in social media at health care provider organizations and understand the organizational context in which these practices are being implemented. Study Design: The study includes an environmental scan of organizations within and beyond healthcare who use social media to listen to clients and customers. Next, case studies will be developed using organizational partners. Case studies will glean data through online reviews of patient and public-generated data, as well as interviews with senior leaders. Population Studied: Health care organizations within Ontario. Current partners include a rehabilitation organization, a division of the Ontario Ministry of Health and Long-Term care and potential a mental health and addiction health care provider. Principal Findings: Preliminary research of patient data online has found that patients express their satisfaction with care providers through online forums. Organizations who 'listen' to these online voices can feed this information into quality improvement cycles. Organizations, however are cognizant of risk management and have concerns about the privacy and influence of social media forum. Patient conversations online, however, can be measured and tools used in this study demonstrate the influence and penetration of these conversations. Conclusions: Case studies developed will test emerging best practices and guidelines on quality improvement and patient-centred care using social media. Case studies will also detail organizational journeys in using this kind of information to inform quality improvement, and will describe the barriers, enablers and challenges in this journey. Implications for Policy, Delivery or Practice: This work will inform the development of an eToolkit, aimed at sharing insights and lessons from patient and caregiver stories online and offers ideas and guidance to other care providers on how to leverage online patient data to support organizational improvement. Funding Source(s): The Change Foundation Poster Number: 10 Patient- and Family-Centered Care - The Impact on Patient Safety: A Comparison Study of Intensive Care Units at an Academic Medical Center Barbara Brumbaugh, M.P.H., Patricia Sodomka, M.H.A.; Janice Probst, Ph.D. Presented by: Barbara Brumbaugh, M.P.H., Health Services Policy and Management, University of South Carolina-Arnold School of Public Health, 122 Twin Creek Farm Road, Aiken, SC 29805; Phone: (803) 640-7763; Email: blbrumbaugh@bellsouth.net Research Objective: Patient- and Family-Centered Care (PFCC) was called out by the Institute of Medicine in 2001 as one of the six aims in improving the quality of health delivery. Despite the fact that there is growing recognition that this model of care results in better outcomes, decreased costs, and greater clinician and patient/family satisfaction, there is still limited research that demonstrates these results. This study examines performance and patient safety measures and outcomes in Adult ICUs at an academic medical center. Study Design: Data was mined from the University HealthSystem Consortium (UHC), Clinical Data Base (CDB). The first study cohort, n=705, was derived from the General Neurology and Neurosurgery Product Line and the second study cohort, n=440, from all other product lines excluding general neurology, neurosurgery and pediatrics. Using these cohorts facilitated comparisons of outcomes for patients in the Neurosciences ICU with those for patients in the Shock Trauma ICU. To acknowledge and to better address the remaining differences in the study populations in these two intensive care units, UHC data were used to compare the observed outcomes in each of the two populations to outcomes predicted by UHC models for those specific populations. Length of stay (LOS), expected LOS per Medicare Severity Diagnosis Related Group (MS DRG) observed costs (calculated using costs to charge ratios), expected costs per MS DRG, potentially avoidable postprocedure complications, and safety indicators were analyzed by statistical methods, examining and comparing frequency, mean, and other measures utilizing SAS version 9.2. P values less than or equal to 0.05 were considered statistically significant. Population Studied: The target population was all adult patients discharged between January 1, 2007 and December 31, 2007 at MCGHealth with 1 to 75 ICU days and attesting physician specialty of neurology, neurosurgery, or trauma. Principal Findings: Costs compared to expected costs per MS DRG were less for patients spending time in the Neurosciences ICU. The observed LOS as compared to the expected LOS was found to be less for patients having stays in the Neuroscience ICU as compared to patients having stays in the Trauma ICU. Patients in the Neurosciences ICU experienced fewer complications than those in the Trauma ICU. Patients in the Neuroscience ICU had less safety issues relative to the AHRQ safety indicators than those in the Trauma ICU. Conclusions: This study suggests that Patientand Family-Centered Care has a positive effect on performance measures such as LOS and costs for ICU patients. It further suggests that patients receiving PFCC experience less complications and safety issues than those patients who stayed in units where PFCC is not universal. Implications for Policy, Delivery or Practice: While further research is needed this area, the findings strongly suggest that the patient- and family-centered care model should be implemented across the continuum of healthcare, even in the ICU to improve patient safety and reduce costs. Poster Number: 11 Growing Old Together? Exploring the Relationship Between Social Capital and Nursing Home Institutionalization among Elderly in the United States Rebecca Cadigan, M.Sc. Presented by: Rebecca Cadigan, M.Sc., Graduate Student, Health Policy Ph.D. Program, Harvard University, 14 Story Street, 4th Floor, Cambridge, MA 02138; Phone: (617) 484-0848; Email: rcadigan@fas.harvard.edu Research Objective: As Americans live longer, elders experience increasingly diverse long-term care needs. While people with significant impairments require the prosthetic physical environment and around-the-clock medical monitoring of a nursing home (NH), many people with lesser impairment can remain in their homes with minimal support. Past research has shown that there are numerous social and economic benefits to allowing elders to select long-term care services that enable aging-in-place. Home and communitybased services have the potential to allow elders to receive care while preserving ties with family, friends, and neighbors, and maintaining connections to religious institutions, social groups, and other community organizations. While social integration is a well-studied correlate of healthy aging at the individual-level, less is known regarding the relationship between area-level social capital and patterns of long-term care utilization. The objective of the present study is to explore the relationship between social capital and risk of institutionalization of elderly across all U.S. counties. It is hypothesized that areas with lower levels of social capital will have higher rates of elders admitted to nursing homes unnecessarily (referred to as “low-care”). This hypothesis is based on the theory that areas with higher levels of social capital are more likely to have resources that allow elders to age in place, such as active civic groups, robust religious communities, accessible transportation networks, generous social services, safe neighborhoods, and opportunities for volunteerism. Study Design: The percentage of low-care NH residents in each county was obtained from Brown University’s Long-Term Care: Facts on Care in the U.S. Website. County-level social capital data were obtained from the Northeast Regional Center for Rural Development. The addresses of all licensed NHs were obtained from the Centers for Medicare and Medicaid Services Nursing Home Compare database, and geocoded using ArcGIS. Univariate and multivariate linear regression were used to explore the relationships between social capital indicators and prevalence of low-care NH residents by county. Maps were created using ArcGIS to depict the geographic variations in social capital and prevalence of low-care NH residents across the U.S. Population Studied: The population of interest is person over age 64 residing in the U.S. The unit of analysis for the present study is all U.S. counties. Principal Findings: Number of civic and professional organizations per capita were both inversely associated with percentage of low-care NH residents at the county-level, controlling for median income, proportion of the population over age 65, and population density. This suggests that counties with a greater relative number of civic and professional organizations have significantly lower rates of unnecessary NH admission. It is unclear whether the aging-in-place of elders is contributing to higher social capital in these areas, or if elders living in communities well endowed with social capital are less likely to enter NHs unnecessarily. It is also possible that there are exogenous factors mitigating these relationships. Conclusions: Several social capital indicators were associated with prevalence of low-care NH residents at the county level, namely number of civic and professional organizations. This suggests that there may be area-level predictors of aging-inplace, and further research is needed to identify the direction and mechanisms of these relationships. Implications for Policy, Delivery or Practice: The identification of area-level characteristics associated with prevalence of low-care NH residents may help to inform policy decisions regarding long-term care services and financing. Funding Source(s): AHRQ Poster Number: 12 State’s Budget Cut Matters for Uncompensated Care Spending? JongWha Chang, M.A., M.S.P.H.; SunJung Kim, B.S.; Isha Patel, M.S.; Rajesh Balkrishnan, Ph.D. Presented by: JongWha Chang, M.A., M.S.P.H., Graduate Fellow, Social and Administrative Science, The University of Michigan at Ann Arbor, 428 Church Street, Ann Arbor, MI 48109; Phone: (734) 936-1505; Email: jochang@umich.edu Research Objective: The study examined the impact of state budget cuts on uncompensated care of general acute care hospital organizations. This study capitalized on the variations in the state of Texas, and California to form a natural experiment testing the joint impact of budget cut status on uncompensated care costs, as well as specific charity care costs and bad debt expenses from indigent patients. Study Design: The budget cuts in the state of Texas occurred in the year 2004. Information was obtained from the Texas Department of Health (TDH) and California Department of Health Services (CDHS) regarding financial characteristics of hospitals, and the American Hospital Directory (AHD) annual survey regarding hospital organizational characteristics. We created three dependent variables; RUCGPR (the ratio of the total uncompensated care costs to gross patient revenue), RCHRGPR (the ratio of charity care to total patient revenue), and RBDGPR (the ratio of bad debt expenses to gross patient revenue). Using a two-period panel data and individual hospital fixed effects, we captured hospital uncompensated care spending that could also have influenced budget cut status. Additionally, the impact of the state budget cut status on hospitals’ uncompensated care spending, charity care spending, and bad debt expenses were also similarly estimated. Population Studied: The number of public, not for profit and for profit hospitals who completed the annual survey in the sample periods, 2002-2005 [416 (Texas) and 352 (California)]. Principal Findings: For state of Texas, results from the fixed effects model confirmed that the year 2005 was directly related to increasing RUCGPR, and RCHRGPR. The coefficients of year dummy of 2005 were significantly and positively associated with RUCGPR (0.4282, p-value <0.05) and RCHRGPR (0.29, p-value <0.1). These results support the findings that the RUCGPR (RCHRGPR) would be more positively associated with 2005 than any other year with other things being equal. However, for the state of California, even though the coefficient of year dummy of 2005 was significant and positively associated with RCHRGPR (0.319, p-value <0.05), the overall coefficient of uncompensated care spending was not statistically significant for 2005. Conclusions: The healthcare industry is characterized by increased regulation, a growing number of uninsured patients, increasingly stringent reimbursement, and competitive practices among hospitals and other providers. Federal and state healthcare agencies are increasing the standards of eligibility for outlier payments and uncompensated care provisions. Tax exempt status of many NFP hospitals is being examined and tied to specific performances, particularly the provision of uncompensated care. This study provides empirical evidence of the impact of budget cut status as reported by Texas and California general acute care hospitals. Characteristics of those hospitals using RUCGPR, RCHRGPR, RBDGPR ratios and other market factors are presented and analyzed. Implications for Policy, Delivery or Practice: This study contributes to prior healthcare finance research for hospitals’ uncompensated care spending as impacted by state regulations. This study finds that if the state has budget cut crisis at specific period, RUCGPR and RCHRGPR significantly impact the budget cut crisis in the same direction. However, if state does not have budget cut crisis at specific period, RUCGPR and RCHRGPR do not significantly impact the budget cut status. The study finds that there is evidence to support hypothesis that the state budget cuts reduce the levels of uncompensated care. Funding Source(s): The University of Michigan at Ann Arbor, College of Pharmacy Poster Number: 13 Shopping Behavior of Colon and Rectum Cancer Patients for Health Care Services Ruei-Yi Chang; Chih-Liang Yaung; Shang-Jyh Chiou, Ph.D. Presented by: Ruei-Yi Chang, Student, Healthcare Administration, Asia University, 500, Lioufeng Road, Wufeng, Taichung 41354, Taiwan; Phone: +8864233234561742; Email: j76926@hotmail.com Research Objective: Shopping behavior for healthcare services is a special phenomenon in Taiwan because patients have moderate accesses to low costing healthcare under the National Health Insurance (NHI) program. The malignant tumor in colon and rectum cancer has occupied the 3rd place as cause of death since 1995. The mortality rate of colon and rectum cancer was 14.2/10000 in 1999, female had higher rate. The goal of this study was to investigate the status of shopping behavior for healthcare services of newly diagnosed colon and rectum cancer patients. Study Design: The study used the cancer dataset from National Health Research Institutes (NHRI) which included all claim information, registry for contracted medical facilities and registry for beneficiaries in 2006. The definition of shopping behavior in this study is defined as inquiring into the services more than 2 providers for test and confirmation before the regular treatment in the first time which determined from the surgical code (V57, V58), radio therapy and chemotherapy. Population Studied: New cases of colon and rectum cancer were extracted using the Principal Diagnosis of ICD-9-CM codes 153-154 and A-code A093 and A094, with no relative diagnosis record before 13 months from the cancer dataset. There were 2,580 cases in this study. Principal Findings: There were 139 cases fit the definition of shopping behavior, male was 44.6% (n=62). The majority was 40~64years old (56.12%). The average duration of shopping behavior was 165 days as compared to 72 days from those who did not. The average times of visits were 25, and those who did not were 7. The average medical expenditures of shopping and not shopping behavior were US$2,842 and $730, respectively. The average number of hospital visiting was 3.44. Most cases occurred in medical centers because they believe that medical center can offer reliable services. Conclusions: This study finds that shopping behavior incurs extraordinary expenses and is a torment problem for NHI in Taiwan when the cost control pressure roars with years. Those patients also take high risk in the delaying cancer treatment especially the better prognosis in the regiment beginning early. Implications for Policy, Delivery or Practice: Further investigations need to explore the impact factors related to the shopping behavior. More research needs to realize the relevant factors either from providers or patients and the influence to the survival rate. Funding Source(s): Asia University Poster Number: 14 Suicide Mortality Trends by Sex, Age, Methods, Season and Region in Taiwan, 1986-2007 Wei-ting Chang, M.S ; Chien Wu Chien, Ph.D. Presented by: Wei-ting Chang, M.S, Graduate, Public Health, Natinal Defence Medical Center, No.161, Section 6, Min-Chuan East Road, Taipei, 114 Taiwan; Phone: +886287923100; Email: moyen1985@msn.com Research Objective: To examine the trends in suicide mortality in Taiwan by sex, age, methods, season, and region between 1986 and 2007. Study Design: Analysis of routine mortality data from the official publications of vital statistics from 1986 to 2007 to determine trends by sex, age, method, season and region. Linear regression was used to test the trends. Population Studied: Population base Principal Findings: A total of 47,148 people in Taiwan died as a result of suicide between 1986 and 2007, and 66.65% of them were males. Hanging was the most common method of suicide, especially among more than 65-year-old elderly. However, the most common method of suicide among 25-49 year of age was poisoning by other gases and vapors. In one year, May to September were higher months of suicide mortality rate. During study period, suicide mortality rate of Taitung County was the highest and decreased, but Nantou County, Koahsiung City and Keelung City increased. Conclusions: Total suicide mortality rate rose, and male was higher than female. Suicide mortality rate of middle age increased significantly. Methods of suicide changed from poisoning by solid or liquid substances into jumping from high place and poisoning by other gases and vapors. Implications for Policy, Delivery or Practice: The prevention programs should focus on male and who suicide by jumping from high place and poisoning by other gases and vapors. Poster Number: 16 The Impacts of Depression and Anxiety on Elderly COPD Patients in Taiwan Ling-hsuan Chang; Ying-Chun Li, Ph.D. Presented by: Ling-hsuan Chang, Graduate Student, Institute of Health Care Management, National Sun Yat-Sen University, 70 Lien-Hai Road, Kaohsiung, 804 Taiwan; Phone: +88675252000 ext. 4870; Email: ksamuel0917@gmail.com Research Objective: Chronic obstructive pulmonary disease (COPD) is a major cause of disability and death worldwide. The prevalence of depression and anxiety in COPD patients is generally higher than those reported in other chronic illnesses, and these mental diseases significantly affect the health expenditures and the course of the diseases on elderly COPD patients. The COPD patients with co-morbid depression, anxiety or other chronic diseases are more impaired and have 50% to 100% higher medical costs than those without depression and anxiety. COPD affects approximately 1.8 million people in Taiwan every year, however, little studies have examined the impacts of mental diseases on elderly COPD patients. This study aims to investigate the depression and anxiety status on COPD patients’ medical care utilizations and health outcomes. Study Design: This study analyzed the nationally representative research database from National Health Insurance program between 2002 and 2006 in Taiwan, by exploring outpatient visits, hospitalizations, and medical expenditures of COPD and its associated co-morbidities. The data analyses were carried out by Chi-square test, multiple linear regression and multivariate logistic regression. Population Studied: Patient aged over 65 with primary diagnosis of COPD and co-morbidity diseases based on ICD-9-CM in Taiwan. To investigate the complications in COPD patients, four diseases such as diabetes, hypertension, heart failure and ischemic heart disease were included in the analyses. Principal Findings: Among the 131,846 COPD patients (63.3%, male), most of them were aged from 65 to 84 (65.9%) and lived in northern Taiwan (44.8%). The results indicated that those who were suffered from depression or anxiety increased medical utilization and costs. Multiple linear regression model showed that age, locations, and hospital level significantly affect the health expenditures of COPD patients with depression or anxiety (p<0.001). Multivariate logistic regression model presented that length of stay in hospital and number of complications significantly affect the probability of hospitalization among the COPD patients with mental diseases (p<0.001). Conclusions: COPD symptoms were usually getting worsen over time and depression or anxiety affect the COPD patients significantly, though the mental diseases are usually under-estimated. The study results demonstrated that COPD patients suffered from depression and anxiety increased the risks on longer length of stay, higher medical expenditures and more complications. Implications for Policy, Delivery or Practice: WHO predicts that COPD will become the third leading cause of death worldwide by 2030. Since mental diseases may worsen elderly COPD patients’ health outcomes, physicians are advised to pay more attention to these types of patients.With on time and appropriate treatments, thus may help to improve quality of care and reduce medical expenditures for these patients. Funding Source(s): National Science Council,Taiwan Poster Number: 15 Linking RNs’ Perception of the Work Environment to Job Satisfaction in Nursing Homes JiSun Choi, M.S.N .; Linda Flynn, Ph.D.; Meg Johantgen, Ph.D. Presented by: JiSun Choi, M.S.N., Doctoral student, University of Maryland School of Nursing, 655 West Lombard Street, Room 475, Baltimore, MD 21201; Phone: (443) 320-3079; Email: jchoi008@son.umaryland.edu Research Objective: Consistent with the nursing practice environments in acute care settings, work environment is assumed to be associated with job satisfaction among nurses working in nursing homes. Yet the specific characteristics of the practice environment that impact job satisfaction have not been identified. The objective of this study was to quantify the effects of various dimensions of the practice environment on job satisfaction among Registered Nurses (RN) in nursing homes controlling for individual and nursing home characteristics. Study Design: A descriptive correlational design was used to conduct a secondary analysis of data from two sources: the parent study that conducted a statewide survey of registered nurses in New Jersey and the Online Survey, Certification, and Reporting (OSCAR) data. Two-level hierarchical modeling was used to examine the relative impact of 5 dimensions of the nursing practice environment while accounting for the clustering of nurses in facilities. Population Studied: Of the approximately 25% of all New Jersey RNs (n = 22,406) that participated in the survey, 340 RNs working as direct care providers in nursing homes where there were at least 4 RN respondents, were used for this study. These represent 63 skilled nursing facilities. Principal Findings: Controlling for individual and nursing home characteristics, nurse participation in facility affairs as well as staff and resource adequacy were positively associated with RNs’ job satisfaction. Ownership status was significantly related to job satisfaction; RNs working in for-profit nursing homes were less satisfied. Conclusions: As in acute care settings, opportunities to participate in facility affairs and having enough staff contribute significantly to higher job satisfaction among RNs working in nursing homes. Implications for Policy, Delivery or Practice: Unlike other nursing home characteristics, characteristics of the practice environment can be modified through administrative actions. Administrative initiatives to enhance RN job satisfaction by creating a more supportive practice environment should include increasing RNs' opportunities to provide meaningful input into organizational decision-making, and ensuring the adequacy of available resources. Embarking on the Magnet Accreditation journey is one mechanism by which hospitals have dramatically enhanced all dimensions of their practice environments, and is an initiative that should be seriously considered by nursing home administrators. Funding Source(s): RWJF, The National Institute Nursing Research (# NR004513) Poster Number: 18 Epidemiology of Hospitalized Burn Patients in Taiwan, 2007 Wu-Chien Chien, Ph.D.; Chi-Hsiang Chung; Lu Pai, Ph.D. Presented by:, Student, Graduate Institute of Life Sciences, National Defense Medical Center, School of Public Health 4209R, No. 161, Section 6, MinChuan East Road, Taipei, 11490 Taiwan; Phone: +886287923100 ext. 18445; Email: g694810042@ndmctsgh.edu.tw Research Objective: The objectives of this study is to find the high-risk groups of death caused by burn inpatient and medical services utilization of hospitalized burn patients, and the factors associated with hospital mortality caused by burn injuries. Study Design: This research brought “inpatient expenditures by admissions (DD)” and “registry for contracted medical facilities (HOSB)” from National Health Insurance Research Database in 2007 into analysis by using SPSS 14.0 software. We defined burn cases as ICD-9-CM N Code 940-949. Principal Findings: The total inpatient rate was 31.04 per 100,000, and males were higher than females (males 37.58 per 100,000, females 31.04 per 100,000). The inpatient rate of child form 0 through 4 years old was higher than any other age groups. Chiayi City had the highest inpatient rate (73.97 per 100,000), followed by Ilan County (61.90 per 100,000), Hualien County (50.98 per 100,000) and so on. There were 7,126 inpatient cases caused by burn injuries (males 61.23%, females 38.77%), the average age of them were 39.73 years old, and each person had 2.5 diseases or injuries. Among hospitalized burn patients, most parts of “site of burn injuries” were limbs (48.12%), “TBSA (total body surface area)” were <10% (39.29%), “degrees of burn injuries” were second degree (57.08%), and “causes of burn” were unintentional burn (89.87%). Among hospitalized burns patients, 53.79% (3,833 people) were consulted at plastic surgical department, 41.36% (2,947 people) were hospitalized in the medicine center, and they received 1.06 surgeries or operations in average; the mean of length of stay was 13.07 days, and the median of medical expenditures was 33,744.5 NT dollars. The number of deaths caused by hospitalized burn was 138 people. The factors associated with hospital mortality caused by burn injuries were ages, the number of other diseases or injuries, sites of burn injuries, intentional burn, hospital level, and the number of operations and treatments by multivariate logistic regression analysis; the explanation of overall model was 43.5%. Conclusions: All factors associated with hospitalized burn injury mortality included ages, the number of other diseases or injuries, sites of burn injuries, intentional burn, hospital level, and the number of operations and treatments by using multivariate logistic regression analysis. Implications for Policy, Delivery or Practice: In order to reduce burn mortality rates effectively, the government and NGOs should continue to promote the burn prevention programs together, especially for the high-risk of death caused by burn inpatient groups (0-4 age groups) Poster Number: 19 Trends of Fall Mortality in Taiwan, 1986-2007 Wu-Chien Chien, Ph.D.; Chi-Hsiang Chung; PingHsun Wu; Chien-Cheng Lai; Lu Pai, Ph.D. Presented by: Chi-Hsiang Chung, Student, Graduate Institute of Life Sciences, National Defense Medical Center, School of Public Health 4209R, No. 161, Section 6, Min-Chuan East Road, Taipei, 11490 Taiwan; Phone: +886287923100 ext. 18445; Email: g694810042@ndmctsgh.edu.tw Research Objective: The objectives of this study were to describe the trends in mortality rates due to fall injury by sex, age, causes, and occupation in Taiwan, 1986-2007. Study Design: Data were obtained from official Vital Statistics System for the period from 1986 to 2007. The types of “fall” include “fall from different level (E880, E881, E882, E884)”, “fall on the same level (E885, E886)”, and “other and unspecified fall (E883, E887, E888)” by using ICD-9-CM. The trends of mortality rates were tested with “curve estimation” by using SPSS 14.0 software. Principal Findings: There were 26,973 deaths caused by fall in Taiwan in the 22-year period, and the predominant cause of fall was “fall from one level to another (E884)” (30.26%). The mortality rates in males were higher than females (males 8.05 per 100,000; females 3.23 per 100,000), and without significantly change through the years. Elders aged over 70 years have the highest mortality rate (49.03 per 100,000). Among people of 70-year old or older, the mortality rates of “fall on the same level” descended in both genders, whereas; the mortality rates of “fall from different level” ascended in males, but not in females. The fall mortality rates varied with types of occupational groups. The highest rate was found with “nonphysical strength labors”, followed by “physical strength labors”. The “managers or administrators” had the lowest fall mortality rate. Conclusions: The mortality rates in males were higher than females, and without significantly change through the years. The fall mortality rates varied with types of occupational groups, and The highest rate was found with “non-physical strength labors”. Implications for Policy, Delivery or Practice: In order to reduce fall mortality rates effectively, we should continue to promote the fall prevention programs for the elderly. However, different target groups should be differentiated for “fall from the same level” and” fall from different level”. Furthermore, safety education for non-physical strength labors should also be enhanced. Poster Number: 20 Medicare Advantage Enrollees in Florida: Are They Healthier than Traditional Medicare Enrollees? Meg Comins, M.P.A .; Barbara Orban, Ph.D.; Etienne Pracht, Ph.D. Presented by: Meg Comins, M.P.A., Instructor, Health Policy and Management, University of South Florida, 13201 Bruce B Downs Boulevard MDC56, Tampa, FL 33612; Phone: (813) 313-7732; Email: mcomins@health.usf.edu Research Objective: The Medicare Modernization Act of 2003 (MMA) increased plan payments to private Medicare Advantage (MA) plans. Opponents claim that these plan enrollees are healthier than traditional Medicare (FFS) enrollees, contributing to higher costs for these plans. Proponents claim that MA plans lead to a reduction in racial and SES health disparities. MA plans have lower premiums and out-of-pocket expenses than FFS. A reduction in MA payments of $400 billion over the next decade is recommended as part of health care reform. This paper examines trends in patient clinical and demographic characteristics over time for Medicare enrollees to determine if healthier beneficiaries are enrolling in MA plans. Study Design: The primary source of data is hospital discharge and financial reports from the Florida Agency for Health Care Administration. Primary diagnosis, admission source, length of hospital stay, and age of FFS and MA enrollees are compared. ANCOVA was used to test for differences between the groups. Population Studied: Florida Medicare and Medicare Advantage enrollees were included in the study. Counties with more than 40% or less than 5% of Medicare eligibles enrolled in MA plans were excluded. Broward and Miami-Dade counties were the highly concentrated counties, and 23-35 rural counties had few or no MA enrollees over the study period. The access to MA plans for rural eligibles has not increased since the legislation. Principal Findings: More MA patients are 79 or younger. MA patients are more likely to be admitted to an Emergency Department (p<.001), with the difference between groups decreasing over time. MA patients are more likely to spend less than 2 days, and less likely to spend 7 or more days in the hospital, p<.001. Conclusions: More admits from the emergency department may be explained by more urgent conditions for MA patients, but could also point to limited access to care. The increase in admissions for MA patients reflects the growth in private fee-orservice (PFFS) MA plans, where traditional managed care tools like selective contracting are not used. These plans are more attractive to sicker patients that would have chosen FFS in the past to keep their provider. As more eligibles switch over to MA plans, the differences in health status will likely decline even more. Implications for Policy, Delivery or Practice: Medicare without supplemental insurance covers about one half of an enrollees medical expenses. MA plans are attractive to lower SES groups that can’t afford supplemental premiums. Higher ED admissions for MA enrollees may support past research on the association between lower SES and reliance on the ED as a source for routine health care. Problems with access to care can be partly attributed to low payments to physicians from the MA plans. A solution may be to require that a portion of payments to MA plans be used to increase plan payments to primary care physicians; this would likely increase access to care and reduce emergency department use. Future research will address practice patterns for lower SES enrollees to determine how to make primary care as accessible as ED care. Poster Number: 21 Does Receiving Primary Care from a Geriatrician Affect Health Care Use and Expenditures for Frail Elders and Elders at the End of Life? Laura D'Arcy, M.P.A. Presented by: Laura D'Arcy, M.P.A., Ph.D. student, Health Policy and Management, University of North Carolina at Chapel Hill, CB #7411, Chapel Hill, NC 27599-7411; Phone: (330) 606-0392; Email: ldarcy@email.unc.edu Research Objective: Older adults generally rely on internal medicine or family medicine physicians for primary care; a small share receives primary care from geriatricians. Geriatricians have a number of skills that distinguish them from other primary care providers (e.g., expertise in managing geriatric syndromes and multiple medications, assisting endof-life decision-making). Primary care from a geriatrician may be particularly beneficial for frail elders and those at the end of life. Evidence on the effect of geriatricians comes from small randomized controlled trials of geriatrics evaluation and management programs that offer conflicting results. Studies also suggest that primary care plays an important role in health care use and expenditures, but existing analyses combine specialties. The objective of this study is to separately estimate the effect of geriatrician use on health care use and expenditures from internal medicine and family medicine physician use. Study Design: Using 2002-2007 Medicare claims data, I compare the associations between primary care provider specialty and health care use and expenditures among six groups of elderly beneficiaries: high geriatrician, medium geriatrician, low geriatrician/high internal medicine, low geriatrician/high family medicine, no geriatrician/ high internal medicine, and no geriatrician/high family medicine use. Outcome variables include emergency department use, inpatient admissions for ambulatory care sensitive conditions, in-hospital death, and inpatient and total expenditures. Since primary care provider specialty may be related to unobservable factors that affect use and expenditures (e.g., supplemental health insurance), I use instrumental variables to exogenously predict provider specialty based on the share of primary care doctors in the area that are geriatricians. Analyses are conducted separately for frail elders and those in the last year of life. Population Studied: The sample is drawn from nearly one million elderly Medicare beneficiaries who had an inpatient admission for acute coronary syndrome in 2003-2004. Approximately 125,000 of these beneficiaries are considered to be frail, and more than half a million died during the study period. In 2003 and 2004, nearly 20,000 beneficiaries had at least one geriatrician visit. Principal Findings: Analyses are presently in process. Based on the literature and descriptive results, I expect that elders who use a geriatrician may be less likely to have an emergency department visit or inpatient admission for an ambulatory sensitive condition and lower expenditures than those who rely on an internal medicine or family medicine physician. Conclusions: Primary care from a geriatrician may play an important role in reducing preventable health care use and expenditures for frail elders and those at the end of life. Treating primary care provider specialty as endogenous to the outcome equation is likely important to obtaining an unbiased estimate of the relationship between provider specialty and health care use and expenditures. Implications for Policy, Delivery or Practice: Estimates indicated that by 2030, 36,000 geriatricians will be needed; current graduation rates from geriatrics fellowship programs suggest there will be only 7,750 geriatricians. Examining whether elders who receive primary care from a geriatrician have lower and less costly health care use than those who rely on other specialties is critical to determining whether and how drastically to change incentives to encourage more physicians to pursue geriatric certification. Funding Source(s): NIA Poster Number: 22 Social Capital and Mental Health: An Examination of the Relationship among Neighborhood Conditions, Primary Caregiver Depression, and Childhood Behavioral Problems Ayesha Delany-Brumsey, M.A.,Vickie Mays, Ph.D., M.S.P.H. Presented by: Ayesha Delany-Brumsey, M.A., C.Phil., Graduate Student, Clinical Psychology, University of California, Los Angeles, 1285 Franz Hall, Box 951563, Los Angeles, CA 90095; Phone: (301) 928-8408; Email: adelanybrumsey@ucla.edu Research Objective: Previous research has established the link between where we live and our mental health. However, relatively little is known about the particular aspects of neighborhoods which may be important in determining this relationship. The primary purpose of this study is to examine how the environment of the neighborhood, both economic and social, can be a contributing factor in the development of child behavior problems. The study also explores the contribution of individual level characteristics including child demographics, caregiver demographics, and caregiver depression to child behavior problems. The proposed model acknowledges that children’s mental health is influenced both by their caregivers, and by the context in which their relationship with their caregiver takes place. Study Design: The data is from the Los Angeles Neighborhood and Family Survey (L.A. FANS), a study of Los Angeles County families and their neighborhoods. The data used here is from Wave 1 of the study which was collected from April 2000 to January 2002 (Peterson et al., 2004). The data were analyzed using two-level hierarchical linear models with robust standard errors in which children are clustered within neighborhoods. The dependent variable is child behavior problems as measured by the Behavior Problems Index (Peterson & Zill, 1986). The individual level predictors are child and caregiver demographic characteristics including family income, child gender, child and caregiver race/ethnicity, caregiver marital status, caregiver educational attainment, and family income. Caregiver depression was also an individual level predictor and was measured using the CIDI-SF (Kessler et al., 1998). The neighborhood level predictors are neighborhood socioeconomic disadvantage, residential instability, and social capital. The questions used to measure neighborhood social capital were first published in Sampson et al. (1997) and Sampson et al. (1999). Population Studied: The participants are 1,535 children between the age of 3 and 17 (M = 8.31, SD = 5.14). The demographic makeup of the sample is as follows: 49% of the children are male and 51% female; 54.62% are Latino, 25.75% White, 9.81% Asian/Pacific Islander, 8.31% Black and 1.51% Native American. Principal Findings: Child behavior problems were not significantly associated with any of the neighborhood level socioeconomic characteristics or neighborhood level social capital. However, behavior problems were significantly predicted by primary caregiver depression. As the number of symptoms endorsed on the CIDI-SF increased so do the number of child behavior symptoms. In addition, younger children displayed more behavior problems than older children. Also, children of caregivers with less than a high school education had more behavior problems than children of more educated caregivers. Conclusions: Child behavior problems was not associated with any of the neighborhood level variables. However, behavior problems were significantly associated with the family level variable of primary caregiver depression. Implications for Policy, Delivery or Practice: The results of this study suggest that one way to reduce the incidence of child behavior problems is to provide supportive services to the caregivers. Services such as mental health counseling, or parent training may reduce the incidence of depression among caregivers which in turn could reduce child behavior problems among the children they are responsible for. Poster Number: 23 Quality Trend in Nursing Homes Nailya DeLellis Presented by: Nailya DeLellis, Ph.D. Student, Health Administration, Virginia Commonwealth University; Email: delellisno@vcu.edu Research Objective: Does change in quality of care depends on nursing home organizational characteristics? Study Design: The study featured a longitudinal comparison of quality measures provided by the Online Survey Certification and Reporting (OSCAR) database Population Studied: The population observed was taken from the OSCAR database. Excluded from analysis were nursing homes that were hospital based and size outliers. Principal Findings: Regarding process and outcome quality, there was a positive correlation between quality measures and staff (RNs LPNs aides) to patient ratios, confirming what has been long established in the literature. A second finding was that belonging to a system, larger size, and higher occupancy had a negative correlation with quality. Definitions for process and outcome quality were those found in the National Quality Clearinghouse website. There were 5 process measures (use of catheters, use of restraints, flu and pneumonia vaccination and pain management) and 6 outcome measures (presence of ulcers, diagnosis of depression, bowel and bladder incontinence, weight loss and bedfast). For all measures average values were calculated. If a nursing home facility had a measure in the upper quartile, it received a score of 1. So each nursing home had 2 scores, one for process and one for outcome, and changes in those score will compared. Conclusions: to be described later based on the findings Implications for Policy, Delivery or Practice: to be described later based on the findings Poster Number: 25 Implications of Applying New WHO Growth Standards on Assessment of Nutritional Status among Under-Five Children in a Rural Health Center in India. Avika Dixit, M.B.B.S.; Uzma Khan, M.B.B.S.; Jane Philip, M.B.B.S. Presented by: Avika Dixit, M.B.B.S., Student, Harvard School of Public Health, 199, Park Drive, Apartment 133, Boston, MA 02215; Phone: (617) 834-8576; Email: adixit@hsph.harvard.edu Research Objective: World Health Organization, after a review of NCHS anthropometric references of 1977 concluded that these did not adequately represent early childhood growth and that new growth curves were necessary. In view of this, WHO generated new curves based on the Multicentre Growth Reference Study. These standards provide a more robust tool for assessing child growth. The design characteristics provide a wider array of references for expanded uses, such as monitoring of childhood obesity and management of early lactation. Since the NCHS growth charts were still in use, we did a study to assess the nutritional status of under-five children using NCHS and WHO standards with the weightfor-age and height-for-age charts, to compare the two standards in detecting malnutrition among children and study the implications of adopting new WHO standards in assessing prevalence and detection of malnutrition. Study Design: We conducted a cross – sectional study where we retrieved from hospital records the anthropometric measurements of 100 under five children in rural Karnataka, India in September 2008. The heights and weights of children were plotted on the weight-for-age and height-for-age charts separately for males and females on the growth charts based on the NCHS reference. These were then plotted on the WHO growth charts and the nutritional statuses according to the two references were compared. Population Studied: Children under five years of age who attended the out-patient department of a community health center in village Karkala, Karnataka, India were selected for the study. Principal Findings: Our study showed that the WHO growth standards pick up more underweight children as compared to NCHS standards (19% vs. 11%). The prevalence rates were higher with the WHO standards for the 0-6 months (n=30), 6-12 months (n=26) and 2-5 years age groups (n=14) than with the NCHS standards (26.7% vs. 6.7%, 15.4% vs. 7.7% and 24.1% vs. 7.1% respectively). However, in the 1-2 years age group (n=30), the prevalence was less with the WHO standards than with the NCHS standards (13.3% vs. 20%). The prevalence was higher with the WHO standards in the first half of infancy. Regarding height-for-age, the prevalence of stunting was less with the WHO standards as compared to NCHS standards (11% vs. 13%). However, the prevalence was higher upto 6 months of age (n=30) with the WHO standards (13.3% vs. 6.7%). Amongst 6-12 months (n=26) and 1-2 year age group (n=30), WHO standards showed lower prevalence (7.7% vs. 15.4% and 13.3% vs. 20% respectively). The prevalence (7.1%) was same in the 2-5 years age group (n=14). Conclusions: Our study, though small in sample size, showed that adoption of the new standards would help in picking up more malnourished children and probably at an earlier stage. Implications for Policy, Delivery or Practice: The new approach is important to improve early detection and proper management of malnourished children and prevent life-long sequelae, which prevent them from achieving their full potential of physical development. Poster Number: 26 Cholera Vulnerability in a Rural Community in Western Kenya Avika Dixit, M.B.B.S. Presented by: Avika Dixit, M.B.B.S., Student, Harvard School of Public Health, 199, Park Drive, Apartment 133, Boston, MA 02215; Phone: (617) 834-8576; Email: adixit@hsph.harvard.edu Research Objective: The study was done in July 2009 to assist UNICEF Kenya in identifying areas requiring intervention for cholera prevention and control. Study Design: A cross – sectional study of ninetysix households, who were interviewed on water handling practices, hygiene and sanitation, and knowledge, regarding acute watery diarrhea including cholera. Water containers, hand washing techniques and condition of latrines were observed. Inpatient and outpatient records were obtained from two health facilities. Interviews were held with key informants. Population Studied: Households in rural area of Muhuru Division, Kenya, located at the shore of Lake Victoria near the Tanzanian border. Principal Findings: During the dry season, majority (79.2%) used lake water and during rainy seasons 76% used rainwater. The respondents said that they washed containers for carrying water everyday (77.1%) and cleaned containers for storage adequately (81.2%). However, both containers were found dirty in almost 75% of the households on inspection. Almost 40% used chlorine to treat drinking water. The technique of hand washing at critical times was found to be inadequate for more than 70% though more than 80% of households had soap. Almost 70% thought use of soap unnecessary. Majority (59.4%) bought cooked food from the market sometimes. Latrine coverage was 27.1%. Amongst those, 65.4% of the latrines’ condition was found to be fair. Majority (81.4%) said they didn’t have enough money to construct one. Amongst the households with under fives (n=85), 47.1 % buried children’s feces. Regarding knowledge about cholera, 81.3% identified the main symptoms; majority (70.8%) knew how it was transmitted, though about 30% did not know how it could be prevented. If a family member had diarrhea, 72.9% said that they would take them to the health facility. Other findings included a lack of national policy and strategy on diarrheal disease control, absence of ORT corners in health facilities, lack of laboratory services, lack of staff capacity in appropriately treating and controlling cholera and inappropriate use and promotion of salt solution instead of sugar-salt solution by the community health workers (CHWs). Conclusions: Due to the lack of culture facilities, Muhuru Bay has never been identified as an area with cholera. Over use of intravenous fluids lead to increased hospitalizations and made cholera treatment more expensive. Poor community awareness with regards to adequate hygiene and sanitation practices, ORS use and water safety was evident. Low latrine coverage due to poverty and collapsing soils, lack of a safe water source and shortage of chemicals for treatment of water compounded the community’s vulnerability to cholera. Implications for Policy, Delivery or Practice: Development of national diarrheal disease control policy and strategy should be expedited and implemented in Kenya. ORS and Zinc should be made available to CHWs on a regular basis, not only during an outbreak. This will enable use of ORS soon after onset of diarrhea. To improve ORS usage as the first line of treatment, establish ORT corners in all health facilities. Develop skills at the community level to identify the need for and bring about improvement and maintenance of community water points. Funding Source(s): UNICEF Poster Number: 27 A Study of Personal Health Records: A Pillar of Meaningful Use for Oregon’s Medicaid Population? Oliver Droppers, M.S., M.P.H., Sherril Gelmon, Ph.D.; Jill Rissi, Ph.D.; Aasta Thielke Presented by: Oliver Droppers, M.S., M.P.H., Research Assistant, Hatfield School of Government, Portland State University, PO Box 751, Portland, OR 97207-0751; Email: Odropper@pdx.edu Research Objective: The State of Oregon, supported by a federal Medicaid Transformation Grant is implementing a personal health record system (PHR) for Medicaid enrollees using a health record bank model. A research team from Portland State University was contracted by the State to evaluate the utility of the PHR based on the experience and perspective of Medicaid enrollees. The study will assess awareness, enrollment, and utilization patterns among active and non-active PHR users, and determine which population groups are more or less likely to initiate and continue using a personally controlled and self-managed PHR. Study Design: The study is quasi-experimental, employing mixed methods through a communityengagement research strategy including use of online surveys, interviews, focus groups, direct observations, and documentation review. Data will be collected during multiple stages of PHR adoption: implementation, ongoing enhancements, and maintenance. An evaluation conceptual framework of key concepts and indicators will guide the research, helping to illustrate barriers to and facilitators of PHR adoption. Population Studied: Potential participants include adults age 18 to 64 enrolled in Medicaid who establish an online PHR during the study period. As of October 2009, Oregon Medicaid covered approximately 384,000 individuals. The priority populations include low-income children in foster care, pregnant and postpartum women, individuals enrolled in disease management, disabled and senior adults. Adults are targeted for enrollment in the first phase; followed by children and their associated caregivers, case managers and/or foster parents. Principal Findings: Preliminary findings indicate success as measured relative to the following indicators: number of registered and active PHR users and providers; user satisfaction and concerns with use of the PHR; the degree of system use by clinicians and professional service providers; and the extent to which participants are willing to allow data collected by the Health Record Bank of Oregon to be used for research and public health purposes. Conclusions: It is critically important that we evaluate the functionality and use of PHRs among vulnerable population groups; and in particular, identify potential benefits and perceived value among Medicaid enrollees and clinical providers. Findings can help inform ongoing and future activities intended to improve enrollment and continuity of use of PHRs among priority Medicaid populations. In addition, findings will help enhance our understanding of the overall feasibility of PHRs among Medicaid clients and assess potential future application and use of the Health Record Bank of Oregon in the context of meaningful health information exchange. Implications for Policy, Delivery or Practice: Medicaid beneficiaries experience high levels of “churn” between public, private and no health insurance coverage. Consequently, increasing their engagement and participation in a PHR through effective outreach, enrollment and utilization of a PHR offers the opportunity to potentially improve health information exchange across the continuum, and enhance the coordination and efficiency in the provision of health services. An enhanced understanding of factors that mediate the decision to establish and use a PHR can guide future efforts to establish, maintain and expand PHRs, and possibly contribute to a broader statewide strategic planning progress designed to achieve "meaningful use" of health IT in Oregon. Funding Source(s): CMS Poster Number: 28 Predictors of Atomoxetine Initiation in Medicaid Children and Youth Newly Diagnosed with Attention Deficit Hyperactivity Disorder Lobna Eldasher; Scott Bilder, M.S.; Stephen Crystal, Ph.D. Presented by: Lobna Eldasher, Research Intern, Institute for Health, Health Care Policy, and Aging Research, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Phone: (609) 914-5647; Email: lmeldasher@gmail.com Research Objective: Atomoxetine was first introduced in late 2002 as an alternative to the stimulant medications methylphenidate and aM.P.H.etamine that are widely used in the treatment of Attention Deficit Hyperactivity Disorder (ADHD). This study focused on the identification of variables that predict the initiation of the nonstimulant atomoxetine vs. a stimulant medication in children and youth after they received a new diagnosis of ADHD. For various reasons, including concerns about contraindications, side effects, and adverse events; as well as the abuse potential of stimulants; it was expected that children and youth initially prescribed atomoxetine after diagnosis would differ in important and predictable ways from those prescribed stimulants. The results of this study provide insight into some of the patient characteristics evaluated by clinicians in their initial selection of an ADHD drug. Study Design: This was a retrospective observational study of fee-for-service Medicaid claims using 2002-2004 Medicaid Analytic Extract (MAX) data for eight states. A series of multivariate logistic regression models were estimated in order to identify patient variables associated with initiation of atomoxetine versus a stimulant following initial diagnosis with ADHD. Predictors included type of ADHD diagnosis (hyperactive vs. inattentive); sex, age, and race/ethnicity; year of diagnosis (2003 or 2004); and the following pre-existing comorbid conditions: drug abuse or dependence, tics, bipolar disorder, conduct disorder, emotional disorders, and developmental delays. Results from the full model containing all variables are reported. Population Studied: The study sample included children and youth aged six through seventeen who had continuous Medicaid eligibility for at least 12 months and who had initiated pharmacotherapy with atomoxetine, methylphenidate, or aM.P.H.etamine following a first diagnosis of ADHD (N=32,110). Principal Findings: Twenty-two percent of newly diagnosed children and youth received atomoxetine and 78% received a stimulant. Beneficiaries with a drug-related disorder had 34% greater odds of being prescribed atomoxetine than persons without such a disorder and beneficiaries with tic disorders had over three times the odds of those without tics. hose with developmental delays had approximately 22% lower odds of being prescribed atomoxetine vs. a stimulant after diagnosis. White beneficiaries, older youth, and females were more likely to initiate treatment with atomoxetine than their nonwhite, younger, and male counterparts. Beneficiaries first diagnosed with ADHD in 2004 (vs. 2003) had approximately 25% lower odds of starting pharmacotherapy with atomoxetine. Beneficiaries diagnosed with the inattentive-only type of the disorder had 30% higher odds of receiving atomoxetine compared to those with hyperactivity. Conclusions: A prior diagnosis of a tic disorder greatly increased beneficiaries’ odds of receiving atomoxetine, reflecting ongoing concern about the use of stimulants in this population. It also appears that choice of ADHD drug reflects prescribers’ concerns about the abuse potential of stimulants; older youth and those with diagnoses of drug abuse or dependence were significantly more likely to have received atomoxetine in place of a stimulant. These results provide some insight into the patient characteristics taken into account by prescribers deciding on an initial choice of ADHD drug. Funding Source(s): RWJF Poster Number: 29 Exploring the Effects of Treatment Processes on the Ischemic Stroke Patients in Taiwan Pei-Hsuan Fang; Ying-Chun Li, Ph.D. Presented by: Pei-Hsuan Fang, Graduate Student, Institute of Health Care Management, National Sun Yat-Sen University, 70 Lien-Hai Road, Kaohsiung, 804 Taiwan; Phone: +88675252000 ext. 4875; Email: pangel0927@gmail.com Research Objective: Ischemic stroke is a commonly seen chronic disease in aged population and at high risk of stroke recurrence, physical and intellectual disability, long-term institutionalization, and death. Antiplatelet agents, such as aspirin and clopidogrel, are the first-line antiplatelet therapies for prevention of recurrent stroke in patients with ischemic stroke. The diverse pharmacological effects of the different antiplatelet drugs not only influence the patient outcomes but also affect the health-care utilizations. International studies have broadly discussed the impacts of antiplatelet agents on ischemic stroke patients, however, little studies have examined such issue in Taiwan. Taiwan implemented national health insurance program and covered over 98% of its residents since 1995. This makes Taiwan an excellent study subject of outcome research because it reduces the potential study biases from health care coverage variations. Therefore, this study aims to explore the hospitalizations and direct medical expenditures of antiplatelet treatments in the aged population for secondary prevention of ischemic stroke. Study Design: This study examined three antiplatelet treatment processes for the aged population in Taiwan –none antiplatelet therapy, aspirin, clopidogrel–by using the National Health Insurance Research Database between 2003 and 2006. The data sets included patients’ demography, prescriptions, and health care history, plus outpatient records, inpatients records, and information about the medical facilities they visited during the study period. The data analyses included Chi-square test, Anova, multiple linear regression and multivariate logistic regression. Population Studied: Patients aged 40 or older who were new cases of ischemic stroke based on ICD9-CM of hospital admissions and readmissions from 2003 to 2004 in Taiwan. Patients were followed for two years and excluded if they shifted antiplatelet therapy during research period. Principal Findings: Among 1422 patients of ischemic stroke, 52.67% were with none antiplatelet therapy, 44.44% with aspirin and 2.88% with clopidogrel. Among 20% of the patients who had hospital readmissions because of the ischemic stroke, 29.63% were readmitted within 14 days after discharge and 12.96% were readmitted within 1530 days after discharge. More health care utilizations were observed in the clopidogrel group than aspirin and none antiplatelet therapy groups (p<0.05). Age and hospital level were significantly affected health care utilizations and length of stay. But the probability of hospital readmissions among three antiplatelet treatments presented no statistically significant difference. Conclusions: Clopidogrel were not significantly effective in the prevention of recurrent stroke in patients with ischemic stroke, but were associated with the increased health care utilizations in Taiwan. By understanding more about factors affecting hospitalization and health care utilization in different antiplatelet treatments of ischemic stroke, we may modify treatment process, reduce unnecessary costs, and improve the health status of patients. Implications for Policy, Delivery or Practice: How to design an optimal drug reimbursement system while ensuring the quality of care and controlling medical cost growth is an important study issue worldwide in recent years. This study provides useful reference for policymakers and health care professionals in care of the ischemic stroke patients. Funding Source(s): National Science Council Poster Number: 30 Social Context and Alcohol Use Disparities in a Racially Integrated Community Ruth Fesahazion, B.S.H.S.; Caryn Bell, B.S.; Natieka Green; Roland Thorpe, Jr., Ph.D.; Thomas LaVeist, Ph.D. Presented by: Ruth Fesahazion, B.S.H.S., Doctoral Student, Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadyway, Baltimore, MD 21205; Phone: (520) 272-5345; Email: rfesahaz@jhsph.edu Research Objective: National estimates of race differences in alcohol use suggest that nonHispanic whites are more likely to be current drinkers; however, African Americans suffer a greater burden of alcohol-related problems. However, findings from national studies fail to account for the social and environmental risk exposures resulting from residential segregation. Thus, little is known about race disparities in alcohol use among individuals who share similar social and environmental conditions. The objective of this study is to determine if racial differences exist in alcohol use between African American and nonHispanic white adults residing a racially integrated community. Study Design: We compared race disparities in 1,408 individuals from the Exploring Health Disparities in Integrated Communities-Southwest Baltimore (EHDIC-SWB) Study with 29,372 individuals from the 2003 National Health Interview Survey (NHIS 2003) to determine if race disparities in alcohol use were attenuated in EHDIC-SWB, a racially integrated urban community without race differences in socioeconomic status. Population Studied: EHDIC (Exploring Health Disparities in Integrated Communities) is an ongoing multisite study of race disparities within communities where African Americans and nonHispanic whites live together and where there are no race differences in SES (as measured by median income). The National Health Interview Survey (NHIS) is nationally representative household survey of non-institutionalized U.S. citizens conducted by the National Center for Health Statistics. Principal Findings: In the NHIS 2003 sample, compared to non-Hispanic whites African Americans had a lower odds of being a current drinker (OR=0.56, 95% CI=0.49-0.64); former drinker (OR=0.84, 95% CI=0.72-0.99); or binge drinker (OR=0.68, 95% CI= 0.58-0.79) independent of covariates. However in the EHDIC-SWB sample, African Americans had similar odds of of being a current drinker (OR=0.95, 95% CI=0.67-1.34); former drinker (OR=0.71; 95% CI=0.50-1.01); or binge drinker (OR=1.02, 95% CI=0.77-1.35) compared to non-Hispanic whites after adjusting for covariates. Conclusions: Among individuals living in a lowincome, urban, racially integrated community with similar exposure to social and environmental risk, race disparities in alcohol use were eliminated. These results suggest that the social environment should be accounted for when developing research, policies, and interventions that address health disparities. Implications for Policy, Delivery or Practice: These results suggest that the social environment should be accounted for when developing research, policies, and interventions that address health disparities. Poster Number: 31 A Comparison of U.S. Army and Civilian Registered Nurses: Influence of Organizational and Personal Factors on Intent to Leave Their Current Organizations Linda Fisher, M.H.A., R.N.; Mary Dietrich, Ph.D. Presented by: Linda Fisher, M.H.A., R.N., Nursing Research, Nursing Research Service, U.S. Army, Madigan Army Medical Center, Tacoma, WA 98431-1000; Phone: (253) 968-2289; Email: linda.w.fisher@vanderbilt.edu Research Objective: The purposes of this study were to measure and compare organizational, personal, and economic factors in two groups of nurses (military and civilian) to: a) determine if and how much difference exists between the two group’s intent to leave their current organizations, b) determine how structural empowerment, psychological empowerment, and job satisfaction factors predict intent to leave, and c) explore the mediating and moderating effects of personal and economic factors on the intent to leave. This is important because poor nurse retention in the US Army at the mid-career level (losses up to 20%) can have devastating implications in future Army Nurse Corps leadership. Study Design: A targeted comparative group design with population sampling of US Army Nurses. Data were collected through use of Vanderbilt University’s REDCap Survey service (A service that provides secure internet survey completion from anywhere in the world). Theoretical and conceptual frameworks of organizational structure and empowerment (including those of Kanter and Laschinger) guided survey content which included the Conditions of Work Effectiveness Questionnaire-II (CWEQ-II), the Psychological Empowerment Instrument (PEI), job satisfaction scale, additional economic and demographic questions, and intent to leave items. Population Studied: The sample included two groups: a) US Army nurses between the ranks of 2nd Lieutenant and Major (n=623) and, b) civilian registered nurses (n=210), randomly selected from the total population of registered nurses employed at Vanderbilt University Medical Center (VUMC) because the VUMC registered nurse population was demographically similar to the US Army population. he ranks of 2nd Lieutenant to Major were targeted because the individuals in that group have the lowest retention rate. Response rates were 19.7% and 24.4% respectively. Principal Findings: Data collection closed in late December 2009 and the study is in the analysis phase. Preliminary analysis indicates no coding problems and a high percentage of completeness of cases. Findings will be available prior to the start of the Annual Research Meeting in June 2010. Conclusions: Conclusions are pending and will be available prior to the start of the Annual Research Meeting in June 2010. Implications for Policy, Delivery or Practice: High nurse turnover can negatively affect nurse work environments, healthcare quality, nurse job satisfaction, and ultimately nurse recruitment. There is value in identifying civilian solutions already in use and solutions that may be unique to military nurses. The findings from this study will provide greater understanding of organizational factors that influence nurses’ intent to leave and provide insight into possible areas for military healthcare organizations to concentrate limited resources to improve nurse work environments that may result in increased military nurse retention. Poster Number: 32 An Examination of Rural-Urban Differences in Prepregnancy Body Mass Index and Gestational Weight Gain Presented by: Alexa Gallagher, M.S.P.H., Student, Rural Health Research Center, University of South Carolina, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210; Phone: (803) 251-6317; Email: GALLAGHA@mailbox.sc.edu Co-authors: Alexa Gallagher, M.S.P.H.; Jihong Liu, Sc.D.; Amy Martin, Dr.PH.; Janice Probst, Ph.D. Research Objective: Having an unhealthy prepregnancy weight and/or gaining an inappropriate amount of weight during pregnancy are known to increase the risk for poor pregnancy and birth outcomes. To date, no studies have examined differences in prepregnancy body mass index (BMI) and gestational weight gain (GWG) in women who reside in rural versus urban areas. Because rural residents tend to have a lower socioeconomic status and poorer access to health care than urban residents, an examination of residence-based differences in prepregnancy BMI and GWG is warranted. We sought to examine prepregnancy BMI and GWG patterns in women residing in rural versus urban areas of South Carolina. Study Design: Data from the 2004-2006 South Carolina birth certificates (n=132,795) were used. Rural/urban residence was determined using RuralUrban Commuting Area (RUCA) codes. Mothers were categorized into 4 groups according to their prepregnancy BMI: underweight (<=18.5 kg/m2), normal weight (18.5-24.9), overweight (25.0-29.9), and obese (>=30.0). GWG was then defined as inadequate, adequate or excessive according to the Institute of Medicine’s 2009 weight gain guidelines. Multinomial logistic regression was used to examine urban and rural differences in prepregnancy BMI and GWG after adjusting for potential confounders (maternal age, race, marital status, education, parity and tobacco use). Population Studied: This study population (n=132,795) included women residing in South Carolina who delivered a liveborn, singleton infant between 2004-2006. Principal Findings: In 2004-2006, 34.7% of women who were pregnant in SC resided in rural areas. Compared to urban pregnant women, rural pregnant women were more likely to be younger, African American, unmarried and have less than a high school education. Rural pregnant women were also more likely to be obese (30.7% v. 25.8%). In multinomial logistic regression analysis, they had higher odds of being obese (adjusted odds ratios (AOR) = 1.21, 95% CI = 1.18, 1.25), overweight (AOR= 1.08; 95% CI = 1.05, 1.11), and underweight (AOR=1.06, 95% CI=1.00, 1.12) than urban women. This relationship was found to be partially explained by the higher proportion of minorities living in rural areas. Regarding GWG, a slightly higher proportion of rural compared to urban women gained inadequate weight (30.0% v. 27.2%) and a slightly lower proportion gained excessive weight (47.0% v. 49.3%). The relationship between GWG and rurality was found to differ by prepregnancy BMI class. Specifically, there were no residence-based differences in GWG in underweight women. Among normal weight women, rural women had an increased odds of inadequate GWG (AOR=1.09, 95% CI=1.04, 1.15). Among overweight or obese women, compared to their urban counterparts, rural women had decreased odds of excessive GWG (AOR=0.92, 95% CI=.87, .98) and a decreased odds of both inadequate (AOR=.85, 95% CI=.80, .91) and excessive GWG (AOR=.86, 95% CI=.81, .92), respectively. Conclusions: Small, but significant differences in prepregnancy BMI and GWG were found between rural and urban women that were not fully explained by socio-demographic differences. Future researchers should further explore reasons for these findings and the resulting health consequences for the rural population. Implications for Policy, Delivery or Practice: Confirmation of these findings may help health care providers better serve and advise their pregnant population. Poster Number: 33 Prescription Drug Plan Enrollment and CostRelated Nonadherence in Medicare Part D Beneficiaries with Diabetes Presented by: Kristin Geonnotti, Doctoral Candidate, Health Policy and Management, University of North Carolina Chapel Hill, CB# 7400, Chapel Hill, NC 27599-7400; Email: klg@unc.edu Co-authors: Mary Roth McClurg, Pharm.D., M.H.S.; Tim Carey, M.D., M.P.H.; George Pink, Ph.D.; Marisa Domino, Ph.D.; Morris Weinberger, Ph.D. Research Objective: Medicare Part D aims to provide seniors with affordable prescription drug coverage. Annual out-of-pocket costs can vary widely between plans. This study will determine the proportion of individuals who are enrolled in lowest- cost plans, characteristics associated with being in a lowest-cost plan, and whether lowest-cost plan enrollment and differential costs are associated with experiencing cost-related nonadherence. Study Design: This observational, cross-sectional study combines data from participant surveys, medical records, and publicly-available CMS plan data. Study participants are surveyed about their Medicare Part D plan, cost-related nonadherence, and plan enrollment decisions. For each beneficiary, we used the CMS Prescription Drug Plan Finder tool to calculate: (1) actual out-ofpocket medication costs for one year based on their current plan and (2) lowest out-of-pocket medication costs for one year if they were enrolled in a plan with the least out-of-pocket spending. Differential costs are the difference between the actual and lowest out-of-pocket costs if all prescriptions are filled for one year. These calculations were made twice: once assuming that prescriptions were filled as written, and again with generic substitutions. Medical record data include patient characteristics, diagnoses, prescribed medications, clinical outcomes, and health services utilization. Descriptive and multivariate logistic regression analyses will be used to determine the proportion of the sample in lowest-cost plans and the association between lowest-cost plan enrollment/differential costs and cost-related nonadherence. Population Studied: Study participants are drawn from diabetes registries at the UNC-Chapel Hill Internal Medicine and Family Medicine practices. Participants include Medicare Part D beneficiaries who: (1) have diabetes; (2) are age 65 and older; (3) are community-dwelling; (4) have had = 1 primary care visit in the past 12 months; and (5) are able to complete a telephone interview. Principal Findings: Of 228 participants, 61.8% are female and 16.7% are dually-eligible for Medicare and Medicaid. Participants take an average of 9.2 medications annually, and 33.6% report experiencing cost-related nonadherence. 22.6% of participants have switched plans in the past year. Lowest-cost plan enrollment and differential costs have been estimated for the 162 participants who granted medical records access. Only 27.2% of beneficiaries are enrolled in a plan that is within 10% of their lowest cost plan, regardless of generic substitution. Differential costs are substantial (mean ± SD = $1140.73 ± $1475.14; median = $707.50). When assuming that generic substitutions were allowed, differential costs are smaller, but still considerable (mean ± SD = $641.10 ± $795.03; median = $449.50). Conclusions: Preliminary results suggest that the majority of beneficiaries are not enrolled in a lowest-cost plan, and are therefore paying substantially more than is necessary to obtain their medications. We are also examining the relationship among differential costs, medication- related non-adherence, clinical outcomes, and health services utilization over a one-year period. Implications for Policy, Delivery or Practice: Policy interventions can target plan enrollment to increase the proportion of beneficiaries in lowestcost plans. For instance, the random autoassignment of dually-eligible individuals could be replaced with a beneficiary-centered assignment process, which considers medication coverage needs. Additional strategies could be developed to simplify the complex enrollment decision-making process facing other beneficiaries and their caregivers. Funding Source(s): NRSA Pre-doctoral Traineeship from AHRQ, sponsored by the Cecil G. Sheps Center for Health Services Research, UNC Chapel Hill, Grant No. T32-HS-000032-19 and the UNC Graduate School Dissertation Completion Fellowship Poster Number: 34 Contributing Factors of Count Discrepancy with respect to Operating Room (OR) Processes Presented by: Hyo Geun Geun, M.P.H., R.N., Doctoral Student, School of Nursing, University of Michigan, 400 North Ingalls Building, Ann Arbor, MI 48109; Phone: (818) 636-2982; Email: geunhyo@umich.edu Co-authors: AkkeNeel Talsma, Ph.D., R.N.; Christine Anderson, Ph.D., R.N. Research Objective: Since the publication of the Institute of Medicine (IOM) report, “To Err is Human (2000),” a variety of organizational characteristics has been examined in relation to patient safety. Accordingly, research focuses have moved toward identifying processes or human factors that contribute to adverse events. In Operating Room (OR) particularly, surgical incorrect counts occur relatively rarely, but the consequences are serious. This lack of a complete count of sponges and instruments has been identified as possible risk factors for retained objects after surgery. Although studies have shown that all the processes and nurse staffing patterns in OR are connected as a system and impact patient outcomes, studies to date about surgical errors have not been examined well. The objectives are to describe the systems factors associated with count discrepancy in acute care settings. Study Design: An exploratory descriptive study was performed. Due to the lack of patient-specific demographic data, only variables related to OR process and staffing pattern were included for analysis. Initial step focused on describing overall surgical count procedures in OR. Then, the distributions of correct and incorrect counts in relation to system and human factors were included. Population Studied: Of surgical cases performed at a hospital in 2008, a total of 7,791 cases with 110 different high risk procedures were included. All data were obtained from the OR electronic record and analyzed using SPSS. Principal Findings: Compared to correct cases (all counts are correct in this group), the other incorrect cases which include at least one count discrepancy show significantly higher percent of selected system factors within incorrect cases when: operations were performed on emergency (16% vs 24 %), weekend (8% vs 13%), in-patient (21% vs 30%), with multiple procedures at a time (4% vs 11%), in cases exceeding the operation time to the next shift (29% vs 62%), begin shifts in the evening (16% vs 17 %) or at night (3% vs 6%) and end shifts in the evening (39% vs 61%) or at night (4% vs 9%). In addition, procedures with higher volume of staff participating and longer operation times appear to show more count discrepancy (p<.001). Conclusions: The count process involves multiple counts at different stages of the procedure, creating the opportunity for systems errors and adverse events. Numerous systems factors have contributed to a count discrepancy including: cases with high complexity, emergency procedure, multiple services, weekend surgeries, longer surgeries (> 4hrs), and higher volume of staff. Implications for Policy, Delivery or Practice: Even if in case counts were documented as correct, surgical counts are not always sufficient for zeroerror surgery. Thus, identifying the relationship between surgical incorrect counts and actual retained objects are needed. In addition, staffing patterns in consideration of fewer rotations and appropriate work time also needs to be developed. Last, further studies should explore whether specific strategies and technologies for screening of highrisk patients in peri-operative process need to be established to reduce count discrepancy. Funding Source(s): Medline Poster Number: 35 Discharge Against Medical Advice: Are the Risks of 30-day Readmission and Mortality Greater? Presented by: Justin Glasgow, M.S., Graduate Student, CRIISP, Iowa City VA 152, 601 Highway 6 West, Iowa City, IA 52246-2208; Phone: (319) 3380581, ext. 3538; Email: justin.glasgow@va.gov Co-authors: Mary Vaughn-Sarrazin, Ph.D.; Peter Kabolie, M.S., M.D. Research Objective: With 1-2% of patients leaving the hospital against medical advice (AMA), there is concern that these patients may suffer increased rates of adverse health outcomes post-discharge. The objective is to determine if patients leaving AMA from a Veterans Administration (VA) hospital experience greater adverse health outcomes as measured by 30-day hospital readmission and mortality rates. Study Design: Case-control study of all patients discharged from VA hospitals between 2004 and 2008. Primary outcome measurements are 30-day mortality and all-cause hospital readmission. Bivariate analyses were used to compare cases and controls on demographics and comorbidities. Separate multivariable Cox proportional hazard models were generated to identify independent risk factors associated with 30-day mortality and readmission. Population Studied: Over the 5 year period, there were 2,204,703 medical admissions to the 129 VA hospitals. Patients that were discharged to a nursing home (6.13%), transferred to another hospital (2.33%), discharged to a non-standard setting (1.28%) and those who died in-hospital during the index admission (2.68%) were excluded allowing for a comparison of AMA patients (cases) and those with a standard discharge to the community (controls). Principal Findings: In the final sample of 1,930,947 admissions, 32,819 (1.70%) were discharged AMA. Over the five year study period AMA rates were relatively constant ranging between 1.65% – 1.74% of discharges. There was variation observed across the 129 hospitals with AMA discharge rates at the 1st quartile of hospitals ranging from 0.42% – 1.29%, while 4th quartile ranges were 2.40% – 5.46%. AMA patients were younger, more likely to be African American, have low income, and have co-morbid alcohol abuse [For all, X2 df = 1, p<0.001]. Readmission rates (17.7% vs. 11.0%, p<0.001) and mortality rates (0.75% vs. 0.61%, p=0.001) were higher in AMA patients. Cox proportional hazard modeling of readmission adjusting for age, income, hospital discharged from, and comorbidity indicated that discharge AMA was the largest hazard for readmission within 30 days (HR = 1.36, 95% CI 1.32 – 1.40). In the 30-day mortality model discharge AMA was a significant hazard (HR = 1.12, 95% CI 1.00 – 1.26). Conclusions: Patients leaving AMA are at increased risk for adverse health outcomes including hospital readmission and death. Multivariable modeling adjusting for demographic characteristics and the presence of co-morbidities reveals that discharge AMA is an independent risk factor for these adverse health outcomes Implications for Policy, Delivery or Practice: Considering the increased risk of adverse outcomes in AMA patients, hospitals should target these patients for discharge transition interventions. Potential interventions include phone follow-up, home visits, or mental health counseling. Alternatively, identifying and ameliorating the factors that lead to AMA discharges may help to reduce the number of patients who leave before achieving clinical stability. This may include factors related to the healthcare team such as provider communication style, access to social services support, or involvement of family in care decisions. Whether targeting patients before or after discharge, clear communication is likely to play a significant role in improving outcomes. Funding Source(s): University of Iowa Clinical and Translational Science Program Poster Number: 36 Switching Statins in a Medicaid Population: The Health Outcomes and Policy Implications of Formulary Restrictions Presented by: Amie Goodin, M.P.P., Research Assistant, Martin School of Public Policy and Administration, University of Kentucky, 3554 Creekwood Drive #17, Lexington, KY 40502; Phone: (606) 499-0940; Email: ajgood3@uky.edu Research Objective: Two incidences of formulary restrictions on statins by Kentucky Medicaid were analyzed to determine whether or not the preferential coverage and the act of switching statins led to adverse health outcomes in patients that were switched to the preferred drug as compared to patients that continued with their originally prescribed statin therapies. Study Design: Medicaid claims data was utilized to collect a sample of Kentucky Medicaid patients affected by a formulary change (“switch”) in 2002 and in 2008. Inclusion criteria were parameterized as the amount of a statin that the patient had prior to the switch and after the switch, as measured by the medication possession ratio. Information regarding whether or not the patient had a stroke, angina, MI, bypass surgery/angioplasty, hypertension, or died before or after the switch date was collected, and concomitant medications as well as demographic characteristics were controlled for in the analysis. Logistic regression and marginal effects analysis were conducted for each of the two time periods. Population Studied: Kentucky Medicaid patients who refilled a prescription for simvastatin, atorvastatin, rosuvastatin, or simvastatin/ezetimibe at least once in the 60 days prior to the date of the formulary change (“switch date”) in 2002 or in 2008. Principal Findings: The difference in age distribution between 2002 and 2008 is striking. It is clear that statins are being prescribed increasingly to younger patients. Patients are typically female and have about a 40% chance of having diabetes. Incidents of MI and stroke are very low across 2002 and 2008 patients, though death appears more frequently in patients that stopped taking all statins after the switch date. The percentage of patients who died after the 2002 switch is much higher than that of 2008 and this is most likely due to the longer period of data collection for 2002 patients. When controlling for demographic characteristics and comorbidities, there is a statistically significant relationship between stopping all statins and death. Age was a significant factor in both the 2002 and the 2008 cohorts, though other risk factors varied between the two time periods. The act of switching statins was only found to be statistically significantly associated with death in 2008, whereas nearly all patients suffering from MI (in 2002), stroke, and angina died within the time frame of the analysis. Conclusions: Formulary restrictions on statins have an impact on health outcomes and the Medicaid population exemplifies many characteristics that make these patients more vulnerable to changes in prescriber behavior than the general population. Implications for Policy, Delivery or Practice: Statins are the top selling class of medications in the United States and costs to tax payers must be balanced with the program’s objective of providing healthcare to the poor and medically indigent. Enacting preferential coverage, though potentially a money saving strategy, can backfire if patients suffer worse health outcomes and need additional services or hospitalizations as a result of inconsistencies in the continuity of treatment. Poster Number: 37 Community Help-Seeking among Part D Beneficiaries Presented by: Melissa Hensley, M.S.W., M.H.A., Doctoral Candidate, George Warren Brown School of Social Work, Washington University in St. Louis, One Brookings Drive, Campus Box 1196, St. Louis, MO 63130; Phone: (314) 725-6283; Email: mahensle@wustl.edu Research Objective: To use qualitative research techniques to explore mentally ill Medicare beneficiaries' use of community helpers such as pharmacists, nurses, and social workers to interpret and utilize their Part D benefits. Study Design: The study used the technique of focused ethnography to obtain in-depth interview information from 26 Medicare beneficiaries with mental illness. Population Studied: Adults with mental illness who were receiving Medicare benefits and were participating in a psychosocial rehabilitation program. Principal Findings: Medicare beneficiaries with mental illness reported a high degree of reliance on community helpers in order to choose an appropriate Part D plan, utilize their benefits, and obtain and utilize their prescription medications. Adults with mental illness reported particularly intense and important relationships with their pharmacists. Conclusions: Community helpers such as pharmacists, nurses, and social workers play an integral role in helping adults disabled by mental illness to utilize their prescription drug benefits. Many adults with mental illness would have great difficulty utilizing their benefits if they did not have these sources of assistance. Implications for Policy, Delivery or Practice: Public sources of funding, such as the Medicare Medication Therapy and Management Program, as well as Medicaid and community mental health funding for nurses and social workers, should continue to support these important community helpers as they work to assist adults disabled by mental illness to get the most out of their benefits. Funding Source(s): National Institutes of Health Poster Number: 38 Cost-Sharing for Colorectal Cancer Screening in Medicare Managed Care Plans, 2001-2008 Presented by: Priya Hirway, M.S., Student, Community Health, Brown University, 121 South Main Street, Providence, RI 02912; Phone: (401) 863-3172; Email: priya_hirway@brown.edu Co-authors: Amal Trivedi, M.D., M.P.H. Research Objective: Although colorectal cancer (CRC) screening reduces deaths from colorectal cancer, less than half of patients receive intervalappropriate screening. Increasing out-of-pocket costs for preventive services has been demonstrated to reduce their use. We therefore determined the cost-sharing amounts for CRC screening services among all Medicare managed care (MMC) plans from 2001-2008. Study Design: Using benefits data from all MMC plans, we determined each plan’s required copayment or coinsurance for CRC screening services (e.g. screening flexible sigmoidoscopy or colonoscopy) within all insurance products offered by the plan. For plans with a range of cost-sharing amounts, we assigned the median value. We tested whether the number of plans requiring cost-sharing and the amount of the mean copayment or coinsurance increased over time using the chisquare and t-tests. Population Studied: All Medicare managed care beneficiaries per year from 2001-2008. The sample size ranged from approximately 6.5 million beneficiaries in 2001 to over 10.5 million in 2008. Principal Findings: The proportion of MMC plans that charged a copayment or coinsurance for colorectal cancer screening services in any of their insurance products increased from 13% to 38% from 2001 to 2008 (p<0.0001). The proportion of MMC enrollees in cost-sharing plans also increased, from 9% in 2001 to 35% in 2008, (p<0.0001). While no plans required coinsurance in 2001, 180 plans (29%) required coinsurance in 2008. Among plans charging a copayment, the mean copayment for colon cancer screening services increased from $12 in 2001 to $50 in 2008, (p<0.0001). The mean coinsurance remained stable at 20% throughout the study period. For enrollees of plans with cost sharing, the mean age was 71.2 years, and 72.1 years for those in plans without cost sharing (p<0.01). The proportion of enrollees who were black or living in areas of low income and education were similar in plans with and without cost-sharing. Conclusions: The number of MMC plans requiring cost-sharing for CRC screening services and proportion of MMC enrollees exposed to such costsharing increased substantially from 2001 to 2008. Among plans that imposed cost-sharing, the use of coinsurance increased in frequency. Implications for Policy, Delivery or Practice: Given the importance of screening in the early detection and treatment of colorectal cancer, the increase in cost-sharing for this preventive service may have negative health consequences. Poster Number: 39 What Can We Expect from the Meaningful Use of Health Information Technology? Presented by: Michael Hoaglin, B.S., Policy Analyst / Medical Student at University of Pennsylvania, Office of the National Coordinator for Health Information Technology, Department of Health and Human Services, 1425 Locust Street Unit 2F, Philadelphia, PA 19102; Phone: (202) 5560077; Email: mhoaglin@med.upenn.edu Co-authors: Melinda Beeuwkes Buntin, Ph.D. Research Objective: The Centers for Medicare and Medicaid Services (CMS) recently issued a proposed rule defining the "meaningful use" of health information technology (HIT) which will qualify providers for Medicare incentive payments. We use the lens of meaningful use to review the literature on the benefits of electronic health records (EHRs). Specifically, we systematically review the HIT literature to determine whether EHR systems meeting more of the proposed meaningful use criteria produce greater health gains and cost savings than more basic EHRs. We also develop a framework to test a set of hypotheses about which patients will benefit the most from EHRs. For example, we hypothesize that EHRs will have greater positive effects for patients with complex care needs and those treated in multiple settings -but may not significantly improve patient outcomes where available evidence does not lend itself to clinical decision support (CDS) or during acute episodes of illness addressed in a single patient encounter. Study Design: We updated the systematic HIT literature review conducted by Goldzweig et al. (Health Affairs 2009) and are stratifying the studies by setting, patient population, and the functionalities of the HIT systems used. Population Studied: Searches of the literature indexed in PubMed turned up 5776 additional articles published since Goldzweig et al.'s review: we expect 200 of these to ultimately meet our review criteria. We will also conduct a search of industry and consultant reports, the Cochrane Database of Reviews of Effectiveness, and popular periodicals. Principal Findings: Preliminary review of the recent literature appears to confirm some of our hypotheses: studies examining the effects of HIT coupled with secure health information exchange (HIE) show better outcomes in terms effectiveness and cost. In the same spirit, settings using computerized provider order entry (CPOE) with a well-designed CDS system show quality and cost gains, as opposed to CPOE alone. In acute medical situations, HIT enhances outcomes for conditions in which timeliness of therapy and data-driven decision-making are determinants of success. At the same time, there are published examples of systems which were implemented poorly or lacked sophistication, contributing to greater inefficiencies and risks to patients. Conclusions: The widespread use of advanced, interoperable HIT systems has the potential to yield greater gains in clinical effectiveness and efficiency than would be expected from the earlier literature examining EHR systems lacking decision support features and the ability to exchange data. In addition, these gains can be expected to be greater among patients with more complex illnesses. Implications for Policy, Delivery or Practice: The programs mandated under the 2009 federal stimulus bill as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act are intended to drive increases in the adoption and meaningful use of interoperable electronic health records. This review indicates that giving providers incentives to achieve meaningful use can be expected to yield health gains and cost reductions -- but challenges remain in the areas of EHR implementation and the development of products that are easier and less expensive to adopt. Funding Source(s): DHHS/ONC Poster Number: 40 Unintentional Poisoning Mortality Trends by Sex, Age and Cause in Taiwan, 1986-2007 Presented by: Yu-Chen Hung, M.S, Graduate, Public Health, National Defense Medical Center, No.161, Section 6, Min-Chuan East Road, Taipei, 114 Taiwan; Phone: +886287923100 ext. 18445; Email: style2498@hotmail.com Lead Author: Wu-Chien Chien, Ph.D Research Objective: To examine the trends of unintentional poisoning mortality in Taiwan by sex, age, and cause between 1986 and 2007. Study Design: We analyze routine mortality data from the official publications of vital statistics from 1986 to 2007 to determine trends by sex, age and cause of death. Linear Regression was used to test the trends. Population Studied: population-based Principal Findings: A total of 12,916 people in Taiwan died as a result of unintentional poisoning between 1986 and 2007. It showed the downward trend in total mortality rate, a decline of 73.6%. The unintentional poisoning mortality rate of male was higher than female (rate ratio: 2.07). Unintentional poisoning mortality rate increased by age, but the mortality rate of all age groups declined. Pesticide (38.3%) and drug (33.7%) were two dominant poisoning agents, yet both the mortality rates declined. The former had the largest decrease (96.1%), then, the later has become the first leading cause of death since 2000, rising 71% from 2000 to 2007. Carbon monoxide mortality rate, the third poisoning agent (9.42%), increased 27%, but the change wasn’t significant during the 22-year period, then, as the second agent since 2002. Conclusions: Although unintentional poisoning mortality rate declined, we should still make more efforts on developing prevention programs to reduce drug or carbon monoxide mortality in the future. Implications for Policy, Delivery or Practice: Basic preventive approaches include eliminating the manufacture or sale of an agent, reducing the length of exposure or the concentration of the poison to non-injurious doses, preventing access to the substance, changing its chemical formulation, and providing appropriate emergency and therapeutic measures. Poster Number: 41 Mental Health Diagnosis and Treatment on AsthmaRelated Services in Medicaid Youth with Asthma Presented by: Eric Jamoom, M.P.H., M.S., Health Services Research, Mangement and Policy, University of Florida, PO Box 100195, Gainesville, FL 32610; Phone: (352) 246-5957; Email: jamoom@phhp.ufl.edu Co-authors: Jeffrey Harman, Ph.D.; Allyson Hall, Ph.D.; Marilyn Dumont-Driscoll, M.D., Ph.D.; David Janicke, Ph.D.; Paul Duncan, Ph.D. Research Objective: An association between asthma and mental health has been well documented. However, quantifying the association of mental health comorbidities, such as depression, anxiety, and attention-deficit hyperactivity disorder (ADHD) on asthma-related health services use and expenditures in youth with asthma and the factors which may mitigate asthma-related utilization in this group remains an area that requires more attention. Therefore, the study aims to understand the impact of specific mental health diagnosis (e.g., ADHD, depression, anxiety) on asthma-related use and expenditure and to understand the role mental health treatment plays on the relationship between mental health and asthma-related use and expenditure. Study Design: This specific study design uses a quasi-experimental, interrupted-time series over 36 months with no-treatment control group. A fixed effect (FE) method was used to quantify the differences in asthma-related cost and utilization among those with a mental health diagnosis of depression, anxiety, and ADHD. Also, a fixed effects approach was used to determine whether mental health treatment mediated asthma-related use and expenditures for those with a mental health diagnosis. Mental health treatment was measured using any treatment and continuous months of treatment (chronicity of treatment). Dependent variables included asthma-related services (ED visits, med/physician claims, inpatient admissions, outpatient visits), asthma-related costs (inpatient, outpatient, med/physician, pharmacy, and total). All analyses were controlled for sex, race/ethnicity, month, and ssi status. Population Studied: Youth with asthma on between age 5 years and 15 years enrolled in Florida Medicaid over three years from 2002 through 2005. Principal Findings: Precursory findings of this population suggest that specific groups of youth with asthma had different asthma-related experiences by mental health diagnosis and mental health treatment. Conclusions: Limitations associated with this study include the common underreport of depression, anxiety, and ADHD in claims data, inability to assess asthma severity, limited framework, external validity limited to Florida Medicaid youth 5-15 years of age, and ICD-9 coding in claims data are often unreliable. Further research is warranted to investigate the impact of asthma in the general nonMedicaid population, as well as examine the impact of mental health diagnosis on other common chronic conditions. Implications for Policy, Delivery or Practice: Effective screening and treatment protocols for youth with asthma may improve health quality and reduce medical costs. Poster Number: 42 Examining Racial Disparities in Persistent Depression and Mental Health Treatment Utilization Presented by: Audrey Jones, Ph.D. Student, Health Services, University of California, Los Angeles, 650 Charles E. Young Drive, 31-269 CHS, Los Angeles, CA 90095; Email: jonesa@ucla.edu Co-authors: Vickie Mays, Ph. D., M.S.P.H. Research Objective: The purpose of this study is to examine how access to different modes of psychiatric treatment is related to racial disparities in the persistence of Depression and Dysthymia. Study Design: Data were obtained from the Collaborative Psychiatric Epidemiologic Surveys; three national surveys that examined the prevalence and correlates of DSM-IV psychiatric disorders. DSM-IV diagnoses were assessed using the World Mental Health Composite International Diagnostic Interview. Persistence was defined as meeting the criteria for Depression or Dysthymia in the last year among those with a history of the disorder. Participants were asked about their history of mental health treatment including medication, counseling or psychotherapy, speaking with medical providers, using alternative treatments, speaking with spiritual or religious provider, and self-help strategies such as hotlines, support groups, or the internet. Logistic regression models were run to examine disparities in treatment utilization for each of the six treatment modalities. Logistic models were run to examine disparities in the persistence of Depression or Dysthymia after controlling for treatment utilization. Finally, stratified models were used to examine the differential effects of treatment utilization across the racial / ethnic groups. All of the models controlled for sociodemographic characteristics, insurance, age of onset, suicide history, and psychiatric comorbidity. Population Studied: Analyses were restricted to 1,791 Non-Hispanic White, Black, Latino, and Asian adults who met the DSM-IV criteria for Depression or Dysthymia at least two years ago. Principal Findings: All three minority groups were less likely than Non-Hispanic Whites to use formal treatment services (speaking with a medical provider, receiving counseling or psychotherapy, or medication treatment). Minorities with a disorder were also less likely to use informal treatment services (religious provider, alternative treatment, and self-help) though the results varied by treatment and racial group. All minority groups were more likely than Non-Hispanic Whites to meet the criteria for a persistent disorder. These effects remained after controlling for differential use of formal and informal mental health treatment. Use of counseling / psychotherapy and self-help strategies were associated with lower persistence. Use of alternative treatments was associated with greater persistence. Speaking with a medical provider, speaking with a religious provider, and use of medication treatments were not associated with persistence after controlling for the other treatment modalities. In the stratified analyses, counseling / psychotherapy, self-help strategies, and alternative treatments were associated with persistence among White adults. However, none of the treatment modalities were associated with persistence in the models for Black, Latino, or Asian adults. Conclusions: Racial minorities with a psychiatric disorder were less likely to receive treatment and more likely to than Non-Hispanic Whites to meet the criteria for a persistent disorder. Some forms of treatment were associated with lower persistence among White adults, but most forms of treatment were not associated with the course of Depression or Dysthymia among the minority groups. Implications for Policy, Delivery or Practice: Recent reports have highlighted racial differences in persistence. More information is needed regarding treatment effectiveness for minority groups as well as cultural factors that may influence the course of depression. Funding Source(s): AHRQ Poster Number: 43 Factors Influencing the Presence of Nursing Home Based Certified Nurse Aid Training Programs Presented by: Hye-Young Jung, B.A., Department of Community Health, Brown University, 121 South Main Street, Box G-S121, Providence, RI 02912; Phone: (401) 863-3172; Email: hye-young_jung@brown.edu Co-authors: Denise Tyler, Ph.D.; Zhanlian Feng, Ph.D.; Vincent Mor, Ph.D. Research Objective: The Omnibus Budget Reconciliation Act of 1987 mandated that all certified nursing assistants (CNA) receive at least 75 hours of training. Previous research indicates a significant decline in facility-based CNA training programs over last decade despite an overall increase in CNA staffing levels. However, no studies have attempted to identify influences leading to the decline. The objective of this study is to identify the determinants of NH based CNA training programs. Study Design: This was an observational, longitudinal design testing for the annual presence of a NH based CNA training program. Fixed effects were included in each model to adjust for time invariant state characteristics and year to year trends. Generalized estimating equations were utilized to account for the longitudinal nature of the data and to adjust the standard errors for repeated observations. Using a discrete-time logit model has the benefit of accommodating both the binary outcome and repeated observations associated with the same facility over time, in addition to accounting for duration effects. Population Studied: Data came from the On-Line Survey Certification and Reporting System. Freestanding NHs with 20 or more beds in the period 1998 through 2008 were included. A total of 15,230 NHs (144,344 facility years) were used in logistic regressions. For the discrete time logistic models, 42,231 facility-years (8720 NHs) were identified as at risk of dropping CNA training programs, whereas 83,311 facility-years (13,488 NHs) were recognized as at risk of adopting programs. Principal Findings: The prevalence of NH based CNA training programs fell from 34.8% in 1998 to 22.8% by 2008. Estimates from the discrete time logit model indicate that a high deficiency score was a strong contributor to NHs dropping CNA training programs (OR 1.56, p < .001), as was being located in an urban area (OR 1.29, p < .001). Large NHs (OR 1.34, p < .001) were more likely to adopt programs, whereas facilities with more CNA hours per resident day were less likely to adopt them (OR 0.68, p < .001). Other organizational factors, such as profit status, chain affiliation, and market competition were also shown to be significant determinants of program status. Logistic estimates were consistent with these results. Conclusions: NHs’ total deficiency score, a measure of regulatory compliance, is an important determinant of whether a NH maintains a CNA training program. Strict state regulations presumably lead to involuntary program termination. A relatively abundant supply of alternative training sites in urban areas may explain why facilities in urban areas are more likely to drop CNA programs, while NHs with insufficient CNA staffing levels are more likely to adopt them. Implications for Policy, Delivery or Practice: The majority of CNA training programs are facilitybased, but their prevalence is steadily declining. Other training sites are increasingly supplying CNAs. Understanding both the organizational and market forces leading to CNA training programs shifting away from NHs provides insight for proper regulatory and oversight adjustments. More importantly, it raises questions about the quality of CNA training and its potential influence on the quality of care received by residents. Funding Source(s): NIA Poster Number: 44 Using Administrative Data to Identify Patients at Risk of Hospital Readmission within 30 Days: The Development of an Algorithm to Identify High Risk Patients Presented by: Jillian Jweinat, B.S., Rush University, Chicago, IL; Phone: (650) 303-6423; Email: Jillian_Jweinat@rush.edu Co-authors: Tricia Johnson, Ph.D.; David Ansell, M.D., M.P.H.; Raj Behal, M.D., M.P.H.; Susan Huerta, Ph.D., M.S., R.N.; Shannon Sims, Ph.D., M.D. Research Objective: The need to systematically identify and intervene on patients at high risk for readmission is critical as a means to improve quality and decrease costs. Little evidence exists about how to measure the risk of readmission. Existing publicly available algorithms for patients at risk for readmission have been developed in other countries or on narrowly defined subsets of U.S. patients using administrative and patient data. When existing algorithms are applied to a broader U.S. patient population, different factors may be important predictors of 30-day readmission, and the costs savings trade-offs will likely differ. In response to this need, Rush University Medical Center (RUMC) committed to developing and validating a predictive algorithm to assess the likelihood for readmission within 30 days of hospital discharge for acute care patients. Study Design: Data for all adult hospital discharges between July 2008 and June 2009 were obtained from the RUMC Financial Data Mart, an administrative database of all hospital discharges. All adult patients age 18 or older who were discharged alive were followed for 30 days to determine whether they were readmitted to RUMC. A binary logistic regression model was fit to estimate the relationship between 30-day readmission and sociodemographic factors, carerelated factors and severity of illness. The performance of the model was tested using sensitivity and specificity. The algorithm was developed using 75% of the sample and validated on the remaining 25%. Principal Findings: A total of 17,265 unique patients were discharged from RUMC during the study time period, with 1,789 (10.4%) readmitted at least once within 30 days of discharge. Of those readmitted, 1,478 (8.6%) were readmitted once; 265 (1.5%) were readmitted twice; and 46 (0.3%) were readmitted three or more times. Predictors included being male; discharged to an inpatient rehabilitation facility or home under the care of an organized home health service organization; general surgery and cardiovascular/thoracic surgery attending physician department; length of stay greater than 4 days; and specific comorbidities including coronary heart failure, renal failure, metastatic cancer, coagulation deficiency and deficiency anemia. The discriminatory power of the algorithm was modest as determined by area under the receiver operating characteristic curve for the development (c=0.690) and validation (c=0.709) samples. Using a cut value of 0.1, the sensitivity was 61.9% and the specificity was 64.7% on the development sample and 68.6% and 61.3% on the validation sample. Conclusions: Hospitals can develop a risk stratification methodology based on their own patient populations using electronic data. Routine administrative hospital episode statistics can be used to identify patients who are at high risk of suffering from multiple readmissions. Implications for Policy, Delivery or Practice: Factors common to those readmitted within 30 days can be determined and interventions around discharge planning and care coordination at the hospital level to keep high-risk patients from being readmitted again can be developed. Systematic identification of patients at high risk for readmission has the potential of reducing avoidable rehospitalizations and unnecessary costs in the health care system. These results are particularly important, with health care reform efforts focused on reducing avoidable readmissions. Poster Number: 45 Diabetic Care in General Practice: An Assessment of Who Guidelines Followed by General Practitioners Presented by: Rukhsana Khan, M.B.B.S., M.P.H., M.Sc., Doctor, Epidemiology, Health Services Academy, Health Services Academy, Park Road, Chak Shehzad, Islamabad, Pakistan; Phone: +00923445509238; Email: drrukhsanakhan@hotmail.com Lead Author: Hameed Durrani, M.B.B.S., M.S.P.H. Research Objective: The aim of the study is to improve the outcome of diabetics by assessing the proportion of the general practitioners following WHO guidelines for the management of diabetes mellitus in Rawalpini city of Pakistan. Study Design: Descriptive- Cross Sectional Population Studied: General Practitioners of Rawalpindi City were selected and interviewed for their knowledge regarding signs, symptoms, laboratory diagnosis, treatment, complications and education of the diabetics as per WHO guidelines Principal Findings: reasonable number of GPs have knowledge of signs, symptoms, and complications of the disease but surprisingly only 17% of the total responded correctly regarding laboratory diagnosis, 61% regarding treatment and 40% educate the patient about the disease. As far as application of knowledge to manage the patient is concerned, only 5% of the total GPs were found following complete (100%) of the WHO guidelines for diabetes management. Conclusions: the general practitioners underdiagnose under-educate the diabetics as per WHO guidelines Implications for Policy, Delivery or Practice: This study provides preliminary but important information about the standards of diabetes care in Pakistan, a country which is already facing steep increase in diabetes prevalence and complications. Improving quality of life for persons with diabetes and reducing morbidity and mortality are major health-care challenges for providers and governments in developing countries. Funding Source(s): Health Services Academy Poster Number: 46 Logic Modeling for Policy Analysis: A Case Study of HIV Testing Policy Change at the VA Presented by: Erika Langer, Department of Health Policy and Management, Boston University School of Public Health, 715 Albany Street, Boston, MA 02118; Phone: (617) 414-6991; Email: elanger@bu.edu Research Objective: Since 2006, both the Centers for Disease Control and Prevention (CDC) and the Department of Veterans Affairs (VA) have issued revised HIV testing policies. These agencies operate within a U.S. context where 1.2 million people are estimated to be living with HIV, and more than 25% of those infected do not know their status. Despite widespread cost-effectiveness of HIV screening in a majority of health care settings, there are a significant number of missed opportunities for testing, and HIV-positive individuals continue to be identified late in the disease process. This study evaluates the extent to which a recent change in VA’s HIV testing policy reflects the current CDC guidance on HIV testing. Using logic modeling, the study compares components of the final rule, “Elimination of Requirement for Prior Signature Consent and Preand Post-Test Counseling for HIV Testing”, published by the VA in the Federal Register in July 2009, and the 2006 Revised Recommendations for HIV Testing from CDC. Agencies' use of research evidence in justification of policy components is also examined. Study Design: This case study is a policy analysis of VA HIV testing policy adoption in 2009. Logic modeling was conducted to examine the sequence of events thought to bring about desired change, as well as the evidence base used to justify linkages between policy components. CDC and VA logic models were analyzed for the extent of policy overlap. Principal Findings: VA has largely replicated the policy logic underlying CDC guidance formulation. The agency draws from a setting-specific evidence base to justify components of its HIV testing policy change. While evidence was given in support of policy resources, activities, outputs, and outcomes, arguments about the longer-term impact of this policy lacked a clear basis of research evidence support. Conclusions: Research utilization differs between policy formulation and adoption stages as contextualized justifications become more relevant to policy argument. By identifying research utilization along the policymaking process, researchers may begin to evaluate how the evidence base for policy changes over time and across settings. This is significant to our understanding of the conditions for evidence-based health policymaking. Implications for Policy, Delivery or Practice: This study aims to identify instances of applied research evidence within policy formulation and adoption decisions as a mode of planning for future policy implementation and evaluation. The use of logic modeling also allows for explicit examination of the actors, context, and content which interact along this process. Findings from this study may inform future evaluation of VA HIV testing policy change, and have additional utility to other health care settings that may be considering adoption of CDC HIV testing recommendations. Poster Number: 47 Patient-Provider Language Concordance and Colorectal Cancer Screening Presented by: Amy Linsky, M.D., Department of Public Health, Health Services Research, Boston University, 64 Perry Street, Brookline, MA 02446; Phone: (617) 277-0148; Email: mcintnm@gmail.com Lead Author: Nathalie McIntosh, M.Sc. Co-authors: Amy Linsky, M.D.; Howard Cabral, Ph.D.; Lewis Kazis, Ph.D. Research Objective: Colorectal cancer (CRC) screening rates are lower in racial and ethnic minorities, and patient-provider language barriers may play a role. Professional interpreters and language-concordant providers may mitigate this disparity. The purpose of this study is to assess the association of the presence of patient-provider language concordance with CRC screening in patients who do not speak English at home compared to rates in those who do. Study Design: We did a retrospective cohort study using the 2002, 2004 and 2006 Medical Expenditures Panel (MEP) Surveys. MEP surveys are nationally representative surveys of noninstitutionalized US civilians. The primary independent variable created three cohorts: English-Concordant (spoke English at home), Other Language-Concordant (did not speak English at home but someone at their provider’s spoke their language or offered translation services), and Language-Discordant (did not speak English at home and no one at their provider’s spoke their language or offered translation). The primary outcome of current CRC screening was defined as receipt of fecal occult blood testing within the past 2 years or endoscopy within the past 5 years. Covariates included: race/ethnicity, age, sex, education, marital status, income, employment, time since last check-up, insurance, physical component score, year, and region. Using survey methods, multivariate logistic regression assessed the association between language concordance and CRC screening. Population Studied: US adults 50 years and older who had no history of colorectal cancer and who completed Medical Expenditures Panel Surveys in 2002, 2004 and 2006. Principal Findings: The final study sample of 23,297 represents 222 million individuals. The majority spoke English at home (96%). English Concordant (n=21,594) were likely to be white nonHispanic (84%) and have a high school education, high income and private insurance. Other Language-Concordant (n=1,463) were likely to be Hispanic (61%), less educated, poor and have public insurance. Other Language-Discordant (n=240) had the highest percentage of Asians (29%) and were likely to be older, unemployed and uninsured. Compared to English speakers, nonEnglish speakers had lower adherence to CRC screening [30.7% vs. 50.8%; Odds Ratio (OR), 0.63; 95% Confidence Interval (CI), 0.52-0.77]. In adjusted analyses, compared to EnglishConcordant, Other Language-Discordant had similar adherence [adjusted OR, 0.83; 95% CI, 0.58-1.20], while Other Language-Concordant had lower adherence [adjusted OR, 0.58; 95% CI, 0.460.72]. Conclusions: Rates of CRC screening are lower in adults who do not speak English at home and were not mitigated by having someone at the provider's who spoke the patient's language. Implications for Policy, Delivery or Practice: Racial and ethnic disparities in CRC screening rates can not be attributed soley to patients' access to someone at their provider's who speaks their language. Other social determinants of health, such as culture, acculturation, and the quality of patientprovider communication may need to be addressed to overcome this health disparity. Poster Number: 48 Factors Associated with Proton Pump Inhibitor Discontinuation in Nursing Home Residents Presented by: Amy Linsky, M.D., Fellow, General Internal Medicine, Boston Medical Center, 801 Massachusetts Avenue, 2nd Floor (GIM), Boston, MA 02118; Phone: (617) 414-2792; Email: amy.linsky@bmc.org Co-authors: John Hermos, M.D.; Elizabeth Lawler, D.Sc.; James Rudolph, M.D., S.M. Research Objective: Continued use of medications, beyond initial indications or targeted endpoints, contributes to over-medication in elderly patients. Proton pump inhibitors (PPIs) are commonly prescribed drugs that are often initiated and continued without clear indication. As nursing home admission is an opportunity for review of medication appropriateness, this study sought to identify factors associated with PPI discontinuation among patients admitted to nursing homes. Study Design: Retrospective cohort study of veteran nursing home patients prescribed PPIs on admission. Baseline exposure to oral PPIs required an active inpatient prescription within the first three days of admission. The primary outcome was PPI usage (“continuation” or “discontinuation”) at 90 days. Covariates included patient sex, age, year of nursing home admission, comorbidities, and prior PPI use, defined as a VA prescription in the 30 days prior to admission. Multivariable logistic regression and 95% confidence intervals (CI) estimated the associations of patient characteristics with PPI discontinuation. Population Studied: The study population included patients, age 40 years and older, admitted to Veterans Affairs (VA) Community Living Centers in 2005-2006 for a minimum stay of 90 days. We identified 26,743 patients, of whom 6,416 (24%) were prescribed a PPI at nursing home admission. Principal Findings: Of baseline PPI users, 2,006 (31%) had the medication discontinued by 90 days while the remaining 4,440 (69%) patients were continued on PPIs. Compared to those with continued PPI use, patients discontinued were similar in age (median age 66 vs. 67 years, p=0.8) and sex (97.4% vs. 96.9% male, p=0.3). There were no statistically significant differences between continuers and discontinuers in prevalence of ICD9-CM coded comorbidities, including diabetes, hypertension, cardiovascular disease, chronic kidney disease, liver disease, malignancy and substance abuse. Those who discontinued were more likely to have prior PPI use (79% vs. 72%, p<0.0001), be admitted in 2006 rather than 2005 (53% vs. 34%, p<0.0001) and have dementia (7.2% vs. 5.7%, p=0.01). Discontinuers were less likely to have chronic obstructive pulmonary disease (COPD) (33% vs. 38%, p=0.0005) and gastric acid or reflux related upper gastrointestinal disorders (34% vs. 42%, p<0.0001). In an adjusted model, factors associated with increased odds of PPI discontinuation were dementia [odds ratio (OR) 1.4; 95% CI 1.1-1.7] and prior PPI use (OR 1.6; 95% CI 1.4-1.8). Diagnoses of upper gastrointestinal disorders (OR 0.68; 95% CI 0.60-0.76) and COPD (OR 0.85; 95% CI 0.76-0.96) were associated with a decreased odds of discontinuation. Conclusions: Within 90 days of admission to a VA nursing home, PPI prescriptions were more likely to be discontinued in patients with prior PPI use - that is, not initiated in the nursing home - and those with dementia. Patients with documented upper gastrointestinal diseases and COPD were less likely to have PPIs discontinued. Implications for Policy, Delivery or Practice: These findings would suggest a reasoned evaluation of PPI needs at early stages of care, but the extent to which physician and system level factors, as well as patient functional status and concurrent medication use, impact decisions of medication discontinuation remains to be elucidated. Funding Source(s): VA Poster Number: 49 The Relationship Between a Physician Incentive Plan and the Hospital Performance Presented by: Nai Yng Liu, M.S., student, Accounting, National Taipei University, 2F.-8, No.5, Fuhe Road., Yonghe City, Taipei County 234, Taiwan (R.O.C.), Taipei, 23449 Taiwan; Phone: +011886960111392; Email: naiyng@gmail.com Research Objective: In this study, we investigate the appropriateness of incentive plans that link physicians’ compensation to the measurement of their performance in a large Taiwan private not-forprofit hospital. Study Design: The main research question in our study is investigated the relationship between a physician incentive plan and the hospital performance. Hospital performance is measured by profitability and efficiency. We use the multiple regression model to examine the relationship between the size of cash bonuses and hospital profitability. The Data Envelopment Analysis (DEA) model is used to measure the operational efficiency of each department in the case hospital. Then, a multi-factor tobit model is used to examine factors that might influence hospital efficiency to examine the effectiveness of the incentive plan. Population Studied: Monthly financial data and related information for twenty-six departments during the period from January 2007 to June 2009 were provided by the case hospital. Principal Findings: When evaluating the relationship between physicians and cash bonuses, we found that physicians’ cash bonuses are significantly negative to hospital performance and efficiency. Using current incentive plan measurement, the case hospital’s per employee productivity contribution is significantly (p<0.001) negative to physicians’ cash bonuses. Meanwhile, the directed costs, most of which can be controlled by physicians, are significantly (p<0.001) negative to the incentive payment too. In addition, using multi-factor tobit model to evaluate the efficiency, we learnt that the case hospital is less efficiency when implementing cash bonuses. Conclusions: Case hospital’s current incentive plan, which based on physicians’ medical practice quantity, jeopardizes its financial situation and decreases its efficiency. The case hospital should design an incentive plan that includes multidimension measurement, such as cost control and efficiency improvement. The case hospital needs to modify its current incentive plan; this inappropriate incentive plan will decay its competition and even might let case hospital facing bankruptcy. Implications for Policy, Delivery or Practice: Our study contributes to the literature by providing empirical evidence that examines the appropriateness of performance measures in physician incentive plans for the healthcare industry. The study also offers useful lessons for practitioners concerning pitfalls (e.g., dysfunctional behavior) to avoid when they design incentive plan for physicians. Poster Number: 50 Impact of Financial Incentives on Physician EMR Implementation and Functionality Use: A Statewide Survey Presented by: Chang Liu, Student, Community Health, HSR Section, Brown University, Box GS121, 121 South Main Street, Providence, RI 02912; Phone: (401) 523-7299; Email: chang_liu@brown.edu Co-authors: Amal Trivedi, M.D., M.P.H.; Rosa Baier, M.P.H.; Rebekah Gardner, M.D. Research Objective: In the context of an economic downturn and the soaring cost of health care, and with limited evidence linking EMRs to improvements in health outcomes at a national level, the federal government is planning an ambitious program to align financial incentives on the implementation and functionality use of computerized patient records. The objective of my research is to justify the costeffectiveness of this approach before a substantial investment is enacted. Study Design: Based on the 2009 Physician HIT Survey of Rhode Island, an annual survey conducted by the Rhode Island Department of Health, we assessed the current state of EMR implementation and functionality use among physicians in active practice in Rhode Island, and compared these results to national and regional data derived from previous studies. Moreover, in this cross-sectional study, we examined the relationship between financial incentives and the possibility of adoption and utilization of EMRs by a two-step regression model. Population Studied: In early 2009, the Rhode Island Department of Health (HEALTH) conducted and administered the 2009 Physician HIT Survey to all 3,248 physicians licensed in Rhode Island. Rhode Island was the first state in the nation to report individual-level measures of health information technology adoption for all licensed physicians. In our study, we excluded respondents who did not have a record in HEALTH’s licensure file, who were not in active practice or providing direct patient care, and whose licensure state was not Rhode Island, Connecticut, or Massachusetts. The overall response rate of the survey was 58.1% (n=1,888). Principal Findings: Based on responses from 58.1% of licensed physicians in both office-based and hospital-based settings, we found that in 2009, 67.6% of the physicians in Rhode Island had some EMR components in their practice, 12.5% of them had “qualified” EMRs (22.7% if CCHIT certification is excluded), and 41.2% of them were eprescribing. On average, responding physicians scored 63.6 (out a possible 100 for maximum use) for “basic” EMR functionality use, and 44.1 for “advanced” EMR functionality use. These results are much higher than the average performance of physicians nationwide. After controlling for the physician and organizational characteristics (e.g., practice setting, practice size, and hours of direct patient care), we found that physicians who were eligible for financial incentives were more likely to adopt and use EMRs than physicians who were not eligible. Conclusions: Our study suggests that aligning financial incentives to physicians may play a crucial role in accelerating the implementation and functionality use of electronic medical records. Implications for Policy, Delivery or Practice: We support the proposed federal program that provides incentive payments to physicians to adopt and “meaningfully use” certified EMRs. Funding Source(s): Rhode Island Department of Health Poster Number: 51 Validating the Post Operative Hip Fracture PSI in the VA Presented by: Julie Lynch, R.N., M.B.A., Research Assistant and Student, Nursing, University of Massachusetts, Boston, 100 Morrissey Boulevard, Boston, MA 02125; Phone: (617) 6995032; Email: julie.lynch001@umb.edu Co-authors: Ann Borzecki, M.D.; Amy Rosen, Ph.D.; Sally MacDonald, R.N. Research Objective: To examine the Agency for Healthcare Research and Quality(AHRQ) post operative hip fracture Patient Safety Indicator (PSI) in the Veterans Health Administration for criterion validity. Secondary analysis was conducted to analyze presence of multisite pain and diagnosis of osteoarthritis in patients. Study Design: The AHRQ’s PSI software was applied to 2003 to 2007 inpatient administrative data from a representative sample of 28 VA hospitals to identify flagged cases of post operative hip fracture. Fourty-six cases were identified. Trained nurse abstractors conducted a retrospective chart reviews of the electronic medical record to determine rates of true positives (TPs) and false positives (FPs). Interrater reliability testing of 2 nurse abstractors was performed on 10% of charts. Cases were examined with respect to baseline clinical characteristics, operative procedures and completeness of a fall risk assessment. Medical records of all cases were then reviewed to analyze reports of multisite pain and diagnosis of osteoarthritis in patients with hip fracture. Population Studied: Surgical admissions between fiscal years 2003-2007 in 28 acute care Veterans Administration Hospitals Principal Findings: Of the 46 cases analyzed, 13 (28%) were true positives (positive predictive value of 28%, and 33 (72%) were false positives. Of the 33 false positives , 24 (70%) were determined to be present upon admission; 5 (15%) patients had falls that occurred in hospital but prior to an operative procedure; 3 (9%) patients were inaccurately coded; 1 (6%) patient had a medical event (stroke) which excluded him. Findings related to presence of multisite pain and diagnosis of osteoarthritis is ongoing. Conclusions: Limiting hip fracture to a secondary diagnosis does not exclude many cases with a hip fracture present upon admission. Low numbers of posterative hip fracture cases identified in this study supports findings by Iezzoni et al. (1994) that postoperative hip fracture continues to be a rare event. 69% of true positives had no fall assessment or were rated as being at no fall risk depsite having many obvious risk factors such as mobility impairment or prior history of falls. Implications for Policy, Delivery or Practice: A present upon admission indicator is needed to identify hip fractures that exist on admission. Chart review of administrative data identified cases of postoperative hip fracture PSI remains a necessary and recommended step for hospitals prior to reporting this measure. Although a rare event, postoperative hip fracture is a complication that is sensitive to nursing interventions to reduce fall risk. Therefore fall risk assessment should be standard of care. Fall risk assessment policies, procedures, and tools should be evaluated by all hospitals to ensure tools are meeting the objective and nurses are adequately trained to conduct fall risk assessment and implement interventions to reduce fall risk. Funding Source(s): VA Poster Number: 52 Racial and Mental Health Disparities in Safe Sex Counseling for Individuals with Substance Dependence Presented by: Meredith Manze, M.P.H., Research Coordinator, Section of General Internal Medicine, Boston Medical Center, 801 Massachusetts Avenue, #2098, Boston, MA 02118; Phone: (617) 414-8441; Email: meredith.manze@bmc.org Co-authors: Debbie Cheng, Sc.D.; Donald Allensworth-Davies, M.Sc.; Jeffrey Samet, M.D., M.A., M.P.H.; Richard Saitz, M.D., M.P.H., F.A.S.A.M., F.A.C.P. Research Objective: Despite a higher prevalence of sexual risk behaviors among people with substance dependence than in the general population, little is known about racial/ethnic and mental health disparities in safe sex counseling and behavior among such people. We sought to identify whether these disparities exist, accounting for sociodemographic variables and quality of patientclinician relationship. Study Design: This study was a cross-sectional analysis using self-reported interview data. Race/ethnicity and mental health were our key independent variables. Three mental health variables were evaluated: depression (9-item Patient Health Questionnaire (PHQ-9) score > 10), psychotic symptoms (?2 symptoms from the BASIS 24 selected items), and any manic/hypomanic episodes (Mini International Neuropsychiatric Interview). Patient self-report of their regular doctor having 'ever talked to them about safe sex' and 'ever practiced safer sex because of their doctor’s advice' were the two dependent variables (Primary Care Assessment Survey (PCAS)). The PCAS “trust” and “communication” scales were used to assess the quality of the patient-clinician relationship. We performed multiple logistic regressions, controlling for age, education, gender and PCAS scale scores, to test associations between mental health and race/ethnicity with each outcome. Each model contained only one mental health variable and one PCAS scale due to correlation among variables. Population Studied: We analyzed data from 275 participants with alcohol and/or drug dependence who indicated they had a regular doctor. Principal Findings: The majority of participants were male (68%) and had at least a high school education (77%); mean age was 40. Most participants had a PHQ-9 score greater than 10 (53%), and reported at least two psychotic symptoms (56%); 40% reported any manic/hypomanic episodes. The mean scores for the trust and communication scales were 73 and 75, respectively (0-100 scale). The majority of participants reported having their regular doctor talk to them about safe sex (71%) and practicing safer sex because of their doctor’s advice (61%). Compared to non-Hispanic Whites (reference group), being Hispanic or non-Hispanic Black race/ethnicity was associated with significantly greater odds of receiving safe sex counseling (adjusted odds ratio (AOR) 2.67, 95% CI:1.01, 7.09; AOR 2.74, 95% CI:1.43, 5.27, respectively) and practicing safer sex due to the advice (AOR 3.76, 95% CI: 1.47, 9.63; AOR 2.26, 95% CI: 1.26, 4.07, respectively). Patients who reported any manic/hypomanic episode had more than two times the odds of reporting having a doctor ever talk to them about safe sex (AOR=2.54, 95% CI: 1.38, 4.70), but no significant association with practicing safer sex as a consequence. We did not detect associations between depression and psychosis with reports of safe sex counseling or practicing safer sex. Conclusions: Minorities and patients with manic episodes appear more likely to receive safe sex counseling and, for minorities, to practice safer sex as a result. The increased counseling for minorities may be in response to their higher rates of unintended pregnancy and sexually transmitted infections. Implications for Policy, Delivery or Practice: Future research should explore provider perceptions of risk of unsafe sex, particularly for minorities and people with mental illness, and why more counseling may not translate into safer sex behaviors for people with manic episodes. Funding Source(s): NIAAA Poster Number: 53 Comparative Effectiveness of Surgery for Lumbar Spinal Stenosis in Older Adults: Trends, Major Medical Complications, and Charges Associated with Surgical Invasiveness Presented by: Brook Martin, Ph.C., M.P.H., Health Services Research Scientist, Comparative Effectiveness, Cost, and Outcomes Research Center, University of Washington, 325 Ninth Avenue; Campus box 359736, Seattle, WA 98104; Phone: (206) 744-1803; Email: bim@u.washington.edu Lead Author: Richard Deyo, M.D., M.P.H. Co-authors: Brook Martin, Ph.C., M.P.H.; Jeffrey Jarvik, M.D., M.P.H.; William Kreuter, M.P.A.; Sohail Mirza, M.D., M.P.H. Research Objective: The fastest growth in lumbar surgery has occurred in older patients with spinal stenosis. Trials indicate that for selected patients, decompressive surgery offers an advantage over non-operative treatment, but surgeons often recommend more invasive fusion procedures. Comorbidity is common in elderly patients, so benefits and risks must be carefully weighed in the choice of surgical procedure. We examine trends in use of different types of spinal stenosis operations and the association of complications, healthcare use, and costs with surgical complexity. Study Design: Retrospective cohort analysis of Medicare claims data for 2002-2006 was used to examine surgical trends. We then focused on 2005 to assess complications and resource use. Operations were grouped into 3 gradations of invasiveness: decompression alone, simple fusion (one or two disc levels, single surgical approach) or complex fusion (more than 2 disc levels or combined anterior and posterior approach). We used multivariate logistic regression, controlling for age, comorbidity, previous spine surgery, and other patient characteristics, to examine the association between surgical invasiveness and serious complications, rehospitalizations within 30 days, and nursing home discharges. Costs were estimates by applying Medicare cost-to-charge ratios to reported charges. Population Studied: Medicare recipients undergoing surgery within U.S. acute care hospitals for lumbar stenosis. We examined trends in overall surgical rates using data from 2002-2006, and then focused on 2005 data (n=36,165) to assess complications and costs associated surgical invasiveness. Principal Findings: Overall surgical rates changed little from 2002-2006, but the rate of complex fusion procedures increased 14-fold, from 1.3 per 100,000 in 2003 to 18.2 per 100,000 in 2006. The risk of lifethreatening complications increased with increasing surgical invasiveness. Compared to decompression alone, the adjusted odds ratio (OR) for life threatening complications among patients undergoing complex fusion was 3.04 (95% CI 2.583.59). A similar pattern was observed for rehospitalization within 30 days (OR 1.98; 95% CI 1.77-2.21) and probability of discharge to a nursing home (OR 2.67; 95% CI 2.42-2.95). Adjusted mean hospital charges for complex fusion procedures were $24,517 compared to $6,593 for decompression alone. Conclusions: Use of complex procedures for spinal stenosis among the Medicare population is increasing, and is associated with greater risk of major complications, mortality, and resource use. Implications for Policy, Delivery or Practice: These findings suggest a need to improve indications for more invasive lumbar spinal stenosis surgery; to involve patients in informed decisionmaking; and to determine the safest and most effective surgical techniques. Funding Source(s): NIAMS Poster Number: 54 An Intervention to Improve Medication Adherence in a Vietnamese Population Under Care for One or More Chronic Conditions Presented by: Jennifer Mason, B.A.; B.S.; M.P.H., Graduate Student, Public Health, San Diego State University, 5500 Campanile Drive, San Diego, CA 92182; Phone: (619) 594-6317; Email: jaymay6@gmail.com Research Objective: The aim of the study is to learn whether increasing patient knowledge about their medications through individual counseling and the use of compliance aids (pill boxes) improves pill-taking behaviors. Study Design: The study design was a prospective randomized pilot study with an enrollment of 8 weeks. Population Studied: The participants were recruited from the Linda Vista Health Care Center in San Diego, California with the inclusion criteria that they were at least 21 years of age, Vientamese and being treated for hypertension, high cholesterol, diabetes and/or asthma. Principal Findings: Significant improvements in pill-taking behaviors were found by self-report with the introduction of pill box usage and baseline education on medicine regimen delivered by a pharmacy student. Additional outcomes on biological measures including lipid panels, glucose levels and blood pressure readings are currently being analyzed. Conclusions: Final write-up and conclusions are currently being drafted. Implications for Policy, Delivery or Practice: Potential benefits are improving chronic disease management for high-risk populations in a community health clinic setting. Further, potentially improve patient-provider relations due to increased knowledge of decision making between traditional values and Western medicine. Poster Number: 55 The Impact of Mental Health/Cognitive Disability Upon Healthcare Utilization: Perspectives from Patients and Healthcare Providers Presented by: M. Maya McDoom, M.P.H., B.S., Ph.D. Candidate, Health Policy and Management, Boston University School of Public Health, 715 Albany Street T3W, Boston, MA 02118; Phone: (617) 414-1362; Email: mmcdoom@bu.edu Co-authors: Mari-Lynn Dranioni, Ph.D., M.Ed. Research Objective: The US Census estimates nearly one in five persons have some type of disability, comprising 54.4 million people. Of the one in five persons, approximately 16.1 million have some level of mental health or cognitive disability . Persons with disabilities often face undue barriers in accessing health services and medical treatment. Differences in perceived barriers to healthcare access between healthcare providers and persons with disabilities can influence the health care experience. This study evaluated the perceptions of barriers to healthcare access between persons with disabilities and healthcare providers. Study objectives were to: 1. assess the impact of disability upon healthcare service utilization; 2. examine the relationship between disability and barriers to healthcare access; 3. determine if a relationship exists between healthcare provider type and perceptions of barriers to healthcare; and 4. compare perceptions of persons with disabilities about their barriers to healthcare to providers’ perceptions. Study Design: Retrospective database review of de-identified survey data examining patientperceived barriers to care compared with healthcare provider perceptions of barriers to care. Population Studied: Persons with disabilities receiving Medicaid benefits enrolled in an HMO and healthcare providers in the state providing care to the population grouped into five categories: outpatient mental health, inpatient mental health, outpatient medical, inpatient medical, and dentists Principal Findings: Persons with mobility limitations had higher odds of utilizing overnight hospital services (OR 1.48, p 0.0298), lower odds of outpatient mental health (OR 0.648, p 0.015) and inpatient mental health services (OR 0.566, p 0.040) compared to those who do not have mobility limitations. Persons with mental health and cognitive disabilities had higher odds of utilizing outpatient mental health, dentists, and inpatient mental health services. Persons with mobility and cognitive limitations had higher odds of experiencing barriers related to need and understanding. Over half of providers indicated daily care for persons with mobility, mental illness, or cognitive limitations. Strikingly, there were significant differences in perception of barriers by provider type. Dentists (OR 4.00, p 0.0012) and outpatient mental health/substance abuse providers (OR 2.52, p 0.0102) were more likely to perceive inadequate insurance coverage compared to outpatient medical providers. Inpatient medical (OR 0.626, p 0.037) and inpatient mental health/substance abuse providers (OR 0.581, p 0.023) were less likely to perceive inadequate insurance coverage compared to outpatient medical providers. Dentists also had higher odds of perceiving barriers related to entering buildings, exam rooms, and restrooms. Conclusions: Health care access is an important issue, but persons with mental health or cognitive disabilities can face barriers to accessing healthcare beyond what can be physically observed. Healthcare providers’ often have very limited awareness and understanding of the barriers of persons with cognitive or mental health disabilities. Implications for Policy, Delivery or Practice: The perception gap between healthcare providers and persons with mental health or cognitive disabilities highlights the importance of addressing the specific needs of persons with different types of disabling conditions rather than assuming that all persons with disabilities face the same challenges in accessing healthcare. There is a need to reduce barriers to care through improvements in medical training, health care practice settings, and health care coverage. Poster Number: 56 Dental Utilization and Edentulism Across Three County Types: Urban, Rural, and High Poverty Rural Presented by: Jordan Mitchell, M.B.A., Research Associate, Health Services Policy and Management, South Carolina Rural Health Research Center, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210; Phone: (919) 760-5650; Email: jpm0901@gmail.com Research Objective: Issues with utilization and access to care, such as lower incomes, lower employment, and the low-density of dentists contribute to people in rural areas being more vulnerable to oral health problems as compared to their urban counterparts. In all income ranges, dental care is deemed as a lower priority than other medical care; thus with the added employersponsored dental insurance variable added to the equation, preventative dental visits are utilized at a much lower rate in rural areas than other medical visits. While there is little literature available on SES and racial impacts on dental visits and tooth loss, there is less information on the rural/urban impact as well as the combination of high-poverty and rural and its impact on dental visits and tooth loss; this paper seeks to address this gap of information. Study Design: Analyses were conducted using data from the Behavioral Risk Factor Surveillance System (BRFSS) from the Centers for Disease Control (CDC) and the Area Resource file (ARF) from Health Resources and Services Administration (HRSA). HRSA is the funding source for this project. All analyses were carried out by SAS and SAS-callable SUDAAN, in order to account for weighting and the complex sample design. Weights were assigned based on the probabilistic factors affecting the selection of a residential phone number by state, adjusting for differences by area codes/regions, number of adults in each household, and non-coverage and non-response. The U.S. Bureau of Census provided data to add weights for the variables of age, sex, race/ethnicity, and household size. Population Studied: The population included individuals 18 years of age and older in the BRFSS survey. Principal Findings: Lower dental visits were significantly (p<.05) related to: males, ages 25-44, Blacks, fair/poor health status, unemployed, some high school – some college attainment, divorced/separated, presence of a chronic disease, cost deferrals, and per-capita incomes of less than $29,972. Higher dental visits were significantly related to: being insured, having a usual source of care, and not being edentulous, and having at least one dentist per a population of one thousand. Higher edentulism rates were significantly associated with: Black, “other” races, fair/poor health status, unemployed, some high school – some college educational attainment, divorced/separated, presence of a chronic disease, cost deferrals, and per-capita incomes of less than $29,972. Lower edentulism rates were associated with: all ages less than 65, being insured, and having at least one dentist per population of one thousand. No significant associations were found by county-type and dental visits/edentulism. Conclusions: While controlling for all variables studied, county type was not significantly associated with differences in dental visits or edentulism at the 95% confidence level. This being said, there are associations at a lower confidence level that influence dental visits and edentulism in the different county types, which need policy changes to ameliorate. Implications for Policy, Delivery or Practice: Possible policy changes could include focusing on dentist availability within rural and especially highpoverty rural areas, dental education in rural counties and incentives for dentists to practice in these disparate areas. Funding Source(s): HRSA Poster Number: 57 Provision of Rehabilitation Therapy in Home Health: Does Payer Matter? Presented by: Tracy Mroz, M.S., Graduate Student, Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, 149 Archimedes Court, Pikesville, MD 21208; Phone: (484) 226-0174; Email: tmroz@jhsph.edu Research Objective: 1) To examine the relationship between primary payer and receipt of home health occupational and physical therapy services; and 2) to examine the relationship between primary payer and number of home health occupational and physical therapy visits. Study Design: This study was a secondary analysis of cross-sectional survey data from the 2007 National Home and Hospice Care Survey (NHHCS) publically-available patient file. Outcomes included dichotomous variables for receipt of OT, PT, or any therapy services and continuous variables for number of OT and PT visits. The key independent variable was primary payer: Medicare, Medicaid, or private insurance. Logistic and linear regression models adjusted for current episode length, age, gender, race, marital status, living arrangement, caregiver presence, cognitive status, functional status, and number of diagnoses. Population Studied: The population studied was adult home health patients in the US. The study sample included 3,647 home health patients aged 35 and over. Using NHHCS-provided weights to account for sampling design yielded a weighted sample of 1,070,682 home health patients, of which approximately 40 percent received either OT, PT, or both therapy services. Principal Findings: Patients with Medicaid as primary payer were significantly less likely to receive any therapy services compared to Medicare patients (adjusted OR (95% CI): .34 (.17-.69); p<.01). Patients with private insurance as primary payer did not differ significantly in receipt of any therapy services with respect to Medicare patients (adjusted OR (95% CI): .72 (.46-1.12); p=.15). A similar pattern of findings persisted when examining receipt of OT and PT services separately. Of the patients who were receiving home health therapy services, Medicaid patients received on average 1.5 fewer PT visits and 2.0 fewer OT visits than Medicare patients, though these differences were not statistically significant (p=.08 and .06 respectively). Privately insured patients received more similar numbers of visits compared to Medicare patients, on average .98 fewer PT visits (p=.15) and .11 fewer OT visits (p=.91). Conclusions: Provision of home health therapy services appears to vary to some extent by primary payer. Medicaid patients are less likely to receive occupational and/or physical therapy services compared to Medicare patients, while privately insured patients receive therapy at rates more similar to Medicare patients. When home health therapy services are received, however, there does not appear to be significant variation in the number of visits per patient by primary payer. Implications for Policy, Delivery or Practice: Changes in Medicare and Medicaid payment policy may help reduce variation in receipt of home health therapy services with respect to primary payer; however, whether therapy services are over-utilized by Medicare or under-utilized by Medicaid remains unclear without linking these data to patient outcomes. Poster Number: 58 Use of Trigger Tools to Detect Adverse Events in Ambulatory Surgery Presented by: Hillary Mull, M.P.P., Research Health Scientist, Research, VA Boston Healthcare System, 150 S. Huntington Avenue, Boston, MA 02130; Phone: (857) 364-2766; Email: hjmull@bu.edu Co-authors: Kamal Itani, M.D.; Haytham Kaafarani, M.D., M.P.H.; Kathleen Hickson, R.N., M.N.; Amy Rosen, Ph.D. Research Objective: Numerous healthcare systems in the U.S., including the Veterans Health Administration (VA), use the National Surgical Quality Improvement Program (NSQIP) to detect surgical adverse events (AEs). The current NSQIP sampling methodology excludes many routine ambulatory surgeries from review. Given the low prevalence of ambulatory surgical AEs, NSQIP may not detect enough events to highlight areas in the ambulatory setting to focus quality improvement initiatives. Trigger tools, algorithms derived from clinical logic to flag cases where AEs have most likely occurred, could potentially complement NSQIP by detecting a higher yield of ambulatory surgeries with a true surgical AE. Study Design: We developed four ambulatory surgical AE trigger algorithms based on clinical input and empirical testing. We compared the number of trigger-flagged surgeries from Oct. 1, 2007 to Sept. 30, 2008 (FY08) using both inpatient and outpatient administrative data from VA Boston Healthcare System (HCS) to the 322 surgeries reviewed in FY08 by VA Boston NSQIP. Using the NSQIP chart review results as the gold standard for AE detection, we refined the triggers to improve sensitivity and specificity. To determine whether our triggers could reliably detect surgical AEs, we ran the triggers on the 783 ambulatory surgeries VA Boston NSQIP excluded from review. A trained nurse abstractor reviewed the trigger-flagged cases using the VA electronic medical record and NSQIP chart abstraction guidelines. We calculated the ratio of true events over flagged events (i.e., the positive predictive value (PPV)), and the 95% confidence interval (CI) for each trigger. Principal Findings: Of the 29% of ambulatory surgeries reviewed by VA Boston NSQIP in FY08, nine had a surgical AE. Five of the nine AEs were detected by at least one of the ambulatory surgical AE triggers. A total of 198 (25.3%) of the 783 surgeries excluded by VA Boston NSQIP in FY08 were flagged by one or more of the four triggers and underwent nurse review. Final trigger algorithms and results were as follows: (1) flagged surgeries with at least one emergency department or urgent care visit within 30 days: PPV = 19% (CI: 11-29%); (2) Flagged surgeries where the patient was admitted to the hospital with a length of stay greater than 24 hours: PPV = 33% (CI: 12-62%); (3) Flagged surgeries where the patient had a hospital admission within 30 days: PPV = 33% (CI: 19-51%); and (4) Flagged surgeries where the patient had at least one primary care visit and one specialty care visit within 30 days: PPV = 6.2% (CI: 2-12%). Conclusions: Compared to 2.8% of surgeries found by NSQIP, 14.1% of the charts flagged by one of the four ambulatory surgical AE triggers were found to have a surgical AE. Because our results are based on a relatively small sample, further research is necessary to confirm these findings. Implications for Policy, Delivery or Practice: Our results suggest that trigger tools have the potential to complement NSQIP’s current sampling design by increasing the yield of ambulatory surgeries with surgical AEs. Improved detection of AEs in the ambulatory surgery setting is critical to ensure patient safety and quality of care. Funding Source(s): VA Poster Number: 59 Racial Differences in Patients' Preferences about Care-Seeking Presented by: Saira Nawaz, M.P.H., Student Researcher, Health Services Research, The Dartmouth Institute for Health Policy and Clinical Research, 30 Lafayette Street, 1st Floor, Lebanon, NH 03766; Phone: (603)-653-3268; Email: saira.nawaz@dartmouth.edu Lead Author: Denise Anthony, Ph.D. Co-author: Laura Yasaitis Research Objective: Disparities in health service use between Black and White patients have been well documented. Explanations for these disparities include lack of health insurance and access to care, variations in income and education, and poor communication and mistrust in the patient-physician interaction. Preferences in care may also drive these differences. The study’s objective was to examine the association between race and patients’ stated preferences for seeking outpatient and specialty care. Study Design: Analyzed survey items that elicited stated preferences for care in two clinical scenarios: chest pain upon walking up the stairs and a lingering cough after an episode of the flu. Outcomes included whether respondents preferred to see a doctor right away, whether they would want cardiac tests or chest X-ray and if they would want to see a specialist. Odds ratios of preference for care-seeking in black vs. white respondents were adjusted for age, sex, median household income, self-reported health, education, self-efficacy and average number of physician office visits in the respondent’s Hospital Referral Region (HRR). Population Studied: Random sample of 4000 Medicare Beneficiaries and an over-sample of 700 Blacks among community-dwelling beneficiaries who were age 65 or older as of July 1, 2003, were entitled to Part A and/or Part B, and who were residents of a US Hospital Referral Region in 2003 and 2004. Principal Findings: Blacks (n=489) were more likely to be younger, female, report that finances were ‘important’ in healthcare decisions, live in areas with lower median household income, have less education, rate their health as ‘fair’ or ‘poor’ and live in HRRs with a higher number of yearly physician office visits per beneficiary, compared to Whites (n= 2110). If experiencing a lingering cough, Blacks were more likely to want to see a doctor at two days rather than wait (45.9% vs 26.6%, adjusted OR=2.03), to request an x-ray even if the doctor told them it was unnecessary (72.3% vs 54.9%, adjusted OR=1.98) and to want to see a specialist even if the doctor told them it was unnecessary (54.1% and 38.1%, adjusted OR=2.36). Blacks were more likely to want to see the doctor right away if they experienced chest pain (59.9% vs 43.3%, adjusted OR=1.94) and to want to see a specialist even if they were told it was unnecessary (70% vs 52.8%, adjusted OR=1.90). Conclusions: Given evidence that Blacks receiver fewer health services compared to Whites, and may avoid or resist health services, we might have expected that Blacks would be less likely to say that they would seek doctor visits or tests when experiencing new symptoms. Yet our results show that Black Medicare beneficiaries are significantly more likely than White beneficiaries to say they would seek visits and tests, even after adjusting for socio-demographic factors. Implications for Policy, Delivery or Practice: Physicians should undergo training in shared decision-making and cultural competency, which have been shown to effectively elicit patient preferences for care. Using Medicare Claims data, our future research will assess whether Black or White patients are more able to assert their stated preferences. Poster Number: 60 Effect of Increased Copayments on Use of Outpatient Mental Health Services among Medicare Managed Care Enrollees Presented by: Chima Ndumele, M.P.H., Graduate Student, Community Health, Brown University, 121 South Main Street, Providence, RI 02912; Phone: (617) 947-0205; Email: chima_ndumele@brown.edu Co-authors: Amal Trivedi, M.D., M.P.H. Research Objective: The impact of increased costsharing on use of mental health services is not well understood, particularly among the elderly. Furthermore, whether vulnerable populations exhibit selective sensitivity to changes in cost sharing for mental health treatment is also unclear. We examined the effects of increased mental health copayments on use of outpatient mental health services among a nationwide sample of elderly individuals in managed care plans, as well as within racial subgroups. Study Design: We used a difference-in-differences (DID) design to assess changes in the proportion of enrollees who received outpatient mental health services in Medicare plans that increased mental health copayments compared to the concurrent trend in matched control Medicare plans that did not increase copayments. We selected all Medicare plans that increased copayments by at least 25% after two consecutive years of stable copayments. We matched concurrent control plans on the basis of US census region, tax status, and model type. The study period was from 2001 to 2007. Analyses were restricted to continuously-enrolled beneficiaries. We constructed generalized linear models that adjusted for age, sex, race, area-level socioeconomic status, clustering within health plans using fixed-effects and repeated measurement of enrollees using GEE. We conducted stratified analyses for white and black enrollees. Population Studied: 601,378 Medicare managed care beneficiaries age 65 and older enrolled in 14 Medicare plans that increased mental health copayments and 404,633 beneficiaries enrolled in 14 matched control plans. Principal Findings: Among the 14 case plans, mean mental health copayments increased from $14.43 to $21.07. In control plans, mean mental health copayments were unchanged at $21.43. Among case plans, the proportion of enrollees that received outpatient mental services declined from 2.4% to 2.3% (P=0.16). Among control plans, the concurrent change was from 1.4% to 1.3% (p=0.07). The adjusted DID was 0.006 percentage points (95%CI -0.002-0.14; p=0.11) Among the 14 case plans, only 4 experienced declines in the proportion of enrollees receiving outpatient mental health services relative to the concurrent trend in the matched control plan. In stratified analyses, the adjusted DID for black enrollees was 0.001 percentage points (95%CI -0.003-0.005; p=0.63). Conclusions: Only a small percentage of Medicare Managed Care enrollees use outpatient mental health services. Among this group, cost sharing increases of approximately 50% had a limited effect upon the proportion of patients using outpatient mental health services. This relationship holds true for both black and white enrollees. Implications for Policy, Delivery or Practice: The low prevalence of mental health service use among the elderly may be driven by factors other than costsharing. Poster Number: 61 Rural/Urban Comparison of Nebraska’s Health Care Workforce: A County-Level Analysis Presented by: Anh Nguyen, M.S.P.H., Health Data Analyst, Health Services Research and Administration, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Phone: (402) 559-3295; Email: anguyen@unmc.edu Co-authors: Preethy Nayar, M.D., Ph.D.; Keith Mueller, Ph.D. Research Objective: This study uses Nebraska county-level data to examine the rural versus urban distribution of eight classes of health care professionals and the correlates of county-level health care provider supply. Study Design: Data for eight classes of health care professionals – primary care providers, primary care physicians, physicians, dentists, general dentists, pharmacists, mental health providers, and psychiatrists – were obtained from the 2007/2008 University of Nebraska Medical Center’s Health Profession Tracking Service survey data. Primary care providers include physicians, nurse practitioners, and physician assistants specialized in primary care specialties. Using the 2003 RuralUrban Continuum Codes, the rural versus urban distribution of professionals were examined with descriptive statistics. Correlations were examined between county-level provider-to-population ratios and county characteristics. Population Studied: The study population includes health professionals practicing in all Nebraska counties in 2007-2008. Principal Findings: In non-metropolitan counties, the average provider-to-population ratios for various actively practicing providers to 100,000 population are: primary care providers (89.3), primary care physicians (119.1), physicians (86.2), dentists (35.5), general dentists (34.6), pharmacists (62.0), mental health providers (34.7), and psychiatrists (1.2). The average provider-to-population ratios for physicians, pharmacists, and psychiatrists are below national average or federal health professional shortage area designation benchmark ratios in non-metropolitan counties. In metropolitan counties, the average provider-to-population ratios for various actively practicing providers to 100,000 population are: primary care providers (68.3), primary care physicians (80), physicians (100.2), dentists (40.4), general dentists (36.8), pharmacists (61.6), mental health providers (51.9), and psychiatrists (4.5). The average provider-topopulation ratios for physicians and pharmacists are below national average benchmark ratios in metropolitan areas. Health professionals tend to be actively practicing in more urban counties, highpopulation counties, high-income counties, counties with lower proportions of an aging population, counties with higher hospital admissions-topopulation ratios, and counties with higher infant mortality rates. Conclusions: Overall, rural counties have lower provider-to-population ratios for physicians, dentists, general dentists, mental health providers, and psychiatrists. Implications for Policy, Delivery or Practice: Rural areas in Nebraska face significant challenges in recruiting and retaining health care professionals. The findings from this study have implications for quantifying the need and demand for health care professionals in workforce planning and policy analysis. Poster Number: 62 Determinant of Access to the Systems of Care for Mentally Ill Juvenile Offenders in Texas Presented by: Gul Nowshad, M.B.B.S., M.P.H., Graduate Research Assistant, Management, Policy and Community Health, School of Public Health, UT Houston, 1200 Hermann Pressler, Houston, TX 77030; Phone: (713) 500-9489; Email: gul.nowshad@uth.tmc.edu Co-authors: Sartaj Alam, M.S; Caesa Nagpal, M.B.B.S. Research Objective: This study examined the socio-demographic, clinical characteristics of juvenile offenders coming in contact first time either with mental health system or with juvenile justice system, and defined the determinant of their first time access to the system of care in Houston Texas. Study Design: We did a secondary analysis of the data; consist of records of Harris County Juvenile Probation Department, of all children and adolescents referred to juvenile probation from 1990 until 2005 and Mental Health records between 1992 and 2006, matched through probabilistic matching method. About 25% of individuals present in the juvenile justice database were also present in the mental health database. The sample size of our study was 23,866. Population Studied: Eligible study population, were mentally ill offenders who were 17 years and younger. Principal Findings: In our sample population 30% of the juvenile offenders, first time come in contact with this pool of care (juvenile probation department and mental health system) is through the door of mental health system while 70% of them first got through the juvenile justice system. Females were 25% of the sample population, and more then third (37%) were White. Female adolescents were 22% depressed compared to males (9%), while female adolescents were 2% suffering from adhd and males were 8%. Age, gender, ethnicity, depression, mood disorders, ADHD, impulse disorders, behavioral disorders and substance abuse disorders were found statistically significant with mentally ill juvenile offenders entering in the pool of care through the portal of Juvenile Probation Department. Juvenile offenders who were one year older were 71% and those who used substance abuse were 80% more likely to enter through the justice portal. Male adolescent were two times more likely to enter through the justice portal. Compared to White, African American were 28% and Hispanics were 22% more likely to enter through the Justice door. Similarly kids who were suffering from depression, impulse disorder, mood disorders, ADHD were more likely to get treatment early from mental health system before getting involved with the justice system. Conclusions: Ethnicity, substance abuse, mental illness like depression, impulse disorder and ADHD will predispose our youth to encounter the justice system as a symptom of their disease instead of getting treatment for their illness. Implications for Policy, Delivery or Practice: These finding will enable researcher, judicial personnel and policy makers to understand the determinants and disparity in access to mental health care system. Funding Source(s): Houston Endowment inc. Poster Number: 63 Association Between Survey-Based NurseReported Healthcare-Acquired Infection Frequency and Hospital-Reported Rates Presented by: Danielle Olds, R.N., M.S.N., M.P.H., Pre-doctoral Research Fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania, Claire Fagin Hall, #388, 418 Curie Boulevard, Philadelphia, PA 22203; Phone: (215) 898-5673; Email: danielle.m.olds@gmail.com Co-authors: Linda Aiken, R.N., Ph.D.; Dr. Jeannie Cimiotti, R.N., D.N.Sc. Research Objective: The collection of adverse outcomes data by caregivers is increasingly burdensome. The objective of this research is to determine whether surveys of nurses about infection frequency provide similar estimates to more burdensome hospital reporting requirements. Study Design: This study is a cross-sectional, correlational secondary analysis of nurse survey data and publicly available data on hospital infection rates. Hospital-reported healthcareacquired infection (HAI) rates were obtained from the Pennsylvania Health Care Cost Containment Council’s (PHC4) publicly available report, "Hospital-acquired Infections in Pennsylvania, Calendar Year 2006". In 2006, Pennsylvania hospitals were mandated to report to the PHC4 rates of HAIs including: surgical site, gastrointestinal, multiple, and “other” infections, and device and non-device related pneumonia, bloodstream infection, and urinary tract infection. Thirteen hospitals used electronic surveillance; the other hospitals used traditional clinical surveillance methods. Nurse survey data were obtained in 2006 from a random sample of registered nurses licensed and residing in Pennsylvania. Nurses reported the names of their primary hospital employer so that survey results could be linked to hospitals. The survey queried nurses on the incidence of healthcare-acquired urinary tract infections (UTI), central-line associated bloodstream infections (CLABSI), and ventilatorassociated pneumonia (VAP). Responses were scored on a 7-point Likert-type scale ranging from no infection to every day occurrence. The hospitallevel mean nurse survey response was calculated for each hospital. The appropriateness of aggregating nurse responses at the hospital-level was determined using the intraclass correlation for each infection type. Spearman’s rho correlation was used to compare nurse-reported frequency of HAIs with hospital-reported rates. Population Studied: The study sample included nurses working on inpatient units of 156 acute care hospitals in Pennsylvania that submitted data to the PHC4. Analyses for VAP were restricted to nurses working on intensive/critical care units (146 hospitals). Principal Findings: Intraclass correlations were calculated for each infection. The lowest was UTI (ICC(1,k) = 0.45); and the highest, CLABSI (ICC(1,k) = 0.71). VAP had an ICC (1,k) of 0.46. In order to obtain an adequate intraclass correlation (ICC(1,k) = .60) and aggregate nurse responses at the hospital-level, correlational analyses were limited to hospitals with at least 30 respondents for UTI (52 hospitals) and at least 7 respondents for VAP (126 hospitals). Nurse estimates of HAI frequency were highly correlated with hospitalreported rates for UTI (n = 52, r = 0.40, p = 0.0034); CLABSI (n = 156, r = 0.53, p < 0.0001); and VAP (n = 126, r = 0.34, p = 0.0001). Conclusions: Nurse estimates of HAI frequency are highly correlated with hospital-reported infection rates for UTI, CLABSI, and VAP. UTI and VAP had wider intra-hospital respondent variation, compared to CLABSI. Implications for Policy, Delivery or Practice: Survey-based nurse reports of HAI frequency may be valid estimates when patient data are unavailable, or in combination with shorter periods of intensive reporting that are burdensome for clinicians. These findings also suggest that nurse reports on patient care may be a valuable component of quality improvement. Funding Source(s): National Institute for Nursing Research Poster Number: 64 Correlates of Perceived Risk of Acquiring HIV in a High HIV/AIDS Prevalence Population: Does Age at First Sexual Debut Matter? Presented by: Elijah Onsomu, M.S., M.P.H., Teaching/Research Assistant, Department of Public Health Sciences, University of North Carolina at Charlotte, 9201 University City Boulevard, Charlotte, NC 28223; Phone: (704) 649-6240; Email: eoonsomu@uncc.edu Co-authors: DaKysha Moore, M.S., Ph.D.; James Kimani, M.A., Ph.D.; Ahmed Arif, M.D., Ph.D., F.A.C.E.; James Studnicki, Sc.D., M.B.A., M.P.H. Research Objective: In 2007, there were 33.2 million people living with HIV worldwide, with 85% of Sub-Saharan Africa (SSA) countries experiencing pandemic situations. Of those living with HIV, 22.5 million (>68%) reside in SSA despite only representing 12% of the world population with women and children experiencing the most impact of the disease (UNAIDS, 2007). Two main objectives for this study are: 1) To determine the association between perceived risk of acquiring HIV and age at first sexual debut among men and women, and 2) To identify correlates associated with perceived risk of acquiring HIV among men and women after first sexual debut. Study Design: Retrospective cross-sectional data from Kenya Demographic and Health Survey-2003 were used. Multivariate multinomial logistic regression analysis was performed. Data were weighted for stratum and primary sampling units attaining linearized standard errors. The main outcome variable is perceived risk of acquiring HIV, while the main independent variable-age at first sexual debut-both categorical variables. Parametric testing using Univariate and Multivariate multinomial logistic regression was performed. Stata version 10.1, utilized for all analyses with statistical significance, was set at p<0.05. Population Studied: Two datasets were used: 1) the female dataset (8,195) 94% response rate; and 2) the male dataset (3,578) 86% response rate. The sample included women aged 15-49 years (reproductive age) and men aged 15-54 years. Principal Findings: Fifty four percent of males aged 15-19 perceived themselves to be at high-risk of acquiring HIV compared to females 47%, p<0.001. Before adjusting for confounding, women who had their first sexual debut at 15-19 years were 9.77 times more likely to perceive themselves to be at high-risk of acquiring HIV compared to those who have not had sex at all (95% CI 6.53-14.62, p<0.001). Men who had their first sexual debut at 15-19 years were 4.34 times more likely to perceive themselves to be at high-risk of acquiring HIV compared to those who have not had sex at all (95% CI 2.17-8.690, p<0.001). After adjusting for confounding, women who had their first sexual debut at 15-19 years were 4.14 times more likely to perceive themselves to be at high-risk of acquiring HIV compared to those who have not had sex at all (95% CI 2.47-6.94, p<0.001). Men who had their first sexual debut at 15-19 years were 3.88 times more likely to perceive themselves to be at high-risk of acquiring HIV compared to those who have not had sex at all (95% CI 1.76-8.55, p<0.001). Conclusions: Women and men who had first sexual debut at an earlier age perceived themselves to have a high-risk of acquiring HIV, which increased with decreasing age. Implications for Policy, Delivery or Practice: HIV/AIDS prevention programs need to pay special attention on age at first sexual debut, particularly children and youth when trying to influence and control HIV infections in Kenya. If first sexual debut is not paid enough attention to HIV infections will continue to increase among this age group. Poster Number: 65 Sexually Transmitted Diseases and Circumcision in Kenya: What Role Do They Play in HIV Transmission? Presented by: Elijah Onsomu, M.S., M.P.H., Teaching/Research Assistant, Department of Public Health Sciences, University of North Carolina at Charlotte, 9201 University City Boulevard, Charlotte, NC 28223; Phone: (704) 649-6240; Email: eoonsomu@uncc.edu Co-authors: Ahmed Arif, M.D., Ph.D., F.A.C.E.; James Studnicki, Sc.D., M.B.A., M.P.H.; Judith Cornelius, M.S., Ph.D.; Ayana Moore, Ph.D., R.A.C.; James Laditka, D.A., Ph.D. Research Objective: CDC has found 2-5 folds of HIV infection if one has STD(s) compared to those without an STD(s). Circumcision as a protective factor for HIV has been documented elsewhere. Two objectives were explored in this study: 1) To determine predictors for HIV, and 2) To determine if there is any relationship between STDs, circumcision and HIV acquisition. Study Design: Retrospective cross-sectional data from the Kenya Demographic and Health Survey2003 was used. Data were weighted for stratum and primary sampling units attaining linearized standard errors. The main outcome variable was HIV test results, a dichotomous variable (negative “0” or positive “1”). The main independent variables were STD(s), a dichotomous variable (does not have STD(s) “0” or has STD(s) “1”), and circumcision, a dichotomous variable (circumcised “0” or uncircumcised “1”). Parametric testing using Univariate and Multivariate logistic regression was performed. Stata version 10.1, utilized for all analyses with statistical significance, was set at p<0.05. Population Studied: Three datasets (female, male and HIV datasets) were merged with a sample size of 6,190 retained for the analysis. These comprised those individuals who were offered an HIV test, accepted and took the test. The sample included women aged 15-49 years (reproductive age) and men aged 15-54 years. Principal Findings: 9% (p<0.001) of men who had STD(s) tested positive for HIV compared to 8% of women, p<0.002. Also, 48% of men who tested positive for HIV were not circumcised, p<0.001. STD(s): After adjusting for confounding, women who had an STD(s) were 3.05 times more likely to test positive for HIV than those who did not have a STD(s) (95% CI 1.34-6.96, p<0.008). Men who had an STD(s) were 2.01 times more likely to test positive for HIV than those who did not have a STD(s) (95% CI 0.92-4.40, p<0.08). Circumcision: After adjusting for confounding, uncircumcised men were 4.23 times more likely to test positive for HIV than those who were circumcised (95% CI 2.517.13, p<0.001). Conclusions: STD(s) among women and men, uncircumcised men in Kenya increased ones likelihood of being diagnosed positive for HIV. Implications for Policy, Delivery or Practice: There is need to continuously monitor and test for STD(s) as a routine among those seeking healthcare. Individuals should also be encouraged to seek medical services if they suspect STD(s) symptoms. Cultural barriers need to be addressed in order to encourage circumcision in communities that do not practice circumcision among men. Circumcision should be related to important community cultural health practices. However, participants need to be made aware that being circumcised does not prevent them from being infected with HIV; hence, condom use should be encouraged. Poster Number: 66 Effect of Practitioner on Chronic Opioid Use in Fibromyalgia Syndrome Patients Presented by: Jacob Painter, Pharm.D., M.B.A., Fellow, Pharmaceutical Outcomes and Policy, University of Kentucky College of Pharmacy, 789 S. Limestone, Lexington, KY 40536-0596; Phone: (859) 260-1960; Email: jtpainter@gmail.com Co-authors: Jeff Talbert, Ph.D. Research Objective: Fibromyalgia syndrome (FMS) is an idiopathic, functional disorder characterized by widespread pain. Fibromyalgia syndrome affects approximately 2-4% of the general population of the United States. Patients suffering from fibromyalgia have been shown to have average total healthcare costs about three times higher than sex and age matched controls. According to a 2004 Journal of the American Medical Association clinical review titled Management of Fibromyalgia Syndrome, pharmacologic therapies of FMS can be divided according to the level of evidence for efficacy that exists. This review found that opioids did not have evidence of efficacy for use in the treatment of FMS. Moreover, evidence since that review indicates the possibility of opioid-induced hyperalgesia in patients being treated chronically with opioids. Our previous research shows that within our population there is an elevated level of chronic opioid use in FMS patients. The goal of our current research is to investigate what practitioner factors influence the use of opioids chronically within this population. Study Design: Our overall inclusion criteria are: age 18-64, continuous eligibility for at least 18 consecutive months, two or more healthcare encounters with a diagnosis of fibromyalgia (ICD-9 code 729.1) within a fiscal year. Patients with malignancy were excluded from this analysis, due to differences in treatment patterns between these patient populations. With these criteria we investigate the characteristics of practitioners that lead to the chronic use of opioids in this population. We describe chronic opioid use in this population as having a day supply of opioids greater than 180 days in a single fiscal year. Attributes we are interested in include physician or other, primary care or specialist, type of specialty, practice type, practitioner location type and geographic location. Population Studied: In order to investigate the prescribing behaviors of practitioners treating FMS we examined patient records for drug utilization patterns and cost information. Data is an extract from a health claims data warehouse consisting of eligibility, pharmacy, institutional, and medical services. The database represents the entire medical and prescription claim history for Kentucky Medicaid recipients from January 1, 2000 to June 30, 2009. This database contains medical information such as diagnoses as indicated by International Classification of Diseases (ICD) codes and procedures as indicated by Current Procedural Terminology (CPT) codes. It also contains information on prescription medication utilization such as drug name, strength, day supply, and prescribing physician. Economic cost data includes Medicaid reimbursement rates for all procedures, services, and pharmaceuticals incurred by recipients. Principal Findings: Although research is ongoing, preliminary results show that division of our sample according to whether they have received chronic opioid therapy results in differences in distribution of diagnosing practitioner according to primary care versus specialist and according to specialty type. Conclusions: Our preliminary findings suggest that this research will illuminate differences among practitioner characteristics that can contribute to explaining what leads to chronic opioid use within this disease population. Implications for Policy, Delivery or Practice: Knowledge concerning practitioner characteristics that contribute to chronic opioid use in fibromyalgia patients will be valuable both to policy makers and to clinical practice, providing insight into evidencebased practice adoption trends. Poster Number: 67 Stakeholders’ Views on Medicare’s Policy of Nonpayment for Hospital-Acquired Urinary Tract Infections Presented by: Jennifer Palmer, M.S., Research Assistant, Center for Health Quality, Outcomes, and Economic Research, ENR Memorial VA Hospital, 200 Springs Road, Bedford, MA 01730; Phone: (781) 687-2855; Email: jennifer.palmer1@va.gov Co-authors: Grace Lee, M.D., M.P.H.; Timothy Hoff, Ph.D.; Maya Dutta-Linn, M.P.H.; Peter Wroe, B.A.; Christine Hartmann, Ph.D. Research Objective: The Centers for Medicare and Medicaid Services (CMS) instituted a new policy in 2008 that limits reimbursement for hospitalizations associated with preventable complications, including certain hospital-acquired infections (HAIs). Some of the goals of the policy include increasing awareness of HAIs and promoting HAI prevention. We explored some implications of this policy by exploring stakeholders’ impressions of one of the selected HAIs: catheterassociated urinary tract infections (CAUTIs). Study Design: Because our study was exploratory, we used qualitative methods to investigate participants’ impressions. We purposively sampled hospitals on a national level, stratifying by bed size, geography, and nurse staffing levels. We sought to attain wide representation of variation in each stratification category. We interviewed infection preventionists (IPs) and intensive care unit (ICU) charge nurses using a semi-structured interview guide. The guide included questions about participants’ perceptions of the policy, about how it is being implemented at their site, and about any related consequences they have observed. For data analysis, we employed components of content analysis with adapted tools from grounded theory. Population Studied: Between September 2009 and January 2010, we interviewed 35 IPs and 5 ICU charge nurses from 35 hospitals. We chose these representatives of the field due to their solid understanding of infection control activities in their facilities and their close involvement in institutional response to the new CMS policy. Principal Findings: Participants discussed CAUTIs in relation to the CMS nonpayment policy both in a positive and in a negative light. Positive comments focused on how the policy increases awareness of and adherence to infection prevention practices around CAUTIs. For example, in some facilities the policy prompted changes in the duration of catheter use or in the criteria for catheter insertion, thereby minimizing unnecessary use. Negative comments focused on the limited utility of: 1) prioritizing efforts to prevent CAUTIs, which were perceived to be a minor complication; and 2) diverting administrative and financial resources away from prevention of other infections with higher rates of morbidity and mortality. Furthermore, some participants felt that nonpayment for CAUTIs did not have a large financial impact on their hospitals’ bottom lines. Finally, in larger hospitals, complete prevention of CAUTIs was thought to be difficult in a high-risk patient population. Conclusions: We conducted an in-depth analysis of stakeholders’ views on the selection of CAUTIs as an HAI in CMS’ new nonpayment policy. IPs and ICU charge nurses did not uniformly consider the inclusion of this particular hospital-acquired condition to be either completely founded or unfounded. Further research should examine insiders’ perspectives on other targeted HAIs in the policy and assess the overall impact of this policy on patient outcomes to be sure there are no unintended negative consequences. Implications for Policy, Delivery or Practice: Stakeholders’ varying support for targeting CAUTIs through Medicare nonpayment has larger implications. CMS might benefit from continued careful review of the targeted HAIs since the policy may divert already limited hospital resources away from alternatively important infections and patient populations. Funding Source(s): National Institute of Allergy and Infectious Diseases Poster Number: 68 Racial/Ethnic, Gender, and Socioeconomic Disparities in Diabetes-Related Hospitalizations among Medicare Beneficiaries Presented by: Felipe Pereira, M.H.S., student, Department of Health Policy and Management, The University of Kansas Medical Center, 3901 Rainbow Boulevard, Kansas City, KS 66160; Email: fpereira@kumc.edu Co-authors: Michael Fox, Sc.D.; David Kingsley, Ph.D.; Megha Ramaswamy, Ph.D., M.P.H. Research Objective: Through the implementation of Medicare Part D in 2006, individuals with diabetes gained broader access to coverage for previously limited items, such as insulin and medical supplies associated with injection. This increased access to coverage should result in a decrease in diabetes-related hospitalizations, with the concurrent effect of reducing disparities. Little has been done previously to demonstrate disparities in the risk of diabetes-related hospitalization among the Medicare population over time. The goal of this study is to examine trends in the risk of diabetes-related hospitalizations among Medicare beneficiaries and to determine whether the implementation of Part D was associated with any reduction in disparities. Study Design: We analyzed data from the 20032007 Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project Nationwide Inpatient Sample. We conducted binary logistic regression to examine risk of being hospitalized due to diabetes mellitus with complications. Hospitalizations with diabetes listed as the primary diagnosis were identified in HCUP through the use of the Clinical Classifications Software, or CCS, which collapses ICD-9-CM codes into smaller number of clinically meaningful categories.9 The CCS code utilized was 50, diabetes mellitus with complications, which contains ICD-9-CM codes from 249.xx and 250.xx. The factors for which we controlled in the analysis were race, income quartile where patients reside, and gender. Population Studied: We examined all hospitalizations from the 2003-2007 HCUP NIS for which Medicare was listed as the primary payer. Principal Findings: Racial and ethnic disparities in the risk of diabetes-related hospitalizations remain largely unchanged between 2003 and 2007, although minority groups, particularly Blacks and Hispanics, remain at significantly higher risk of hospitalization compared to Whites. However, gender and income disparities in risk have increased between 2003 and 2007, with males showing significantly higher risk than females, while the risk of hospitalization for those in the lower three income quartiles significantly increased relative to the highest income quartile between 2003 and 2007. Conclusions: The data demonstrates that disparities in diabetes-related hospitalizations persist among racial/ethnic minorities and are growing among men and the poor. The evidence suggests that greater availability of insulin coverage through the implementation of Part D has not reduced disparities in the risk of hospitalization, and in fact may be exacerbating certain disparities. Implications for Policy, Delivery or Practice: Medicare needs to place greater focus on measuring and tracking disparities in high cost, preventable hospitalizations such as those related to diabetes. Additionally, confronting the sources of these disparities is a challenge that Medicare, as a payer of health services, must address through targeted interventions. Poster Number: 69 Attitudes Toward Drug-Eluting Stent Use and Distribution of Regulatory Focus Type among Interventional Cardiologists in New York State Presented by: Feng Qian, M.D., M.Sc., Ph.D. candidate in Health Services Research and Policy, Community and Preventive Medicine, University of Rochester, 601 Elmwood Avenue, Box 644, Rochester, NY 14642; Phone: (585) 275-9496; Email: feng_qian@urmc.rochester.edu Co-authors: Charles Phelps, Ph.D., M.B.A.; Frederick Ling, M.D.; Edward Hannan, Ph.D.; Peter Veazie, Ph.D. Research Objective: The safety of drug-eluting stent (DES) use was called into question in 2006. Literature in psychology suggests that regulatory focus type (promotion vs. prevention) orients physicians toward using different strategies to approach a task: ensuring against errors of omission (promotion) vs. ensuring against errors of commission (prevention). However, the attitudes toward DES use after safety concerns were expressed and the distribution of regulatory focus type among interventional cardiologists are unknown. The objectives of this study are: (1) to examine the attitudes toward DES use among interventional cardiologists in New York State (NYS) after DES safety concerns were expressed, and (2) to investigate the distribution of regulatory focus type among these interventional cardiologists. Study Design: We conducted a questionnaire survey of interventional cardiologists in New York State from October 2008 to April 2009 by mail, email and fax. The questionnaire included face valid items to measure the attitudes toward DES use, valid Regulatory Focus Questionnaire to measure the regulatory focus type, and items collecting demographic information. Population Studied: Interventional cardiologists in New York State. Principal Findings: We received total 119 valid returned questionnaires and the response rate was 47%. There are no statistically significant differences regarding the demographic factors between the respondents and the non-respondents. The vast majority of interventional cardiologists (92%) agreed or strongly agreed that DES is a revolutionary technology and that DES use will increase in the future (70%). The regulatory focus type of interventional cardiologists was predominantly of the promotion type (89%). We found that age and gender were significant predictors of the promotion score, but we did not find any demographic factors were significant predictors of the prevention score. Conclusions: Despite the DES safety issues reported in 2006-2007, interventional cardiologists have a very positive attitude regarding DES use and most of them predict the continual growth of DES use in the future. Such information is valuable in predicting the modality change in coronary revascularization therapy. Furthermore, the vast majority of interventional cardiologists were found to be promotion focused, which means that they are concerned about achieving positive outcomes and they want to prevent errors of omission. Implications for Policy, Delivery or Practice: To the best of our knowledge, this is the first study to report the distribution of regulatory focus type among physicians. As suggested by the theory in psychology, this finding can lead to more effective interventions in conveying medical messages to physicians and changing their behavior. Poster Number: 70 Primary Coronary Revascularization Utilization Pattern Change and Practice Variation in DrugEluting Stent Era in New York State Presented by: Feng Qian, M.D., M.Sc., Ph.D. candidate in Health Services Research and Policy, Community and Preventive Medicine, University of Rochester, 601 Elmwood Avenue, Box 644, Rochester, NY 14620; Phone: (585) 275-9496; Email: feng_qian@urmc.rochester.edu Co-authors: Charles Phelps, Ph.D., M.B.A.; Frederick Ling, M.D.; Edward Hannan, Ph.D.; Peter Veazie, Ph.D. Research Objective: Drug-Eluting Stent (DES), the newest medical device in percutaneous coronary intervention (PCI), was perceived as a revolutionary medical technology due to its substantial reduction of the restenosis rate when it was approved by FDA in April 2003. However, the safety of DES use was called into question in 2006 due to increased late stent thrombosis. Further, literature suggests that practice variations in DES use occurred during the initial adoption period in 2003. The objectives of the study were: (1) to describe the relationship between DES adoption and coronary revascularization utilization pattern change in New York State, and (2) to test the hypotheses: (i) DES played a strong substitution role for Bare Metal Stent (BMS) in 2003 and 2004, (ii) BMS played a strong substitution role for DES in 2006, and (iii) there were medical practice variation in DES use across the study years 2003, 2004 and 2006. Study Design: We used New York State’s Statewide Planning and Research Cooperative System (SPARCS) data, a comprehensive and accurate data base administered by New York State Department of Health, to describe the coronary revascularization pattern change in the DES era and assess the above hypotheses. Since we were not sure how Coronary Artery Bypass Graft (CABG) utilization was affected since DES adoption, we examined the relationship between the CABG and the PCI procedures. Population Studied: Patients who was hospitalized and received primary coronary revascularization during the study period in New York State. Principal Findings: Total 102,078 patients who received the first isolated coronary revascularization procedures were included in the study. Our findings confirmed above hypotheses for the Pearson correlation coefficient r equaled -0.93 (p=0.0003), 0.79 (p=0.002), and -0.77 (p=0.004) for DES and BMS in 2003, 2004, and 2006 respectively. We found that the coefficient of variation (COV) for DES use in primary coronary revascularization in New York State were 0.30, 0.24, and 0.25 for 2003, 2004, and 2006 respectively. However, CABG volume remained stable and was positively correlated with the PCI volume across the above years. Conclusions: There are significant coronary revascularization utilization pattern changes and consistent practice variation in DES use in New York State. Implications for Policy, Delivery or Practice: It suggests corresponding changes in hospital reimbursement and physician reimbursement policies to achieve an optimal rate of revascularization treatments. Future research is needed to identify the causes of practice variation. Poster Number: 71 Medical Tourism: A Systematic Review of the Literature Presented by: Zo Ramamonjiarivelo, M.B.A., Doctoral Student, Health Services Administration, University of Alabama at Birmingham, 603, WEBB Nutrition Sciences Bldg., 1675 University Boulevard, Birmingham, AL 35294; Phone: (205) 239-3462; Email: zoramam@uab.edu Lead Author: Anantachai Panjamapirom, M.B.A., M.S. Co-authors: Gouri Gupte, Ph.D. Candidate, M.H.A.; Zo Ramamonjiarivelo, M.B.A.; Shamly Austin, Ph.D. Candidate, M.H.A.; David Au, B.A. Research Objective: Medical tourism is the concept of travelling to a foreign country to seek medical care. It has grown at a rapid pace during recent years. This study has systematically reviewed the extant literature on medical tourism published up to December, 2009. Specifically, this study contributes to the literature by (1) Specifying the methodology used (2) Listing number of articles published by database (3) Examining number of articles published based on keywords, and (4) Determining the streams in the medical tourism literature and their related sub-streams. Study Design: This study systematically reviewed articles that met the following inclusion criteria: articles that were entirely published in English peerreviewed journals, and articles and abstracts that were available in online databases. The following keywords were used: medical tourism, health tourism, wellness tourism, spa tourism, health seeking travelers, reproductive tourism, dental tourism, fertility tourism, medical outsourcing, and transplant tourism. These 10 keywords were searched in 8 databases: PubMed, ABI/Inform Complete, JSTOR, Science Direct, Springer Link, Wiley InterScience, CINAHL, and Web of Knowledge. The articles’ publication dates were not part of the inclusion criteria to allow a comprehensive analysis of research trends in medical tourism. Principal Findings: Our search yielded a total of 1137 items. Of which, 738 were not journal articles, 33 were duplicates within the same databases and 127 were similar articles in different databases. These were excluded from our analyses. Thus, the study had a final sample of 239 articles. The articles included in our analyses were published in 141 different journals from 1990 to 2009. 30.3% articles were found in Web of Knowledge, 26.8% in PubMed, 17.8% in Science Direct, 9.6% in CINAHL, 6.6% in Wiley InterScience, 4.8% in ABI/Inform Complete, 2.5% in Springer Link, and 1.9% in JSTOR. The keyword search found that 45.6% of the articles could be attributed to medical tourism, followed by transplant tourism (18.4%), health tourism (11.7%), reproductive tourism (10.0%), medical outsourcing (5.0%), dental and fertility tourism (3.3% respectively), spa tourism (1.3%), wellness tourism (0.8%) and health seeking travelers (0.4%). Conclusions: Publication trends in medical tourism reflect a recent increase in interest among researchers. A significant increase in articles published was observed after the year 2000. 2009 saw a sharp increase in the number of articles attributable to medical tourism, transplant tourism, and health tourism. Although publication trends in medical tourism indicate an increase in number of published articles in recent years, the concept has not acquired a clear and universal definition. Our analyses observed an overlap between the 10 keywords used in this study. The exhaustive literature review determined that a dominant and formal journal classification scheme, disciplinedetermined categories, and consensus among medical tourism contributors do not currently exist. Implications for Policy, Delivery or Practice: Lack of a universal definition and understanding of medical tourism creates confusion not only among the recipients and providers of healthcare, but also among scholars, policy makers and third-party payers. An explicit and mainstream definition of medical tourism and a comprehensive analysis on the available literature will benefit these stakeholders. Poster Number: 72 A Study of the Effect of Parental Charateristics and Child Safety Interventions on Childhood Injury Rates Presented by: Leslie Rideout, F.N.P., Pediatric Trauma Nurse Coordinator, Kiwanis Pediatric Trauma Institute, Floating Hospital for Children/Tufts Medical Center, 800 Washington Street, Box 344, Boston, MA 02111; Phone: (617) 636-1380; Email: lrideout@tuftsmedicalcenter.org Research Objective: Injuries are a major health problem for young children. “An estimated one half of all unintentional, nonfatal injuries occur in the home environment” (Scheidt, Harel, Trumble, Jones, Overpeck, & Bijur’s study as cited in Gielen, et al., 2007). The purpose of this study is to assess those factors which influence the utilization of child safety interventions and the resultant impact that this may have on early childhood injury reduction. Hypothesis: Implementation of child safety interventions result in a decrease in injury rates when controlling for other factors among children followed in primary care practices. Study Design: Secondary data analysis utilizing the Healthy Steps for Young Children Program in the Inter-University Consortium for Political and Social Research (ICPSR) database. A path analysis to assess those factors which influence the utilization of child safety interventions and the resultant impact that this may have on early childhood injury reduction was undertaken. Variables for the analysis were identified in the codebooks that accompany the data. The selected data was downloaded into the statistical software, STATA. Descriptive and multivariate regression analyses were completed. Population Studied: The data in this study pertains to children 30-33 months of age. The population studied includes only children who are followed by one of 15 pediatric primary care providers and who speak English or Spanish fluently. The majority of the respondents surveyed were mostly middle income, with some post high school education, and a mean age of 30, whose child was followed by a pediatric primary care provider. Principal Findings: Study suggests that parental characteristics are associated with the implementation of childhood safety interventions. When education, marital status and age are held constant, income is not associated with safety intervention implementation. This study did not show a correlation between safety interventions and injury rates. Conclusions: This study assessed for a small number of safety interventions, however, there are many different causes attributable to childhood injuries. The probability of a child not incurring an injury could be due to factors suggested in the literature such as parental supervision, the child’s temperament and personality, and other behavioral characteristics (Abboud Dal Santo, et al., 2004; Schwebel & Gaines, 2007). This study suggests that injury prevention involves more than just the implementation of child safety measures. Future research needs to be continued in the area of injury prevention outcomes to better ascertain the impact of these initiatives on childhood injury rates. The active involvement of parents and caregivers as well as passive environmental approaches and legislative enforcement are probably more encompassing of child safety interventions necessary to prevent childhood injuries. Implications for Policy, Delivery or Practice: Implications for practice include the provision of evidence-based anticipatory guidance and teaching for parents/caregivers about early childhood injury prevention. Poster Number: 73 Cost-Effectiveness Analysis of a Cooling Protocol to Induce Therapeutic Hypothermia in Out-of-Hospital Cardiac Arrest Presented by: Monica Rochman, B.S.N., R.N., Ph.D. Student, Nursing Business and Health Systems, Univeristy of Michigan, 400 North Ingalls Room 4170, Ann Arbor, MI 48109; Phone: (734) 846-6077; Email: mrocwal@umich.edu Co-authors: Comillia Sasson, M.D. Research Objective: Over 300,000 cases of outof-hospital cardiac arrest (OHCA) occur annually in the United States and survival estimates to hospital discharge are generally less than 10%. Anoxic neurological injury is a major cause of morbidity and mortality in patients who are resuscitated after a cardiac arrest. The 2005 American Heart Association Guidelines recommend induction of hypothermia for out-of-hospital cardiac arrest to improve neurological outcomes after reperfusion. OHCA patients have significant costs to the U.S. health system and hypothermia treatment adds to those costs. It is unclear whether the benefits of therapeutic hypothermia justify these additional costs. The aim of this study was to evaluate whether implementation of a hypothermia protocol justified the costs accrued with OHCA patients. Study Design: A decision tree was constructed to analyze the costs and outcomes of an intention-to – treat analysis comparing pre and postimplementation phases of an intravenous hypothermia protocol. A cost effective analysis was conducted with key parameters including conditional probabilities of patients in a shockable or non-shockable rhythm, health states based on cerebral performance categories (good and poor neurological outcomes) of patient data and median reimbursements obtained from actual billing data (CPT codes) collected. The main outcomes measured were quality adjusted life years, which were obtained from recent literature. Population Studied: The study sample included 245 emergency department patients at a University hospital who experienced OHCA between the years 2005-2008. Principal Findings: Preliminary analysis showed that males comprised 68% of the sample (n=166). The median age of all patients was 57 years. The median length of stay in the hospital was 8.96 days. The primary payor was Medicare 46.9% (n=115), followed by private insurance, 35.1%, (n=86). Posthypothermia protocol implementation resulted in 0.73 quality adjusted life years compared to 0.47 in the pre-hypothermia protocol phase. The incremental cost effectiveness ratio was $31,113 per quality adjusted life year. Conclusions: From a societal perspective, preliminary results demonstrate the implementation of a hypothermic protocol could justify the costs and allocation of healthcare dollars towards therapeutic hypothermia for OHCA patients. Limitations include lack of randomization, and a small sample size of patients limited to a single tertiary care facility. Results eM.P.H.asize the importance of investigating this issue with larger, more definitive studies. Implications for Policy, Delivery or Practice: Preliminary results demonstrate that the hypothermia protocol improved survival and outcomes after a cardiac arrest and costs less than $100,000/QALY gained. As a result, quality of life for survivors could be improved with less costs attributed to quality of life years gained. Poster Number: 74 Prevalence of Previously Recognized Alcohol and Other Substance Use Disorders among VA Patients Who Screen Postivie for Alcohol Misuse Presented by: Anna Rubinsky, M.S., Research Health Science Specialist, Services Research and Development, VA Puget Sound Health, 1100 Olive Way Suite 1400, Seattle, WA 98122; Phone: (206) 324-2146; Email: Anna.Rubinsky@va.gov Co-authors: Gwen Lapham, M.S., M.S.W.; Daniel Kivlahan, Ph.D.; Emily Williams, Ph.D., M.P.H.; Eric Hawkins, Ph.D.; Katharine Bradley, M.D., M.P.H. Funding Source(s): VA Poster Number: 75 Research Objective: Brief alcohol counseling interventions are effective for reducing alcohol consumption among patients who drink above recommended levels (i.e. alcohol misuse). Further, more intensive treatment is often recommended for patients with alcohol misuse who have alcohol use disorders (AUD), other substance use disorders (SUD) or history of addictions treatment. However, the prevalence of previously recognized AUD/ SUD among patients who screen positive for alcohol misuse is unknown. Among Veterans Affairs (VA) patients who screened positive for alcohol misuse, we estimated the proportion who had previously recognized AUD/ SUD, including diagnoses or treatment documented in the year prior to screening. Study Design: The AUDIT-C is a validated screen for alcohol misuse scored 0-12 points, with higher scores reflecting greater consumption. A positive screen for alcohol misuse was defined as =3 points for women and =4 points for men. AUD/SUD diagnoses and outpatient addictions treatment documented in the year prior to alcohol screening were obtained from VA administrative records. The prevalence of previously recognized AUD/ SUD was evaluated across risk groups based on AUDITC scores: 3 or 4-5, 6-7, 8-9 and 10-12 points. Population Studied: This study included VA patients who screened positive for alcohol misuse on the Alcohol Use Disorders Identification Test Consumption (AUDIT-C) questionnaire between July 2006 and March 2009 and were randomly selected for standardized medical record review for the VA’s Office of Quality and Performance. Principal Findings: Among 23,607 eligible VA patients who screened positive for alcohol misuse, 26.5% had an AUD diagnosis, 10.6% had a SUD diagnosis and 10.3% had VA outpatient addictions treatment, documented in the past year. The total prevalence of previously recognized AUD/ SUD (including treatment) was 28.7%; and increased as AUDIT-C scores increased: 15.8%, 35.7%, 49.2% and 73.5% for AUDIT-C scores 3 or 4-5, 6-7, 8-9 and 10-12, respectively. Conclusions: Many patients who screen positive for alcohol misuse on the AUDIT-C have previously recognized AUD/SUD. Patients with higher AUDITC scores are very likely to have had prior AUD/DUD diagnoses or treatment, including nearly 75% of those in the highest risk group. Implications for Policy, Delivery or Practice: Patients with higher AUDIT-C scores may benefit from more intensive interventions and/or medications for alcohol dependence, and health care systems implementing alcohol screening and brief intervention need to consider the resources necessary to address the needs of patients with AUD/SUD. Modeling Causes of Aggressive Behavior in Patients with Dementia Presented by: Kavita Sail, M.S., Graduate Research Assistant, Management Policy and Community Health, University of Texas, School of Public Health, Houston, 1200 Hermann Pressler Drive, Houston, TX 77054; Phone: (713) 500-9483; Email: Kavita.R.Sail@uth.tmc.edu Co-authors: Robert Morgan, Ph.D.; A. Lynn Snow, Ph.D.; Jessica Davila, Ph.D.; Mark Kunik, M.D. Research Objective: Aggression is among the most distressing and dangerous of symptoms experienced by individuals with dementia, yet uncertainty remains about its incidence and causes. Our prior work has demonstrated higher levels of baseline caregiver burden, pain and decline in mutuality over time to be associated with increased risk of aggression in patients with dementia. However, we believe that onset of aggression is a consequence of complex interrelations between various psychosocial factors in patients with dementia. In this longitudinal study, we used a structural equation modeling approach to test a conceptual model of associations between constructs predicting the development of aggression in non aggressive patients newly diagnosed with dementia. Study Design: Patients already aggressive, residing in a nursing home or having a caregiver less than 8 hours a week were excluded. Patients and caregivers were assessed over 24 months starting at baseline and then at months 5, 9, 17, 21 and 25. Aggression was evaluated using the Cohen-Mansfield Agitation Inventory. Independent variables were assessed using the Hamilton Rating Scale for Depression, Philadelphia Geriatric Center Pain Intensity Scale, Burden Interview, Mutuality Scale and Pleasant Events and Activities Schedule Alzheimer’s Disease. Cognitive impairment was assessed with The Dementia Rating Scale. Yearly incidence of new aggression was calculated, and a structural equation model was used to analyze associations between independent variables and onset of aggression. Population Studied: Study participants were VA patients over age 60, newly diagnosed with dementia. Principal Findings: Of the 215 enrolled patients, 89 (41%) developed aggression (unadjusted incidence of aggression of .37/year at risk). Mean dementia severity and mutuality scores at baseline were significantly lower among aggressive patients than among nonaggressive patients; mean scores for depression, hallucinations, delusions, and caregiver burden were higher. Our structural model for predicting onset of aggression showed a good fit to the data (ChiSquare = 8.12, p > 0.05; CFI = 0.954; TLI = 0.915; RMSEA = 0.046). Higher levels of baseline caregiver burden (p < 0.05) and decline in mutuality over time (p < 0.05) were our primary predictors of increased risk of aggression in our SEM model. The significance of the relation between pain and onset of aggression was dependent on whether presence of aggression or time to development of aggression is modeled, while the relation between depression and aggression appeared to be mediated jointly by pain and caregiver burden. Conclusions: We found potentially mutable factors internal and external to the patient that were associated with development of aggression. Our SEM findings clarify the relationships found in our prior work and highlight their significance in predicting the development of aggression in dementia patients. Implications for Policy, Delivery or Practice: Antipsychotics remain the predominant treatment of aggression, but have limited efficacy and can have serious side-effects. Consequently, our findings have important preventive and treatment implications for the almost 40% of dementia patients that become aggressive each year. Funding Source(s): VA Poster Number: 76 Expansion of Newborn Screening Panels: A Formal Program Evaluation of Krabbe Disease Screening in New York State stakeholder groups described in the CDC Framework: 1. those involved in program operations, 2. those served or affected by the program, and 3. those in a position to make decisions about the program. Principal Findings: Research in progress expected completion: May 2010 Conclusions: This research will provide objective, scientific information for public health decision makers in all states considering inclusion of Krabbe disease in their newborn screening panel. Implications for Policy, Delivery or Practice: Newborn screening is recognized as a successful part of the preventative health system in all states and territories of the United States. Advancement in technology has increased the number of disorders that could be included in these programs, however, it is not clear that having the ability to screen for a disorder justifies inclusion in a screening program. In 2006, New York became the only state to add Krabbe disease,a progressive fatal neurological diseasee, to the newborn screen. To date, there has been no formal evaluation of this program. Funding Source(s): Sigma Theta Tau - Alpha Zeta chapter Poster Number: 77 Impact of the Medical Home on the Safety and Quality of Health Care in Canada Presented by: Roberta (Bobbie) Salveson, Doctoral Candidate, Center for Health Policy, Columbia University School of Nursing, 617 West 168th Street GB-239, New York, NY 10032; Phone: (212) 241-7055; Email: rls2128@columbia.edu Co-authors: Paticia Stone, Ph.D. Presented by: Andrea Scobie, M.H.S.A., Ph.D. Student, College of Pharmacy, Dalhousie University, 5968 College Street, Halifax, B3H 3J5 Canada; Phone: (902) 494-6023; Email: andrea.scobie@dal.ca Co-authors: Neil MacKinnon, Ph.D.; Sean Higgins, B.Sc.; Holly Etchegary, Ph.D.; Rhonda Church, M.D. Research Objective: The purpose of this study is to conduct a formal program evaluation of newborn screening for Krabbe disease in New York State using the CDC Framework for Program Evaluation in Public Health. The aims of the study are: 1. assess if Krabbe disease screening is meeting the stated goals of the New York State newborn screening program for each of the stakeholders using this program, 2. assess the Krabbe disease test characteristics with the most recent data available, and 3. assess the cost to identify one true positive Krabbe disease screening result. Study Design: The CDC Framework for Program Evaluation in Public Health provides the guideline for collection of data. Data will be collected from a variety of sources in New York State, including published brochures, public health law, technical manuals, stakeholder interviews, annual newborn screening reports, meeting minutes,coding, and charge reports. Data will be analyzed using qualitative and quantitative methodologies. Population Studied: Using purposive sampling, participants will be recruited to represent Research Objective: To explore the relationship of a medical home to self-reported risk factors for medical error and self-reported indicators for quality of care. Study Design: The Commonwealth Fund's 2007 International Health survey in seven countries was the primary data source. We focused only on the Canadian data. Using SPSS, we explored the relationship between a medical home and a number of variables based on leading indicators for quality primary health care as developed by the Canadian Institute for Health Information, including: access, medical error, coordination, confidence, emergency department use and patient-provider relationship. Chi-square tests were used for categorical variables and Mann-Whitney U tests for ordinal variables. Population Studied: As part of a seven-country health policy survey, the Commonwealth Fund surveyed a sample of 3003 people 18 years and older in Canada’s 10 provinces and 3 territories between 6 March and 7 May 2007. Principal Findings: Of Canadians surveyed, 51% did not have a medical home. Based on the 2006 census, this extrapolates to nearly 13 million adult Canadians. Overall, the presence of a medical home was associated with self-reported improved access to health care services, coordination of the services received, confidence in the services received and provider knowledge. Self-reported medical and medication error rates were higher among those without a medical home. However, emergency department use patterns were similar among those with and without a medical home. Conclusions: The presence of a medical home is associated with perceived safer and higher-quality patient care. Ensuring that Canadians have a medical home through primary health care reform may be an effective means to mitigate medical and medication errors while increasing patient satisfaction and strengthening patient–provider relationships. Implications for Policy, Delivery or Practice: Greater eM.P.H.asis on primary health care through the promotion of medical homes may offer patients and providers a more effective means to navigate the Canadian health care system. Given Canada's history of slow change within the primary care arena it is unlikely that change will take place quickly. Nonetheless, there is mounting evidence that concept of medical homes will help to increase the quality and safety of care received by Canadians. Poster Number: 78 Pharmacy Staff Perceptions of Medication Incident Reduction and Reporting in Nova Scotia Presented by: Andrea Scobie, M.H.S.A., Ph.D. Student, College of Pharmacy, Dalhousie University, 5968 College Street, Halifax, B3H 3J5 Canada; Phone: (902) 494-6023; Email: andrea.scobie@dal.ca Co-authors: Neil MacKinnon, Ph.D.; Todd Boyle, Ph.D.; Heidi Deal, B.Sc.; Tom Mahaffey, Ph.D. Research Objective: Medication incidents (MI) can have serious consequences for the health of Canadians and the perceived safety of community pharmacy practice. The objective of this research was to assess pharmacy staff perceptions of various strategies for MI reduction and reporting in community pharmacies, and how such perceptions differ between staff and ownership type. Study Design: The Pharmacy Perceptions of Safety Survey (PPSS) contained twenty-three questions aimed at assessing the state of MI identification and disclosure in Nova Scotia pharmacies as related to the role of continuous quality improvement (CQI) and safety culture. Multivariate analysis of variance (MANOVA) was used to examine the overall difference of means for each group. Significance for all calculations was set a priori at the .05 level. All calculations were performed using SPSS (version 15.0). Population Studied: Community pharmacy staff were recruited on a volunteer basis from thirteen pharmacies in Nova Scotia representing rural and urban locations, independent and chain ownership and high and low prescription volume. Staff positions included Staff Pharmacist, Pharmacist Manager and Pharmacy Support Staff (i.e., technician, student and intern). Pharmacy ownership encompassed Independent, Corporate and Franchise pharmacies. Principal Findings: Respondents indicated that the use of pharmacists to help select drug therapies would be the most effective strategy to reduce MIs, whereas sharing learnings with colleagues and assuring anonymity when reporting would increase MI reporting. Celebrating reporting of errors and limiting the use of abbreviations were seen as the least effective strategies. MANOVA results indicated that practitioner type played an overall significant role in staff preferences to increase MI reporting (F=1.775, p=0.027), indicating significant differences between pharmacists, managers and support staff in how they view strategies for MI reporting. Ownership type did not have an overall significant impact on either MI reduction (F=1.520, p=.095) or reporting (F=1.357, p=.152). Conclusions: The results of this study indicate that some MI reduction and reporting strategies may be more successful than others within the community pharmacy context. Staff perceptions may rely heavily on the actions of their colleagues, and creating a comfortable environment to share error experiences may lessen hesitance to report. Respondents also viewed anonymity for pharmacists and pharmacy technicians as an important strategy to increase MI reporting and this finding coincides with literature that suggests that ensuring anonymity can improve error reporting by reducing staff fears of blame and punishment. Implications for Policy, Delivery or Practice: This study has shown that there is a great deal of variation among pharmacy staff with regards to their perceptions of MI reduction and reporting strategies. This presents challenges for improving MI reporting at both the community pharmacy and regulatory authority levels. Ensuring that community pharmacy staff perceptions and expectations are incorporated into MI reporting and reduction strategies will ultimately increase the likelihood of widespread adoption. Funding Source(s): Social Sciences and Humanities Research Council Poster Number: 79 Self-Reported Medical, Medication and Lab Error in Eight Countries: Risk Factors for Sicker Adults Presented by: Andrea Scobie, M.H.S.A., Ph.D. Student, College of Pharmacy, Dalhousie University, 5968 College Street, Halifax, B3H 3J5 Canada; Phone: (902) 494-6023; Email: andrea.scobie@dal.ca Co-authors: Neil MacKinnon, Ph.D. Research Objective: The objective of this study was to identify risk factors associated with selfreported medical, medication and laboratory error and explore their role in the likelihood of experiencing an error. Study Design: The Commonwealth Fund’s 2008 International Health Policy Survey of chronically ill patients in eight countries was the primary data source for this research. Bivariate analysis was used to determine significant explanatory variables (p <.01) for exclusion in the binary logistic regression model. Odds ratios were calculated to explore which risk factors most greatly explain the likelihood of experiencing an error. Population Studied: The Commonwealth Fund’s 2008 International Health Policy Survey of chronically ill patients was conducted in Australia, Canada, France, Germany, the Netherlands, New Zealand, the United Kingdom and the United States. The final sample consisted of 9,944 adults 18 years of age and older who were considered to have chronic and ongoing health needs. Eligible adults had to have self-reported at least one of the following criteria: (1) fair or poor health condition, (2) a serious or chronic illness, injury or disability that has required a lot of medical care in the past two years, (3) hospitalization (for something other than uncomplicated delivery of a baby) in the past two years or (4) major surgery in the past two years. Principal Findings: Results of the bivariate analysis resulted in eight variables being included in the logistic regression analysis: age, education level, number of chronic conditions present, number of doctors seen in past two years, presence of care coordination problem, poor communication with doctor, prescription drug in the past two years, and emergency room use within the past two years. The inclusion of all eight variables was justified by the Omnibus tests of model coefficient significance (chisquare = 933.456, p=.000) and the model was able to accurately predict 77.4% of the cases. The Hosmer and Lemeshow Test was non-significant (chi-square=12.503, p=.130), indicating that the model fit the data well. Conclusions: The final regression model indicates that there are a number of risk factors associated with the likelihood of experiencing a health care error among the eight countries studied. Although some demographic factors, including age and education level do play a role, risk factors with the greatest ability to predict experiencing an error encompassed issues with coordination and continuity of care and provider knowledge of a patient’s medical history. Implications for Policy, Delivery or Practice: Ensuring that providers have access to necessary patient information, and educating patients as to the importance of keeping their providers up-to-date, could greatly reduced the risks associated with experiencing an error. Greater development and use of electronic health records and organizational practices aimed at continuity of care can help to achieve this. Furthermore, greater understanding by patients of the risks associated with health care can help to engage patients in participating in error prevention strategies. Overall, the identification of risk factors help policymakers and organizations to proactively reduce the likelihood of patients experiencing an error through greater examination of system- and organization-level practices. Poster Number: 80 Family Health History Discussion in PatientProvider Encounters Presented by: Nina Shiang, B.S., Graduate Student Associate, Verdict, 7400 Merton Minter Boulevard, San Antonio, TX 78229; Phone: (210) 617-5238; Email: shiang@uthscsa.edu Co-authors: Joann Seo, B.A.; Eva Shipp, Ph.D.; Nedal Arar, Ph.D. Research Objective: This study will attempt to characterize discussion(s) of family health history in the clinical setting and also detail potential inadequacies when this topic is discussed. Study Design: Cross-sectional, Observational Study Population Studied: Patients served by primary physicians at the Audie L. Murphy Memorial Veterans Hospital (VHA) in San Antonio, TX from 2003 to 2005 Principal Findings: Of the 131 total encounters transcribed among the 37 patients, only 24 encounters (18.3%) included discussion of FHH. In new patients, 16 encounters (66.7%) included discussion of FHH, while in established patients only 8 encounters (33.3%) included discussion of FHH. In new patients, discussion of FHH most frequently occurred in the first encounter (62.5%). In established patients, no observed pattern could be ascertained. Providers initiated discussion on 14 of these encounters (58.3%) and patients initiated discussion on 10 of these encounters (41.7%). In provider initiated FHH discussion, satisfactory levels of discussion were most frequently achieved (>3 elements of FHH discussed) while in patient initiated FHH discussion, moderate levels of discussion were most frequently achieved. FHH discussion included topics of diabetes management, cancer, and cardiovascular disease (CVD). In provider initiated FHH discussion, exchange on cancer and CVD were most frequently observed, 58.3% and 41.7% respectively. Additionally, the relationship between FHH discussion and discussion of self-care management (SCM) topics were assessed. The average number of SCM topics discussed was 6 (std = 2.9; range: 213). Patient-provider discussion of SCM was related to discussion regarding FHH information (p< 0.05). Conclusions: In this study, providers were more likely to initiate discussion on family health history among new patients. In provider initiated FHH discussion, satisfactory levels of discussion were most frequently achieved (>3 elements of FHH discussed) while in patient initiated FHH discussion, moderate levels of discussion were most frequently achieved. Additionally, FHH discussion was highly correlated with topics of cancer and CVD. Implications for Policy, Delivery or Practice: Family health histories could be one means to this end through the implementation of personalized preventive care strategies. The publication of these results may benefit both the clinical and scientific community. Social scientists may use this data to design clinical interventions aimed to best facilitate and improve patient-provider communication on the topic of family health history. Funding Source(s): VA Poster Number: 81 Trends in Length of Stay among Patients Who Leave Against Medical Advice from U.S. General Hospitals Between 1988 and 2003 Presented by: Rima Tawk, M.S., M.P.H., Graduate assistant, Health Policy and Administration, University of Illinois at Chicago, 1603 W Taylor Street, Room 722, Chicago, IL 60612; Phone: (312) 413-1468; Email: rtawk1@uic.edu Research Objective: The aims of the study are twofold: to examine the national trend in hospital resource utilization among patients who leave against medical advice (AMA) from US general hospitals between 1988 and 2003; and to explore changes in the healthcare system and the factors that have precipitated the change. Study Design: The study is a secondary data analysis from the National Hospital Discharge Survey (NHDS) conducted by the National Center for Health Statistics. NHDS provides nationally representative estimates on the characteristics of patients, lengths of stays, diagnoses, and surgical and nonsurgical procedures in hospitals of different bed sizes, ownerships, and geographic regions of the US. Utilizing a complex multistage stratified probability sampling design, the NHDS annually collects data from a sample of approximately 300,000 inpatient medical records from a national sample of about 500 nonfederal short-stay care hospitals. Population Studied: This study is limited to AMA adults (18 yrs and over) between 1988 and 2003. We used a sample of 35,616 AMA patients representing a weighted total of 3,986,936. Years of data were collapsed into intervals to reflect the changes that have shaped the healthcare system. To date, there is a paucity of published literature on the hospital resource utilization of AMA patients and the factors that predict their length of stay (LOS). Most of the previous studies on AMA discharges have shown that mental illness was an important predictor of such discharges. Principal Findings: Males leave about a quarter a day before females (p=0.0008). Patients whose age category ranged between 18 to 44 years and 45 to 64 years leave approximately before 0.9 days (p<.0001) and 0.6 days (p=<.0001) respectively than the 65+ age category. Blacks stay more than half a day than whites (ß=0.61; p<0.0001), other race stay less than a quarter of a day than whites (p=0.0134). Singles stay more than a quarter a day than married (p=0.0317). With respect to region, patients discharged from the Northeast stay 0.4 days longer than patients discharged from the South region (p=<.0001) while patients discharged from the West stay 0.3 days longer than patients discharged from the South region (p=<.0030). Regarding insurance coverage, patients on Medicare stay approximately 0.7 days more than patients on private insurance (p<0.0001). Patients on Medicaid stay approximately more than half a day than patients on private insurance (p<0.0001). Self-pay patients leave a quarter a day earlier than patients on private insurance (p=0.0285). Patients discharged from hospital bedsize (6-99) leave about one day earlier than patients who are discharged from 500 + bedsize category (p=<.0001). Patients from hospital bedsize (100-199) leave 0.88 day earlier than patients who are discharged from 500 + bedsize category (p=<.0001). Patients from hospital bedsize (200-299) leave 0.71 day earlier than patients who are discharged from 500 + bedsize category (p=<.0001). Patients from a bedgroup (300-499) leave about half a day a day earlier than patients who are discharged from 500 + bedsize category (p=<.0001). The ownership of hospitals did not yield significant results in all categories. On average, patients with mental illness stay half a day more than patients without mental illness (p=<.0001).Gender and Marital Status did not change across intervals.The significant predictors that changed across time were African Americans, Medicaid insurance and the West region. Conclusions: LOS has significantly decreased across time intervals (p<0.0001). Hospital ownership influences LOS less over time. Data reveal substantial regional variation in particular the West had a substantial decrease in LOS. Patients covered by Medicaid had shorter LOS. Implications for Policy, Delivery or Practice: AMA patients pose problems for service delivery systems because they experience short hospitalizations but multiple readmissions and therefore increased healthcare costs. It is important to examine factors that either facilitate or impede utilization of services among patients who do not adhere to medical treatment. LOS can reveal useful information about the performance of hospitals and it has been accepted as a robust index of system performance. Its magnitude can be influenced by system as well as patient –related factors. The results may offer insights to reduce AMA discharges. Poster Number: 82 The Impact of Length-of-Stay on Hospital Acquired Adverse Drug Events: A Regression Discontinuity Approach Presented by: Mark Unruh, M.S., Ph.D. Candidate, Department of Community Health, Brown University, 121 South Main Street, Box G S121, Providence, RI 02912; Phone: (831) 4207039; Email: mark_unruh@brown.edu Co-authors: Vincent Mor, Ph.D. Research Objective: To quantify the effect of inpatient length-of-stay on hospital acquired adverse drug events. Study Design: Using the 2006 New York State Inpatient Database, we employ a regression discontinuity design to assess the influence of length-of-stay (LOS) on the likelihood of experiencing a hospital-acquired adverse drug event (ADE). Medicare’s prospective payment system creates an incentive for hospitals to discharge patients as soon as possible, which is partially offset by reduced inlier payments for short stays. Since Medicare bases LOS on the number midnights spent in the hospital, the number of hours constituting LOS will vary by time of admission. For patients to have the same LOS, those admitted near, but after, midnight will need to spend more hours in the hospital than will admissions just prior to midnight. Admission through the emergency department (ED) shortly before or after midnight should be a random process, creating a treatment group (post-midnight admissions) and the proper counterfactual (pre-midnight admissions). Our empirical strategy utilizes two-stage least squares estimation with heteroskedastic-robust standard errors adjusted for clustering within hospitals. An assignment rule, equal to one for post-midnight admissions and zero for pre-midnight admissions, is incorporated as an instrumental variable. The firststage estimates the relationship between time of admission and LOS. The reduced-form derives the relationship between LOS and hospital acquired ADEs. Population Studied: The study population includes patients 65 and older admitted through hospital EDs in the state of New York, in 2006, with Medicare listed as the primary payer. Only individuals admitted plus or minus two hours of midnight were included. Principal Findings: The observable characteristics of the two groups are well-balanced. In the firststage we find that, on average, individuals admitted in the hour following midnight have a LOS that is approximately 10 hours longer compared to admissions in the hour prior to midnight. Likewise, those admitted after midnight are 8% more likely to experience an ADE. The ratio of the reduced-form and first-stage estimates indicates that each additional hour in LOS adds 0.8% risk of experiencing an ADE, on average. After adjusting for clustering within hospitals, estimates remain significant at the 5% level. These results were robust to samples comparing admissions that took place from 10:00 to 10:59 PM to those entering the ED from 12:00 to 12:59 AM. Additionally, estimates obtained using samples composed of nondeferrable conditions had consistent results. Nondeferrable conditions were identified by diagnoses with similar admission rates for each day of the week, including weekends, consistent with recent studies. This indicates that any potential confounding due to unusual treatment patterns near midnight, such as those associated with staff shift changes, are unlikely to account for our results. Conclusions: We conclude that hospital acquired ADEs are common and that longer LOS presents additional risk for acquiring an ADE. Implications for Policy, Delivery or Practice: Our results indicate that LOS is amenable to policy, putting some patients at increased risk of experiencing an ADE. Since many hospital acquired ADEs are preventable, reducing the likelihood of a patient experiencing one provides an opportunity to simultaneously improve the quality of care and reduce costs. Funding Source(s): NIA Poster Number: 83 Understanding the Cultural Impact of Familismo on Mental Health Services Utilization among Latinos in the U.S. Presented by: Alice Villatoro, B.A., Ph.D. Student, Health Services, UCLA School of Public Health, 650 Charles E. Young Drive, 31-269 CHS, Los Angeles, CA 90095-1772; Phone: (310) 8252594; Email: avillato@ucla.edu Co-authors: Vicki Mays, Ph.D., M.S.P.H. Research Objective: There is strong empirical evidence that untreated mental disorders are associated with substantial morbidity. Hence, it is important to examine the underlying mechanisms that may deter help-seeking behaviors for mental health services within the Latino community since this population generally underutilizes mental health specialty services. The aim of this study was to examine how familismo, a prominent value on familial loyalty and solidarity in the Latino culture, may be a cultural determinant of mental health service utilization among Latino adults. Study Design: Data utilized came from the 20022003 National Latino and Asian American Study (NLAAS), a nationally representative community household survey examining the prevalence of mental health disorders and services utilization of Latinos and Asian Americans. Familismo was examined as the combined effect of family-provided emotional support and level of familial cultural conflict. Logistic regressions were performed to examine the relationship between familismo and lifetime mental health service utilization, controlling for sociodemographic, access, need, and immigrant experience characteristics. Sample design variables and sample weights developed by Heeringa et al. (2004) were utilized in the analyses to correct for clustering, unequal probabilities in selection during the sampling stage, and nonresponse patterns of underrepresented populations in the sample. Population Studied: The sample included 2554 non-institutionalized Latino adults (18 years of age or older) residing in the U.S. Principal Findings: Latinos reported high levels of family-provided emotional support and low levels of familial cultural conflict. Low rates of lifetime mental health service utilization were also observed. The results showed that higher levels of both familyprovided emotional support (OR=1.17, 95% CI: 1.03-1.35) and familial cultural conflict (OR=2.13, 95% CI: 1.41-3.22) were associated with higher likelihoods of lifetime utilization among Latino adults. However, familial cultural conflict appeared to be a more robust predictor of service use than family emotional support. A significant interaction between lifetime diagnosis status and perceived need was also observed (OR=0.16, 95% CI: 0.080.32). Though individuals with clinical need for mental health services showed high rates of utilization, Latinos with both a history of mental illness and subjective need for mental health care were significantly less likely to utilize services in comparison to Latinos with no prior diagnosed mental illness. Other significant predictors of utilization included years residing in the U.S, years of education, language, and subethnic identification. Conclusions: The results of these analyses illustrate the importance of family, most especially family conflict, on mental health services utilization among Latinos in the U.S. Though Latino families have been traditionally characterized as supportive entities, the results of this study imply that the use of mental health services for emotional or substance-related concerns becomes an important outlet for Latinos with high levels of familial conflict as these services may provide the help and support they lack in their family immediate environments. Additionally, the interaction suggests that the question of utilization appears to be most relevant to those in need for services. Implications for Policy, Delivery or Practice: The findings from this study can assist health care providers in the development of culturally competent strategies aimed to improve access to and utilization of mental health services for Latinos. Poster Number: 84 The Sensitivity of Adverse Event Cost Estimates to Diagnostic Coding Error in Administrative Data Presented by: Gavin Wardle, M.B.A., B.Sc., Ph.D. Candidate, Health Policy, Management, and Evaluation, University of Toronto, 95 Bertmount Avenue, Toronto, M4M 2X8 Canada; Phone: (416) 220-2210; Email: gavin.wardle1@gmail.com Co-authors: Walter Wodchis, Ph.D.; Geoff Anderson, Ph.D.; G. Ross Baker, Ph.D.; Audrey Laporte, Ph.D. Research Objective: Previous research has established a consensus that diagnostic data elements are recorded with error in hospital administrative data. However, as yet, there is no published study that has quantified the impact of coding error on estimates of the costs of adverse events. Given the increasing importance of these estimates for hospital payment policy and for assessments of the business case for patient safety, this is an important gap in the literature. This study aims to fill this gap by examining the impact of coding error on estimates of the excess cost of each of the eleven nursing sensitive adverse events studied by Needleman et al. (NEJM 2002). Study Design: A retrospective cohort analysis of originally reported hospital administrative data and corresponding records from a large reabstraction study. Analysis revealed that adverse event coding in the original data had low sensitivities and low positive predictive values and that the reabstraction data were biased against adverse events that had a low impact on hospital resources. A hybrid data set was constructed to redress these problems and to establish a reference standard. In each data set, propensity score matching and multivariate regression analysis were used to estimate the excess cost of each adverse event. Coding errorinduced variation was examined by comparing the cost estimates derived from the three data sets. Population Studied: All adult, non-elderly medical and surgical admissions (n=9,670) included in a reabstraction study of complex cases from 16 Ontario hospitals. Patient specific case costs were obtained from the Ontario Case Costing Initiative database. Principal Findings: Estimates of the excess costs of the adverse events derived from the reference standard data ranged from $24,286 (metabolic derangement) to $48,897 (hospital-acquired sepsis). Coding errors in the originally reported data caused the excess costs of the adverse events to be underestimated, on average, by 27 percent. In contrast, the bias against low cost adverse events in the reabstraction data caused the excess costs to be overestimated, on average, by 34 percent. At the institutional level, coding induced misestimation of the cost attributable to adverse events ranged from 48 percent underestimated to 2 percent overestimated. Conclusions: Estimates of adverse event costs are highly sensitive to coding error. Adverse event costs are likely to be significantly underestimated if the error is ignored. Implications for Policy, Delivery or Practice: The finding that coding error in administrative data can cause the costs of adverse events to be significantly underestimated, coupled with the observation that the likelihood of error is ignored in most studies, suggests that previous assessments of the business case for patient safety may have been biased against the cost effectiveness of patient safety improvements. Furthermore, the observed extent of institutional level variation in adverse event coding indicates that administrative data are inadequately reliable as a basis for adverse event payment policies or for public reporting of adverse event rates. Funding Source(s): Health System Performance Research Network Poster Number: 85 Does High Cost Sharing in Physician Care Reduce Health Care Utilization and Expenditure Differently for People with Severe Disease than Those Without? Presented by: Haichang Xin, Ph.D. student, Department of Health Services Research, University of Florida, 101 S. Newell Drive, PO Box 100195, Gainesville, FL 32610-0195; Phone: (352) 273-6627; Email: hsppyxhc@phhp.ufl.edu Research Objective: This study examines the potential differential impact of cost-sharing in physician care on health care utilization and expenditure for those with and without severe health conditions. By providing empirical evidence, this study’s findings will inform policies that help protect and prevent the severely ill from exacerbating their poor health status and financial burden, as well as save cost for the society at the aggregate level. This present study fills the following gaps in the literature by focusing costsharing on physician care, and using representative sample of the whole population. Study Design: The study adopted a crosssectional study design from the 2007 Medical Expenditure Panel Survey data. The Hausman test eliminated the concern of the potential endogenous problem between cost-sharing and health care utilization or expenditure (p=0.12). Negative binomial regressions and two-part models were employed to estimate the utilization and expenditures. Population Studied: Subjects were included with an age of 18 or older with the full year of insurance coverage in the United States. Disease severity is measured by physical component score (PCS), and a dummy severity variable was then created with two groups of individuals whose PCSs fell within the bottom tertile and the top tertile. Cost-sharing was calculated by dividing out-of-pocket expenditures by total expenditures for each person, then a dummy cost-sharing variable was created with the cut off points of 20% in Medicare and private plans and mean values in Medicaid. Principal Findings: The data was analyzed with STATA. Among the 13,020 selected subjects, although an insignificant differential impact was found in physician care utilization (p=0.34), costsharing, severity and their interaction had expected signs. Specifically, severely ill individuals reduced MD visits less than the general population in response to high cost-sharing. As a component of MD visits, primary care physician visits analysis demonstrated the significant differential impact (p=0.00). In downstream inpatient care utilization, although an insignificant differential impact was found (p=0.34), cost-sharing, severity and their interaction demonstrated expected signs. Specifically, severely ill individuals increased inpatient care more than the general population, which suggested that the suppressed MD visits due to high cost-sharing were released in the downstream inpatient services. As for expenditures, in all physician care, inpatient care and overall services the differential impact demonstrated consistent positive directions for both parts, but was significant in part one (p=0.04, 0.00 and 0.00 respectively) and insignificant in part two (p=0.36, 0.79 and 0.48 respectively). Conclusions: In conclusion, the differential impact of cost-sharing was basically confirmed. Specifically, it demonstrated that severely ill people, in response to high cost-sharing, tended to reduce less health care utilization and expenditures that were crucial to maintain their health. Implications for Policy, Delivery or Practice: Therefore, this vulnerable people should be treated differently. Specifically, a low cost-sharing policy should be designed to reflect and match their situation. This study will highlight the necessity and importance of insurance policy design in terms of differentiation and specification for its target population. Furthermore, it will inform the current debate on health care reform, especially how a universal plan, rather than specialized plans for subpopulations, would complement the existing public and private designs. Poster Number: 86 Digital Divide in a Personalized Health Record Presented by: Cyrus Yamin, B.S., Medical Student, Brigham and Women's Depatment of General Medicine, Harvard Medical School, 156 Allston Street, Cambridge, MA 02139; Phone: (617) 413-4714; Email: cyamin@gmail.com Co-authors: Srinivas Emani, Ph.D.; Jonathan Wald, M.D.; Andrew Karson, M.D., M.P.H.; Stuart Lipsitz, Deborah Williams, Sc.D., M.H.A.; David Bates, M.D., MSc. Research Objective: Electronic personal health records (PHR) offer the potential of enhancing patient-practice communication and streamlining of administrative functions-such as appointment requests, referral requests, and prescription refills. At the same time, the “digital divide,” the population-level gap in Internet access, hinders the role a PHR plays in the delivery of care. This study assesses the existence of a "digital divide" associated with a PHR. Study Design: Retrospective analysis of a PHR implemented at over 50 practices at Partners Health Care in Massachusetts. Population Studied: Rates of PHR and degree of usage of PHR among adopters based on total unique usage requests. Adopters were those defined as registering online for the PHR. Principal Findings: 37,599 patients adopted the PHR since its inception in 2002. Compared to a random sample of non-adopters, adopters were more likely to be female (OR, 1.32, 95% CI, 1.281.36) and have greater than two chronic conditions (OR=1.396, CI 1.34-1.482). Blacks and Hispanics were less likely to be adopters (OR .397, 95% CI .294-.351, OR .321 95% CI .294-.351, respectively). Adopters were stratified based on unique usage requests in 2007 and 2008: 0-1 requests comprised 61.5% of usage; 1-4 requests comprised 25.1%; 59 requests comprised 9.1%; > 10 requests comprised 4.2%. To develop an area-based socioeconomic measure for adopters, we geocoded adopter’s home address to the census block level, and linked it to the 2000 Census poverty levels. After adjusting for practice level clustering and fitting to a Poisson Model the degree of usage was best predicted by the number of patient comorbidites (with more comorbidities increasing usage), followed by patient's race (whites over blacks and hispanics), and insurance status (private insurance over Medicare). The area-based socioeconomic measure was not associated with degree of usage. Conclusions: Despite increased rates of Internet access, those population groups most likely to benefit from PHRs still are less likely to initiate use. Among those who do adopt, however, higher usage does not appear to be associated with socioeconomic status. Implications for Policy, Delivery or Practice: Perhaps once a person has joined a PHR, thereby demonstrating some level of Internet access, variations in usage might instead reflect overall heath service utilization trends, while the “digital divide” poses less of a barrier than once suggested. Funding Source(s): Other, Harvard Medical School, Brigham and Women's Hospital Poster Number: 87 Medical Savings Account in China and the Effect of Its Balances on Outpatient Utilization Presented by: Vivienne Hui Zhang, M.Sc., Ph.D. Student, Department of Management and Marketing, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong; Phone: +85261805323; Email: chefyzhang@hotmail.com Research Objective: Medical Savings Account (MSA) is established for insured individuals to pay for their own medical expenses to control costs, and save money for future medical needs. Some literature in China suggested that the presence of MSA has a negative effect on equity in health care financing, and recommended to reduce the role of personal MSA. However, these studies were only based on the estimated MSA balances, and impossible to distinguish the previous year’s balances from current year’s contributions. This study will fill this gap by using real data of MSA balances, and examines the effect of MSA balances on outpatient services utilization among different income groups. Study Design: Drawing on theoretical framework from Andersen’s behavioral model of health services use, we investigated individual enabling factors measured by MSA balances to evaluate health policy in China. The city in this study, Guangzhou is a typical large city in southern part of China, and it is representative with respects to population size, age structure and income levels. The study first divided MSA account-holders into four groups, based on the contributions reflecting income levels. Age-gender adjustment mean expenditures in 2007 were then calculated to see whether income affects the expenditure of MSA with similar medical needs. Then, within each group, two-part model was applied to study the effect of MSA balances in December 2006 on the expenditures in 2007. The first part used logit model to estimate the effect on probability of outpatient usage, and a log-linear model in the second part was employed to study the incurred level of its expenditures for users only, holding other factors fixed. This stratified analysis was used to control the income effect. Population Studied: Sample (N=93,752) is the first group of insured employees since MSA scheme was launched in the city in 2002. Six years data include each MSA account-holder previous years’ balances and current years’ contributions, expenditures between 2002 and 2007. Principal Findings: Age-gender adjustment mean expenditures in 2007 were significantly different among these groups after controlling health needs. MSA account-holders in different income groups had different health behaviors. In the lowest income group, MSA balances were positively related to probability of outpatient usage and its expenditures. However, for the highest income group, more MSA balances were significantly associated with lower usage probability and less medical spending. For the two medium income groups, the MSA balance was also significantly associated with probability of usage and its expenses when holding other factors fixed. But the relationship was non-linear. Conclusions: The impact of MSA balance on outpatient utilization is different among four income groups. Low income insured employees use health services as long as they have funds in MSA. They may not have enough balances to cover their necessary health services. But high income groups have lower utilization as MSA balances increase. More savings in MSA are available for high income people. Among two medium income groups, MSA can play its role. Implications for Policy, Delivery or Practice: Income may be a governing effect of the behaviors of the MSA usage. Polices targeted to different income groups may be needed to strengthen the role of MSA. For low income insured employees, government can give additional subsidies to their personal MSA. Regarding high income groups, we suggest to extend the application of available MSA balances. For example, enrollees can use their own MSA to pay for family members’ medical expenses, or purchase complementary private insurances. Poster Number: 88 Can Family Income Impact Children's Limitations Due to Chronic Conditions? Presented by: Lucy Bilaver, M.P.P., M.S., Ph.D. candidate, School of Social Service Administration, University of Chicago, 1313 E. 60th Street, Chicago, IL 60637; Phone: (773) 256-5158; Email: labilave@uchicago.edu Research Objective: To identify a causal effect of income on parent's perceptions of their children's limitations due to chronic conditions. Analysis of NHIS and NLSY data has revealed that parents of children in poverty report more activity limitations than their higher income counterparts, but it is unknown whether this is due to a spurious or causal relationship. Study Design: A individual fixed effects instrumental variable design will be applied to observational data. The instrumental variable for family income will exploit large expansion of the Earned Income Tax Credit during the 1990's. Population Studied: Data on the children of the NLSY 1979 female respondents will be used. Eleven waves of data have been collected on over 11,000 children. The study population will include over 9,000 children with outcome data in at least one time period between 1988-2006. Principal Findings: Twelve percent of the children in the sample had an activity limitation reported at some point during the study period. In crosssectional models controlling for child, mother, and other household characteristics, a $10,000 increase in family income was associated with a -.36% decrease in the probability of parents reporting a activity limitation. After controlling for child fixed effect, the association decreases and becomes statistically insignificant. Using expansion in the EITC to create an instrumental variable for reported income reveals a positive causal effect of income on the probability of reporting any activity limitation. Specifically, a $10,000 increase in family income implies a .8 percent increase in the likelihood of reporting a activity limitation. Conclusions: Family income is a causal determinant of the way in which parents perceive the limiting effect of their children's chronic conditions. Implications for Policy, Delivery or Practice: There may be a disparity in the availability and affordability of services to support children with chronic health conditions in families with high income versus low income. There needs to be further description of this causal relationship to understand the source of this disparity. Funding Source(s): AHRQ Poster Number: 95 The Transportation Disadvantage Index: Progress Towards Developing a New Community Measure of Child Health Access Barriers Presented by: Stephen Borders, Ph.D., M.S.H.P., Associate Professor, School of Public, Nonprofit and Health Administration, Grand Valley State University, 401 West Fulton Street, Grand Rapids, MI 49504; Phone: (616) 331-6569; Email: borderss@gvsu.edu Co-authors: Roy Grant, M.A.; Dennis Johnson, M.A. Research Objective: Transportation is a frequently cited barrier to healthcare access, but researchers have rarely evaluated the problem in depth. It is generally recognized that having health insurance alone does not assure access to the healthcare system. Particularly in health professional shortage areas, geographic problems (distance and availability of transportation) may complicate healthcare access. We sought to identify areas where transportation barriers are particularly acute for children by developing a Transportation Disadvantaged Index. Study Design: Using 2004-2006 hospital discharge data from the Texas Department of State Health Services (TDSHS), a multiple regression design was used with ambulatory care sensitive conditions (ACSC) admissions as a proxy for children’s access to healthcare services. We used ordinary least squares regression to identify predictors of nonemergent ACSCs by zip code in Travis County, Texas and seven contiguous counties. Using Geographical Information System (GIS), we mapped the level and intensity of ACSCs by zip code. Covariates included the ratio of automobiles to population 16 and older, distance to the nearest federally qualified health center (FQHC), percent of working population 16 and older that takes public transportation to work, urban or rural Census Bureau designation of zip code and a rich array of personal socioeconomic characteristics. We used factor analysis to group socioeconomic factors into meaningful categories, revealing three underlying dimensions: 1) zip codes dominated by high levels of minorities receiving public benefits in the form of welfare and Medicaid (“TANF Families”), 2) zip codes dominated by high poverty areas that were most likely eligible but not enrolled for public benefits and spend a high proportion of income on housing (“Working Poor”) and 3) zip codes dominated by single-female headed households with high numbers of women in the workforce, less likely to be minority (“Working Mothers”). Population Studied: Using hospital discharge data from TDSHS, we identified 15,862 emergency department (ED) visits in the eight county area attributable to children 17 years or younger. Principal Findings: Of the 15,862 ED visits during the study period by children ages birth-17, 2,883 (18.1%) were classified as non-emergent ACSCs. Among children utilizing ED services for ACSCs, there were strong inverse relationships by zip code between ratio of automobiles (p<.013) and percentage of Working Mothers (p<.05). ED use for ACSCs was also associated with percentage of working population taking public transportation to work (p<.004) and percentage of population living in a rural zip code (p<.028). Travel distances to FQHCs were greatest in rural areas. Conclusions: The results suggest that distance to health care services (rural zip code) and availability of personal transportation are associated with greater utilization of ED services for ACSCs. This suggests that transportation is a strong barrier to timely access of child healthcare services. Implications for Policy, Delivery or Practice: Factors associated with transportation barriers to child healthcare access can be identified and mapped using hospital discharge data. Policy makers can target these areas for interventions to enhance the availability of non-emergency medical transportation, deployment of mobile clinics and additional primary care services (e.g., new FQHCs) to improve child access to appropriate preventive and primary healthcare services, potentially improving outcomes and lowering the cost of care. Funding Source(s): WKK, The Children's Health Fund Poster Number: 96 Clinical Characteristics Influence Parent-Reported Quality of Life among Children with Attention Deficit Hyperactivity Disorder Presented by: Eugenia Chan, M.D., M.P.H., Assistant in Medicine, Division of Developmental Medicine, Children's Hospital Boston, 300 Longwood Avenue, Boston, MA 02115; Phone: (617) 355-3070; Email: eugenia.chan@childrens.harvard.edu Co-authors: Chao-Yu Guo, Ph.D.; Sara Toomey, M.D., M.P.H.; Janine Molino, M.S.; Stephen Porter, M.D., M.P.H. Research Objective: Children with ADHD experience poorer health-related quality of life (HRQL) relative to typical peers, but the extent to which HRQL is associated with key clinical characteristics is unknown. We investigated the relationship between parent-reported HRQL and disease control, ADHD medication side effects, comorbid psychiatric conditions, and complexity of ADHD care environment. Study Design: We analyzed data collected during a clinical trial on how parents shared information about their child’s ADHD with medical providers. Parents reported on ADHD symptoms, current prescribed ADHD medications and side effects, and HRQL. The normalized Psychosocial Summary Score (range 0-100) from the 50-item Child Health Questionnaire-Parent Form was the primary outcome. Predictors included disease control status based on NICHQ Vanderbilt symptom counts; severity of ADHD medication side effects; results of Vanderbilt screen for anxiety/depression, oppositional defiant disorder, and conduct disorder; and whether the primary manager of the child's ADHD also prescribed the ADHD medications. Multivariate linear regression analyses adjusted for child age, gender, and parent race/ethnicity, and adjusted beta estimates were re-transformed into scaled HRQL scores. We considered a 5-point difference in scaled HRQL score to be clinically meaningful. Population Studied: Parents of children age 5-12 with ADHD treated with prescription medication, recruited from diverse communities in greater Boston. Of 271 parents screened, 194/271 were eligible and 182/194 were enrolled. We analyzed 177 parents with complete data. Principal Findings: Overall, mean±SD Psychosocial Summary Score was 37.5±12. Parents reported their children to have poor disease control (63%), more than minimal side effects (71%), and positive co-morbidity screen (50%). In both crude and adjusted analyses, higher HRQL was significantly associated with good disease control (adjusted beta 0.7, p<0.001), minimal medication side effects (adjusted beta 0.36, p<0.006), negative co-morbidity screen (adjusted beta 0.67, p<0.001), and the same clinician managing care and prescribing medications (adjusted beta 0.33, p<0.03). Expected improvement in scaled HRQL scores were +9.2 for good (vs. poor) disease control, +8.8 for a negative (vs. positive) comorbidity screen, +4.7 for minimal (vs. more than minimal) side effects, and +4.3 for the same (vs. different) manager as prescriber. Conclusions: In this community sample, parents reported significantly higher HRQL for their children with ADHD when there was better symptom control, fewer medication side effects, no symptoms of psychiatric co-morbidities, and a less complex care team structure to support disease management. Implications for Policy, Delivery or Practice: Optimizing care for children with ADHD may substantially improve their HRQL. Strategies for optimizing HRQL may include both improvements in disease-specific management as well as a more streamlined care team. Funding Source(s): NLM Poster Number: 97 Do Provider-focused Interventions Improve the Prescribing of Daily Asthma Controller Medications to Children? Presented by: Janet Coffman, Ph.D., M.A., M.P.P., Assistant Professor, Philip R. Lee Institute for Health Policy Studies, University of California, San Francisco, 3333 California Street, Suite 265, San Francisco, CA 94118; Phone: (415) 476-2435; Email: Janet.Coffman@ucsf.edu Co-authors: Michael D. Cabana, M.D., M.P.H.; Arpi Bekmezian, M.D.; Christine Cho, M.D., M.P.H.; Adam Hersh, M.D., Ph.D.; Megumi Okumura, M.D. Research Objective: Since 1997 the National Heart Lung and Blood Institute has recommended that physicians prescribe daily controller medication to all persons with persistent asthma to reduce the frequency and severity of asthma exacerbations. Previous studies suggest that physicians do not consistently follow this guideline. Our objective was to conduct a systematic review of studies of interventions to increase the prescribing of daily controller medication regimens to children with persistent asthma. Study Design: We conducted a systematic review randomized controlled trials (RCTs) and cluster RCTs that assessed the effect of interventions aimed at improving the prescribing of asthma controller medications. The primary outcome assessed was the likelihood of prescribing an asthma controller medication (e.g., an inhaled corticosteroid). The secondary outcomes were utilization of acute care services (e.g., emergency department visits for asthma), and health outcomes (e.g., days with asthma symptoms). We searched MEDLINE, EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials. Two teams of three reviewers independently reviewed abstracts. Differences among team members and between the two teams were resolved by consensus. Population Studied: Selection criteria included publication in English and analysis of effects on the prescribing of asthma controller medications to children aged 0-17 years. We included interventions delivered to individual clinicians with prescribing authority, groups of clinicians, or health care organizations. Because we were interested in interventions that sought to directly influence clinicians’ prescribing behavior, interventions delivered only to patients or caregivers were excluded. Principal Findings: We screened 699 abstracts, selected 98 articles for further review, and identified nine articles that met the inclusion criteria. All interventions had two or more components, which included educational materials (n=8 studies), conferences (n=6), educational outreach visits (n=5), individualized treatment recommendations for clinicians' patients (n=5), audit and feedback (n=1), and local opinion leaders (n=1). Five of the nine studies reported that the interventions were associated with statistically significant increases in the prescribing of daily controller medications. Interventions that provided clinicians with treatment recommendations tailored to the needs of individual patients were more likely to improve prescribing practices than interventions that provided general information about recommended prescribing practices. Of the six studies that examined the effects of the intervention on use of acute care services for asthma, only two reported a statistically significant reduction in emergency department visits and none reported a reduction in hospitalizations. The two studies that evaluated the impact of the intervention on health outcomes found few statistically significant differences between the intervention and control groups. Conclusions: RCTs of interventions to increase prescribing of asthma controller medications to children with persistent asthma have reported inconsistent effects on prescribing, acute care use, and health outcomes. Interventions that provide specific treatment recommendations for individual patients are more likely to increase prescribing than interventions that only provide general information. Implications for Policy, Delivery or Practice: Provider-focused interventions alone appear to be insufficient to improve prescribing and health outcomes for children with asthma. Multi-faceted interventions which eM.P.H.asize individualized treatment recommendations and which target patients and caregivers as well as providers may be necessary. Funding Source(s): World Health Organization Poster Number: 98 Resource Use for Children Undergoing Congenital Heart Surgery in Pediatric Hospitals Presented by: Jean Connor, D.N.Sc., R.N., Director of Nursing Research Cardiovascular Program, Cardiovascular, Childrens Hospital Boston, 300 Longwood Avenue, Boston, MA 02115; Phone: (617) 355-8890; Email: jean.connor@cardio.chboston.org Co-authors: Kimberlee Gauvreau, Sc.D. Research Objective: To describe overall resource use and breakdown of charges by type of service for patients undergoing congenital heart surgery in free-standing pediatric hospitals. Study Design: ICD-9-CM codes were used to identify patient admissions undergoing congenital heart surgery using the Pediatric Health Information System (PHIS) database years 2007-2008. Adjusted billed charges (charges billed in the medical record adjusted by the wage/price index) were abstracted for patients using PHIS CTC codes. Aggregate charges overall and by type of service were identified. Charges were further stratified by Risk Adjustment for Congenital Heart Surgery (RACHS-1) risk categories. Items within each charge category were abstracted for further description. Population Studied: <18 years of age undergoing congenital heart surgery in a pediatric institution with an annual volume of 25 cases or more over 2 years. Patient admissions coded as heart transplants and premature infants/neonates with PDA closure as the only cardiac procedure were excluded. Principal Findings: The total aggregate billed charges for the 19,565 admissions from 34 hospitals were $3,894,072,623. The median adjusted billed charges per admission were $114,721. Of the six sub-charge categories, “Other” accounted for 45.4% of the aggregated charges ($1,766,633,414, median $52, 545 per admission, with a maximum of $2,719,266). After “Other”, Lab 14.5%, Clinical 13.0%, Pharmacy 11.5%, Supply 9.8%, and Imaging 5.5% accounted for decreasing percentages of the total aggregate charges. These sub-charge proportions were similar within each of the six RACHS-1 risk categories, with “Other” accounting for 42.8%-47.2% of the adjusted billed charges. Items with the highest aggregate charges identified as “Other” included, “operating room service”, “pediatric cardiac intensive care unit”, “pediatric intensive care unit”, “neonatal intensive care unit”, and “pediatric coronary care unit”. Conclusions: Hospital care for children undergoing congenital heart surgery generated significant billed charges with a wide variation in range. Of note, “Other” services including operating room and intensive care unit services contributed to over 40% of the billed hospital charges. The proportion of “Other” billed charges remained relatively unchanged regardless of RACHS-1 risk category. Implications for Policy, Delivery or Practice: Currently between 75% and 85% of health care resources and costs are consumed by 10% of the population. Children born with congenital heart disease are included in this complex population of patients. Care for these children in this study generated significant billed charges with wide variation. The magnitude of clinical complexity and its impact on billed charges remains unclear. Further examinations require focus on institutional variation of overall charges and sub-charge categories as well as examinations of institutional variation in charge structures for specific area/ unit services. Poster Number: 99 A Comparison of Head Circumference Growth Curves for Children from Birth to 3 Years Presented by: Carrie Daymont, M.D., Fellow in General Academic Pediatrics, Department of Pediatrics, University of Pennsylvania/Children's Hospital of Philadelphia, 3535 Market Street Suite 1550, Philadelphia, PA 19104; Phone: (267) 4260684; Email: daymont@email.chop.edu Co-authors: Wei-Ting Hwang, Ph.D.; Chris Feudtner, M.D., M.P.H., Ph.D.; David Rubin, M.D. M.S.C.E. Research Objective: To determine the validity of the head circumference growth curves produced by the U.S. Centers for Disease Control and the World Health Organization in a large U.S. primary care population. Study Design: Retrospective cohort study. We created smoothed head circumference curves from our population and compared them to published curves, specifically addressing the proportion of observations above the 95th and below the 5th percentile for each set of curves. Population Studied: We analyzed 415,458 head circumference observations from the electronic medical records of 75,412 patients in a primary care network that covers three mid-Atlantic states. Principal Findings: Large differences exist between the primary care network curves and the CDC and WHO curves, especially at the 95th percentile. Conclusions: The overall proportion of subjects above the 95th/below the 5th percentile was 5.0%/4.5% for primary care network, 6.1%/4.6% for NCHS, 8.0%/3.1% for CDC, and 13.3%/3.1% for WHO. The proportions varied by age. Using the CDC curves, the proportion above the 95th percentile increased from 0.23% for children under two weeks of age to 12.0% for children 12 months old. Using the WHO curves, the proportion above the 95th percentile was over 5% at all ages with a maximum of 18.0% for children above 24 months. Implications for Policy, Delivery or Practice: Use of the CDC and WHO head circumference curves could result in clinically significant misclassifications of children with larger heads. The direction of bias has the potential to delay diagnosis of intracranial pathology in children under two months of age using the CDC curves and to cause excessive evaluation of healthy children beyond six months of age using either the CDC or WHO curves. Funding Source(s): NIH-NRSA Poster Number: 100 Understanding Fast Food Choices and the Influence of Calorie Labeling on Children and Adolescents Presented by: Brian Elbel, Ph.D., M.P.H., Assistant Professor of Medicine and Health Policy, Division of General Internal Medicine, New York University, 423 East 23rd Street, 15-120N, New York, NY 10010; Phone: (212) 263-4283; Email: Brian.Elbel@nyumc.org Co-authors: Joyce O. Gyamfi, M.S. Research Objective: Obesity is an enormous public health problem, and children have been particularly highlighted for intervention. Particularly of concern is children’s fast food consumption. However, we know very little about how children or their parents make fast food choices, including how they react to calorie labeling. The goal of this study was to determine the influence of mandatory, citywide calorie labeling on food choices of children and adolescents in New York City and to better understand their fast food choices. Study Design: Natural Experiment. Survey and receipt data were collected from New York City, and Newark, NJ (as a comparison city). Study restaurants included four of the largest chains located in NYC and Newark: McDonald’s, Burger King, Wendy’s, and Kentucky Fried Chicken (KFC). Population Studied: Sample included 349 children and adolescents aged 0-17 years who visited the restaurants with their parents or alone before or after labeling was introduced. Children and adolescents who came to the restaurant with a parent comprise of 69% of the study sample, with 31% visiting the restaurant alone. By design, 76% of our sample was surveyed in NYC. Approximately 47% of the participants were males, with 54% in the 13-17 age groups. 65.9% of the participants identified themselves as Black, 23.5% were Latino, and the remaining 10.6% were of mixed race or White. Principal Findings: Among adolescents, 57% of the sample in NYC and 18% in Newark saw calorie labels post-labeling; although only 9% indicated that the labels influenced their meal choice. The mean calories purchased by children (via their parents) and adolescents in the pre-labeling period were 684 for males and 612 for females; this did not significantly differ in the post-labeling period for NYC or Newark. Approximately 35% of adolescents ate fast food six or more time per week. Additionally, 72% of adolescents reported that taste was the most important factor in their meal selection. The majority of adolescents in NYC underestimated or did not know the amount of calories in their meals (70.1%); this was marginally improved after the introduction of labeling (61.0%). Almost all adolescents indicated they made their fast food choices without the involvement or input of the parent. However, about half indicated that at home, their parents decide (24%) or they decide jointly (16.8%). Conclusions: In our relatively small study, while most adolescent in low-income, urban areas saw calorie labels, few indicated utilizing the information in their food choice. Calories purchased were unchanged for children and adolescents during our study period. Adolescents tended to underestimate the calories they purchased. Most adolescents value taste most of all in their food choice. Finally, parental involvement tends to play a larger role in food choice at home than at fast food restaurants. Implications for Policy, Delivery or Practice: In our study, food choice of adolescents and parents’ choices for their children did not change as a result of calorie labeling. This work highlights the need for greater attention to food and obesity policies that pay particular attention to children, adolescents, and families, including how fast food choices are made and can be influenced. Funding Source(s): RWJF Poster Number: 101 2009 NHPS Delaware Child Care Provider Survey: Exploring the Relationship Between Awareness, Policies, and Practices and Behaviors Presented by: Tiho Enev, Ph.D., Senior Scientist, Policy, Evaluation and Research, Nemours Health and Prevention Services, 252 Chapamn Road, Newark, DE 19711; Phone: (302) 444-9246; Email: tenev@nemours.org Co-authors: Alex Camacho, Ph.D. Research Objective: The 2009 Delaware Child Care Provider Survey is a critical component of a systems-level evaluation model that studies the relationship between a) the center director awareness of nutrition and physical activity guidelines, b) center policies, and c) staff practices and behaviors in childcare settings. It provides data to empirically test and validate the systematic relationships between these three components. Study Design: The 2009 Delaware Child Care Provider Survey has a version for center directors and for teachers. The Director’s Version consists of four sections: 1) Center Demographics 2) Nutrition: a)Awareness of Nutrition Standards b)Center Policies Regarding: i. Nutrition Standards, ii. Nutrition Education, Training, and Monitoring, iii. Staff Behaviors, 3) Physical Activity (PA) and Screen Time (ST): a) Awareness of PA and ST Standards, b) Center Policies Regarding: i. PA and ST Standards, ii. PA Education, Training, and Monitoring, iii. Staff Behaviors, and 4) Directors’ perceptions on: a) Support from Administration, Staff, and Parents, b) Available Resources, and c) Monitoring of Childcare Quality. The Teacher’s Version is based on a 1-to-1 mapping framework – whereas questions addressing center policies in the Director’s Version have corresponding practice or behavior questions in the Teacher’s version. This two-level survey design allows comprehensive analysis of 1) the congruency between directors’ and teachers’ self-reports, 2) Relationships between a) directors’ awareness, b) center policies, and c) staff practices and behaviors, and 3) effect of center and staff demographics, center resources, training and monitoring on the above domains and their dynamics. An innovative approach was used to administer the survey to achieve better results. Previous experience with data collection in child care settings has shown that: a) it is difficult to reach the teachers without going through the center director, which might contaminate the information, b) surveying only the center’s director about staff practices and behaviors might lead to aggregation and distortion of information, and c) traditional approaches (mailing surveys) are not rewarding and have to be combined with multiple telephone follow-ups in order to achieve the desired response rate. To overcome these limitations, the surveys were administered to the center director and two randomly selected teachers during a scheduled visit at the center by a survey administrator. Population Studied: A stratified random sample of 160 licensed childcare centers, representative of Delaware’s population of 450 childcare centers spread in all three counties. Principal Findings: The preliminary findings from the pilot study suggest a positive relationship between the level of a) awareness, b) policy implementation and c) staff practices and behaviors. Comprehensive analyses will be performed once the final data is available (February, 2010). Conclusions: Targeted multi-level surveys can be used to study complex environments and provide insights to inform the programmatic work of public health organizations. Implications for Policy, Delivery or Practice: The results of the analysis provide critical insight into the mechanisms behind NHPS’ programmatic work within the child care sector. Specifically, results assist the organization in understanding where to concentrate programmatic work in the future by determining the extent that awareness, policies, and practices are interrelated. Funding Source(s): RWJF Poster Number: 102 Factors Associated with Myopia Treatment Adherence for School Children in Taiwan Presented by: Yi-Ting Fang, Student, Institute of Health & Welfare Policy, School of Medicine, National Yang-Ming University, 155 Sec. 2 Li-Nong Street Peitou, Taipei. Taiwan ROC, Taipei, Taiwan 11221; Phone: +886228267017; Email: yt620601@yahoo.com.tw Co-authors: Pu Christy, Ph.D.; Huang Nicole, Ph.D.; Ginger Liu, M.S.; Chou Yiing-Jenq, Ph.D.; Chou Pesus, Dr.PH. Research Objective: To determine the factors associated with myopia treatment adherence by using a national representative longitudinal database. To measure the impact of Atropine concentration on myopia treatment adherence Study Design: The National Health Insurance (NHI) claim data (1999-2005) was used to conduct a historical cohort study for the population in Taiwan. We choose the newly Atropine users in 2001 for treating their myopia, and followed for 4 years. Treatment effect model was used to correct the endogeneity between dependent and independent variables in this analysis. The dependent variable was Atropine adherence, which was defined by Medication Possession Ratio (MPR). Good adherence was defined as MPR >=80%, bad adherence as MPR<20%. The independent variables including age, gender, school grade, residential area, urbanicity, mydriatic drug and Atropine concentration (1%, 0.5%, 0.3%, 0.1%). Population Studied: National health insurance claim data is a representative sample (1/20) of all medical claims in Taiwan. We choose those between 4~15 years of age in 2001, which included 14,475 school children. Principal Findings: Mean MPR of all mydriatic eyedrop decreased substantially over time, with the trend being 115.6%, 74.0%, 42.1%, 29.7%, & 22.5% in 0.5 yr, 1yr, 2yr, 3yr & 4yr follow up. Proportion of good atropine adherence (MPR>=80%) was 54.3%, 34.8%, 12.0%, 3.6% & 1.1% in 0.5 yr, 1yr, 2yr, 3yr & 4yr. Factors associated with lower MPR including school grade (grade 6-9, p<0.05 respectively), residential area (northern area, p=0.019), urbanicity (combination area, p<0.0001), most common used mydriatic as tropicamide (p<0.0001) and higher Atropine concentration, but not gender (p=0.942). Results from the treatment effect model revealed that lower concentration atropine eyedrop such as 0.5% atropine (p<0.0001)or tropicamide(p<0.0001) as the most common mydriatics eyedrop predicted better treatment adherence compared with using 1% atropine. Conclusions: The myopia treatment adherence of school children was dropping rapidly from 115.6% in 0.5 year to 22.5% in 4 year post first prescription. The adherence to Atropine was even worse (54.3% in 0.5 year and 1.1% in 4 years). School grade, residential area, urbanicity and different mydriatic drug are key factors associated with MPR. Lower concentration and short acting mydriatic eyedrop showed a better treatment adherence, while less photophobia and near work difficulty was associated. Implications for Policy, Delivery or Practice: The prevalence of myopia was rising rapidly in Taiwan, Hong Kong and Singapore, its 60-80% in young adults. The prevalence of high myopia was rising as well (0.2% in 1983 and 3.4% in 2000). High myopia was associated with increasing risk of cataract, glaucoma and retinal diseases. There are evidence that regular Atropine eyedrop application (usually use every night before sleep) can halve myopia progression. Good control of myopia progression depends heavily on mydriatic eyedrop adherence. Ophthalmologists may consider changing the prescription of mydriatic eyedrop to enhance myopia treatment effect. Poster Number: 103 Bed Usage in the Pediatric Intensive Care Unit Presented by: Evan Fieldston, M.D., M.B.A., M.S.H.P., Robert Wood Johnson Clinical Scholar, RWJ Clinical Scholars Program and Pediatrics, University of Pennsylvania School of Medicine, 423 Guardian Drive, 1303A Blockley Hall, Philadelphia, PA 19104; Phone: (215) 573-2585; Email: fieldsto@upenn.edu Co-authors: Christian Terwiesch, Ph.D.; Joshua Metlay, M.D., Ph.D.; PICU Research Group Research Objective: Use real-time observation to describe utilization, flow through, and bottlenecks of pediatric intensive care unit (PICU) beds at a large, urban, academic children's hospital. Study Design: A recording tool was developed through clinical and operational expert input and through iterative pilot use. It was then used to collect >20,000 bed-hours of real-time observation of patient flow in the pediatric intensive care unit (PICU) over 5 non-consecutive weeks. Population Studied: Twenty-four beds in a PICU at a children's hospital. Principal Findings: 82% of bed-hours were used for critical-care value-added services, 8% on logistics, 9% on non-value-added uses, and 1% unclear. 95% of all bed-hours were consumed on 14 activities. There were wide variations in timing on certain logistical and non-value-added services, suggesting that bottlenecks can be identified and improved to maximize functional capacity. Conclusions: Much time in the PICU was spent caring for patients at high levels of intensity. Identifiable periods of logistical and non-valueadded occupancy were identifiable, as well as bottlenecks. Process improvement work can be directed at areas of delay uncovered by this systematic frontline analysis, to maximize functional capacity, which may improve quality (safety, efficiency, effectiveness, timeliness, patientcenteredness, equity), access, staff satisfaction, education, and value. Implications for Policy, Delivery or Practice: Pediatric Intensive Care Units (PICU), with limited number of beds and resource-intensive services, are a key component of flow and an important place for optimization. PICUs are crossroads for many patients and delays in moving them in or out can negatively impact clinical status and may decrease overall efficiency. Delays in moving patients out of the PICU, when no longer in need of critical care services, may mean that value-added services are being denied to other patients -- a form of waste. This study demonstrates a methodology to evaluate micro-system efficiency, determine utilization of resources, and identify bottlenecks for improvement. Funding Source(s): Leonard Davis Institute of Health Economics Working Group Grant Poster Number: 104 Addressing Children's Hospital Crowding by Smoothing Occupancy Presented by: Evan Fieldston, M.D., M.B.A., M.S.H.P., Robert Wood Johnson Clinical Scholar, RWJ Clinical Scholars Program and Pediatrics, University of Pennsylvania School of Medicine, 423 Guardian Drive, 1303A Blockley Hall, Philadelphia, PA 19104; Phone: (215) 573-2585; Email: fieldsto@upenn.edu Co-authors: Matthew Hall, Ph.D.; Samir Shah, M.D., M.S.C.E.; Marion Sills, M.D., M.P.H.; Anthony Slonim, M.D., Dr.PH.; Angela Myers, M.D., M.P.H.; Courtney Cannon; Susmita Pati, M.D., M.P.H. Research Objective: To quantify the effect of smoothing on crowding at children's hospitals. Study Design: Daily inpatient census & standardized length-of-stay ratios (SLOSR) were calculated for 39 free-standing, tertiary-care children's hospitals in the Pediatric Health Information System (PHIS) for 2007. Midnight census was used to calculate daily occupancy. A retrospective smoothing algorithm set each hospital-day's occupancy to the hospital's mean occupancy for each week. Post-smoothing reductions in weekly maximum occupancy were averaged for the entire year for each hospital. We determined the number of patients beyond 85%, 90%, 95%, and 100% occupancy levels pre- and post-smoothing, and the change in the number of hospitals, patient days, and patients exposed to these levels of occupancy. Population Studied: 39 free-standing children's hospitals. Principal Findings: Hospitals' mean occupancy was 70.9%-108.1% on weekdays and 65.7%-94.9% on weekends . Weekday occupancy exceeded weekend occupancy (median difference 8.2%points (IQR: 7.2-9.5)). Mean post-smoothing reduction in weekly maximum occupancy across all hospitals was 6.6%-points (IQR: 6.2-7.4). By smoothing, 39,607 patients from the 39 hospitals were removed from exposure to occupancy levels >95%. Conclusions: Smoothing occupancy over a week can provide hospitals with a useful strategy to reduce crowding. Implications for Policy, Delivery or Practice: High levels of hospital occupancy are associated with poorer patient outcomes, decreased access, and increased provider stress. Hospitals respond to crowding in a number of ways, but often focus on reducing length of stay (LOS). For hospitals already functioning at reasonable levels of efficiency, additional efforts to reduce LOS may not sufficiently increase functional capacity. In children's hospitals, median LOS is 2-3 days, so throughput improvement may be limited in reducing crowding. Managing scheduled admissions through smoothing has been proposed as an alternative strategy to reduce variability in daily occupancy and thereby reduce weekday crowding. Our study confirms that smoothing occupancy would reduce the risk of crowding and the number of patients exposed to high-occupancy conditions. Funding Source(s): RWJF Poster Number: 105 Patterns of Patient Flow at Children's Hospital Presented by: Evan Fieldston, M.D., M.B.A., M.S.H.P., Robert Wood Johnson Clinical Scholar, RWJ Clinical Scholars Program and Pediatrics, University of Pennsylvania School of Medicine, 423 Guardian Drive, 1303A Blockley Hall, Philadelphia, PA 19104; Phone: (215) 573-2585; Email: fieldsto@upenn.edu Lead Author: Meera Ragavan Co-authors: Bhuvaneswari Jayaraman, M.P.H.; Evan Fieldston, M.D., M.B.A., M.S.H.P. Research Objective: Determine how admission/discharge and occupancy patterns vary over time at a large children's hospital. Study Design: Census data for a fiscal year were abstracted: date/time of admission/discharge, emergent/scheduled, length of stay (LOS). Hourly census was calculated with a SAS macro; peak daily census were extracted. For pts with LOS 7 days, pt-hours-generated by admit day = avg LOS (hrs) for each day x number of admissions. Coefficient of variation (CV; std dev/mean) assessed variability. Population Studied: All pediatric patients hospitalized in one fiscal year at a large, urban, academic children's hospital. Principal Findings: Among 22,310 admits (mean 1859/month, SD 150, CV 8.1%), 22% were scheduled. CVs on emergent & scheduled admits per month were equal (9.8% vs. 9.7%). May, July, August had >1 SD fewer emergent admits than mean, while June had >1 SD more scheduled admits. By day of week, emergent admits had CV 12.0%, while scheduled admits had CV 65.3%, driven by lack of weekend admits (and fewer on Thurs-Fri). For LOS 7 days (84% pts), each day generated mean 154,248 pt-hours of business (SD 33,816; CV 21.9%). Emergent pt-hours generated by admit day CV 9.6%, while scheduled CV 15.7%. Mondays generated 25.2% of all scheduled pthours; Tues, Wed 20% each. Median LOS for scheduled patients admitted on Mon was 2.1 days, while 1.2-1.3 on other weekdays. Wed and Thurs had highest peak census (1 SD above mean census). Conclusions: Scheduled admissions are a major contributor to variability in occupancy and risk of mid-week crowding. Predictable patterns lead to high occupancy on some days and unused capacity on others. Hospitals interested in optimization, value, and avoiding crowding should assess their patterns. Further studies should link variability to outcomes (quality, access, finance, education, and staff satisfaction). Implications for Policy, Delivery or Practice: Optimization of patient flow is crucial to improving quality and value in healthcare, but variability comes from many sources, including artificial variability on scheduling patients to enter hospitals. This study confirms that artificial variability can be a significant challenge (and opportunity) for hospitals that face days of high occupancy. Funding Source(s): RWJF Poster Number: 106 Delayed and Forgone Care Due to Cost for Families with Chronic Conditions in High-Deductible Health Plans Presented by: Alison Galbraith, M.D., M.P.H., Assistant Professor, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215; Phone: (617) 509-9893; Email: alison_galbraith@hms.harvard.edu Co-authors: Dennis Ross-Degnan, Sc.D.; Stephen B. Soumerai, Sc.D.; Meredith B. Rosenthal, Ph.D.; Charlene Gay, B.A.; Tracy A. Lieu, M.D., M.P.H. Research Objective: Cost sharing is known to reduce health care use, leading to concerns about high-deductible health plans (HDHPs). Few studies of HDHPs have evaluated families. Our objectives were to (1) evaluate the probability of delayed or forgone care due to cost in families with chronic conditions in HDHPs compared with traditional health plans, and (2) compare the effects of HDHPs on health care use by adults and children within families. Study Design: We conducted a cross-sectional phone and mail survey between April and December 2008. The primary outcome was report of any delayed or forgone care (including acute care, emergency department visits, chronic disease care, check-ups, or tests) due to cost in the prior 12 months. We collected data for adults and children separately, conducted family-level analyses using multivariate logistic regression, and calculated predicted probabilities of delayed or forgone care due to cost using the mean or modal values for covariates in the model. Population Studied: We surveyed families with a child <18 years old insured by a large Massachusetts health plan. We identified families enrolled for the prior 12 months with at least one member with an ICD-9 code for a chronic condition. Of these, we selected all families in HDHPs (with annual family deductibles >$1000) and twice as many families in traditional plans without deductibles. Principal Findings: We surveyed 297 families in HDHPs (median family deductible = $2000) and 523 families in traditional plans (response rate 46%). In adjusted analyses, families in HDHPs were significantly more likely than those in traditional plans to report delayed/forgone care due to cost overall for any family member (24.2% vs. 9.3%, respectively; p< 0.001) and for any adult in the family (17.5% vs. 7.8%, p< 0.001), but not for children (2.1% vs. 1.1%; p=0.23). Conclusions: Delayed or forgone care due to cost is significantly more likely for families with chronic conditions in HDHPs compared to traditional plans. In particular, adult members of families enrolled in HDHPs appear to be at increased risk compared to those in traditional plans. For children, the prevalence of delayed or forgone care due to cost is low and not significantly different within families in HDHPs and traditional plans. Implications for Policy, Delivery or Practice: A differential response to increased cost-sharing in HDHPs may exist for adults and children within a family. The clinical significance of reported delayed or foregone care merits further investigation. Funding Source(s): RWJF Poster Number: 107 Stemming the Increase of Childhood Overweight and Obesity in Delaware Presented by: Allison Gertel-Rosenberg, M.S., Senior Policy and Program Analyst, Office of VP of Policy and Prevention, Nemours, 252 Chapman Road, Christiana Building, Suite 200, Newark, DE 19702; Phone: (302) 444-9171; Email: agrosenb@nemours.org Co-authors: Debbie I. Chang, M.P.H.; Vonna Drayton, Ph.D. Research Objective: The evaluation assesses the population-level longitudinal impact of Delaware’s multi-sector healthy eating and physical activity interventions on children’s knowledge, attitudes, behaviors and health outcomes. The evaluation also explores changes to the system-level environments where children live, learn and play. Study Design: A quasi-experimental evaluation design, documenting and measuring specific indicators (related to knowledge, attitude and behavior changes), assesses the aggregate impact of policy and practice changes in the child’s environment and on population behavior over time. The design is efficient for longitudinal research involving longer time periods, which are necessary for demonstrating population level health outcome changes. This evaluation also captures the degree of policy, practice, and system changes occurring at the state and local levels that are likely to facilitate, and sustain, population-level changes in the long term. Population Studied: The population studied is a representative sample of Delaware children and related systems and environments. Principal Findings: Results from the 2008 Delaware survey suggest that the prevalence of overweight and obesity for Delaware children ages 2-17 years has not changed significantly since measured in 2006. Specifically, no statistically significant (p=0.09) differences in BMI categories were observed between 2006 and 2008. Furthermore, no statistically significant changes in prevalence of overweight and obesity were observed within geographic and demographic categories between 2006 and 2008. For example, the prevalence in Sussex County (41.6% in 2006 versus 39.4% in 2008) and the prevalence among non-Hispanic Whites (35.9% in 2006 versus 37.5% in 2008) were statistically unchanged. There are, however, clear demographic differences within years. Compared to non-Hispanic Whites, nonHispanic Blacks had significantly higher prevalence of overweight and obesity in 2006 (p=0.019), and also in 2008 (p=0.003). Overall, there was a fourfold increase (from 5% to 19%) between 2006 and 2008 in Delaware households’ awareness of the 52-1-Almost None message. When there was parental message awareness, significantly more children age birth through 17 years engaged in one hour of physical activity per day (10% vs. 26%, p=0.000) and moderate to vigorous physical activity for more than 20 minutes (21% vs. 33%, p=0.022) between 2006 and 2008. Conclusions: Early results show that the initiative has stemmed the increase in the prevalence of childhood overweight and obesity with findings that prevalence is statistically unchanged for children since 2006. Nemours’ initiative has also spurred increased knowledge of healthy eating and increased physical activity in school and care settings, resulting in policy and practice changes. This model, of focusing on population health and changing policies and practices in multiple settings through strategic partnerships, knowledge mobilization and social marketing, can effectively address obesity and other complex problems facing children today. Implications for Policy, Delivery or Practice: The data indicate that changes are being implemented in systems – schools, child care, primary care – with associated changes in healthy eating and physical activity behaviors, and ultimately health outcomes. The results of this initial evaluation provide evidence for the efficacy of a comprehensive prevention-oriented model. Investments have proved valuable in many ways, including establishing community collaboration and capacity to address other childhood issues and leveraging resources from multiple sources to affect children’s health. Funding Source(s): Nemours Poster Number: 108 Healthy Kids, Healthy Future: Health Promotion in Early Care and Education Presented by: Allison Gertel-Rosenberg, M.S., Senior Policy and Program Analyst, Office of the VP of Policy and Prevention, Nemours, 252 Chapman Road, Christiana Building, Suite 200, Newark, DE 19702; Phone: (302) 444-9171; Email: agrosenb@nemours.org Lead Author: Debbie Chang, M.P.H. Co-authors: Anne De Biasi Research Objective: Combating childhood obesity in early care and education settings is an untapped opportunity. Current national and state efforts tend to focus on improving wellness and preventing obesity in elementary and secondary schools, often overlooking the need for wellness policies in the early care and education system. Research, however, supports the need to provide healthy nutrition and physical activity environments for children at young ages. Therefore identification, promotion and evaluation of policies and practices that foster healthy environments must become a high priority. Study Design: Scattered efforts around the country aim to improve nutrition and increase physical activity in early care and education settings, but greater collaboration and dissemination of these efforts is needed. Recognizing the need for a multidisciplinary approach to child health promotion and obesity prevention, a conference to advance research, policy and practice in the areas of child care and obesity prevention was initiated. Three explicit goals of the conference were identified. Identify promising practices and tools across the nation that are addressing the current childhood obesity epidemic; Identify current promising policies as well as policy opportunities at the state and federal levels that would support obesity prevention/health promotion in child care settings; Identify research gaps in the field. Population Studied: The conference was used to elicit multiple stakeholders’ views on the issues and opportunities pertaining to childhood obesity in early child care settings. Principal Findings: Many participants at the conference have been working to develop, support and implement children’s health promotion and obesity prevention polices at the local, state and federal levels. This conference was one of the first opportunities for stakeholders across disciplines to share efforts that have been successfully implemented in their communities. The nation’s leaders discussed their expertise in policies, practices and tools in topics including the importance of oral health, limited screen time and breastfeeding, as well as general nutrition and physical activity wellness strategies. Conclusions: As a next step to continue advancing the field, leaders have decided to form the Healthy Kids, Healthy Future Steering Committee, intended to support continued collaboration among the field’s top leaders. The committee will follow up on the many ideas generated at the conference to move the field forward; will continue sharing best practices and policies to encourage dissemination and adoption in the states; and will partner on other innovative strategies to improve children’s health in early care and settings, including policy change and research. Implications for Policy, Delivery or Practice: Bringing together the leaders and experts in the early care and education, nutrition, physical activity, oral health, and child health fields, who in the past have generally worked in silos, with the purpose of discussing promising practices and tools, policy opportunities, and gaps in the evidence base propelled the field forward. Supporting collaboration of efforts, thereby breaking down these silos, allows for a larger scale more effective outcome. These combined efforts, to improve nutrition and physical activity environments in early care and education settings will help create a lifetime of healthy habits for children in the United States. Funding Source(s): Nemours Poster Number: 109 Nationwide Trends in Inpatient Pediatric Cardiac Interventional Procedures from 1997-2007: On-Line Estimates from the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality Presented by: Darryl Gray, M.D., Sc.D., Medical Officer, Center for Quality Improvement and Patient Safety, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850; Phone: (301) 427-1326; Email: darryl.gray@ahrq.hhs.gov Co-authors: Kamal Pourmoghadam, M.D.; Alan Hsu, B.A.; Jennifer Moore, M.P.H.; Claudia Steiner, M.D., M.P.H.; Marshall Jacobs, M.D. Research Objective: Pediatric heart disease (including congenital and acquired lesions of the heart/great vessels) affects 1-2 million Americans of all ages. However, little is known about overall frequencies or outcomes of procedures used to treat these conditions. We used aggregate administrative data to examine US care patterns and outcomes associated with inpatient pediatric cardiac interventional procedures. Study Design: This retrospective descriptive study used estimates from HCUP’s annual Nationwide Inpatient Sample (NIS) and its triennial Kids’ Inpatient Database (KID). The NIS captures administrative data for all discharges from a weighted sample of ~20% of US community hospitals. The KID reflects weighted samples ~10% of normal newborn discharges and ~80% of other pediatric discharges. We identified International Classification of Diseases-Clinical Modification (Ninth Revision) codes for therapeutic (rather than purely diagnostic) cardiac procedures performed via transcatheter or surgical approaches. We queried HCUP’s on-line aggregate data (http://hcupnet.ahrq.gov) to estimate volumes, mean length of stay (MLOS), billed hospital charges, payer mix and inpatient mortality for 0-17 year-olds discharged with these principal procedure codes. Hospital charges, which generally exceed costs but do not include physician fees, were expressed in 2007 dollars using Producer Price Index ratios. We used Census data to generate population-based rates. Population Studied: Weighted, nationally representative estimates of US discharges Principal Findings: NIS procedure discharge rates for 0-17 year-olds in 1997 and 2007 were 37.5 /100,000 and 36.4/100,000 respectively. However, yearly rates fluctuated considerably (e.g., 38.1, 61.0, and 39.3/100,000 in 2004, 2005 and 2006 respectively). KID’s figures were more stable. For an estimated 30,816 discharges (43.5/100,000) in 1997, inpatient mortality=4.6%, MLOS=12.8 days, aggregate charges=$3.3 billion. Payers included private insurance (56.5%; 52.6% of charges) and Medicaid (33.2%; 37.4% of charges); 3.1% were uninsured. KID rates for 2000 and 2003 were 41.1 and 42.5/100,000, while NIS rates were 32.8 and 26.5/100,000 respectively. The 2006 KID estimated that there were 34,434 discharges (46.7/100,000). Mortality=3.4%, MLOS=22.1 days, aggregate charges=$5.9 billion. While private insurance covered 48.0% (44.3% of charges), Medicaid cases (42.8%) generated 47.2% of charges; 2.3% were uninsured. The 2006 KID estimated that there were 19,531 discharges (472.9/100,000) of infants. Mortality=5.1%, MLOS=33.7 days, mean charges=$230,743/case. In contrast, among 14,903 discharges of 1-17 year-olds (21.4/100,000), mortality=1.1%, MLOS=6.1 days, mean charges=$94,907/case. These findings mirror patterns seen in earlier KID and NIS data. Conclusions: Sampling considerations and other factors make the KID a more robust source than the NIS for inpatient pediatric cardiac procedure data. KID procedure volumes and rates rose modestly from 1997 to 2006; unadjusted mortality declined. However, as measures of resource use (and indirect measures of treatment intensity), MLOS and inflation-adjusted charges nearly doubled, and Medicaid payments increased. Infants had considerably higher procedure rates, mortality, MLOS and charges than did 1-17 year-olds. Implications for Policy, Delivery or Practice: The considerable discharge volumes, resource use and mortality associated with pediatric cardiac procedures (especially for infants) indicate the societal importance of these interventions. These findings, along with our observations of growing Medicaid involvement and of possible underrepresentation of uninsured patients (~11-15% of US children) reflect HCUPnet’s useful aggregate data. They argue for more population-based encounter-level research on patterns and outcomes of pediatric cardiac procedures. Poster Number: 110 Oral Health in Rural South Carolina: The Importance of the Relationship Between School Nurses and the Dental Community Presented by: Jeff Hatala, M.M.C., M.B.A., Graduate Research Associate, SC Rural Health Research Center, University of South Carolina, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210; Phone: (803) 251-6317; Email: jhatala31@gmail.com Lead Author: Amy Brock-Martin, Dr.PH. Co-authors: Kyle Shah; Janice Probst, Ph.D. Research Objective: To understand the challenges faced by school nurses in getting their students dental care, and to see if rural school nurses have greater challenges than urban school nurses. Study Design: Electronic survey was used to gather the data from school nurses. Electronic list of nurses is maintained by SC Dept. of Health and Environmental Control. Urban Influence Code was matched with the zip code of the school to determine which schools were rural. Population Studied: school nurses in South Carolina (n=900) Principal Findings: Over 85% of school nurses responded to the survey. Rural school nurses face more challenges than urban school nurses. When examining the challenges faced by school nurses with rural location, we find that lack of parent involvement is the only statistically significant finding (p <.05). Via logistic regression, we further investigated the relationship between lack of parent involvement and rural location; we found rural school nurses, when compared with urban school nurses, are almost 1.7 times more likely to face the challenge of lack of parent involvement. Conclusions: The challenges that school nurses reported they faced are not driven by the dental community, but by the parents of the children needing oral health services. The key to providing successful oral health care to school-age children lies in parental involvement and support for their children. Implications for Policy, Delivery or Practice: As many of these parents may be unmarried parents with hourly jobs, taking time from work may reduce the family income. One possible recommendation is for dentists in rural areas to periodically offer extended hours during non-traditional work time or some weekend hours to allow those children to receive dental care. Nurses, schools and the dental community can leverage their positive partnership to develop ways that further encourage parents to support their children. Future research may want to examine perceptions of school nurses from other states as well. Funding Source(s): American Dental Association and the South Carolina Dental Association (SCDA) Poster Number: 111 Is Emergency Department Utilization Associated with Primary Care Utilization among Low-Income Children? Presented by: Margaret Holland, Ph.D., M.P.H., postdoctoral fellow, Department of Pediatrics & School of Nursing, University of Rochester, 601 Elmwood Avenue, Box SON, Rochester, NY 14618; Phone: (585) 273-2054; Email: margaret_holland@urmc.rochester.edu Co-authors: Byung-Kwang Yoo, M.D., Ph.D.; Harriet Kitzman, Ph.D.; Peter Szilagyi, M.D., M.P.H.; Linda Chaudron, M.D., M.S.; Helena Temkin-Greener, Ph.D., M.P.H. Research Objective: Experts are concerned about high use of emergency departments (ED), resulting in elevated healthcare costs and frequent overcrowding of EDs. Low-income children are known to use the ED more than higher-income children. There is some evidence that increased community-level primary care capacity may decrease ED use. However, few studies have examined the relationship between ED and primary care use among low-income children. We examined if primary care use (well-child care (WCC) and sick visits) is associated with overall ED visits and with potentially avoidable ED visits among low-income children. Study Design: Ordered logistic regression was utilized to determine if primary care use was associated with each of 5 ED visit categories: all ED visits, injury/ingestion only, reasons other than injury/ingestion, ambulatory-care sensitive (ACS) conditions (may be avoidable with timely primary care), and non-ACS conditions. All models controlled for children's chronic conditions, birthweight, and demographics. Medical records for children were collected from birth to 24 months. Interviews at the mother’s enrollment (during pregnancy) and at 12 and 24 months after birth provided demographic information. Population Studied: 433 low-income, urban mother-child pairs from the Nurse-Family Partnership MeM.P.H.is trial control group (observed without intervention). Primiparous women were recruited from an obstetrical clinic and met 2 of 3 high-risk criteria: unmarried, unemployed, or less than 12 years of education. Principal Findings: On average, children had 2.7 ED visits, 10.1 sick visits, and 5.0 of 9 recommended WCC visits over 2 years. Twelve percent of ED visits were for injury/ingestion; 49 percent of ED visits were for ACS conditions. More sick visits to primary care were associated with more ED visits when all ED visits was the outcome (OR: 1.18, p<0.001). This association held for all other subsets of ED visits, although the magnitude was significantly lower for injury/ingestion visits only (OR: 1.03, p<0.04) and non-ACS visits (OR: 1.11, p<0.001). WCC visits were not associated with ED utilization. These results did not change when WCC and sick visits were estimated together in the same models. Conclusions: Sick visits to primary care were associated with increased ED use among individuals in this population of low-income children, even when controlling for chronic conditions. Wellchild care visits were not associated with ED use. Unlike in other populations, in which greater access to primary care visits are associated with fewer ED visits, in this low-income population more primary care visits for illness are associated with more ED visits. Implications for Policy, Delivery or Practice: If these findings are replicated, it may be that among low-income children primary care visits do not deter ED visits. Efforts to lower healthcare costs may need to focus on other areas. Funding Source(s): AHRQ Poster Number: 112 How Well Does the Children with Special Health Care Needs Screener Identify Children with Disabilities? Presented by: Amy Houtrow, M.D., M.P.H., Assistant Professor, Pediatrics, University of California, San Francisco, 500 Parnassus, San Francisco, CA 94143; Phone: (415) 476-3899; Email: houtrowa@peds.ucsf.edu Co-authors: Joan Hilton, Ph.D.; Megumi Okumura, M.D. Research Objective: Children with disabilities are amongst the most vulnerable members of society. It is a public health goal to improve the health and quality of life of children with disabilities. A screening instrument that identifies children with disabilities would be of benefit to the health services research community. The Children with Special Health Care Needs (CSHCN) Screener is used in multiple national surveys to identify CSHCN and could be a valuable tool to identify those with disabilities. At this time, there are no studies validating its use as a screening tool for disabilities. Therefore, our objective is to determine the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the CSHCN Screener for CSHCN with disabilities. Study Design: We used the National Survey of Children with Special Health Care Needs 2005-06 (N= 40,723). CSHCN with disabilities could potentially be identified in the Screener by the set of questions used to determine which children have conditions that last at least one year and are associated with limitations in their ability to do the things most children of the same age can do. In the Health and Functional Status of the Survey, seven of the 14 ‘difficulty’ questions are relevant to disability – difficulties with mobility/coordination, self-care, fine motor skills, learning, communicating, vision despite correction, and hearing despite hearing aids. We used these questions as our markers of disability in order to test the sensitivity, specificity, positive and negative predictive value of the Screener. Population Studied: Nationally representative sample of CSHCN aged 0-17 years in the United States. Principal Findings: Using our seven disability questions, 49.3% of CSHCN were identified as having at least one disability. Cognitive disabilities were identified in 43.4% of CSHCN, while physical disabilities were identified in only 22.8%. In contrast, 21.4% of respondents identified their child as having a disability on the Screener. The Screener’s PPV was 82.1%, the NPV was 59.6%, the sensitivity was 35.7% and the specificity was 92.4%. While nearly 60% of respondents with a child who had mobility, self care or fine motor disabilities identified their child has disabled on the Screener, only one third of children with cognitive disabilities were identified by the Screener as having a disability. Conclusions: The CSCHN Screener does not identify all CSHCN with disabilities. Implications for Policy, Delivery or Practice: If the Screener is used to estimate the prevalence of disability in childhood, millions of children with disabilities will not be identified. This will lead to low estimates of disability prevalence that could have significant policy implications. As children with disabilities require more health and related services than other children and face significant social challenges and barriers to their well-being, it is imperative to accurately identify these children in order to provide needed services and funding. Researcher utilizing the CSHCN Screener should consider using other measures of disability available in national datasets when studying children with disabilities. Funding Source(s): AHRQ, NIH-NICHD Poster Number: 113 Enhancing Pediatric Psychopharmacology for ADHD in North Carolina’s Medicaid Program Presented by: Charles Humble, M.S.P.H., Ph.D., Director, Analytic Services, AccessCare, 3500 Gateway Centre Boulevard, Suite 130, Morrisville, NC 27560; Phone: (919) 380-9962; Email: chumble@ncaccesscare.org Co-authors: Peter Scott Jensen, M.D.; Lynn Wegner, M.D.; Steven Wegner, M.D., J.D.; Christopher Kratochvil, M.D.; Alan Stiles, M.D. Research Objective: To examine the characteristics and baseline treatment practices of primary care providers (PCP) who care for pediatric patients with Attention Deficit/Hyperactivity Disorder (ADHD) in North Carolina’s largest network of Medicaid providers (AccessCare). These data will underpin subsequent tests of the relative impact of two interventions of differing intensity, each designed to increase the likelihood that providers will employ expert-recommended “best practices” in the assessment and treatment of children and adolescents with ADHD, the most common psychiatric diagnosis in children. Results of this pilot program will inform decisions regarding future directions in provider training in North Carolina’s Medicaid program and possibly elsewhere. Study Design: Physicians and other providers who prescribe medications in AccessCare member practices were invited to attend an intensive, 3-day training in pediatric psycho-pharmacology in November, 2009. One condition for attendance was willingness for the PCP’s practice to be randomized to receive complementary training for the practice’s care coordinator to enhance the coordination of ADHD care. The program includes baseline and follow-up assessment of trainees’ knowledge of current practice guidelines for ADHD and selfassessed competence using them to diagnose and monitor care of patients. Clinical teaching is reinforced though hands-on opportunities for sustaining practice and problem-solving vis-à-vis obstacles to implementation, the use of key opinion leaders, access to additional web-based tools that PCPs can use to obtain information and learn at their own pace. Support networks are developed by conducting training in small PCP peer groups and through bi-weekly conference calls. The intervention group received additional training for care coordinators and office staff in specific strategies designed to identify and remove obstacles to use of diagnostic scales and symptom checklists. Population Studied: A volunteer sample of 55 providers actively caring for pediatric patients with ADHD covered by NC’s Medicaid program Principal Findings: Initial analyses show that providers in the Intervention and Usual Care arms of the study are balanced in terms of numbers of patients with ADHD diagnoses and regional dispersion across the state. Overall they report seeing an average of 91 pediatric patients with psychiatric problems per week. At baseline, 95% of providers rate their competence treating ADHD as Good or Excellent. Sixty-one percent of providers report caring for 80-100% of child patients with ADHD without consulting other providers. Stimulant therapy is the favored method of treatment. Fiftyeight percent said that prescribers in similar settings use parent and teacher rating scales to assess ADHD symptoms at baseline; 29% of similar providers would test different medication doses each week during initial titration; and only 19% would use parent side effects scales during regular visits. Conclusions: Although Medicaid providers at baseline report high levels of competence treating ADHD in pediatric patients, their descriptions of community norms in various aspects of treatment suggest opportunities for improving the use of clinical practice guidelines for ADHD diagnosis and treatment with pediatric patients – the principal outcomes in this pilot study. Implications for Policy, Delivery or Practice: Demonstration of successful improvement in ADHD care in the primary care setting may allow more cost-effective options for appropriate and patientfriendly care for North Carolina’s pediatric Medicaid clients. Funding Source(s): NIMH Poster Number: 114 Lifetime Medical Cost Attributable to Early Childhood Obesity and a Simulation of Affordable Interventions Presented by: Frick Kevin, Ph.D., M.A., Professor, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadway, Rm. 606, Baltimore, MD 21205; Phone: (410) 614-4018; Email: kfrick@jhsph.edu Lead Author: Sai Ma, Ph.D. Co-authors: Kevin D. Frick, Ph.D. Research Objective: Obesity continues to be a public health crisis in the United States: over the last three decades, the obesity rate for preschoolers has tripled to 12%. Childhood obesity is linked to numerous adverse health consequences such as obesity in adulthood and other comorbidity, which can further result in unfavorable social consequences such as reduced lifetime academic achievement, loss of productivity, and a reduced income earning capacity. Consequently, policymakers and researchers began to pay increasing attention to early interventions. Yet, no calculation has been made to assess under what conditions early interventions could be economically justified. Therefore, this study seeks to answer: 1) What are the lifetime medical costs attributable to early childhood obesity? And 2) At what level of effectiveness and cost would a population-based early intervention be affordable? Study Design: This study relies on three data sources: the prevalence of obesity at all ages was estimated from the National Health and Nutrition Examination Survey, the persistence of obesity from childhood to adulthood was determined by a thorough literature review, and medical costs attributed to obesity was estimated from the 2006 Medical Expenditure Panel Survey, using a standard two-part econometric model. Simulations were then conducted to estimate cost-savings of interventions that take place at different ages with a range of effectiveness. Population Studied: The study population includes all noninstitutionalized Whites, Blacks and Hispanics living in the United States. Pregnant women are excluded. Principal Findings: The literature review suggests between 50% and 75% obese children at age 5 will remain obese in adulthood. In 2006, each obese adult spent $1,548 (41%) more, and each obese child (6-17) spent $264 (27%) more on annual medical expenditure than normal-weight counterparts. Lifetime medical cost attributable to obesity is calculated by race, gender, and smoking status. For example, compared to a white nonobese female non-smoker, the additional average lifetime medical cost of a white obese female nonsmoker is $140,919, among which, $36,279 is attributable to early childhood obesity. Results of the simulations reveal that if the goal is to prevent 500,000 obese children becoming obese adults, we would need early interventions (0-5) at 55% effectiveness level, or interventions (6-11) at 25% effectiveness or later interventions (12-17) at an effectiveness of 20%. As for cost-savings, at 50% effectiveness, population-based interventions at 0-5 can achieve $41 per capita medical cost-savings, interventions at 6-11 yield $90 per person, and interventions at 12-17 can save $119 medical cost per person. Conclusions: Our simulation shows that population-based childhood interventions, even with moderate effectiveness and only considering medical cost-savings, would yield positive economic returns. Implications for Policy, Delivery or Practice: Interventions could play a critical role in preventing childhood obesity, reversing obesity after it occurs, and avoiding adult obesity among those who are obese as children. Our study demonstrates the significant returns of intervening early childhood obesity and should motivate policy-makers to take serious actions to encourage the development of new effective intervention, especially given that government currently takes the largest share of medical cost attributable to obesity. Funding Source(s): The PEW Charitable Trusts & the Zanvyl and Isabelle Krieger Fund. Poster Number: 115 Association Between Acanthosis Nigricans and Risk Factors for Type 2 Diabetes among Hispanic Children in a Texas-Mexico Border Community Presented by: Sion Lee, Research Assistant, South Texas Border Health Disparities Center, The University of Texas - Pan American, ITT Building, Room 1.404Q, 1201 West University Drive, Edinburg, TX 78541-2999; Phone: (956) 316-7937; Email: sionlee@fas.harvard.edu Co-authors: Suad Ghaddar, Ph.D.; Doreen Garza, M.P.H.; David Salazar, M.S.; Patricia Keck, M.S.N., R.N. Research Objective: Acanthosis nigricans (AN) is a dermatologic condition characterized by velvety hyper-pigmentation and thickening of skin folds. In general, AN is associated with obesity and can be an indication of various conditions related to insulin resistance. The objective of this study is (1) to report on AN prevalence rates among Hispanic children in a Texas-Mexico border community, and (2) to examine associations of AN with other risk factors for type 2 diabetes. Study Design: Data is from the 2005 Texas Risk Assessment for Type 2 Diabetes in Children, a state-level program that screens children for the AN marker in Texas public and private schools. Children who are positively identified with the marker undergo additional assessments of body mass index (BMI) and blood pressure. Our analysis focuses on a subset which includes children who were screened for obesity and hypertension irrespective of their AN diagnosis. We utilize binary logistic regression to assess factors associated with the presence of the AN marker. Population Studied: Students of a school district in a predominantly Hispanic Texas-Mexico border community characterized by high rates of obesity (34% of county population vs. 26% nationwide) and diabetes prevalence (17% of county population vs. 8% nationwide). Principal Findings: Of 6,822 students screened, 99.6% were Hispanic and 51% male. Students were almost evenly distributed among four grade levels (3rd, 5th, 7th, and 9th). AN was detected among 22.8% of the subjects. Approximately 9% of the students screened were hypertensive and 11.6% pre-hypertensive. About a quarter were obese and 17.2% overweight based on age- and genderspecific BMI categorization. Binary logistic regression results revealed that AN was less prevalent among males (OR: 0.55, 95% CI: 0.480.64), and more prevalent among 5th (OR: 1.76, 95% CI: 1.44-2.14) and 7th (OR: 1.66, 95% CI: 1.37-2.03) graders relative to the younger group. Those who were obese (OR: 41.39, 95% CI: 33.8850.57), overweight (OR: 8.02, 95% CI: 6.49-9.91), hypertensive (OR 1.41, 95% CI: 1.12-1.77), and pre-hypertensive (OR 1.47, 95% CI: 1.21-1.79) were also more likely to have the AN marker. Conclusions: Our findings reflect the increasing trend in AN prevalence rates among Hispanics. While earlier studies reported rates of 5-7% within this group, more recent studies report rates that are similar to those found in this study (22.8%). Furthermore, the presence of the AN marker is associated with obesity and hypertension, both of which are risk factors for type 2 diabetes. Implications for Policy, Delivery or Practice: Screening programs constitute the basis to identifying at-risk populations and to guiding prevention efforts for type 2 diabetes. Our results underscore the importance of intervention programs that address childhood obesity. Current policies of the Texas Risk Assessment program include notifying parents and issuing medical referrals. Future efforts should include following-up on ANpositive students and the outcomes of the physician referral process. Findings from this program have also triggered interventions in the border school district analyzed (increasing physical activity duration beyond the state-mandated level, nutritious lunch menus and snacks, etc.). Preliminary results suggest positive effects on obesity rates. Future research will explore the effects of these interventions on obesity, hypertension, and AN prevalence rates. Funding Source(s): CDC Poster Number: 117 Seven Year Mortality Trend at U.S. Children's Hospitals for Patients Critically Ill on the First Hospital Day Presented by: James Levin, M.D., Ph.D., Chief Medical Information Officer, Children's Hospital of Pittsburgh of UPMC, 4401 Penn Avenue, Pittsburgh, PA 15224; Phone: (412) 692-6756; Email: jim.levin@chp.edu Research Objective: Although mortality is relatively uncommon at United States children's hospitals, the subset of patients who are critically ill on the first day of hospitalization are at higher risk. Successfully treating these patients challenges care delivery systems. A previous report from The Children's Hospital of Pittsburgh of UPMC (CHP) concluded that there had been a significant increase in risk adjusted mortality in the five months after the introduction of the computerized provider order entry (CPOE) phase of an electronic medical record (EMR). This study extends that analysis in four ways: 1) All patients on vasoactive medications on the first day of hospitalization are included, 2) Post-implementation time frame is extended to 6 years, 3) The population is broadened to include patients from 20 hospitals, 4) The APR-DRG risk of mortality (ROM) classification is employed to predict mortality ratios. Study Design: A retrospective study was performed using administrative data. Patient encounters were included if the patient received one or more vasoactive medications on the first day of hospitalization. These medications are commonly used for a broad range of critically ill patients and are rarely used outside of an intensive care setting. The mortality ratio for each ROM group within the study population was used to calculate standardized mortality ratios (SMR). Population Studied: Data were analyzed from the Pediatric Health Information System (PHIS, Child Health Corporation of America), 1,544,037 consecutive inpatient discharges from 2002 to 2008 were evaluation. 684,682 patients received one or more vasocative medications on the first day of hospitalization. Principal Findings: From 2002 to 2008 the unadjusted mortality ratio declined from 8.4% to 6.7% and the SMR declined from 1.16 to 0.91 (22%, p<0.01). At CHP, the SMR declined from 1.20 to 0.91 (-24%, p<0.10). All 20 hospitals showed improvements. The hospital interquartile range was -9% to -32%. During the first 6 months of CPOE at CHP the SMR increased from 1.08 to 1.17 (+8%, NS) when compared to the last 6 months prior to CPOE. Increases of this magnitude or larger occurred during 32% of the quarters at CHP and 33% of all hospital quarters. Conclusions: Between 2002 and 2008 there was significant decrease in the proportion of critically ill patients failing to survive to discharge from 20 children's hospitals. It is common for the SMR to fluctuate when looking at a single hospital over a relatively short period of time. Implications for Policy, Delivery or Practice: The study demonstrates improvements in pediatric critical care over 7 years. Comparisons over shorter time frames or between individual hospitals need to be interpreted with caution, however. Improvements in risk adjustment methodology are needed but the low frequency of deaths will continue to make comparisons challenging. CHP was one of the first children's hospitals in the country to begin a mutliyear implementation of an EMR and in 2009 became the first pediatric hospital to achieve a completely digital care environment. Although a previous study raised the question of an unintended consequence of health information technology, the current analysis does not support an unusual increase in mortality in the first months after CPOE introduction. Poster Number: 119 Measuring Medical Homes: Tools to Evaluate the Pediatric Patient- and Family-Centered Medical Home Presented by: Rebecca Malouin, Ph.D., M.P.H., Assistant Professor, Department of Family Medicine and Department of Pediatrics and Human Development, Mcihigan State University, B-101 Clinical Center, East Lansing, MI 48824; Phone: (517) 884-0453; Email: rebecca.malouin@ht.msu.edu Co-authors: Sarah Merten, M.P.H. Research Objective: The pediatric medical home has historically been defined by care that is accessible, family-centered, continuous, comprehensive, coordinated, compassionate and culturally effective. Differentiating a practice that meets criteria as a medical home from one that does not is of great importance in determining (1) which activities successfully transform practices and (2) which degree of “medical homeness” is associated with better outcomes and reduced healthcare expenditures. Furthermore, identification of some standard measurement criteria is recommended for practices participating in pilot projects to reduce provider and practice reporting fatigue, and allow for comparison of outcomes across projects. The objective of this research was to identify and review instruments for use as an assessment tool for “medical homeness” using the attributes within the American Academy of Pediatric’s (AAP) Desirable Characteristics of a Medical Home. Study Design: The study design is that of a literature review. Instruments were identified through a literature review using PubMed and through informal interviews with opinion leaders in the fields of maternal and child health and pediatrics. Instruments were rated based on number of questions pertaining to the following characteristics: comprehensiveness, coordination, continuous, accessibility, family-centered, compassion and cultural effectiveness. Population Studied: The unit of analysis is an instrument. Instruments were selected for review if their purpose is to explicitly assess pediatric medical homeness or if they include at least two of the attributes of the AAP’s Desirable Characteristics of a Medical Home. Principal Findings: Sixteen instruments were identified and reviewed. Across all instruments assessed, coordination and family-centered care were the most represented attributes of the patient and family-centered medical home. Accessibility and compassion were the least represented attributes, likely due to the level of specificity used in the examples of accessibility within the Desirable Characteristics of a Medical Home described by the AAP and the difficulty in developing a measure of compassion. The Family-Centered Care SelfAssessment Tool and the Primary Care Assessment Tools (PCAT) contained the most elements of the pediatric medical home as defined by the AAP. None of the tools included more than one element of all domains as defined by the Desirable Characteristics of a Medical Home. Conclusions: The fact that none of the instruments included more than one question relating to the domains as defined by the Desirable Characteristics of a Medical Home may be partly due to the fact that the elements described within the AAP practice accessibility domain, such as acceptance of all insurance and accessibility by public transportation, are quite specific. Consensus on the specific elements to be included within each attribute of the patient and family-centered medical home is needed. Implications for Policy, Delivery or Practice: Identifying instruments with immediate practical relevance for providers, families and patients is of critical importance. Having immediately useful information available from comparable practice surveys will encourage patients, families and providers to remain engaged in the evaluation process as well as provide critical information that can actually affect the transformational process through provision of quality improvement reports. The American Academy of Pediatrics is publishing this work as a book titled, “Measuring Medical Homes: Tools to Evaluate the Pediatric- and Family-Centered Medical Home”. Funding Source(s): HRSA, American Academy of Pediatrics Poster Number: 120 The Role of State Early Intervention (EI) Eligibility Policy on EI Participation Rates Among Young Children with Special Health Care Needs Presented by: Beth McManus, P.T., M.P.H., Sc.D., RWJ HSS Scholar, Population Health Sciences, University of Wisconsin-Madison, 610 Walnut Street, 707 WARF, Madison, WI 53726; Phone: (617) 529-8138; Email: mcmanus2@wisc.edu Co-authors: Marie McCormick, M.D., Sc.D.; Dolores Acevedo-Garcia, Ph.D.; Micheal Ganz, Ph.D.; Penny Hauser-Cram, Ed.D. Research Objective: In this study, we sought to describe differences in Early Intervention (EI) participation across US state among a cohort of young children with parent-reported developmental delays and disabilities. Study Design: This was a cross-sectional multilevel analysis. Logistic multi-level models were used to estimate the relative contributions of child socio-demographic and developmental characteristics, and state EI eligibility policy on EI participation. We first derived a model of access to EI services based on the socio-demographic and special needs characteristics of the children. We then examined the effects of state eligibility policies using multi-level modeling to account for the clustering of children nested within states. This approach also permitted us to examine the crosslevel interaction between state EI eligibility policy and individual poverty status, controlling for other factors. Population Studied: We used the 2005-2006 National Survey of Children with Special Health Care Needs (CSHCN) to select a cohort of CSHCN at risk for neurodevelopmental delay. We selected children less than three years of age who had a diagnosis or parent report of developmental difficulty that affected their function at least some of the time. In addition, children also met one of the following Maternal and Child Health Bureau CSHCN criteria: requiring more medical, educational, or behavioral services when compared to children of similar age; or receiving or needing physical, occupational, or speech therapy; or having functional limitations; or having behavioral or developmental difficulties. Principal Findings: We observed an overall rate of EI participation of 45.7% that ranged 23.1% to 83.3% across the states. EI participants were less likely to be Hispanic, living in a multi-racial family, poor, with a developmental delay, or with less severe impairments. The probability of receiving EI was lower for children living in states with more strict EI eligibility criteria than those with liberal criteria (0.43 vs. 0.52).Poverty influenced this association with the adjusted probabilities of receiving EI for poor (<100% Federal Poverty Level, FPL) and non-poor children (> 185% FPL) being 0.18 and 0.36, respectively. Among non-poor children, those living in states with strict eligibility criteria were nearly as likely as poor children living in states with liberal eligibility criteria to receive EI (0.33 vs. 0.36). Conclusions: Our results of this study reveal marked disparities and unmet needs in EI participation as a function of both characteristics of the child and the state program. Implications for Policy, Delivery or Practice: Our findings highlight areas of unmet need for EI services within vulnerable populations and the contribution of state policies to ameliorating or exacerbating these disparities. They have important policy implications to guide improved outreach to families of children with special health care needs. Funding Source(s): CDC Poster Number: 121 Social Inequalities in Preschool Special Education Participation Among Children with Developmental Delays and Disabilities Presented by: Beth McManus, P.T., M.P.H., Sc.D., RWJ HSS Scholar, Population Health Sciences, University of Wisconsin-Madison, 610 Walnut Street, 707 WARF, Madison, WI 53726; Phone: (617) 529-8138; Email: mcmanus2@wisc.edu Co-authors: Adam Carle, Ph.D.; Dolores AcevedoGarcia, Ph.D.; Michael Ganz, Ph.D.; Penny HauserCram, Ed.D.; Marie McCormick, M.D., Sc.D. Research Objective: In this study, we examined state variability in preschool Special Education participation among a cohort of children in the United States with parent-reported developmental delays and disabilities. In addition, we sought to determine to what extent child characteristics and state socio-economic attributes explained state variability. Study Design: We used a cross-sectional multilevel analysis and fit a series of multi-level logistic models to determine 1) overall state differences in children’s receipt of preschool Special Education, 2) the relative contribution of child socio-demographic characteristics, and 3) the effect of state income inequality, Special Education funding sources and state Special Education eligibility policy, controlling for child and family characteristics. Population Studied: We used data from the 20052006 National Survey of Children with Special Health Care Needs (CSHCN) and selected a sample population of preschool-aged children (ages 3-5) whose parents reported a developmental delay or disability that affected the child’s function at least some of the time In addition, children also met one of the following Maternal and Child Health Bureau CSHCN criteria: requiring more medical, educational, or behavioral services when compared to children of similar age; or receiving or needing physical, occupational, or speech therapy; or having functional limitations; or having behavioral or developmental difficulties. Principal Findings: The observed an overall rate of Special Education participation of 42.5%. However, we found significant variation across states in rates of Special Education ranging from 14.3%% to 65.4%. Special Education recipients were more likely to be non-poor [adjOR: 1.3, 95% CI:(1.02, 1.73)]; male [adjOR:1.67; 95% CI: (1.32, 2.09)], and have severe developmental disabilities [(OR: 3.68; 95% CI: [2.76, 4.90)]; and least likely to be Black, non-Hispanic [adjOR: 0.65; 95%CI: (0.47, 0.90)]. Special Education participation rates were highest (54%) in states with the least income inequality and lowest (31%) in the most unequal states (p<0.001). Above and beyond child and family characteristics, the income disparity between most and least equal areas was significantly associated with an increased odds [adjOR: 2.29; 95% CI: (1.5, 5.42)] of receiving Special Education and this pattern persisted across all states [IOR:1.5, 3.5]). Conclusions: We found marked social disparities and unmet need in preschool Special Education participation that stemmed, in part, from individual child characteristics, but to an additional extent, from state socio-economic attributes. Implications for Policy, Delivery or Practice: Our findings suggest that state income inequality translates into disparate opportunities for education for children with disabilities. Strategies to ameliorate inequalities might include reducing barriers to Special Education by 1) promoting community-level developmental screening and referral, 2) ensuring seamless transition between Early Intervention and preschool Special Education, 3) bolstering universal preschool and inclusion programming for children with disabilities, and 4) assessing Special Education implementation to reduce undue financial burden to communities and psychological distress to families. Funding Source(s): CDC Poster Number: 122 The Effect of Sibling Configuration on Children’s Access and Use of Medical Care Presented by: Sean Orzol, M.P.H., M.A.E., Doctoral Candidate, Health Management and Policy, University of Michigan, 1415 Washington Heights M3141, Ann Arbor, MI 48109; Phone: 734560-3111; Email: orzol@umich.edu Co-authors: Thomas Buchmueller, Ph.D. Research Objective: Family structure is acknowledged as a potentially important factor in determining a child’s access to medical care. Previous research has documented an inverse relationship between the size of the family and children’s use of medical care. These findings are often used to lend support to the “resource dilution hypothesis” – the larger the family the less resources, including health care resources, can be allocated to any one child. What is often ignored in such research is that family size is correlated with birth order, and that some of the observed relationship between family size and access to medical care might therefore be a marker for a birth order effect on access to care. Whereas the resource dilution hypothesis implies that children in larger families may be receiving less than the optimal amount of medical care, if it is birth order rather than family size that matters, this normative conclusion may not be warranted. This study investigates the effect of sibling configuration on children’s access and use of medical care. Specifically, it examines the extent to which birth order and the number of children in a family is related to various measures of access to health care. Study Design: We use data obtained from the 1998-2006 National Health Interview Survey (NHIS) and the 1996, 2000, and 2004 panels of the Survey of Income and Program Participation (SIPP) and proceed in two steps. First, we run multivariate regressions on cross sectional data, allowing us to explore the relationship by looking at “betweenfamily” differences in sibling configuration. Second, we utilize information on multiple children per family in the SIPP and run models accounting for unobserved heterogeneity using family fixed effects. Population Studied: A nationally representative sample of children aged 0 to 15 years. Principal Findings: Findings using the NHIS suggest that some aspects of children’s health care may be influenced by family size, giving support to the dilution of resources hypothesis. We also find some evidence that birth order may be related to the type and amount of care children receive, independent of family size. Conclusions: Our preliminary results suggest that both family size and birth order may each be an important factor influencing some types of children’s use of medical services. We find suggestive evidence that the resource most impacted by size of the family is parental time, not financial. Implications for Policy, Delivery or Practice: Sibling configuration is complex and important information might be missed if the correlation between birth order and family size is not considered when modeling its relationship on child outcomes. Children are dependent upon their parents to obtain and initiate health care services, as such, health care practitioners may need to consider a child’s family context when administering or planning their health care services. Additionally, understanding the mechanism through which family size may affect health care access and utilization is essential if we are to develop effective tools to ensure timely and appropriate health utilization of children at risk. Poster Number: 123 Antipsychotic Polypharmacy among Michigan Medicaid Youth Presented by: Robert Penfold, Ph.D., Instructor, Department of Population Medicine, Harvard Medical School, 133 Brookline Avenue, 6th Floor, Boston, MA 02215; Phone: (617) 509-9826; Email: robert_penfold@hphc.org Co-authors: Kelly Kelleher, MD, M.P.H.; Brandon Strange, M.D.; Kathleen Pajer, M.D.; Wei Wang, M.Sc. Research Objective: The prevalence of antipsychotic polypharmacy has been increasing in adult populations. Our objective was to measure the prevalence of pediatric antipsychotic polypharmacy and identify the the most common diagnoses associated with this prescribing pattern. Study Design: We employed a longitudinal cohort study design. Antipsychotic polypharmacy was defined as the concurrent use of two or more antipsychotic medications for a minimum of 60 consecutive days. We calculated age and sex standardized rates of polypharmacy between 2000 and 2003. We also calculated the prevalence of mental health diagnoses among children using multiple antipsychotic medications. Population Studied: We identified all individuals aged 6 to 21 years who were continuously enrolled in Michigan Medicaid between January 2000 and December 2003. Principal Findings: The rate of antipsychotic polypharmacy in the Michigan Medicaid youth population nearly tripled between March 2000 and October 2003 from 1.85 to 5.73 per 100,000 person days of eligibility. Of the 122 individuals using multiple antipsychotic medications, 44.0% had at least one diagnosis of mental retardation. Approximately 12% of individuals had at least one diagnosis for a psychotic disorder. Concomitant prescribing of risperidone with another atypical antipsychotic was the most common (42.5%) treatment strategy with quetiapine being the most common addition. Conclusions: Antipsychotic polypharmacy among Michigan Medicaid youth followed a similar growth trend to that observed in adult populations over the same time period. However, the treatment strategy is most common among children with moderate to severe mental retardation. Antipsychotic polypharmacy in the Michigan Medicaid population does not appear to be related to treatment refractory psychotic disorders or externalizing disorders. Implications for Policy, Delivery or Practice: There is very little evidence supporting the use of multiple antipsychotic medications in children and adolescents. The results of this study suggest that much antipsychotic polypharmacy in the Michigan Medicaid population is inappropriate. Given the risks that antipsychotic medications pose to the developing body and brain, policy makers should consider strategies that strictly limit antipsychotic polypharmacy. Funding Source(s): NIMH Poster Number: 124 Primary Injury Prevention and Mortality from Motor Vehicle Crashes among Children and Adolescents in the United States: From Safety Behaviors to Healthy Environments Presented by: Luis Pinet-Peralta, M.Sc., Research Assistant, Public Policy, University of Maryland Baltimore County, 8030 Watermill Court, Elkridge, MD 21075; Phone: (410) 680-6969; Email: lpinet1@umbc.edu Research Objective: The objective of this research is to evaluate the effects that primary prevention policies, particularly those associated with the physical and the social environments, have had on reducing the mortality risk from motor-vehicle crashes involving young children and adolescents in the United States. Study Design: This is a retrospective study based on 1997-2005 data from the FARS, the IIHS, the U.S. Census, U.S. Presidential elections and U.S. labor statistics, and analyzed using negative binomial regression, maximum likelihood estimation and fixed-effects. Population Studied: Children and adolescents involved in fatal motor vehicle crashes in the United States between 1997 and 2005. Principal Findings: I expect to find significant reductions in the proportion of deaths among states with primary enforcement of restraint laws, mandatory driver education programs and checkpoint s compared with states with secondary or inexistent laws. I also expect to find mortality reductions among states with speed reduction and traffic calming measures compared with states where such measures are not available. Conclusions: The research provides an initial evaluation of environmental modification policies and fatal injuries from motor vehicle crashes among children and adolescents at the national level and using a longitudinal perspective. Implications for Policy, Delivery or Practice: Results may be useful to policy-makers and public health practitioners involved in injury prevention and control program development and implementation. Studies that have provided evidence supporting the positive impacts of environmental modifications on injury prevention have been executed in Europe only, where childhood fatal motor vehicle injury rates have been reduced considerably more than in the United States. Poster Number: 125 Do Parents Perceive What Their Children Perceive about Symptoms and General Health? An Analysis Using Longitudinal Data Presented by: Christy Pu, Ph.D., Assistant Professor, Department of Public Health, National Yang-Ming University, Li-Nong Street, Sec 2, Peitou, Taipei, Taiwan 155; Phone: +886285906914; Email: christypu@hotmail.com Co-authors: Nicole Huang, Ph.D.; Yiing-Jenq Chou, Ph.D. Research Objective: This research examines the relationship between perceptions of symptoms by adolescents and their self-rated health (SRH) and whether these perceptions matter when the parents rate the general health of these adolescents. Study Design: We analyzed 1,634 adolescents (814 boys and 820 girls) from the Youth Project conducted by the Academia Sinica of Taiwan. Data from two waves (wav1=2001, wave 3=2003) were used. Two physical and two mental symptoms were used :(1) headache (2) feeling dizzy (3) feeling lonely and (4) feeling depressed. The generalized estimation equation (GEE) with a time trend was used to determine the association between these symptoms and the reporting of reduced health by adolescents. A separate regression was carried out using the reports of the parents. The kappa statistic was used to determine agreement between the adolescents’ own reports and their health as reported by their parents and how such agreement change over time. Population Studied: 1,634 adolescents form Northern part of Taiwan Principal Findings: The results showed that for the adolescents’ own reports, the four perceived symptoms (headache, dizziness, loneliness and depression) were closely associated with reporting reduced general health by the adolescents, but these perceptions were not picked up by their parents in their ratings of the adolescents’ general health. For depressive symptom, parents of girl subjects who had reports of “a little” (OR=0.73, p<0.05), and “sometimes” (OR=0.57, p<0.01) were significantly associated with lower odds of reporting reduced health for these adolescents. Time was significant with OR=0.17 (p<0.01) and OR=0.64 (p<0.01) for the adolescent and parent reports, respectively. The kappa statistic showed that agreement between adolescents’ reports and parents’ reports for general health decreased over time. Conclusions: Perceived symptoms are an important factor in adolescents’ rating of their own general health, but this is no true for the parents’ reports of the adolescents’ general health; furthermore, the degree of agreement decreases over time. Parents may not be good proxies when assessing the health of adolescents. Implications for Policy, Delivery or Practice: When adolescents are the subjects of interest, parents are often used as proxy raters since children and adolescents are sometime assumed to be unreliable respondents. In addition, parents, instead of physicians, are the adults with whom the adolescents have most frequent contact, thus they are responsible for monitoring the health status of the adolescents. It is thus important to ensure parents are aware of their children’s health status for proper treatments to be undertaken. Funding Source(s): Academia Sinica, Taiwan Poster Number: 126 School Gardens: A Comprehensive Nutrition Education Approach to Improve Vegetable Knowledge, Attitudes and Consumption among School Aged Children Presented by: Shelia Roundtree, M.D., M.P.H., Physician, Internal Medicine, Department of Veteran's Affairs, 3510 Augusta Road, Greenville, SC 29605; Phone: (864) 525-8482; Email: tuunee01@yahoo.com Co-authors: James Hardin, Ph.D.; Denise Hodo, M.P.H.; Khosrow Heidari, M.S.; Joseph Beraho, M.D.; George Nixon, M.D. Research Objective: Childhood overweight and obesity constitute a formidable public health challenge. The cost in terms of morbidity, mortality and fiscal burden are virtually incalculable. Overweight children tend to become overweight adults. This study sought to determine whether a school garden based curriculum could favorably influence childrens' vegetable knowledge, attitude and consumption. Study Design: Two groups of school children participated in a comprehensive, validated school garden curriculum. The children in the control group received usual grade-appropriate instruction with no special eM.P.H.asis on nutrition or vegetable consumption. Those in the intervention group planted, prepared and consumed fresh vegetables. Throughout the intervention classroom teachers taught nutritional facts as outlined in the curriculum. Pre and post intervention test data were analyzed using analysis of variance adjusting for school, sex, group, time, and the interaction of group and time. Knowledge was assessed from a 5-item multiple choice test while satisfaction was assessed using 10 vegetable-specific Likert scale questions. Population Studied: Our sample consisted of 345 school-aged (8-12 years) children from two schools in one school district. Principal Findings: Students in the intervention group had significantly higher post-study knowledge scores than those students in the control group (p<0.001). Compared to the control group, students in the intervention group showed higher satisfaction for vegetables (p=0.003). Specifically, the children in the intervention group showed higher satisfaction scores for romaine lettuce (p<0.001), peppers (p<0.001), and spinach (p=0.017). There were no significant findings for sex or school. Conclusions: This school garden project favorably influenced students' knowledge and attitudes concerning vegetables as well as their vegetable consumption. Implications for Policy, Delivery or Practice: This work underscores the critical role classroom instruction can play in the armamentaria to combat obesity and overweight. Nutrition education can be more effectively integrated into existing science curricula. Likewise, gardening can occur in the setting of physical education and even the related arts. Further, this work implies the need for development of standards based curricula materials and teacher training in the areas of gardening and nutrition. Clearly, adequate funding must be in place to support these efforts. Funding Source(s): Local Foundation Poster Number: 127 Reasons for Critical Care Inter-facility Transports of Neonatal and Pediatric Patients to a Tertiary Care Academic Children’s Hospital Presented by: Ranna Rozenfeld, M.D., Associate Professor of Pediatrics, Pediatric Critical Care Medicine, Children's Memorial Hospital/Feinberg School of Medicine, 2300 Children's Plaza, Box #73, Chicago, IL 60614; Phone: (773) 880-4891; Email: rrozenfeld@northwestern.edu Co-authors: Donna Woods, EdM, Ph.D.; Sally Reynolds, M.D.; Michael Kelleher, M.D.; Paul Leonardi, Ph.D.; Borko Jovanovic, Ph.D. Research Objective: To assess the reasons for inter-facility transfer of pediatric patients to an urban tertiary/quaternary care academic pediatric medical center. Study Design: All inter-facility transports brought to the facility, including critical care transports by dedicated transport teams were reviewed for medical diagnosis, day, time, month, and location of accepting unit (ED, PICU, NICU, ward). Categories of reason for transport diagnoses were independently assessed by 5 physicians representing differing pediatric specialties involved in transports (ED, critical care, neonatology, general pediatrics). The transport data was then classified into broad categories of diagnosis. Frequencies were estimated. Population Studied: All pediatric transports from September 2002 through January 2008 were included - premature infants, neonates, infants, children and adolescents. Principal Findings: There were 8346 transports of which return transports (397) and transports out of the institution for radiation therapy (177) were excluded. There were 7,772 transports remaining for inclusion. The reasons for transfer included 134 diagnoses with at least 3 transports (6933). For the remainder of transports (839) the reason occurred in <3 transports. Of the 7,772 patient transfers, the most frequent diagnoses included: respiratory distress (861), seizures (652), congenital heart disease (CHD) (403), prematurity (242), diabetic ketoacidosis (226), and prematurity with respiratory distress syndrome (213). Of the diagnoses listed as CHD, 279 were listed as CHD, 22 coarctation of the aorta, 20 tetrology of fallot, 17 transposition of the great vessels, 9 aortic stenosis, 3 hypoplastic right heart, 24 hypoplastic left heart, 12 pulmonary stenosis, 8 total anamolous pulmonary venous return and 9 ventricular septal defect. Reasons for transport were classified as follows: respiratory (23.8%), neurologic (12.0%), pediatric surgery (10.3%), neonatal (10.3%), cardiac surgery (7.4%), general pediatric conditions (7.0%), trauma (5.8%), acute life threatening events (4.0%), neurological surgery (4.0%), otolaryngology (ENT) (3.7%), endocrine/allergy (3.6%), cardiology (3.2%), gastroenterology (2.6%), hematology/oncology (1.4%), and kidney/urology (1%). The month of January had the highest volume of transfers and transfers were most frequent on the first day of each month. Transports also occurred most frequently on Wednesdays and Fridays. The most frequent time of day for transport was consistently between 3PM and 12AM. Conclusions: This study provides details of the pattern of pediatric emergency transports to an urban pediatric center. Over 50% of the transfers were related to only 4 of the reason for transfer categories: respiratory (23.8%), neurologic (12.0%), pediatric surgery (10.3%), neonatal (10.3%). Implications for Policy, Delivery or Practice: The results of this study could be useful for institutional and regional planning and resource allocation. Understanding the timing of volume and flow of transports can enable the transport services to be adequately staffed for the potential transport calls. Understanding the most frequent types of transports can assist with development of appropriate staffing of the transport team, the appropriate units in the hospital, as well as having the appropriate consultants available to care for these patients. Funding Source(s): AHRQ Poster Number: 128 Racial/Ethnic Variation in the Relationship Between Adolescent Health Status and the Intention to Attend College Presented by: Tetine Sentell, Ph.D., Assisant Professor, Office of Public Health Studies, University of Hawaii at Manoa, 1960 East West Road, Biomed D104G, Honolulu, HI 96822; Phone: (808) 956-5781; Email: tsentell@hawaii.edu Research Objective: Educational attainment is a key predictor of adult health status, yet decisions to pursue higher education are typically made in adolescence. The relationship between adolescent health status and college intention is not fully understood. If poorer adolescent health status is associated with lower expectations for college education, this will inform future interventions to improve both adolescent and adult health. Understanding variation in this relationship by race/ethnicity will help target efforts to decrease health disparities. Study Design: Data were used from the 3,971 adolescents ages 12-17 who completed the 2003 California Health Interview Survey and were currently attending school. Participants selfreporting plans to attend college/university were compared to those reporting other plans (e.g., job, military). Self-reported health status was measured as (1) poor/fair, (2) good, and (3) very good/excellent. Control variables in multivariate logistic models included age, poverty, gender, race/ethnicity, and parental education. Models were performed with the entire sample, and for each race/ethnicity separately to identify variation in the relationship of adolescent health to education intention. Population Studied: Participants were diverse: 34% Hispanic, 9% Black, 10% Asian, 42% White, and 5% other. Average age was 14; 49% were female. Nineteen percent did not plan to attend college; this varied significantly by race/ethnicity from 22% of Hispanics (highest) to 11% of Asians (lowest) (Chi2=33.04;p=.01). Ten percent reported poor/fair health, 30% good health, and 60% very good/excellent health. Principal Findings: In unadjusted analyses, 27% of adolescents with poor/fair health, 23% in good health, and 17% in poor health did not plan to attend college. In multivariate models, both adolescents in poor/fair health (OR 0.50; 95%CI: 0.32-0.80) and those in good health (OR 0.63; 95%CI: 0.48-0.82) were significantly less likely to plan on college compared to those in very good/excellent health. When racial/ethnic groups were considered separately, Asian adolescents in fair/poor health were dramatically less likely to plan on college (OR 0.09; 95%CI: 0.14-0.62) compared to Asians in very good/excellent health. White adolescents in good health were significantly less likely to plan on college (OR .53; 95%CI: 0.39-.72) compared to those in very good/excellent health. No significant associations between health and college intention were seen in African American or Hispanic subpopulations. Conclusions: Nearly 1 in 5 adolescents did not plan to attend college, a key predictor of adult health status. Adolescents who self-reported either fair/poor or good health were significantly less likely to plan on college compared to those in very good/excellent health. Important variation was found in the relationship of adolescent health to college intention by race/ethnicity. Implications for Policy, Delivery or Practice: Promotion of adolescent health is important for teens' immediate quality of life, but also represents a critical contribution to their future health and health-related opportunities. This study suggests that investment in adolescent health to promote higher educational attainment may be a key pathway by which child health promotion efforts could lead to better adult health opportunities. However, this study also suggests that health is not the critical factor limiting Hispanic and African American college intentions, which should be considered in efforts to decrease health disparities. Poster Number: 129 Recent Trends in Sugar-Sweetened Beverage Consumption and Childhood Obesity in California Presented by: Lu Shi, Ph.D., Senior Analyst, Health Services, University of California, Los Angeles, 3271 Sawtelle Boulevard, Apartment 106, Los Angeles, CA 90066; Phone: (315) 395-8025; Email: lushi.pku@gmail.com Co-authors: Jeroen Van Meijgaard, M.A. Research Objective: The prevalence of overweight among US children and adolescents appears to be leveling off. Few studies have looked at recent changes among risk factors that might help explain these encouraging developments in obesity trends. We present an analysis of recent data from the California Health Interview Survey (CHIS) that examines trends in childhood and adolescent obesity as well as trends in sugar-sweetened beverage (SSB) consumption, and discuss the possible associations between these trends. Study Design: We compared three separate crosssectional samples (2003, 2005 and 2007) from biennial California Health Interview Survey (CHIS) for three age groups, age 2-5, age 6-11, and age 12-17. We estimate the crude prevalence of high SSB consumption (defined as having more than one soda or other sweetened drinks during the previous day) for each age group in each wave of CHIS. Two measures of obesity were used: weightfor-age (WTA) at or above the 95th percentile on national growth charts for children aged 2 to 11, and Body Mass Index (BMI) for age at or above the 95th percentile on national growth charts for adolescents aged 12 to 17. Logistic regression analysis is used to estimate adjusted odds ratios of consuming high levels of sugar-sweetened drinks in 2005 and 2007 compared to the baseline year of 2003. Population Studied: Children and adolescents living in California. Principal Findings: From 2003 to 2007, each age group experienced a substantial decline in high sugar-sweetened drink consumption (16.4% to 5.0% for age 2-5, p<.001; 22.5% to 9.9% for age 611, p<.001; 35.7% to 25.7% for age 12-17, p<.001). Declines in the prevalence of children’s obesity were significant among children age 2-5 (p<.001) and age 6-11 (p <.05) but not among adolescents (p=.42). Children and teenagers surveyed in 2005 and 2007 were significantly less likely than those surveyed in 2003 to have consumed more than one SSB in the previous day after adjusting for gender, age, race/ethnicity, poverty level and parental education. Conclusions: This study shows a downward trend in the consumption of SSB among California children and adolescents, a trend that is independent of demographic and economic trends in the state. While there has been no significant change in adolescent obesity prevalence, the substantial decline in both childhood obesity and adolescent SSB consumption has the potential to lead to a decline in obesity prevalence among adolescents in future years. However, there is insufficient information in the CHIS survey to determine whether a reduction in SSB consumption can be attributed to the legislation of California's SB 677, which put restrictions on soda sales on school properties. Implications for Policy, Delivery or Practice: Policy actions on SSB consumption might have had relatively rapid impacts on the prevalence of health risk factors in the population. Further research is needed to examine the contribution of declining SSB consumption on the leveling off of obesity trends and the extent to which these declines are attributable to new policies and programs. Particularly valuable will be comparisons between states, comparisons with national data and continued monitoring of trends in California. Poster Number: 130 Racial Disparities in the Incidence of Adverse Events for Hospitalized Pediatric Patients Presented by: Richard Smith, Ph.D., Associate Professor, College of Business, University of South Florida St. Petersburg, 140 Seventh Avenue South, COB 348, Saint Petersburg, FL 33701; Phone: (727) 873-4943; Email: smithrb@mail.usf.edu Co-authors: Lisa Simpson, M.B., B.Ch., M.P.H., F.A.A.P.; Gerry Fairbrother, Ph.D. Research Objective: Racial disparities in health care are well documented phenomena, although questions persist about their cause. Increasingly, the literature cites quality differences in facilities where white and nonwhite patients receive care as opposed to differences in treatment by providers or hospitals. In the area of children’s health, AcevedoGarcia and colleagues (2008) suggest various pathways in which children’s health is adversely affected by residential racial segregation, including segregated health care settings and the associated disparity in quality of treatment. The objective of this study is to determine whether hospitals that largely treat nonwhite patients provide a lower quality of care to children than other hospitals. Much attention has been given to the incidence of preventable medical errors in hospitals in the wake of two alarming reports from the Institute of Medicine, To Err is Human and Crossing the Quality Chasm. Thus, this study uses recently developed, and pediatric-specific, patient-safety indicators to examine the incidence of adverse events for all non-newborn inpatients up to age 17. Study Design: A multivariate logistic regression, at the patient-discharge level, is used to estimate the probability a pediatric patient experiences a potentially preventable adverse event, controlling for patient and hospital characteristics. The key explanatory variable characterizes the hospital according to the proportion of nonwhite pediatric discharges. Population Studied: The sample consists of over 1 million discharges of children, age 0 to 17, but excluding normal newborns, who met criteria for being at risk of experiencing at least one of 8 preventable adverse events. Data come from the 2007 Nationwide Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ). The 2007 NIS contains complete inpatient discharge information for over 1,000 community hospitals in 40 states. Weights are provided to allow for setting the value of sample measures relative to national estimates. Principal Findings: Preliminary results indicate there is a small but statistically insignificant increase in the odds of an adverse event for children in hospitals with a higher proportion of nonwhite discharges. On the other hand, there is a large and significant decrease (OR = 0.492) in the odds of an adverse event for children who are in hospitals with the highest relative to the lowest proportion of Medicaid patients. Conclusions: Based on these results, racial disparities in health outcomes for children do not seem to stem from differences in the quality of care between hospitals that treat a high proportion of nonwhite patients and other hospitals. Implications for Policy, Delivery or Practice: These findings suggest that policymakers need to look to other pathways, perhaps even outside the health care setting (e.g. education, environment) to explain racial disparities in the health outcome of children. Funding Source(s): HRSA, Maternal and Child Health Bureau Poster Number: 131 Geographic Disparities in Service Utilization by Medicaid and CHIP-Eligible Children with Autism Presented by: Angela Snyder, Ph.D., M.P.H., Senior Research Associate, Georgia Health Policy Center, Georgia State University, 14 Marietta Street, Suite 221, Atlanta, GA 30303; Phone: (404) 413-0285; Email: angiesnyder@gsu.edu Co-authors: Daniel Crimmins, Ph.D.; Mei Zhou, M.S. Research Objective: To compare service utilization patterns of children diagnosed with autism living in urban and rural areas of Georgia. Study Design: Retrospective cross-sectional study comparing children diagnosed with autism living in rural and urban areas of Georgia on both the types of providers accessed and the frequency and costs of health services utilized. County-level Rural-Urban Continuum Codes (RUCC) are used to define rural and urban residence for each child and two measures of provider supply are used as independent variables. Control variables are categorized according to the theoretical framework for the study of healthcare access first described by Aday and Andersen (1974). Predisposing factors include the child’s race/ethnicity and gender, enabling factors include eligibility type and whether or not the child was continuously enrolled in public insurance for the full year. Age group is used as a measure of need because previous research has shown that age is associated with the breadth of services children use. Multivariate methods including both logistic and ordinary least squares regression will be used to study specific utilization patterns that show a geographic disparity in the descriptive and bivariate analyses. Population Studied: The study sample includes 5,682 children who were younger than 21 years of age and received a primary or secondary diagnosis for autistic disorder associated with a Medicaid or CHIP reimbursed claim in calendar year 2005 in Georgia. This sample represents 0.47% of the 1.2 million Medicaid and CHIP enrolled children in that year. Principal Findings: Descriptive results suggest that children living in rural areas are somewhat similar on the predisposing characteristics, with black children less likely to live in rural areas. There is a difference in the enabling characteristics regarding program eligibility: more disabled children live in rural areas and more children on Medicaid waiver programs, with higher incomes, live in urban areas. Need as measured by age group is similar between groups. Similar to previous research, children living in urban areas are more likely to visit a pediatrician, while children living in rural areas are more likely to visit a family practitioner. Surprisingly, children in rural areas were slightly more likely to visit a physician specialist. More predictably, children in urban areas are more likely to visit a therapist. In regards to expenditures, children residing in rural areas utilize more pharmacy services while children residing in urban areas utilize more outpatient services. Multivariate results are in process and will be completed by June 2010. Implications for Policy, Delivery or Practice: Because this study examines community and delivery system factors that may create geographic disparities in access, findings may suggest policy interventions to decrease barriers and improve the systems of care for children with special health care needs including autism. Funding Source(s): Pending funding from HRSA Poster Number: 132 Is Parent Health Literacy Associated with ParentReported Quality of Life among Children with Attention Deficit Hyperactivity Disorder? Presented by: Sara Toomey, M.D., M.Phil., M.P.H., Instructor, Division of General Pediatrics, Children's Hospital Boston, 21 Autumn Street, 2nd Floor, Boston, MA 02215; Phone: (857) 218-4076; Email: sara.toomey@childrens.harvard.edu Co-authors: Janine Molino, M.S.; Eugenia Chan, M.D., M.P.H.; Chao-Yu Gao, Ph.D.; Stephen Porter, M.D., M.P.H. Research Objective: The aim of our study was to investigate the relationship between parent health literacy and health-related quality of life (HRQL) in a community-based sample of children with ADHD. Study Design: We conducted a cross-sectional analysis of parents of children with ADHD. Parents reported on ADHD symptoms, current prescribed ADHD medications and side effects, and HRQL. The normalized Psychosocial Summary Score (range 0-100) from the 50-item Child Health Questionnaire-Parent Form (CHQ50) was the primary HRQL outcome. The primary independent variable was parent score on the Test of Functional Health Literacy in Adults (TOHFLA). Multivariate linear regression analysis adjusted for disease control status, side effects, parent race/ethnicity, parent gender, and parent level of education. Scaled HRQL effect sizes were calculated using the adjusted beta-coefficients. A 5-point difference was considered to be a clinically meaningful change in HRQL for the CHQ50. Population Studied: We analyzed data collected from parents of children with ADHD from diverse communities in greater Boston who participated in a clinical trial on information-sharing in ADHD. Of 271 parents screened, 194/271 (72%) were eligible and, of those, 182/194 (94%) were enrolled. Two parents were excluded post-hoc. We analyzed 177 parents with complete data. 94% of parents were female and 50% were non-White. 27% had a high school education or less. Principal Findings: The parents were largely literate with only 6% scoring inadequate/marginal on the TOFHLA. Mean HRQL was 33.9 (SD 12.5) for parents with inadequate/marginal literacy compared to 37.7 (SD 12.0) for parents with adequate literacy. In multivariate analysis, parents with inadequate/marginal literacy had a clinically relevant lower HRQL although it did not reach statistical significance (expected difference in scaled HRQL 5.9, p=.12). Additional significant covariates included disease control (expected difference in scaled HRQL 14.4, p<.001) and presence of more than minimal side effects (expected difference in scaled HRQL 7.6, p<.001). No additional parent traits were associated with HRQL. Conclusions: Parent health literacy may be associated with HRQL for children with ADHD and demonstrates the strongest association with child HRQL among the parent traits studied. Implications for Policy, Delivery or Practice: Low health literacy is known to be associated with poor health outcomes and HRQL. Children with ADHD experience poorer HRQL relative to typical peers. If, as our study suggests, parent health literacy is associated with HRQL for children with ADHD, interventions targeting improvement in HRQL should consider addressing parent literacy in proposed strategies. Funding Source(s): National Library of Medicine Poster Number: 133 Adolescent Body Mass Index is Associated with an Increase in Medical Encounters for Musculoskeletal Injuries Presented by: Carolyn Valdez, Quality Improvement Associate, Patient Safety and Quality, Denver Health, 645 Acoma Street, Denver, CO 80204; Phone: (303) 436-5491; Email: Carolyn.Jagunich@dhha.org Lead Author: Greg P. Gutierrez, M.D. Co-authors: Simon J. Hambidge, M.D., Ph.D. Research Objective: There is limited data on the association between body mass index (BMI) and musculoskeletal (MSK) injury in children and adolescents. Most information is limited to questionnaires and chart reviews of cohorts of about 200 children. Our large urban vertically integrated health care system allows us to analyze a large cohort of individuals over the course of many years. We hypothesized that an increase in BMI would be associated with an increased risk of MSK injuries in our pediatric population. Study Design: Our study consisted of a retrospective chart review of pediatric patients with access to Denver Health’s community health care centers. We examined patients in terms of demographics, documentation of BMI data, history of injury, and comorbid conditions in order to examine this association. Population Studied: The cohort was narrowed down to 30,509 children ages 2-17 years old with 2 or more primary care visits from 2005 to 2008 in the Denver Health system and limited to patients with documented BMI data (or height and weight) in our records. Patients with a BMI under 10 or over 60 were excluded along with patients that had no recorded BMI data during the study period. Patients were grouped into BMI categories according to the national percentiles according to their age and gender. Patients with percentiles greater than or equal to 95% were classified as obese, and between 85-94% were classified as overweight. All others fell into the non-obese category. Principal Findings: Of the 30,509 children, 18% were obese; 15% were overweight; 67% were non obese; and 39% of the cohort had an Injury Related Medically Attended Event (IRMAE). The number of injuries per child ranged from 0 (70%) to 5+ (1%). 18% of the cohort had comorbid conditions. In bivariate analysis, higher BMI was associated with a greater population percentage of IRMAEs: nonobese 22%, overweight 25% and obese 27% (p<.0001). There were increased IRMAEs in patients with a comorbidity (P<.0001), with increasing age (P<.0001), and in males versus females (P<.0001). Multivariate analysis demonstrated an increasing trend for IRMAE with increasing weight: overweight children were more likely to be injured than non-obese (OR 1.090, 95% CI 1.019-1.161, p<0.01) and obese children were more likely to be injured than non-obese (OR 1.102, 95% CI 1.025-1.185, p< 0.01). Conclusions: This is the first study in American children to demonstrate an increased risk for musculoskeletal injury requiring a medical visit with increased BMI. Furthermore, the risk appears to increase from non-obese to overweight to obese. Given that obese children have been shown to be less physically active than their non-obese peers, our results suggest that children with higher BMI are at significantly increased injury risk when they are active. Possible reasons include relative muscle weakness, poor proprioception and deconditioning. Implications for Policy, Delivery or Practice: The findings from this study will be taken into consideration by our institution while planning interventions related to obesity in the pediatric setting. Our findings suggest that, in addition to counseling families about the importance of physical activity, providers and parents should be aware of the increased risk for injury in obese children. Poster Number: 134 Rural/Urban, Racial/Ethnic, and Socioeconomic Disparities in Lifestyle Counseling for Overweight and Obese Adolescents Presented by: Amy Wallace, M.D., M.P.H., Senior Scholar, Veterans Rural Health Resource Center-Eastern Region, Veterans Affairs Medical Center, 215 N. Main Street, WRJ, VT 05009; Phone: (802) 295-9363 ext. 6072; Email: aew@dartmouth.edu Research Objective: Overweight and obesity are associated with serious health and social consequences, and are steadily increasing among rural, minority, and socioeconomically disadvantaged populations. Encouraging lifestyle changes: diet, exercise, and weight loss, should be the initial approach for providers treating adolescents with these issues. We examined the likelihood of lifestyle counseling among patients age 13 to 21 years across gender, rural/urban locales, racial/ethnic groups, median ZIP Code income, educational and area poverty levels during preventive and primary care appointments. Study Design: We used the 2006 and 2007 National Ambulatory Medical Care Survey database in a cross-sectional study design to evaluate the likelihood of lifestyle counseling for overweight and obese adolescents during preventive and primary care visits. We examined prevalence of overweight and obesity and calculated odds ratios to determine the relative likelihood of lifestyle counseling across residence locale, demographic, and socioeconomic characteristics. Population Studied: From the 2006 and 2007 National Ambulatory Medical Care Survey database, we extracted 7,714 records representing 262 million preventive and primary care visits for non-pregnant patients age 13 to 21 years with documented BMI>25 or diagnosis of obesity. Among these, 3,248 records representing approximately 109 million patients received lifestyle counseling. Principal Findings: The overall prevalence of overweight or obesity among 13 to 21 year olds seen in outpatient visits was not statistically different across gender (21% of females and 20% of males) or residence locale (21% for urban and suburban patients, 20% for rural patients). Providers offered lifestyle counseling during only 33% of preventive and primary care visits for overweight and obese adolescents. Across all demographic groups, providers were 91% more likely to counsel overweight urban (p<.0001) and 31% more likely to counsel suburban adolescents compared to rural adolescents (p=.009). Odds ratio for counseling for urban compared to suburban and rural adolescents remained highly significant after adjustment for other demographic and socioeconomic variables. Other factors associated with greater likelihood of lifestyle counseling were male gender (OR 1.45, p<.0001), Asian race (OR=1.52 , p=.003 compared to non-Hispanic whites, all other race/ethnic comparisons nonsignificant), private insurance payer (OR=1.28, p<.0001 compared to other payer types). Percent community poverty, median community income and community educational level did not significant predict for lifestyle counseling. Conclusions: Overall, providers are neglecting lifestyle counseling for overweight and obese adolescents during preventive and primary care visits. When provided, demographic groups with high obesity prevalence: rural patients, females, Blacks and Hispanics are less likely to receive counseling those groups for whom obesity is less prevalent (urban and suburban adolescents, males, and Asians). Community level economic variables that describe relative disadvantage: lower median community income and education level, and higher percent poverty, did not predict lower likelihood of counseling; however, lack of private insurance was significantly associated with lower likelihood of counseling. Implications for Policy, Delivery or Practice: While providers should provide counseling aimed at nutrition, exercise, and weight loss to all overweight adolescents during routine preventive care visits, they should be especially attentive to population segments with higher obesity prevalence. Early adoption of healthy lifestyle habits may prevent a lifetime of obesity-related health problems. Funding Source(s): VA Poster Number: 135 Raising Awareness of Youth Healthy Eating and Physical Activity Behaviors: Short-Term Effectiveness of a Social Marketing Campaign Presented by: Hongmei Wang, Ph.D., Assistant Professor, Health Services Research and Administration, College of Public Health, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Phone: (402) 559-9413; Email: hongmeiwang@unmc.edu Co-authors: Liyan Xu, M.S.; Anne Skinner, B.S.; Molly O'Dell, M.D. Research Objective: Changing the eating and physical activity behaviors is considered the very first step to tackle the youth obesity epidemic. Behavior change in turn is based on the improved knowledge of youth on the important health messages. Across the nation, mass media campaign is one of the mostly commonly used tools to covey the health messages to youth. It is important for the policy makers to understand the effectiveness of a social marketing campaign in delivering health messages and changing behaviors. This study aims to measure the effectiveness of a local social marketing campaign promoting five recommendations on dietary and physical activity behaviors to youth. Study Design: The social marketing campaign is funded locally and carried out by an advertising company using mass media including TV, radio, billboards, and website. The five principle recommendations for youth are: 5 servings of fruits and vegetables; 4 glasses of water; 3 servings of low-fat dairy; 2 or less hours of screen time, and 1 or more hours of physical activity a day. The researchers utilize a quasi-experiment design to measure the campaign effectiveness. A phone survey was conducted after the campaign is completed in September 2009 to collect awareness, knowledge, and behavior information of the targeted audience. Knowledge and behavior changes of respondents exposed to the campaign were then compared to those of respondents not aware of the campaign. Demographic information was also compared between these two groups to ensure the group similarity. T-test and Chi-squared test were used to examine the significance of the results. Population Studied: A random sample was selected from all households in local community with children aged 5 to 18 years old and with a fixed phone number listed. A total of 1,030 households were surveyed. For households with youth aged 12 to 18 years, one youth was randomly selected to complete the survey. The total sample size of the youth was 504, with a response rate of 59.6%. For households with children aged 5 to 11 years, a parent or guardian was asked to answer knowledge questions and behavioral questions of a randomly chosen child in the household. 526 parents were included and the response rate of this group was 78.1%. Principal Findings: For both parents and youth surveyed, those who were aware of the campaign are more likely to reported correct responses to the knowledge questions regarding the five recommendations than those not aware of the campaign. Significant differences in behaviors were also found between those who were aware of the campaign and those not aware of the campaign. However, the significance in behavior changes was not consistent across the five recommendations. Parents who were aware of the campaign were even found less likely to report that their child ate five servings of fruits and vegetables and less than two hours of screen time a day. Conclusions: Social marketing campaign targeting youth can be effective in delivering health messages to increase knowledge of youth in a short term. However, additional in-depth education and health promotion efforts may be necessary for children to understand the messages and follow the recommendations to change their behaviors in the long run. Poster Number: 136 Prescription Antihypertensive Drug Use in Children Presented by: W. Pete Welch, Ph.D., Senior Consultant, Federal Health, The Lewin Group, 3130 Fairview Park Drive, Sutie 800, Falls Church, VA 22042; Phone: (703) 269-5605; Email: Pete.Welch@Lewin.com Co-authors: Wenya Yang, M.A., M.P.A.; Joseph Flynn, M.D., M.S.; Perdita Taylor-Zapata, M.D. Research Objective: Legislative initiatives intended to improve pediatric labeling of prescription medications have had significant impact on pediatric drug development. In 1997, the Food and Drug Administration Modernization Act (FDAMA) provided incentives for companies to voluntarily test drugs in pediatric populations in exchange for 6 additional months of market exclusivity. In 2002, the Best Pharmaceuticals for Children Act (BPCA) created a mechanism for studies of drugs without patent protection. In 2003, the Pediatric Research Equity Act (PREA) required that pharmaceutical companies conduct studies in pediatric populations of any medication likely to be used in children. These developments have resulted in a proliferation of pediatric clinical trials and updating of pediatric labeling. In this study we sought to determine whether anti-hypertensive drugs prescribed for use in children are actually indicated for pediatric use and have FDA-approved pediatric labeling. Study Design: Using the database of a large commercial insurer with approximately 20 million covered lives, we defined our study population as children who were continuously eligible for medical and pharmacy benefits in the calendar year 2008. We identified pediatric patients (age=18) with hypertension using Episode Treatment Groups (ETGs), a commercial software package that organizes claims into episodes of care by combining information from diagnosis, procedure codes, and drug NDC codes from patient claims. Pharmacy claims of the patients receiving antihypertensive drugs were then extracted to calculate drug user rate and days of supply by therapeutic class and drug agent. The prescribed drugs were categorized based on the availability of pediatric labeling (as indicated either in the FDA-approved label or in the 2004 Fourth Report by the National High Blood Pressure in Children and Adolescents Working Group and an indication for pediatric use. Population Studied: 2,912 pediatric patients with primary (n=2,379) and secondary (n=533) hypertension. Principal Findings: 685 (22%) of primary hypertensive patients were treated with any antihypertensive drugs, as were 384 (72%) secondary hypertensive patients. Of the 1,069 patients treated, 87% were treated with labeled drugs that were indicated (73% of supply days), 32% were treated with non-labeled drugs that were indicated (23% of supply days), and 3% were treated with a labeled drug that was not indicated (2% of supply days). Because some patients were treated with multiple drugs, these percentages sum to more than 100%. 5% of patients (2% of supply days) could not be categorized. Additionally, at least 12% of pediatric patients with hypertension received treatment with agents whose label information predated FDAMA. Conclusions: Among hypertensive pediatric patients receiving any type of antihypertensive medications, the vast majority were being treated with drugs that are indicated for pediatric use. However, a substantial proportion of children with hypertension are being treated with drugs that lack FDA-approved pediatric labeling, or whose labeling predates the recent legislative initiatives. Implications for Policy, Delivery or Practice: While recent legislative efforts have greatly improved the availability of pediatric labeling for antihypertensive medications, our finding that many non-labeled medications are still widely used suggests that greater efforts are needed to fulfill the mandate of FDAMA, BPCA and other legislative initiatives to provide safe and effective medications for children. Funding Source(s): National Institute for Child Health and Human Development Poster Number: 137 Economic Perspectives on Child Obesity Presented by: Frederick Zimmerman, Ph.D., Chair, Department of Health Services, University of California, Los Angeles, Box 951772, Los Angeles, CA 90095-1772; Phone: (310) 825-1971; Email: fredzimmerman@ucla.edu Research Objective: Child Obesity is high and rising, and represents one of the most significant public health threats of our era. Considerable research has explored the sources of socioeconomic disparities in childhood obesity and diet. Economists have made a modest contribution to this discussion to date, eM.P.H.asizing the role of food subsidies in lowering prices for calorie-dense foods, and the role of labor-saving devices in reducing the time costs of food preparation. This analysis critically examines three theoretical traditions within economics—neo-classical economics, behavioral economics, and institutional economics—for their value in explaining and contributing solutions to the childhood obesity epidemic. Study Design: For each of the three strands of economics, a formal model of diet choice is developed, and testable implications of the model are derived. In the neo-classical model, diet is an individual, rational choice by fully-informed parents. Preferences are assumed to be parent-specific and exogenous, and prices are assumed to be exogenous, but subject to change by tax policy. In the behavioral economics model, diet choices are individual, but are strongly influenced by availability, by hyperbolic discounting, and by physiological cues such as portion size. Prices, availability, and portion size are assumed to be modifiable by policy. In the institutional model, neo-classical and behavioral models are embedded in a particular cultural-economic structure that shapes both preferences and choice sets. Prices, availability, and portion size are modifiable by policy, but so are demand shifters, such as advertising, industrial structure, and the ways in which public discussions over obesity are framed. Principal Findings: Little empirical support exists for the neo-classical model of rational, informed decision-making in its strict representative agent form. Considerable evidence exists to support a behavioral economics model of diet choice. However, behavioral factors are useful in explaining the aggregate trend of diet choice, they are not very good at explaining socio-economic disparities in diet outcomes. The institutional model predicts increasing obesity when the effective price of advertising falls, as it has over the past 3 decades, and that children of parents with the lowest wages are the most likely to be exposed to the obesogenic effects of television advertising. Implications for Policy, Delivery or Practice: The neo-classical model suggests that a tax on obesogenic foods, such as sugar-sweetened beverages, will disincentivize high-caloric diets. This policy is likely to fail because the price elasticity of sugar-sweetened beverages is low, implying that a very large tax—in excess of 50% of the purchase price—will be required to have any meaningful effect on demand. The behavioral economics model suggests solutions such as making fruits and vegetables more prominently available in the school lunch room. Such policies hold considerable promise, but may fail if they are not broadened to include the whole food environment. The institutional model suggests that poor diet choices are largely the result of heavy advertising. While this problem will not be easy to redress, it is the only way to achieve meaningful impact on the epidemic in child obesity. Poster Number: 138 Specialty Referral Communication and Completion in the Community Health Center Setting Presented by: Katharine Zuckerman, M.D., M.P.H., Assistant Professor, Pediatrics, Division of General Pediatrics and Child and Adolescent Health Measurement Initiative, Oregon Health and Science University, 707 SW Gaines Road, Mail Code CDRC-P, Portland, OR 97239; Phone: (503) 494-6726; Email: zuckerma@ohsu.edu Co-authors: Kerrie Nelson, Ph.D.; Tara Bryant, B.A.; James Perrin, M.D.; Karen Donelan, Sc.D. Research Objective: Parent and provider disagreement about a child’s care at the time of specialty referral may lead to incomplete referral (not attending a specialty visit when referred by a primary care provider). This project’s objectives were (1) to assess the overall rate of specialty referral completion among children referred by pediatric community health center providers for specialty care at an affiliated tertiary care center (2) to assess parent-provider concordance in views of seriousness of the referred child’s health problem, necessity of specialty referral, and parental understanding of the referral, and (3) to assess whether parent and provider ratings of seriousness of problem, necessity of referral, and parental understanding were associated with referral completion. Study Design: Two months after referral to specialty care, parents and primary care providers were contacted to complete a survey which rated seriousness of problem, necessity of referral, and parental understanding on a 4-part rating scale (“definitely yes”-“definitely no”). Parents were surveyed by telephone, and providers completed self-administered surveys attached to a copy of their clinic note from the referral visit. Using electronic health records, we assessed whether specialist visits were completed or missed. We used Pearson correlation coefficients [PCC] to summarize parent-provider concordance in seriousness of problem, necessity of referral, and parent understanding. We applied logistic regression to test the associations of parent and provider ratings for each variable with referral completion. Population Studied: Parents of 501 children seeking care from 28 pediatric primary care providers in two community health centers located in disadvantaged Massachusetts communities. All children were referred for pediatric specialty consultation at an affiliated tertiary care center. Principal Findings: 27% of specialty referrals were not completed. Parents and providers agreed in ratings of seriousness of the problem 33.3% of the time, in ratings of the necessity of referral 49.2% of the time, and in ratings of parental understanding of referral 62.1% of the time. Parent-provider concordance on rankings was low for all measures (PCC 0.10 for seriousness of problem, -0.09 for necessity of referral, and -0.02 for parent understanding of referral). On multivariate analysis, significant factors associated with incomplete referral included lower parent rating of necessity of referral (Odds Ratio [OR] of referral completion 0.14 for “somewhat no” vs. “definitely yes”; confidence interval [CI] 0.12-0.66) and lower provider rating of seriousness of problem (OR 0.41 for “somewhat no” vs. “definitely yes”; CI 0.17-0.97). The survey response rate was 70% for parent surveys for 98% provider surveys. Conclusions: Nearly 3 in 10 pediatric specialty referrals were not completed. Parents and providers frequently disagreed about the necessity of specialty referral and the seriousness of referred children’s health problems. When parents thought a problem was less serious, and when providers thought a referral was less necessary, the referral was less likely to be completed. Implications for Policy, Delivery or Practice: These data suggest that there is significant room for improvement in parent-provider specialty referral communications, and that low-quality communication may be associated with incomplete referral. To decrease incomplete referral rates, providers should take a family-centered approach to referral decision-making and provide additional support to families that feel referral is less necessary. Funding Source(s): CRICO Risk Management Foundation Poster Number: 139 Redeveloping Closed Military Installations with a Health in All Policies Approach Presented by: Holly Avey, Ph.D., M.P.H., Senior Research Associate, Georgia Health Policy Center, Georgia State University, 14 Marietta Street, Suite 221, Atlanta, GA 30303; Phone: (404) 413-0291; Email: havey@gsu.edu Co-authors: Heather Devlin, M.A.; Naima Wong, Ph.D., M.P.H.; Jane Branscomb, B.E.; Karen Minyard, Ph.D.; Karen Cheung Research Objective: Health in All Policies (HiAP) is a strategy that strengthens the link between health and other policies, creating an environment that supports people’s ability to lead healthy lives. HiAP addresses health across sectors, including housing, transportation, education, employment, land use, environment and agriculture. Incorporating health-supporting policies in all areas of community development can address the key determinants of health equity. Fort McPherson is an Army installation in Georgia that set to close in 2011 as part of the Department of Defense’s Base Realignment and Closure (BRAC) program. The vacated military property offers Metro Atlanta its largest single redevelopment opportunity in many years, with profound economic and health implications for new residents, neighboring communities and the region. The Georgia Health Policy Center and Centers for Disease Control and Prevention (CDC) are collaborating with McPherson Local Redevelopment Authority (LRA) and other stakeholders to bring a Health in All Policies perspective to BRAC redevelopment activities at Fort McPherson. The research objective is to use Fort McPherson as case study and work with national, state and local stakeholders to operationalize the concept of Health in All Policies and create a framework for incorporating health into future base closures and other large-scale redevelopments. Study Design: Up to 20 semi-structured key informant interviews will be conducted with federal, state, and community stakeholders to understand their diverse perspectives and needs. In keeping with the exploratory and qualitative nature of this study, key informants will be identified using a snowball sampling technique in which individuals refer those they know, who in turn refer those they know, and so on. Initial informants will be identified with the assistance of colleagues. Interview categories will include federal stakeholders to understand the BRAC process and authority structure, and community and state leaders to understand the policy environment. Based on the knowledge gained from key informant interviews, stakeholders will be mapped with respect to power and influence. Structured opportunities will be designed, using principles from whole scale system change, for community, state, and federal stakeholders to mutually explore health-promoting development policies. A Health in All Policies framework will be developed using results and insights from these exploratory meetings. Population Studied: BRAC stakeholders and decision-makers. Principal Findings: Base closure is a complex and highly prescribed process that takes years to complete and redevelopment may span decades and yet there are a limited number of opportunities to interject a Health in All Policies approach. These include the design guidelines, zoning stipulations and the developer’s agreement. Conclusions: By incorporating health into the policy development process across sectors and at multiple levels, we can begin to address the key determinants of health and health equity with a more systematic and holistic approach. Implications for Policy, Delivery or Practice: The redevelopment of Fort McPherson presents a unique opportunity to demonstrate the impact on the health and well-being of residents when a community is designed with a Health in all Policies approach. Findings will inform a model that could be used to incorporate health-promoting policies in other base closures and other large-scale redevelopments such as automobile manufacturing plants. Funding Source(s): CDC, through a cooperative agreement with the National Network for Public Health Institutes Poster Number: 143 Does Loss of Safety Net Hospitals in a Community Disproportionately Affect Racial and Ethnic Minority Groups? Presented by: Gloria Bazzoli, Ph.D., Bon Secours Professor, Health Administration, Virginia Commonwealth University, P.O. Box 980203, Richmond, VA 23298-0203; Phone: (804) 8285223; Email: gbazzoli@vcu.edu Co-authors: Woolton Lee, Ph.D.; Hui-Min Hsieh, M.B.A.; Lee Rivers Mobley, Ph.D. Research Objective: Safety net hospitals (SNHs) are thought to play a critical role in the U.S. health system by providing health care services for vulnerable populations. SNHs also frequently offer a variety of social and outreach services, which could potentially reduce disparities among ethnic and racial minority groups. This may be especially true for minority individuals living near an SNH because they will have ready access to these facilitating services. Our study examined whether closure or ownership conversions of nearby SNHs had a disproportionate effect on uninsured and Medicaid patients, especially for non-Hispanic black and Hispanic individuals. Study Design: Hospital discharge data for the states of Arizona, California, Florida, and Wisconsin were examined from the early 1990s to 2003. Our primary access measure was distance traveled by patients to hospitals for inpatient care. Both closure and for-profit conversion represent events that reduce safety net resources available to nearby communities. Our analysis looked separately at five types of hospital admissions based on primary diagnosis: ambulatory care sensitive conditions, referral sensitive conditions, marker conditions, births, and mental health and substance abuse admissions. The first three types are commonly examined in studies of access to care, and the remaining two represent types of hospitalizations common among the uninsured and Medicaid populations. Population Studied: We examined patients treated in urban hospitals in the four study states. Patients were classified based on race/ethnicity and payer status. Based on our analysis of travel patterns to urban hospitals in each study state, we classified patients based on whether or not they lived near to SNHs that ultimately closed or converted to forprofit status by the ending year of the study. In addition, other patient characteristics that might affect patient travel patterns were controlled in multivariate models, including comorbidities, the emergent nature of the admission, hospital characteristics, health system characteristics, and neighborhood characteristics. Principal Findings: Generally, we found that uninsured, Medicaid, and Medicare patients experienced added travel for many types of hospital care in the ending year of our study relative to what was observed for privately insured patients. The uninsured and Medicaid effects were more common among non-Hispanic blacks and Hispanics than in white populations. Longer travel for Medicare patients was predominantly present among whites and Hispanics. However, these effects appear to be related to general health system changes and not associated with SNH closure or conversion per se. Conclusions: Our results suggest that access to inpatient care, as measured by distance traveled to obtain care, may have become more problematic for certain insurance types and for minority patients over time. However, these access problems appear to be related to general health system changes rather than proximity to changes in SNH structure and resources. Implications for Policy, Delivery or Practice: Our results suggest that SNHs are not a panacea to eliminating disparities across insurance or race/ethnicity groups. Policymakers likely need to look more broadly at systemic health system issues and changes over time to identify factors that have created and sustained health disparities. Funding Source(s): National Heart, Lung and Blood Institute Poster Number: 144 Variations in Specialty Care in Patients with Chronic Diseases: A Case of Primary-Specialty Disconnect or Patient Preference? Presented by: Jessica Bellinger, Ph.D., M.P.H., Postdoctoral Fellow, Institute for the Partnerships to Eliminate Health Disparities, University of South Carolina, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210; Phone: (803) 251-6317; Email: jbellinger@sc.edu Co-authors: Saundra Glover, Ph.D.; Edith Williams, Ph.D.; Rahnuma Hassan, M.H.A. Research Objective: Existing health disparities research typically explores patient levelcharacteristics and system-level characteristics, such as provider availability and characteristics. However, a model of patient-centered care includes aspects of shared care. Primary care serves as a complement for specialty services by providing a medical home with continuity of care while the expertise of specialists improve outcomes. The study purpose is to determine racial and ethnic variation in specialty care utilization by perceived health and chronic disease status. Study Design: The Commonwealth Fund’s 2006 Health Care Quality Survey is a nationallyrepresentative telephone survey of adults living in the United States measuring health care utilization and quality of care. Data include self-reported health status, patient preference and behaviors, and other measures. The survey has an adult sample of 3,535 respondents. A stratified minority sample design was employed to ensure a representative sample of minorities. Logistic regression and chi-square analysis were used in the analysis of the primary outcome, self-report of specialty care. SAS 9.2 was used to perform all analyses appropriately weighted for survey estimates. Population Studied: To reduce loss of information and account for missing data, respondents with missing values from relevant items were not included in our final sample (n=2475), whites (43%), African Americans (32%), and Others (25%). More African Americans reported poor health (23%) than whites (20%). African Americans reported more chronic diseases (hypertension, diabetes, heart disease) than other respondents (p<.0001). Principal Findings: African Americans were less likely to report specialty care than whites when controlling for age, income, and health insurance status (AOR=0.81; 95% CI 0.67, 0.99). Compared to the youngest respondents (18-44 years old), the oldest respondents were more likely to report specialty care (AOR=1.76; 1.35, 2.31). Respondents lacking health insurance were less likely to report specialty care use (AOR=0.42; 0.28, 0.61). Other negative predictors of specialty care were lack of prescriptive coverage with health insurance plan (AOR=0.59; 0.42, 0.85) and poor perceived health (AOR=1.74; 1.33, 2.23). African Americans were more likely to report at least one chronic disease than whites (AOR=1.66; 1.33, 2.08). Conclusions: Overall, perceived need (as measured by self-report of health), race/ethnicity, access, and age were predictors of both specialty care use and chronic disease status. Low income respondents were more likely to report specialty care use, which suggests that public health insurance programs increase appropriate access to care. Implications for Policy, Delivery or Practice: African Americans reported higher rates of chronic disease, indicating risk of poor health outcomes and a greater need for specialty care; however, African Americans were less likely to report specialty care use. Such findings represent an opportunity to work towards the elimination of health disparities. System-level barriers, such as the availability of providers (both primary and specialty), could positively impact racial and ethnic disparities given that lack of a usual source of care was a negative predictor of specialty care and chronic disease. However, this is not the complete solution in isolation. Over 90% of the African Americans in the sample reported a regular health care provider. This suggests a need for interventions targeting personlevel barriers, such as self-efficacy and chronic disease knowledge. Funding Source(s): National Center on Minority Health and Health Disparities (NCMHD) at the National Institutes of Health (NIH) Poster Number: 145 Disparities in Cervical Cancer Prevention and Control Practices, Knowledge, and Preferences among Women Living in the Southeastern United States Presented by: Jessica Bellinger, Ph.D., M.P.H., Postdoctoral Fellow, SC Rural Health Research Center, University of South Carolina, 220 Stoneridge Drive, Suite 204, Columbia, SC 29210; Phone: (803) 251-6317; Email: jbellinger@sc.edu Co-authors: Heather Brandt, Ph.D.; Jan Probst, Ph.D.; Saundra Glover, Ph.D. Research Objective: The introduction of the Pap test contributed to significant reductions in cervical cancer mortality. The introduction of the HPV vaccine may contribute to reductions. Effects of appropriate screening have not been distributed equally across groups, contributing to excess mortality and disparities. In South Carolina, AfricanAmerican women are more likely to die of cervical cancer than white women. Access, social determinants, and women’s knowledge and preferences for appropriate prevention and screening contribute to disparities. The objective of this study was to examine the effects of access, social determinants, and women’s knowledge and preferences on cervical cancer prevention and control practices. Study Design: Random-digit dial telephone interviews were used to collect data in a populationbased HPV survey in South Carolina. Access measures included health insurance and a regular source of care. Screening was measured by a Pap test within three years of interview. HPV vaccine acceptability was measured by receipt of the vaccine or willingness to vaccinate a child under 18 years of age. HPV and Pap test knowledge were measured separately using indices. Social determinants of interest were lifetime experiences of discrimination and distrust in the health care system. Multivariate logistic regression determined outcome predictors (Pap test or HPV vaccine acceptability) using appropriate survey design procedures in SAS 9.2. Population Studied: Potential subjects (18-70 years) were randomly selected. The interview response rates for the primary sample and the African American oversample were 36.7% and 34.0% with 1,029 respondents. Incomplete interviews and “other” minority groups were excluded from analysis (n=986), African-American (30.5%) and white respondents (69.5%). Principal Findings: Most respondents (87%) reported Pap tests. More African Americans (70.3%) preferred annual Pap tests even if advised by a provider about longer intervals compared to white women (55.4%, p<.0001). Twenty percent reported the HPV vaccine; however, 77% were willing to vaccinate themselves or their children under 18 years of age. More African Americans reported high experiences of perceived discrimination (34.2%) than whites (4.0%) (p<.0001). Nearly half of the African-American respondents reported provider counseling during their last Pap compared to a third of white women; however, African Americans reported lower knowledge (p<.0001). Access was a greater predictor of cervical cancer screening than social determinants or preferences. Women with a regular provider (AOR=2.819; 95% CI 1.449, 5.483) and private health insurance (AOR=2.970 CI 1.364, 6.469) were more likely to report Pap tests, controlling for race, and knowledge. Provider counseling had an impact on Pap tests (AOR=2.007 CI 1.27, 3.19) not vaccine acceptability. Conclusions: There was high acceptability for innovation in cervical cancer prevention and control practices. However, African-American women viewed the health care system more negatively and reported more discrimination, which may contribute to a lack of trust in provider recommendations. Access was the strongest predictor of a recent Pap test. Implications for Policy, Delivery or Practice: The findings indicate barriers to cervical cancer prevention and control, which may contribute to mortality disparities. Further research is needed to identify preferences for HPV innovation to inform the development of HPV interventions. Improved access, especially to safety net health centers, would increase cervical cancer screening and may lead to reduced disparities. Funding Source(s): NCI Poster Number: 146 Through Our Eyes: Perspectives of Young Black Men on Factors Affecting Transition to Manhood Presented by: Nazleen Bharmal, M.D., M.P.P., NRSA Fellow, Department of GIM/HSR, University of California, Los Angeles, 911 Broxton Avenue, 3rd Floor, Los Angeles, CA 90024; Phone: (310) 7940150; Email: nbharmal@mednet.ucla.edu Co-authors: Arleen Brown, M.D., Ph.D.; David Kennedy, Ph.D.; Loretta Jones, M.A.; Charles LeeJohnson, M.S.W.; D'Ann Morris Research Objective: To have young, Black men from Los Angeles County identify and discuss factors affecting their transition to manhood using photovoice Study Design: We used CBPR/CPPR principles to form a 12-person collaborative of academic and community members from various organizations. To date, the collaborative has defined goals for the partnered project to address premature mortality in Black men, developed a project protocol, participated in data collection and analysis, and developed a preliminary dissemination plan. The protocol was approved by the RAND Corporation IRB. We used photovoice for data collection. Each participant was given a digital camera to take a minimum of 50 and maximum of 300 photographs over four months. Participants individually discussed photographs with an advisory board member using the SHOWeD method. Each participant used pile-sorting methods to discuss major themes with an advisory board member. Participants then selected 6-10 representative pictures to put into a group collection of photographs. In a separate session, each participant, pile-sorted the group photographs and discussed themes with an advisory board member. All pile-sorting sessions were audio recorded and transcribed. Pile-sorts of group pictures were analyzed using multidimensional scaling and hierarchical cluster analysis to systematically compare participants’ themes and identify patterns of associations between sorted photographs. Major themes and related quotes were also elicited from the pile-sorting transcripts. Population Studied: Eligible participants were 1626 year old Black men who had lived most of their lives in Los Angeles. Candidates were recruited by advisory board members. Principal Findings: Twelve recruited participants completed all phases of the project. The participants had a mean age of 20 years, 25% were enrolled in higher education, 33% employed full time, 75% grew up in single-parent/fostercare homes, and 50% had been incarcerated and/or involved in gangs. Four clusters emerged from the group collection of photographs. The participants interpreted the clusters as: 1) Struggles faced in manhood. Pictures and quotes of police harassement, incarceration, institutional racism, lack of stable finances or job opportunities, homelessness, neighborhood effects, lack of direction/despair, family challenges (including poor health of caretakers), and substance abuse/dependence. 2) Inspiration and/or social support. Pictures and quotes depicted family, friends, coaches, religion and church, music, nature, and people from car clubs & communitybased organizations. 3) Role of Sports. Pictures and quotes showing sports as teamwork, an outlet/escape, fitness, entertainment, and personal accomplishment pivotal during their transition to adulthood. 4) Los Angeles lifestyle. Commentary and pictures about the opulence and excess of living in LA, including expensive homes, rich neighborhoods, high-end fashion, entertainment industryluxury/sports cars, beautiful/picturesque views, and abundance of fast food restaurants. Most men discussed this lifestyle as unattainable (except the fast food), but recognized the influence of LA life on their personal and professional goals. The theme analysis of experiences, which is ongoing, will generate additional themes that participants identify from their individual photos as important in their transition to manhood. Based on the project findings, priority areas will be identified by the advisory board and participants. Community dissemination of the results may include sharing findings with community, school-based, and policy organizations that affect healthy outcomes for Black men through workshops, town hall meetings, interactive gallery exhibit, and popular press articles. Conclusions: CBPR and photovoice are effective methods to engage young, Black men to identify and discuss factors affecting their transition to manhood, contextualize research findings, and participate in dissemination. Implications for Policy, Delivery or Practice: These methods not only allow traditionally disenfranchised individuals and communities to identify and document pertinent issues of concern, but also to create the design and implementation of strategies that foster positive change. Our small project has led to the formation of a community service/advocacy young men's group for the participants, as well as a broader coalition among the advisory board members to pursue a charter school focused on young boys of color. Funding Source(s): RWJF, Clinical Scholars Program Poster Number: 147 Massachusetts Leads the Way: Pay for Performance to Reduce Racial/Ethnic Disparities Presented by: Jan Blustein, M.D., Ph.D., Professor of Health Policy and Medicine, Health, New York Unversity/Wagner Graduate School, 295 Lafayette Street, New York, NY 10012; Phone: (212) 998-7427; Email: jan.blustein@wagner.nyu.edu Research Objective: Massachusetts is the first state to provide financial incentives to hospitals to adopt practices and processes that reduce racial/ethnic disparities in health care. Hospitals recently began to receive payments though the MassHealth (Medicaid) program in a phased program that began with public reporting and is moving toward performance-based payments. This study sought to understand the terms of MassHealth's P4P/disparities program, assess implementation challenges, and identify factors associated with variations in hospital performance. Study Design: We used a mixed methods approach to understand the program’s workings, implementation, and early impact. We reviewed public documents and held open-ended in-depth interviews with state employees. Additionally, we analyzed the first year of performance and payment data to assess the extent to which hospitals met reporting requirements, and to determine the degree to which performance on disparities measures was associated with hospital characteristics. Population Studied: Our quantitative analysis examined the performance of the 66 acute care hospitals that participated in MassHealth's Hospital Pay-for-Performance initiative in RY2008. Principal Findings: During RY2008 hospitals were eligible for payments for reporting and/or performance on two dimensions: (1) organizational cultural competence, as measured by a selfassessment tool, and (2) disparities in clinical care for 4 conditions. Implementation challenges included: (a) rolling out a complex program during the relatively tight timeline dictated by statute; (b) selecting and developing measures that were appropriate for a Medicaid population; (c) conveying reporting requirements to hospitals; and (d) identifying valid and reliable disparities indices. Hospital success in meeting reporting and performance requirements varied. For the cultural competence self-assessment, 21 of the hospitals (32%) were ineligible for incentive payment due to data deficiencies (failed timely reporting or inadequate documentation). Of the 45 that reported successfully, most received scores below 50% on the self assessment instrument. Hospitals were more successful in reporting clinical performance by racial/ethnic subgroup, with only 4 (6%) failing to provide acceptable data. However, there was little measurable within-hospital disparity in care on the clinical measures. In part, this was due to small sample sizes for each clinical condition, and relatively homogeneous patient populations in most hospitals. Conclusions: The MassHealth P4P/disparities program is in the early stages of implementation and refinement. Hospitals had difficulties with reporting requirements around the cultural competence self-assessment, but were able to provide patient-level race/ethnicity data for clinical services. Realities such as small sample sizes and limited within-hospital racial diversity have proven to be significant barriers to executing a credible program to enhance racial equity in health care. Implications for Policy, Delivery or Practice: Pay-for-performance may be a useful tool to reduce disparities in health care. Massachusetts' experience provides a model for other states and entities hoping to adopt this approach. However, early experience suggests that the task is logistically and technically challenging. National well-validated measures are needed that apply to low income populations served by Medicaid. Successful implementation of P4P/disparities will require flexibility and sustained engagement by policymakers and stakeholders. Poster Number: 148 Geographic Variation in Service Connection Disability Ratings in the American Community Survey Presented by: Michel Boudreaux, M.S., Research Assistant, School of Public Health, Division of Health Policy and Managment, University of Minnesota, 2221 University Avenue SE, Suite 345, Minneapolis, MN 55414; Phone: (651) 503-4079; Email: boudr019@umn.edu Co-authors: Yvonne Jonk, Ph.D.; Kathleen Thiede Call, Ph.D. Research Objective: In 2008, the American Community Survey (ACS) added a question addressing veterans’ service connection (SC) disability ratings. The primary objective of this paper is to examine geographic variation in veterans’ SC ratings by state and to identify explanatory factors. We also assess the quality of this new variable for Department of Veteran Affairs (VA) policy related questions. Study Design: Descriptive analysis of SC ratings by state is followed by regression analyses accounting for potential explanatory variables. To asses the quality of the SC variable, the consistency of SC responses with other information obtained in the survey is described. Next, ACS results are compared to counts published in the Veterans Benefits Administration (VBA) annual Benefits Report. Since the ACS sample frame does not include all the populations included in VBA data and covers a slightly different time period (CY 2008 versus FY 2008), VBA reports are not a perfect standard. Thus, we examine the relative difference of the ACS and other general population surveys to VBA data. Population Studied: U.S. veterans. Data comes from the ACS, an ongoing survey of the U.S. population that samples roughly 3 million addresses. Related survey topics include veteran status, period of service, socio-economic characteristics, and disability measures that are related, but not equivalent to SC disability. Principal Findings: Initial examination of SC rating by state found that nationally, 21% of veterans had ratings of 70% or more, after excluding veterans reporting a 0% rating and those refusing to report their rating. West Virginia had the highest percentage of such veterans (29.8%) and North Dakota had the lowest (13.7%). Since some variation is to be expected, further adjusted analyses will address whether state-level variation in SC ratings can be explained by differences in veterans’ socio-economic and servicecharacteristics. Anomalies were found for veterans reporting a 0% rating, but overall results approximated administrative counts. Discrepancies were similar to other general population surveys. Self-reported income was generally consistent with self-reported SC rating. However, the average ‘other income’ (which includes all “VA payments”) for veterans reporting a 50-60% SC rating was less than VBA compensation amounts published by the VA. The percentage of those with an ACS defined disability by rating category trended in the right (higher rated veterans were more likely disabled). Conclusions: Preliminary results found geographic variation in SC ratings by state. These results indicate that the geographic variation found by previous researchers persists. While data anomalies were found, the ACS is a useful source of information for policy makers and analysts interested in the well-being of veterans. Implications for Policy, Delivery or Practice: SC rating is a primary determinant of the level of financial support and health care access granted to disabled veterans. Previous studies have found ratings disparities by gender, race, and geography that cannot be explained by differences in impairment. Thus, quality data and careful monitoring of disabled veterans is of critical concern to policy makers seeking to improve the equity of the VA disability system and to those interested in assessing the needs of disabled veterans. Poster Number: 149 Perceived Discrimination and Patient Experience with Care Presented by: Thomas Bryant III, M.S.W., Doctoral Student, Health Services Research, Management & Policy, University of Florida, Health Science Center, PO Box 100195, Gainesville, FL 32610-0195; Phone: (904) 253-2263; Email: bryantt3@ufl.edu Co-authors: Robert Weech-Maldonado, M.B.A., Ph.D.; Allyson Hall, Ph.D. Research Objective: Examine the relationship between patients' perceptions of discrimination, and their experiences with Medicaid as shown by the Consumer Assessments of Healthcare Providers and Systems (CAHPS) reports and ratings of care. Study Design: Data consist of randomly surveyed Florida Medicaid beneficiaries from September 2007 to December 2007. The survey included the Health Plan CAHPS 4.0 instrument and a set of items assessing patient experiences with discrimination. There was a 40% response rate, 1877 completed surveys. The data is limited to respondents with a personal doctor, resulting in 1509 completed surveys. The dependent variables are Health Plan CAHPS 4.0 reports (getting needed care, timeliness of care, doctor communication, and health plan customer service) and ratings of care (personal doctor, specialists, health care, and health plan). Independent variables include measures of patient experiences with racial/ethnic discrimination. Variables related to systematic differences in survey responses are used as casemix adjustors: gender, age, education, and health status. Data are analyzed using analysis of variance (ANOVA) and ordinary least squares regression. Population Studied: Non-HMO Florida Medicaid beneficiaries from September 2007 to December 2007. Principal Findings: Study results show that a significant proportion (9%) of the sample perceive discrimination as a result of race/ethnicity. Respondents who experienced discrimination sometimes significantly report more difficulties getting needed care (B=-21.7; p<.0001), getting care quickly (B=-11.5; p=.005) and communicating well with their doctors (B=-13.8; p<.0001) than those who never experienced discrimination. Moreover, patients who perceived discrimination sometimes significantly gave lower ratings for care received (â=-13.2; p<.0001), their personal doctor (B=-7.5; p=.005), specialist (B=-7.8; p=.017) and health plan's customer service (B=-13.83; p<.0001) compared to respondents who never experienced discrimination. These results suggest that perceptions of race/ethnic discrimination are associated with lower CAHPS reports and ratings of care. Conclusions: The results suggest that perceptions of discrimination based on race/ethnicity and Medicaid insurance are associated with lower CAHPS reports and rating of care. Implications for Policy, Delivery or Practice: Findings imply that Medicaid health plans should use quality improvement efforts to address perceptions of discrimination as a barrier to care for their enrolled patient population. Findings suggest that reducing perceptions of discrimination can result in improved CAHPS reports and ratings of care. The study also suggests the importance of assessing cultural competency from the patients' perspective, and including these measures in patient health care surveys. Poster Number: 150 Rise of Tobacco Use among the Hmong in Minnesota as Perceived by Community Leaders Presented by: Diana Burgess, Ph.D., Assistant Professor/Core Investigator, Department of Medicine and Center for Chronic Disease Outcomes Research (CCDOR), University of Minnesota and Minneapolis VA Medical Center, One Veterans Drive, Minneapolis, MN 55417; Phone: (612) 467-1591; Email: diana.burgess@va.gov Co-authors: Jeremiah Mock, M.Sc., Ph.D.; Nina Alesci, M.P.H.; Barbara Schillo, Ph.D.; Steven Foldes, Ph.D.; Jessie Saul, Ph.D. Research Objective: Research suggests that smoking is becoming an increasing problem among the Hmong in the United States. Traditionally, in Laos, very few Hmong adults smoked tobacco and it was almost unheard of for Hmong youth to smoke. However, studies of tobacco use among this population are sparse. The purpose of this study was to gain a deeper understanding of tobacco-related attitudes, beliefs, and behaviors in the Hmong community and to gain insights into strategies for reducing tobacco use in this population. Study Design: Data were derived from a larger community-based participatory research study examining tobacco use within four Southeast Asian communities in Minnesota through key informant interviews with formal and informal community leaders. Southeast Asian members of the research team, who were fluent in English and their native language, conducted semi-structured interviews lasting 60-90 minutes. Interviews were taperecorded, transcribed, and translated into English when necessary and reviewed by another bilingual researcher to assure the accuracy of the translation. Data were analyzed using grounded theory. Initial results were presented these findings to members of Hmong community who served as informal advisors to the research project, and were modified based on their feedback. Population Studied: Key informants consisted of 7 female and 7 male Hmong key informants, ages 24 to 65, living in Minnesota, who had been in the US from 12-24 years. The key informants volunteered with civic organizations. Nine key informants spoke English and Hmong equally and 5 spoke only Hmong. All female key informants stated that they had never smoked cigarettes. Of the men, 2 were current smokers, 2 were former smokers, and 3 had never smoked. Principal Findings: Informants felt that living in the U.S. had contributed to the rise of cigarette smoking within their ethnic community. Whereas in Laos, very few Hmong male youths smoked and were admonished for smoking, and female youths were never seen smoking, in Minnesota it had become commonplace to see both genders of Hmong youths smoking. The key informants’ construction of this problem was centered primarily on social concerns rather than health concerns, in which Hmong youths’ public displays of smoking were seen as acts of disregard for, and rejection of traditional Hmong cultural norms, due to adoption of “American” values. Informants believed that middleaged Hmong men and elders took up smoking while living in Minnesota because of their traumatic and difficult life experiences rather than because they were trying to preserve “traditional” roles. Informants also believed that Hmong people in Minnesota had learned very little about the negative health effects of smoking. Conclusions: Key informants believed that traumaand relocation-induced stress, anxiety, and depression (among elders) and the adoption of American values (by youth), had a substantial negative influence on tobacco use and norms in their ethnic community. Implications for Policy, Delivery or Practice: There is a need for additional research to validate the findings that emerged from this qualitative study, as well as research that focuses on smoking among youth, which was a major concern among key informants. Nonetheless, this study points to the need for policy makers and advocates to address the specific root causes underlying smoking among different segments of the Hmong community. It is also important that health care professionals who care for Hmong refugees and immigrants to be aware of and provide culturally meaningful resources to address their smoking as well as other psychiatric disorders and psychosocial problems. Funding Source(s): Clearway Minnesota and Blue Cross Blue Shield of Minnesota Poster Number: 151 Self-stigma, Stress, and Smoking among African American and American Indian Women Smokers: An Exploratory Qualitative Study Presented by: Diana Burgess, Ph.D., Assistant Professor/Core Investigator, Department of Medicine and Center for Chronic Disease Outcomes Research (CCDOR), University of Minnesota and Minneapolis VA Medical Center, One Veterans Drive, Minneapolis, MN 55419; Phone: (612) 467-1591; Email: diana.burgess@va.gov Co-authors: Rachel Widome, Ph.D.; Sean Phelan, M.P.H.; Michelle van Ryn, Ph.D., M.P.H.; Steven S. Fu, M.D., M.S.C.E. Research Objective: Research suggests that negative emotions and difficulty coping with stressful events might impede women’s ability to quit smoking. The following qualitative study explores the interrelationship between smoking behavior and negative emotions among a sample of racial/ethnic minority female smokers. Study Design: Data were derived from a larger study, the Perspectives of Ethnic Minority Smokers (POEMS) project, involving sixteen 90-minute focus groups with current and former smokers from ethnic minority communities who were recruited by community organizations. In the first stage of analysis, focus group transcripts were coded and analyzed by three reviewers to identify emergent themes. In this second stage, grounded theory was used to analyze a subset of the findings involving smoking both a way to cope with and also a source of negative emotions and stress. Population Studied: The current analyses include 16 female African American and American Indian smokers from 3 focus groups. The focus groups were conducted in a large metropolitan area in the Midwest. Principal Findings: Consistent with prior research, participants reported using smoking as a tool to cope with stress and negative emotions. Deprivation from smoking—either due to a deliberate quit attempt or to the inability to obtain cigarettes—was associated with negative states such as anger, irritability, and distress. In addition, women expressed negative emotions (e.g. guilt, anxiety, disgust) and negative images of themselves (e.g., weak, “not very smart”) due to their inability to quit, despite the negative consequences they experienced from smoking. These negative self-perceptions are consistent with stigmatized views of smokers held by the public. Women also expressed feelings of defiance about their smoking despite pressure to quit and identified external factors, including those linked to race and social disadvantage, which contributed to their inability to quit. These findings are discussed in the context of research on social stigma. Conclusions: The negative emotions, self-stigma and shame experienced by low income American Indian and African American women smokers may contribute to continued smoking and disrupt attempts to quit smoking. Future research is needed to explicitly examine the role of negative emotions, stress and stigma among low-income minority women smokers in order to develop effective tobacco cessation intervention for this vulnerable group of smokers. Implications for Policy, Delivery or Practice: Results point to the need for tobacco control initiatives aimed at socially disadvantaged women to address the negative emotions that may hinder cessation. Such interventions might include helping women find alternative ways to cope with life stressors and negative emotions. It is also important to ensure that tobacco control initiatives do not contribute to the stigmatization felt by women who smoke. In particular, it is suggested that messages avoid depicting socially disadvantaged mothers who smoke as a source of harm to their children and instead depict them as individuals who are important in their own right, and worthy of the health benefits that quitting smoking would bring. Funding Source(s): Clearway Minnesota Poster Number: 152 Racial and Ethnic Differences in Diabetes among People with Psychiatric Disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions Presented by: Leopoldo Cabassa, Ph.D., Assistant Professor, Psychiatry, Columbia University/New York State Psychiatric Institute, 1051 Riverside Drive Room 1715, Unit 11, New York, NY 10032; Phone: (212) 543-5311; Email: cabassa@pi.cpmc.columbia.edu Co-authors: Roberto Lewis-Fernández, M.D.; Jorge López Castroman, M.D.; Carlos Blanco, M.D., Ph.D. Research Objective: The aim of this study was to examine racial and ethnic differences in diabetes in a nationally representative sample of adults with psychiatric disorders. Study Design: Data were drawn from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative study conducted in the United States (U. S.). The AUDADIS-IV, a structured diagnostic interview, was used to determine psychiatric diagnostic assessments of past-year mood, anxiety, and alcohol/ substance abuse disorders, and lifetime personality disorders. The presence of diabetes and other common medical conditions (e.g., cardiovascular disease, hypertension, liver disease) was determined by two questions. Participants were asked whether they had a particular medical condition (e.g., diabetes) in the last 12 months. If they answered “yes”, then they were asked whether this diagnosis was confirmed by a doctor or other health professional. Those responding “yes” to both questions were categorized as having the medical condition in question. Multivariate logistic regression models adjusting for sociodemographic variables (e.g., age, gender, education) and common diabetes risk factors (i.e., body mass index, comorbid medical conditions and use of psychotropic medications) were used to examine racial and ethnic differences in diabetes across a variety of psychiatric conditions (e.g., mood, anxiety, alcohol/substance abuse). Diabetes rates were compared between nonHispanics whites (reference group) and several racial and ethnic minority groups including African Americans, Hispanics, Native Americans, and Asians/Pacific Islanders. Population Studied: This study used a nationally representative sample of 34,653 noninstitutionalized adults 18 years of age or older. Principal Findings: African Americans, Hispanics, and Native Americans with a variety of psychiatric conditions reported significantly higher rates of diabetes than non-Hispanics whites and Asian/Pacific Islanders with similar mental health needs. The higher prevalence of diabetes among African Americans and Hispanics with psychiatric disorders when compared to their non-Hispanic whites counterparts persisted even after adjusting for sociodemographic variables and common diabetes risk factors. Odd Ratios (OR’s) for African Americans ranged from 1.75 (95% CI:1.31-2.32) for diabetes and any personality disorders to 1.96 ( 95% CI:1.24-3.11) for diabetes and any mood disorders. OR’s for Hispanics ranged from 1.87 (95% CI: 1.23-2.86) for diabetes and any mood disorders to 3.09 (95% CI 1.50-6.36) for diabetes and any alcohol/drug abuse disorders. Across each of the psychiatric disorders examined, no significant differences were reported between non-Hispanic whites and Native Americans and Asian/Pacific Islanders in the rates of diabetes once we controlled for sociodemographic variables and diabetes risk factors. Conclusions: This study presents racial and ethnic disparities in diabetes among a nationally representative sample of people with common psychiatric conditions. Implications for Policy, Delivery or Practice: The higher prevalence of diabetes among African Americans, Hispanics, and Native Americans with psychiatric conditions suggests that targeted efforts are needed to screen and monitor the physical health of these groups in both mental health and primary care settings. Culturally appropriate prevention and treatment strategies are needed to reduce the negative impacts of diabetes and its complications among racial and ethnic minority communities in the U. S. Funding Source(s): NIDA, New York State Office of Mental Health Poster Number: 153 Are Black Patients More Likely to Receive Total Knee Arthroplasty in Lower-Quality Hospitals? Presented by: Xueya Cai, Ph.D., Research Assistant Professor, Internal Medicine, University of Iowa Carver College of Medicine, SE 615 GH, 200 Hawkins Drive, Iowa City, IA 52242; Phone: (319) 384-8512; Email: xueya-cai@uiowa.edu Co-authors: Peter Cram, M.D.; Mary VaughanSarrazin, Ph.D. Research Objective: Total knee arthroplasty (TKA) is performed to relieve pain and improve function for patients with advanced knee osteoarthritis. Substantial evidence suggests that despite the dramatic expansion in indications of TKA, blacks are less likely to receive this procedure compared to whites. It is less clear, however, whether blacks are more likely to undergo procedures in lower quality hospitals than whites when they do receive the procedure. Two previous studies found that nonwhite patients tend to receive TKA in lower- volume (likely lower-quality) hospitals. In this study, we estimated hospital quality using a composite outcome defined as complication or mortality within 90 days of surgery, adjusted for patient risk. We then examined the association between race and admissions to low-quality and high- quality hospitals. Study Design: We analyzed 100% Medicare Provider Analysis and Review (MedPAR) data to identify patients undergoing primary TKA (ICD-9CM code 81.54) between July 2002 and June 2005 (n=635,439). A random-intercept logistic regression model of 90-day postoperative complications (sepsis, hemorrhage, pulmonary embolism, deep vein thrombosis, wound infection requiring readmission and death) was estimated, adjusting for patient demographics, admission source, admission year, and co-morbidities using a previously published algorithm. The ratios of observed-to-expected outcomes (O/E ratio) were calculated for each hospital. Hospitals were then classified into high-quality (O/E in the bottom quintile of all hospitals), low-quality (O/E in the highest quintile), and intermediate-quality (middle three quintiles) groups. We further identified white and black patients undergoing primary TKA between July and December of 2005. A multinomial logit model was estimated to test the independent impact of race on admissions to high-quality and low-quality hospitals defined above. The models controlled for patient age, gender, admission source, comorbidities, education level and household income (based on zipcode-level US census data), travel distance to hospital (based on miles between patient residence and hospital zipcode), and geographic location of patient residence (urban or rural). Population Studied: Over 727,411 Medicare admissions to 3611 hospitals for primary TKAs between 2002 and 2005. Principal Findings: Between July and December of 2005, 87,019 whites and 4,953 blacks underwent TKA. Blacks were less likely than whites to receive TKA in high-quality hospitals (6.1% vs 10.2%, p<0.0001), and more likely to receive TKA in lowquality hospitals (21.4 vs 11.9%, p<0.0001). Black patients had lower household income and traveled shorter distance for admission. Multivariable analyses showed that blacks were less likely to use high-quality hospitals (OR=0.84, 95% CI 0.72-0.92), and more likely to use low-quality hospitals (OR=1.76, 95% CI 1.61-2.10) than whites. Sensitivity analysis confirmed our findings when high-quality and low-quality hospitals were defined using alternative cut-off points of the risk-adjusted complication rate. Conclusions: Black Medicare patients tend to receive TKA in lower-quality hospitals. Implications for Policy, Delivery or Practice: This study finds that in addition to the welldocumented under-utilization of arthroplasty among blacks, black patients who do receive TKA tend to be admitted to lower quality hospitals. Further studies are necessary to uncover the mechanisms at the patient, referring physician and system-ofcare levels that lead to the racial disparity in access to high-quality hospitals for TKA. Funding Source(s): RWJF Poster Number: 154 Systematic Measurement Error’s Influence on Disparities in National Rates of Children with Special Health Care Needs Across Spanish and English Speaking Households Presented by: Adam Carle, Ph.D., M.A., Assistant Professor, Department of Pediatrics: Division of Health Policy and Clinical Effectiveness, Cincinnati Children's Hospital and Medical Center; University of Cincinnati, 3333 Burnet Avenue, Cincinnati, OH 45226; Phone: (513) 803-1650; Email: adam.carle@cchmc.org Research Objective: Non-English speaking children often experience poorer health and greater care obstacles than English speakers. This includes English speaking children with non-English speaking parents. Yet, research suggests large differences in the rates of US children with special health care needs (CSHCN) across English (14%) and Spanish speaking families (4.6%). A result opposite much disparities research. And, a finding that suggests that children from Spanish speaking homes may require fewer resources than children from English speaking families. However, culture and translation may affect the way parents answer questions about their children, resulting in differences that reflect systematic measurement error (i.e., measurement bias) not true differences. Before concluding that disparities across Spanish and English speaking children reflect true differences and allocating resources, research must establish that the instrument used to identify CSHCN, the CSHCN Screener, provides equivalent measurement in English and Spanish. This study investigates this. Study Design: I used multiple group (MG) multiple indicator-multiple cause (MIMIC) item response theory (IRT) to investigate whether the CSHCN Screener provides equivalent measurement across English and Spanish versions. MG-MIMIC models, based in structural equation modeling and IRT, powerfully investigate measurement bias: the possibility that parents of children with identical health respond dissimilarly to questions about their children’s health as a function of the language in which they answer the questions. MG-MIMIC do this by developing equations that describe how parents respond to questions about their children. Subsequently, one tests the equivalence of these equations across Spanish and English speaking parents. Population Studied: Data came from the 20052006 National Survey (NS) of CSHCN, a large, representative survey of US children (n = 350,345) aged 0-17 years old. Principal Findings: MG-MIMIC that included cross-group differences in education and income as influences on measurement uncovered no statistically significant systematic measurement error across English and Spanish versions of the CSHCN Screener. However, a “naïve” model excluding education and income’s influences, found statistically significant measurement bias. Conclusions: Results demonstrated that responses provided equivalent measurement across English and Spanish versions among children with similar socio-demographics, increasing confidence in research showing differences in the prevalence of CSHCN across English and Spanish speaking children examined within similar sociodemographics. However, results showed that comparisons across Spanish and English speaking families without regard to other sociodemographics will lead to biased results, calling into question work comparing CSHCN across Spanish and English families without taking into account systematic differences in the distribution of education and income across these groups. Implications for Policy, Delivery or Practice: These findings eM.P.H.asize the value of culturally sensitive research and clinical practice. Individuals’ sociodemographic backgrounds can potently influence how they respond to questions, causing responses in one language to mean something different than similar responses in another language. Using model-based estimates can mitigate systematic measurement error and lead to more accurate disparities estimates and research. When conducting research across distinct racial, ethnic, and/or cultural groups, investigators should establish the equivalence of the measures used to insure the validity of results before developing policy and allocating resources based on the results. Poster Number: 155 Conducting Propensity Score Analyses in Complex Survey Data with Design Weights to Evaluate Policies Aimed at Reducing Health Disparities Presented by: Adam Carle, Ph.D., M.A., Assistant Professor, Department of Pediatrics: Division of Health Policy and Clinical Effectiveness, Cincinnati Children's Hospital and Medical Center; University of Cincinnati, 3333 Burnet Avenue, Cincinnati, OH 45229; Phone: (513) 803-1650; Email: adam.carle@cchmc.org Research Objective: Policy makers and investigators frequently wish to evaluate the effectiveness of policies aimed at reducing health disparities. However, an inherent tension exists in research of this type: one cannot randomly assign individuals to policy exposure conditions (policy exposure vs. no exposure). This limits causal conclusions, as confounding variables likely influence the likelihood that individuals are exposed to a policy. For example, states differ in their policies (or lack thereof) aimed at eliminating health disparities. Simultaneously, sociodemographic variables predict individuals’ states of residence. As a result, the propensity to benefit (or not) from a policy is correlated with characteristics of individuals exposed to the policy. Thus, to make stronger causal statements about a policy’s effectiveness, analysts need to acknowledge that the propensity for exposure to a policy differs across individuals. Propensity score methods have gained prominence as an effective method for handing this bias. In essence, propensity score methods “balance” the groups (exposed vs. unexposed) in terms of a set of covariates in an effort to equate the groups and make stronger causal conclusions. Survey data often offer the best datasets within which to conduct this research. However, large scale surveys frequently employ complex designs and include design weights. Unfortunately, little to no published literature guides investigators on how (or whether) to include weights in propensity score methods, including score development and utilization of the scores in analyses. In this paper, I address this. I offer practical summary advice for researchers seeking to incorporate propensity score methods in the presence of design weights. Study Design: Using data from the 2005-2006 National Survey of Children with Special Health Care Needs (NS-CSHCN), I compare the performance of unweighted and weighted propensity score methods across four popular propensity score matching methods: nearestneighbor, radius, kernel, and stratification matching. I also demonstrate the effect of failure to include design weights when estimating the propensity score. Population Studied: The NS-CSHCN provides data on the prevalence of special health care needs and their impact on children and their families. Children (n = 40,723) ranged in age from 0 to 18 years. Design weights make the data representative of children nationally and within states. Principal Findings: Failure to include weights in the propensity score’s development resulted in appreciably different propensity scores compared to developing the scores by including the weights. Likewise, across matching methods, failure to include weights in propensity score analyses resulted in significantly different, biased results. Conclusions: When evaluating policy’s effects in complex survey data, analysts should include the weights in the propensity score development and subsequent analyses. Researchers should not ignore weights. Failure to do so results in biased estimates. Implications for Policy, Delivery or Practice: Propensity score methods let health disparities research make stronger causal statements regarding the effects of policies. Large scale surveys offer health services research excellent opportunities to advance health disparities research and evaluate effective policy and practice, especially when incorporating propensity score methods. However, in order to properly use large scale survey data with design weights, researchers must adopt the practices described in this research. Otherwise, they will draw inappropriate conclusions. Poster Number: 156 Patient and Clinician Discussions of Physical Activity: Findings from an Underserved Population Presented by: Jennifer Carroll, M.D., M.P.H., Assistant Professor, Family Medicine, University of Rochester Medical Center, 1381 South Avenue, Rochester, NY 14620; Phone: (585) 506-9484; Email: jennifer_carroll@urmc.rochester.edu Co-authors: Paul Winters, M.S.; Ronald Epstein, M.D.; Kevin Fiscella, M.D., M.P.H. Research Objective: The 5As guidelines are an evidence-based framework for behavioral health counseling. The 5As, in which a clinician Asks about, Advises, Agrees upon, Assists and Arranges a follow-up plan, is promising as a counseling strategy in primary care to promote physical activity in underserved populations. The research objective is to report findings of patient and clinician 5As use in physical activity discussions in an urban primary care setting. Study Design: The study design is a two-group pilot RCT with family medicine clinicians as the unit of randomization. The RCT is a clinician training intervention currently underway to promote 5As discussions about physical activity in an underserved primary care population in Rochester, NY.The intervention includes novel electronic health records tools to prompt 5As discussion and tailor referral options for accessible community resources for physical activity. Here, we report on 70 baseline audiorecorded patient-clinician visits followed by a patient survey and interview asking about their recall of physical activity discussions with their primary care clinician. Clinicians also completed surveys asking about use of the 5As in physical activity discussions. Population Studied: Twelve family medicine clinicians from two federally qualified community health centers and 70 of their patients. Clinicians were family physicians (64%), nurse practitioners (18%) and physician assistants (18%), averaging 15 years work experience (range 2-33 years). Patients had a mean of 42.6 years, and were 72% African American, 16 % Hispanic, and 14% Caucasian. Most(71%) had Medicaid insurance. Principal Findings: Patients’ average BMI was 32.6; weight-related comorbidities included diabetes (18%), hypertension (34%), depression (24%), and osteoarthritis or chronic pain (62%). Clinicians and patients reported similar communication gaps in 5As discussions. Clinicians reported difficulty with Assist and Arrange steps such as low confidence about negotiating a treatment plan (79%) and limited knowledge of community resources (75%). Patients also reported that their clinicians used Assist and Arrange skills less frequently (41%, and 18% respectively) compared the other As. Ninetysix percent of patients were highly interested getting a physical activity guided plan or referral from their clinician to an accessible, low cost community program for physical activity. Clinicians indicated a strong desire to learn more about referral options incorporated via the electronic health records system (100%). Conclusions: Clinicians and patients reported that Assist and Arrange skills were least frequent in physical activity discussions. Though clinicians reported Assist and Arrange to be challenging, both clinicians and patients were highly interested in incorporating Assist and Arrange into physical activity counseling through enhanced knowledge of accessible community resources for physical activity. Implications for Policy, Delivery or Practice: To improve clinician-patient communication about physical activity for underserved populations, accessible, low cost community resources for physical activity referrals are needed. We also need simple and effective referral procedures for clinicians and their patients. Electronic health record tools may be a promising strategy to facilitate communication and generate referrals to community programs. Funding Source(s): NCI Poster Number: 157 Investment in Nursing Key to Reducing Disparities in Outcomes in Minority Serving Hospitals Presented by: Margo Brooks Carthon, Ph.D., R.N., Post Doctoral Fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, 418 Curie Boulevard, Philadelphia, PA 19104; Phone: (215) 898-8050; Email: jmbrooks@nursing.upenn.edu Co-authors: Ann Kutney Lee, Ph.D., R.N.; Jeannie Cimmiotti, Ph.D., R.N.; Doug Sloane, Ph.D.; Linda Aiken, Ph.D., R.N. Research Objective: Few studies have examined the relationship between minority patient health outcomes and nursing care, despite nurses’ centrally important role in acute care. This research study’s objective was to determine whether hospitals with higher proportions of black patients differ in nurse and patient satisfaction compared to hospitals with fewer black patients, and if so why. Study Design: This study was a cross sectional analysis of three data sources collected in 20062007, including a large survey of hospital nurses’ perceptions of working conditions in four large states (California, New Jersey, Pennsylvania, and Florida), hospital patient discharge data obtained from these four states, and the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. Linear regression models were used to evaluate the relationship between the proportion of Black patients, patient satisfaction, and nurse-assessed quality measures. Population Studied: Hospital patient discharge data were used to obtain the percentage of Black patients in each hospital. The percentage of Blacks in hospitals was divided into three equal categories. A total of 429 hospitals in the 4 states met the data requirements for inclusion. Principal Findings: The percentage of patients who would definitely recommend the hospital to friends and family was 3% lower in hospitals with the highest proportion of Black patients, as compared to the hospitals with the fewest Blacks. In the context of HCAHPS data, this difference is sizable and statistically significant. Fewer patients in the hospitals with the highest numbers of Black patients also reported that nurses always communicated well with them, and always received help when they needed it. Nurses working in hospitals with the highest proportion of Black patients reported poorer quality of care and were less confident that patients could manage their care upon discharge, as compared to nurses working in hospitals with the fewest Black patients. These negative effects persisted, but were moderated, when controlling for nurse staffing levels and the nurse work environment. Conclusions: Patients in hospitals with higher proportions of Blacks are more dissatisfied than patients in hospitals with the fewest number of Blacks. Nurses’ perceptions of quality follow a similar pattern. Fewer Black patients received care in hospitals with good nurse work environments including adequate nurse staffing, explaining in part their higher levels of dissatisfaction. Implications for Policy, Delivery or Practice: The results suggest that a promising strategy for reducing racial disparities in hospital outcomes is to invest in improving nurse staffing and the quality of the nurse work environment in minority serving hospitals. Funding Source(s): NINR/NIH T32 NR 0714 Poster Number: 158 Looking Forward – Looking Back: The Use of Historical Analysis as a Qualitative Method to Address Contemporary Health Disparities Presented by: Margo Brooks Carthon, Ph.D., R.N., Post Doctoral Fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, 418 Curie Boulevard, Philadlephia, PA 09104; Phone: (215) 898-8050; Email: jmbrooks@nursing.upenn.edu Research Objective: Despite the recognition that historical and cultural factors significantly influence patterns of health and illness among minorities, studies which employ rigorous historical analysis of community health activism in minority communities are limited. This research study’s objective was to examine the pre and post health outcomes of an anti- tuberculosis campaign taking place between 1913 and 1925, in a Black South Philadelphia community. Results are then used to determine the utility of historical analysis as a useful qualitative method to evaluate the effectiveness of past policies and programs to reduce disparities. Study Design: Social historical methodology was employed for the completion of this study. Main outcomes of interest were tuberculosis death rates pre and post anti-tuberculosis campaign and the influence of collaborative networks in advancing public health interventions. Population Studied: Primary archives were used to describe and define the collaborative antituberculosis efforts of three Philadelphia-based civic associations: the Starr Centre, the Whittier Centre and the Phipps Institute. Sources were reviewed from the Barbara Bates Center for the Study of the History of Nursing, Temple Urban Archives, and the University of Pennsylvania General Archives. Secondary source analysis of vital statistics, newspapers, major historical work on nurses and physicians and sociological and historical monographs detailing the lived experience of Black Philadelphians was performed. Principal Findings: In 1900, Blacks living in Philadelphia suffered from TB mortality rates which were two - three times higher than native white residents. After decades of coping with excessive deaths, Black community members, along with a number of civic associations and health professionals organized to wage a war on the infectious disease. Subsequent to these efforts, a precipitous decline in TB mortality in the Black community occurred. Prior to the TB campaign of 1914, Philadelphia’s Black community was largely invisible in the war on TB. The inclusion of Black nurses and physicians, in conjunction with collective efforts of public-private partnerships to address both the health and material needs of Black community members, led to an increase in TB prevention efforts among members of the Black community. Conclusions: Findings from this study reinforce the importance of social cohesion and collective efficacy to improve health outcomes in minority communities. Results further suggest that the use of historical analysis may serve as a valuable qualitative measure to evaluate evidence and identify diverse strategies to address enduring public health dilemmas. Implications for Policy, Delivery or Practice: Given the persistence of disparities among racial minorities over the last century, the purposeful integration of history, policy, and practice offers compelling insights and direction for health equity initiatives today. Funding Source(s): AHRQ, NINR/NIH T-32 (NR0714) Poster Number: 159 Barriers to Accessing Care among South Asian Breast Cancer Patients Presented by: Neetu Chawla, M.P.H., Research Associate; Doctoral Candidate, Health Services; Division of Cancer Prevention and Control Research, University of California, Los Angeles, 650 Charles Young Drive South, Los Angeles, CA 90095-6900; Phone: (310) 825-7430; Email: nchawla@ucla.edu Research Objective: To understand the barriers faced by South Asian breast cancer survivors in utilization of cancer care. Study Design: Semi-structured, in-depth interviews were conducted among South Asian breast cancer survivors in English and four South Asian languages (Bengali, Hindi, Gujarati, and Urdu). All interviews lasted between 60 and 90 minutes, were audiotaped, and later transcribed. Interviewers were trained according to the protocol of the UCLA Institutional Review Board. The data collection instrument included both quantitative and qualitative questions. Open-ended questions covered a range of topics, including the utilization of care, spiritual needs, psychological well-being, and social support. Data from the utilization of care domain were analyzed for emergent themes and identification of barriers to cancer care. Population Studied: Forty South Asian women living in Southern California ages 18 and older with a previous diagnosis of breast cancer. Principal Findings: The ages of women ranged from 28 to 80 years, with the average age of women being 55 years. The ethnic breakdown of the sample was as follows: 53% Indian; 19% Pakistani; 19% Sri Lankan; and 8% Bangladeshi. Approximately 19% of the participants were in active treatment for their breast cancer whereas 78% of participants reported that their cancer was in remission. The time of diagnosis varied widely in the sample, ranging from March of 1980 to August of 2007. The majority of the sample (75%) reported that cancer was diagnosed at an early stage. Approximately 75% of women completed the interview in English and the remainder in a South Asian language. The sample included notable proportions of South Asians with lower socioeconomic status, with approximately 28% reporting high school education or less and 23% reporting an annual household income of less than $32,000 per year. Analysis of open-ended responses within the utilization of care domain revealed a number of barriers to care faced by South Asian women. Women who interviewed in a South Asian language were more likely to describe problems in communicating with providers and obtaining information. Across insurance status, women expressed difficulties in obtaining diagnoses, particularly those who were younger ages and who found their breast cancer themselves. Women without a family history of breast cancer suggested that physicians seemed less concerned about the disease and less likely to order additional tests during the diagnostic phase. Other barriers described distance to treatment facilities during chemotherapy and radiation, lack of information about treatment options, and difficulties obtaining second opinions. Several women also described receiving help from another breast cancer survivor in navigating their treatment and felt this positively shaped their treatment experience. Conclusions: South Asian breast cancer survivors described several barriers to obtaining their care and treatment. Communication with providers, particularly among non-English speaking South Asians was raised. In addition, women described delays in diagnosis and difficulties in navigating treatment (e.g. obtaining second options, need for additional information). Implications for Policy, Delivery or Practice: Health care practitioners should make efforts to reduce delays in breast cancer diagnosis, improve communication, and provide navigational support to South Asians with breast cancer. Cancer facilities should provide language assistance and consider peer navigators when delivering services to this population. Funding Source(s): California Breast Cancer Research Program Poster Number: 160 Health Disparities among Elderly Medicare Beneficiaries with Diabetes and Multiple Co-Morbid Chronic Conditions Presented by: Lichun Chia, Ph.D., Postdoctoral Fellow, Medicine, University of Pittsburgh, 230 Mckee Place, Pittsburgh, PA 15213; Phone: (412) 692-2011; Email: lic22@pitt.edu Co-authors: Howard Degenholtz, Ph.D. Research Objective: Racial and ethnic disparities in health care have important implications for health care providers, administrators and policy makers. Health care providers are expected to provide high quality of care to all patients based on need. In patients with diabetes, inadequate treatment and management of the conditions can result in complications. Racial and ethnic minorities have disparities in access to and use of primary care. Evidence-based studies have shown that complications of diabetes can be prevented with appropriate monitoring and management; however, there are disparities in quality for DM care. Few studies have examined the contribution of race/ethnicity to health disparities among people with diabetes and multiple chronic conditions. The purpose of this study was to compare access to care and diabetes related care management and outcomes between racial and ethnic minorities and Caucasians with diabetes and additional comorbid conditions. Study Design: This was a secondary data analysis using the nationally representative 2002 Medicare Current Beneficiary Survey data. Self reported information related to functional status, diabetes conditions, care management and access to care are included in the analysis. Univariate and bivariate, and regression analyses were used to examine the racial and ethnic differences in access to care and utilization of health care service. Population Studied: Medicare Beneficiaries 65 and older who have diabetes were included in the study. People who have end-stage renal diseases and live in nursing homes or assisted living facilities were excluded from the analysis. The final analytic sample had 2372 observations. Beneficiaries were divided into four racial/ethnic groups: Caucasian/Non Hispanic, African American/Non Hispanic, Hispanic, and others. Principal Findings: Approximately 64% of Caucasian beneficiaries reported that their general health was good to excellent compared to 50-54% for African Americans, Hispanic and other racial/ethnic groups respectively. While the number of comobidities was similar among the groups, the prevalence of specific comorbid conditions varied. Caucasians had higher rates of coronary heart diseases and osteoporosis, Hispanics reported higher rates of Chronic Obstructive Pulmonary Disorders, and African Americans had higher rates of hypertension. African Americans were also more likely to be prescribed insulin for controlling their diabetes and had worst blood glucose control. Hispanic and African Americans were more likely to report using an emergency room for primary care and had more difficulty of getting needed care. Finally, racial and ethnic minorities were more prone to diabetes related complication such as eye problems. Conclusions: These findings indicate that racial/ethnic disparities among Medicare beneficiaries with diabetes are evident. Minority groups are less likely to have usual source of care, poor control of their blood sugar, having more trouble of getting needed care and have more diabetic complications. Implications for Policy, Delivery or Practice: There is significant potential for better providing needed care to improve health outcomes and reduce complications among vulnerable minority populations. Longitudinal studies are necessary to assist policy makers in tracking system improvements. Funding Source(s): AHRQ Poster Number: 161 Reducing Racial and Ethnic Disparities in Health Care: Partnerships Between Employers and Health Plans Presented by: Patricia Collins Higgins, Ph.D., M.P.H., Researcher, Health, Mathematica Policy Research, 1549 Wild Rose Court, Golden, CO 80403; Phone: (303) 997-7216; Email: thiggins@mathematica-mpr.com Co-authors: Melanie Au, M.P.P.; Erin Fries Taylor, Ph.D., M.P.P. Research Objective: To assess current health plan/employer partnerships addressing disparities, provide an overview of barriers that prevent more partnerships from forming, and discuss strategies to encourage increased involvement of employers in the future. Study Design: Qualitative case study including document review and in-depth interviews with over a dozen key informants. Population Studied: We interviewed large employers, health plan representatives, government officials, and national experts. Principal Findings: Despite an increased focus on value-based purchasing among employers, it remains rare for employers to be working directly on disparities, either internally or in partnership with health plans. A few notable partnerships have recently emerged between large employers and health plans and between the Office of Minority Health and the National Business Group on Health. Additionally, some employers are beginning to assess health plans’ disparities work through evaluation tools such as eValue8. Barriers to greater employer involvement in disparities reduction include lack of employer awareness of the importance and cost of disparities, concerns about the legality of sharing employees’ race and ethnicity data, and the perceived administrative burden and cost of disparities assessments. Several strategies may increase employer involvement in this work, including educating employers and employees on the causes and consequences of disparities, promoting the business case for disparities reduction, eM.P.H.asizing the legality of r/e data sharing, and creating more visible and cohesive national leadership around these issues. Conclusions: In the current economic environment, disparities assessment and reduction is a secondary priority for employers and health plans alike according to several purchasers and plans. However, some employers, particularly those with a diverse workforce, realize that addressing disparities ultimately has the potential to reduce health care costs and create a more productive and healthy workforce. Leading health plans continue to work towards more fruitful collaborations with employers and development of better methods of disparities assessment. Implications for Policy, Delivery or Practice: As disparities continue to be discussed by health plans, purchaser coalitions, and political figures, more employers may recognize disparities as a salient issue that is closely tied to value-based purchasing. Moreover, demographic shifts in U.S. workforce may eventually spur more employers and health plans to work together to reduce health care disparities, according to several experts. As the U.S. population continues to diversify and employers become more attuned to the direct and indirect costs of health care disparities, collaboration between purchasers and health plans on reducing disparities may increase. Funding Source(s): AHRQ Poster Number: 162 Impact of Health Literacy and Socioeconomic Status on Ethnic Disparities in Asthma Presented by: Laura Curtis, M.S., Statistical Analyst, Institute for Healthcare Studies, Northwestern University, 750 N Lake Shore Drive, 10th Floor, Chicago, IL 60611; Phone: (312) 5035538; Email: l-curtis@northwestern.edu Co-authors: Michael S. Wolf, Ph.D., M.P.H.; Kevin B. Weiss, M.D., M.P.H.; Leslie C. Grammer, M.D. Research Objective: Racial/ethnic disparities are well documented in asthma. While socioeconomic status has long been implicated as an explanatory factor, limited literacy has more recently been viewed as a potentially modifiable trait driving asthma inequities. We sought to determine whether literacy mediated the association between race and asthma outcomes. Study Design: Participants completed a face-toface interview and were followed longitudinally by phone every 3 months for 2 years as part the Chicago Initiative to Raise Asthma Health Equity (CHIRAH) study. Health literacy was measured using the Rapid Estimate of Adult Literacy in Medicine (REALM) and data regarding participant demographics, socioeconomics, and asthma (symptoms, limitation to activities, medication and urgent care use) were collected by self report at baseline. Asthma knowledge was assessed using an 11-item assessment developed for this study. Asthma control (well controlled vs. not well/poorly controlled) was classified based on NAEPP 2007 guidelines and the mini-Asthma Quality of Life Questionnaire (AQLQ) was used to measure asthma quality of life (AQoL). We used a form of exploratory regression-based mediational analysis to examine the explanatory nature of health literacy and socioeconomic status in the association between race and longitudinal asthma related outcomes (knowledge, quality of life, and control) across 7 time points. Population Studied: 345 community dwelling adults (99 Latino, 198 African American, and 48 White) in Chicago with persistent asthma and complete baseline data were included in this analysis. Principal Findings: Rates of limited literacy differed significantly across the three racial groups: 31% Latinos, 38% African Americans, compared to 13% Whites (p=0.003). Controlling for age, gender, and duration of asthma, African American participants had less asthma knowledge (ß=-.66, 95% CI -1.02 to -0.29, p<.001) and lower asthma quality of life (ß=-.48, 95% CI -0.80 to -0.16, p=.003) than White participants. Literacy alone reduced these disparities by more than 30% for both outcomes (Knowledge ß=-.45, 95% CI -0.78 to -0.11, p=.01; AQoL ß=-.32, 95% CI -0.62 to -0.02, p=.04). The addition of SES reduced these differences further, to a point of non-significance. Differences in asthma knowledge and quality of life between Latino and White participants were partially explained by literacy and SES, but remained significant (Knowledge ß=-.61, 95% CI 0.99 to -0.23, p=.002; AQoL ß=-.31, 95% CI -0.59 to -0.03, p=.03). Ethnic disparities in asthma control were fully accounted for by literacy and SES across all racial groups (African American vs. White OR=1.08, 95% CI 0.61 to 1.92, p=.79; Latino vs. White OR=0.79, 95% CI 0.44 to 1.41, p=.42). Conclusions: Limited literacy was identified as a significant mediator to the relationship between race/ethnicity and all examined asthma outcomes. Socioeconomic indicators also explained these associations. Implications for Policy, Delivery or Practice: Efforts to reduce asthma disparities should consider health literacy promotion strategies as well as improving access and quality of care. Specifically, evidenced based patient education and counseling interventions are available that could mitigate the impact of literacy and thereby reduce inequities. Funding Source(s): NHLBI Poster Number: 163 The Effect of Patient-Physician Racial/Ethnic and Language Concordance on Quality of Diabetes Care Presented by: Lisa Diamond, M.D., M.P.H., Research Physician, Health Policy Research, Palo Alto Medical Foundation Research Institute, 795 El Camino Real, Ames Building, Palo Alto, CA 94301; Phone: (650) 853-3383; Email: diamondl@pamfri.org Co-authors: Sukyung Chung, Ph.D.; Latha Palaniappan, M.D., M.S.; Harold Luft, Ph.D. Research Objective: Diabetes mellitus (DM) and its complications are disproportionately higher in racial/ethnic (R/E) minority groups. Emerging evidence suggests that patient-physician R/E and language concordance may affect patient treatment and medication adherence. We examine whether R/E and language concordance affects DM quality measures in a diverse ambulatory health care system where all patients have similar access to health care, high quality providers, and interpreter services. We hypothesized that patient-physician R/E and language concordance has more effect on outcomes, rather than process measures, as the latter requires patient education and adherence. Study Design: Cross-sectional Population Studied: We linked data on patient and physician characteristics and DM quality measures from the Palo Alto Division of the Palo Alto Medical Foundation (PAMF), a large multi-specialty group practice in northern California. PAMF collects selfreported R/E and preferred language information at registration. R/E and language concordance was based on the primary care physician (PCP) assigned to the patient. All active patients in the DM registry (n=5,994) as of August 2009, matched with 168 PCPs were included. Multilevel random effects models took account of clustering within physicians while including patient (demographics, comorbidities, likelihood of seeing the same PCP, and insurance type) and physician (experience and DM panel size) factors. The quality indicators included four process measures (glycosylated hemoglobin (HbA1c) within 6 months, blood pressure (BP), LDL cholesterol, and foot examinations within one year) and four outcome measures (HbA1c<7% or <8%, target BP<130/80, and target LDL cholesterol = 100mg/dL). Principal Findings: Patients represent diverse R/E (45% non-Hispanic white (NHW), 27% Asian/Pacific Islander (API), 11% Hispanic/Latino, 5% Black/African American, and 12% other race) and preferred language (English 73%, Spanish 3%, Chinese 3%, 11% other). Physicians were also of diverse R/E (60% NHW, 36% API, and 4% Hispanic/Latino), with some non-English language proficiency (Spanish 23%, Chinese 14%), 22% other). Hispanic/Latino patients were least likely to have a R/E concordant PCP (2%), compared to API (14%) and NHW (32%) patients. Most (98%) of non-English speaking patients had a language discordant PCP. In multivariate analyses, there were significant differences in DM care by patient R/E: API patients were more likely to have had a foot exam (p<.001) and to achieve target BP (p<.01) and LDL (p<.01) compared to NHW patients. Black/African American patients were less likely to achieve target BP compared to NHW (p<.01), and Hispanic/Latino patients were less likely to have HbA1c<8% (p<.0001). Hispanic/ Latino patients with a R/E concordant PCP were more likely to have had their HbA1c checked (p<.01) and API patients with R/E concordant PCP were more likely to achieve a HbA1c<7% target (p=.02) compared to R/E discordant patients. Preferred language and language concordance were not significantly associated with any of the DM quality measures. Conclusions: R/E and patient-physician R/E concordance were associated with better performance on some DM quality measures. Neither language preference nor language concordance was associated with DM process or outcome measure achievement. Implications for Policy, Delivery or Practice: Disparities in DM care across R/E groups, even among insured patients with access to the same PCPs within an organization, suggest that we need a better understanding of how R/E and R/E concordance affect DM quality of care. Future interventions to address quality of DM care may seek to target R/E discordant patient-physician groups. Funding Source(s): The California Endowment Poster Number: 164 Use of Different Treatment Options by Rural Early Stage Prostate Cancer Patients Presented by: Mark Doescher, M.D., M.S.P.H., Director, Family Medicine, WWAMI Rural Health Research Center, University of Washington, 4311 11th Avenue NE, Suite 210, Seattle, WA 98105; Phone: (206) 685-0402; Email: mdoesche@uw.edu Lead Author: Laura-Mae Baldwin, M.D., M.P.H. Co-authors: Roger Rosenblatt, M.D., M.P.H.; Shilpen Patel, M.D.; Michael Porter, M.D., M.S.; Holly Andrilla, M.S. Research Objective: Maintaining the highest quality cancer care is inherently difficult in rural areas due to the paucity of cancer care specialists, diagnostic services, and therapeutic services. This study compares use of different treatment options between rural and urban prostate cancer patients to identify potential inequities in service access and treatment choice. Study Design: Retrospective cohort study using 2004-2006 data from rural and urban in 10 states with Surveillance, Epidemiology, and End Results (SEER) cancer registries. We compared unadjusted rates of different treatments between rural and urban cancer patients, and conducted logistic regression analysis to examine the odds of definitive treatment with recommended surgery or radiation therapy versus non-definitive treatment (active surveillance or non-standard surgical treatment) among rural and urban patients adjusting for sociodemographic (age, race/ethnicity, marital status), cancer (stage), and contextual characteristics (state). Population Studied: 78,874 urban and 10,638 rural prostate cancer patients ages 18 and older with clinical T1c and T2 stage disease. Principal Findings: 70.3% rural and 73.4% urban patients (p=.000) received definitive treatment; 25.6% rural and 24.4% urban patients were in active surveillance (p=.005); 4.1% rural and 2.3% (p=.000) urban patients received non-standard surgical treatment only (local tumor destruction/excision, simple prostatectomy). Of patients with definitive treatment (n=62,397), 47.9% rural and 50.0% urban patients (p=.001) were treated with radical prostatectomy; 33.6% rural and 34.0% urban (p=.45) with external beam radiation; and 18.5% rural and 16.0% urban (p=.000) with radioactive pellet implantation. The adjusted odds of urban patients receiving definitive therapy was 1.31 (CI 1.23-1.39) times that of rural patients. Conclusions: Rural patients are significantly less likely to receive definitive treatment for early stage prostate cancer and are significantly more likely to receive non-standard, less comprehensive surgical treatments and to be in active surveillance. When they do receive definitive treatment, it is more likely to be a one-time radioactive pellet treatment. Taken together, these findings suggest that rural prostate cancer patients may make treatment decisions based on logistical factors such as geographic barriers or limited capacity. Implications for Policy, Delivery or Practice: These findings, combined with results from further studies designed to understand how rural patients learn about and choose their prostate cancer treatments, will elucidate whether these patients have difficulties accessing their preferred cancer services, and why. With this information, interventions at the level of physician practice and service delivery can be developed to alleviate ruralurban disparities in cancer service. Funding Source(s): HRSA Poster Number: 165 Does Residential Sprawl Contribute to Women's Risk of CHD? Presented by: Christine Eibner, Ph.D., economist, Economics and Statistics, RAND Corporation, 1200 S. Hayes Street, Arlington, VA 22202; Phone: (703) 413-1100 ext. 5913; Email: eibner@rand.org Co-authors: Beth Ann Griffin, Ph.D.; Chloe E. Bird, Ph.D.; Regina A. Shih, Ph.D.; Mary Ellen Slaughter, M.S.; Jose J. Escarce, M.D., Ph.D. Research Objective: We assessed the relationship between metropolitan statistical area (MSA) level urban sprawl and incident coronary heart disease (CHD) among women, adjusting for individual sociodemographic characteristics, baseline health status and health behaviors. Study Design: We used 2-level hierarchical Cox proportional hazard models (e.g. shared frailty models) to analyze the Women’s Health Initiative Clinical Trial (WHI CT) data, merged with a continuous measure of MSA-level sprawl developed by Ewing and colleagues. Participants were ages 50-79 at baseline, recruited at 40 clinical centers and 36 satellite locations, enrolled between 1993 and 1998, and followed until March 2005. We examined 3 outcomes: time until first CHD event (myocardial infarction (MI), revascularization, and hospitalized angina), time until CHD death or first MI, and time until CHD death. The urban sprawl index captured residential density, mixed land use, the concentration of development within the central city, and street connectivity for 83 MSAs. Population Studied: The sample (n=44,418, after limiting to WHI CT women living in MSAs with sprawl data) was 79.5% non-Hispanic white, 11.3% non-Hispanic black, 4.5% Hispanic, and 4.7% other; 60.0% were married at baseline, 94.6% had at least a high school education, and 65.9% had household incomes between $20,000 and $75,000 (categories ranged from <$10,000 to =$150,000). Although restricting the WHI CT (n=68,132) to women in MSAs with sprawl data reduced sample size, demographic characteristics were similar in the full and restricted samples. Principal Findings: After controlling for individuallevel sociodemographic characteristics including age, race, education, income, martial status, region, family history of MI, and study arm as well as baseline health measures (BMI, waist hip ratio, physical activity, self-reported history of diabetes, hyperlipidemic medication use and/or self-reported high cholesterol, hypertension) and health behaviors (smoking, alcohol use, hormone use), we found that women residing in sprawling MSAs experienced shorter time to first CHD event or time to CHD death or MI. Living in an area with less urban sprawl was associated with decreased risk of a first CHD event and CHD death or MI (HR = 0.95 per standard deviation increase in the Ewing index, 95% CI = 0.91-0.99; HR = 0.91, 95% CI = 0.860.97, respectively). When we examined the four components of sprawl individually, residential density had the most pronouced effect. Living in a higher residential density MSA was associated with a decreased risk of CHD event (HR = 0.94, 95% CI = 0.91-0.97) and CHD death or MI (HR = 0.90, 95% CI = 0.86-0.95). Conclusions: Urban sprawl was independently associated with greater CHD risk, above and beyond individual-level baseline characteristics. The index’s residential density component had the most noteworthy independent effect, suggesting that a beneficial effect of population may explain the findings, which held even after adjusting for neighborhood SES. Implications for Policy, Delivery or Practice: Our findings suggest that land use and development patterns in urban areas may influence cardiovascular disease risk. Due to their increased risk of CHD events, screening and prevention efforts may need to be more aggressive for women living in areas with greater sprawl. Funding Source(s): National Heart, Lung, and Blood Institute Poster Number: 166 Rural – Urban Disparity in Colon Cancer Screening among Elder Medicare Beneficiaries: Does Rurality Matter? Presented by: Lin Fan, M.S., Student, Community and Preventive Medicine, University of Rochester, 601 elmwood Avenue, Rochester, NY 14642; Phone: (585) 705-7534; Email: lin_fan@urmc.rochester.edu Co-authors: Katia, Noyes, Ph.D.; Supriya, Mohile, M.D., M.S. Research Objective: To examine urban-rural disparity of Colorectal cancer (CRC) screening among the elder Medicare beneficiaries and assess rurality’s independent impact on receipt of CRC screening. Study Design: Cross sectional study. We included community dwelling Medicare beneficiaries 65 years of age and older from 2005 Medicare Current Beneficiary Survey (N=11,488). Rural-Urban Commuting Area Codes (RUCAs) were used to characterize 4 types of rural and urban status. Selfreported time-appropriate CRC screening practice (fecal occult blood test [FOBT] last year or colonoscopy / sigmiodoscopy in past 5 years), FOBT in past 2 years, and colonoscopy / sigmiodoscopy in past 5 years were compared among the 4 types of urban and rural areas; independent impact of rurality on receipt of screening was evaluated using weighted logistic regression. Population Studied: Community dwelling Medicare beneficiaries 65 years of age and older Principal Findings: Residents of urban areas were significantly more likely to receive time-appropriate screening (55.5% [95% CI: 53.7% - 57.2%] of urban beneficiaries, 50.1% [95% CI: 45.2% - 54.9%] of those from large rural / town, 47.5% [95% CI: 43.0% - 52.0%] from small rural / town, and 42.7% [95% CI: 38.3% - 47.0%] from isolated rural / town , P<0.0001). Similar patterns were observed for FOBT in past 2 years and colonoscopy / sigmiodoscopy in past 5 years. After controlling for age, gender, race, income, education, health insurance, HMO, health status, and health conditions, rurality was still significantly associated with time appropriate screening (P<.0001), FOBT in past 2 years, and colonoscopy / sigmiodoscopy in past 5 years. Conclusions: CRC screening is less than satisfactory, and about half of the elder Medicare beneficiaries do not receive time-appropriate CRC screening. There is evidence of urban-rural disparity in CRC screening among elderly Medicare beneficiaries. Implications for Policy, Delivery or Practice: Special attention should be paid to rural areas, particular small and isolated rural / towns to increase CRC screening practice. Further research is needed to understand the reasons for the urbanrural disparity to better inform policy intervention. Poster Number: 167 Residential Segregation and the Availability of Primary Care Physicians Presented by: Darrell Gaskin, Ph.D., Associate Professor, African American Studies, University of Maryland, 2169 Lefrak Hall, College Park, MD 20742; Phone: (301) 405-1162; Email: dgaskin@aasp.umd.edu Co-authors: Gniesha Dinwiddie, Ph.D.; Kitty Chan, Ph.D.; Rachael McCleary, B.A. Research Objective: To examine the association between residential segregation and geographic access to primary care physicians. Study Design: Using data from the 2006 American Medical Association master file and the 2000 Census, we computed the population to primary care physician (PCP) ratio for each zip code in a metropolitan statistical area (MSA). We defined PCP shortage areas as those zip codes with no PCP or a population to PCP ratio of greater than 3500. We excluded zip codes with populations of less than 200 persons. Using logistic regression analysis we estimated the association between whether a zip code was a PCP shortage area and the minority composition of the zip code and degree of segregated in the zip code’s MSA. Minority composition was measured by a set of indicator variables that denoted whether the zip code was predominately (50% or more) African American, predominately Hispanic, or predominately Asian. We used the Census Bureau’s MSA measures of segregation. Five segregation measures for each minority group were considered: dissimilarity index, isolation index, spatial/clustering index, centralization index and concentration index. In the logistic regression, we controlled for distribution of the population by age, gender, poverty status, education attainment, and home ownership in the zip code. We also controlled for clustering within county. Population Studied: Our sample consists of 15,900 zip codes located partially or completely in an MSA or which 15801 have segregation data for each minority group. Of these zip codes, 4.9% were predominately African American, 4.4% were predominately Hispanic, and 0.2% were predominately Asian. Principal Findings: Overall we found that predominately African American zip codes were more likely to be a PCP shortage area (OR = 1.65 p = 0.001). However, this relationship varies with the degree of segregation in the MSA. As segregation measured by the dissimilarity index, centralization index and concentration index increased the odds of being a PCP shortage area increased for African American zip codes. The odd ratios for low segregation area ranged from 0.96 to 1.23 compared to high segregation areas which ranged from 2.16 to 2.70. We found that when the clustering index for Asian was included in the model, the predominately Asian zip codes in low segregation areas were more likely to be PCP shortage areas (OR=3.43) compared to high segregation areas (OR = 0.93). We did not find an association between predominately Hispanic zip codes and PCP shortage areas. Conclusions: African American communities in highly segregated MSAs and Asian communities in low segregated MSAs are at risk of having too few PCPs. Implications for Policy, Delivery or Practice: Efforts should be made to improve geographic access to PCPs in African American communities in segregated MSAs and Asian communities in low segregated MSAs. Future studies should assess whether limited geographic access to PCPs in these predominately African American and Asian communities contribute to race disparities in the use of PCP services. Funding Source(s): NCMHD Poster Number: 168 Residential Segregation, Physician Shortage and the Use of Primary Care Services Presented by: Darrell Gaskin, Ph.D., Associate Professor, African American Studies, University of Maryland, 2169 Lefrak Hall, College Park, MD 20742; Phone: (301) 405-1162; Email: dgaskin@aasp.umd.edu Co-authors: Gniesha Dinwiddie, Ph.D.; Kitty Chan, Ph.D.; Rachael McCleary, B.A.; Thomas LaVeist, Ph.D. Research Objective: Do residential segregation and physician availability explain disparities in the use of primary care services. Study Design: Using data from the 2006 Medical Expenditure Panel Survey, the 2000 Census and the 2006 American Medical Association master file, we determined whether race/ethnic disparities in primary care service use were associated with residential segregation and the availability primary care physician (PCP). We used 5 measures of primary care service use: 1) office based physician visits, outpatient department physician visits, office based non-physician visits, outpatient department non-physician visits, and having a usual source of care (USC). At the individual level we controlled for age, gender, marital status, insurance status, educational attainment, employment status, region, and health status. We linked to the MEPS data, 6 measures of residential segregations: the minority composition of the zip code and 5 MSA measures of segregation for each minority group. Minority composition was measured by a set of indicator variables that denoted whether the zip code was predominately (50% or more) African American, predominately Hispanic, or predominately Asian. The five segregation measures for each minority group were the dissimilarity index, isolation index, spatial/clustering index, centralization index and concentration index. To measure PCP availability, we computed the population to primary care physician (PCP) ratio for the zip code. We defined PCP shortage areas as those zip codes with no PCP or a population to PCP ratio of greater than 3500. We estimated logistic and negative binomial regression analyses assuming primary care use has two parts: initiation and subsequent use. We estimated a base model using on the MEPS data, and then models using each of the segregation and physician availability variables separately. Population Studied: We restricted are our sample to 20775 adults living in MSAs. Principal Findings: Preliminary findings suggest that disparities in primary care use were associated with residential segregation and PCP availability especially for non-physician services. The impact varies by segregation measure and by race/ethnic minority group. Conclusions: African Americans and Hispanics who are exposed to segregation are less likely to use primary care services. Asians in segregation areas are more likely to use primary care services. Implications for Policy, Delivery or Practice: Efforts should be made in improve access to primary care physician services in African American and Hispanic communities in segregated areas. Funding Source(s): NCMHD Poster Number: 169 Patient Navigation Utilization among Native American Cancer Patients in the Northern Plains Presented by: B. Ashleigh Guadagnolo, M.D., M.P.H., Assistant Professor, Radiation Oncology, The University of Texas M.D. Anderson Cancer Center, 1515 Holcombe Boulevard, Unit 97, Houston, TX US 77030; Phone: (713) 563-2341; Email: aguadagnolo@gmail.com Co-authors: Michelle Sargent, R.N.; Amy Boylan, R.N.; David Koop, R.N.; Kevin Molloy, R.N.; Daniel Petereit, M.D. Research Objective: Native Americans (NA) in the Northern Plains suffer disparately high cancer mortality rates compared with the general US population and NA in other regions. We developed a culturally-specific patient navigation (PN) program as a component of a multi-faceted effort to reduce cancer-related health disparities in this region. While studies of PN for assisting patients through the cancer screening/diagnosis process are available, relatively little published data exists regarding PN for patients undergoing cancer therapy. Our goal was assess relative intensity of PN utilization for different courses of therapy. Study Design: This is a prospective cohort study to evaluate PN utilization among NA cancer patients. The PN program (Walking Forward Program) provides culturally-competent navigators to assist patients with navigating cancer therapy, obtaining medications, insurance issues, communicating with medical providers, and travel and lodging logistics. Navigators included trained lay health workers (both NA and non-NA) as well as individuals with formal health care training (e.g., R.N.). Lakota language services and educational materials were available. All patients received PN throughout cancer treatment. Additionally, community navigators live and work on the reservations providing an embedded resource for cancer patients returning to their reservation communities following cancer treatment. The non-parametric Mann-Whitney test was used to test for differences between mean number of hospital-based navigator encounters for subgroups of patients receiving various cancer treatment regimens. Population Studied: Hospital-based recruitment of 332 NA cancer patients in Rapid City, SD who received PN services throughout cancer treatment between 2/2004 and 9/2009. Principal Findings: The median participant age was 60 years (range, 16-89 years). Median distance lived from the cancer center was 121 miles (range, 10-444 miles). The majority of patients were referred for PN for financial assistance (54%) or logistical support (35%). Other reasons included (> 1 reason possible): psycho-social support (35%), care coordination (22%), advocacy (20%), or education (20%). The median number of contacts with a navigator was 12 (range, 1-119). Median time spent with the navigator at first contact was 40 minutes (range 10-250 min.) and 20 min for subsequent contacts. Patients undergoing radiation therapy (RT) had more contacts with a navigator than those not receiving RT (mean, 25 vs. 13 contacts, respectively; p=0.0001), as did those receiving chemotherapy vs. those who did not (mean, 24 vs. 15 contacts, respectively; p=0.001). Patients who received both chemotherapy and RT also had more encounters with a navigator than those not receiving both modalities (mean, 30 vs. 16 contacts, respectively; p=0.0001). Patients undergoing curative treatment had an average of 21 contacts with a navigator compared to 17 contacts for patients receiving palliative treatment (p=0.02). Conclusions: NA patients who received more intensive cancer care sought more PN services. The primary reasons for accessing PN services included financial assistance and travel/lodging support. Implications for Policy, Delivery or Practice: These data may have implications for resource allocation for PN in vulnerable populations receiving intense or complicated treatment regimens. Research is needed as to whether PN improves treatment adherence, outcomes, and quality of life. Funding Source(s): NCI Poster Number: 170 Disparities in Receipt of Supportive/Palliative Care Services among Individuals with Lung Cancer Presented by: Michael Halpern, M.D., Ph.D., Senior Fellow, Health Services and Social Policy Research, RTI International, 701 13th Street NW, # 750, Washington, DC 20005; Phone: (202) 9747813; Email: mhalpern@rti.org Co-authors: Debra Holden, Ph.D.; Anne Larsen, M.S. Research Objective: Increased eM.P.H.asis is being placed on patient-centered care, particularly for individuals with serious medical conditions. For individuals diagnosed with cancer, patient-centered care involves addressing all symptoms, including those caused by the underlying disease or by cancer treatments. However, reports suggest disparities in receipt of care for symptoms such as pain, decreased levels of functioning, and psychological distress among individuals with cancer. We conducted this study to explore disparities in receipt of supportive/palliative care services among an insured elderly population with lung cancer. Study Design: We used data from NCI’s Surveillance, Epidemiology and End Results (SEER) cancer registry linked to Medicare claims data (SEER-Medicare) to assess disparities in receipt of pain management, physical/occupational therapy (PT), psychological/psychiatric testing or treatment services during the first 12 months after diagnosis. Separate multivariate logistic regressions were performed to assess disparities based on patient sociodemographic and clinical factors on the receipt of each category of supportive/palliative care services. Regressions controlled for cancer stage; age at diagnosis; sex; race/ethnicity; rural/urban residence; dual Medicare-Medicaid enrollment (a proxy for low income status); comorbidities; and area-based socioeconomic status indicators. Population Studied: All individuals in the SEER registry with a lung cancer diagnosis continuously enrolled in Medicare parts A and B for at least 12 month following diagnosis were included. Principal Findings: Among 33,186 individuals with lung cancer, Black patients were significantly less likely to receive pain management services or psychological treatment compared with White patients. Women were more likely than men to receive PT and psychological testing or treatment. Older patients were more likely to receive PT or psychological testing, but less likely to receive pain management or psychological treatment compared with younger patients. Patients with dual MedicareMedicaid coverage were less likely to receive pain management than were non-duals, but more likely to receive PT and psychological testing and treatment. Individuals with multiple comorbidities were more likely to receive all of the supportive/palliative care services examined. Patients from areas with higher rates of adults having only a high school education were significantly less likely to receive pain management or PT. Those from areas with high rates of nonEnglish speakers were also less likely to receive pain management services, but were more likely to receive psychological testing. Conclusions: Significant disparities were observed in receipt of supportive and palliative care services among an elderly, insured population with lung cancer. Disparities based on patient sociodemographic characteristics were observed despite controlling for clinical characteristics such as cancer stage and level of comorbidities. Implications for Policy, Delivery or Practice: From these data, we cannot determine whether these observed disparities are related to differences in patient preference, clinician practice patterns, type of health care facility where treatment is received, and/or other factors. Further research is needed to understand the basis for these disparities. In particular, studies need to examine the effects of patient preference and recommendations or referrals for supportive/palliative care services by clinicians on receipt of these services. Poster Number: 171 Massachusetts Health Reform and Use of ReferralSensitive Inpatient Procedures Presented by: Amresh Hanchate, Ph.D., Research Assistant Professor, General Internal Medicine, Boston University School of Medicine, 801 Massachusetts Avenue, #2077, Boston, MA 02118; Phone: (617) 638-8889; Email: hanchate@bu.edu Co-authors: Karen Lasser, M.D., M.P.H.; Alok Kapoor, M.D., M.P.H.; Danny McMormick, M.D., M.P.H.; Meredith Manze, M.P.H.; Nancy Kressin, Ph.D. Research Objective: Massachusetts (MA) is the setting of a landmark experiment in health care reform that has sharply expanded health coverage since its inception in 2006. In the absence of any previous research, our objective is to examine whether expanded insurance coverage has improved access to selected major inpatient procedures (total knee replacement (TKR), percutaneous transluminal coronary angioplasty (PTCA), coronary artery bypass graft (CABG) and total/partial hip replacement (THR)) that are typically underutilized by minority patients. Study Design: We analyzed MA Hospital Inpatient Discharge Data on all non-federal MA hospital discharges from 2004-2008 (fiscal years) for 2,656,554 white patients, 195,481 black patients, and 172,852 Hispanic patients. State-level annual counts of individual procedures were stratified by county, sex, race/ethnicity and age (21-44, 45-54 and 55-64), resulting in n=1,320 observational units after combining the five years of longitudinal data. To convert procedure counts into incidence rates (number of procedures/10,000 population), we obtained Census population data to create an ‘exposed population measure’ for each observational unit. We used direct standardization and hierarchical negative binomial regression models to estimate changes in the use of procedures over two years following the onset of reform. We used the Wald test to estimate differences in utilization rates among black and Hispanic non-elderly adults (age 21-64) compared to their white counterparts. To separate the impact of health reform from secular temporal effects that may also effect untargeted population, we use a difference-in-difference approach contrasting the pre/post change with those among patients >= age 65, assuming they have continuous Medicare coverage. Population Studied: MA-residing patients discharged from MA hospitals during 2004-2008 for the following surgical procedures: TKR (n=53,633), PTCA (n=60,475), CABG (n=16,701) and THR (n=42,991). Principal Findings: Between 2006 and 2008, total state-level volumes increased for TKR (+22%) and THR (+7%), and decreased for PTCA (-15%) and CABG (-8%). While there was a secular increase in TKR and THR incidence rates between 2004-2006 (pre-reform) and 2008 (post-reform), the increases were larger for blacks (TKR=53% THR=13%; all pvalues<0.05) and Hispanics (TKR=44%; THA=8% p-values>0.05) than for whites (TKR=24%; THR=8%). While there was a decrease in PTCA incidence rates, the decreases for blacks (17%) were smaller than that for whites (22%; p values <0.05). For CABG, the decrease in incidence rate was of similar magnitude across the three cohorts. While similar changes in rates for minorities were found among the elderly, their magnitude was generally smaller; for instance, the increase in incidence of joint replacement procedures for nonelderly minorities was larger than that for elderly. Conclusions: Following health reform, there has been a larger increase (or smaller decrease) in the use of some common inpatient procedures among minority non-elderly adults in MA. We will further examine if utilization differences are associated with geographical location and access to safety-net hospitals. Implications for Policy, Delivery or Practice: These preliminary findings indicate that insurance coverage expansion from the MA health reform may have increased utilization of procedures among racial and ethnic minorities due to pent-up demand. Funding Source(s): NIH/NINDS Poster Number: 172 Racial & Ethnic Disparities in Inpatient Outcomes for Ischemic Stroke Admissions: A Stratified Socioeconomic Status Approach Presented by: Amresh Hanchate, Ph.D., Research Assistant Professor, General Internal Medicine, Boston University School of Medicine, 801, Massachusetts Avenue, #2077, Boston, MA 02118; Email: hanchate@bu.edu Co-authors: Elaine Hylek, M.D.; Griffith Bell, M.Sc. Research Objective: Even though there are over half a million inpatient admissions for acute stroke in the US each year, little attention has been given to examining racial and ethnic disparities in their outcomes, especially adverse outcomes such as inpatient mortality and paralysis. This may partly be due to the fact that unadjusted inpatient mortality rates are lower for minorities compared to whites; given that minority stroke patients are relatively younger, it appears that these rates obscure large differences in risk factor profile by race and ethnicity. Adjusting for these differences, our objective is to quantify the extent of differences in adverse outcome rates by race and ethnicity. In particular, our focus is on these differences associated with poorer socioeconomic status among minorities. Such an investigation requires stratifying each racial and ethnic cohort by socioeconomic status and examining the immense diversity within each (racial/ethnic) cohort. Stratifying each cohort by median zip-code income, we estimate rates of three adverse outcomes for patients admitted for acute stroke -- inpatient mortality, paralysis and coma, and compare these rates across income strata within same racial/ethnic cohort. Study Design: Pooling the universe of inpatient discharge records from four states (Arizona, Massachusetts, Pennsylvania and Texas), we stratified all admissions for ischemic stroke for adults >= 45 years of age by sex, age (44-64, 6574, 75-84 and 85+), race/ethnicity (white, black, Hispanic and other) and zip-code median income (first quartile, second quartile, top two quartiles combined). Paralysis and coma were defined based on secondary diagnosis codes. Secondary diagnosis codes (ICD-9) were used to identify paralysis and coma, and to identify patient risk factors (including hypertension, heart failure and diabetes). Pooled multilevel logistic regression models were estimated to measure mean differences in outcomes across strata. Population Studied: All patients admitted with the principal diagnosis of ischemic stroke during 20052008 in all civilian hospitals in AZ (n=15,831), MA (n=16,438), PA (n=17, 958) and TX (n=20,066). Principal Findings: Unadjusted mean outcomes rates were 5.1% (inpatient mortality), 22.6 percent (paralysis) and 1.3 percent (coma). Confirming previous findings, unadjusted inpatient mortality was lowest for blacks (3.8%), followed by Hispanics (4.1%) and whites (5.4%). However, comparing the income gradients for inpatient mortality for the three racial and ethnic cohorts, the gradient for blacks is the steepest, followed by that for Hispanics. Among blacks, risk-adjusted inpatient mortality ranged from 2.7% among the highest income cohort to 4.5% among the poorest cohort (66 percent higher; p <0.01); the corresponding excess mortality was 52% among Hispanics and 31% among whites. Similar comparison for paralysis outcome indicated that the gradient for Hispanics was the steepest. No significant gradient was found for coma. Conclusions: Among minority patients admitted for ischemic stroke, those residing in poorer neighborhoods experienced worse outcomes (inpatient death and paralysis) than their counterparts living in higher-income neighborhoods; in comparison, this gap is narrower among white patients. Implications for Policy, Delivery or Practice: While mean rates of adverse inpatient outcomes for patients admitted for ischemic stroke are lower for minorities in general, compared to those for whites, they obscure substantial disparities associated with poorer socioeconomic status. One implication is that barriers to care may be potentially higher for poorer minorities when compared to those for poorer whites. Funding Source(s): NINDS Poster Number: 173 Factors Associated with Early Postpartum Depression Among Black and Latino Mothers Presented by: Elizabeth Howell, M.D., M.P.P., Assistant Professor, Health Evidence & Policy, Mount Sinai School of Medicine, One Gustave L. Levy Place, Box 1077, New York, NY 10029; Phone: (212) 659-9567; Email: elizabeth.howell@msnyuhealth.org Co-authors: Jason Wang, Ph.D.; Howard Leventhal, Ph.D. Research Objective: To assess the relationship between race, demographic factors, and clinical factors with early reported postpartum depression among Black and Latino mothers. Study Design: As part of a randomized controlled trial, enrolled mothers are interviewed at baseline during their postpartum hospital stay to assess depression, anxiety, and other factors. Depression is assessed using a validated depression screening instrument, the Edinburgh Postnatal Depression Scale. The associations of early postpartum depression with race, other demographic characteristics, past history of depression, and clinical factors were examined using bivariate and multivariable analyses. Population Studied: 460 self-identified Black and Latino postpartum women who had uncomplicated deliveries at an urban hospital. Eligible subjects are women >18 years of age, English or Spanish Speaking, had working telephones, and had infants whose birthweights were > 2500 grams and 5minute Apgar scores >6. The recruitment target for this randomized controlled trial is to enroll 530 Black and Latino mothers. Principal Findings: Mean age was 28 (range 1846); 66% of the sample were Latino and 34% were Black. Thirty-six percent were foreign born, 21% spoke Spanish, 62% had Medicaid insurance and 56% earned < $30,000 annually. Overall 15% screened positive for depression (EPDS score >10) and there were no racial/ethnic differences in rates of depression. Depression was more common in mothers born in the US than mothers born outside of the US (10% vs. 18%, p=.01), English speakers than Spanish speakers (17% vs. 8%), p=.02), single mothers as compared with married mothers (19% vs. 13%, p=.056), mothers with comorbid illness vs. mothers without comorbid illness (22% vs. 13%, p=.02), and mothers with a past history of depression as compared with mothers without a past history of depression (47% vs. 9%, p<.0001). Rates of depression did not differ by insurance status, delivery type, or presence or absence of antepartum complications. After adjusting for race, other demographic factors, past history of depression, delivery type, comorbid illness, and complication status, depression was more common in mothers with a past history of depression (OR of 8.21, 95% CI: 4.47, 15.08). Conclusions: Racial/ethnic differences in rates of reported postpartum depression did not exist among Black and Latino early postpartum mothers. Past history of depression in this low income population of mothers was the strongest correlate of early postpartum depression. Implications for Policy, Delivery or Practice: Further research is needed to assess the impact of early depression screening on the mental health outcomes of high risk women, particularly in Black and Latino communities. Funding Source(s): National Center for Minority Health and Health Disparities Poster Number: 174 How are Iraq/Afghanistan Veterans with Health Problems Faring in the Labor Market? Presented by: Jennifer Humensky, Ph.D., PostDoctoral Fellow, Center for Management of Complex Chronic Care, Edward Hines Jr VA Hospital, 5000 S. Fifth Avenue (151H), Building 1, B251, Hines, IL 60141; Phone: (708) 202-5863; Email: Jennifer.Humensky@va.gov Co-authors: Denise M. Hynes, Ph.D.; Neil Jordan, Ph.D.; Kevin Stroupe, Ph.D. Research Objective: Veterans returning from World War II and the Korean War generally fared well in the labor market following their service. However, this pattern was different for Vietnam veterans, who encountered more difficulties in the labor market. Previous research has shown that veterans in better health and those who learned skills more translatable to the private sector fared better in the job market. The popularity of specific wars has also been shown to affect re-entry into the job market. However, the labor market experience for Iraq/Afghanistan veterans is not wellunderstood. While the Iraq/Afghanistan wars are largely unpopular with the American public, support for the troops is high, thus the impact of any stigma is uncertain. Our research objective was to examine the labor market experience of Iraq/Afghanistan veterans, and then to examine whether labor market outcomes varied by health status, and whether this relationship has varied over time. Study Design: We used a multilevel, repeated observations model to identify a trajectory of labor market outcomes (participation in the labor force, probability of any earnings, and enrollment in school) for veterans in good and poor health. The empirical model was based on the Ownsworth and McKenna (2004) model of labor market participation of persons with traumatic injuries, and controlled for a variety of individual and contextual characteristics associated with labor market outcomes, including demographics, education level, previous military service, locality, and state unemployment rate. Population Studied: We analyzed the most recent three panels from the March Current Population Survey (CPS): 2006-2007, 2007-2008 and 20082009. Information on service in Iraq/Afghanistan was not available in CPS prior to 2006. The 20082009 cohort included 125,623 persons age 18-65; about 925 were Iraq/Afghanistan veterans. Of the Iraq/Afghanistan veterans, about 86% were in the labor force, about 89% had earnings and about 5% were enrolled in school. Principal Findings: Iraq/Afghanistan veterans in good health had similar employment outcomes to non-veterans. No statistically significant differences were found between veterans and non-veterans in good health in 2009 in labor force participation and probability of any earnings. Veterans were less likely to be enrolled in school (ß=-0.06, p<0.01) than non-veterans. However, veterans in fair or poor health in 2009 had lower odds of labor force participation (OR=0.11, p<0.01), and any earnings (OR=0.74, p<0.01), compared to veterans in good health. Results were generally consistent from 2006-2009. Conclusions: Although Iraq/Afghanistan veterans in good health have been doing well in the labor market, veterans in fair or poor health have been encountering more difficulties. Persons in poor health generally perform less well in the labor market, and this holds true for veterans. More research is needed to determine which health problems are associated with employment problems and whether participation in specific treatment programs results in better outcomes. Implications for Policy, Delivery or Practice: Returning veterans with health problems may be especially vulnerable to employment difficulties. The Veterans Administration and other veteran service organizations should consider targeted approaches to help veterans succeed in the labor market. Poster Number: 175 The Impact of Race and Hospital Racial Makeup on Readmissions for Heart Failure Presented by: Karen Joynt, Fellow, Health Policy and Management, Harvard School of Public Health, 677 Huntington Avenue, Boston, MA 02115; Phone: (617) 432-5551; Email: kjoynt@partners.org Co-authors: Ashish K. Jha, M.D., M.P.H. Research Objective: Reducing readmissions for patients admitted with heart failure (HF) is a major policy initiative, partly driven by the fact that HF is the most common cause of hospitalizations and readmissions in the Medicare program. Prior studies have suggested that blacks may have higher readmission rates than white patients, yet the reason for this disparity is not well understood. We sought to determine whether location of care plays an important role in racial disparities. Study Design: We used Medicare claims data from 2006-2007 to categorize hospitals based on the proportion of black patients they cared for, designating those hospitals in the top decile as “minority-serving.” We created risk-adjusted generalized linear regression models, accounting for clustering within hospitals, with patient race and hospital racial makeup as our primary predictors, and 30-day readmission as our primary outcome. Population Studied: 699,450 Medicare patients with a primary discharge diagnosis of HF. Principal Findings: In analyses fully adjusted for patient characteristics, black patients had higher 30-day readmission rates (24.4% versus 23.7%, p<0.0001) than white patients, but this difference disappeared after accounting for where black patients received their care: adjusting for whether blacks were admitted to minority-serving hospitals or not, we found no racial difference in readmission rates (25.0% for black patients versus 24.7% for white patients, p=0.15). Risk-adjusted 30-day readmission rates were higher at minority-serving hospitals overall (26.0%) than at non-minorityserving hospitals (23.6%, p<0.0001), and this difference was consistent after controlling for race (26.0% versus 23.7%, p<0.0001). At minorityserving hospitals, black patients had a slightly higher 30-day readmission rate than white patients (26.6% versus 25.6%,p=0.004). However, there were no disparities in readmission rates at nonminority-serving hospitals: both black and white patients had identical 30-day admission rates, at23.5% (p=0.96). Conclusions: We found that elderly black patients in the U.S. overall have higher 30-day readmission rates than white patients. However, this effect disappeared when taking into account the hospitals where black patients receive a large proportion of their care: minority-serving hospitals had significantly higher readmission rates, and accounting for the location in which patients sought care explained most of the national disparity in readmission rates. In fact, black patients at nonminority-serving hospitals had significantly lower admission rates than white patients at minorityserving hospitals. Implications for Policy, Delivery or Practice: Racial disparities in HF outcomes seem to be primarily a systems problem – the hospital at which a patient seeks care, and not patient race, is the primary driver of racial disparities in readmission. These findings suggest that focusing on quality improvement at poor-performing, minority-serving hospitals may have the potential to improve quality of care for all HF patients while simultaneously reducing disparities in HF care. Funding Source(s): NIH Training Grant Poster Number: 176 Exploring Cultural Sensitivity in the National Drug Abuse Treatment System Survey Presented by: Mimi Kim, Ph.D., Investigator, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 725 Martin Luther King Jr. Boulevard, CB#7590, Chapel Hill, NC 27599-7590; Phone: (919) 843-6883; Email: mimi@unc.edu Co-authors: Daniel L. Howard, Ph.D.; Paul Godley, M.D., Ph.D., M.P.P. Research Objective: Evidence suggests that one of the most effective strategies for addressing the racial disparities in substance abuse treatment is to provide services in a culturally sensitive manner yet defining cultural sensitivity remains complicated. A limited amount of research has suggested the importance of client-provider ethnic matching as one dimension of cultural sensitivity that could be effective in the delivery of health services. Cultural sensitivity is one way for organizations to promote better outcomes for the repeat clients, many of whom are minorities, they treat. Despite the apparent outcome advantage to providing culturally sensitive services in treatment, little research has gone further to examine other service characteristics that may define culturally sensitive treatment. This analysis assesses the extent to which service and organizational level variables predict cultural sensitivity, as defined by a clientprovider ethnic matching in addition to cultural sensitivity, over time in outpatient substance abuse treatment (OSAT) units. Study Design: The data were collected for the 1995 and 2005 National Drug Abuse Treatment System Survey (NDATSS) data set. Repeated measure models examined the relationship of cultural sensitivity over time to several service, organizational, and client characteristics variables. Population Studied: The unit of analysis was a physical facility with resources dedicated primarily to treating individuals with substance abuse problems on an ambulatory basis. Principal Findings: In the multivariable analysis final models, results indicate that OSAT units with smaller client/staff ratios, affiliations with hospitals, clients who are younger than 50 years of age, and a higher percentage of dually diagnosed clients are more likely to be culturally sensitive. Conclusions: Focusing on service provision and organizational characteristics that positively predict cultural sensitivity can inform various ways to foster and develop culturally sensitive treatment practices and longer, more positive client outcomes. Implications for Policy, Delivery or Practice: These findings are significant for several reasons. First, this analysis uses a nationally-representative sample and thus the data are particularly useful for understanding the OSAT system as a whole. Second, because the study uses a split-panel design, this analysis examines changes in the nation’s outpatient drug abuse treatment system over time as well as providing an accurate picture of the system (i.e., as a result of adding treatment units to the sample at each wave of data collection). Third, this analysis is examining treatment practices that have a potentially significant empirical relationship to specific treatment outcomes and the long-term well-being of an underserved population. Therefore, examining specific treatment characteristics as they relate to specific treatment outcomes can aid researchers, policymakers, and clinical managers to examine the extent to which their treatment system is meeting clients’ needs and where the strengths and weaknesses of the system may lie. Finally, this analysis examines organizational characteristics that may be associated with changes and variation in treatment practices that significantly impact long-terms outcomes in the client population. By looking at these associations, this analysis identifies specific characteristics that contribute to a treatment units’ ability to establish longer, more positive client outcomes or areas of improvement related to positive outcomes. Funding Source(s): NCMHD Poster Number: 177 Predicting Glaucoma Diagnosis in an Elderly Sample: Revisiting the Established Populations for Epidemiologic Studies of the Elderly Study Presented by: Mimi Kim, Ph.D., Investigator, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 725 Martin Luther King Jr. Boulevard, CB#7590, Chapel Hill, NC 27599-7590; Phone: (919) 843-6883; Email: mimi@unc.edu Lead Author: Daniel Howard, Ph.D. Research Objective: The prevalence of vision impairment and blindness are higher among older individuals in the United States. Furthermore, African-Americans are twice as likely to be blind or visually impaired compared to their Caucasian counterparts. There is also evidence of several potential risk factors associated with vision loss in addition to or independent of natural aging. Research has found a wide range in the prevalence of vision impairment among different racial groups. Though research has examined race as an important factor in defining the scope of glaucoma in the United States, further exploration into other specific factors may help inform the design of preventive services to decrease rates of blindness due to glaucoma among minority groups. There remains an underreporting of individual and service factors that may predict glaucoma diagnosis by race. This paper intends to further analyze the association between glaucoma diagnosis and several other covariates, including service level factors, with particular attention to race among the EPESE participants. Study Design: This analysis employed generalized estimating equations (GEE) to simultaneously test for trends across time for each of the demographic, health characteristics, health services, and healthcare provider characteristic domains according to each racial group using a logistic link function in the GEE analysis. Population Studied: This observational, longitudinal study is based on participants from the North Carolina Established Populations for the Epidemiologic Studies of the Elderly (NC EPESE). Principal Findings: When controlling for patient health characteristics for both racial groups, having diabetes is a significant predictor for Caucasians and a marginally significant predictor for AfricanAmericans but in opposition between the two groups. Specifically, Caucasians without diabetes are more likely to have a glaucoma diagnosis. In contrast, having diabetes was a marginally significant predictor of a glaucoma diagnosis among African-American study participants. Also, the slightly higher number of women in the sample in relation to the prevalence of glaucoma suggests a possible association between gender and glaucoma as suggested by other research. Conclusions: These findings suggest that specific demographic, patient health characteristics, health provider characteristics, and the burden of disease may be important predictors of glaucoma diagnosis over time for African-Americans and should be further investigated. Furthermore, the finding for diabetes in the multivariable models suggests a potentially important physiological difference between the racial groups in relation to glaucoma. Implications for Policy, Delivery or Practice: The findings suggest that working Caucasians who have cataracts, but not diabetes, and are hesitant to see a doctor when necessary are more likely to have a glaucoma diagnosis. The diagnosis of cataract is common and this finding may represent an association with having a condition to seek eye care more than a true association between cataracts and glaucoma. Furthermore, glaucoma may be more likely in African-Americans who have cataracts with co-occurring diabetes and have been dissatisfied with the medical care they have received. In sum, this analysis provides individual-level characteristics and different service-level issues within different ethnic groups. These data may help to design studies to develop and test more precisely targeted interventions to improve a full range of healthcare services that are often needed by elderly patients. Funding Source(s): NCMHD Poster Number: 178 Examining Race and Depression among a Sample of Aging Medicaid Patients: A Longitudinal Analysis Presented by: Mimi Kim, Ph.D., Investigator, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 725 Martin Luther King Jr. Boulevard., CB#7590, Chapel Hill, NC 27599-7590; Phone: (919) 8436883; Email: mimi@unc.edu Lead Author: Daniel Howard, Ph.D. Co-authors: Mimi Kim, Ph.D.; Paul Godley, M.D., Ph.D., M.P.P. Research Objective: Research has shown that depression is associated with morbidity, mortality, decreased quality of life, increased medical costs, and the co-occurrence with a myriad of other diagnoses. Rates of depression for older, community dwelling adults have ranged between one-fourth to one-fifth percent. Service barriers in addition to low detection, misdiagnosis, and lack of treatment are particular concerns for older adults with depresion. Furthermore, due to the high needs of aging populations, depression is also often placed as a lower treatment priority for older adults, especially when coupled with such a high rate of physical health comorbidities. Yet, despite the prevalence of depression, its documented association to other chronic medical conditions, and the inarguable impact of socioeconomic conditions (e.g. race, income) on both physical and mental health status, there is a paucity of research that has examined depression among the aging and differences between races. This study explores what differences there are between AfricanAmericans and Caucasians in terms of major, mild, and other depression when controlling for other demographic and treatment variables. Study Design: Analyses for this study employed generalized estimating equations (GEE) to simultaneously test for trends across time for each of the demographic, geographic areas, types of mental health treatment, antidepressant drug class, and principal diagnosis domains across the three different depression categories using a logistic link function in the GEE analysis. Population Studied: This study used 2000 and 2004 Medicaid claims data from six states (Michigan, New Jersey, Florida, Georgia, Colorado and Washington). Participants were included according to the following criteria: 55 years or older; African-American or Caucasian; and at least one long term care Medicaid claim. Principal Findings: The three individual, multivariate logistic models look at predicting major depression, minor depression, and other depression. When looking at the results of the multivariable model for major depression, according to domains for the ease of discussion here, older African-American men who are not Medicare recipients are less likely to have a diagnosis of major depression. Similarly, older African-American men who are not Medicare recipients are also less likely to have a diagnosis of minor depression when controlling for all other variables in the model over time. But older African-American men who are not Medicare recipients are more likely to have a diagnosis of other depression. Conclusions: With such variability in severity of diagnosis comes the challenge of service providers to provide appropriate and patient-specific care for aging adults who face a myriad of psychosocial and physical challenges. Implications for Policy, Delivery or Practice: This analysis strives to provide a stepping stone from which future research can examine depression in order to contribute to treatment development for this high-need population. Considering the unique needs of individuals with varying levels of depression can help to tailor interventions to more effectively target the needs of aging individuals who are challenged in coping with their mental health needs. Funding Source(s): NCMHD Poster Number: 179 Perinatal Depression among Hispanic Women: Defining Depression and Treatment Preferences Presented by: Sandraluz Lara-Cinisomo, Ph.D., Assistant Professor, Child and Family Development, University of North Carolina, Charlotte, 9201 University City Boulevard, Charlotte, NC 28223; Phone: (704) 687-8179; Email: slaracin@uncc.edu Co-authors: Katherine Wisner, M.D.; Rachel Burns, M.P.H.; Diego Chavez-Gnecco, M.D. Research Objective: Perinatal depression is a significant mental health condition that may lead to serious health and mental health outcomes for mothers and their children (Weissman et al., 2004). There has been a growth in the number of studies examining treatment options for perinatal depression including the use of antidepressants and psychotherapy. However, most studies have focused primarily on white women (Gaynes et al., 2005). Given the expected rapid growth of the Hispanic community and the public health importance of treating depression, it is vital that we have a better understanding of how Hispanic women define depression and determine their depression treatment preferences if we are to effectively and appropriately treat Hispanic perinatal women suffering with depression. To address this need, we conducted a qualitative study with Hispanic perinatal women to gather information about their definition of depression, determine their treatment preferences and establish guidelines for implementing their preferred mental health treatments. Study Design: Focus group interviews were conducted with Hispanic perinatal women. A standardized interview protocol available in Spanish and English was used to guide the interviews. Five areas of inquiry guided the interviews: Defining depression and postpartum depression, Treatment Preferences, Barriers to Treatment, and Suggestions for treatment delivery. Qualitative data analyses were conducted with the focus group interview as the unit of analysis. Population Studied: Twenty-one prenatal and postpartum Hispanic women participated in focus group discussions. Principal Findings: Our analyses revealed that Hispanic women in our study define depression as a set of symptoms: crying, irritability and withdrawal. With regard to coping with these symptoms, the data revealed three primary approaches, including seeking social support from family, friends, distracting oneself (i.e., focusing on a specific task) and withdrawing from others. We also found a hierarchy of treatment preferences, with use of their own coping as the preferred approach followed by the use of social support, and third, but less desirable, was seeking help from a mental health profession. However, there were a lot of misconceptions about what a mental health provider can do to help. There were also a number of fears and noted risks associated with seeking professional mental health care, such as feeling pressured to take antidepressants or losing custody of their child. The use of antidepressants as a treatment option was not endorsed. However, participants said they would be more willing to take antidepressants after the birth of their child than during pregnancy and only if no other treatments were effective. Conclusions: Given the treatment preferences reported, it is important that health care providers and researchers ensure that perinatal depression interventions address the treatment preferences of the target population. Implications for Policy, Delivery or Practice: If we are to address the mental health needs of Hispanic perinatal women suffering with depression, it will be vital that we take great care in providing culturally appropriate health care services that meet the social and mental health needs of this population. Poster Number: 180 Racial/Ethnic Disparities in the Health and Healthcare of U.S. Adolescents: Has Anything Changed Over the Years? Presented by: Hua Lin, Ph.D., Biostatistical Consultant III, Department of Pediatrics, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390; Phone: (214) 648-5034; Email: hua.lin@utsouthwestern.edu Lead Author: May Lau, M.D., M.P.H. Co-authors: Rosa Avila, M.S.P.H.; Hua Lin, Ph.D.; Glenn Flores, M.D. Research Objective: Little is known about racial/ethnic disparities in health and healthcare of adolescents, and whether these disparities have changed over time. The goal of this study was to examine adolescent racial/ethnic disparities in medical and oral health, access to care, and use of services, and to determine whether these disparities changed from 2003-2007. Study Design: The National Survey of Children's Health (NSCH), sponsored by the Maternal and Child Health Bureau and conducted by the National Center for Health Statistics using the State and Local Area Integrated Telephone Survey mechanism, was a random-digit-dial telephone survey conducted in 2003 and 2007 on a nationally representative sample of households with children 0-17 years old. Disparities were examined for 40 measures of medical and oral health, access, and use of services for youth 10-17 years old. Bivariable and multivariable analyses were used to identify disparities in African-American, Latino, Asian/Pacific Islander, Native American, and multiracial youth, compared with white youth. Zscores were used to examine time trends from 2003 to 2007. Population Studied: A nationally representative sample from the 2003 and 2007 NSCH (n=48,741 and n=45,897, respectively) of US households of adolescents 10-17 years old at the time of the interview. Principal Findings: After adjusting for eight socioeconomic factors in multiple logistic regression analyses of the 2007 wave, persistent disparities were noted over time for one or more racial/ethnic minority groups. For example, minority adolescents were more likely to have the following: suboptimal medical and oral health, overweight/obesity, asthma, no health insurance, no personal doctor or nurse (PDN), insufficient time spent with the PDN, problems obtaining specialty care, and no specialty or mental health care in the past year. Compared with white youth in 2007, Latino, African-American, and multiracial youth had about double the odds of suboptimal medical and oral health, and Latinos, African-Americans, Native Americans, and multiracial youth had significantly greater odds of being uninsured and having no PDN. Certain disparities were especially prominent for specific racial/ethnic groups: for Latinos, having suboptimal medical health; for African-Americans, having suboptimal oral health, being overweight/obese, and having sporadic insurance; for Asian/Pacific Islanders, having no specialty and mental health care in the past year; and for Native Americans, having behavior problems, no medical insurance, no PDN, insufficient time spent with PDN, problems getting specialty care, and needing more medical care than others. Multiracial youth also had many disparities compared with white adolescents. Most racial/ethnic health and health care disparities persisted between 2003 to 2007, and two significantly worsened: problems obtaining specialty care in African-Americans, and ADHD in multiracial youth. Conclusions: US adolescents experience many racial/ethnic disparities in physical and oral health, access to care, and use of services. Almost all disparities persisted from 2003 to 2007, while some disparities worsened over time. Implications for Policy, Delivery or Practice: Results from this study may inform future research and policy on reducing adolescent racial/ethnic disparities in health and healthcare. Poster Number: 181 The Primary Language Spoken at Home and Health and Healthcare Disparities in U.S. Adolescents: Has the Tincture of Time Reduced Disparities? Presented by: Hua Lin, Ph.D., Biostatistical Consultant III, Department of Pediatrics, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390; Phone: (214) 648-5034; Email: hua.lin@utsouthwestern.edu Lead Author: May Lau, M.D., M.P.H. Co-authors: Rosa Avila, M.S.P.H.; Hua Lin, Ph.D.; Glenn Flores, M.D. Research Objective: Little is know about disparities and their trends over time in youth from non-English-primary-language (NEPL) homes compared with youth from English primarylanguage (EPL) homes, and even less is known about disparities among NEPL youth. The goal of this study was to examine disparities and their trends over time in medical and oral health, access to care, and use of health services in NEPL youth. Study Design: The National Survey of Children's Health, sponsored by the Maternal and Child Health Bureau and conducted by the National Center for Health Statistics using the State and Local Area Integrated Telephone Survey mechanism, was a random-digit-dial telephone survey conducted in 2003 and 2007 of households with children 0-17 years old. Bivariable and multivariable analyses were performed for all youth 10-17 years old to identify disparities in 40 measures of medical and oral health, access to care, and use of services. Among NEPL youth, sub-analyses compared Latinos, Asian/Pacific Islanders (APIs), and whites. Z-scores were used to analyze time trends in disparities from 2003-2007 (significance tested at a<.05). Population Studied: A nationally representative sample from the 2003 and 2007 NSCH (n=48,741 and n=45,897, respectively) of US households with adolescents 10-17 years old at the time of the interview. Principal Findings: In multivariable analyses adjusting for 8 sociodemographic factors, NEPL youth had significantly greater adjusted odds than EPL youth of having suboptimal medical and oral health status, no medical insurance, no personal doctor/nurse, and no specialist or routine preventive dental visit in the past year. In the sub-analysis for the 2007 wave, compared with NEPL white youth, NEPL Latinos had greater odds of having suboptimal medical (odds ratio [OR], 4.8; 95% confidence interval [CI], 2.5-9.9) and oral (OR, 2.4; 95% CI, 1.1-5.4) health, no medical insurance (OR, 2.7; 95% CI, 1.1-6.5,), and unmet dental care needs (OR, 16.2; 95% CI, 1.7-154.1). NEPL APIs had greater odds of no mental health visit in the past year (OR, 7.2; 95% CI, 1.4-36.3), and NEPL Latinos and APIs had greater odds of having no personal doctor/nurse (OR, 3.9; 95% CI, 1.5-10.1; OR, 5.7; 95% CI, 1.4-22.8) and no preventive dental care in the past year (OR, 4.7; 95% CI, 1.4-15.4; OR, 4.4; 95% CI, 1.2-16.1). Almost all disparities for NEPL youth (vs. EPL youth) persisted between 2003 and 2007. Two disparities significantly worsened: NEPL vs. EPL youth needing more medical care than others, and for NEPL Latinos vs. whites, having ADHD. Conclusions: NEPL youth experience multiple disparities in medical and oral health, access to care, and use of health services, and almost all disparities persisted over time. Compared with NEPL white youth, NEPL Latinos and APIs also face many disparities, most of which have continued over time. Implications for Policy, Delivery or Practice: Results of this study may help target policy to improve health and healthcare disparities in NEPL youth, including reducing language barriers for NEPL youth. Poster Number: 182 Promoting Access and Reducing Out-of-Pocket Prescription Drug Costs for Vulnerable Medicare Part D Patients Presented by: Helene Lipton, Ph.D., Professor, Institute for Health Policy Studies, University of California, San Francisco, 3333 California Street, Suite #265, San Francisco, CA 94118; Phone: (415) 476-2964; Email: smitha@pharmacy.ucsf.edu Co-authors: Amanda Smith, M.P.H.; Timothy Cutler, Pharm.D.; Marilyn Stebbins, Pharm.D. Research Objective: Given the complexity of the Medicare Part D prescription drug benefit and annual plan changes, many Medicare beneficiaries often lack knowledge and skills needed to select an optimal Part D plan. This problem is especially prevalent in vulnerable populations, where lack of resources and limited English proficiency are barriers to navigating the benefit effectively. Our objective was to reach these vulnerable populations and lower their annual out-of-pocket (OOP) prescription drug costs through one-on-one prescription drug plan counseling. Study Design: Students from seven California schools of pharmacy were trained in Part D to provide one-on-one counseling in multiple languages, under faculty supervision. Outreach events were conducted primarily during the Part D open enrollment period, which occurs each year between November 15 and December 31. Annual estimated OOP costs for each participant’s current prescription drug plan and the lowest-cost plan (if different) were obtained by entering their current medication regimen online, using the Medicare Prescription Drug Plan Finder tool. Prescription drug cost-related non-adherence behaviors also were identified through a questionnaire. Population Studied: Outreach was targeted toward vulnerable Medicare beneficiaries, defined as low-income individuals whose annual income is less than 300% of the Federal Poverty Level. Events were conducted in low-income clinics, housing complexes, community centers and other settings serving vulnerable Medicare patients. From October 2008 through December 2009, 90 outreach events were conducted and 1,552 beneficiaries received individualized Part D counseling. The majority of those counseled (80%, n=1,245) were identified as low-income, using the criterion specified above. Our study population of 1,029 is a subset of these low-income beneficiaries who were enrolled in a stand-alone prescription drug plan (as opposed to a Medicare Health Plan, which provides both medical care and prescription drug coverage). Principal Findings: Only 26% of the study population (n=243) were enrolled in the lowest-cost prescription drug plan. Based on counseling recommendations, 400 beneficiaries enrolled in a lower-cost Part D plan, going from a median plan cost of $354.75 to $124.50, for an average OOP cost-savings of 69%. Of the 1,029 beneficiaries, 949 (92%) were receiving additional governmental assistance with their prescription medication costs (i.e., Medicaid or the low-income subsidy (LIS)); 867 (84%) were from ethnic/racial minority groups; 624 (61%) had limited or no English proficiency; and 490 (48%) did not complete high school. In addition, 50 beneficiaries were identified as LISeligible and received assistance with their LIS applications during counseling. Of note, 304 (30%) beneficiaries reported prescription drug cost-related non-adherence behaviors during the last year, including not filling prescriptions due to cost and/or skipping doses. Conclusions: Evidence suggests that increases in out-of-pocket prescription drug costs lead to nonadherence behaviors with adverse health consequences. Our findings suggest that targeted outreach by trained pharmacy advocates can locate vulnerable patient populations in need of Part D counseling and successfully reduce their out-ofpocket prescription drug costs. Our data further show that the majority of vulnerable beneficiaries identified in this study is still struggling with medication costs and can maximize their benefit with targeted outreach by trained experts. Implications for Policy, Delivery or Practice: Vulnerable populations of Medicare beneficiaries are ill-equipped to navigate the complex Part D program alone. That so many are unable to realize the intended benefits of Part D suggests a gap in policy objectives and implementation. Our research suggests that policymakers can use targeted outreach programs to ensure that vulnerable populations have access to benefits offered and are not adversely affected by policy changes. Funding Source(s): The Amgen Foundation Poster Number: 183 Use of Outpatient Care in VA and Medicare among Disability-Eligible and Age-Eligible Veterans Presented by: Chuan-Fen Liu, Ph.D., M.P.H., Investigator, Health Services Research & Development, VA Puget Sound Health Care System, 1100 Olive Way, Suite 1400, Seattle, WA 98101; Phone: (206) 764-2587; Email: chuanfen.liu@va.gov Co-authors: Christopher Bryson, M.D., M.S.; Mark Perkins, Pharm.D.; Nancy Sharp, Ph.D.; Matthew Maciejewski, Ph.D. Research Objective: Prior research on Medicareeligible veterans has focused almost exclusively on age-eligible veterans, but veterans who are disability-eligible for Medicare represent a large and growing proportion of VA users. This study compares use of VA and Medicare outpatient services by veterans who are disability-eligible or age-eligible for Medicare. Study Design: This is a retrospective cohort study. We obtained information on primary care, specialty care, and mental health visits from 2001-2004 VA administrative datasets and Medicare claims. We examined differences between disability- and ageeligible veterans in primary care, specialty care, and mental health outpatient visits using generalized estimating equations. Population Studied: The study includes a cohort of 4,704 disability-eligible veterans and 10,816 ageeligible veterans who were VA primary care users and were also eligible for Medicare in FY2000. Principal Findings: A significant proportion of Medicare eligible veterans used Medicare for primary care and specialty care, but not mental health care. Disability-eligible veterans were less likely than age-eligible veterans to use Medicare services for primary care (30% vs. 40% in 2001, p<0.001) and specialty care (62% vs.73% in 2001, p<0.001), but not mental health care (6% vs. 2% in 2001, p<0.001). Similar patterns were observed in each year of the study period. Multivariate analysis results show that disability-eligible veterans had more VA visits for primary care (adjusted incidence rate ratio [aIRR]=1.11, p<0.001) and specialty care (aIRR=1.19, p<0.001), and more total (VA+Medicare) visits for primary care (aIRR=1.07, p<0.01) and specialty care (aIRR=1.07, p<0.01) than age-eligible veterans. Disability-eligible veterans were more likely than age-eligible veterans to have any VA mental health visit (odds ratio (OR)=1.71, p<0.001), any Medicare mental health visit (OR=1.46, p<0.01), and any mental health visit in either system (OR=1.73, p<0.001). There were no significant differences in numbers of VA mental health visits, Medicare mental health visits or total mental health visits among mental health care users. Conclusions: This study shows that both disabilityand age-eligible VA primary care patients use significant primary care and specialty care services outside of VA. Further, this study documents greater outpatient care needs for primary care, specialty care, and mental health care among disability-eligible veterans than age-eligible veterans, especially for VA care. Implications for Policy, Delivery or Practice: Current disability-eligible veterans have greater health care needs than age-eligible veterans. VA and Medicare will need to be prepared for the future needs of disability-eligible veterans, particularly younger veterans returning from Iraq and Afghanistan and Iraq wars. Establishing care coordination protocols between VA and Medicare systems will ensure efficient use of taxpayer resources and smoother transitions to VA care for disabled veterans. Funding Source(s): VA Poster Number: 184 Successful Recruitment of Black and Latino Women in a Behavioral Educational Intervention to Reduce Postpartum Depression Presented by: Anika Martin, Assistant Professor, Health Evidence & Policy, Mount Sinai School of Medicine, One Gustave L. Levy Place, Box 1077, New York, NY 10029; Phone: (212) 659-9567; Email: elizabeth.howell@msnyuhealth.org Co-authors: Amy Balbierz, M.P.H.; Edna Bisson; Howard Leventhal, Ph.D.; Elizabeth Howell, M.D., M.P.P. Research Objective: To determine reasons for refusals among self-identified Black and Latino postpartum mothers approached to participate in a postpartum depression intervention trial; and to revise recruitment strategies based on patient feedback. Study Design: This is an ongoing randomized controlled trial of 530 Black and Latino postpartum mothers testing whether a behavioral educational intervention reduces postpartum depression. Participants randomized to the intervention arm receive a 2-step intervention that prepares and educates mothers about modifiable factors associated with postpartum depression (e.g. distress from physical symptoms, deficits in social support, low self-efficacy, and distress from infant colic), bolsters social support, enhances management skills, and increases participants’ access to resources. Participants are surveyed at 3weeks, 3-months, and 6-months to assess depressive symptoms and other factors. All women who refuse to participate in the trial are asked openended questions about their reasons for refusal. Responses were transcribed, reviewed for similar themes, arranged into distinct categories, and organized as a taxonomy of reasons for refusal. Based on the taxonomy, we made targeted revisions to our recruitment methods. Population Studied: Eligible participants are selfidentified Black and Latino postpartum women who had uncomplicated deliveries at an urban hospital. Eligible subjects are women >18 years of age, English or Spanish Speaking, had working telephones, and had infants whose birthweights were > 2500 grams and 5-minute Apgar scores >6. The study has enrolled 460 self-identified Black and Latino mothers and this study presents results for the114 Black and Latino mothers who have refused to participate in this randomized controlled trial. Principal Findings: Of the 574 Black and Latino postpartum mothers approached during their hospital stay, 114 women refused to participate (Refusal rate of 19.9%). Seventy-two percent (n=82) of the patients were Latino and 38% (n=32) were Black. The taxonomy of refusals derived from patient responses has six main categories related to: 1) lack of interest, 2) having already been through childbirth before, 3) time commitment, 4) feeling overwhelmed, 5) patients moving from the area, and 6) confidentiality. Based on patient responses we revised our recruitment strategy to alleviate mothers’ concerns. We eM.P.H.asized the following elements: 1) a focus on women’s health, 2) postpartum mother’s health is understudied and participants could add to the knowledge base, 3) flexible schedule for follow-up, and 4) explained the process of confidentiality. The refusal rate has declined over 25 weeks of enrollment from 40% to 19.9%. Conclusions: Tracking of patient refusals and modifying recruitment methods based on patient feedback improved recruitment of Black and Latino mothers for a postpartum depression intervention trial. Implications for Policy, Delivery or Practice: Tracking patient refusals and tailoring recruitment methods based on patient responses may improve recruitment of Black and Latino participants in randomized controlled trials. Funding Source(s): National Center for Minority Health and Health Disparities (NIH) Poster Number: 185 Health Care Screening and Preventive Practices among Hispanic and Non-Hispanic Adults in the United States Presented by: Margaret McDonald, Ph.D., Director, Health Economics and Outcomes Research, Global Market Access, Pfizer Inc, 235 East 42nd Street, New York, NY 10017; Phone: (212) 733-3093; Email: margaret.m.mcdonald@pfizer.com Co-authors: Michael B. Lustik, M.S. Research Objective: Ethnic disparities in health care quality have been documented previously, but current knowledge of screening and preventive measures among Hispanic adults remains incomplete. This study contributes to our knowledge of preventative care by examining current national estimates of flu shots, sigmoidoscopy or colonoscopy, prostate-specific antigen tests, mammograms and Pap tests among Hispanic and non-Hispanic white adults aged 20 years and older. Study Design: Cross-sectional observational study design. Population Studied: Analysis of nationally representative data collected from Hispanic and non-Hispanic white adults aged 20 years and older participating in the Behavioral Risk Factor Surveillance System (BRFSS) 2008 (N= 23,325 Hispanic; 320,417 non-Hispanic whites). Principal Findings: Hispanic adults aged 50 years and older have significantly lower rates of having received a flu shot in the past year compared with same aged non-Hispanic white adults (45% vs. 54% for men, respectively; 50% vs. 59% for women, respectively; age-adjusted). Significant differences in annual flu shot rates persist among Hispanic and white adults 65 years and older (64% and 72%, respectively). Hispanic men aged 50 years and older are significantly less likely than same-aged white men to have had a prostatespecific antigen test within the past 2 years (58% vs. 71%, respectively) or of ever having had a colonoscopy/sigmoidoscopy (47% vs. 66%). Hispanic women 50 years and older have significantly lower screening rates for colon cancer than white women (52% vs. 65%, respectively; ageadjusted). Mammogram rates for Hispanic and white women aged 40 to 64 years are 73% and 76% (p = 0.02); mammogram rates are 80% and 79%, respectively, among women aged 65 years and older. Rates for having a Pap test within the past 3 years are similar for Hispanic and white women: 88% and 89% (age 20-39 years); 86% and 87% (age 40-64 years); and 71% and 67% (age 65+ years). Conclusions: Hispanic adults are less likely than non-Hispanic white adults to have received flu shots and sigmoidoscopies or colonoscopies. Hispanic men have lower rates of having had a prostate specific antigen test. Implications for Policy, Delivery or Practice: Effective approaches, including physician education and community outreach are needed to reduce these preventative medicine disparities. Poster Number: 186 The Social Construction of Racial/Ethnic Disparities in Diabetes – A Case of Misplaced Concreteness? Presented by: John McKinlay, Ph.D., Senior Vice President and Chief Scientist, Health Services and Disparities Research, New England Research Institutes, Inc, 9 Galen Street, Watertown, MA 02472; Phone: (617) 972-3012; Email: jmckinlay@neriscience.com Co-authors: Carol Link, Ph.D.; Rebecca Shackelton, Sc.M.; James Meigs, M.D.; Lisa Marceau, M.P.H. Research Objective: Racial/ethnic disparities in diabetes are widely considered an incontrovertible epidemiologic fact. This paper questions whether the reported racial/ethnic variation in diagnosed diabetes accurately reflects the actual distribution of (undiagnosed) diabetes in the population. Study Design: We employ data from two different but complementary studies—a community-based epidemiologic random sample survey and a balanced factorial experiment concerning primary care physician decision making for diabetes. Population Studied: Study 1 – The Epidemiologic Survey: 5503 adults (1767 black, 1877 Hispanic, 1859 white; 2301 men and 3202 women) from throughout the greater Boston, MA area. Study 2 – The Factorial Experiment: 192 licensed internists, family physicians, or general practitioners practicing in New Jersey, New York, or Pennsylvania. Principal Findings: No significant race/ethnicity differences were found in the prevalence of diabetes symptoms within SES level (?2 p>.35). Significant SES differences are found (?2 p<.0001), with higher prevalence among lower SES. Our experimental data show physicians pattern their diagnosis of diabetes by race rather than by SES (blacks (73.4%), Hispanics (60.9%), whites (48.4%) (p=.009) despite the fact that all patients presented with exactly the same signs and symptoms of diabetes. Diagnosed diabetes in the epidemiologic survey and NHANES data followed the same pattern. Conclusions: Our results suggest a racial/ethnic patterning of clinical decisions by primary care providers. While the actual prevalence of undiagnosed diabetes symptoms is patterned far more strongly by SES than race/ethnicity, when they are presented for diagnosis they are patterned more by race/ethnicity (than by SES). Physicians attending to (more visible) race/ethnicity, ignoring (less obvious) SES, may produce prevalence rates similar to the SES distribution of diabetes. Misplaced concreteness results in searching for genetic and bio-physiologic explanations which distract from the more important SES differences which shape the actual prevalence of diabetes. Implications for Policy, Delivery or Practice: Searching for causes and eventually interventions associated with race/ethnicity (like genetics, family history and bio-physiology) may distract from the search for factors associated with the real culprit – the significant effect of SES on the prevalence of diabetes in society. Funding Source(s): NIDDK and NCMHD Poster Number: 187 State Policies and Language Access in California's Commercial HMOs Presented by: Christopher Moreland, M.D., M.P.H., Fellow, Internal Medicine, University of California, Davis, 4150 V Street, Suite 2400, Sacramento, CA 95834; Phone: (916) 734-7005; Email: cmoreland@ucdavis.edu Co-authors: Dominique Ritley, M.P.H.; Julie Rainwater, Ph.D.; Patrick Romano, M.D., M.P.H. Research Objective: Report the status of language access services for California’s limited English proficient (LEP) health maintenance organization (HMO) members within the context of public reporting (on a state-sponsored website) and impending state regulation. Study Design: We conducted a retrospective, descriptive analysis of HMO responses to the California Office of the Patient Advocate’s annual survey, administered from 2003 through 2008. Responses were stratified by product line and/or language. Population Studied: California’s nine largest fullservice HMOs and other HMOs which serve the state’s Medicaid (Medi-Cal) population. Combined, these groups represent over 90% of Californian HMO members. Principal Findings: From 2003 to 2008, during California’s public reporting of HMO language services and before implementation of state language mandatory reporting requirements in 2009, the percentage of HMOs providing in-person interpretation at medical points of contact free of charge to consumers increased to over 80% across all product lines. From 2006 to 2008, the percentage of commercial product lines providing in-person medical interpretation in threshold languages (for which such services became mandatory in 2009) increased from 64% to 94%. From 2004 to 2008, the percentage of commercial HMO product lines matching new LEP members to providers by language increased from 50% to 71%. In 2005, 64% of commercial product lines and 56% of Medicare product lines provided telephone interpretation services in all seven surveyed languages, compared with 79% and 83%, respectively, in 2008. Throughout the reporting period, Medi-Cal and Healthy Families product lines provided nearly all language services due to state contract requirements. Conclusions: HMOs increasingly provided language access services in varying forms for LEP Californians from 2003 to 2008 during a period of public reporting but before implementation of state regulations. Such changes within commercial product lines appear more pronounced than those within state-contracted product lines. Implications for Policy, Delivery or Practice: Public reporting of HMO language access services may have been effective in encouraging such services, particularly within commercial product lines. It is too early to assess the additional effects of the regulatory mandate implemented in 2009. Funding Source(s): Health Resources and Services Administration Poster Number: 188 The Impact of Residential Segregation on Racial Disparities in Infant Health Presented by: Kwame Nyarko, B.A., Graduate Research Assistant, Health Management and Policy, University of Iowa, 5206 Westlawn, Iowa City, IA 52242; Phone: (319) 335-7180; Email: kwame-nyarko@uiowa.edu Co-authors: George Wehby, Ph.D. Research Objective: African-American infants have significantly poorer health outcomes compared to White infants. We examine the effects of racial residential segregation on the birth outcomes of African-American infants and the extent to which population and area-level characteristics explain these effects. Furthermore, we evaluate the role of unobserved heterogeneity in the relationship between segregation and infant health and assess the heterogeneity in the effects of residential segregation by unobserved area-level endowments that impact infant health. Study Design: The study uses county-level data from the US census and Natality surveys for 1990 and 2000 and from the area resource files. We measure residential segregation by the dissimilarity and the isolation indices. The study outcomes include low birth weight (LBW) and preterm birth rates of African-American infants. We estimate the effects of segregation on the means of the infant health outcomes using random and fixed effect models. We also apply quantile regression to estimate the effects of segregation on the quantiles of the infant health outcomes. Quantile regression evaluates the heterogeneity in effects of segregation by unobserved factors that determine the county’s location on the distribution of these outcomes. Population Studied: The study sample includes 235 counties of 100,000 or more residents and at least 50 annual African-American live births. Health, behavioral, demographic and socioeconomic county-level factors are measured for the AfricanAmerican population. Principal Findings: Ignoring unobserved factors, both measures of residential segregation have significant negative effects on infant health that is explained to a large extent by the observed population and area-level characteristics. The remaining effects of residential segregation are entirely explained in most segregation and infant health specifications by unobserved fixed effects that may result in overestimation of the effects of residential segregation if they are not causally related to segregation. The study also finds that the negative impacts of residential segregation are primarily at the low quantiles of adverse birth outcomes and not at the higher quantiles. In other words, segregation impacts infant health in areas with low rates of adverse birth outcomes and high area-level endowments that improve infant health, but segregation has insignificant effects in areas with high rates of adverse birth outcomes and poor endowments for infant health. Conclusions: The study results suggest that residential policies alone may not have large effects on reducing racial disparities in infant health, especially in areas with very high rates of adverse birth outcomes among African-American infants, and that they should be combined with policies that improve area-level endowments for infant health. Implications for Policy, Delivery or Practice: Policies that enhance area-level endowments that are relevant for infant health are needed to increase the returns of residential policies in reducing racial disparities in infant health. Funding Source(s): CDC, NIH Poster Number: 189 Racial Differences in Patient Satisfaction with a Blood and Marrow Transplant Case Management Program Presented by: Nancy Omondi, M.B.A., M.S., Manager, Health Services Research, Health Services Research, The National Marrow Donor Program, 30001 Broadway St. N.E Suite 100 OPA, Minneapolis, MN 55413; Phone: (612) 884-8518; Email: nomondi@nmdp.org Co-authors: Ellen Denzen, MS; Debbie Jacobson; Elizabeth Murphy, Ed.D, R.N. Research Objective: Blood and marrow transplantation (BMT) is a complex and resourceintense treatment for patients with life-threatening hematologic disorders. The National Marrow Donor Program operates the national registry of volunteer donors and facilitates BMT. Its Office of Patient Advocacy (OPA) includes a case management team that provides one-to-one telephone counseling to patients and their caregivers to address transplant-related questions. Previous research has addressed the impact of race on patient satisfaction; it has been demonstrated that satisfaction increases access to health services. We surveyed recipients of OPA case management services to evaluate patient satisfaction by race. Secondarily, survey responses were used to improve OPA’s case management services. Study Design: This cross-sectional study utilized an eight item questionnaire administered via mail without follow-up. Key evaluation areas were: helpfulness of the information and services provided; overall satisfaction with case management; and demographic information. Subjects were asked to describe follow-up actions taken as a result of the information/services provided and to recommend ways to improve these services. Helpfulness of the information and services provided was assessed using a three-point Likert scale. Satisfaction was assessed through the response to: “Would you recommend the OPA to someone else in your situation?” (yes, maybe, no, don’t know), which was used to create a Patient Satisfaction Index (PSI). Race was categorized as White and Other because of limited respondents in race categories other than White. Recommendations for improvement and follow-up actions were analyzed qualitatively. Population Studied: Our study population included all BMT patients and their caregivers living in the U.S. who directly contacted OPA case managers between October 1, 2007 and September 30, 2008. Of the 989 self-administered surveys that were mailed, 241 (24%) evaluations were returned. Principal Findings: Whites comprised 86% of the respondents. More than 65% of respondents found medical information provided by the Case Managers helpful. Overall, 54% of respondents took follow up action as a result of information or services provided by case management. There were no significant differences between Whites and Other Races recommending OPA to others or taking a follow up action. The overall PSI was 89%. Respondents who reported satisfaction with OPA case management services were more likely to take follow-up action compared to those not satisfied (p<.05). Conclusions: OPA case managers successfully addressed the transplant-related needs of patients from all racial groups. Most patients were satisfied with transplant case management and patient satisfaction did not differ by race. Transplant case management impacted informed decision making as shown by follow-up actions taken by respondents. In addition, respondents provided feedback regarding other transplant information/services that would be helpful to them. Implications for Policy, Delivery or Practice: One-to-one case management and provision of transplant information and services have a major impact on patient transplant decision-making, ultimately improving access to health services. Addressing satisfaction disparities could improve access to health services. Funding Source(s): The National Marrow Donor Program Poster Number: 190 Race Disparities in Hospital Discharge Disposition: The Role of Model Misspecification Presented by: Eberechukwu Onukwugha, Ph.D., Assistant Professor, Pharmaceutical Health Services Research, University of Maryland School of Pharmacy, 220 Arch Street, Baltimore, MD 21201; Phone: (410) 706-8981; Email: eonukwug@rx.umaryland.edu Lead Author: Jason Bergtold, Ph.D. Co-authors: Eberechukwu Onukwugha, Ph.D. Research Objective: Evidence for race disparities in hospital discharge disposition have been studied previously and results may depend on the statistical model that is used to calculate the risk ratios. In particular, a misspecified model can provide misleading evidence regarding the direction and magnitude of effect. The objective of this study is to compare the evidence for race disparities in poststroke hospital discharge disposition under alternative specifications of the multinomial logistic regression model. Study Design: The Probabilistic Reduction (PR) approach provides an alternative approach for specifying discrete choice models using observational data. Within the PR approach, the functional form of the choice probability for an individual includes an index function that depends explicitly on the inverse conditional distribution. An empirical application used cross-sectional data from a state-wide confidential inpatient hospital discharge data including admissions occurring between January 2000 and December 2005. Population Studied: The sample was limited to live discharges among adult (i.e. aged greater than or equal to 18 years) patients admitted for a stroke in Maryland. A traditional multinomial logistic regression model specification with limited interactions and a model specified following the PR approach were estimated and compared. Marginal effects for both the individual covariate of interest (‘Non-Caucasian race’) and the interactions of interest: (i) ‘patient age’ x ‘race’; (ii) ‘insured status’ x ‘race’; and (iii) ‘hemorrhagic stroke’ x ‘race’, were estimated. Individual marginal effects were estimated as the mean marginal effect across respondents. Interaction effects were calculated as the mean across respondents. Standard errors for all marginal effects and interaction effects were estimated using a delete-d jackknife estimator. Statistical significance of marginal effects was set at the 10% level. Principal Findings: Application of inclusion/exclusion criteria resulted in 69,921 live discharges following a stroke-related admission. The distribution of discharge disposition outcomes was as follows: home (N = 7,730), home health care (N = 525), rehabilitation (N = 9,997), nursing home (including intermediate care) (N =7,323), discharges against medical advice (N = 4,755), and all other (N = 39,591). Misspecification tests indicate that the PR approach provides a better fit and that the traditional specification of the model is misspecified. The marginal effect (standard error) results indicate differences between the traditional and PR specifications as concerns the likelihood that non-Caucasians will be discharged home (32.7% [0.005] less likely vs. 7.6% [0.001] less likely) or will require additional nursing or intermediate care (22.5% [0.009] more likely vs. 3.2% [0.001] more likely). Interaction effects of interest, compared across model specifications, were either both statistically significant and opposite in sign (‘age’ x ‘race’) or both statistically significant, of the same sign, but of different magnitudes (‘hemorrhagic stroke’ x ‘race’; ‘insured status’ x ‘race’). Conclusions: We found that the evidence for the existence and extent of race disparities in poststroke hospital discharge outcomes varied across statistical model specification approaches. Implications for Policy, Delivery or Practice: Efficient public investment in programs that address race disparities depends on the availability of reliable information regarding the existence and extent of disparities. We show that the statistical model specification approach is a key consideration when identifying potential sources of bias in disparities research. Funding Source(s): NIH Roadmap K12 program Poster Number: 191 Health Literacy and Communication Quality in Organizations Presented by: Chandra Osborn, Ph.D., Assistant Professor of Medecine, General Internal Medicine and Public Health, Vanderbilt University Medical Center, 1215 Twenty-First Ave South, Suite 6000, MCE North Tower, Nashville, TN 37232; Phone: (615) 936-8468; Email: chandra.osborn@Vanderbilt.Edu Co-authors: Matthew K. Wynia, MD, M.P.H. Research Objective: Effective health communication is fundamental to quality care for all patients. Communication challenges are also powerful contributors to disparities since patients with limited health literacy are more often minorities. Inadequate health literacy leads to misunderstanding health information, difficulty following medical instructions and worse health outcomes. Employing effective communication practices may be one of the most important interventions to address the widespread burden of limited health literacy. We used patient surveys to explore the relationship between health literacy status and receiving patient-centered communication in thirteen clinics and hospitals serving communication-vulnerable patient populations. Study Design: An assessment of organizational patient-centeredness was developed through a multistakeholder consensus process. The assessment was validated in a field test with thirteen widely-varying health care organizations, including six hospitals and seven clinics nationwide. During field testing, patient surveys were distributed that included seven items to assess perceptions of patient-centered communication. One third of patients surveyed also completed items measuring health literacy. Population Studied: Surveys were collected from 5,929 patients, of whom 2,116 also completed items about health literacy. Principal Findings: Most patients were between age 25-44, female and a member of a racial/ethnicminority group. One third had limited English proficiency, and most were receiving care from a federally qualified health center or large/urban medical center. Nearly half reported visiting this facility two-five times in the last six months. The majority of patients had health literacy challenges, reporting problems learning about their medical condition because of difficulty understanding written information (53%), a lack of confidence in completing medical forms by themselves (61%) and needing someone to help them read hospital/clinic materials (57%). Logistic regression models showed that, after adjustment for patient demographic characteristics and organization type, patients with limited health literacy were 21-78% less likely than those with adequate health literacy to report that their organization “always” provides patient-centered communication across the seven communication items (20 of 21 p-values <0.05). In additional multivariable models using a scaled composite of the seven items, limited health literacy remained associated with lower communication quality. Conclusions: Many of the health consequences associated with limited health literacy may be caused or exacerbated by ineffective, non-patientcentered communication. This study demonstrates that patients with inadequate literacy are considerably less likely to report receiving patientcentered communication from the organizations where they seek care, across an array of communication quality indicators. Implications for Policy, Delivery or Practice: Organizational change to alleviate disparities by addressing health literacy requires leadershipdriven modifications of internal operations, increasing staff awareness and competency, improving provider access to training on effective health communication, and continued monitoring of organizational performance to identify changes in quality improvement opportunities. Funding Source(s): The California Endowment Poster Number: 192 Stigma among Colorectal Cancer Patients Presented by: Sean Phelan, M.P.H., Research Fellow, Family Medicine and Community Health, University of Minnesota, 925 Delaware Street SE, Minneapolis, MN 55414; Phone: (612) 625-9106; Email: phel0085@umn.edu Co-authors: Michelle van Ryn, Ph.D.; Joan Griffin, Ph.D.; Diana Burgess, Ph.D. Research Objective: People with stigmatized medical conditions experience adverse psychological and physiological health outcomes and may delay medical care and if they perceive that they are devalued by their health care providers or other people. Furthermore, self-blame for conditions that are perceived to have behavioral causes may have negative effects as well. The goal of the project was to measure experiences of stigma, self-blame, and discrimination among patients with colon or rectal cancers, and assess whether these experiences are related to stressrelated mental health outcomes. Study Design: A patient questionnaire assessing a variety of domains of patient characteristics and experiences was developed by a team of NCI, VA, DOD and University of Minnesota scientists. A single item measure of perceived discrimination in attaining health care was used, as well as items measuring perceived stigma associated with colorectal cancer, and self-blame. Outcome measures consisted of validated measures of depression, anxiety, overall health, and pain, as well as measures of patient-centered quality of care. The questionnaire was pilot-tested in the fall of 2009 among all VA patients who received a diagnosis of colorectal cancer in any VA facility in 2008 and were alive at the time of the survey. Patients were ascertained from the VA Cancer Registry and vital status confirmed through computerized medical records. Associations between stigma related experiences and patient health outcomes and reported quality of care will be assessed using multivariate regression techniques. Population Studied: There were 2018 living patients with colorectal cancers diagnosed at Stage 1 or higher during 2008 as ascertained from the registry. Of the 2018 patients in the sample, 67% (1421) returned completed questionnaires. Most (94%) were male, reflecting the VA population. The median age was 67 with a range of 26 to 94. Principal Findings: There was considerable variation in patient reports of stigma, discrimination, and perceived blame. For example, 12% of patient reported experiencing discrimination by health care providers, 26% felt that they were at least partially to blame for their illness, and 25% felt that there was a stigma that goes with having their condition. Conclusions: Some patients with colon or rectal cancers experience stigma and discrimination related to their condition, and may blame themselves for acquiring the disease. These occurrences may have implications for patient mental health and other outcomes. Implications for Policy, Delivery or Practice: Stigma may an important stressor for patients with colon or rectal cancers that may contribute to their health outcomes. Physical and mental health care providers should consider this when working with this patient population. Funding Source(s): NCI Poster Number: 193 What Characterizes Counties Successful in Breast Cancer Screening? Presented by: Maria Pisu, Ph.D., Assistant Professor, Medicine/Preventive Medicine, University of Alabama at Birmingham, 1530 3rd Avenue S., MT 628, Birmingham, AL 35298-4410; Phone: (205) 975-7366; Email: mpisu@uab.edu Co-authors: Robert S. Levine, M.D.; Robert Oster, Ph.D.; Alana Cantor, Ph.D.; Michelle Martin, Ph.D. Research Objective: In the US, there is a wide geographic and racial variation in breast cancer screening. The objective of this study is to better understand how communities successful at promoting breast cancer screening in black and white women compare with less successful ones in socioeconomic status and medical resources availability and type. Study Design: We obtained county-level breast cancer screening rates (CO-BCSR) for white and black women from Medicare administrative claims for a sample of 1,000,000 women older than 64 continuously enrolled in Medicare fee-for-service plans. Women resided in 172 counties with the highest numbers of breast cancer deaths in black women. Counties were classified in 4 types: Failing, i.e., black and white CO-BCSR lower than the respective race average CO-BCSR; With Disparity, i.e., black CO-BCSR lower and white CO-BCSR higher than the respective race average CO-BCSR; With Reverse Disparity, i.e., black CO-BCSR higher and white CO-BCSR lower than the respective race average CO-BCSR; and Successful, i.e., with black and white CO-BCSR higher than the respective race average CO-BCSR. Using data from the Area Resource File, we identified economic factors and medical resource availability and type that may be associated with county type. We used discriminant analysis to identify variables that would characterize each county type, and multinomial logistic regression to compare county types. Population Studied: US Counties and women enrolled in Medicare Principal Findings: The average CO-BCSR was 42.3 per 100,000 (range: 20.8-58.2) for black, and 48.7 (range: 29.7-65.2) for white women. Counties were: 56 Failing, 23 With Disparity, 26 With Reverse Disparities, and 67 Successful. The socioeconomic variables that best predicted the county classification were: percentage of county population living below the federal poverty level, county average household income. The medical resources variables that best predicted county type were: proportion of hospitals with associated medical schools and HMO penetration. Other variables included were: median age of women in the county, percent of black females, number of MDs, primary care physicians, and female MDs per 100,000 females, number of hospitals per 100,000 females, percentages of hospitals with mammography centers. Results of the multinomial logistic regression showed that, compared to Failing counties, counties were more likely to be Successful if they had smaller proportions of foreign born and black female populations, lower incomes, fewer hospitals and lower HMO penetration. Compared with counties with Reverse Disparities, counties were more likely to be Successful if they had fewer hospitals, lower proportion of hospitals associated with medical schools, and lower HMO penetration. Successful counties did not differ from counties With Disparities in all variables examined. Conclusions: Successful counties are not necessarily richer than failing counties or counties with disparities, and do not differ significantly in the availability of most medical resources. Existing type of care (e.g., medical schools or HMOs) may differentiate county types. Implications for Policy, Delivery or Practice: More research is needed to understand what makes counties successful and how to transfer successful models to failing counties or counties with pronounced disparities. Funding Source(s): NCI Poster Number: 194 The Role of Dentists in Alleviating Racial/Ethnic Disparities in Dental Care: Does Availability of Discounted Care Increase Affordability? Presented by: Nadereh Pourat, Ph.D., Associate Professor, Univeristy of California, Los Angeles Center for Health Policy Research, 10960 Wilshire Boulevard, Suite 1550, Los Angeles, CA 90024; Phone: (310) 794-2201; Email: pourat@ucla.edu Co-authors: Ron Andersen, Ph.D.; Marvin Marcus, D.D.S., M.P.H.; Dylan Roby, Ph.D.; Gina Nicholson, M.P.H. Research Objective: Research indicates that racial/ethnic disparities in oral health care may be attributable to access. Lack of insurance is linked with fewer dental visits. Also, dental insurance policies with higher out-of-pocket costs which may lead to foregoing dental care among insured who can not afford these costs, including many low income and non-white groups. The uninsured seeking lower cost services can obtain care in community clinics with dental care capacity or identify private dentists who offer sliding scale fees. Since the majority (96%) of the dentists are in private practice, availability of dentists offering discounts may be crucial in insuring affordability and subsequent access. This study examines if higher rates of private dentists who offer discounted care in an individual’s Medical Service Study Area (MSSA) has an impact on foregoing needed dental care due to costs. It is hypothesized that a higher percentage of dentists in an MSSA who offer discounted dental care reduces the likelihood of racial/ethnic groups to forego dental care due to costs. Study Design: Data from the 2003 California Health Interview Survey (CHIS) and a 2003 representative survey of California dentists were merged at the MSSA level. The percentage of dentists in an area that reported offering discounted dental care in their primary practice per MSSA was merged with CHIS data. SAS v. 9.3 GLIMMIX models were used and included individual level demographic and socioeconomic data as well as MSSA level data. All analyses were adjusted for CHIS and dentist survey design. Population Studied: The sample included 40,000 adults, with 25,400 whites, 2,500 African Americans, 6,700 Latinos, and 3,800 Asian Americans. Principal Findings: Latinos (31%) and African Americans (22%) were more likely to forego needed dental care due to costs that Asian Americans (16%) and whites (14%). Preliminary findings indicate that the higher percentage of dentists who offer discounted care is associated with the lower likelihood (OR=0.68) of foregoing dental care due to costs in an MSSA, in an unadjusted model. However, the models controlling for individual level variables indicate that that this relationship is no longer significant. Rather, lack of dental insurance, low income, age, and gender are among individual variables that determine the likelihood of foregoing dental care due to costs. Conclusions: Our findings indicate that availability of discounted dental care may be negatively associated with foregoing care, however, factors such as dental insurance are more important in insuring affordability of dental care. Data is lacking on the extent of the discount provided by dentists. Insubstantial discounts are unlikely to change affordability. If most dentists do not provide sufficient discounts no impact on affordability is observed. Implications for Policy, Delivery or Practice: Recessions and budget cuts compound the financial difficulties of populations with the lowest socioeconomic status, many of whom are members of non-white racial/ethnic groups and reduce their ability to obtain dental care. The absence of dental insurance coverage can not be remedied by provision of discounted dental care and health care policy should focus on improving dental coverage and comprehensiveness of such coverage. Funding Source(s): NIDCR Poster Number: 195 Black-White Disparities in Mortality among Middle Aged Adults: Can Health Insurance Be the Solution? Presented by: Janice Probst, Ph.D., Associate Professor, Health Services Policy and Management, University of South Carolina, 800 Sumter Street, Columbia, SC 29208; Phone: (803) 777 7426; Email: jprobst@sc.edu Co-authors: Katrina M. Walsemann, Ph.D.; Jessica D. Bellinger, Ph.D.; James Hardin, Ph.D. Research Objective: Disparities in life expectancy between white and non-white populations in the US are marked. While infant mortality contributes to this difference, the majority of excess deaths occur in middle age. Our research seeks to ascertain whether health insurance helps to ameliorate racial disparities in mortality among adults aged 45 - 64. Study Design: Data were drawn from the 2004 National Health Interview Survey (NHIS) Linked Mortality File. This file links respondent information from the nationally representative NHIS to death records through 2002. Population Studied: Our analysis examines respondents between the ages of 45 and 64 during interview years 1986, 1989-2000. We excluded 1987-1988 because no insurance information was collected. Records with missing data on any variable were also excluded, for a sample size of 217,748. We used Cox proportional hazard models to calculate mortality hazard ratios (HR) by race/ethnicity and insurance status at time of interview (privately insured, publicly insured, uninsured). Respondent demographic, resource and health status characteristics were held constant in multivariable analysis. All analyses were stratified by sex and weighted to account for the complex sample design. Principal Findings: Overall, 77.1% of respondents reported private insurance, 11.1% public insurance, and 11.8%, uninsured. Minorities were more likely to be uninsured (18.2% black, 27.2% Hispanic, and 17.5% other adults, versus 9.5% of white respondents). In analysis holding age and interview year constant, black adults had an elevated risk of death (Female: HR 1.62, CI 1.52-1.72. Male: HR 1.57, CI 1.48-1.66) compared to white adults. Hispanics, regardless of sex, did not differ in risk from whites, whereas men from other racial origins were at lower risk of death than whites (HR: 0.83, CI 0.73-0.95). Adjustment for insurance alone reduced the hazard ratio for blacks, regardless of gender, but did not fully eliminate disparities (Female: HR 1.31, CI 1.23- 1.40. Male: HR 1.32, CI 1.25-1.41), which remained after further adjustment for socio-economic status, region, rurality, and health status (Female: HR 1.11, CI 1.04-1.19; Male HR 1.08 CI 1.02-1.16). Adjustment for insurance status resulted in significantly lower risk of death for Hispanic women compared to white women. Further adjustment for socio-economic status, region, rurality, and health status resulted in significantly lower risk of death for Hispanics of either gender compared to white adults. Of note, uninsured individuals were at higher risk of death in all analyses. Conclusions: Health insurance appears to ameliorate some of the black-white disparity in mortality, but does not fully eliminate it. Implications for Policy, Delivery or Practice: Expansion of insurance coverage across the US population through health care reform may not be sufficient to eliminate race-based disparities in risk of death. Additional research is needed into contextual factors, such as neighborhood income or distance to providers, which may influence health and survival. Research into the lowered risk of death experienced by middle-aged Hispanic adults may provide insight for other minority populations, as well. Funding Source(s): HRSA Poster Number: 196 The Impact of Subjective and Objective Socioeconomic Status on Health: Do the Results Differ Between Subjective and Objective Health Measures? Presented by: Christy Pu, Ph.D., Assistant Professor, Department of Public Health, National Yang-Ming University, Li-Nong Street, Sec 2, Peitou, Taipei, Taiwan 155; Phone: +886285906914; Email: christypu@hotmail.com Co-authors: Nicole Huang, Ph.D.; Yiing-Jenq Chou, Ph.D. Research Objective: This research aims to determine whether the relationship between subjective socioeconomic status (SES) and health depends on types of health measures. Study Design: This research used the data from the Survey of Health and Living Status of the Middle Age and Elderly in Taiwan (SHLS) conducted by the Bureau of Health Promotion, Department of Health in Taiwan. The survey consists of 5 waves (1989, 1993, 1996, 1999 and 2003). Educational attainment and the respondent’s major occupation were used as measures for objective SES, and selfrated satisfaction on financial position was used to measure subjective SES. Self-rated health (SRH) was used to measure subjective health status. SRH is dichotomized into those who reported reduced health (SRH not equal to “Excellent” or “Very good”) and those who did not report reduced health, at the survey wave before death. Mortality was used to measure objective health outcome. For both objective and subjective measures, Cox proportional hazard models were estimated to allow for comparison. Population Studied: 4,049 nationally representative elders (65 years and above) in Taiwan Principal Findings: Subjective SES was positively and significantly associated with subjective health measure (SRH). Compared with those who reported “satisfied” for financial satisfaction, those who reported “average” (HR= 1.20, p< 0.01) and “unsatisfied” (HR=1.29, <0.01) were more likely to report reduced health. However, subjective SES was not significantly associated with objective health (mortality). On the other hand, objective SES (education) was more significantly associated with mortality than with SRH, with those who had higher educational attainment had lower HR for mortality. Conclusions: The correlation found between subjective SES and subjective health measures may be simply caused by personal traits, such as, whether the person is pessimistic. A pessimistic person may perceive himself to be in poor financial condition and the same pessimism also lead him to perceive himself to be in poor health. Thus the association found between subjective SES and selfreported health may simply reflect such individual characteristics. Implications for Policy, Delivery or Practice: Research that investigates the relationship between subjective SES and health do not compare results when subjective and objective health measures are used. We argue that the association between subjective SES and health status depends on whether the health measure is also subjective, and this should be taken into consideration in related research. Poster Number: 197 Availability of Translation Services and Translated Documents in High Performing Hospitals Presented by: Marsha Regenstein, Ph.D., M.C.P., Research Professor, Dept of Health Policy, Center for Health Care Quality, George Washington University, 2121 K Street, NW, Suite 200, Washington, DC 20037; Phone: (202) 994-8662; Email: marsha.regenstein@gwumc.edu Co-authors: Lea Nolan, M.A. Research Objective: There is little guidance on the “how” to deliver translation, despite recent activities by three major accrediting bodies, the National Committee on Quality Assurance, the Joint Commission and the National Quality Forum, to include requirements related to translating vital documents into languages spoken by patients in a community. Research has been conducted on the best way to translate documents, such as the idea of “back-translating” to ensure quality and leaving a trail of documentation about how the material was translated. This study assesses the current translation practices of hospitals that are considered high performing in language services. Study Design: We developed a survey for hospital translation services directors. The datasource was completed surveys from telephone interviews, fielded November 2008 through January 2009. We generated descriptive statistics on hospital background, who provides translation services, policies and procedures regarding translation services, quality control for translations, storage and accessibility of translated documents, and costs of translation services. We also collected hospitals’ written policies pertaining to translation services. Population Studied: The population in this study are 35 high-performing hospitals, defined as hospitals who have extensive experience with or have been innovative in their approach to providing languages services. We identified 53 potential subjects, using prior research projects, hospital association membership listings, and data on distribution of ethnic diversity and immigrant population. Principal Findings: A majority of respondents use contract translators (29) but almost as many use staff interpreters to translate (27). Few hospitals have staff dedicated to translation. The majority of hospitals (24) translate any document that is requested, although some make a distinction and translate any vital document. Hospitals without standardized policy leave it to the individual departments to determine what should be translated. The majority of respondents (27) have an in-house quality control process in place, but the remaining 8 do not. Hospitals report a variety of storage options, including an intranet for all staff, storage drive in the language services office, and central repository for all translated documents. Nearly half of hospitals have centralized costs and do not charge requesting departments for translations, four provide free translation services to hospital staff, and others charge depending on the type of translated document. Although less than half could estimate the costs of providing translations, our data suggests that the annual cost of in-house translations ranges from $8,000-$900,000. External costs range from $1,000-$117,000 per year. Conclusions: Translation services are provided through a variety of methods, depending on patients’ specific language needs and availability of qualified translators. Even with varying resources available for translating and storing documents, all hospitals should implement quality control procedures to ensure the quality of their translated documents. Implications for Policy, Delivery or Practice: This study uses guidance from the field to formulate trends and determine best practices for the delivery of translation services in health care settings. These results also serve as a baseline for accrediting bodies and policymakers to develop systematic requirements and processes for institutions on how to develop effective policies and practices related to the delivery of translation services and translation of health care materials. Funding Source(s): RWJF Poster Number: 198 Disparities in Meeting the 12 LyM.P.H. Node Minimum Standard Examination after Resection for Colon Cancer Presented by: Kim Rhoads, M.D., M.S., M.P.H., Assistant Professor, Surgery, Stanford University, 300 Pasteur Drive H3680F, Stanford, CA 94305; Phone: (650) 736-8406; Email: kim.rhoads@stanford.edu Co-authors: Jennifer Cullen, Ph.D.,M.P.H.; R. Adams Dudley, M.D., M.B.A.; Sherry Wren, M.D. Research Objective: Disparities in colon cancer outcomes are well documented. Improved 5-year survival has been shown to correlate with having 12 lyM.P.H. nodes (LN) examined after colon cancer resection, since ensuring that LNs are negative determines stage and the need for chemotherapy. The National Quality Forum has recently endorsed this practice standard as a measure of the quality of colon cancer surgery. However, there is significant variation in compliance with this metric. The purpose of the current study is to determine if there are racial and ethnic disparities in meeting the12 lyM.P.H. node minimum standard examination and secondarily to determine the effect of the standard on disparities in survival after colon cancer resection. Study Design: The current study is a retrospective analysis of a large administrative database from the California Cancer Registry (CCR) and the California Office of Statewide Health Planning and Development (OSHPD). Chi-square analyses and logistic regression models were used to assess for differences in the percent of patients having 12 LN examined and the percent being under staged (stopping at <12 LN examined when none have been positive). Models were adjusted for demographics, tumor location, year of treatment and hospitals’ annual volume, percent Medicaid, and teaching status. Cox proportional hazard models for mortality were adjusted for these factors and urgency of surgical intervention. Population Studied: All cases of colon cancer contained in the CCR database during the years 1996-2006, inclusive, were linked to patient discharge abstracts from OSHPD for the same years. Patients with ICD9 codes for the primary diagnosis of colon cancer, who had concomitant codes for major colon resection, were included. Patients with stage IV disease and those with missing data on lyM.P.H. node counts were excluded. The final cohort included 62,928 records. Whites represented 73%; Blacks 7%; Hispanic patients 11% and Asian/Pacific Islander 9%. Principal Findings: Blacks, Hispanics and Asians were 18%, 22% and 6% less likely to have 12 LN examined. Hispanics had 11% higher odds of being under staged. Use of high volume, teaching and high compliance rate hospitals was associated with a 20%, 21% and 3%, respectively, increased odds of meeting the standard. Percent Medicaid patients within a hospital was not significantly correlated with LN exam variation. Mortality disparities persisted despite adjustment for receipt of the standard LN examination. Analysis of mortality stratified by race showed a significant effect of having 12 lyM.P.H. nodes examined on outcomes for whites, but not for other races. Conclusions: Variation in receipt of the 12 LN minimum standard after colon cancer resection does not explain disparities in survival, but is associated with increased risk for under staging of Hispanics. Our study suggests that there are other factors contributing to the persistence of disparities in colon cancer outcomes. Implications for Policy, Delivery or Practice: Increased efforts should be made to ensure that the 12 LN minimum standard is met in all patients to avoid under staging and potentially, under treatment of colon cancer. Funding Source(s): RWJF Poster Number: 199 Does Socioeconomic Status Moderate the Association of Race with Morbidities During Pregnancy Episodes? Presented by: Douglas Roblin, Ph.D., Senior Research Scientist, The Center for Health Research / Southeast, Kaiser Permanente Georgia, 3495 Piedmont Road NE, Building 9, Atlanta, GA 30305; Phone: (404) 364-4805; Email: Douglas.Roblin@KP.Org Co-authors: Peter Joski, M.S.P.H.; Donald Bachman, M.S.; Mark Hornbrook, Ph.D. Research Objective: African American adults generally have higher prevalence of morbidities than whites in the United States. Living in lower socioeconomic status (SES) neighborhoods increases the likelihood of poor health. The extent to which lower SES contributes to a higher rate of pregnancy complications for African Americans requires investigation. We explored racial differences in likelihood of maternal morbidities and whether these differences were moderated by neighborhood SES. Study Design: Pregnancies were defined from linked birth certificates and hospital records. Morbidities during pregnancy were ascertained from all outpatient and inpatient diagnoses and procedures classified by a previously validated maternal morbidity grouper. SES was measured from a factor analysis of 7 US Census measures associated with tract or block group of residence. Factor scores were divided into quartiles. Likelihood of selected morbidities was estimated using logistic regression adjusted for race, SES quartile, and mother’s age. Parameter estimates were adjusted for repeated observations per woman during the study period. Population Studied: 9,726 pregnancies among 8,517 non-Hispanic African American women and 10,272 pregnancies among 8,652 non-Hispanic white women enrolled with Kaiser Permanente Georgia (KPGA) from 2000-2006. Principal Findings: 14% of pregnancies were characterized by non-hereditary anemia, 13% by hypertension, and 7% by mental disorders. African American women were more likely than white women to live in lowest SES quartile neighborhoods (32% vs. 16%; p<0.05). Adjusted for age and SES, pregnancies characterized by non-hereditary anemia and hypertension were significantly (p<0.05) more likely among African Americans than whites (OR = 2.24 [95% CI: 2.45, 2.04] and 1.30 [95%: 1.42, 1.18], respectively). Mental disorders were significantly less likely among African Americans (OR = 0.50 [95% CI: 0.57, 0.44]). Stratified by race and adjusted for age, low SES neighborhoods had a significantly greater moderating effect among whites than among African Americans. Among whites, the adjusted ORs for the lowest SES quartile (vs. highest) were 1.21 (95% CI: 1.40, 1.01) for hypertension, 1.97 (95% CI: 2.40, 1.61) for non-hereditary anemia, and 1.27 (95% CI: 1.57, 1.03) for mental disorders. Conclusions: Neighborhood SES had a significant moderating effect on selected morbidities during live birth pregnancy episodes in this HMO. Compared to African American women, living in low SES neighborhoods significantly increased the risk of major morbidities during pregnancy episodes among white women. Implications for Policy, Delivery or Practice: In an insured and generally middle class population, both race and SES were associated with likelihood of hypertension, non-hereditary anemia, and mental disorders among women during pregnancy. While coverage, access and affordability have been suggested as reasons for differences in health risks by race and SES, our study’s findings suggest other factors – such as biologic, behavioral, or social differences – must be considered in the debate about racial and SES disparities. Funding Source(s): CDC Poster Number: 200 Emergency Room Use and Delays in Prescription Drugs are Higher among African-Americans When Compared to Other Commercial HMO Enrollees Presented by: Dylan Roby, Ph.D., Assistant Professor, Health Services / Center for Health Policy Research, University of California, Los Angeles School of Public Health, 10960 Wilshire Boulevard, Suite 1550, Los Angeles, CA 90024; Phone: (310) 794-3953; Email: droby@ucla.edu Co-authors: Gina Nicholson, M.P.H.; Gerald Kominski, Ph.D. Research Objective: This study examines delays in fulfilling prescribed medications, delays in obtaining needed medical care, visits to emergency rooms, and the presence of a usual source of care among insured African Americans in public and commercial HMOs. Study Design: Using 2007 California Health Interview Survey (CHIS) data, we conducted descriptive analyses of HMO enrollment, payer source, and race/ethnicity. To determine if these differences persist after adjusting for sociodemographic and health differences between ethnic groups, we conducted separate logistic regression analyses for each insurance type to control for selection bias. Population Studied: These analyses were conducted for the adult, non-elderly population (1864) enrolled in HMOs based on 2007 CHIS respondents. Principal Findings: African-American HMO enrollees were more likely to use the ER than other ethnic groups. Although ER use is similarly high for both whites and African Americans enrolled in public HMO plans (predominantly Medi-Cal), there is a distinct difference between African Americans and whites who are enrolled in commercial HMO plans. African Americans enrolled in commercial HMOs were more likely to use the ER (25.4% in Kaiser and 24.9% in other commercial plans) compared to other ethnic groups in commercial HMOs. Rates of prescription drug delays are about 5% higher for commercially insured African Americans in Kaiser compared to whites. However, a much larger disparity exists for African Americans enrolled in other commercial HMO plans compared to whites. African Americans have an almost 10% higher rate of delaying needed prescription medications than whites. Separate regression models for each insurance type were used to isolate the potential effects of demographics, health status and race/ethnicity among the separate insurance status groups. African Americans were more likely to use the ER (OR = 1.51, p<0.05) when enrolled in commercial Kaiser and were more likely to delay prescriptions (OR = 1.66, p<0.05) when enrolled in other commercial HMO plans. Predictors of ER use in the commercial HMO model were fair/poor health status and chronic illness. In the commercial Kaiser HMO model, ER use was predicted by African-American race, fair/poor health status and chronic illness. Predictors of prescription delays in commercial HMO enrollees were AfricanAmerican race, female gender, fair/poor health status and chronic illness. Conclusions: This disparity suggests other barriers still exist for HMO-enrolled African Americans in California in terms of avoiding ER visits and delaying prescriptions. Implications for Policy, Delivery or Practice: In California, the largest proportion of African Americans in HMO plans are enrolled in Kaiser Permanente, which operates on an integrated staff model that could include ER, urgent care, on-site pharmacy and various other services on one hospital campus. This type of convenience and increased access to ER services could potentially impact patterns of use among Kaiser enrollees. Greater delays in obtaining prescription drugs for African-American commercial HMO enrollees could be due to high copayments, limited pharmacy benefits, lack of access to in-network pharmacy services covered by the HMO, or perception of need by the patient. We do not see similar prescription delays for African-American commercial Kaiser HMO enrollees, who may have better access to on-site pharmacy services compared to other commercial HMO enrollees. Funding Source(s): California Office of the Patient Advocate Poster Number: 201 Access to Health Care for Latino Mixed-Status Families Presented by: Kara Ryan, M.P.P., Health Policy Research Analyst, Office of Research, Advocacy, and Legislation, National Council of La Raza, 1126 16th Street, NW, Washington, DC 20036; Phone: (202) 776-1703; Email: kryan@nclr.org Co-authors: Patricia Foxen, Ph.D. Research Objective: Research has shown that children in mixed-status families are much more likely to be uninsured than children born to citizen parents, largely due to barriers to employer-based and public coverage programs for which they are eligible. However, there has been limited research on the experiences of mixed-status families within the health care system. To assess the potential implications of the structure of the health care system for Latino mixed-status families, NCLR conducted a series of focus groups in October 2009. This research focused on the influence of parent uninsurance on insured children’s health care access and quality, with eM.P.H.asis on the experience of mixed-status families. Study Design: The seven focus groups took place in four sites—Charlotte, North Carolina; Chicago, Illinois; Portland, Oregon; and Fairfax, Virginia. The sites were chosen based on several factors, including characteristics of the Latino population (e.g., size, nascent or established) and the policies of selected states’ public coverage programs. Five panels included Latino parents who were uninsured but whose children had health insurance, with one panel made up of parents in fully-insured families, and one panel composed of parents whose family members were all uninsured. Four of the seven panels were composed entirely of immigrant parents with citizen children. Population Studied: The participants were Latino parents of U.S. citizen children under age 18. More than half of the participants were noncitizens, including both legal and undocumented immigrants, and the remainder were citizens. Principal Findings: The following five themes emerged from this research: 1) Overall, state public coverage programs are critical to health care access for citizen children in mixed-status families. 2) However, parents in these families have dramatically lower access to health coverage and care and report poorer health. 3) Families’ experiences navigating the public coverage system were inconsistent from state to state. 4) Affordability is a significant problem, even when children are insured. 5) Parents recognize the comprehensive nature of their children’s health insurance, but perceived some differential treatment based on ethnic identity as well as their status as public coverage recipients. Conclusions: Access to health coverage for children in mixed-status families is critical to their health care access, but varies by community. Even when children are insured, parents have difficulty paying for medical services, and they often have no access to coverage or care themselves. More research is necessary to understand how Latino parents’ poor access to health care impacts the well-being of the family unit. Implications for Policy, Delivery or Practice: At this point, final health care reform legislation may improve access and quality for Latinos in mixedstatus families, or it may actually impose new barriers, therefore widening health care disparities. In either case, these findings provide insight into the issues that must be addressed in order to close gaps in Latinos’ health care access and quality. Funding Source(s): Atlantic Philanthropies Poster Number: 202 Does Patient-Navigator Racial/Ethnic Concordance Improve Patient Barrier Identification? Presented by: M. Christina Santana, M.P.H., Researcher, Section of Internal and General Medicine, Women's Health Unit, 801 Massachusettes Avenue, Crosstown Building, Suite 470, Boston, MA 02118; Phone: (617) 638-8036; Email: christina.santana@bmc.org Co-authors: Sharon Bak, M.P.H.; Kristine Beaver, M.P.H.; Stephen Evans; Karen Freund, M.D., M.P.H.; Tracy Battaglia, M.D., M.P.H. Research Objective: Preliminary data suggests that Patient Navigation, which targets individual barriers to care, is an effective strategy to reduce cancer health disparities. While most navigation programs are culturally tailored, there are no studies examining the role of navigator race/ethnicity on outcomes. Boston is one of nine sites participating in the multi-site, NCI Patient Navigation Research Program (PNRP) which aims to reduce delays in cancer care among underserved with cancer screening abnormalities. Our objective is to examine the role of racial/ethnic concordance of patient and navigator on the identification of barriers to care, as an intermediate outcome. Study Design: Three of the six Boston PNRP Community Health Center sites (CHC’s), with a breast navigator were included. Racial/Ethnic concordance was determined by first categorizing patient and navigators into White or Non-White groups, and then they were matched for concordance (yes/no) based on those categories. The outcome of interest was the presence or absence of barriers to care, as documented by the Navigator. Due to racial differences in the identified barriers outcome analyses, we stratified by patient racial/ethnic groups of White and Non-White using chi-squares. Population Studied: Eligible women were 18 years or older, and had an abnormal breast cancer screening test at one of the 3 breast navigated CHC sites. Women were navigated until a diagnostic resolution was reached during January 2007-June 2008 study recruitment period. Principal Findings: Preliminary findings for 503 women showed a mean age of 49 ±12; 58% are non-White, 63% speak English as their primary language; 78% had an abnormal imaging test and 35% had private health insurance. Of the 10 breast Navigators, 70% are White and 20 % speak a language other than English. Overall 40% of the patient-navigator pairs were concordant by race/ethnicity. Overall, Non-White women were more likely to have barriers present compared with White women (79% vs. 50%, p <0.0001). NonWhite concordant pairs were as likely as Non-White discordant pairs to have barriers present (81% vs. 78%, p =0.838), however, White concordant pairs where less likely to have barriers present compared to White discordant pairs (41% vs. 72%, p <0.0001). Conclusions: Non-White women have more barriers documented by a Navigator compared to White women. The lack of association between racial/ethnic concordance and identification of barriers may reflect differences in burden of barriers found in racial groups rather than racial/ethnic concordance. Our future analyses will include a larger sample size and thus address the limitation of our conclusion for racial/ethnic concordance pairs. Implications for Policy, Delivery or Practice: Our findings suggest that Non-White women may have more barriers to care compared to White women, supporting cancer care intervention efforts for racially/ethnic groups. Future studies, with a larger sample size, can help inform how racially/ethnic concordant patient and navigator pairs are associated to barriers to care. Funding Source(s): NCI Poster Number: 203 National Scan of Efforts to Reduce Health Care Disparities Presented by: Sarah Scholle, M.P.H., Dr.P.H., Assistant Vice President, Research, National Center for Quality Assurance, 1100 13th St. NW, Suite 1000, Washington, DC 20005; Phone: (202) 955-1726; Email: scholle@ncqa.org Lead Author: Jessica French Co-authors: Esther Han, M.P.H.; Ignatius Bau, J.D.; Sarah Hudson Scholle, M.P.H., Dr.PH. Research Objective: Despite continuing evidence that health care disparities persist, little progress has been made to close the gaps in the quality of health care delivered to racial, ethnic and linguistic minorities. Our objective is to catalogue current national-level efforts to reduce health care disparities, and to identify gaps and opportunities to accelerate progress in closing the quality chasm. Study Design: We conducted an internet search of disparities reduction efforts and classified each effort we found by the nature of the project, target audience(s), and topic(s) addressed. Iterative reviews by experts in disparities identified missing efforts and helped classify them. We tabulated the efforts in each category and conducted cross-tabs to understand the full range of activities. Finally, we conducted interviews with experts on their interpretation of our results and obtained their recommendations for actions to accelerate progress. Population Studied: We sought national-level efforts using the following search terms: cultural competency; language access; health care disparities; health care equity; culturally and linguistically appropriate services (CLAS); multicultural health care; minority health; health care for underserved; health care for vulnerable populations. We excluded initiatives with diseasespecific, population-specific or organization-specific foci and efforts related to the social determinants of health disparities and efforts that were solely focused on research. Principal Findings: We found activity in all categories, with more activity focused on planning, evaluation, training or education, and fewer efforts focused on implementing practice changes. More efforts targeted health care professionals and policy-makers, and few targeted consumers. We identified some efforts to develop standards of performance. Some of these findings reflect limitations of our methods. Our selection of national efforts excluded local activity that targeted consumers or focused on implementing change at a local practice level. Despite the many efforts underway, their impact on disparities has been negligible. Conclusions: Our experts identified severa l opportunities to accelerate improvement: The Department of Health and Human Services Office of Civil Rights could more proactively enforce Title VI anti-discrimination provisions. Health care executives need evidence of a return on the financial investment required to act. Employers, the primary purchasers of health care, need evidence that health care disparities affect their workplaces, and they need to know of potential interventions. Medicare and Medicaid have made small, periodic investments in disparities, but a continued priority focus is needed to sustain performance improvements. Consumers need to know that disparities exist and what they can do about them. The HITECH Act and a recent Institute of Medicine report recommending standardized collection and reporting of race, ethnicity and language data by health care organizations are potential catalysts for change through broader implementation of health information technology. Moreover, both the House and Senate versions of national health reform legislation include multiple provisions directed at reducing health care disparities. Implications for Policy, Delivery or Practice: There are many potential sources of leverage, but ultimately , sustained investment in quality improvement and practice transformation, together with increased engagement of purchasers and consumers, will be necessary to effect significant progress in reducing health care disparities. Both investment and engagement depend on demonstrating the link between disparities and each stakeholder’s priorities. Funding Source(s): The California Endowment Poster Number: 204 Using Search Engine Query Data to Track Pharmaceutical Utilization Presented by: Nathaniel Schuster, B.S., Medical Student, University of Michigan Medical School, 507 Glen Court, Ann Arbor, MI 48104; Phone: (952) 237-8648; Email: nschu@med.umich.edu Co-authors: Mary Rogers, Ph.D., M.S.; Laurence McMahon, Jr, M.D., M.P.H. Research Objective: Since patients consult the internet for health information, Google search behavior might correlate with healthcare utilization. As a test case, search engine query data for search terms “Lipitor” and “simvastatin” were evaluated for temporal and geographic correlation with benchmarks of resource utilization. Study Design: Using 2004-2008 Google Trends and Google Insightsfor Search data, search terms "Lipitor" and "simvastatin" were evaluated for change over time. Then, query data was tested forcorrelation with Lipitor revenues. Finally, query data of 26 US metropolitan areas was tested for correlation with service use per Medicare beneficiary as percent of the national average, a benchmark of geographic variation. Population Studied: Individuals using Google search engine 2004-2008. Principal Findings: Regression of the slopes of search engine query datafor search terms “Lipitor” and “simvastatin” were different pre-June 23, 2006(the day that simvastatin came off-patent) versus post-June 23, 2006(p<0.001). Lipitor's annual percent change in revenues for 2004-2008 correlated positively with Lipitor's average query index (p<0.01) and negatively with simvastatin’s average query index (p<0.05). Both geographic variation in the “Lipitor” query index and the “Lipitor” to “simvastatin” query index ratio for 26 metropolitan areas correlated with service use per Medicare beneficiary (both p<0.05). Conclusions: Query data shows search behavior correlates withpharmaceutical revenues and metropolitan area healthcare utilization. Implications for Policy, Delivery or Practice: This study suggests that search engine query data has the potential to provide researchers and policymakers with a novel data source for studying geographic variations in health care utilization which can highlight important characteristics of a community's culture in the use of healthcare. Search engine query data has great potential for research since it is available for free, in real-time, at researchers' fingertips. Poster Number: 205 The Intended and Unintended Consequences of Clinical Guidelines in Reducing Health Care Disparities Presented by: Rebecca Shackelton, Sc.M., Associate Research Scientist, Health Services and Disparities Research, New England Research Institutes, Inc, 9 Galen Street, Watertown, MA 02472; Phone: (617) 972-3119; Email: rshackelton@neriscience.com Co-authors: John McKinlay, Ph.D.; Lisa Marceau, M.P.H.; Carol Link, Ph.D. Research Objective: People of lower socioeconomic status (SES) carry a greater burden of disease in the United States than people of higher SES. Lower SES is associated with increased coronary heart disease, diabetes and overall mortality. Physician decision-making and physicians’ perceptions of their patients are affected by a patient's SES. Consequently, lower SES patients can experience inequality at two levels. Having thoroughly documented variations in clinical practice by SES, quality assurance experts and professional organizations developed lists of items that a physician ought to take when presented with a likely case of some disease. It was presumed that close adherence to these lists (guidelines) by individual practitioners encountering individual patients would eventually produce desirable standardization of medical care and eventually a reduction in the health care variations. The intended consequence of guidelines, indeed the raison d’être presented to gain provider acceptance, was the improvement in the quality of care and ultimately the reduction or elimination of healthcare variations. In this study we first examine whether clinical guidelines are achieving their intended consequences (reduction of health disparities). Second, we contemplate potential unintended consequences of clinical guidelines highlighting an important distinction between the stated purpose of some social action and their generally unrecognized but objective functional consequences. Study Design: As part of a factorial experiment we presented primary care doctors (n=192) with clinically authentic vignettes of a “patient” with already diagnosed diabetes with an emerging foot neuropathy systematically varied by patient SES. Their proposed clinical actions were compared with established practice guidelines for this clinical situation. Population Studied: We recruited a total of 192 primary care physicians, practicing with New York, New Jersey, and Pennsylvania, stratified by gender and level of clinical experience. Principal Findings: Physicians participating in our experiment were less likely to ask questions, give advice, prescribe medications, conduct examinations and testing, and refer the lower socioeconomic patients. After establishing the existence of these consistent socioeconomic disparities in the proposed management of the diabetes scenario, we found that reported use of practice guidelines had no measurable effect towards their reduction (one intended consequence). However, the reported use of practice guidelines appeared to precipitate more clinical actions without eliminating documented disparities. Conclusions: Principal reasons for the introduction of clinical practice guidelines were the desire to improve the quality of medical care and the reduction of well-documented healthcare disparities. From our experimental data and with respect to the management of diabetes, guidelines do not appear to be accomplishing their primary stated purpose. However, they do appear to ensure that more of everything is done (without reducing or eliminating healthcare disparities), and potentially contribute to the ever increasing costs of medical care. Implications for Policy, Delivery or Practice: Consistent with other research we find clinical practice guidelines are not producing a principal intended result, and may even produce unintended consequences. Funding Source(s): NIDDK Poster Number: 206 URBAN40: A Quasi-Experimental Study on the Population Health Impact of a Neighbourhood Programme in the Netherlands Presented by: Karien Stronks, Ph.D., Prof., Department of Public Health, Academic Medical Center, Meibergdreef 15, Amsterdam, Netherlands; Phone: +31205664892; Email: k.stronks@amc.uva.nl Co-authors: Anton Kunst, Ph.D.; Mariel Droomers, Ph.D.; Birthe Jongeneel, M.Sc.; Cees Hoefnagels, Ph.D. Research Objective: There is a widespread agreement that a policy aimed at tackling health disparities should focus on the social determinants that are considered the ‘root causes’ of health disparities, including education, income and the neighbourhood environment. Little is known about the extent to which policies aimed to change these determinants, so-called upstream policies, are effective in preventing health problems. In view of this, a window of opportunity was opened by the decision taken by the Dutch government in 2007, to spend several billion Euros to increase the liveability of 40 deprived districts, focusing on problems of housing, employment, education, integration and safety. From a public health perspective, this programme provides a ‘natural experiment’ to study the health effects of changing physical and social conditions at the neighbourhood level. Study Design: URBAN40 (acronym for Upstream policy Research on health and Behaviour Across disadvantaged Neighbourhoods (40)) will study the impact of the ‘40 districts plan’ in terms of prevention of health problems among the inhabitants. It uses a quasi-experimental, repeated cross-sectional design, based on routinely collected data. All 40 districts will be compared with 40 control districts, with regard to changes in living environment (neighbourhood conditions, unemployment rates, individual socio-economic position etc.), more specific health determinants (smoking, housing conditions, physical activity etc.) and the occurrence of health problems (quality of life, chronic diseases etc.). Population Studied: Inhabitants of 40 ‘intervention’ and 40 control neighbourhoods, aged 18 years and older. Principal Findings: A large number of health relevant measures within the 40 districts have been identified, including creation of green belts, sports facilities and employment opportunities, and housing improvements. In addition, the mechanisms through which the measures might have an impact on (determinants of) health have been specified, based on current knowledge on the link between social determinants and more specific health determinants on the one hand, and health problems on the other. These analyses show that the measures taken within the programme might affect the health status of the inhabitants through a material, social and psychosocial mechanism. The logic models specifying these mechanisms will be used to derive specific hypotheses as to the effect of these measures, to be tested in the quasiexperimental design. Conclusions: The measures taken within a policy programme aimed at the improvement of the liveability of deprived neighbourhoods in the Netherlands, potentially have an impact on the health status of the inhabitants in these neighbourhoods, even though health issues were not part of the policy programme. The actual health impact will be assessed in future analyses. Implications for Policy, Delivery or Practice: The relevance of this study is rooted in the opportunity to obtain more insight into the effectiveness of upstream interventions to prevent health problems. Funding Source(s): Dutch council for health research and development Poster Number: 207 Members’ Perceptions of Race and Ethnicity Data Collection by Health Plans in Massachusetts Presented by: Kalahn Taylor-Clark, M.P.H., Ph.D., Research Director, Engelberg Center for Health Care Reform, HVHC Initiative, The Brookings Institution, 1775 Massachusetts Avenue, Suite 600, NW, Washington, DC, DC 20036-2103; Phone: (202) 797-6072; Email: ktclark@brookings.edu Lead Author: Romana Hasnain-Wynia, Ph.D. Co-authors: Kalahn Taylor-Clark, M.P.H., Ph.D.; Ayodola Anise, M.H.S. Research Objective: To examine perceptions and concerns of health plan members about race and ethnicity data collection by health plans and assess members’ preferences for racial and ethnic categories. Study Design: Qualitative study using a moderator guide with specific questions about attitudes and preferences for race and ethnicity data collection. Focus groups were stratified by race and ethnicity and Spanish language. Themes were derived based on the series of questions in the guide and the participants’ discussions and comments. Analysis was guided by a grounded theory perspective. Population Studied: Six focus groups that included 54 total participants, all of whom belonged to either a private or public health plan. Backgrounds of individuals included the following groups: Caucasian/White, African American/Black, Chinese, Multiracial (Portuguese, Brazilian, Cape Verdean), Hispanic/Latino Spanish-speaking, and Hispanic/Latino English-speaking. Principal Findings: Emergent themes included: 1) Skepticism and concern about collecting data; 2) Utility of collecting data; 3) Members’ need to understand why health plans would collect these data; 4) Importance that health plans provide a clear explanation to members about data collection; 5) Concerns about privacy and confidentiality; and 6) Methods for how health plans should inform members about the collection of race and ethnicity data. Participant concerns about health plans asking their race and ethnicity focused on lack of transparency about how the information would and would not be used. Participants expected their health plans to explain, preferably in writing, why they were asking for this information. Participants reacted positively to health plans’ intent to collect data to improve care. Preferences for racial/ethnic categories (broad categories vs. more specific granular ethnicities) differed among the participant groups. Conclusions: Members have concerns about health plans asking for information on race and ethnicity, but they also understand the utility of using this information to improve care for diverse populations. Health plans can improve the process of and members’ confidence in collection of race and ethnicity data by: 1) Providing a clear rationale to members about why plans are collecting these data; 2) Describing how it would and would not be used; and 3) Adhering to a list of categories that strikes a balance between simplicity and enough granular detail to capture the demographic make-up of the community. Additional qualitative quotes from focus group participants provide context to the emergent themes. Implications for Policy, Delivery or Practice: Health plans play a central role in strategies to address racial and ethnic disparities in health care, which remain a national concern. The lessons learned in Massachusetts – where the Massachusetts Health Care Quality and Cost Council now requires all health plans to report race and ethnicity data – may be applied in other states and nationally as health plans design programs to systematically collect such data through direct reporting by their members. Funding Source(s): RWJF Poster Number: 208 A Qualitative Case Study of How Organizations Use Data on Race and Ethnicity to Reduce Disparities and Improve the Quality of Care Presented by: Ruth Thorlby, M.Sc., Senior Fellow in Health Policy, Policy, King's Fund, 11-13 Cavendish Square, London, England UK W1G 0AN; Phone: +442073072646; Email: r.thorlby@kingsfund.org.uk Co-authors: Selena Jorgensen, B.A.; Bruce Siegel, M.D., M.P.H.; John Ayanian, M.D., M.P.P. Research Objective: Healthcare organizations have been urged to reduce racial and ethnic disparities in the quality of care. A first step in this process is the collection and analysis of healthcare data by patients’ race and ethnicity. This study explored the experience of healthcare organizations that had collected, analyzed and used data to understand the challenges and benefits that these efforts foster. Study Design: In depth interviews were conducted with participants at various healthcare organizations across the United States. The organizations were a selected from a sample identified as being advanced in the collection and use of race/ethnicity data by a literature review and contact with expert informants. Up to five interviews were conducted at each organization and participants were asked about the process of collecting race and ethnicity data and how the data had been analyzed and used. Interviews were recorded, transcribed and analyzed for emerging themes using Nvivo 8 qualitative analysis software. Population Studied: 39 staff members at 8 organizations: a multi-site hospital network, two teaching hospitals, three health plans and two community health centers Principal Findings: Although the organizations were at varying stages of development in their use of race and ethnicity data, all reported that staff were comfortable collecting these data after appropriate training, and most patients were willing to report their race or ethnicity. All three health plans reported that direct data collection from all their members was difficult because of sensitivities on the part of some members about the potential uses of data and had supplemented the patient data with data based on proxy measures such as geo-coding. All organizations had attempted to analyze these data, usually by race stratification of quality indicators already in use. Some organizations had attempted to adjust for confounding factors while others had not. Some interpreted a disparity as any statistically significant difference between groups while others had set a threshold of a certain absolute percentage difference between groups. Some used ‘white’ patients as the comparator; others interpreted a disparity as any difference between the best performing group and other groups. Where disparities were revealed, data were often used to design and assess improvement initiatives. Where disparities were absent, some organizations had begun to develop new, more sensitive indicators based on the disparities literature. The community health centers reported challenges in finding resources for data analysis. All organizations believed the data could provide a much more robust underpinning for action on disparities. Conclusions: These healthcare organizations had all successfully collected data from patients but for health plans the process was more challenging. All organizations attempted to analyze their data but with very different methods and understanding of what constituted a disparity. Analyses of these data are perceived to provide a robust basis for action to reduce disparities within healthcare organizations. Implications for Policy, Delivery or Practice: Collection and analysis of patient-level data by race and ethnicity is possible at the level of the healthcare organization but community health centers may need extra resources while health plans may require new strategies, such as state mandates, to encourage members to share their data. The heterogeneity of approaches to understanding and measuring disparities poses a challenge and may require clearer guidance from accrediting or governmental agencies if disparities are to be addressed in a consistent and robust manner in healthcare organizations across the United States. Funding Source(s): CWF Poster Number: 209 Clinicians’ Views of an Intervention to Reduce Racial Disparities in Diabetes Outcomes. Presented by: Ruth Thorlby, M.Sc., Senior Fellow in Health Policy, Policy, King's Fund, 11-13 Cavendish Square, l, United Kingdom W1G 0AN; Phone: +442073072646; Email: r.thorlby@kingsfund.org.uk Co-authors: Selena Jorgensen, B.A.; John Ayanian, M.D., M.P.P.; Thomas Sequist, M.D., M.P.H. Research Objective: Interventions that improve clinicians’ awareness of racial and ethnic disparities and improve their communication skills are considered promising strategies for reducing disparities in health care. This qualitative study assessed clinicians’ views of an intervention involving cultural competency training and racestratified performance reports designed to reduce racial disparities in diabetes outcomes, as well as their perceptions of the causes and potential solutions to these disparities. Study Design: Interviews were conducted with clinicians who had recently participated in a randomized intervention to reduce racial disparities in diabetes outcomes. The clinicians worked with Harvard Vanguard Medical Associates (HVMA), an integrated multispecialty group practice based in eastern Massachusetts. Earlier studies with HVMA had shown that disparities in intermediate outcomes of diabetes (achieving adequate glycemic, blood pressure, and cholesterol control) had persisted despite the adoption of a quality improvement program (electronic medical records and chronic care model). To address these disparities, 62 clinicians were randomized to receive cultural competency training and monthly race stratified performance reports for one year. After the randomized study was concluded, we conducted semi-structured interviews with clinicians. Interviews were transcribed and analyzed for emerging themes using Nvivo 8 software. Population Studied: 17 clinicians from the original intervention group, of whom 12 were physicians, 4 were Nurse Practitioners, and 1 was a Physician Assistant. Principal Findings: Most clinicians acknowledged the presence of racial disparities in diabetes control among their patients, but a small number rejected this premise or believed that race was not the root cause of any perceived differences between groups. Those who did accept that there were disparities described a complex set of causes, including socioeconomic factors such as low incomes, living in areas with poor access to fresh food and limited opportunities to exercise. Other factors mentioned included low levels of trust in the medical profession, poor eating habits, communication barriers due to language and low literacy. The clinicians perceived only some of these causes to be within their power to change, such as switching patients to less expensive generic drugs. Clinicians were able to identify additional services or programs that would help them address disparities, for example culturally tailored nutrition advice, outreach to patients within their communities, and group visits to allow patients to learn from each other. Some clinicians challenged the premise of the intervention, focusing on socioeconomic factors as the primary cause of disparities, rather than patients’ race. The performance reports and training were generally well received but some clinicians did not feel empowered to act on the information presented. Conclusions: Cultural competency training and performance reports may raise clinicians’ awareness of racial and ethnic disparities but may not be sufficient to empower them to make a measurable impact on reducing disparities in health care outcomes. Implications for Policy, Delivery or Practice: Organizations committed to reducing disparities may need to employ strategies that offer concrete initiatives to improve patient access along with clinician-focused interventions such as enhanced information and training for their clinicians. Clinicians should be seen as a source of ideas for action based on their insights about why disparities may be occurring among their own patients. Interventions that are built on clinician action also need to respond to those clinicians who have doubts about the role of race as a driver of poor outcomes or access. Funding Source(s): CWF Poster Number: 210 Disparities in Labor Analgesia Utilization Presented by: Paloma Toledo, M.D., Postdoctoral Fellow, Institute for Healthcare Studies, Northwestern University, 251 E. Huron Street F5704, Chicago, IL 60611; Phone: (312) 472-3585; Email: p-toledo@md.northwestern.edu Co-authors: Cynthia Wong, M.D.; William Grobman, M.D., M.B.A.; Romana Hasnain-Wynia, Ph.D. Research Objective: There is evidence that there are racial/ethnic differences in the use of epidural analgesia for labor pain relief. However, the reasons for this disparity have not been described. The purpose of this study was to evaluate the factors that influence decisions regarding management of labor pain in patients of different racial/ethnic backgrounds. Study Design: A survey was developed based on existing validated surveys that included domains for socioeconomic status, assimilation, acculturation, trust, and family cohesiveness. Questions regarding knowledge of labor analgesia were developed. The survey underwent expert panel review. Cognitive interviews were conducted with members of the survey population for content validity. The final survey was administered via face-to-face interviews with women admitted for labor and delivery who had not yet requested labor pain relief. The method of labor analgesia utilized was recorded after delivery. Groups were compared using the KruskalWallis statistic. After univariable selection, significant variables were entered into a multivariable logistic regression model to determine predictors of epidural analgesia utilization. Population Studied: English-speaking laboring women admitted to Northwestern Memorial Hospital in Chicago: 224 Caucasians, 71 Hispanics, and 53 African-Americans were interviewed. Principal Findings: Caucasian patients were more likely to be married, have a higher level of education, higher income, and have private health insurance than the other groups (P<0.001). The rate of epidural analgesia utilization was 92%, 73%, and 77%, respectively, in the Caucasian, Hispanic and African-American patients (P<0.01). Despite expecting more pain during labor than Caucasian women, Hispanic and African-American women were more likely to report that they would not use epidural analgesia (P<0.001). Patients reported with equal frequency that providers discussed labor analgesia, however Caucasian patients were more likely to use of prenatal classes and books as sources of information, and were more likely to consult with their family members in their decision making (medical and non-medical) (P<0.01). African-American patients trusted their physicians less than Hispanic and Caucasian patients (P<0.01). In contrast, Caucasians trusted their insurance plans less than Hispanic or AfricanAmerican patients (P<0.001).The multivariable analysis indicated that the method of labor analgesia the patient expected to use was a significant predictor of epidural analgesia utilization (OR 42.4, 95% CI 11.2, 159.7), as was consulting with family when making decisions (OR 20.6, 95% CI 1.42, 297.9), and higher income (OR 1.4, 95% CI 1.1, 1.8). Women with less trust in physicians were less likely to receive epidural analgesia (OR 0.22, 95% CI 0.08, 0.61). Conclusions: A racial disparity in labor epidural utilization exists and appears related to pre-existing expectations, sources of information, and physicianpatient relationships. Implications for Policy, Delivery or Practice: Further research should explore the promising methods and means for educating women about labor analgesic options in pregnancy. Funding Source(s): Evergreen Grant Poster Number: 211 Underutilization of Cancer Screening among Individuals with a Family History of Breast and Colorectal Cancer Presented by: Jennifer Tsui, M.P.H., Doctoral Student Researcher, School of Public Health, Department of Health Services, University of California, Los Angeles, 650 Charles Young Drive South, Room A2-125 CHS Box 956900, Los Angeles, CA 90095-6900; Phone: (310) 206-2165; Email: jentsui@ucla.edu Co-authors: Ninez Ponce, Ph.D., M.P.P.; Sara Knight, Ph.D.; Aimee Afable-Munsuz, Ph.D.; Uri Ladabaum, M.D., M.S., Robert Hiatt, M.D., Ph.D.; Jennifer Haas, M.D. M.Sc. Research Objective: Disparities in cancer screening among average risk populations have been well-established in the literature. Less is known about whether and to what extent sociodemographic and healthcare market factors, such as having insurance or a recent doctor visit, explain variations in screening among adults who report a family history of cancer and may be at higher risk. This study aims to identify segments of this population who are vulnerable to breast and colorectal cancer screening underuse, and who could benefit from targeted cancer prevention efforts. Study Design: Retrospective, cross-sectional analysis of self-reported data from the 2005 California Health Interview Survey (CHIS). Breast (BC) and colorectal cancer (CRC) screening underuse were evaluated separately using weighted multivariate logistic regression models accounting for individual factors among adults reporting moderate or high risk family history. We use the CDC Risk Stratification Tool to categorize average versus moderate or high risk individuals. Screening underuse was defined for BC as women with a family history of breast and/or ovarian cancer who did not receive a mammogram within the past 2 years; for CRC as adults with a family history of colon cancer who did not receive a sigmoidoscopy within the past 5 years or a colonoscopy within the past 10 years. Population Studied: Adult participants from the CHIS 2005 cancer control module. BC screening analysis included women, ages 40-64 years old, with a family history of breast and/or ovarian cancer and no personal history of breast cancer. CRC screening analysis included adults, ages 50-64 years old, with a family history of colon cancer and no personal history of colon cancer. Principal Findings: Low income (0-99% of the Federal Poverty Level (FPL)) women with a family history of breast and/or ovarian cancer had higher odds (OR 2.40; 95%CI:1.07-5.35) of mammography underuse compared to women with higher income (FPL >300%). Compared to women in urban areas, women in rural areas had increased odds of underuse (OR 1.68; 95%CI:1.03-2.75). No significant differences were found in mammography underuse by race/ethnicity. Among adults at-risk for CRC, Latinos have increased odds of screening underuse (OR 3.44; 95%CI:1.51-7.84) compared to non-Latino whites. Similar to mammography underuse, low income adults at-risk for colon cancer had higher odds of underuse (OR 3.20; 95%CI:1.24-8.24) compared to those in the highest income level. In both models, healthcare market factors were associated with higher odds of screening underuse. Conclusions: We found both healthcare market and sociodemographic disparities in screening among individuals with a family history of breast and colon cancer. Healthcare market factors have been found in a national population-based study on breast cancer, but the sociodemographic disparities we found in the diverse California sample of higher risk adults is a new finding. Implications for Policy, Delivery or Practice: With the advent of new technologies targeting diagnostics and therapies for familial cancers, disparities in uptake of these new technologies may widen by sociodemographic factors. It is important to continue to target low-income, underinsured and Latino (for CRC) populations with higher risk of cancer. Healthcare reform that incorporates coverage gains would help to ensure cancer screening disparities do not widen. Funding Source(s): NCI Poster Number: 212 and patients for their input, to lead to targeted interventions. Population Studied: The population included 1274 patients, 47% are White, and 42% are Black. All patients recieve care at the UNC Family Medicine Center. Principal Findings: Black and White patients differed (p<.001) in all measures of disease control: proportions with HbA1c>9 (21.7% vs. 10.1%, respectively), HbA1c<7 (47.3% vs. 60.2%), diastolic BP>90 (21.5% vs. 12.0%), LDL>130 (21.9% vs. 13.8%), LDL<100 (60.8% vs. 51.1%) but also HDL>45 (66.8% vs. 54.4%). Stratified analyses showed significant differences in the magnitude of black-white differences across the clinic’s four provider teams. Conclusions: These findings of racial group differences in diabetic outcomes were presented to the clinic’s providers and staff and focus groups are now being held with Black patients of the clinic. Beyond staff education, interventions will be devised based on recommendations by staff, providers and patients, and future outcomes monitored for narrowing of race-group differences. Implications for Policy, Delivery or Practice: This unique quality improvement effort could be used as a model for improving health care disparities within individual medical systems. Funding Source(s): UNC Internal Grant Poster Number: 213 Identifying and Reducing Differences in Disease Control Between Black and White Diabetic Patients of the UNC Family Medicine Center: A UNC ERACE Disparities Initiative Presented by: Amy Wallace, M.D., M.P.H., Senior Scholar, Veterans Rural Health Resource Center-Eastern Region, Veterans Affairs Medical Ccenter, 215 N. Main Street, WRJ, VT 05009; Phone: (802) 295-9363 ext. 6072; Email: aew@dartmouth.edu Co-authors: Anselm Beach, M.S. Presented by: Eddie Turner, M.D., Fellow, Family Medicine, University of North Carolina, 590 Manning Drive, Chapel Hill, NC 27599; Phone: (919) 966-4363; Email: ejturner@med.unc.edu Co-authors: Donald Pathman, M.D., M.P.H.; Bonzo Reddick, M.D., M.P.H.; Randall Teal Research Objective: The methods of quality improvement have been proposed as one approach for identifying and then addressing health care disparities within a given clinical organization. This project uses quality improvement approaches to identify and address disparities for Black and White diabetics who receive care at UNC’s Family Medicine Center, through analyses of its diabetes registry. Study Design: Black and White patients were compared on group proportions meeting NCQA target thresholds for glucose, hypertension control and lipid control. Additional statistical analyses explored possible reasons for group differences, and then findings were presented to practitioners Rural-Urban, Demographic, and Socioeconomic Disparities in Lifestyle Counseling for Overweight and Obesity During Preventive Care Visits Research Objective: Overweight and obesity have reached epidemic proportions and are associated with serious health and social consequences. Obesity is especially prevalent among rural, minority, and socioeconomically disadvantaged populations. Achieving and maintaining a healthy weight by adopting healthy lifestyle habits may prevent later obesity-related problems and reverse existing ones. Encouraging lifestyle changes through proper nutrition, exercise, and weight loss, is the recommended initial approach for providers treating overweight patients. We examined the likelihood of lifestyle counseling among patients age 18 and older across rural/urban locales, gender, racial/ethnic groups, median ZIP Code income, educational, and poverty levels during preventive or primary care appointments. Study Design: We used a cross-sectional study design to examine likelihood of lifestyle counseling during preventive and primary care visits for non- pregnant overweight and obese adults from the 2006 and 2007 National Ambulatory Medical Care Survey database. We calculated odds ratios to describe providers’ likelihood of lifestyle counseling during preventive/primary care visits across ruralurban residence locale, demographic, and socioeconomic characteristics described above. Population Studied: We extracted 11,203 records representing 832 million preventive and primary care visits for non-pregnant patients age 18 and older with BMI>25 or diagnosis of obesity. Of these, 2,939 records representing approximately 103 million visits included lifestyle counseling. Principal Findings: Providers offered lifestyle counseling in only 26% of preventive or primary care visits with overweight and obese patients. Across all demographic and socioeconomic categories, providers were 44% more likely to counsel suburban-dwelling overweight patients (p<.0001) and 63% more likely to counsel urban patients (p<.0001) compared to rural patients. Adjusting for multiple demographic and socioeconomic variables, odds ratios for lifestyle counseling was 1.31 (p=.0004) for suburban and 1.42 (p<.0001) for urban patients compared to rural patients who were overweight or obese. Providers were significantly more likely to counsel overweight Hispanic compared to Whites (OR=0.61, p<.0001 or Asians (OR=0.51, p=.006), and equally likely to counsel Blacks compared to other races. Patients ages 40 to 59 were more likely to receive counseling compared to patients ages 18 to 40 (OR=1.24, p=.009) but those ages 60 and older were equally likely to receive counseling. Providers were equally likely to counsel overweight men and women. Among socioeconomic variables examined: percent community poverty, median community income, median community educational level and insurance type, none were significant predictors for lifestyle counseling. Conclusions: Overall, providers are neglecting lifestyle counseling for overweight and obese patients during preventive care visits. Providers may be stretched for time, or doubt the effectiveness of their efforts; however, we question whether these justifications explain why providers offer counseling to some overweight patients and not others. When provided, only Hispanic ethnicity, middle age, and urban residence locale predict for higher likelihood of receiving counseling. With and without adjustment for other demographic and economic variables, rural populations are significantly less likely to receive lifestyle counseling directed at nutrition, exercise, and weight loss. Implications for Policy, Delivery or Practice: Given the high prevalence of overweight and obesity in rural America, providers treating overweight rural patients should encourage healthy lifestyle habits through counseling during preventive and primary care visits. Funding Source(s): VA Poster Number: 214 The Distribution of Medicare Beneficiaries Across Plans by Race and Ethnicity Presented by: Robin Weinick, Ph.D., Senior Social Scientist and Director of Public Sector Initiatives, 1200 South Hayes Street, Arlington, VA 22202; Phone: (703) 413-1100 ext. 5151; Email: rweinick@rand.org Co-authors: Marc Elliott, Ph.D.; Amelia Haviland, Ph.D.; Katrin Hambarsoomian, M.S.; Elizabeth Goldstein, Ph.D. Research Objective: We assess the extent to which the racial/ethnic composition of Medicare Advantage (MA) and Part D Prescription Drug (PDP) plans reflect that of their service areas, particularly the the extent to which plans systematically underrepresent or overrepresent minority beneficiaries-Blacks, Latinos, or Asians/Pacific Islanders (API). Study Design: We estimate three-way crosstabulations of self-reported race/ethnicity, Medicare contract (“plan”) and county of residence using 451,902 responses to the 2009 Medicare CAHPS, poststratified to represent all 46 million Medicare beneficiaries using CMS administrative race/ethnicity and other administrative variables. This permitted estimates of the self-reported racial/ethnic composition of 541 MA and 82 PDP plans, and estimation of the racial/ethnic distribution of all Medicare beneficiaries in the geographic area in which each plan operates. For each plan, we defined its geographic service area as the set of counties in which it had enrollees. Within this area, we calculated the racial/ethnic distribution by weighting all Medicare beneficiaries at the county level by the geographic distribution of the reference plan, giving greater weight to the counties in which the plan was most active. We used scatterplots and correlations to compare area and plan racial/ethnic proportions. Population Studied: Medicare beneficiaries Principal Findings: Within MA and PDP plans, the proportion of Medicare beneficiaries from various racial/ethnic groups is highly correlated with the racial/ethnic composition of their geographic service areas; the correlation coefficient for Latinos is 0.91 (0.98) for MA plans (PDPs); for African Americans 0.85 (0.61); and for Asians 0.83 (0.99), p<0.0001 in all instances. No plan underrepresents Blacks, Latinos, or API by 20 percentage points relative to their service areas, but of 541 MA plans, 40 enroll a minority group at proportions 30 percentage points or more higher than the corresponding proportion in the service area. For example, a plan with 61% API members operates in a service area in which 11% of Medicare beneficiaries are API. A few plans’ enrollees consist almost solely of Latinos or API (e.g. 96% Latino enrollment in a 23% Latino service area); these plans overtly specialize in these groups’ needs. No PDPs enrolled a minority group in a proportion that exceeded the overall rate in its service area by 30%. Conclusions: Our findings indicate little cause for concern that some MA and PDP substantially underserve particular racial/ethnic groups. However, we do find that certain MA plans disproportionately draw specific racial/ethnic minorities. This is particularly true of Latinos and Asians, for whom plans with certain services – such as customer service representatives who speak languages other than English may be more attractive. Plans that concentrate Blacks may do so via marketing efforts. The relatively large service areas for PDPs may limit the ability to concentrate by race/ethnicity. Implications for Policy, Delivery or Practice: For Medicare to contribute to reducing racial and ethnic disparities in the U.S., beneficiaries must have equal access to high-quality plan options. Our results reassuringly indicate that MA and PDP plans do not underrepresent minority enrollees. Future research should address the extent to which plans that concentrate and specialize in the care of minority beneficiaries provide better experiences for such beneficiaries than other plans. Funding Source(s): CMS Poster Number: 215 Breast Cancer Screening among Medicaid Managed Care Members with a Work-Limiting Disability Presented by: Sharada Weir, D.Phil., Assistant Professor, Center for Health Policy and Research, University of Massachusetts Medical School, 333 South Street, Shrewsbury, MA 01545; Phone: (508) 856-7852; Email: sharada.weir@umassmed.edu Co-authors: Heather Posner, M.S.P.H.; Jianying Zhang, M.P.H.; Georgia Willis, Ph.D.; Jeffrey Baxter, M.D.; Robin Clark, Ph.D. Research Objective: Examine evidence of disparities in breast cancer screening for an insured, but vulnerable, population of women enrolled in Medicaid because of a work-limiting disability. Study Design: Individual-level data were obtained for women who met the National Committee for Quality Assurance’s 2007 Healthcare Effectiveness Data and Information Set (HEDIS) criteria for the breast cancer screening measure (i.e., female, ages 42-69 at the end of 2006, and continuously Medicaid-insured during 2005-2006). Compliance with screening guidelines was assessed for each individual using HEDIS criteria (i.e., at least one routine mammography screening in 2005 or 2006). Disability status was determined from Medicaid eligibility records. We modeled mammography screening as a binomial logistic function with member characteristics, comorbidities, health services utilization, primary care provider type, and health plan as explanatory variables. Separate models for women with and without a work-limiting disability were also estimated. Adjusted odds ratios were computed from the logistic regression results. Population Studied: Massachusetts Medicaid Managed Care members meeting HEDIS criteria for breast cancer screening in the 2005/2006 measurement period (n=35,878). Principal Findings: Two-thirds of women in our data qualified for Medicaid because of disability. They were older (54 vs. 48 years of age, on average), and had higher rates of substance abuse/dependence (17% vs. 8%), smoking (16% vs. 10%), domestic violence (1% vs. 0.7%) and major depression (34% vs. 13%) than other women. Although unadjusted breast cancer screening rates were roughly equal for women with and without disability in Massachusetts, after adjusting for confounders disability status had a significant negative association with screening mammography (OR=0.76; p<0.0001). Several variables were important predictors regardless of disability status. Women with alcohol or drug use disorders had substantially lower odds of screening, as did those who smoked or had at least one emergency department visit. Having a higher overall illness burden or a diagnosis of domestic violence reduced the odds of screening for women with disabilities but not for non-disabled women. Both groups benefited from more ambulatory care visits, but the impact on screening was much larger among women with disabilities. Living more than 5 miles from a mammography facility was negatively associated with screening among women with a disability but not among those without. Living in an area with more college educated women was positively associated with screening in the nondisabled group but did not increase screening among women with disabilities. Conclusions: Our analysis provides evidence of disparities in routine mammography screening for women with disabilities and suggests several contributory factors. For instance, our finding on distance to screening facilities suggests that inadequate transportation may be one barrier. On the other hand, our finding on ambulatory visits suggests that provider efforts to promote screening are particularly effective for women with disabilities. Implications for Policy, Delivery or Practice: Nationwide, as of 2008, rates of routine mammography for Medicaid managed care plans averaged only 50-55%. Given that a majority of eligible women served by Medicaid have disabilities, and studies have shown that women with disabilities are more likely to be diagnosed with late stage disease, a focus on improving rates of screening for women with disabilities is overdue. Funding Source(s): MassHealth (Massachusetts Medicaid Agency) Poster Number: 216 Racial Disparity in the Quality of Diabetes Care: Do Physicians Treat Minority Patients Differently or Do Minority Patients Receive Care from Different Types of Physicians? Presented by: Weifeng Weng, Ph.D., Health Services Researcher, American Board of Internal Medicine, 510 Walnut Street Suite 1700, Philadelphia, PA 19106-3699; Phone: (215) 606-4134; Email: wweng@abim.org Co-authors: Bradley Gray, Ph.D.; Rebecca Lipner, Ph.D. Research Objective: Using patient-level chart audits, we examined disparities in quality of diabetes care received by minority (black nonHispanic, Hispanic) versus white patients from board-certified internists. We parsed these differences between physicians and within physicians’ patient panel. Study Design: We defined disparities as differences in quality of care measures after controlling for patients’ age and gender. We measured within versus between physician disparity by comparing results from linear-probability versus fixed-effects models, adjusting standard error for clustering of patients within physicians. We then utilized Blinder-Oaxaca decomposition to identify proportion of between physician disparity explained by physicians’ cognitive skills (equated score on first attempt of internal medicine certification examination; certification in endocrinology subspecialty), a practice-infrastructure measure (NCQA's Physician Practice Connections (PPC)), and insurance revenue source (% of revenues from Medicare and Medicaid patients). Quality measures included: intermediate-outcomes (A1C, blood pressure and LDL good and poor controls), diabetes care process (A1C test, lipid profile, eye and foot exam, nephropathy assessment) and preventive care (influenza and pneumococcal vaccination, nutrition and physical activity plan). Population Studied: In years 2008-2009, 774 internists completed American Board of Internal Medicine’s practice characteristics survey and Diabetes Practice Improvement Module with 17,896 chart audits and 774 physician surveys. Principal Findings: Overall, disparities in quality of care across racial/ethnicity groups as measured by process of care were small (<1%) except for black patients’ pneumococcal vaccination (difference=3.3%; SE=2.1%). However, a much different pattern emerged among intermediate-outcome measures for black patients in that they had worse intermediate-outcome measures comparing to whites with the largest disparity in blood pressure control (<130/80) (difference=-10.4%; SE=1.3%). Hispanic patients had worse outcomes in only the A1C measures relative to whites (e.g. A1C>9%: difference=7.1%; SE=1.3%). Most of the disparities in intermediate-outcome measures were due to variation within physicians’ panel of patients (mean within variation/total variation=75.8%) rather than between physicians. For example, black patients’ LDL <100: within difference=-6.4% (SE=1.2%) versus between difference=-2.3% (SE=0.8%). On average, our physician level factors explained 74.4% of between variation; insurance revenue source explained 55.9%, cognitive skills explained 24.4% while practice-infrastructure explained only 0.2% of this between variation. Conclusions: Do physicians treat minority patient differently? Do minority patients receive care from different types of physicians? There were no significant disparities observed in process measures between or within physician patient panels. However, blacks had significantly worse intermediate-outcome measures than whites while Hispanics had worse outcomes in A1C measures. Disparities in intermediate-outcome measures were largely due to variation within physicians’ patient panel rather than between. For intermediateoutcomes, the dominant physician level factor was insurance revenue source; practice-infrastructure explained little between-physician variation. Implications for Policy, Delivery or Practice: Our findings suggest that interventions targeted at improving intermediate-outcome measures rather than processes of care are more likely to address racial/ethnic disparity. The fact that between physician variation was small indicates that addressing disparity may require interventions targeted at meeting different needs of minority patients. Improving cognitive skills for boardcertified internists treating minority patients might somewhat reduce the between physician variation that do exist. Conversely, our results indicate that policies designed to improve practice infrastructure as measured by the PPC would not materially affect racial/ethnic disparities. Poster Number: 217 Infant Mortality in Appalachian States: The Influence of Poverty, Race/Ethnicity, and Geography Presented by: Nengliang Yao, M.S., Ph.D. candidate, Health Policy and Administration, The Pennsylvania State University, 604 Ford Building, University Park, PA 16802; Phone: (814) 380-1251; Email: ayao@psu.edu Co-authors: Marianne Hillemeier, Ph.D.; Stephen Matthews, Ph.D. Research Objective: Recent studies have found that health outcomes in Appalachia are disproportionately poor compared with those in the rest of the nation. While historic impoverishment is thought to be an important factor, the mechanisms underlying health disadvantage in Appalachia remain unclear. This study explores spatial inequalities in infant mortality rates over time among geographic sub-regions within the 13 Appalachian states, examining the influences of geographical location, county poverty level, and race/ethnic composition. Study Design: This study uses longitudinal countylevel data extracted from the Area Resource File, which contains data on variable of interest for the years 1976 through 2004. The dependent variable is the 5-year average infant mortality rate. Descriptive statistics are provided for the sampled counties, and hierarchical multiple regression models are fit incorporating interaction effects and spatial lags. The models test the impact on infant mortalities of sub-regional differences in geography, percent of the population in poverty, and the percent of the population who are African American, and examine interaction effects between location and poverty at four time periods: 1976-1980, 19871991, 1996-2000, and 2000-2004. Population Studied: The population of interest resides in 1064 counties of 13 Appalachian states: southern mountain region (N=184 counties), southern non-mountain region (N=197), central mountain region (N=89), central non-mountain region (N=66), northern mountain region (N=147), and northern non-mountain region (N=381). Principal Findings: Infant mortality rates decreased substantially in all sub-regions over the last three decades. The lowest and highest rates of infant mortality occurred respectively in the northern mountain region and southern non-mountain region. In general, mountain counties had lower infant mortality rates than non-mountain counties, except in the central region. Regional inequality of infant mortality persisted over time but decreased in more recent decades. In the multivariate regression analyses, higher poverty rate and percent African American were each predictive of higher rates of infant mortality in all regions at all time periods. No interaction effect of poverty and geographic location on infant mortality was found. Poverty played the most important part in predicting life chances for infants born in the regions studied. The percentage African American also had a significant effect on infant mortality rates however this effect declined over time. Living in the southern mountain region was associated with comparatively higher infant mortality during three out of the four time periods studied. Conclusions: Regional differences in infant mortality were mostly explained by the inequality in poverty rates and race/ethnic composition, but some regional differences remained significant. Controlling for other factors, the southern mountain region experienced excess infant death rates. Implications for Policy, Delivery or Practice: Understanding spatial inequality and changes in infant mortality at the county level provides useful information for health planning and policy development. In addition to poverty and disadvantage associated with race/ethnicity, policymakers in Appalachian states should also pay attention to health disadvantages associated with geographic region of residence. Poster Number: 218 Rural-Urban Differences in Access to Preventive Care Services Presented by: Jangho Yoon, Ph.D., M.S.P.H., Assistant Professor, Jiann-Ping Hsu College of Public Health, Georgia Southern University, Cone Hall, Room 1043, PO Box 8015, Statesboro, GA 30460; Phone: (912) 478-2416; Email: jyoon@georgiasouthern.edu Co-authors: Stuart Tedders, Ph.D. Research Objective: Previous research indicates that residents of rural areas are at greater risk of various health problems compared to their urban counterparts. Lack of access to preventive health care services has been suggested as one of the fundamental factors associated with rural-urban health disparities. The purpose of this study is to investigate rural-urban disparities in evidencebased utilization of preventive care services. Study Design: Data were derived from the 2008 Behavioral Risk Factor Surveillance System (BRFSS) which provides detailed information on utilization of preventive health care services for residents in all 50 states and the District of Columbia. The BRFSS is a random telephone survey of civilian, non-institutionalized adults, and uses a complex multi-stage cluster sample design. The sample used for this study includes 368,401 adults aged 18 to 64. Outcome variables include dichotomous indicators for a routine checkup within 2 years and clinically meaningful utilization of preventive care services for diabetes (influenza vaccine, pneumococcal vaccine, glycosylated hemoglobin check, and foot exam by a health professional) and cancer screening (mammogram, clinical breast exam, Pap test, blood stool test, and sigmoidoscopy). We estimated multivariate logit models, accounting for the complex survey design. Our key independent variables are residence categories which include rural and non-metropolitan urban residence. Residence in a metropolitan area served as a reference category. The residence variables were constructed using a 9-level ruralurban continuum classification scheme developed by the U.S. Department of Agriculture. To isolate the independent effect of rural residence, we controlled for a comprehensive set of demographic and socio-economic factors as well as health status. Population Studied: U.S. adults aged 18–64. Principal Findings: The likelihood of obtaining regular checkups decreased with rurality; lowest for rural residents (p < 0.01). For persons with diabetes, there was no significant association between rural residence and influenza and pneumococcal vaccination. However, rural residence was associated in a linear fashion with a greater likelihood of having glycosylated hemoglobin check and foot examination (p < 0.01). Regarding cancer screening, increased rurality was negatively associated with the likelihood of having mammogram (p < 0.05), clinical breast examination (p < 0.05), blood stool test (p < 0.01), and sigmoidoscopy (p < 0.01). Our results were consistent to different definitions of rural residence. Conclusions: Rural residents are less likely than non-rural residents to obtain clinically meaning levels of preventive care services, particularly regular checkups and cancer screening. Implications for Policy, Delivery or Practice: Continued efforts are needed to eliminate the current rural-urban gap in access to preventive care services. Improving regular checkups and cancer screening among rural residents, rather than targeting manageable chronic health conditions such as diabetes, may be more efficient use of limited public resources to address rural-urban health disparities. Poster Number: 219 Reasons for Refusals among Women Approached to Participate in a Postpartum Depression Intervention Trial Presented by: Amy Balbierz, Assistant Professor, Health Evidence & Policy, Mount Sinai School of Medicine, One Gustave L. Levy Place, Box 1077, New York, NY 10029; Phone: (212) 659-9567; Email: elizabeth.howell@msnyuhealth.org Co-authors: Jessica Block; Rebecca Tyrrell; Caron Zlotnick, Ph.D.; Elizabeth Howell, M.D., M.P.P. Research Objective: To determine reasons for refusals among mothers approached to participate in a postpartum depression intervention trial; and to examine whether racial/ethnic differences in reasons for refusal exist. Study Design: This is an ongoing randomized controlled trial of 530 Black and Latino, and 530 White and other minority postpartum mothers testing whether a behavioral educational intervention reduces postpartum depression. Participants randomized to the intervention arm receive a 2-step intervention that prepares and educates mothers about modifiable factors associated with postpartum depression (e.g. distress from physical symptoms, deficits in social support, low self-efficacy, and distress from infant colic), bolsters social support, enhances management skills, and increases participants’ access to resources. Participants are surveyed at 3weeks, 3-months, and 6-months to assess depressive symptoms and other factors. All women who refuse to participate in the trial are asked openended questions about their reasons for refusal. Responses were transcribed, reviewed for similar themes, arranged into distinct categories, and organized as a taxonomy of reasons for refusal. Racial and ethnic differences in reasons for refusal were then explored. Population Studied: Eligible participants are postpartum women who had uncomplicated deliveries at an urban hospital. Eligible subjects are women >18 years of age, English or Spanish Speaking, had working telephones, and had infants whose birthweights were > 2500 grams and 5minute Apgar scores >6. Bilingual research assistants recruit and consent patients during their postpartum hospital stay. Principal Findings: Of the 1061 women approached to participate in this study, 245 refused (23.1%), and 816 mothers enrolled in the trial. Refusal rates were higher for White and non-Black or non-Latino mothers (26.9%, 131/487 approached) versus Black and Latino mothers (19.9%, 114/574 approached). The taxonomy of reasons for refusals derived from patient responses has six main categories related to: 1) lack of interest, 2) having already been through childbirth before, 3) time commitment, 4) feeling overwhelmed, 5) patients moving from the area, and 6) confidentiality. The reasons for refusals did not differ by race/ethnicity; however, the rank order of reasons for refusal differed by race/ethnicity. Black and Latino mothers vs. White and other minority mothers were more likely to report that they were not interested in research (44% vs. 27%, p=.005) and less likely to report that the study was too much of a time commitments (33% vs. 51%, p=.005). Black and Latino mothers vs. White and other minority women were also less likely to report they felt too overwhelmed with their current situation to participate and more likely to report concerns about confidentiality. Conclusions: Although women from all racial/ethnic backgrounds refused to participate in this trial for the same sets of reasons, Black and Latino versus White mothers rank ordered reasons for refusals differently. Implications for Policy, Delivery or Practice: Tracking patient refusals and tailoring recruitment methods based on patient responses may improve recruitment of women from different racial/ethnic backgrounds for randomized controlled trials. Funding Source(s): NIMH Poster Number: 229 A Longitudinal Analysis of the Relationships Between Neighborhood SES, Neighborhood Residential Stability, and Mortality among Women in the U.S. Presented by: Chloe Bird, Ph.D., Senior Sociologist, RAND, 1776 Main Street, PO Box 2138, Santa Monica, CA 90407; Phone: (310) 3930411; Email: chloe@rand.org Co-authors: Regina Shih, Dr.PH.; Christine Eibner, Ph.D.; Beth Ann Griffin, Ph.D.; Mary Ellen Slaughter, M.S.; Tamara Dubowitz, Sc.D., Jose Escarce, Eric Whitsel Research Objective: A substantial literature finds that, even after controlling for individual-level factors such as income and education, neighborhood-level social conditions are associated with individual health. Yet, it is unclear whether key aspects of neighborhood environments such as neighborhood socioeconomic status (NSES) and residential stability each influence risk for specific causes of death. Therefore, we assessed the risk for different causes of death associated with both NSES and residential stability, adjusting for individual-level characteristics, including health status. We examined both all-cause and causespecific mortality to determine whether NSES and residential stability independently influence the risk of cardiovascular (CVD), cancer and accidental mortality. Such effects may operate through different social, behavioral and physiologic pathways. Study Design: Using 2-level hierarchical Cox proportional hazard regression models, we analyze the Women’s Health Initiative Clinical Trials (WHI CT) data, merged with neighborhood (Census tractlevel) data. We examined all-cause mortality using age at death, as well as age at death for each of the three leading causes of death in the WHI cohort: CVD, cancer, and accidents. The NSES index includes census tract-level socioeconomic measures. Residential stability is assessed as the percentage of census tract residents who lived in the same home 5 years earlier. We assessed the sensitivity of our findings to selection effects of both observed and unobserved covariates. Population Studied: Participants age 50–79 years were recruited (1993–1998) at 40 clinical centers and 36 satellite or remote sites, and followed through March 2005. We are examined data from 57,113 women (81.6% non-Hispanic white; 9.9% non-Hispanic black; 4.5% Hispanic; 4.0% other). At baseline, 60.8% were married, 94.4% had at least a high school education, and 63.6% had household incomes under $50,000. Principal Findings: Women in lower NSES neighborhoods experienced significantly higher risk of all-cause death, controlling for individual-level characteristics. Compared to residing in a neighborhood at the 75th percentile of NSES, living in one at the 25th percentile is associated with 1.13 times greater hazard for death (95% CI = 1.06, 1.19). In addition, living in a neighborhood with a higher residential stability was associated with decreased hazard for death (0.96; 95% CI = 0.93, 0.99), controlling for NSES. Additional analyses will examine the relationships between NSES, residential stability and cause-specific death. Preliminary analyses suggest that residential stability is not equally protective across the different causes of death. Conclusions: Living in a lower NSES neighborhood was independently associated with greater risk of death, suggesting policies that improve NSES may also yield health returns. In addition, the protective effect of living in a neighborhood with higher residential stability suggests that social aspects of stable communities are salutary and independent of NSES and individual-level socioeconomic characteristics and health status. Implications for Policy, Delivery or Practice: Our findings have implications for disease prevention and treatment, and suggest a need to pay greater attention to neighborhood contextual effects on women’s morbidity and mortality both clinically and in policy development. Further work is needed to assess what may be different mechanisms for increased risk of CVD-, cancer-, and accidentaldeath. Funding Source(s): NHLBI Poster Number: 230 Individual and Neighborhood Effects Associated with Stigma and Quality of Life among HIV-infected Urban African American Men Presented by: Aaron Buseh, Ph.D., M.P.H., M.S.N., Associate Professor, College of Nursing, University of Wisconsin-Milwaukee, 1921 East Hartford Avenue, Room 569, Milwaukee, WI 53211; Phone: (414) 229-5462; Email: aaronbg@uwm.edu Co-authors: Sheryl Kelber, M.Sc.; Patricia Stevens, Ph.D.; Chang Gi Park, Ph.D. Research Objective: Neighborhood characteristics are increasingly recognized as contextual factors necessary for understanding health, risk behaviors, disease patterns and treatment and prevention trajectories. This research uses a multidimensional approach to the understanding of quality of life among African American men living with HIV/AIDS by: (a) exploring and describing individual and neighborhood constructs influencing stigma and quality of life (QOL), and (b) developing and testing a model about the pathways of influence between individual and neighborhood factors in the experience of HIV stigma relative to QOL. Study Design: Cross-sectional descriptive survey design was used to examine selected sociodemographic variables, their association and influence on the quality of life among a sample of urban African American males. Questionnaires were administered assessing: individual factors, neighborhood social disorder; self efficacy; social stigma and QOL. Data were analyzed using descriptive and inferential statistics. Population Studied: Participants were recruited through a community-based organization in an urban setting a Midwestern state. A snowball sampling technique was used to obtain a sample of (n=117) African American men (18 years or older) who self-reported as being HIV-infected. Principal Findings: Participants ranged in age from 21 to 60 years (M=42.62, SD=8.25). The average length of time since diagnosis =13.17 years (SD=7.63). Over 75% of the men had at least a high school diploma. Over half identified their sexual orientation as bisexual or homosexual. Neighborhood effects, self efficacy, perceived stigma and current drug use were significantly correlated to QOL. Current drug users perceived more stigmas, less self efficacy and reported poorer QOL than non-drug users. Forty-one percent of the variance in QOL was explained by individual factors, neighborhood social disorder, self efficacy and stigma. Stigma mediated the effects of neighborhood social disorder on QOL and the domains of physical health and environment. Conclusions: Results from this study provide support for the need to recognize and address self efficacy, as well as stigma and neighborhood social disorder, including illicit drug use, to improve the quality of African American HIV-infected individuals’ lives. While focusing on clinical indicators of HIV disease and associated co-morbidities is undeniably necessary for improving quality of life for persons living with HIV/AIDS, it is not sufficient. We contend that a more multilevel conception of QOL is necessary, one that fully recognizes the large effects psychosocial and environmental variables such as self-efficacy, HIV stigma, and neighborhood social disorder can have in reducing quality of life for urban populations. Implications for Policy, Delivery or Practice: As AIDS becomes a manageable chronic condition it has become necessary to develop culturally appropriate, empirically validated models that will assist health practitioners in working to improve QOL among HIV infected African American men. Our findings demonstrate that neighborhood characteristics and stigma had negative effects on QOL while self efficacy contributed positively to QOL. Interventions are necessary that incorporates both individual and neighborhood factors. Funding Source(s): University of Wisconsin Graduate School Research Growth Initiative (RGI) Award, Proposal No: 01-075. Poster Number: 231 Prenatal Health Behaviors and Postpartum Depression: Is There an Association? Presented by: Rada Dagher, Ph.D., M.P.H., Assistant Professor, Health Services Administration, University of Maryland, College Park, 3460 14th Street NW, Apartment 233, Washington, DC 20010; Phone: (301) 405-1210; Email: radadagher@yahoo.com Co-authors: Edmond Shenassa, Sc.D., M.A. Research Objective: To investigate the associations of cigarette smoking, caffeine intake, and vitamin intake during pregnancy with postpartum depression at 7 weeks after childbirth. Postpartum depression is a common and debilitating mental disorder with a complex etiology; however, scarce research has examined its association with prenatal health behaviors. Study Design: Study participants were recruited from the postpartum floor at the Women and Infant's Hospital in Providence, Rhode Island, from 2005 through 2009. Eligible women were interviewed in-person while hospitalized for childbirth. A follow-up interview was conducted 7 weeks after delivery at each of the participants’ homes with a 79% response rate (N=622). Postpartum depressive symptoms were measured using the Edinburgh Postnatal Depression Scale. Ordinary Least Square (OLS) analyses were conducted to examine the associations between prenatal health behaviors and postpartum depressive symptoms. Population Studied: The study population consisted of all women delivering at the selected hospital. To participate in the study the mothers had to be at least 18 years of age, speak English, and agree to sign the consent form approved by the IRB. Principal Findings: The women averaged 28 years old, 46% were married, 31% had a college degree or higher, 76% were white, and 82% were born in the US. In regards to prenatal health behaviors, 38% of women smoke cigarettes, 62% drank coffee, 68% drank soda, 28% drank tea, and 81% took prenatal vitamins during their pregnancy. OLS analyses showed the following prenatal health behaviors were significantly associated with worse postpartum depressive symptoms: smoking cigarettes anytime during pregnancy and prenatal drinking of soda. Moreover, having an infant that refuses feedings, being stressed out by the responsibility of being a parent, and having difficulty balancing responsibilities because of one’s children, were stressors associated with worse depressive symptoms. Finally, having a lower level of education, being born in a country other than the US, and using both bottle-feeding and breastfeeding as compared to only bottle-feeding increased depressive symptoms. Conclusions: This study found a high percentage of women to be smoking during pregnancy and that there exists an association between cigarette smoking and worse postpartum depressive symptoms. Due to the cross-sectional study design that precludes causal inferences, it is possible that depressed women use smoking as a selfmedication mechanism or that smoking cigarettes results in changes in mood. Similar conclusions can be applied to the relationship between drinking soda and postpartum depression. Implications for Policy, Delivery or Practice: Issues for primary healthcare providers and clinicians to consider include evaluating women for risk of postpartum depression, identifying prenatal health behaviors such as smoking and drinking caffeine. Moreover, healthcare providers can advise women on the importance of seeking social support during the childbirth transition to cope with their new role as mothers and decrease their feelings of stress due to additional responsibilities. Future research should investigate the mechanisms that mediate the associations of smoking cigarettes and drinking caffeinated products with postpartum depression and explore other prenatal health behaviors such as alcohol intake, drug use, and exercise in relation with postpartum depression. Funding Source(s): Maternal and Child Health Bureau, Department of Health and Human Services Poster Number: 232 “The Best of Both Worlds: Women's Preferences for Medical Intervention in Childbirth Presented by: Alexandra Dalton, Ph.D., Postdoctoral Fellow, Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, 725 Martin Luther King Jr. Boulevard, CB# 7590, Chapel Hill, NC 27599; Phone: (919) 843-3392; Email: adalton@schsr.unc.edu Research Objective: Vital statistics data reveal trends towards both high- and low-intervention childbirths over the past 30 years. Though interesting, this data reveals little about women’s preferences for medical intervention during childbirth. This study sought to understand these trends of medicalization and demedicalization within the context of women’s decision-making and to uncover any dissonance between women’s preferences and birth realities. Study Design: This study was conducted a part of a larger, mixed-methods study on trends in the medicalization of childbirth. This study utilized semistructured, face-to-face interviews with 35 pregnant women to elicit information on their preferences for medical intervention during childbirth. Participants were recruited through emails sent to two listservs for parents and through word of mouth. Interview topics included childbirth preferences, factors affecting those preferences, and resources utilized in developing birth plans; some demographic information was also collected. Interviews were audio recorded and transcribed, and were examined using content analysis. Population Studied: The population of interest was pregnant women in the Triangle region of North Carolina. Participants ranged in age from 23-40 and were predominately white, married, and welleducated. Slightly less than half of participants were expecting their first child. Participants represented a variety of planned birth experiences, including a range of providers, locations, and preferences for medical intervention. Principal Findings: The majority of women interviewed reported wanting to attempt a natural (i.e. drug-free) birth. However, most of those women also wanted to be in a hospital with immediate access to medical interventions should they change their mind about pain management or require emergency care during childbirth. In other words, they are looking for the best of both worlds. Women who planned to give birth in a birth center or at home typically were concerned that, in a hospital setting, they would be pressured to undergo medical procedures (episiotomy, induction, etc.) that were not clinically necessary or pressured to undergo a cesarean section before other alternatives were exhausted. Some women who planned to give birth in a hospital planned to incorporate more holistic elements, such as hiring a doula or working with midwives, to ensure that the birth reflected their personal preferences to the greatest extent possible. Women reported that their preferences and plans for childbirth were most often affected by the experiences and recommendations of their friends, their partners’ preferences, logistic or practical considerations, and prior life experiences. Conclusions: The findings of this study suggest that many well-educated, white women are seeking the best of both worlds, with rescue technology available in a demedicalized environment. They prefer to give birth in a setting offering immediate access to medical intervention, but also want their personal preferences to be respected, when clinically appropriate. Implications for Policy, Delivery or Practice: Increased use of preference-sensitive, shared medical decision-making, when clinically appropriate, may help relieve the tension between women’s preferences and common medical practices. In addition, greater attention should be paid to promoting the options available to women during childbirth that may help address women’s needs, including alternatives such as birth centers, hospital-based midwifery practices, or nonpharmacologic pain relief techniques. Funding Source(s): Linda K. George Research Fund, Duke University Department of Sociology Poster Number: 233 Gender Differences in Use of Off-Pump and OnPump Cardiac Bypass Graft Surgery and Associated In-Hospital Mortality: U.S. Community Hospitals in 2007 Presented by: Bola Ekezue, M.P.H., Doctoral Student, Public Health Sciences (Health Services Research), University of North Carolina-Charlotte, 9201 University City Boulevard, Charlotte, NC 28223; Phone: (704) 905-0249; Email: bekezue@uncc.edu Co-authors: Jim Laditka, Ph.D, D.A., M.P.A; Sarah Laditka, Ph.D, M.A, M.B.A. Research Objective: A growing number of studies of coronary artery bypass graft (CABG) surgery suggest better outcomes for patients with off-pump surgery, compared to conventional on-pump surgery. There is some evidence that women may have lower risk with off-pump surgery. More research in this area is needed using nationally representative data. We examined gender differences in hospital mortality following on-pump and off-pump CABG surgery. A secondary objective was to examine whether differences in other characteristics explain the benefits of off-pump CABG in women. Study Design: Data were from the 2007 Nationwide Inpatient Sample (NIS), which includes all discharges from a 20% sample of U.S. community hospitals. Analyses, stratified by onpump and off-pump status, included chi-square and multivariate logistic regression weighted for national representation. The outcome was in-hospital mortality. The exposure variable of principal interest was gender. Controls included the number of coronary arteries bypassed, 21 comorbid conditions, demographic characteristics (age, race, health insurance, median household income), and hospital characteristics (CABG volume, teaching status, location). Population Studied: 50,237 adults ages 40+ with CABG surgery. Principal Findings: In-hospital mortality was significantly higher for women than for men for both on-pump (3.82%, 2.16%, p<.0001) and off-pump (4.71%, 2.90%, p<.0001). Women had 11% higher adjusted odds of having off-pump CABG than men (Odds Ratio, OR 1.11, 95% Confidence Interval CI 1.08-1.14); the analogous result for on-pump was OR 0.90, CI 0.88-0.92. Women had significantly higher rates of non-cardiovascular conditions and indicators of coronary disease severity. Among those with the off-pump procedure, adjusted mortality odds were 39% higher for women (OR 1.39, CI 1.25-1.55); among those with on-pump, the mortality odds for women were 44% higher (OR 1.44, 95% CI 1.35-1.54). Mortality risk factors for both CABG techniques were comorbid congestive heart failure, myocardial infarction, valve disorder, nutritional deficiency, electrolyte disorder and concurrent CABG/percutaneous coronary intervention procedure or valve replacement. Comorbid atherosclerosis in non-coronary vessels and chronic renal failure were risks for on-pump CABG. Among women: with off-pump CABG, Blacks had 81% greater odds of mortality than nonHispanic Whites (OR 1.81, CI 1.31-2.52); but 44% lower odds of mortality with on-pump (OR 0.56, CI 0.44-0.72). Among men: with off-pump CABG, Blacks had 106% higher odds of mortality (OR 2.06, CI 1.56-2.72); there was no analogous difference for on-pump CABG. Conclusions: Women having either on-pump or off-pump CABG have substantially higher risk of inhospital mortality than men. Black women and men both have particularly high risks of mortality following off-pump CABG. Implications for Policy, Delivery or Practice: Increasing evidence suggesting beneficial effects of off-pump over on-pump CABG is likely to cause more patients to request the off-pump procedure. Caution is suggested, as our findings indicate that Blacks with the off-pump procedure may have particularly high risk of in-patient mortality. Although we controlled for the number of coronary arteries bypassed and many relevant comorbid conditions, unmeasured differences in disease severity may have contributed to the results. More research is needed to explore the relationship between surgeon experience and adverse outcomes. Poster Number: 234 Patient Follow-Up Post Emergency Visit for Heart Failure (HF): Is there Gender Bias in Referral to Specialized Clinics? Presented by: Debbie Feldman, Ph.D., Associate Professor, École de Réadaptation, Université de Montréal, C.P. 6128 succ. Centre-ville, Montréal, Canada 3C 3J7; Phone: +5145282400 ext. 3935; Email: debbie.feldman@umontreal.ca Research Objective: Multidisciplinary HF Clinics are effective for managing this condition. On average, there are two to three times as many men than women in these clinics despite equal prevalence of HF. The objectives of our study were to: investigate whether men and women who had an emergency department (ED) visit for HF were subsequently referred to specialized HF clinics; describe when this referral occurred and explore factors that were related to prompt referral. Study Design: Within 6 weeks of discharge, participants were contacted and interviewed by telephone. The interview consisted of questions related to services (those received in the past, and any consultation or referral post discharge), sociodemographics, the Stanford self-efficacy scale, and the Minnesota Living with Heart Failure Questionnaire. The interview was repeated subsequently at 3 and at 6 months. In addition, a research nurse completed a standardized chart review at recruitment, 3 and 6 months. Analysis consisted of descriptive statistics regarding delays to referral, logistic regressions which modeled referral to the clinic at 6 weeks, 3 months and 6 months post ED visit as a function of gender, sociodemographics, severity, comorbidities, preferences regarding service providers and selfefficacy. Population Studied: Patients with HF were recruited by nurses in 8 hospital EDs in Quebec. Principal Findings: Of the 416 patients included in this study, 339 finished the 6 months follow-up period. Mean age of these 339 patients was 76.0 years (±10.5) and 50.4% were women. At 6 weeks post ED visit, 99 (24%) were referred to specialized HF clinics. This figure increases to 121 (31%) at 3 months and 128 (38%) at 6 months. More men were referred at each of these times (p < 0.0001). Multivariate logistic regression indicated that men were more than twice as likely to be referred within 6 months of their ED visit (adjusted OR 2.3, 95%CI 1.3, 4.2). Other factors associated with referral were younger age (adjusted OR 0.95, 95% CI 0.92, 0.98) and lower comorbidity (adjusted OR 0.84, 95% CI 0.75, 0.95). Conclusions: More than a third of patients (38%) with HF were referred to HF clinics within 6 months following their ED visit. Younger male patients with lower comorbidity are more likely to be referred to clinics. Implications for Policy, Delivery or Practice: Research has shown that these clinics benefit all HF patients. Standardized referral guidelines should be developed in order to ensure that these clinics are accessible to all patients who may require these services. Funding Source(s): CIHR Poster Number: 235 Using Collaborative Modeling to Improve Birth Outcomes Presented by: Rachel Ferencik, M.P.A., Research Associate, Georgia Health Policy Center, Georgia State University, P.O. Box 3992, Atlanta, GA US 30302; Phone: (404) 413-0307; Email: rachel@gsu.edu Co-authors: Heather Devlin, M.A.; Karen Minyard, Ph.D.; Chris Soderquist, B.S.; Angela Snyder, Ph.D., M.P.H. Research Objective: Despite being a rich nation, low birth weight trends in the United States resemble those in many of the world’s poorest and most impoverished countries. Many ways to improve healthy birth outcomes are known, including reducing unintended pregnancies, increasing birth spacing, reducing maternal smoking and improving access to comprehensive health care. Despite this knowledge, the number of babies born at low and very low birth weights is increasing. This project’s objective was to examine policy and program alternatives from a systemic perspective and to focus state efforts on the highest leverage opportunities to reduce low birth weight births, their complications and resulting economic and societal costs. Study Design: This collaborative modeling project was initiated by a state health agency. The collaborative systems modeling team includs state agency representatives, legislative staff and experts in maternal/child health, obstetrics, and epidemiology. The model groups women into four categories: women of child bearing age with and without a reproductive plan and women of child bearing age at risk or not at risk of a low birth weight birth. The model simulats movement between groups based on the impact of interventions to reduce low birth weight. Interventions were selected using a combination of data from clinical trials and program evaluations and expert consensus, where published evidence was lacking. Interventions could either improve the pre-conception odds of a woman having a normalweight birth or improve the post-conception odds that subsequent births would be of normal weight. Four preconception interventions were modeled: 1) increasing a woman’s general health knowledge; 2) increasing family planning coverage; 3) providing primary care during inter-conception; 4) increasing pregnancy health knowledge. Four post-conception interventions were also modeled: 1) improving pregnancy health knowledge; 2) implementing Centering Pregnancy Models; 3) home visits for high risk pregnancies; and 4) increasing Medicaid coverage for pregnant women. A simple user interface enables users to explore the interventions, alone or in combination and at varying intensities, in terms of their impact on low birth weight rates and the associated health care cost over the coming decade. The model is designed for real-time, hands-on exploration in a learning lab environment. Participants are encouraged to predict outcomes, articulate theories and inquire into any differences between their expectations and the model’s outcomes. Population Studied: Women of child bearing age Principal Findings: Preliminary results show that increasing the percentage of women with a reproductive plan begins to reverse the trend in low birth weight over the next ten years. We hypothesize that focused inter-conception care for women at risk of low birth weight will have a strong effect on reducing low birth weight. However, it is likely that multiple, intensive and sustained interventions will be required over time to achieve desired reductions in low birth weight. Complete results will be available in April 2010. Implications for Policy, Delivery or Practice: Using a collaborative system modeling process and perspective, this project brought together legislative staff, researchers, and content experts to develop a set of actionable policy options that can be used to inform state policy to reduce low birth weight. The resulting model provides a framework, a common language and a credible and accessible tool that enables interested stakeholders to engage in more rigorous discussions about effective and feasible interventions and policy options for reversing the trend of low birth weight. Funding Source(s): Georgia Department of Community Health Poster Number: 236 Emergency Department Utilization by Males May Drive Overall ED Utilization Rates Presented by: Kathleen Fuda, Ph.D., Sr. Associate, Health Policy Practice, Abt Associates Inc., 55 Wheeler Street, Cambridge, MA 02138; Phone: (617) 520-2493; Email: kathy_fuda@abtassoc.com Co-authors: Rachel Fisher, M.S., M.P.H., R.D. Research Objective: To determine whether gender plays a role in determining a state’s overall per capita utilization of emergency department (ED) visits. In 2005, annual statewide per capita ED visit rates varied widely, from a low of 262/1000 in California to a high of 642/1000 in West Virginia. Although per capita ED visit rates are higher among women than among men when measured nationally, it is not known whether gender-based differences in utilization patterns are consistent across the states, and whether total statewide utilization rates may be more closely linked to utilization by males or females. Study Design: We analyzed Massachusetts statewide data to determine age and gender utilization rates for all ED visits, including those resulting in admission, and compared them to national ED utilization rates as estimated by the NHAMCS. In addition, we used AHRQ’s HCUPNet tool to determine the number of ED visits by gender in the seven states for which data were available in 2005; used census estimates to derive gender specific utilization rates for each state; and compared them to the total ED utilization rates for each state. Population Studied: ED patients in Massachusetts, Hawaii, Iowa, Minnesota, Nebraska, New Hampshire, Utah, and Vermont. Principal Findings: Analysis of Massachusetts ED data showed that the state as a whole had a higher than average per capita utilization rate (425/1000 vs. 372/1000 nationally). However, Massachusetts females’ ED utilization was actually lower than the national average, while Massachusetts males had substantially higher per capita rates. This was not driven primarily by age distribution; females were at or below national averages in most age categories, and males were higher than average in every category except for children <15 years, so that the overall male per capita rate for all ages was higher than that for females, reversing the usual pattern (430/1000 for males vs. 383 for females/1000). Aggregate statistics for gender-specific ED visits in Massachusetts in 2005, and seven additional states available through HCUPNet, indicated that other states’ overall ED utilization are similarly correlated with disproportionately high percentages of ED visits attributable to males (r=.30). Hawaii is an outlier as the state with the second lowest ED utilization rate in the country in 2005; when it was removed from the data, the correlation was much stronger (r=.92). Conclusions: Gender may play an underrecognized role in driving ED utilization rates. The reasons why males in some states are disproportionately more or less likely to visit emergency departments compared to female residents of the same states deserve further exploration. Implications for Policy, Delivery or Practice: Most hypothesized drivers of ED utilization, such as poor access to primary care, geographical factors, payer type, injury and disease patterns, etc. may affect males and females differently, which should be considered in research and policymaking. In addition, there may be gender-specific beliefs or attitudes that may vary geographically and help to explain the patterns discovered. Finally, many attempts to discourage “inappropriate” ED visits, such as increased copayments, apply to all population groups regardless of utilization patterns; more targeted approaches might be more successful while minimizing negative effects. Poster Number: 237 Defining Caseload for Patient Navigation Presented by: Mary Howard, B.S., Research Assistant, Women's Health Unit, Boston University School of Medicine, 801 Massachusetts Avenue, Boston, MA 02118; Phone: (617) 638-8036; Email: mbhoward@bu.edu Co-authors: Karen Freund, M.D., M.P.H.; Christina Santana, M.P.H.; Kristine Beaver, M.P.H.; Sharon Bak, M.P.H.; Tracy Battaglia, M.D., M.P.H. Research Objective: Patient navigation is an innovative type of care management designed to reduce cancer disparities. As many sites adopt this model of care, a frequent query is how to assess appropriate caseload for these new positions. While data on the effectiveness of patient navigation interventions appears promising, there is a lack of literature that describes methods to assess appropriate caseload for optimal effect of navigator intervention. Boston University and its affiliated Community Health Centers (CHCs) is one of nine sites participating in the National Cancer Institute Patient Navigation Research Program (PNRP), which aims to develop and test navigation to reduce delays in delivery of standard cancer services after an abnormal breast cancer screening. The purpose of this study is to develop and apply measure of caseload comparable across settings, and describe the caseload across three CHCs with breast health navigators participating in the Boston PNRP. Study Design: A subset of Boston PNRP sites with patient navigation for breast cancer screening was the focus of this study. Navigators target female patients with abnormal breast cancer screening, with fewer than 10 cases annually navigated during treatment for breast cancer. Review of the literature identified several concepts to consider in navigator caseload: (1) a simple count of number of patients (2) total patient-days in navigation, (3) documented time spent navigating, and (4) complexity of navigated patients, as defined by problem (diagnostic evaluation versus cancer care) and number of barriers to care. We examined the following factors for each navigation site: absolute number of cases navigated, patient-days in navigation, and total documented patient-navigator encounters. A formula was developed to calculate caseload from the patient-days assessment: Total patient-days in navigation divided by Total days of observation divided by FTE of navigator. After a caseload score was calculated for each health center, we compared caseload by site to number of navigated patients, encounters, and complexity of navigated patients. Population Studied: Eligible participants were women over 18 with a Breast Imaging Reporting and Data System (BIRADS) 0, 3, 4, or 5 mammogram at the participating CHCs from 7/1/2007 through 6/31/2008. Patients were navigated until their screening abnormality was resolved with a definitive diagnosis (cancer or noncancer) or until the end of cancer treatment. Principal Findings: The calculated caseload scores were 26.3, 71.8, and 75.8 for CHCs A, B and C respectively. This large variation in caseload can be somewhat accounted for by numbers of navigated patients during this time frame (98, 175 and 248, respectively). The number of documented encounters by navigators did not correlate with the caseload score. Conclusions: The caseload scores for breast health navigation in Boston PNRP varied across CHCs. The caseload score correlates somewhat with number of patients, but may allow a better reflection of the complexity of the care needed for individual patients. Linking this measure with patient outcomes will better illuminate the range in caseload. Implications for Policy, Delivery or Practice: Developing an understanding of caseload is essential to implementing viable patient navigator programs. A calculation of caseload can also be linked to outcomes and the size of a navigator’s caseload can be controlled for in future analyses. Funding Source(s): NCI Poster Number: 238 Gender Differences in Management and Outcomes of Acute Myocardial Infarction Patients- The Role of Health Information Presented by: Nicole Huang, Ph.D., Associate Professor, Institute of Hospital and Health Care Administration, National Yang Ming University, 155 Li-Nong Street, Section 2, Taipei, Taiwan 112; Phone: +886228267372; Email: syhuang@ym.edu.tw Co-authors: Yiing-Jenq Chou, M.D., Ph.D.; ChengHua Lee, M.D., Dr.PH. Research Objective: Providing information or health knowledge to less advantaged patients has been suggested as a major strategy to reduce health disparities. Sex-based differences in access to care and outcomes reported by some studies have raised the concern of sexual discrimination against women. We wonder whether a higher level of medical information would help to narrow such “disparities,” while many argue that gender differences in medical care mainly result from clinical manifestation. In such cases, we would expect this difference to be observed among wellinformed women and men. Furthermore, whereas the existing evidences are limited mostly to western populations, due to heterogeneity in culture and traditional gender role patterns in Asian societies, gender issues in medical care may be more serious in Asian populations. The objectives of this study are to compare cardiac procedure use and mortality between men and women in a typical Asian population, and to determine whether such sex differences exist among health professionals and their relatives. Study Design: Retrospective analyses were conducted using the National Health Insurance data. for patients, who had been admitted to a hospital for acute myocardial infarction in Taiwan between 1997-2002. Main outcome variables included use of catheterization and revascularization within 1 year of the index admission, and 1-year mortality. Patient characteristics (age, gender, relationship to health professionals, comorbidity, residential region), physician characteristics (age, gender, specialty), and hospital characteristics (accreditation level, case volume) were adjusted in the models. Generalized Estimating Equations and Cox proportional hazard models were applied. Sensitivity analyses were also conducted for different age strata, and general patients with a higher socioeconomic status. Population Studied: Patients who had been admitted to a hospital for acute myocardial infarction in Taiwan between 1997-2007. Principal Findings: General Taiwanese women not only underwent fewer cardiac catheterization (+35.4% vs 59.7%; P<0.001) and revascularization (25.4% vs 47.4%; P<0.001) than men, but also had higher 1-year mortality rate (52.1% vs 19.1%; P<0.001). In contrast, sex differences in procedure uses observed among health professionals were much smaller in magnitude (catheterization: 38.1% vs 41.6%; P=0.59; revascularization: 23.8% vs 31.1%; P=0.24). Nonetheless, after adjusting for potential confounders, either general women or female professionals were considerably less likely to undergo cardiac catheterization and revascularization than their male counterparts. General women and female professionals had significantly higher mortality risks than their male counterparts. Sex differences observed in procedure use and mortality (P for interactions > 0.05) were not smaller when a patient was a health professional. Conclusions: Women who have had an AMI undergo an invasive procedure less often, and suffer a worse survival outcome than men in a typical Asian population. More importantly, sex differences persist among health professionals and relatives who are considered better informed and more privileged when they become patients. Implications for Policy, Delivery or Practice: The preliminary results suggest that the presence of similar gender difference among informed consumers may indicate factors such as clinical manifestation may be more plausible explanations for the observed gender differences in access to invasive procedures and outcomes. Funding Source(s): Taiwan National Science Council Poster Number: 240 Birth after Cesarean Section: Changes Over a TenYear Period in New Jersey. Presented by: Ya-lin (Aileen) Huang, M.S., Ph.D. candidate, Health policy and management, Emory University, 1518 Clifton Road Room 623, Atlanta, GA 30322; Phone: (404) 693-7546; Email: yahuang@emory.edu Research Objective: To determine whether the variation of choices of delivery methods among parturients with previous Cesarean section over time has impacts on related maternal and neonatal outcomes. Study Design: A retrospective analysis of all hospital births from 1997-2006 in New Jersey using discharge data from New Jersey State Inpatient Database (SID), part of Healthcare Cost and Utilization Project (HCUP). We compared maternal and neonatal outcomes between a trial of labor and elective repeat Cesarean delivery among women with previous Cesarean delivery. Outcomes of interest were maternal and neonatal mortality, major maternal complications such as hemorrhage, infection and thrombotic condition, major neonatal complications such as 5-minute Apgar score <7, respiratory distress syndrome and neonatal injury. All analyses are undertaken by year to assess trends over time. Population Studied: Women experiencing the next birth after at least one Cesarean section delivered in New Jersey hospitals between 1997 and 2006, and their neonates, as linked through hospital discharge data. We identify 142,121 deliveries with previous Cesarean section and 108,012 motherneonate pairs. Principal Findings: Over the ten-year period, the rate of successful vaginal birth after cesarean section (VBAC) declined significantly in New Jersey (31%-7%). Both the rates of maternal complication and neonatal complications declined over time. The neonatal mortality rate in babies whose mothers had a trial of labor was higher than those babies born after an elective repeated Cesarean section (OR=1.63; 95% CI: 1.11-2.64) although the absolute numbers are very small. There was no difference in maternal mortality risk between the two groups. Neonatal complications were more frequent in the trial of labor group, take respiratory distress syndrome for example (OR=1.44; 95% CI: 1.29-2.87). Conclusions: Rates of VBAC have declined over this ten-year period. Rates of maternal and neonatal mortality and morbidity are generally in the low range and improved over time. Implications for Policy, Delivery or Practice: Women may benefit from shared decision-making tools and enhanced physician-patient communication on the subject of comparative benefits and risks when determining their birth preferences after Cesareans. More research to predict which women are likely to achieve a successful VBAC is essential. Poster Number: 239 Understanding Women Veterans’ Use, and Unmet Needs, for Reproductive Health Services in the Veterans Administration Presented by: Kristin Mattocks, Ph.D., Associate Research Scientist, Internal Medicine, Yale University, 950 Campbell Avenue, 11-ACSLG, West Haven, CT 06510; Phone: (413) 548-6777; Email: kristinmattocks@yahoo.com Co-authors: Cara Nikolajski, B.A.; Sally Haskell, M.D.; Cindy Brandt, M.D., M.P.H.; Jennifer McCallHosenfeld, M.D.; Sonya Borrero, M.D., M.S. Research Objective: Women veterans constitute a growing population of VA users. Among other medical and mental health services, many women utilize the VA for reproductive health care services, including routine gynecological care, mammography, and infertility services. However, little is known regarding women’s knowledge of the availability of these services, nor the extent to which available services meet women’s needs. Therefore, the objectives of this study were to: 1) explore women veterans’ experiences with reproductive health services in the VA; 2) understand what reproductive health needs were not being met, and 3) assess how the VA could improve the scope and quality of reproductive health services offered to women veterans. Study Design: A series of focus groups consisting of 5-8 women veterans enrolled in the VA Healthcare System were conducted at VA Pittsburgh and VA Connecticut. The focus groups were audio-taped, transcribed, and analyzed to identify emergent themes. A standard protocol was used to ask participants to discuss: Reproductive health care services used at the VA, knowledge of the full range of reproductive health services available, barriers to receiving reproductive care, and recommendations for improvement of reproductive health care at the VA. Population Studied: Research participants included 21 women veterans, ranging in age from 29-46, receiving care in women’s health clinics at VA Pittsburgh and VA Connecticut. Principal Findings: Analyses revealed that many women veterans were unaware of the range of reproductive health care services available to them. While nearly all the women had received routine gynecological care from the VA, including Pap smears, contraception, and mammography, women had varying levels of knowledge and experience regarding pregnancy and infertility care. Several women were unaware that pregnancy and infertility care were available from fee-basis providers outside the VA. Women were generally satisfied with the care they received from VA providers for their reproductive health needs, though some women expressed dissatisfaction with the degree of gender-specific training among medical residents working in women’s health clinics in the VA. Recommendations for improved reproductive health care within the VA included readily available information detailing what reproductive health services are available, more flexible hours to meet women’s needs, and more extensive genderspecific training of medical residents providing care in women’s health clinics in the VA. Conclusions: Women utilize a broad array of reproductive health care services in the VA. However, we identified a number of important reasons why women may not be accessing the full range of reproductive health services available to them. Chief among these reasons was a perceived lack of available information regarding the full range of VA benefits available for reproductive health care. Implications for Policy, Delivery or Practice: The VA has made significant progress over the last decade to improve the quality of care it provides to its women veterans. The VA must make efforts to ensure that women are aware of the reproductive health services available to them, and that services provided through fee basis providers outside the VA are easily accessible and coordinated with ongoing VA care. Funding Source(s): VA Poster Number: 242 Comparing Primary Care Appointment Wait Time for Women Veterans When Both General Primary Care Clinics and Women’s Health Clinics Are Available Presented by: David Mohr, Ph.D., Center for Organization, Leadership and Management Research, VA Boston Healthcare System, 150 South Huntington Avenue (152M), Boston, MA 02130; Phone: (857 364-5679; Email: david.mohr2@va.gov Co-authors: Justin Benzer, Ph.D.; Marjorie Nealon Seibert, M.B.A.; Bert White, M.B.A., D.Min. Research Objective: Women Veterans comprise about 14% of the Veteran population. Many VA health care centers have changed structures and processes to provide care in women’s health clinics to meet the needs of this population. This study examines waiting times for VA medical hospitals and community clinics that provide both a general internal medicine clinic and a women’s health clinic in their primary care service. Study Design: We used administrative data for the study that was collected between October 2006 to September 2007. The outcome variables for this study consisted of average appointment wait time and the percentage of appointments completed within 31 days of request. We ran a Poisson regression to identify significant factors associated with longer waiting times, including type of clinic, four U.S. Census regional areas, urban or rural indicator, total number of appointments, new to established patient ratio, teaching hospital affiliation, and hospital or community-based designation. Population Studied: To be included, a site needed both a general internal medicine and women’s health clinic and at least 100 appointments by women Veterans during the 12 month period. A total of 155 sites were included. Only women patients seen in either of these two clinics were included. A total of 185,227 appointments were made to women’s health clinics and 313,150 appointments were made to general internal medicine for the study sites. Principal Findings: The average wait time was 7.21 days for women’s health clinics compared to 4.82 for general internal medicine clinics. The mean wait was longer in women’s health clinics (SD=4.14). Approximately 95.7% of appointments were completed within 31 days of request in women’s health clinics compared to 97.3% in general internal medicine clinics. The regression model for average appointment wait time indicated lower appointment volume, a higher rate of new patients, and western geographic region were associated with longer appointment wait times. Conclusions: For medical centers with both general internal medicine and women’s health clinics, the average wait time for women was slightly longer in women’s health clinics. Additional factors that influenced this relationship were appointment demand variables. The supply of providers was not modeled for each clinic in this study, but could be a contributing factor to the longer wait times. Another reason for the wait may have involved greater time to conduct genderspecific tests or procedures. Differences in procedures used between the clinics could be an area for further investigation to explain this difference as well as patient preference with choice of clinic and wait time. Implications for Policy, Delivery or Practice: Although the women’s health clinics had slightly longer waiting times, the difference was an average of 2.4 days. Possible factors that could reduce this wait may include staffing and resources in women’s health clinics. Funding Source(s): VA Poster Number: 243 DACOWITS: An In-Depth Analysis of Women in the Military Plan B as Insurance: The Effect of OTC Emergency Contraception on STIs and Abortions Presented by: Laura Nelson, M.P.H., Research Associate, Altarum Institute, 4401 Ford Avenue, Suite 800, Alexandria, VA 22302; Phone: (703) 575-1892; Email: laura.nelson@altarum.org Co-authors: Christina Borrelli, M.H.A.; Erin Haslag, M.P.H.; Karen Metscher, Ph.D.; Lorraine Babeu, Ph.D. Presented by: Anjali Oza, The University of Chicago, 211 E Ohio Street Apartment #2417, Chicago, IL 60611; Phone: (281) 961-0757; Email: aoza@uchicago.edu Research Objective: The objective of this study is to use quantitative data to identify significant differences in reported mental well-being, physical well-being and stress-levels between genders in the Military. Study Design: The Department of Defense's Health Related Behaviors (HRB) responses were used in an analysis (correlation, regression testing of the survey questionnaire responses). Random selection of 60 DoD Services installations with > 500 personnel assigned were sampled and grouped by Service, Major Command, and Region (CONUS/OCONUS) and 10 Coast Guard Installations Active-duty personnel randomly selected at installations based on pay grade and gender. The survey was administered anonymously on-site. The variables of interest included survey questionnaire measures for mental well-being, physical well-being and stress-levels. The sample frame includes 28,546 responses, with a response rate of 70.6% (vs. 51.8% in 2005 Survey). Significant differences in gender responses and patterns are detailed through the quantitative analysis. Population Studied: Active Duty Military Personnel (females) Principal Findings: The 2005 DACOWITS analysis reported significant health, stress-level and stressor differences existed between genders amongst Military personnel. The 2008 HRB data was recently released and the analysis of the significant differences will be analyzed, reported and compared to the 2005 data. Conclusions: There are significant (p-value >= 0.05) differences in stress levels and stressors encountered among the genders serving in the Military. Identifying key stressors and enacting policies to promote health and reduce stress is critical to sustaining the mission of our Military. Implications for Policy, Delivery or Practice: The primary objective of the DACOWITS analysis is to provide meaningful information that will enable policy makers and Military leadership to enhance, improve and continue to support women in the Military. Poster Number: 244 Research Objective: The United States has the highest number of unintended pregnancies and abortions among Western industrialized countries. Emergency contraception is 89 percent effective in preventing unintended pregnancy when taken within 72 hours of unprotected sex. In August 2006, the FDA announced that Plan B, commonly referred to as the “morning after pill”, would be made overthe-counter for women 18 and older. This paper argues that the introduction of over-the-counter access to Plan B lowered the risk of unintended pregnancy and thereby lowered the costs of unprotected sex. Consequently, the policy played a significant role in the decline in abortion between 2005 and 2007, but may have led to an increase in risky sexual behavior on the margin as women engaged in more sex and substituted away from contraceptive methods such as condoms, birth control pills, withdrawal, and abstaining from sex. This may have resulted in an increase in sexually transmitted infections (STIs). Study Design: I employ a difference-in-difference approach to explore the impact of pharmacy access to Plan B on STIs and abortions. My identification assumption relies on the trends for early and late adopter states being the same prior to the policy change. I include state level controls for public health infrastructure, funding for family planning, concentration of planned parenthoods, and number of abortion providers. I include county level fixed effects to control for time invariant county level attributes that may be correlated with risk behavior, policy uptake, or the effectiveness of the policy. Population Studied: I have a balanced sample of 1.5 million women followed continuously over time. I use claims data from MarketScan, the largest collection of employer-based patient data. Principal Findings: I find that improved access to Plan B accounts for as much as 37.2 percent of the decline in abortion and up to 17.8 percent of the increase in STIs between 2005 and 2007 among women ages 15-29. I perform a range of sensitivity analysis and robustness checks to address the concern that early and late states may not be comparable. I find that the results are consistent. The potential direct medical cost savings from Plan B use is $1.47 billion and the increase in medical cost from the subsequent rise in STIs would cost $283 million. Conclusions: I find that there are advantages and disadvantages to making a low-toxicity drug like Plan B available over-the-counter. Given the ethical debate surrounding abortion and given that some people believe Plan B is equivalent to termination, how we weigh the consequences of the policy really depends on how society places value on each outcome. Implications for Policy, Delivery or Practice: The findings are relevant for understanding how public health policy affects individuals’ incentives and for discussing the policy’s impact on direct medical costs to the healthcare system. Funding Source(s): AHRQ Poster Number: 245 Creating a Quality Measurement Strategy for Women of Reproductive Age Presented by: Sarah Scholle, M.P.H., Dr.PH., Assistant Vice President, Research, National Center for Quality Assurance, 1100 13th Street NW Suite 1000, Washington, DC 20005; Phone: (202) 955-1726; Email: Scholle@ncqa.org Co-authors: Natalie Davis; Dana Rey, M.P.H.; Beth Tapper, M.A.; Carol Weisman, Ph.D. Research Objective: Performance measurement is a powerful tool for driving improvements in the quality of care. The most commonly used quality measures for women of reproductive age focus on gender- specific preventive screenings and pregnancy-related visits; they do not consider the full range of women’s preventive needs. The purpose of this project was to identify a comprehensive framework for evaluating the quality of preventive care for women of reproductive age, including pregnancy-related care. Study Design: The National Committee for Quality Assurance (with funding from Centers for Disease Control and Prevention and Health Resources and Services Administration), working with the American Medical Association convened Physician Consortium for Performance Improvement, reviewed existing guidelines and measures for preventive and pregnancy-related care for women of reproductive age. A group of diverse stakeholders was convened to create a framework for prioritizing relevant measurement efforts. The workgroup discussed goals, principles, key priorities, as well as barriers, for quality measurement and improvement. Population Studied: Women of reproductive age Principal Findings: Based on the recognition that women’s overall health affects the woman and pregnancy-related experiences and outcomes, the panel recommended quality measurement should address the full range of women’s health care needs, including gender-specific needs as well as conditions where gender differences exist in prevalence, quality of care or outcomes. Second, issues of care coordination across multiple health care providers and across women’s life stages should be considered. Third, women’s needs from underserved/minority communities should be addressed. The panel suggested that priorities for measurement should focus on outcomes for healthy women and normal childbirth. Key areas for measurement include: mental and behavioral health, substance use, obesity and nutrition, cancer screening, chronic disease identification and management, and reproductive life planning. Two cross cutting issues were noted: the need for engaging women in health care decision making and health promotion, as well coordinated care among different care providers (especially care divided between generalists and reproductive health specialists). For pregnancy-related care, priorities for measurement include: availability of prenatal record at the time of delivery, sharing risks identified in pregnancy with the ongoing care provider, and overuse of procedures (such as elective induction of labor prior to 39 weeks and cesarean section). A new conceptualization of postpartum care is needed, as current measures do not address post-pregnancy needs. Related concerns include: methods for educating and engaging consumers in their health care; improvement of data sets and reducing barriers to data sharing across providers and settings; and reimbursement and liability concerns with regard to preventive and pregnancy-related services. Conclusions: Quality measurement for women of reproductive age should focus on women’s comprehensive health needs, should support care coordination and data sharing across care providers and life stages, and should engage women in their health and health care. Implications for Policy, Delivery or Practice: Federal efforts to monitor quality in Medicaid and to encourage adoption of health information technology offer new opportunities for implementing a broader framework for the quality of women’s health care. NCQA, the AMA-PCPI and the American College of Gynecologists are currently developing a pregnancy-related care measure set. Funding Source(s): CDC Poster Number: 246 Do New Guidelines and Technology Make the Routine Pelvic Exam Obsolete? Presented by: Carolyn Westhoff, M.D., M.S., Family Planning Division Director, Obstetrics & Gynecology, Columbia Presbyterian Medical Center, 622 W. 168th Street PH 16-69, New York, NY 10025; Phone: (212) 305-7070; Email: clw3@columbia.edu Co-authors: Heidi Johnson, M.P.H.; Maryam Guiahi, M.D. Research Objective: In the United States, the routine pelvic exam is the core of the periodic gynecological examination, and widely tolerated by asymptomatic patients who accept this as a necessary part of health maintenance. Is this routine examination beneficial for the asymptomatic woman? Specific justifications for the pelvic exam include: 1. screening for sexually transmitted infections (STIs), especially Chlamydia and N. gonorrhea, 2. evaluation prior to the initiation of hormonal contraception, 3. screening for cervical cancer, and 4. detecting early cases of ovarian cancer. Study Design: We reviewed relevant literature and professional guidelines to explore the validity of these justifications for the standard use of the pelvic exam in asymptomatic women. Population Studied: English language literature. Principal Findings: 1. Highly sensitive and specific DNA amplification tests for Chlamydia and N. gonorrhea now permit use of easy-to-obtain specimens, including urine and self-administered vaginal swabs. Most women prefer these approaches over a pelvic exam. 2. Findings from a pelvic exam do not affect the decision to prescribe or withhold hormonal contraception; therefore, relevant authorities now explicitly state that a pelvic examination is not needed for initiation of these contraceptives. 3. Recent American College of Obstetrics and Gynecology guidelines recommend no cervical cancer screening before age 21. Cervical screening from age 21-30 can occur every 2 years, and then every 2-3 years until age 65 or hysterectomy. These recommendations for less frequent cervical cancer screening, along with use of urine or swab-based STI testing, markedly decrease the number of times that a clinician needs to carry out a speculum exam to sample the cervix. While the speculum exam is still the main approach to obtain specimens for cervical cancer screening, the new guidelines indicate that a woman might need this only 15 times in her lifetime. 4. In the United States, the speculum exam is routinely accompanied by a bimanual pelvic exam for the palpation of the uterus and ovaries, especially intended to detect ovarian cancer. Clinical trial data, however, show that bimanual exams do not lead to earlier detection of ovarian cancer. In most European countries asymptomatic women do not undergo routine bimanual exams. Conclusions: The pelvic exam is not needed to screen for STIs, to initiate hormonal contraception, nor does it assist in early detection of ovarian cancer. The speculum exam is now needed far less often for cervical cancer screening. No evidence identifies benefits of a pelvic exam in the early diagnosis of other conditions in the asymptomatic woman. Implications for Policy, Delivery or Practice: Speculum and bimanual examinations are uncomfortable, disliked by many women, and use scarce time during a well woman visit. Eliminating the pelvic exam from most of these visits will free resources to provide other services of proven benefit. Asymptomatic women may be able to seek preventive services from a broader spectrum of clinicians, including those who do not routinely perform pelvic exams. Finally, such changes will allow gynecologists more time for the diagnostic evaluation of symptomatic women and for providing specialist services. Poster Number: 247 Gender Differences in Medication Therapy Management Programs Presented by: Donghui Wu, Ph.D., MEDai Inc., 4901 Vineland Road, Suite 450, Orlando, FL 32811; Phone: (321) 281-4561; Email: dwu@medai.com Co-authors: Ognian Asproughov, Ph.D.; Anton Berisha, M.D. Research Objective: This study focuses the gender differences of Medicare beneficiaries in Medication Therapy Management Programs (MTMP). We study the gender differences in utilization patterns in drugs, occurences of adversary drug interactions, and conditions/costs progress over time. Study Design: This is retrospective data study. The study includes one year prescription history of about 800,000 eligible Medicare members from multiple states. The prescriptions are categorized into 88 treatment classes, and adversary drug interactions are defined based on treatment classes. There severities of adversary drug interactions based on potential harms/side effects to members's health conditions. Population Studied: About 800,000 eligible Medicare members are selected from near two million members from a nation Medicare sponsor. 39% of the 800,000 eligible members are male, 61% are female. Principal Findings: We find major gender differences in usage patterns in drug usage in terms of treatment classes, adversary drug interactions, costs, and further future prospects, i.e. effectiveness of MTM programs. Conclusions: It is very important to pay attention to the gender differences in terms of drug usage patterns, adversay drug interactions if MTM program want truely improve quality of life Medicare beneficiaries and reduce future costs. Implications for Policy, Delivery or Practice: It is very important for policy maker to put gender specific and disease specific requirement into MTM program requirement and guidelines for eligibility for enrollmet in MTM program. Funding Source(s): Company R&D Poster Number: 248 Trends in the Incidence of IUD Insertion in the United States: Data from a Population with Employer-Sponsored Insurance Presented by: Xin Xu, Ph.D., Prevention Effectiveness Fellow, Economist, WHFB, DRH, NCCDPHP, Centers for Disease Control and Prevention, Atlanta, GA 30341; Phone: (770) 4886470; Email: iip5@cdc.gov Co-authors: Maurizio Macaluso, M.D., Ph.D.; Lijing Ouyang, Ph.D.; Scott Grosse, Ph.D. Research Objective: The prevalence of intrauterine devices (IUD) is low among women of reproductive age in the United States. The objective of this study was to examine the trend in IUD insertions and related medical expenditures between 2002 and 2007 in a population of women covered by employer-sponsored health insurance (ESI). Study Design: We conducted a population-based study using the MarketScan Commercial Claims and Encounter Enrolled Population database. We identified women, 15 to 49 years old, who filed a claim for the insertion of an IUD or IUS (intrauterine system, i.e., the Levonorgestrel-releasing IUD) between Jan. 1, 2002 and Dec. 31, 2007. The numerator for incidence calculations was the number of patients having at least one insertion reimbursement in that year, while the denominator was the number of patients under ESI plans with IUD/IUS coverage. We adopted the MarketScan national weights to generate nationally representative estimates. Population Studied: Women of reproductive age with employer-sponsored health insurance coverage in the United States. Principal Findings: The IUD/IUS insertion incidence in the ESI-covered population increased from 2/1,000 eligible women of reproductive age in 2002 to more than 8/1,000 in 2007, largely due to the increase in IUS insertion incidence from 0.5/1,000 to 6.0/1,000 during the same time period. The insertion incidence increased the most among women aged 25 to 34 years, from 4/1,000 in 2002 to almost 16/1,000 in 2007. The IUD/IUS insertion incidence was relatively high among states on the West and East coasts. The average annual increase in insertion incidence rates was more pronounced in Southern states where the incidence was low in 2002. Among the 10 states with the largest absolute growth in IUD/IUS insertion, the incidence increased on average from 3.1/1,000 in 2002 to 13.5/1,000 in 2007, while the incidence among the 10 states with the smallest growth only increased from 2.4/1,000 to 5.5/1,000. The annual medical expenditures associated with IUD/IUS insertions in this population increased from 26.7 million dollars in 2002 to 86.0 million dollars in 2007, after adjusting for inflation (both monetary terms are in 2007 dollars). Conclusions: The IUD insertion incidence in the United States has increased substantially from 2002 to 2007, mainly driven by the remarkable growth in the number of IUS insertions. Substantial geographic disparity exists in insertion rates. The increases in medical expenditures were also largely driven by the growth in IUS insertions. Implications for Policy, Delivery or Practice: IUDs have lower contraceptive failure rates than any other reversible contraceptive method, and higher rates of IUD use should be associated with fewer unwanted pregnancies. Additional research is needed to understand whether the recent growth in IUS insertions and the state disparity in IUD/IUS insertion incidence are related to differences in provider attitudes and local policies. Poster Number: 249 A Comparison of Intrauterine Device Users and Non-Intrauterine Device Contraceptive Users in a Nationally Representative Survey Presented by: Xin Xu, Ph.D., Prevention Effectiveness Fellow, Economist, Women's Health and Fertility Branch (WHFB), Centers for Disease Control and Prevention; Email: xinxu@cdc.gov Co-authors: Maurizio Macaluso, M.D., Dr.PH.; Jennifer Frost, Ph.D.; John Anderson, Ph.D.; Kathryn Curtis, Ph.D.; Scott Grosse, Ph.D. Research Objective: Little is known about the characteristics of intrauterine contraceptive device (IUD) users in the United States. The objective of this study was to describe demographic and reproductive characteristics, family background, and demand for reproductive health services among IUD users, and their reasons for choosing IUDs. Study Design: We adopted women aged 15-44 years old who responded to the 2002 National Survey of Family Growth (NSFG) and used any reversible contraceptive methods during 01/199903/2003. We divided them into five groups according to a hierarchy of methods: IUD, longacting hormonal, pills and patch, barrier, and others. We compared users in these categories with respect to self-reported demographic and reproductive characteristics; family background; and demand for reproductive services. Logistic regression was used to evaluate multiple predictors of IUD use. Analysis took into account the complex sampling scheme of the NSFG. We employed data from a telephone survey conducted by the Guttmacher Institute in 2004 to investigate reasons for choosing IUDs. The Guttmacher survey consists of 1,978 randomly selected women aged 18-44 who were currently at risk of unintended pregnancy. The Guttmacher samples were also weighted to reflect the U.S. female population. Population Studied: Women of reproductive age in the United States. Principal Findings: Compared to women using other reversible contraception, IUD users were more likely to be 25-34 years old (odds ratio (OR 2.0)), to be foreign born (OR 2.1), to have lived in a rented property (2.0), and to have never worked in their life time (OR 2.0), but less likely to be never married (OR 0.4), mot to have had sexual intercourse every month during the previous 12 months prior to the interview (OR 0.3), and to have had no live birth (OR 0.2). IUD users were more likely to have had a mother with at least a high school education (OR 2.6) and less likely to have had teenage mothers (OR 0.6). Each of these variables was statistically significant (95%) in the multiple logistic regression analysis. IUD users were also more likely to have had a medical checkup or test related to a birth control method (51.1% vs 33.3%) and more likely to have received counseling about birth control during the 12 months prior to the interview (33.5% vs 26.5%). The three most frequently reported reasons for choosing IUDs were the method’s ability to prevent pregnancy (86.4%), the method’s ability to not interrupt sex (70.5%), and the provider’s recommendation to use it (60%). IUD users also reported the highest level of satisfaction among all users of reversible contraceptive methods (82.3% vs 61.4%). Conclusions: IUD users differ markedly from users of other reversible contraception. The IUD was well perceived among most users. Implications for Policy, Delivery or Practice: IUDs have lower contraceptive failure rates than other reversible contraceptive method, and higher rates of IUD use should lead to fewer unwanted pregnancies. Women with the characteristics described above may be more receptive to promotional messages about IUD use. Health care providers’ perceptions about the IUD could also be crucial for the success of IUD promotion. Poster Number: 250 A Mixed Methods Study Exploring the Value of an Interprofessional Patient Safety Education Course to Nursing Students Presented by: Amy Abbott, Ph.D., R.N., Assistant Professor, School of Nursing; Center for Health Services Research and Patient Safety, Creighton University, 2500 California Plaza Office 193A, Omaha, NE 68178; Phone: (402) 280-2055; Email: aabbott@creighton.edu Co-authors: Kevin Fuji, Pharm.D.; Karen Paschal, P.T., D.P.T., M.S.; Kimberly Galt, Pharm.D.; Ph.D. Research Objective: Equipping nurses with knowledge, skills, and attitudes to improve patient safety is critical for reducing harm and injury due to errors in patient care. Educators must prepare students with foundational knowledge to keep patients safe in challenging and ever-changing healthcare environments. The purpose of this pilot study was to understand nursing students’ attitudes about the value of interprofessional patient safety education to their professional development and its value and role in health professions’ curricula. Study Design: An exploratory mixed methods design was used. Quantitative data was analyzed using information obtained from all students’ course evaluation questionnaire, final examination performance, final case study performance, and classroom assessment techniques. Critical case sampling was used to identify interview participants. Interviews were guided by three key ideas: 1) the role of the nursing profession, the individual nurse, and the nursing student in the context of patient safety; 2) how skills and attitudes learned in the course will change behavior as a student and future practitioner; and 3) recommendations for incorporation of patient safety content into nursing curriculum. Interviews were transcribed, checked for accuracy, and in vivo coded by each investigator. Themes were developed from the interviews using the quantitative data as a contextual framework for the qualitative findings and nursing student performance was compared with the entire class to distinguish if learning differed significantly from the other professions. Population Studied: 27 students enrolled in an interprofessional patient safety course participated in the study (7 nursing, 19 pharmacy, and 1 law). Quantitative data were collected from all students. Six nursing students were interviewed. Principal Findings: Students’ course average was 95.2% with no differences noted between nursing students and the rest of the class. Students averaged 88.7% on the final case study, designed to assess students’ abilities to comprehensively apply knowledge learned to a specific situation involving multiple professions. The final examination, designed to assess overall knowledge and recall of core patient safety material, had an average of 89.2%. Students estimated 80% of the material was new knowledge and not taught in other courses. All students felt the course material was essential or enriching for all health professions. The qualitative themes that emerged were awareness, ownership, and action. The awareness theme described students becoming aware of the science of patient safety and what it meant in their role as a professional. Ownership described role identification of both self and others in patient safety. Action described students spreading the word, advocating for patients, and ensuring safe patient care delivery. Those involved in patient care were able to describe application of the course content in their work environment. Conclusions: Nursing students perceive high value in using an interprofessional format to learn about patient safety. Students perceive the science of patient safety as foundational and core knowledge needed by all health professionals. Implications for Policy, Delivery or Practice: Findings will inform educators about the meaning of this interprofessional patient safety education experience to professional nursing student development. A values-oriented patient safety education framework is responsive to nursing students and may enrich opportunities for nursing student education. Funding Source(s): Creighton University Office of Academic Excellence and Assessment Poster Number: 252 Implementation of an Interdisciplinary Coordination Intervention Presented by: Justin Benzer, Ph.D., Post-doctoral Fellow, Center for Organization, Leadership, and Management Research, Department of Veterans Affairs, 150 S. Huntington Avenue, Boston, MA 02130; Phone: (857) 364-5691; Email: justin.benzer@va.gov Co-authors: James Burgess, Ph.D.; Irene Cramer, Ph.D.; David Mohr, Ph.D.; Jenny Sullivan, Ph.D. Research Objective: The report of the President’s New Freedom Commission on Mental Health eM.P.H.asizes that mental health and physical health problems are interrelated components of overall health and are best treated in a coordinated care system. The purpose of this study was to determine the facilitators and barriers to implementing a team-based, interdisciplinary model of primary care-mental health integration (PC/MHI) using a transformational change model (VanDeusen Lukas et al., 2007). Study Design: Semi-structured interviews were conducted with a PC and a MH leader at each of the 17 sites. Additional interviews were conducted with 37 front line clinical staff, with at least one mental health and one primary care person interviewed at each site. Interviewees were asked to describe how the process of coordinating primary care and mental health care had changed since they joined the clinic, and how processes could be further improved. Interview transcripts were coded with respect to the transformational change model elements of leadership (commitment to change), improvement initiatives (staff involvement), alignment (goals and resources across organizational levels), and integration (bridging intra-organizational boundaries). Population Studied: Eight medical facilities and nine large outpatient clinics in one geographic region within the Veterans Health Administration were included in the study. In response to a national mandate to provide integrative mental health care, local leaders had implemented a model whereby mental health workers were co-located with primary care. Principal Findings: Interviews revealed differences between sites in both the degree of colocation, the degree of collaboration between primary care and mental health providers, and the structures, processes, and professions used to bridge the boundary between primary care and mental health. Leadership served as a facilitator to the implementation of PC/MHI through planning, procuring necessary resources, and encouraging communication between clinics. Most sites did not describe active involvement of frontline staff in the development of improvement initiatives, but where present, these efforts were seen as critically important in developing effective procedures. Integration problems included failure of PC providers to utilize PC/MHI services and shifting responsibility for patient care between PC and MH providers. Some sites were found to have good alignment, as evidenced by adequate training and resources for PC/MHI implementation. Resource constraints were commonly cited as barriers, but in several sites resource availability was not observed to affect quality of integration, as providers were able to develop innovative solutions to implementation challenges in resource constrained facilities. Conclusions: Local barriers and facilitators influenced the implementation of the PC/MHI model. This study supports the propositions of the transformational change model, and in particular reinforces the importance of leadership in the implementation of integrative, interdisciplinary interventions. Leadership was cited as a barrier to change or as a facilitator that was reported to overcome barriers of alignment or integration. Implications for Policy, Delivery or Practice: This study indicates that leadership is important for bridging boundaries between professions, for ensuring resource support, and for promoting staff involvement in improvement initiatives. Planned innovations, particularly those that bridge organizational boundaries require leadership support, and clinical staff should be actively involved in the discussion and revision of innovation procedures to fit clinic needs. Funding Source(s): VA Poster Number: 253 Teaching Service Census Caps and Unit-Based Admission of Patients Decreases Resident Workload, Improves Duty Hour Compliance, and Maintains Patient Safety Presented by: Rosa Cabanela, Ph.D., MS Health Services Analyst, Health Care Policy & Research, Mayo Clinic, Pavilion 3, Rochester, MN 55901; Phone: (507) 538-0220; Email: cabanela.rosa@mayo.edu Lead Author: Darcy Reed, M.D. Co-authors: James Naessens, Sc.D., M.P.H.; Rosa Cabanela, Ph.D.; Andrew Halvorsen, M.S.; Uma Thanarajasingam, M.D., Ph.D.; Furman McDonald, M.D. Research Objective: To reduce workload and enhance education, we implemented a census cap of 14 patients on the six Internal Medicine hospital teaching services at Mayo Clinic. In addition, we developed a unit-based admissions process in which patients and their multidisciplinary care team were geographically consolidated on a single hospital unit. This study sought to examine the impact of these two interventions on residents’ workload, educational conference attendance, duty hour compliance, and patient safety. Study Design: Difference in differences design comparing internal medicine teaching services with other general medicine hospital services for 12 month periods before and after the interventions. Residents reported workload and duty hours via monthly survey. Conference attendance was recorded using a card-swipe system. Patient safety variables including mortality, adverse events (e.g. medication errors, falls), and AHRQ Patient Safety Indicators (PSI) were determined for all patients before and after the interventions. To control for hospital-wide temporal trends, patient safety variables were also collected for all patients hospitalized on internal medicine non-teaching services during the study period. Variables were compared before and after the interventions using Fisher’s exact test, t-tests, and multivariate logistic regression. Significance was set at 0.01 to account for multiple comparisons. Population Studied: All 10,541 patients and 280 residents on all six Internal Medicine teaching services one year before and one year after the interventions were included. Principal Findings: After implementation of the interventions, residents’ perception of the appropriateness of their workload improved from a mean (SD) of 3.17 (1.09) on a 5-point scale to 3.89 (0.67), p< .0001. Residents’ ability to obtain 10 hours rest between shifts improved from 361.9 to 364.5 violation-free days/year (p< .0001), and their ability to work no more than 24 consecutive hours with 6 hours for education and patient hand-off improved from 361.2 to 364.0 violation-free days/year (p<.0001). Additionally, residents’ conference attendance increased by 12%, p< .0001. In logistic regression analyses adjusted for expected mortality, there were no significant differences before compared to after the interventions for resident versus control services in the percentage change in mortality rate (0.90% change vs. -0.18% change, p=.22), adverse events (-0.48% change vs. 1.06% change, p=.03), or Patient Safety Indicators (-1.64% change vs. 1.48% change, p=.24). Conclusions: The implementation of teaching service census caps and unit-based admissions decreases resident’s workload, improves duty hour compliance, increases conference attendance, and does not adversely affect patient safety. Implications for Policy, Delivery or Practice: In the wake of broad-based policy changes reducing residents’ work hours, systems-based solutions to reduce work hours and workload without compromising patient safety are needed. Implementation of service census caps and unitbased admissions processes have beneficial effects for resident learning and no deleterious impact on patient quality or safety, but careful planning of such changes is necessary. Further studies are needed to examine the feasibility of these interventions among different specialties and patient populations. Poster Number: 254 Psychological Ownership and Organizational Change: Engaging Health Care Providers in New Program Implementation Presented by: Vivian Chan, M.P.P., Interdisciplinary Studies Graduate Program, University of British Columbia, 953 West 16th Avenue, Vancouver, Canada ; Phone: (604) 7614919; Email: vwychan@interchange.ubc.ca Co-authors: Smillie, Kristen, M.A.; Kazanjian, Arminee, Dr.Soc. Research Objective: This paper explores the theoretical concept of psychological ownership and its potential effects during an organizational change environment. Case studies from Canada will be presented and discussed to elaborate recent literature on the theoretical concepts of psychological ownership and territoriality. Study Design: The authors conducted secondary analysis on data from a larger research program on knowledge exchange in cancer survivorship programming in diverse settings across Canada. The research team utilized “thick description” to organize the data, an ethnographic approach used to elucidate an understanding of a specific event or behavior within the social context that it occurs. The results were compiled into experiential accounts and presented in a series of reports to practitioners, policy makers and academics at local and national levels. Population Studied: Clinical program team members from six different cancer survivorship initiatives during the implementation and planning phases of the respective initiatives Principal Findings: Our literature review indicated that the inherent need for ownership and sense of territoriality is pervasive in an organizational setting. It seems natural that people instinctively defend that which they see as theirs (Brown & Robinson, 2007). Psychological ownership is the feeling of possessiveness and of being psychologically tied to the object (Pierce et al., 2001: 299). The object of possession can be physical (e.g. a thing, a person, a place) or social (e.g. an idea, a group, a work role) in nature. Territorial behaviour such as behaviours for constructing, communicating, maintaining, and restoring territories around those objects in the organization toward which one feels proprietary attachment were evident when examining the experiential accounts from the cancer survivorship clinical intervention programs. Paré, Sicotte, and Jacques’s (2006) posit that feelings of psychological ownership towards the clinical information system may be developed through active physician involvement during the implementation of the clinical system. They were able to show that physician’s attitudes, as conceptualized as psychological ownership toward the clinical information system, are related to the subsequent usage of the information system. However, Brown and Robinson (2007) cautioned that the feeling of ownership and territoriality might not always lead to positive organizational behaviour. Resistance to change as a result of strong proprietary attachment to existing objects is one of the dysfunctions of psychological ownership and territoriality. Conclusions: We were able to highlight how clinical program team members exhibited positive and negative aspects of psychological ownership and territorial behaviour during the planning and implementation phases of selected cancer survivorship initiatives. We subsequently reflect on how positive and negative aspects of territoriality and psychological ownership influenced the implementation of these programs. Implications for Policy, Delivery or Practice: If the need to possess and a sense of territoriality are prevalent, how are we to identify these behaviours when developing change management strategies? What are the routes to positive aspects of psychological ownership to support health care providers through organizational and practice change? How do we avoid or reduce negative aspects from creating a resistant organizational culture? Answers to these questions will lead to a better understanding of successful organizational change strategies and consequently, more effective initiatives. Sense of territoriality and ownership are universal human attributes which may be expressed and enacted in a variety of ways within systemspecific conditions. Examining aspects of the Canadian health system that yields positive results in the process of change management would be instructive to other health care systems and in different care settings. Funding Source(s): Canadian Institutes for Health Research Poster Number: 255 Perceived Facilitators and Barriers to Improving Internal Medicine Residency Curricula Presented by: Kristina Cordasco, M.D., M.P.H., M.S.H.S., Associate Scientist, Adjunct, Health, The RAND Corporation, 1776 Main Street, P.O. Box 2138, Santa Monica, CA 90407-2138; Phone: (310) 393-0411 ext. 6364; Email: kcordasc@rand.org Co-authors: Cristina Boccuti, M.P.P.; Craig Lisk, M.S.; Nicole Lurie, M.D., M.S.P.H.; Marianna HortaCapelli, B.A.; Barbara Wynn, M.A. Research Objective: Over the past 50 years, the delivery of medical care has changed dramatically with advances in technology, population aging and diversification, and rising prevalences of chronic diseases. Training in internal medicine, however, has changed little. There have been multiple calls for reforms in residency training to better prepare our physician workforce in the knowledge and skills needed. In response to these calls, accrediting organizations of allopathic and osteopathic residency programs have begun incorporating new topics into required curricula. We conducted an exploratory study for the Medicare Payment Advisory Commission (MedPAC) of how internal medicine (IM) residency programs are training their residents in the competencies of systems-based practice, practice-based learning and improvement, and communication. As part of this study, we asked IM residency program directors to comment on facilitators and barriers to improving their curricula in these competencies. Responses regarding facilitators and barriers is the the focus of this paper. Study Design: Using semi-structured interviewing techniques, we asked each program director to describe their program’s approach to training in topics in each of the three competencies, and then asked them to describe the facilitators and barriers they have experienced in improving the curricula in that competency. At the conclusion of the interview, we asked about overall facilitators and barriers for curricular improvement. Each interview was audiorecorded. Using detailed notes taken from reviewing each audio-recording, and content analysis with techniques from grounded theory, we identified and then described the common themes that emerged from comments on facilitators and barriers. Population Studied: We invited a randomlyselected 59 program directors of allopathic and osteopathic programs to participate in one-hour interviews, 26 (44%) of whom agreed to and completed the interview between November 25 and December 29, 2008. No incentives were offered. Principal Findings: Eight themes emerged from directors’ comments on facilitators and barriers to improving curricula in these competencies: (1) presence or lack of information technology resources; (2) presence or lack of faculty expertise in these topics; (3) presence or lack of faculty time protected for curricula development and implementation; (4) characteristics and resources of the program’s setting; (5) presence or lack of institutional support for training in these topics; (6) competing priorities for resident time; (7) residents’ baseline knowledge and interest in these topics; and (8) scarcity of research in educational and evaluation strategies for these topics. Conclusions: Graduate medical education funding policies, accreditation standards, certification exam topics, undergraduate medical education and investment in research of educational and evaluation strategies act as facilitators and barriers to curricula innovation in residency programs. Implications for Policy, Delivery or Practice: Examining and potentially intervening in these factors, so that incentives are aligned with desired changes, could have a significant positive impact on how well IM programs are preparing our nation’s physician workforce to care for our 21st century population. Funding Source(s): The Medicare Payment Advisory Commission (MedPAC) Poster Number: 256 Effect of Increased Insurance Coverage under Health Care Reform on the Demand for Primary Care and Specialist Physicians Presented by: Tim Dall, M.S., Managing Director, The Lewin Group, 3130 Fairview Park Drive, Suite 800, Falls Church, VA 22042; Phone: (703) 2695743; Email: tim.dall@lewin.com Co-authors: Paul Hogan, M.S.; Yaozhu Chen, M.P.A. Research Objective: Estimate the implications of increased health insurance coverage through health care reform on the demand for physicians and the projected future excess demand. Study Design: Controlling for demographics (age, sex, race/ethnicity), healthcare utilization patterns of the insured are compared to utilization patterns of the uninsured using 2007 data from the National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, Nationwide Inpatient Sample, and National Health Interview Survey. Differences in health status and prevalence of chronic diseases for the insured and uninsured are analyzed using the National Health and Nutrition Examination Survey and National Health Interview Survey. Based on differences in utilization patterns between the insured and other similar uninsured, an estimate of the increase in utilization, and the change in resources utilized are estimate from the data. Using data from CDC's Behavioral Risk Factor Surveillance System, we estimated rates of uninsured by demographic group for each state. These inputs are entered into the demand component of a Physician Supply and Demand Model. Estimates of the effects on current and future demand, and the implications for the excess demand (shortage) of physicians are examined under multiple scenarios related to increase insurance coverage. Scenarios include 100% coverage, as well as expanding coverage to include currently uninsured U.S. citizens (reaching approximately 96% coverage). Population Studied: The U.S. resident population. Principal Findings: Likely effects of proposed expanded medical coverage under health care reform on utilization will result in about a 4-7% increase in demand for physicians. The increase, however, will vary by physician specialty and by state. Because most of the over 65 population is already covered under Medicare, and most children are covered through private insurance, Medicaid or CHIP, there is not likely to be a large increase in utilization from children and the elderly by expanding medical coverage. Among adults under age 65, there is a mix of healthy uninsured that likely will see little increase in healthcare utilization and uninsured with chronic conditions such as diabetes and cardiovascular disease that will likely see substantial increases in utilization. Preliminary findings will be updated to incorporate the latest health care reform legislation on expanded insurance coverage. Conclusions: Health care reform legislation to expand medical coverage will create a modest increase in demand for physicain services at a time when there are already concerns about an inadequate supply at the national and local level. Implications for Policy, Delivery or Practice: The findings can serve to improve health workforce policy and planning. The overall increase in demand, and the variation in this increase across areas of specialization, may have policy implications for undergraduate and graduate medical education resources and policy planning. Poster Number: 257 Results from the First and Second Cohorts of the VA Nursing Academy: Using VA-Nursing School Partnerships to Reduce the Clinical Nursing Faculty Shortage Presented by: Aram Dobalian, Ph.D., J.D., Research Health Scientist, COE Healthcare Provider Behavior, Department of Veterans Affairs, 16111 Plummer Street (152), Sepulveda, CA 91343; Phone: (818) 891-7711 ext. 7182; Email: aram.dobalian@va.gov Co-authors: Candice Bowman, Ph.D., R.N.; Tamar Wyte, D.P.T., M.P.H.; Darya Friedman, M.P.H.; Barbara Simon, M.A.; Jack Needleman, Ph.D. Research Objective: According to HRSA, the U.S. is experiencing a moderate shortage of registered nurses (RNs). About 22,000 RNs will be eligible for retirement within the Department of Veterans Affairs (VA) this year. It has been suggested that much of this shortfall is due to a lack of qualified nursing faculty. Consequently, VA established the VA Nursing Academy, a 5-year pilot program that funds faculty positions at 15 competitively selected partnerships of VA facilities and nursing schools. The Academy is designed to expand nursing faculty, enhance professional development, increase student enrollment, promote innovations in education and practice, and increase recruitment and retention of nurses within VA. We are in year three of five of our national evaluation of the program. Study Design: We conducted over 120 semistructured interviews (45-120 minutes) that assessed the partnerships’ structures and the consequences of their activities during the first ten partnerships’ initial year. Population Studied: Nursing leadership, local partnership project directors, nursing faculty, nurse managers, nursing students, and nursing staff. Principal Findings: Most partnerships completed faculty hiring by the end of the first year. Teaching responsibilities were usually limited to clinical instruction. A few Academy faculty were offered the opportunity to teach an entire didactic class, most often in skills or simulation labs. Faculty workload was generally believed to be greater than what was expected, although most stated that it was within reasonable limits. Most partnerships met their increased student enrollment quota for the year. Initially, students were sometimes resistant to the idea of having clinical rotations at the VA. However, after exposure to the VA, most students were much more positive about the experience and enthusiastic about going back to the VA because, in comparison with non-VA facilities, students were allowed to participate more in hands-on patient care, nursing staff were friendlier and more helpful, and veteran patients liked receiving care from them. Creatively selecting areas used for clinical placements, such as perioperative areas, rehabilitation units, nursing homes, and outpatient clinics, was a source of innovation. We identified critical themes that influenced “Launch-Year achievement,” i.e. what was feasibly attainable after one year of a partnership’s implementation. Key domains identified that potentially influence performance include local market conditions, leadership involvement and commitment, scope of faculty roles and development, intra-organizational facilitation, communication, power sharing, problem solving mechanisms, pre-existing relationship between partners, presence of champions, stability of partnership personnel, and perceived benefits of the Academy. Conclusions: Of these key domains, our observations across partnerships have led us to eM.P.H.asize inter-organizational collaboration (e.g., teamwork between direct and indirect participants across partnering institutions regarding specific issues, strategies, or decisions) as a critical factor in enabling these partnerships to be successful. In designing and implementing future partnerships, organizations should consider each of these domains that influenced Academy partnership performance during the Launch Year. Implications for Policy, Delivery or Practice: The Academy may serve as a model for how best to design and structure partnership relationships between two distinct institutions, with intrinsically divergent needs. Funding Source(s): VA Poster Number: 258 Persistent Primary Care Health Professional Shortage Areas (HPSAs) and Health Care Access in Rural America Presented by: Mark Doescher, M.D., M.S.P.H., Director, WWAMI Rural Health Research Center, Family Medicine, University of Washington, 4311 Eleventh Avenue NE, Suite 210, Seattle, WA 98105; Phone: (206) 616-9207; Email: mdoesche@u.washington.edu Co-authors: Meredith Fordyce, Ph.D.; Susan Skillman, M.S.; J. Elizabeth Jackson, M.A.; Roger Rosenblatt, M.D., M.P.H. Research Objective: Primary care Health Professional Service Areas (HPSAs) help states and communities increase their primary care supply through eligibility for loan repayment, Federally Qualified Health Center and Rural Health Clinic designation, and other mechanisms. This study examined whether persistence of primary care HPSA designation in rural counties was associated with lower population socioeconomic status (SES) and deficiencies in access to health care services, including provider supply. Study Design: Cross-sectional analysis of U.S. rural county characteristics by their primary care HPSA designation, classifying counties as: never HPSAs; intermittent partial-county HPSAs; persistent partial-county HPSAs; intermittent wholecounty HPSAs; and persistent whole-county HPSAs. Population Studied: The primary care HPSA categories were used to assess: per capita supply of clinically active family physicians, general internists, general pediatricians and obstetriciangynecologists using the 2005 American Medical Association and American Osteopathic Association Masterfiles; socioeconomic-demographic characteristics using U.S. Census Bureau data; and access to care using data from the 2004/5 Behavioral Risk Factor Surveillance System. Principal Findings: Distribution: Of 2,051 U.S. rural counties in 2005, there were 308 (15% of all rural counties) “never” HPSAs, 370 (18.0%) “intermittent partial-county” HPSAs, 490 (24%) “persistent partial-county” HPSAs; 195 (105) “intermittent whole-county” HPSAs; and 688 (33%) “persistent whole-county” HPSAs. Sociodemographics: A gradient occurred in which SES was lowest in persistent whole-county HPSAs, while counties never receiving a HPSA designation had the highest SES status (e,g, persistent poverty characterized 28.1% of persistent whole county HPSAs vs. 5.8% of never HPSA counties). A racial/ethnic gradient was observed in which minorities made up the highest percentage of the population in persistent whole-county HPSAs, while the fewest minority group members lived in the never HPSAs (e.g., minorities characterized 21.6% of persistent whole county HPSAs vs. 11.4% of never HPSA counties). Access: A gradient of decreased access occurred in which access was poorest in persistent whole-county HPSAs for: primary care physician supply (39.3 per 100,000 population of persistent whole county HPSAs vs.72.3 per 100,000 population in never HPSAs); the percentage of adults lacking a regular primary care provider (22% in persistent whole county HPSAs vs. 17% in never HPSAs); the percentage lacking health insurance coverage (21% in persistent whole county HPSAs vs. 16% in never HPSAs); and the percentage foregoing needed health care because of its cost (18% in persistent whole county HPSAs vs. 14% in never HPSAs). Conclusions: This five-level classification of rural counties measuring partial- vs. whole-county persistence of primary care HPSA designation stratifies rural populations by SES, race/ethnicity, primary care supply, health insurance uptake and access to needed health care services. Those U.S. rural counties that were persistently designated as whole-county HPSAs had much lower SES and adults residing in these counties reported substantial financial obstacles to obtaining needed health care services. Rural counties persistently designated as whole-county HPSAs faced severe provider shortages and adults residing in these locations were less likely to have a regular primary care provider. Implications for Policy, Delivery or Practice: The ability to identify persistence and extent of HPSA designation may be a valuable tool in selecting counties with higher levels of need. Funding Source(s): HRSA Poster Number: 259 Dentist Supply, Access to Dental Care, and Oral Health among Rural and Urban Residents: A National Study Presented by: Mark Doescher, M.D., M.S.P.H., Director, WWAMI Rural Health Research Center, Family Medicine, University of Washington, 4311 Eleventh Avenue NE, Suite 210, Seattle, WA US 98105; Phone: (206) 616-9207; Email: mdoesche@u.washington.edu Co-authors: Gina Keppel, M.P.H.; Susan Skillman, M.S. Research Objective: Dentists in rural locations are in short supply compared to urban locations. However, whether low rural supply adversely influences dental health care access and oral health status is not well understood. To address this gap in knowledge, we examined relationships between dentist supply and dental access, preventive care, and oral health among U.S. rural and urban adults. Study Design: We conducted a cross-sectional assessment of data from the 2006 Behavioral Risk Factor Surveillance System of the Centers for Disease Control and Prevention, a nationally representative survey. These data were used to identify dental access (visits to a dentist or dental clinic in the past year), preventive care (teeth cleaning in the past year), and oral health (permanent tooth loss). Data from the 2008 American Dental Association Dentist Masterfile were used to examine the influence of per capita dentist supply on these measures. Population Studied: A representative sample of U.S. civilian, non-institutionalized adults aged 18 or older was examined (n=355,720). Rural residence was grouped as metropolitan (urban) or nonmetropolitan (rural) county of residence based on the county-based Office of Management and Budget taxonomy, and smaller/more isolated rural locations were classified using the 2003 Urban Influence Code groupings of the Economic Research Service of the U.S. Department of Agriculture. Principal Findings: After adjustment for sociodemographic and other factors, rural residents were significantly less likely than urban residents to report having a dental visit (Adjusted Odds Ratio [AOR] 0.87, 95% Confidence Interval [CI] 0.84 to 0.91) or teeth cleaning (AOR 0.83, CI 0.81 to 0.87) in the past year, and they were significantly more likely to report having had any permanent teeth extracted (AOR 1.19, CI 1.14 to 1.23). As dentist supply increased, the likelihood of having one or more dental visits and teeth cleaning in the past year increased, and the likelihood of undergoing permanent tooth extraction due to dental decay or disease decreased in both urban and rural locations (p<0.001 for each model). Rural adults residing in counties having the lowest quintile of dentist supply were less likely than their counterparts living in the highest quintile counties to report having a dental visit (61% vs. 69%, respectively) and teeth cleaning (59% vs. 68%), and they were more likely to report having had any permanent teeth extracted (57% vs. 46%). Conclusions: U.S. rural adults utilize fewer dental services and have more permanent tooth loss, even after adjusting for differences in socio-demographic characteristics. However, in rural and urban locations increases in dentist supply were associated with improvements on these access and outcome measures. Implications for Policy, Delivery or Practice: Dentists are an essential component of rural health care and higher supply is related to improved dental care and better oral health. Yet rural communities struggle to recruit and retain sufficient numbers of dentists to meet their oral health care needs. Policies to increase rural dentist supply may lead to improvements in dental access, preventive care and oral health outcomes of US rural adults. Funding Source(s): HRSA Poster Number: 260 Enhancing the Delivery of Preventive Care at Primary Care Practices in Underserved Communities Using Shared Outreach Workers Presented by: Carlene Duncan, M.P.H., Program Manager, PCIP, NYC Department of Health and Mental Hygiene, 161 William Street, 5th Floor, New York, NY 10038; Phone: (347) 882-0186; Email: cduncan1@health.nyc.gov Lead Author: Carlene Duncan, M.P.H. Co-authors: Daniel Halevy, M.D.; Amanda Parson, M.D., M.B.A.; Kaleena Colon Research Objective: 1) Examining the impact of outreach workers as a shared resource among electronic health record-enabled small practices on the quality of care of patients and encouraging patients to see their primary care physician (PCP) on a regular basis to get recommended care. 2) Examining the cost effectiveness of this outreach strategy. This will be measured by analyzing Revenue Value Units (RVU) through the number of patient visits at the practices. Study Design: The role of a prevention outreach specialist (POS) was defined as a layperson without specific healthcare certification, who received training in the use of the electronic health record in order to identify patients with the targeted chronic conditions. One POS was recruited and was embedded at a single primary care practice. The first part of the pilot involved the identification of patients with asthma during the peak asthma season, and the generation of appointment reminder letters. The second part of the pilot involves the recruitment of four additional specialists, each working with four practices. The specialists will identify patients with all of the targeted at-risk conditions and will coordinate with the practices to prioritize and conduct outreach activities, through phone calls and letters to patients recommending that they make appointments, fill prescriptions, and receive education about their lab test results. Population Studied: Primary care practices in New York City’s underserved communities and their patients who are identified as being at-risk for chronic disease. The at-risk population consists of patients with cardiovascular disease, hypertension, hyperlipidemia, asthma, smoking, diabetes and obesity. All practices are enrolled in the Primary Care Information Project, in which they use an EHR with an integrated registry tool, making it possible to use the practices' own clinical data to systematically identify patients with gaps in care. Principal Findings: Of the 567 patients with the targeted at-risk chronic conditions, over 60% returned for recommended care during the intervention period. The return rate varied depending on the disease area, from 40% for patients requiring improved blood pressure and cholesterol control, up to 60% for patients requiring an assessment for antithrombic therapy. Fifty five percent of patients responded to the intervention by returning for a diabetes management visit. Of the 199 asthma patients identified during the peak asthma allergy season and were sent a reminder letter, over 50% patients returned for recommended care within eight weeks.Over a course of 6 months, 567 unique patients were enrolled and received the intervention, leading to 475 phone calls and 199 letters. Conclusions: This pilot demonstrated the feasibility of embedding a POS in a primary care practices located in underserved communities in order to ensure the delivery of timely and appropriate care. We were able to measure patient follow up to the intervention and plan to compare these rates with historical and contemporary controls. Implications for Policy, Delivery or Practice: The goal of this project is to demonstrate the value, cost savings and quality improvement of a shared outreach worker. If such an approach is successful, then the concept may be broadly embraced throughout New York State and throughout the country. We believe that the elements of this project are highly replicable, particularly as it has been proven among independent, highly under-resourced practices. Funding Source(s): Pfizer Poster Number: 261 Where will North Carolinians with Cancer Find Treatment? An Assessment of the Oncology Workforce Presented by: Danielle Durham, M.P.H., Research Associate, Research, The Carolinas Center for Medical Excellence, 100 Regency Forest Drive, Suite 200, Cary, NC 27518-8598; Phone: (919) 380-9860; Email: ddurham@thecarolinascenter.org Lead Author: William Carpenter, M.H.A., Ph.D. Co-authors: Franziska Rokoske, P.T., M.S.; Karen Knight; Anna Schenck, M.S.P.H., Ph.D. Research Objective: The purpose of this research was to examine cancer treatments at the county level to identify which counties face a potential shortage of oncology physicians given their cancer burden. The paper examines the burden of cancer based on North Carolina cancer cases diagnosed from 2003-2007, focusing on care provided for the top ten cancers: Female breast, Colon and Rectum, Kidney and Renal pelvis, Lung and Bronchus, Melanomas of the skin, Non-Hodgkin LyM.P.H.oma, Ovarian, Prostate, Urinary bladder and Uterine. Study Design: A cohort study design was used to identify cancer patients and their treatments. The North Carolina Central Cancer Registry (NCCCR) provided information for cancer cases diagnosed from 2003 to 2007. Cases were linked with Medicare data to identify Medicare enrollees. Medicare claims data were obtained for Medicare enrollees to identify their cancer treatments. Cancer incidence was calculated for each North Carolina county using the Medicare county enrollment as the denominator and Medicare cancer cases as the numerator. Cancers with the highest incidence rates for male and females combined were included in the study. Cancer treatments were identified by the presence of cancer diagnoses and treatment codes on the claims and were classified into three categories: radiation treatments, surgical treatments, medical treatments (which includes chemotherapy). Physicians were identified by their UPIN number and their geographic location was determined based on their office address contained in the Medicare files, which was geo-coded to the centroid of the office zip code. Population Studied: A total of 15,810 North Carolina Medicare enrollees were diagnosed with cancer in 2005. The study population was limited to cancer cases diagnosed among North Carolina residents and non-HMO Medicare enrollees age 65 and over as of January 1 with at least 11 months of Part B coverage in 2005. Principal Findings: Of the leading four cancers, prostate cancer had the highest number of cases (n=2664), followed by breast cancer (n=2304), lung cancer (n=2367) and colon cancer (n=2004). Across all cancers, 13% of NC counties had no physicians providing cancer treatments for Medicare enrollees. This occurred often in counties with higher incidence rates. The mismatch between cancer incidence and physicians providing treatment varies by type of cancer and type of treatment. Physicians providing cancer treatments to Medicare enrollees with prostate cancer had the greatest coverage across the state, although 18% of counties had no treatments attributed to county physicians. The largest gap in cancer physicians was seen for lung cancer, with 42% of NC counties having no treatments attributed to physicians with addresses in that county. The lack of any physicians providing radiation treatment was observed more frequently than the absence of physicians providing surgical or medical treatments. Conclusions: Cancer burden in some North Carolina counties is not matched by the availability of treatment. An aging workforce may have implications for availability of treatment in the future. Implications for Policy, Delivery or Practice: Funding Source(s): University Cancer Research Fund, The University of North Carolina at Chapel Hill Poster Number: 262 Expanding Pharmacists’ Roles in Preventive Health related to Infant Feeding Presented by: Roger Edwards, Sc.D., Assistant Professor, Bouvé College of Health Sciences, Northeastern University, 360 Huntington Avenue, 206 Mugar Building, Boston, MA 02115; Phone: (617) 373-8344; Email: ro.edwards@neu.edu Research Objective: With their knowledge of medication safety, highly visible roles in the community, and frequent interactions with soon-tobe and new parents, pharmacists are in key positions to expand their roles in the promotion and support of breastfeeding as optimal infant feeding. Improving rates of breastfeeding will have a significant public health impact today and in the years ahead. Only 11.3% of infants are breastfed exclusively for six months (American Academy of Pediatrics recommendation). The objective of this research is to analyze existing contact that pharmacists have related to infant feeding and to identify opportunities to expand pharmacists’ roles in breastfeeding and improved infant formula feeding. Study Design: We initially performed a needs analysis to determine the nature of existing shortfalls related to supporting breastfeeding/infant feeding based on literature review. We then conducted twenty structured interviews of pharmacy and breastfeeding experts to obtain their insights and feedback using flowcharts of all possible contact opportunities during four periods: prepregnancy, prenatal, delivery, and postnatal. We matched unmet needs with pharmacists’ opportunities and capabilities. We also analyzed infant feeding/breastfeeding policy statements worldwide to learn more about activities of pharmacists in other countries. Population Studied: Pharmacists Principal Findings: Women want to breastfeed longer but discontinue because of inadequate support, notably from health professionals. Over 90% of women receive medication in the week following giving birth. Pharmacists have multiple opportunities in which to engage parents and the general public on optimal infant feeding. Good matches between unmet needs and capabilities were identified in: provision of health promotion resources and public awareness campaigns, assistance with purchase of breastfeeding products and pumps, and provision of information, support, and referral related to commonly encountered difficulties as well as medication use during lactation. Absence of adequate pharmacy education/knowledge was identified as a barrier. Absence of a professional organization position statement, as exists for professional pharmacist organizations in other countries, also creates hurdles. Conclusions: Our qualitative research approach identified that pharmacists are underutilized resources that could play important roles in supporting improved infant feeding behaviors. This research established the foundation for a broader research program including conducting interventionbased studies of roles pharmacists can play in improving infant feeding. Implications for Policy, Delivery or Practice: Evidence for the health risks of not breastfeeding continue to accumulate. Breastfeeding results in substantive health improvements in the short term and long run for both infants and mothers; yet, community-level support for this important health behavior is inadequate in much of the US. Leveraging an underutilized resource such as pharmacists to address unmet preventive health needs is especially important in our current health care delivery environment. Optimal intervention efforts still need to be studied. Infant feeding education received by pharmacy students and continuing professional pharmacist education should be expanded. A certification program for pharmacists can enhance lactation expertise in pharmacy. Position statements for consideration by the American Pharmacist Association are currently being developed. Medication therapy management is a recent example of how pharmacist clinical services have been effectively utilized to improve patient outcomes and reduce health care costs; improved infant feeding support by pharmacists has that same potential. Poster Number: 263 What about Everyone Else? Trends among the Non-Physician and Non-Nurse Healthcare Workforce Presented by: Bianca Frogner, Ph.D., Assistant Professor, Health Services Management and Leadership, The George Washington University, 2175 K St. NW, Suite 320, Washington, DC 20037; Phone: (202) 994-3816; Email: bfrogner@gwu.edu Research Objective: This study examines the trends among a largely ignored, but sizable and growing portion of the healthcare workforce - nonphysician and non-nurse workers in healthcare – in Australia, Canada, and the US. This study then disaggregates the healthcare workforce trends in the US into specific occupations and discusses the impact of technology adoption on healthcare workforce trends. Study Design: The study is an exploratory analysis of longitudinal data as an initial step in understanding dynamics in this understudied population. For the trend in “other” healthcare workforce, the author calculates the remaining healthcare workers after subtracting out nurses and physicians from the total healthcare workforce estimates. The author compiles annual data for specific occupations among the “other” workers with a focus on occupations that have contributed the most to the growth of the healthcare workforce. Population Studied: Healthcare workforce data collected by the Organization for Economic Cooperation and Development Health Dataset of 2009 provides national survey estimates in Australia, Canada, and the US from 1970 to 2008. For the US, the occupation specific data is from the Occupational Employment Statistics, a semi-annual panel survey of 1.2 million establishments collected by the Bureau of Labor Statistics from 1999 to 2008. Principal Findings: Non-physician and non-nurses are over three-quarters of the US workforce, 70% in Canada, and 60% in Australia in the most recent year of data. The US always had more “other” healthcare workers per capita and has been growing faster than the other two countries over the 38 year period. However, all three countries have seen a deceleration in the growth of “other” workers over the time period. A closer examination of occupations suggests that technicians/ technologists, administrators and support staff are the largest categories of workers that have also been rapidly increasing in the US. By the conference date, technicians/technologists will be further disaggregated to identify specific technologies that may have been complementing the growth of the healthcare workforce. Data to perform similar occupation analysis in Australia and Canada is not available Conclusions: The rapidly growing healthcare workforce in the US compared to Canada and Australia are associated with rapidly growth among “other” healthcare workers. Disaggregation of occupations in the US shows that technicians/technologists, administrators and support staff are large contributors to the growth. The growth of technicians/technologists is consistent with previous studies that have identified technology as a driver of the growth of healthcare spending. The growth of administrators and support staff is consistent with studies about administrative waste due to the complex third party payment system in the US as well as the insufficient use of technologies that increase productivity, such as health IT. Implications for Policy, Delivery or Practice: By focusing on physician and nurses, the literature has ignored a significant portion of the healthcare workforce. The “other” healthcare workers play an important role in the delivery of healthcare and also contribute to the bulk of labor costs. Disaggregating occupational trends in the healthcare labor force is a conduit for linking discussions of technology to total healthcare spending. Funding Source(s): NIMH Poster Number: 264 The Influence of Local Area Physician Supply on the Dispersion of Care among Medicare Patients with a Consistent Diagnosis Presented by: An-Chen Fu, M.S., College of Pharmacy, The University of Iowa, 115 S. Grand Avenue, Iowa City, IA 52242; Phone: (319) 5129734; Email: anchen.fu@gmail.com Co-authors: John M. Brooks, Ph.D. Research Objective: Commentators have suggested that greater local area physician supply leads to the use of more physicians by patients, resulting in diffuse, uncoordinated, and wasteful care. However, we have found no studies that demonstrated direct relationships between local area physician supply and the use of physicians by individual patients. To fill this gap, we isolated a set of patients with a consistent diagnosis and course of treatment and investigated whether local area physician supply leads to the use of more physicians by these patients and more care dispersed across physicians during their first treatment course. Study Design: We estimated multiple regression models that relate local area physician supply in four specialty categories to the number of physicians used by patients within a consistently- defined first course of treatment and the dispersion of visits across physicians during the first course of treatment. Visit dispersion is measured via a Physician Visit Index that ranges from 0 to 1 and is derived from the Herfindahl concentration index. The closer the index is to 1, the more concentration patient visits were to fewer physicians. The explanatory variables are local area physician supply by specialty measured as the number of unique physicians in four specialty categories per 1,000 patients within 50-miles of patient zip codes. Population Studied: Stage III colorectal cancer patients diagnosed during 1992 to 2001 receiving surgery and chemotherapy but not radiation therapy during their first course treatment (n=6539) in SEER-Medicare-linked database. Principal Findings: Local area physician supply had significant affect on the number of physicians used by each patient and the dispersion of visits across physicians. However, the directions of these relationships varied by specialty. Local area primary care and oncologist supplies had positive effects on the number of physicians used and care dispersion. Whereas, local area surgeon supply negatively affected the number of physicians used and care dispersion. Conclusions: Our results show that local area physician supply affects the use of physicians by patients but that these relationships are specialtyspecific. Greater local area supply of primary care physicians and oncologists lead to increased physician utilization and care dispersion. However, greater local area surgeon supply decreased the number of physicians seen by patients and the dispersion of care across physician. Implications for Policy, Delivery or Practice: Commentators have suggested that greater local area specialist supply promotes greater care dispersion leading to wasted healthcare resources. Our study indicates that for certain physician specialties (surgeons), greater local area supply leads to the use of fewer physicians and less care dispersion. Perhaps specialists in areas with greater supply have more time to allocate to individual patients, thereby, lower the need to pass patients along to other providers. Future investigation can use the variation in physician use that is attributable to local area physician supply to assess the effects of care dispersion on patient outcomes and costs. Poster Number: 265 High-Performance Work Practices in Healthcare Management: Five Case Studies of Best Practices in Healthcare Organizations Presented by: Andrew Garman, Psy.D., Associate Professor and Associate Chair, Health Systems Management, Rush University Medical Center, 1700 W Van Buren, Suite 126 TOB, Chicago, IL 60612; Phone: (312) 942-5402; Email: Andy_N_Garman@rush.edu Lead Author: Ann Scheck McAlearney, Sc.D., M.S. Co-authors: Paula H. Song, Ph.D.; Megan McHugh, Ph.D.; Julie Robbins, M.H.A.; Michael Harrison, Ph.D. Research Objective: A capable workforce is central to delivery of high-quality care. Evidence from a breadth of sources outside and within healthcare suggests that innovative human resource practices (known as high-performance work practices (HPWPs) - including systematic personnel selection and incentive compensation -help attract and retain highly qualified health care staff; HPWPs also enhance individual and team performance. Hence, HPWPs may represent an underutilized healthcare improvement strategy. We investigated exemplary uses of HPWPs and their possible link to care quality and patient safety. Study Design: Following an extensive literature review, we performed five case studies of U.S. healthcare organizations purposively selected based on known success with HPWP use. Site visits in 2009 included in-person interviews with key organizational and clinical informants and collection of documents on HPWPs. Interviews were recorded and transcribed verbatim to permit rigorous qualitative analysis. Population Studied: Case study sites were purposively selected based on their reputation as exemplars for innovative human resource practices and to provide variability in organizational context, approach to the selected HPWPs, and their potential to serve as best practice examples worthy of attention and possible emulation by other healthcare organizations. Seventy-one key informants included human resources professionals, organizational leaders, clinical leaders, quality improvement professionals, information systems managers/directors, finance and accounting professionals, and select administrative and clinical personnel involved in HR practices. Principal Findings: Across sites and key informants, senior leadership support, capabilities of the implementers of the HPWPs, and organizational financial conditions were reportedly important in influencing the adoption and use of HPWPs. The four HPWP subsystems we had previously characterized as directly relevant to healthcare—organizational engagement, staff acquisition/development, frontline empowerment, and leadership alignment/development were reportedly eM.P.H.asized in each of the five organizations. While direct evidence of links between HPWPs and both employee outcomes (e.g., turnover, higher satisfaction/ engagement) and care system and organization-level outcomes (e.g., fewer “never events”, innovation adoption, lower agency costs, and lower turnover costs) was largely unavailable, informants consistently noted that they believed such links to exist, and that future data collection could quantify the links. Conclusions: These case studies provide examples and preliminary evidence of how HPWPs can improve operations and impact quality of care and safety in healthcare organizations. While further research is needed to assess the applicability of HPWPs to diverse settings and to assess the generalizability of our findings on HPWP impacts, we would encourage development of highperformance work systems within healthcare settings and assessment of their contributions to quality, safety, and other dimensions of organizational performance. Implications for Policy, Delivery or Practice: From a practitioner perspective, our findings highlight the importance and potential impact of HPWPs in healthcare organizations, and provide direction about best practices for these organizations to consider. From an academic perspective, these findings lay the groundwork for future research into a more definitive link between HPWP and quality outcomes; additional research will provide further insight as to which of the practices will have the highest leverage for improving quality and safety in healthcare. Funding Source(s): AHRQ Poster Number: 266 Psychosocial Stress at Work and Quality of Care among Surgeons in Germany Hospitals - Analysis of Survey Data using Structural Equation Modelling Presented by: Kirstin Grosse Frie, M.A., research associate, Center of Psychosocial Medicine, University Medical Center Hamburg-Eppendorf, Martinistr. 52, Hamburg, Germany 20246; Phone: +004940741054509; Email: k.grosse-frie@uke.unihamburg.de Co-authors: Jens Klein; Karl Blum, Dr.; Johannes Siegrist, Prof.; Olaf von dem Knesebeck, Prof. Research Objective: Psychosocial stress at work among physicians is a research topic of increasing importance. The effort-reward-imbalance model (ERI) is an established model to analyze psychosocial stress at work. The ERI-Model implies that high efforts and low rewards lead to chronic stress. Several international studies among health care professionals tested the model’s assumptions and proved that psychosocial work stress is a predictor of impaired health, burnout and depression. However, only a few studies examined associations between work stress and quality of care. Study Design: A cross-sectional standardized mail survey was conducted in German hospitals with a general surgical and gynecological ward. The questionnaire included the ERI-Questionnaire, a validated and reliable instrument consisting of scales for Overcommitment (specific cognitive and motivational pattern), efforts and rewards. Rewards were measured by the three sub-dimensions esteem, job security/ job promotion and salary. Respondent’s health care performance was measured by self-evaluation. Questions were phrased according to the SERVQUAL, a multipleitem scale for measuring service quality and the Physician Achievement Review, a multisource feedback questionnaire to assess the competencies of practicing surgeons. Additionally, two questions about the frequency of diagnostic and therapeutic errors were introduced. To analyze the association between work stress and health care quality structural equation modelling (SEM) was performed. Furthermore, gender and occupational position were additionally introduced into the model. Population Studied: 1,311 surgeons working in 489 hospitals (response rate 65%). Principal Findings: Results of the SEM showed significant chi-squares but fit indices for the model were good (CFI>0,96, RMSEA<0,4). Five latent health care dimensions were differentiated by confirmatory factor analysis: service quality, psychosocial health care, quality management, diagnosis and errors. No significant associations of high efforts and low rewards with these health care dimensions were found. Significant associations between high rewards and the three health care dimensions service quality, quality management and errors, implied better care in these dimensions. Significant associations between efforts and psychosocial health care as well as between overcommitment and diagnosis respectively errors, implied less quality of care. Conclusions: This study shows that psychosocial work stress according to the assumptions of the ERI-Model is not associated with a poorer evaluation of health care quality. It seems that there are other mechanisms between job stress and health care quality. Efforts and especially rewards seem to be important on their own and efforts can not be moderated by high rewards. Implications for Policy, Delivery or Practice: For redesigning physician's workplace environment it should be accounted for that higher rewards are associated with a higher evaluation of health care, but they should not be established to compensate high efforts. Funding Source(s): Hans Böckler Stiftung Poster Number: 267 The Changing Face of Primary Care Medicine: Implications for Workforce Development Presented by: Timothy Hoff, Ph.D., Associate Professor of Health Policy and Management, Health Policy, Management, and Behavior, University at Albany, SUNY, Room 181, GEC Building, 1 University Place, Rensselaer, NY 12144; Phone: (518) 402-6512; Email: thoff@albany.edu Research Objective: Primary care medicine is increasingly unattractive to medical students. Primary care specialties are also undergoing internal demographic shifts that have implications for workforce development. These shifts include increasing numbers of women physicians and international medical graduates (IMGs) going into primary care, an increasingly older primary care physician (PCP) cohort, and a younger PCP cohort that has different expectations regarding career and work. There is a need to examine the work experiences, values, and career expectations of PCPs to better understand the workforce recruitment and retention strategies that can attract more of the demographic groups already picking primary care in greater numbers. Study Design: A qualitative approach was employed involving semi-structured interviews with 88 PCPs practicing within a variety of distinct work settings. The qualitative approach was chosen to obtain rich description of how these newer PCP demographic groups think about their work and careers, and to explore what their perceptions and experiences imply for primary care workforce recruitment and retention strategies. Data were coded and analyzed using Atlas.ti software and a content analytic approach. Population Studied: Eighty-eight primary care physicians stratified on the basis of primary care specialty, age, career stage, gender, race and ethnicity, type of employment status, employment setting, and geographic location. These sampling strata were selected purposively, consistent with the qualitative approach, based primarily on the study focus which is exploring PCP cohorts according to age, gender, and ethnic background. By having an appropriate number of PCPs interviewed across the different cohort groups, constant comparison of interview data could occur both within and across the different groups. Principal Findings: The results suggest differences in career and work expectations between women, younger, and non-U.S. citizen PCPs compared to older, male, and white PCP cohorts. These differences relate to desired everyday job structures, motivations for choosing and remaining in primary care, preferred types of primary care work, and preferences regarding patient relationships. Several of these expectations were similar across the newer PCP demographic groups. Many of the expectations differed when compared to those held by older PCPs, especially concerning preferences among newer demographic groups for flexible, compartmentalized work schedules, adequate time off from work, and work based purely in the office ambulatory care setting. Conclusions: The descriptive findings inform the development of specific workforce recruitment and retention strategies in primary care medicine, which is losing practitioners faster than it can replace them. Implications for Policy, Delivery or Practice: From a practice level perspective, shifting preferences for particular types of job structures and time away from work encourages the consideration of new employment arrangements for PCPs that are non-traditional and may impact the the physician-patient relationship. In addition, younger cohort expectations regarding traditional PCP work such as hospital medicine and preferences for more office-based ambulatory care work requires policy eM.P.H.asis on making the ambulatory care setting the focal point for the right mix of rewards and incentives to keep PCPs satisfied and interested in continuing as primary care practitioners. Poster Number: 268 Analysis of the Effects of Primary Care Education in Japan Presented by: Genta Kato, M.D., Emergency Physician, Department of Primary Care and Emergency Medicine, Kyoto University Hospital, 54 Shogoin Kawahara-cho, Sakyo-ku, Kyoto, Japan 606-8507; Phone: +81757513126; Email: qq9f8hn9@gmail.com Research Objective: To clarify the existing problem concerning new residency training system in Japan, which shifts the focus from specialist training to primary care education from 2004 under the control of the Health, Labor and Welfare Ministry. Study Design: Analyzing qualitative data from unstructured interviews involving doctors who train new residents. Population Studied: 18 advising doctors being chosen by snowball sampling. Principal Findings: Under the new training system, residents belong to a general hospital in the first two years, and rotate between several specific departments. They learn each specialty for around two months. Some advising doctors are skeptical about whether the content of their education and the shortness of the period to which they are exposed to each specialty is effective. Others criticize residents' motivation to learn, since advising doctors must educate all residents, many of whom will never practice the teaching doctors’ specialty in the future. However, emergency physicians and general internees tend to be positive about the new residency training system. On the other hand, some young advising doctors positively evaluate this system because residents can broaden the scope of their learning. Conclusions: Although protocol for instruction is published by the Health, Labor and Welfare Ministry, most of the teaching doctors themselves are not primary care physicians, but specialists. Many teaching doctors do not feel satisfied with their instruction, because the new residency training system is not clear about whether it aims to yield many primary care physicians or to give residents common and practical medical literacy. Implications for Policy, Delivery or Practice: In Japan, patients’ accessibility to medical institutions is considered to be relatively convenient in that patients can visit various doctors regardless of their specialist field. However at the same time, some specialists cover the same territory as other physician with different specialties, including primary care, since the borders between one specialty and another are to some extent obscure. It is often said that the concept of ‘primary care’ is not well-established among patients and doctors in Japan. For example, the certifying system for primary care physicians is only 17 years old. In the Japanese new residency training system, ‘primary care’ practices are considered to be common knowledge for all doctors. Educated senior residents have no chance to make use of their skills as primary care physicians because from the 3rd year of their career they choose a specialty and from that point forward are trained only in that specialty. Even if we want to compare the new system with an old system in which residents were taught specific knowledge and skills from the beginning, it is difficult to estimate how much residents’ knowledge of primary care have been improved and upgraded. Since residents must spend their first two impressionable years acquiring skills of a primary care physician, policy makers should define the concept of ‘primary care’ and settle a specific image of goal more clearly to enhance the effectiveness of this education system. Poster Number: 269 Relationship of Regional Variations in the Use of ENT procedures for Children in NY State to Regional Variations in Physician Distribution Presented by: Lawrence Kleinman, M.D., M.P.H., Vice Chair, Health Evidence & Policy, Mount Sinai School of Medicine, One Gustav Levy Place, New York, NY 10029; Phone: (212) 659-9556; Email: lawrence.kleinman@mssm.edu Co-authors: Natalia Egorova, Ph.D. Research Objective: Describe regional variations in use of childhood otolaryngic (ENT) surgeries in NY State and their relationship to the number of primary care physicians (PCP) and surgical subspecialists (SSS) in each region, controlling for the number of children in each region. Study Design: Analysis of administrative data (SPARCS) for children <= 16 y.o. who had ambulatory surgery in NY State in 2006; 11 regions were defined by NY State Dept of Health. Physician data for 2006 are from Annual NY Physician Workforce Profile (SUNY Albany 2007). Linear regression used 3 predictor variables: number of children, PCP, and SSS per region. As outcomes for three models we looked at tonsillectomy and/or adenoidectomy(TnA), tympanostomy tube (TT) insertion, and either TnA or TT. We also regressed the square root of each outcome to confirm distributional assumptions. Population Studied: All children under 16 years of age who had an ambulatory surgery at a facility reporting to SPARCS, which is intended to be a comprehensive statewide data reporting system and serves as NY State's data source for the federal Health Care Utilization Project data collection. Principal Findings: Region populations vary from ~250,000 to 650,000 children. 10.3% of SSS were otolaryngologists and 24.6% of PCP pediatricians. Regional variation is considerable: TT range 1.3-8.5 per 1000 children (statewide mean 4.3), TnA 1.79.9 (5.1), either 2.6-15.8 (8.3) Models for all three outcomes had consistent results, as did those using SQRT(outcome). Controlling for population, the marginal increase in the number of surgeries associated with each SSS was slightly more than the decrease associated with each PCP. Betas for the model regressing either TT or TnA were: population of children 0.02; surgical specialists 8.8; primary care provider -6.8, r-squared=0.88, all betas <.05. Conclusions: Childhood ENT surgery is known to be highly discretionary. In NY in 2006 ENT surgery use varied by region directly proportional to the number of surgical specialists, and inversely proportional to the number of PCP. If causal, extrapolation would estimate an average marginal impact of 84.5 more surgeries per year for each ENT surgeon and of 27.7 fewer surgeries per year for each pediatrician per region. Limitations include ecological data from one state and lack of granularity of specialty within each region. Strengths include high quality full population data. Implications for Policy, Delivery or Practice: This early study suggests that the phsyician disribution and specialty distribution may influence the use of ENT surgery in children. Our findings suggest that surgery use increases as the mumber of surgical specialists increase and decrease as the number of primary care providers increase. If confirmed this could have important implications for quality and cost of care and provides data to guide physician workforce policy. Poster Number: 270 The Frontline Healthcare Worker: An Underrecognized Resource for a 21st Century Healthcare System Presented by: Thomas Konrad, Ph.D., Senior Fellow, Cecil G. Sheps Center for Health Svcs Research, University of North Carolina at Chapel Hill, 725 MLK, Jr. Boulevard CB 7590, Chapel Hill, NC 27599-7590; Phone: (919) 966-2501; Email: bob_konrad@unc.edu Co-authors: Emmeline Chuang, A.B.; Jennifer Craft Morgan, Ph.D.; Janette Dill, M.A., M.P.H. Research Objective: Frontline healthcare workers (FLWs), consisting of 7 million workers in 32 health care occupations, currently constitute about half the US healthcare workforce. These workers have median annual wages <$40K and often less than a bachelor’s degree. Although FLWs play a critical role in the delivery of “hands on” healthcare, little systematic information exists about their life circumstances, work motivations, job satisfaction, and how they view their contributions to health outcomes across different types of healthcare organizations. This study fills that gap. Study Design: Data used for this study were drawn from an eight-page survey administered to 819 FLWs working in 42 health care employers. These data were collected as part of a baseline assessment of FLWs within Jobs to Careers, a national program supporting partnerships of health care employers, educational institutions, and other organizations across the U.S. Survey items included questions about FLW demographics, job history, wages, and job perceptions. Job perception items were adapted from existing instruments, aggregated into multi-item scales, assessed for validity reliability, and examined. Analysis of variance of scale means and percentages and chisquare tests comparing categorical variables (p<.05) were used to assess cross-segment variability. Population Studied: Frontline workers across four major health care sectors: hospitals, long-term care (LTC), community health centers, and behavioral health centers. Principal Findings: Frontline workers within our sample are overwhelmingly female (90%), minorities (50%), and dependent on their paycheck as the sole source of family income (60%). A significant percentage are also single mothers (20%). These FLWs have positive perceptions of quality of care that their employers provide and high global job satisfaction (7.9 and 7.1 on 10-pt scales) especially with intrinsic aspects of work (i.e., carework). Although there is widespread dissatisfaction with work overload (2.6 on an 8-pt scale), FLWs express high levels of commitment to current employers--only 10% are considering leaving their jobs. Some cross-sector differences are observed in specific facets of job satisfaction. In LTC settings, where entry level educational requirements are lower, only 20% of respondents have some college (as opposed to 40% in other sectors). LTC workers have somewhat lower wages and are less satisfied with career opportunities and supports than FLWs in other settings. Conclusions: FLWs--a sizable, ubiquitous, and critical yet relatively invisible component of the healthcare system--can be considered a single workforce, with a common set of demographic and socioeconomic challenges, positive perceptions of their core work, and high levels of commitment to their employers. However, these FLWs face many common barriers to skill and career development, suggesting that similar approaches may be used to improve their situation and enhance their contributions to health care quality and population health. Particular challenges are found in the LTC segment of the workforce. Implications for Policy, Delivery or Practice: Given high demand for FLWs and evidence of that they can be committed to employers and patients, increased private and public investment in the career development of these workers by employers, educational institutions, and workforce development organizations seems warranted. Funding Source(s): RWJF, The Hitachi Foundation, US Dept of Labor Poster Number: 271 Using Health Policy Education Targeted toward Underserved Patients to Promote Interdisciplinary Collaboration Presented by: Helene Lipton, Ph.D., Professor, Institute for Health Policy Studies, University of California, San Francisco, 3333 California Street, Suite #265, San Francisco, CA 94118; Phone: (415) 476-2964; Email: smitha@pharmacy.ucsf.edu Co-authors: Amanda Smith, M.P.H.; Cindy Lai, M.D.; Timothy Cutler, Pharm..; Marilyn Stebbins, Pharm.D. Research Objective: Given recent and anticipated health reforms, it is critical to improve health policy literacy among medical students, residents, and other health professionals. One such reform is Medicare Part D (“Part D”), a federal program providing drug coverage for Medicare patients. In 2006, we developed an interdisciplinary Peer Educator program, in which pharmacy students educate health professionals about Part D. After demonstrated success of this initiative at our own institution, our objectives were: (1) to assess whether this Peer Educator program can be replicated at other institutions and (2) to evaluate the impact of the program on learners’ Part D knowledge, intent to collaborate with pharmacists, and awareness of the special challenges underserved Part D patients confront. Study Design: The program was expanded statewide by training faculty champions at six additional California pharmacy schools to develop their own Part D Peer Educator programs. Peer Educators were pharmacy students selected through a competitive application process. Part D policy lectures ranged from one-to-two hours and used a case-based approach to demonstrate specific strategies that physicians and other prescribers can use to ensure access to appropriate drug plans and decrease out-of-pocket drug costs for underserved patients. A pre-post survey was administered to all attendees. Population Studied: Targeted audiences included students, residents, nurse practitioners and faculty from health professional schools and academic medical centers. From October 2008 to November 2009, Peer Educators delivered 36 Part D lectures statewide to 1,011 health professionals. A total of 950 pre-post surveys were completed (response rate = 94%). Principal Findings: Lack of Part D training was evidenced by the fact that before the lecture, 60% of learners reported no prior exposure to Part D. Using the Wilcoxon signed-ranks test, ten of eleven outcome measures were improved significantly, compared to baseline (p<0.0001). The biggest gains were noted in learners’ knowledge of the Part D benefit and their ability to identify clinically relevant resources to help patients. Learners also significantly increased their awareness of challenges confronting underserved Part D patients and their intention to collaborate with pharmacists on patient activities including drug product selection, formularies, Part D insurance issues, and drug costs. Improvements were consistent across all schools. Of the 950 learners, 86% rated the overall quality of instruction on a 5-point Likert scale (1=poor, 5=excellent) as either “very good” or “excellent”. Similarly, 83% of participants rated the information presented as “very useful” or “extremely useful” (1=not at all useful, 5=extremely useful). Conclusions: With a combination of dedicated faculty champions and clinically relevant material, the Peer Educator program was rapidly integrated into six additional schools of pharmacy, demonstrating that trained students can significantly improve health policy knowledge, attitudes toward other health care professionals, and increase the likelihood of interdisciplinary collaboration. Implications for Policy, Delivery or Practice: Lack of Part D training for health professionals limits their ability to help patients’ realize the intended benefits of Medicare Part D. Our research suggests that academic health centers, working with policymakers, should initiate health policy education programs that also foster interdisciplinary collaboration, especially regarding care delivery for underserved patients. Funding Source(s): The Amgen Foundation Poster Number: 272 An Exploration of the Relationship Between Employee’s Personality Characteristics and the Implementing Effect of Hospital Learning Organization Models Presented by: Chenchung Ma, Ph.D., Assistant Professor, Healthcare Administration, I-Shou University, 8, Yida Road, Yanchao Township, Kaohsiung County, Taiwan 824; Phone: +073836187; Email: up000238@isu.edu.tw Lead Author: Chien-Chang Yang, M.H.A. Co-authors: Patricia Moulton, Ph.D.; Paul Su, Ph.D. Research Objective: In the knowledge-based economical age, entrepreneurs who apply the learning organization model will enhance their competitive advantage. A learning organization is an organization that facilitates the learning of all its members and continuously transforms itself. Learning organization can lead better employee satisfaction. The learning organization model has become the successful model that business desires. Whether the learning organization can be implemented well or not depends on the staff in the organization. The personality characteristics of employees can deeply influence the effect of learning within an organization. This research was conducted to find out how employee’s personality characteristics related to implementation effectiveness in five Taiwan hospitals who have implemented the learning organization model. The results will provide valuable information to other healthcare organizations as they start to implement learning organization models in their facility, especially when recruiting staff. Study Design: This study used a cross-sectional research design to identify the relationship between employee’s personality characteristics and the implementing effect of hospital learning organization models. The structured questionnaire for this study contained 57 items in three parts: (1) Employee’s personality characteristics contained 30 items and measured by a five-point Likert-type scale, (2) Learning organization models contained 20 items and measured by a five-point Likert-type scale, and (3) demographics contained 7 items. This cross-sectional design involves the collection of data at one point in time. Population Studied: The target population for this study was employees at five hospitals in northern, central, southern, and eastern areas of Taiwan. Each hospital distributed 100 questionnaires via human resource department staff to physicians, nurses, medical technicians, and administrative staff. A total of 500 questionnaires were distributed and 419 completed questionnaires were returned resulting in a response rate of 83.8%. Principal Findings: Analysis of variance (ANOVA) demonstrated that the implementing effect of learning organization varied significantly based on gender, age, marital status, level of education, job position, job category, and year of service. Openness to experience, conscientiousness, extraversion, and agreeableness all had positive correlations with the implementing effect of learning organization. Only neuroticism showed a negative correlation with implementation effectiveness ((R)= -0.284, P<0.01). Conclusions: This study indicates that the higher the educational level, the greater likelihood of better implementation of the learning organization model. Medical technicians and administrative staff had higher scores of the implementation of the learning organization models. In the future, when healthcare organizations recruit and select the employee, they should take level of education into consideration. Furthermore, they should also encourage their employees to attend on-the-job training courses. Another result indicated that the employee’s personality characteristics will influence the effectiveness of the learning organization model. Therefore, when healthcare organizations recruit and select employees, they should consider employee’s personality characteristics in order to find the appropriate employee to serve in healthcare organizations. Implications for Policy, Delivery or Practice: This study provide valuable information to other healthcare organizations as they start to implement learning organization models in their facility, especially when recruiting staff. Poster Number: 273 Increasing the Supply of Nurse Educators Presented by: John Marcotte, Ph.D. Center for Health Outcomes & Policy Research, University of Pennsylvania, PA 19104-4217; Phone: (215) 8987716; Email: marcotte@nursing.upenn.edu Lead Author: Robyn Cheung, R.N., Ph.D.; Email: cheungr@nursing.upenn.edu Research Objective: The object of this study is to assess what factors increase or decrease the likelihood that nurses will work in nursing education. In order to be an educator, a nurse must at least obtain a master's degree; therefore, this study also assesses what factors influence educational advancement among nurses. Study Design: The data are from multiple cohorts of nurses dating from the 1960s through the mid2000s. The design has two stages. The first stage examines what affects whether nurses obtain advanced degrees (master's and above) while the second stage looks at what influences whether nurses with advanced degrees work in nursing education. Since the data contain degree dates, we are able to analyze how long until nurses earn second or third degrees and how long before nurses engage in nursing education. Because the data cover multiple decades, we also examine age, period and cohort effects. Population Studied: Nurses from the 1960s through today are the study population. Principal Findings: Initial degree is a strong determinant of whether nurses ultimately obtain a degree that qualifies them for teaching. Nurses whose first degree is an Associate's as opposed to a Bachelor's rarely advance. Results also show differentials about ethnic groups in the rate of obtaining advanced degrees and engaging in teaching. Conclusions: While both Associate's and Bachelor's degrees qualify nurses to work. Only the Bachelor's is a potential gateway to obtaining an advanced degree. As a result, a study of what determines the supply of nurse educators must examine factors affecting both the earning of advanced degrees and the engaging in teaching. Implications for Policy, Delivery or Practice: The key policy question is how to increase the number of nurses who work in nursing education. From a policy standpoint, nurses should be encouraged to obtain a BSN as the first degree. Without an initial BSN, nurses are effectively locked out from teaching. Increasing the number of qualified nurse educators will ultimately produce more nurses. Poster Number: 274 Economic Burden of Illness for the United States Workforce With Chronic Musculoskeletal Pain Conditions: Arthritis, Back and Fibromyalgia Pain Presented by: Margaret McDonald, Ph.D., Director Health Economics and Outcomes Research, Global Market Access, Pfizer Inc, 235 East 42nd Street, New York, NY 10017; Phone: (212) 733-3093; Email: margaret.m.mcdonald@pfizer.com Co-authors: Marco daCosta DiBonaventura, Ph.D.; Stacey Ullman, M.H.S. Research Objective: Few studies have simultaneously assessed the impact of pain and productivity loss for US workers with arthritis, back problems or fibromyalgia. This study updates the current literature by comparing absenteeism, presenteeism, and average annual direct and indirect health care costs for US workers reporting pain from these chronic musculoskeletal conditions to workers without these painful conditions. Study Design: Cross-sectional study design. Work productivity was assessed using the Work Productivity and Activity Impairment (WPAI) questionnaire. Four subscales (absenteeism, presenteeism, overall work impairment, and activity impairment) are generated in the form of percentages of time missed due to health. Direct costs were total employer medical costs and indirect costs were costs associated with absenteeism and presenteeism. Population Studied: Analysis of national data collected from employed (full-time, part-time, or self-employed) US adults aged 20 to 64 years participating in the US National Health and Wellness Survey (NHWS) 2008 (N=30,828). Principal Findings: Of the 122 million US workers aged 20 to 64 years, 34% reported pain in the past 12 months. Among these workers, 24%, 46%, and 4.1% reported arthritis, back or fibromyalgia pain, respectively, in the past month. Absenteeism among workers with arthritis, back or fibromyalgia pain is 8.2%, 7% and 15.3%, respectively. For workers without arthritis, back or fibromyalgia pain, absenteeism is 4.3%, 4.2% and 4.5%, respectively (p<0.0001 for all absenteeism differences). Presenteeism (reduced productivity while working) is highest for workers with fibromyalgia pain (45.3%), followed by workers with arthritis or back pain, 31.9% and 27.3%, respectively. Among workers without fibromyalgia, arthritis or back pain, presenteeism is 16.2%, 15.2% and 14.6%, respectively (p<0.0001 for all presenteeism differences). Average annual direct health care costs per worker with fibromyalgia pain vs. without fibromyalgia pain are $6,082 vs. $2,437; indirect costs are $15,966 vs. $6,269; total costs are $22,048 vs. $8,706 (p<0.001 for all cost differences). Arthritis pain sufferers had 2 times the annual total health care costs per worker than nonsufferers ($16,787 vs. $8,148; p<0.0001); back pain sufferers and non-sufferers had average total health care costs of $14,151 and $7,899, respectively (p<0.0001). Conclusions: Chronic, painful conditions are costly to employers. Pain sufferers generally reported twice the level of absenteeism and presenteeism, and higher associated annual health care costs relative to non-sufferers. Fibromyalgia pain sufferers had the highest impairment metrics and associated costs. Implications for Policy, Delivery or Practice: Increasing awareness and effective programs and polices can encourage proper risk management, treatment and prevention. Poster Number: 275 Frontier America's Health Workforce Supply and Population Health Outcomes Presented by: Preethy Nayar, M.D., Ph.D., Asst. Professor, Health Services Research and Administration, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198; Phone: (402) 559-1981; Email: pnayar@unmc.edu Co-authors: Bettye Apenteng; Ahn Nguyen, M.P.H.; Keith Mueller, Ph.D. Research Objective: The objective of this study was to examine and compare the county level characteristics including demographics, workforce supply and population health outcomes of frontier and non-frontier counties in the United States. Study Design: The study design is a crosssectional descriptive study. Population Studied: All counties in the United States were studied using the Community Health Status Indicators (CHSI) 2008 data. The definition of frontier county used is the conventional definition of less than 7 persons per square mile. In 2005, of a total of 3141 counties in the US, 419 were frontier counties. Principal Findings: Frontier counties have a significantly higher proportion of elderly and white population. Although not statistically significant, frontier counties also have a higher poverty rate.Frontier counties have a lower average life expectancy as compared to non-frontier counties (66 vs. 76). Frontier counties also have a significantly lower ratio of primary care physicians per 100,000 population and dentists per 100,000 population(not statistically significant)and a higher rate of Health Professional Shortage Area or HPSA single-county, primary medical care, health professional shortage area designation. Conclusions: “Very little exists in the published literature on the health, mental health and related problems in these [frontier] areas” (Wagenfeld, 2000).This study decribes the unique challenges that frontier counties face in terms of demographics, population health outcomes and health workforce supply. Implications for Policy, Delivery or Practice: Frontier counties in America face significant challenges in terms of access to health care delivery due to geographical isolation. Policy makers should take in to consideration these unique challenges and design innovative solutions, including a greater use of telehealth initiatives, to address these issues. Funding Source(s): Other Govt Poster Number: 276 Perceptions of Work Environment, Burnout, and Job Dissatisfaction: Are There Differences Between International and U.S. Nurse Graduates? Presented by: Donna Felber Neff, Ph.D., R.N., Assistant Professor, College of Nursing, University of Florida, PO Box 10087, Gainesville, FL 326100187; Phone: (352) 273-6334; Email: dneff@ufl.edu Co-authors: Jeannie Cimiotti, D.N.S., R.N.; June Nogle, Ph.D.; Linda Aiken, Ph.D., R.N., F.A.A.N. Research Objective: In the US, the state of Florida employs the second highest number of internationally educated nurses. The purpose of this study was to determine if differences exist in international nurse graduates and US educated nurses’ perceptions of the professional practice environment, job-related burnout, and job satisfaction. Study Design: This was a secondary analysis of 2007 survey data collected from a random sample of registered nurses licensed and residing in the state of Florida. Nurses’ were queried on a number of items that included demographics, work setting, aspects of the work environment, satisfaction with their work, and perceived job-related burnout. The quality of the nurse work environment was measured by the Practice Environment Scale of the Nursing Work Index. Nurse job-related burnout was measured using the Maslach Burnout Inventory – Human Services Survey. Population Studied: Nurses met inclusion criteria if they provided direct patient care (n=6628) in an adult acute care hospital. Nurses were categorized based on their basic nursing education as obtained in the US or elsewhere. Principal Findings: Of the hospital nurses included in our sample 5,734 (87%) were educated in the US. When compared to US educated nurses, significantly larger proportions of internationally educated nurses had a BSN degree and were significantly more satisfied with their jobs. While there were no significant differences, more than a third of the nurses in both groups reported high levels of job-related burnout as defined for health care providers. Furthermore, internationally educated nurses reported a significantly more favorable mean score on work environment on four of the five subscales of the Practice Environment Scale - staffing and resource adequacy; nurse participation in hospital affairs; nursing foundations for quality of care; nurse manager ability, leadership, and support. There were no significant differences between the two groups in mean scores of the subscale collegial nurse physician relationships. Conclusions: When compared to US educated nurses, internationally educated nurses are more likely to have a BSN, have a better perception of the work environment and are more satisfied with their jobs. However, both groups of nurses report high level of job-related burnout. Implications for Policy, Delivery or Practice: Currently in the US, there are 116,000 nurse vacancies in hospitals, and it is projected that the demand for registered nurses will continue to grow by 2 to 3% each year. Active recruitment of international nurse graduates has increased substantially to address this shortage. Based on previous work describing the work environment of nurses and patient outcomes, the findings from this study suggest that the use of internationally educated nurses should complement the quality of care provided by US trained counterparts. However, job-related burnout continues to plague registered nurses regardless of their country of origin. Poster Number: 277 Does Use of Supplemental Nurses Increase Hospital Costs? Presented by: Katia Noyes, Ph.D., Associate Professor, Department of Community and Preventive Medicine, University of Rochester Medical Center, 601 Elmwood Avenue Box 644, Rochester, NY 14642; Phone: (585) 275-8467; Email: katia_noyes@urmc.rochester.edu Lead Author: Ying Xue, D.N.Sc. Co-authors: Andre Chappel, Ph.D. candidate; Linda Aiken, Ph.D.; Deborah Freund, Ph.D.; Katia Noyes, Ph.D. Research Objective: The United States is in the midst of a nursing shortage, which is expected to intensify as baby boomers age and the need for health care grows. At the same time, there is tremendous pressure on hospital administrators to design organizational systems that are both efficient in cost and offer high quality of care. The purpose of this study is to examine the impact of use of supplemental registered nurses (SRNs) on quality of care and cost. Study Design: Data on patient satisfaction, inhospital mortality, and nurse turnover are regularly collected for performance assessment. Medication errors, falls, and pressure ulcers were reported by clinicians. Costs associated with admissions, total reimbursement (net revenue) and direct costs per patient stay were obtained from the hospital’s billing and administrative records. These financial measures were then aggregated by quarter to the unit level. The length of stay in each unit was also derived from the billing records and aggregated by quarter to the unit level. The quarterly financial measures for each unit were then divided by the total patient days per unit. The quarterly per day financial measures were adjusted for patient casemix (mean age, percent male, and patient severity and comorbidities) and clustered at the unit level. We used the risk-adjusted per day financial measures and risk-adjusted quality indicators for the cost-effectiveness analysis (CEA). To calculate the incremental cost-effectiveness ratio (ICER) for each unit (n=17), we used the unit with the lowest percentage of SRNs among all RNs across all quarters (0.43%) as a control. Population Studied: The study examined patient discharges in adult medical, surgical, and ICU units in a large Upstate New York teaching hospital between 2003 and 2006. Principal Findings: Higher charges were associated with higher revenue and higher costs (correlation 0.9). Very low and very high SRN use (up to 13%) was associated with higher costs compared to units with near average SRN use. Patients in most of the units had lower overall satisfaction with care than patients in the control unit with the lowest SRN use and, hence, these units were dominated by the control unit. Units with higher SRN use had lower mortality and higher per diem costs than the lowest SRN use unit, with ICERs between $2,953 per life saved to $75,295 per life saved. In respect to medication errors, the units with higher SRN use spent between $166 and $2,252 per error reduced compared to the unit with the lowest SRN use. Finally, the majority of units had about the same or worse RN turnover than the control unit (with lowest use of SRNs), but had higher per diem costs. Conclusions: Our results indicate that the underlying reason for why certain hospital units use SRN may be more important than overall percent of SRN and total SRN time. We found no evidence that use of SRN leads to higher hospital costs. Implications for Policy, Delivery or Practice: Use of SRNs could be one strategy for hospitals to supplement nurse staffing without experiencing negative economic consequences. Funding Source(s): RWJF Poster Number: 278 Recruiting and Retaining Primary Care Physicians in Urban Underserved Communities: The Importance of Having a Mission to Serve Presented by: Kara Odom Walker, M.D., M.P.H., M.S.H.S., Robert Wood Johnson Clinical Scholar, University of California, Los Angeles, 911 Broxton Avenue, 3rd floor, Los Angeles, CA 94110; Phone: (215) 292-4963; Email: kodom@mednet.ucla.edu Co-authors: Gery Ryan, Ph.D.; Robin Ramey, M.S.; Felix Nunez, M.D., M.P.H.; Robert Splawn, M.D., M.P.H.; Arleen Brown, M.D., Ph.D. Research Objective: Improving the supply of the physician workforce in the safety net must remain a national priority. In Los Angeles County, however, recent funding cuts and hospital closures have reduced the number of providers serving minority, underserved and uninsured populations. Working with a community advisory board (CAB), comprised of researchers, medical educators, physician leaders, and community clinic administrators, our objective was to identify strategies to enhance recruitment and retention of primary care physicians in urban underserved settings. Study Design: We conducted a community based participatory research qualitative study through indepth, semi-structured interviews. We recruited participants using snowball sampling, starting with a first wave of referrals from the CAB followed by 2 waves of referrals from interviewed physicians. Research team members trained in qualitative interviewing techniques used a standard interview guide. Transcriptions were reviewed independently by two research team members and coded into themes by the investigators using pile-sorting methods (intercoder reliability, Kappa=82.6%). Population Studied: Forty-two non-Latino White, African American and Latino physicians who reported their specialty as primary care (internal medicine, family medicine or pediatrics) and practiced over 20 hours/week in a clinical setting, were equally stratified into underserved and nonunderserved areas, defined by a census tract or comprehensive clinic designated as a Health Profession Shortage Area within Los Angeles County. Principal Findings: The 42 participating primary care physicians ranged in age from 31 to 73 years (mean age 48 years, SD=12); 45% were female; 56% had no educational debt; and 21% had loan repayment obligation. By specialty, 53% were in internal medicine, 30% were in family medicine, 17% were in pediatrics. Three major themes emerged in relation to selection of current geographic and population based practice decisions: 1) personal motivators, 2) career motivators, and 3) clinic support. We found that themes describing personal motivators (e.g. personal mission and self-identify) for choosing a practice were more common among physicians who worked in underserved areas than those who did not. In contrast, physicians in non-underserved areas were more likely to cite work hours and lifestyle as reasons for selecting their current practice location or leaving an underserved area. Regardless of their race or ethnicity, the majority of physicians who practiced in underserved areas reported feeling a unique connection to the particular community in which they practiced. Notably, none of the physicians who trained in a non-underserved setting went to work in an underserved setting underscoring the importance of training in underserved locations. Conclusions: Ultimately, a concerted health care workforce policy can address distribution disparities in underserved areas and comprehensively address challenging issues such as benefits, salary, lifestyle, work schedule, and physician specialty distribution. Enlightened and informed recruitment strategies should seek out, develop and train a corps of motivated, mission-driven, and committed primary care physicians and retaining them by employing strategies to improve work/life balance. Implications for Policy, Delivery or Practice: The current health care reform debate provides unique opportunities to develop and implement policies that support both a larger primary care workforce and incentives that encourage physicians to practice into shortage areas. Funding Source(s): RWJF, University of California Los Angeles Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30AG021684 Poster Number: 279 Workforce Challenges in Delivering Healthcare to Elderly and Low-Income Populations: Wyoming Medical Providers’ Acceptance of Medicaid and Medicare Patients Presented by: Davis Patterson, Ph.D., Research Scientist, Department of Family Medicine, WWAMI Center for Health Workforce Studies/Rural Health Research Center, 4311 11th Avenue NE, Suite 210B, Seattle, WA 98105; Phone: (206) 543-1892; Email: davisp@uw.edu Co-authors: Susan Skillman, M.S.; C. Holly Andrilla, M.S.; Mark Doescher, M.D., M.S.P.H. Research Objective: National studies show differences in healthcare providers’ acceptance of patients according to type of insurance. Wyoming, a highly rural state, offers an intriguing case study of state and federal healthcare policies targeting low income and elderly patients. EqualityCare, Wyoming’s Medicaid program, offers “Pay for Participation” provider incentives and reimburses providers at high levels compared with Medicare and other states’ Medicaid programs. EqualityCare also covers a narrower segment of its low-income population than do many other states. This study sought to (1) determine the extent to which Wyoming medical professionals currently serve Medicaid and Medicare enrollees, (2) identify factors associated with provider acceptance of new patients, and (3) consider policy options for strengthening the health workforce and patient access to high-quality care. Study Design: Cross-sectional surveys of all Wyoming healthcare facilities and multiple types of licensed professionals, using contact lists maintained by state licensing boards, were conducted in late 2008 and early 2009 via postal mail, internet, fax, and e-mail. Population Studied: This study analyzed survey data (response rates in parentheses) from 261 medical clinics (83%), and three types of providers: 561 physicians (56%, including osteopathic physicians), 108 physician assistants (62%), and 132 advanced practice nurses (56%). Principal Findings: Wyoming ambulatory care providers accepted both Medicaid and Medicare patients more readily than did U.S. physicians as a whole. More Wyoming ambulatory care providers reported accepting at least some new Medicaid patients (96%) than Medicare patients (91%). This pattern is reversed among all U.S. physicians (72% v. 86% in 2008). Clinics that accepted new Medicaid patients (mean of 12.4 staff FTEs) were larger than those that did not (5.2 FTEs). Specialists were more likely than primary care providers, and rural were more likely than urban physicians, to accept new Medicaid and Medicare patients. In clinics that served more rather than fewer Medicare patients, new patients waited longer for an appointment. Conclusions: Providers’ higher rates of accepting new Medicaid patients, relative to both national rates and Medicare acceptance rates in Wyoming, provide preliminary evidence that Wyoming’s EqualityCare policies have had a positive effect. Providers vary significantly, however, and systematically, in their acceptance of both types of insurance. Implications for Policy, Delivery or Practice: Wyoming offers insights into the effectiveness of state and federal policies to insure low-income and elderly populations, particularly relevant to states with significant rural populations. As Medicaideligible populations grow in an economic downturn, maintaining coverage levels is a formidable challenge for declining state budgets. Smaller clinics, particularly those that are the sole healthcare providers in a community, may require special incentives to ensure Medicaid patient access. Meanwhile, as elderly populations grow in Wyoming and elsewhere, healthcare access may become increasingly limited without changes to Medicare reimbursement policies, such as the Dorgan-Conrad amendment to health reform legislation. Providers in isolated rural communities may feel socially or financially obligated to accept all patients, contributing to the higher rural Medicaid and Medicare acceptance rates found in this study. Further stress to reimbursement in rural areas due to an increasing proportion of Medicare patients or other factors ultimately could exacerbate shortages of rural primary care providers. Funding Source(s): Wyoming Healthcare Commission Poster Number: 280 Policy Implication of the Narrowing Scope of Primary Care Practice Presented by: Stephen Petterson, Ph.D., Sr Health Policy Researcher, Robert Graham Center, 1350 Connecticut Avenue, Washington, DC 20036; Phone: (202) 331-3360; Email: spetterson@aafp.org Co-authors: Nicole Johnson, M.D.; Jason Rinaldo, Ph.D. Research Objective: As health care reform focuses on primary care as the solution to the current national health care climate, policy will declare which services are eligible for primary care incentive reimbursements. However, the proposed services per the Medicare Payment Advisory Commission (MedPAC) may be too restrictive. Squeezed on one side by nurse practitioners and physician assistants and on the other side by subspecialists, the de facto scope of practice of U.S. primary care physicians has narrowed substantially in past decades. MedPAC’s proposals to limit a definition of primary care to Evaluation and Management CPT codes may worsen this trend. To inform current policy discussions, this study presents evidence about the range and variation the practices engaged in by family physicians (FPs). Study Design: We use questions about the percent of time providing emergency care, urgent care, major surgery, maternity care, office surgery, pain management, palliative care, pre- and post-op care, and hospital care. Diplomates were also asked whether they provided prenatal care, care of newborns and the average annual number of deliveries. Our independent variables include practice structure (solo, group, partnership, other), years in practice, gender and a four-category measure of rurality (urban, large rural, small rural, isolated rural and rural frontier) based on the RuralUrban Commuting Area (RUCA) classification. Methods: STATA 9.2 was used to obtain simple descriptive statistics and multivariate logistic regression models. Population Studied: 2009 ABFM Administrative data. ABFM obtains detailed practice characteristics from FPs. Starting in 2005, this information is available from nearly every diplomate taking the certification exam (n=26,186). Principal Findings: FPs are engaged in a wide range of activities, but any particular activity accounts for a relatively small percentage of their work week. One exception is urgent and emergency care, due mainly to a small fraction of diplomates (5%) who devote nearly 100% to either type of care. For instance, while about 40% of FPs devote some time to office surgery, on average this amounts to less than 1.5% of their time. The multivariate results show considerable variation across practices. FPs in rural areas are substantially more likely to perform procedures—major and minor surgery as well as delivering babies—and are more likely to practice emergency care, pain management and palliative than their urban counterparts. Female FPs are significantly more likely practice maternity and newborn care than male FPs, but less likely to perform procedures. Physicians with fewer years of practice are significantly less likely to deliver babies or perform procedures in their office. They are significantly more likely to practice urgent care. Conclusions: Reform measures that attempt to define primary care via claims-based definitions of scope risk harming some providers absent knowledge of the current breadth and scope of practice. This is particularly true for rural providers whose broad scope includes procedural care not currently included in reform bill definitions. Implications for Policy, Delivery or Practice: The disparity between MedPAC’s defined scope of primary care and those proposed by the professional societies that comprise and represent primary care physicians must be reconciled. Policy that allows exemptions, lower thresholds, or considers a broader scope of practice of primary care services must be considered as health care reform unfolds. Funding Source(s): HRSA, ABFM Poster Number: 282 General Internal Medicine and Medicare Spending Variation Presented by: Stephen Petterson, Ph.D., Senior Health Policy Researcher, Robert Graham Center, 1350 Connecticut Avenue Suite 201, Washington, DC 20036; Phone: (202) 331-3360; Email: spetterson@aafp.org Co-authors: Robert Phillips, M.D., M.S.P.H.; Bridget Teevan, M.S. Research Objective: Healthcare costs for people naming a general internist as their usual source of care are significantly higher compared to those with a family physician (FP), and a much higher proportion of general internists would not be eligible for proposed primary care bonuses. This study sought to understand their relationship to variations in healthcare spending. Study Design: Dartmouth data for hospital referral region (HRR, n=307) and primary care service areas (PCSA, n=6542) allow ecologic observation of relationships between clinicians, utilization and costs. At the PCSA level, we examined the relationship of Part A Medicare costs to quintiles of per capita general internists and FPs and to quintiles of per capita non-primary care physicians. For HRRs, we examined the association of nonprimary care specialists with general internists and FPs; and the association of Medicare expenditure with general internists and FPs. We also examined the association between primary care as a percentage of the physician workforce and growth in Medicare spending between 2000 and 2006 using least-squares linear regression, weighting observations by HRR 2000 population, and adjustments for baseline expenditures and potential ecologic confounders, and finally this association in HRRs with more non-primary care specialists. Population Studied: General internal medicine physicians and family physicians. Principal Findings: Within PCSAs, Medicare Part A costs per beneficiary increased as general internists increased, regardless of non-primary care physician count; whereas, costs per beneficiary declined as FP counts increased, particularly in areas with more specialists. In the HRR analysis, there was a strong positive association between non-primary care specialists and general internists (r=.848, p<.001), but a negative association with FPs (r=-.234, p<.001). There was a significant positive association between Medicare spending (Part A and B) and availability of general internal medicine (GIM) within HRRs (r=.404, p=<.001), but a significant negative association for FPs (r=-.593, p<.001). There is a strong association between the percentage of the total physician workforce that is primary care in an HRR and supply of FPs (.767, p<.001) Adjustments for baseline expenditures and ecologic variables made the cost-reducing effects of primary care growth insignificant, except in regions with more specialists where a 10% increase in the percent primary is associated with a 1.06% decrease in the annual growth rate (p=.056). Conclusions: Ecologic analyses are consistent with patient- and physician-level analyses, suggesting that the general internists’ role may contribute to cost variation. General internists are more likely to locate like non-primary care specialists, but this does not explain the ecologic association with increased costs. The reduction in Medicare spending associated with growth of primary care, particularly in areas with more specialists, is largely explained by family medicine. Implications for Policy, Delivery or Practice: Differences in cost outcomes for general internal medicine and family medicine is beginning to blur the cost savings previously attributed to primary care. The remarkable difference compared to family physicians begs further studies of practice differences. One suggestion is that internal medicine training may lead to practicing to specialty epidemiology and practice patterns rather than those more typical to primary care. Poster Number: 281 Medical Directors’ Evaluation of Physician Workload, Organizational Problems and Organizational Climate in Hospitals: The Results of a Survey of 551 German Hospitals Presented by: Holger Pfaff, Ph.D., Professor, Medical School & Human Sciences Faculty, University of Cologne, Eupener Straße 129, Köln, Germany 50933; Phone: +004922147897100; Email: holger.pfaff@uk-koeln.de Co-authors: Antje Hammer, M.A.; Nicole Ernstmann, Ph.D.; Oliver Ommen, Ph.D.; M.D., M.P.H. Research Objective: To assess, how a hospital’s top management, especially medical directors, see the current state of physician workload, organizational problems and organizational climate in German hospitals. Study Design: In 2008, a cross-sectional representative study was conducted. Among the scales included in the standardized written questionnaire were “physician workload” (6-item scale), “organizational problems” (6-item scale), and “organizational climate” (4-item scale). For each scale, respondents were given four response options, with scores ranging from 1 (do not agree) to 4 (completely agree). Population Studied: 1224 medical directors from all hospitals in Germany with at least one internal medicine and one surgery unit. A total of 551 medical directors filled out the questionnaire, giving a response rate of 45.2%. Principal Findings: The average score on the "physician workload” scale was 19 points (range: 6– 24 points). For example, 90% of the medical directors surveyed agreed with the statement that physicians are required to work at very high speed and are often put under a lot of time pressure. In addition, over 65% felt that physicians' work involves a great deal of physical strain. The average score on the "organizational problems” scale was 13 points (range: 6–23 points). Over 35% of the medical directors agreed with the statement that the patient admission process usually results in organizational problems and the rescheduling of patient check-ups at the hospital. 50% of the medical directors also indicated that hospital checkups often involve long waiting times. Over 20% of those surveyed felt that there are communication problems between the hospital wards and between physicians and nursing staff. The average score on the "organizational climate" scale was 11.3 points (range: 4–16). Over 30% of the medical directors surveyed disagreed with the statement that there is a sense of unity and understanding in the hospital and over 20% disagreed that there is a sense of mutual trust, or a "we" feeling, among employees in the hospital. Furthermore, approximately 19% considered the overall work climate in the hospital to not be good. Conclusions: The results of the survey show that the medical directors see hospital physicians as being subjected to a heavy workload. Additionally, the medical directors surveyed also find hospitals' internal operations to have significant shortcomings, especially with regards to appointment scheduling and waiting times. Nearly one-fifth of those surveyed considered the essential collaboration between individual wards and between physicians and nursing staff to be at an insufficient level. Approximately 20% also found the hospitals’ organizational climate to be deficient. Implications for Policy, Delivery or Practice: The results of this study provide us with an initial assessment of physician workload, organizational problems and organizational climate in hospitals from the eyes of medical directors throughout Germany. Since medical directors are key persons in the health care system, their assessment is highly relevant to policy and practice in hospitals. The results of this survey should therefore be taken seriously. Funding Source(s): German Medical Association Poster Number: 283 Employment Options for Low-Skilled Workers in Baltimore: Workforce Training Issues and Challenges Presented by: Luis Pinet-Peralta, M.Sc., Research Analyst, Health Policy Research Center, Optimal Solutions Group LLC, 5825 University Research Court, Suite 2800, College Park, MD 20737; Phone: (310) 918-5038; Email: lpinet1@umbc.edu Co-authors: Mark Turner, Ph.D.; Christabel Dadzie, M.I.A. Research Objective: The objective was to identify viable occupations for low-skilled workers and offer alternatives in the Baltimore Metropolitan Statistical Area. Study Design: This was a retrospective, descriptive study using Standard Occupational Classification System data from the Bureau of Labor Statistics and Baltimore metropolitan statistical area employment data from the U.S. Census. Using a set of inclusion and exclusion criteria, we performed a 3-stage analysis that included an evaluation of occupational clusters, risk analysis and semi-structured interviews. Occupations were evaluated based on net job openings (availability), education requirements for entry into the occupation (accessibility), income and wage growth (advancement potential) for each occupational cluster. Risk analysis followed the methodology previously used on a national study and focused on outsourcing, technological innovation and industry decline for each occupational cluster. Lastly, a qualitative assessment was performed using semi-structured interviews, which were arranged with 25 of 46 potential key stakeholders, including local leaders, educators and employers, for a response rate of 70%. The interviews were conducted between the months of June and August 2008. Population Studied: Baltimore Metropolitan Statistical Area according to the U.S. Census Bureau Principal Findings: Ten professional occupations, concentrated in six employment clusters were identified, with average earnings of $46,874.00, wage growth of $45,486.00 and 3,029 available positions. Most entry-level occupations require high-school education and offer opportunities for professional development. Employer-based and school-based training is available for all occupations. Soft skills, science, reading and writing can enhance growth opportunities and upward mobility. Conclusions: The occupations identified provide reasonable entry wages and wage growth potential, are accessible and have career advancement options. The emerging green-job industry may also offer viable opportunities, particularly in the construction and utility sectors, with appropriate training programs. Implications for Policy, Delivery or Practice: Policies meant to assist low-skilled workers gain the needed hard and soft skills necessary to secure better work need to address both the technical and the social deficiencies that represent barriers to better employment. Social deficiencies are more difficult to address because of the need for more inter-network collaboration, social participation and political action. The challenge remains to integrate specific local policy interventions with comprehensive workforce reform and, more importantly, evaluate the effects these policies have on labor markets for low-skilled workers in the United States. Funding Source(s): The Ford Foundation Poster Number: 284 Institutional Volume Shifting of Pediatric Surgical Care in North Carolina, 1997-2006 Presented by: Stephanie Poley, B.A., Research Associate, Health Policy Research Institute, American College of Surgeons, 725 MLK Jr. Boulevard, CB # 7590, Chapel Hill, NC 275997590; Phone: (919) 843-7661; Email: stephanie_ poley@unc.edu Co-authors: Daniel von Allmen, M.D.; Thomas Ricketts, Ph.D., M.P.H.; Elizabeth Walker, M.S.P.H. Research Objective: In recent years, concern has intensified regarding the adequacy of the U.S. pediatric surgical workforce. Pediatric surgeons have noted increasing case volume, which may be a result of general surgeons in community hospitals avoiding pediatric cases due to concerns about liability, lack of confidence due to by minimal exposure to pediatric cases during the general surgical residency training, or pressure to take on more “bread and butter” adult cases due to an emerging general surgery workforce shortage. This study examined North Carolina inpatient discharge data between 1997 and 2006 to identify trends in pediatric surgical utilization, to test the hypothesis that pediatric surgical cases are becoming concentrated in that specialty. Study Design: Discharges with one of 934 ICD-9 procedure codes considered general surgery cases, for patients under 19 years old were examined. Records were summarized and analyzed by institution, provider, and county of patient origin. Discharge data were linked to files containing information about institutions and providers using the facility ID and UPIN. Descriptive and multivariate analyses were performed to examine longitudinal trends in the characteristics of patients and type of procedures associated with facilities and providers. Population Studied: Patients under 19 years old presenting at a North Carolina hospital between 1997-2006 requiring a surgical procedure. Principal Findings: Throughout the study period, tertiary care facilities accounted for just over half of the state’s pediatric surgical discharges. Between 1997 and 2006, pediatric surgical case volume increased by 11% overall, with a concentration in the State’s six tertiary care facilities. Surgical discharges for all ages increased by 31% in the same period, with no statistically significant difference in location in tertiary versus community hospitals. Tertiary care facilities experienced an 18% increase in pediatric surgical cases over the ten-year period, while the 109 community hospitals discharged only 5% more pediatric surgical cases in 2006 than in 1997. Appendectomies accounted for nearly one-third of pediatric surgical procedures in community hospitals, while tertiary care facilities had a broader mix of procedures. Eighty-eight percent of procedures in community hospitals were therapeutic, whereas more than 20% of all pediatric surgical procedures in tertiary care facilities were diagnostic. Patients in tertiary care hospitals were younger and the average length of stay and total charges were higher than in community hospitals. Conclusions: Between 1997-2006, pediatric surgical cases became more concentrated in large tertiary care facilities. Implications for Policy, Delivery or Practice: Documenting the changes in pediatric surgical operative volume for facilities and pediatric surgeons is important for workforce and facility planning. Volume shifts observed in this study are unlikely to be isolated to North Carolina. Pediatric surgical residency programs may need to expand training slots to meet future demand for services. Further, general surgery residency programs may need to consider changes in the volume and/or content requirements for pediatric surgical cases during residency in order to prepare new trainees to confidently and appropriately treat pediatric patients. Additionally, significant changes in the volume of pediatric surgical cases seen in tertiary care (training) facilities may have implications for surgical training programs if the trend affects training capacity or quality. Funding Source(s): American College of Surgeons Poster Number: 285 The Impact of Resident Duty Hour Reform on Hospital Readmission Rates Presented by: Matthew Press, M.D., Clinical Scholar, Robert Wood Johnson Foundation Clinical Scholars Program, University of Pennsylvania, 13th Floor, Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104-6021; Phone: (401) 3741928; Email: matthew.press@uphs.upenn.edu Co-authors: Jeffrey Silber, M.D., Ph.D.; Amy Rosen, Ph.D.; Patrick Romano, M.D., M.P.H.; Yanli Wang, M.S.; Kevin Volpp, M.D., Ph.D. Research Objective: A key goal of resident duty hour reform by the Accreditation Council for Graduate Medical Education (ACGME) in 2003 was to improve patient outcomes. Prior research has demonstrated little to no impact of this reform on a variety of outcome measures. The effect on hospital readmission rates, which may have been particularly influenced by disruptions in continuity of care that resulted from the reform, is unknown. The objective of this study was to assess whether resident duty hour reform led to a relative improvement or worsening of readmission rates among Medicare patients in hospitals of different teaching intensity. Study Design: Observational study using difference-in-differences analysis with hospital discharge data from July 1, 2000 to June 30, 2005. Fixed effects logistic regression was used to examine the change in the odds of readmission in more versus less teaching-intensive hospitals before and after the duty hour reform, adjusting for patient comorbidities, age, sex, admission source, common time trends, and hospital. Primary outcomes were 30-day all-cause readmission, allcause readmission or death within 30 days of discharge, and all-cause readmission or death within 30 days of admission. Population Studied: All unique Medicare patients (n=8,282,802) admitted to short-term acute-care nonfederal hospitals with principal diagnoses of acute myocardial infarction, congestive heart failure, gastrointestinal bleeding, stroke or a DRG classification of general, orthopedic, or vascular surgery. Principal Findings: In medical and surgical patients, no significant relative increases or decreases in the odds of readmission were observed in more versus less teaching-intensive hospitals in either the first or second year following the reform. For the combined medical group, postreform year 1 odds ratio (OR) = 0.99, 95% confidence interval (0.94-1.03), and postreform year 2 OR = 0.99 (0.95-1.04). For the combined surgical group, postreform year 1 OR = 1.03 (0.98-1.08) and postreform year 2 OR = 1.02 (0.98-1.07). The findings for the other outcomes—-readmission or death within 30 days of discharge and readmission or death within 30 days of admission—-were qualitatively similar. Our results remained unchanged after the following stability analyses: excluding patients admitted to hospitals in New York State, expanding the inclusion criteria for index admissions, adjusting for patients discharged against medical advice, and removing the adjustments for comorbidity, hospital transfer, and nursing home admission source. Conclusions: Teaching hospital readmission rates neither improved nor worsened in association with ACGME duty hour reform. These findings were robust to the use of composite measures of readmission and mortality and were insensitive to changes in patient selection and alterations in severity adjustment. Implications for Policy, Delivery or Practice: Any potential adverse consequences of resident duty hour reform on continuity of care did not lead to observable changes in readmission rates. This finding adds to the evidence that the reform in 2003 did not generally improve or worsen patient outcomes. Funding Source(s): NHLBI Poster Number: 286 Attitudes Toward Drug-Eluting Stent Use and Distribution of Regulatory Focus Type among Interventional Cardiologists in New York State Presented by: Feng Qian, M.D., M.Sc., Ph.D. candidate in Health Services Research and Policy, Community and Preventive Medicine, University of Rochester, 601 Elmwood Avenue, Box 644, Rochester, NY 14642; Phone: (585) 275-9496; Email: feng_qian@urmc.rochester.edu Co-authors: Charles Phelps, Ph.D., M.B.A.; Frederick Ling, M.D.; Edward Hannan, Ph.D.; Peter Veazie, Ph.D. Research Objective: The safety of drug-eluting stent (DES) use was called into question in 2006. Literature in psychology suggests that regulatory focus type (promotion vs. prevention) orients physicians toward using different strategies to approach a task: ensuring against errors of omission (promotion) vs. ensuring against errors of commission (prevention). However, the attitudes toward DES use after safety concerns were expressed and the distribution of regulatory focus type among interventional cardiologists are unknown. The objectives of this study are: (1) to examine the attitudes toward DES use among interventional cardiologists in New York State (NYS) after DES safety concerns were expressed, and (2) to investigate the distribution of regulatory focus type among these interventional cardiologists. Study Design: We conducted a questionnaire survey of interventional cardiologists in New York State from October 2008 to April 2009 by mail, email and fax. The questionnaire included face valid items to measure the attitudes toward DES use, valid Regulatory Focus Questionnaire to measure the regulatory focus type, and items collecting demographic information. Population Studied: Interventional cardiologists in New York State. Principal Findings: We received total 119 valid returned questionnaires and the response rate was 47%. There are no statistically significant differences regarding the demographic factors between the respondents and the non-respondents. The vast majority of interventional cardiologists (92%) agreed or strongly agreed that DES is a revolutionary technology and that DES use will increase in the future (70%). The regulatory focus type of interventional cardiologists was predominantly of the promotion type (89%). We found that age and gender were significant predictors of the promotion score, but we did not find any demographic factors were significant predictors of the prevention score. Conclusions: Despite the DES safety issues reported in 2006-2007, interventional cardiologists have a very positive attitude regarding DES use and most of them predict the continual growth of DES use in the future. Such information is valuable in predicting the modality change in coronary revascularization therapy. Furthermore, the vast majority of interventional cardiologists were found to be promotion focused, which means that they are concerned about achieving positive outcomes and they want to prevent errors of omission. Implications for Policy, Delivery or Practice: To the best of our knowledge, this is the first study to report the distribution of regulatory focus type among physicians. As suggested by the theory in psychology, this finding can lead to more effective interventions in conveying medical messages to physicians and changing their behavior. Poster Number: 287 A Research Agenda for the Physician Assistant Profession Presented by: Christal Ramos, M.P.H., Data Research Analyst, Data Management and Research, American Academy of Physician Assistants, 950 N. Washington Street, Alexandria, VA 22314; Phone: (703) 836-2272; Email: cramos@aapa.org Co-authors: Sabrina Smith, D.H.A.; Bill Leinweber, M.B.A. Research Objective: To outline a research agenda for the physician assistant (PA) profession. Study Design: The American Academy of Physician Assistants (AAPA) will host a research summit on March 4-5, 2010. Research summit participants will work in groups by topic of expertise to identify and reach consensus on a framework for the research agenda. After the summit, AAPA, its board of directors, and key participants from the research summit will work within the framework developed at the summit to finalize strategies and specific items for the research agenda. AAPA will gain buy-in on the agenda from the three other PA organizations (The National Commission on the Certification of Physician Assistants, the Physician Assistant Education Association, and the Accreditation Review Commission on Education for Physician Assistants). Population Studied: This research summit will bring together representatives from practicing PAs, the PA academic and regulatory communities, PAs engaged in research, health services researchers, health economists, thought-leaders from federal agencies, industry, think tanks, and private foundations that have a demonstrated commitment to health care delivery and health policy research. Principal Findings: AAPA anticipates the research agenda will address: 1. Key questions regarding the PA profession such as: (a) The contributions and impact of the PA profession on health care broadly, on specific health outcomes and on providing care for vulnerable populations (b) The positioning of the profession on the health care delivery team (c) The current and future workforce needs of the profession (d) How the changing health care landscape will impact the profession (e) Utilization, cost and financing issues pertaining to the PA profession. 2. Core strategic, specific, measurable, achievable, realistic and time-specific (SMART) goals. 3. Individual and institutional stakeholders within the PA community and beyond, that have a strong interest in and motivation for advancing and supporting a research agenda for the profession. Conclusions: The research agenda will outline key issues and research strategies to inform the future of the PA profession in American health care. Implications for Policy, Delivery or Practice: In a time where our health care system is in the midst of reform, PAs have the potential to be part of the solution to improve quality, cut costs, to serve an increasingly diverse and aging population, and to fill shortages. As the country seeks to open access to care through the expansion of insurance coverage, the need for health care providers will increase as well. To ensure our nation’s health workforce meet our population’s needs, there must be an organized effort to collect and analyze data to inform workforce policies. The research agenda will serve as the first step towards this type of organized effort for the PA profession. Poster Number: 288 Physician Location Decisions Across States Between 2000 and 2007 Presented by: Charles Roehrig, Ph.D., Vice President, Altarum Institute, 3520 Green Court, Suite 300, Ann Arbor, MI 48105; Phone: (734) 3024646; Email: charles.roehrig@altarum.org Research Objective: There is a growing concern among states about looming physician shortages, both in primary care and selected specialties. This has led to the development of strategies to increase physician supply, including expanding in-state medical school enrollment capacity, increasing instate residency training positions, and taking steps to increase retention of physicians trained within the state. Our research objective is to examine the broad pattern of physician state-level location decisions between 2000 and 2007 and determine the extent to which they are driven by changes in state-level physician demand as opposed to other factors that can be influenced by states. Study Design: We use AMA Masterfile data to determine each state’s share of active physicians by specialty in 2000 and 2007. We estimate each state’s share of physician demand by specialty for these two years using state-level population by age and sex combined with specialty-specific per capita physician demand estimates adjusted for age and sex. We then use regression models to estimate the extent to which changes in a state’s share of the national physician supply are determined by changes in that state’s share of physician demand. We also model the extent to which other factors influence changes in state physician shares. Population Studied: Physicians actively practicing in the U.S. as of December 31, 2000 and December 31, 2007. Principal Findings: Between 2000 and 2007, Texas and Arizona saw the largest gains in their share of physicians, while New York and New Jersey had the largest losses. Our initial regression models use changes in state shares of population, a primary determinant of physician demand, as a substitute for changes in state physician demand. The coefficient on the change in demand shares is .88; thus, the change in supply closely tracks the change in demand. We also find evidence that states with relatively high physician-to-population ratios at the start of the analysis period, and states with older physician populations, tend to have a lower supply share in 2007 than what would be predicted based upon changes in demand. We are currently increasing the precision of our regression results by replacing the change in state population with the change in actual physician demand, and examining the impact of changes in state shares of medical school graduates and residency positions. Conclusions: These findings suggest that the primary determinant of changes in state shares of the national supply of physicians is the change in state shares of demand for physicians. Our results also suggest that states that are richly supplied with physicians are slowly regressing toward the mean, and that states with relatively older physician populations may be lagging in their replacement of those that retire. Implications for Policy, Delivery or Practice: While states may be attempting to influence their share of the national physician pool, physicians move to states where demand for their services is growing. This finding clearly informs state policy decisions regarding the location or expansion of medical schools and residency training positions. Funding Source(s): HRSA Poster Number: 289 Factors Related to the Recruitment and Retention of Primary Care Physicians at Community Health Centers: A Statewide Physician Survey Presented by: Judith Savageau, M.P.H., Epidemiologist/Biostatistician, Center for Health Policy and Research, Univniversity of Massachusetts Medical School, 333 South Avenue, Shrewsbury, MA 01545; Phone: (508) 856-4333; Email: judith.savageau@umassmed.edu Co-authors: Linda Cragin, M.S.; Donna Johnson, L.I.C.S.W.; Joan Pernice, R.N., M.S.; Joan Bohlke, M.S.; Warren Ferguson, M.D. Research Objective: Massachusetts ranks sixth nationally for the number of federally-funded community health centers (CHCs), with 34 located in medically underserved communities. 52 CHCs, including hospital-licensed, provide care at 185+ sites, making CHCs a significant part of the Massachusetts health care system. When Massachusetts implemented universal health insurance coverage in 2006, CHCs were on the primary care frontline. National news reported success in insurance coverage yet highlighted the exacerbation of primary care shortages as many community-based physicians closed their practices. Our objective was to characterize the Massachusetts CHC primary care physician (PCP) workforce and identify factors related to preparedness, recruitment and retention. Study Design: The University of Massachusetts Medical School, Massachusetts League of Community Health Centers (MLCHC), and Massachusetts Department of Public Health developed and implemented an on-line crosssectional survey of PCPs at MLCHC sites. Population Studied: 572 physicians (58% response rate) practicing in 46 CHCs. Principal Findings: CHC PCPs are predominantly female (59%), white (75%), non-Hispanic (88%), work full-time (72%), speak at least one additional non-English language (61%), and have been in practice an average of 13 years. 60% were hired since 2000; 39% practice Family Medicine, 31% Internal Medicine, and 27% Pediatrics. 16% are foreign-trained medical graduates. 22% had postgraduate medical education debt over $100,000 and 9% currently have similar debt. 48% are current or former visa/loan repayment program participants. Our mixed-model regression analyses identifying factors related to the likelihood of PCPs continuing to work in a CHC environment and with underserved populations in the next five years noted that females, those practicing in more urban areas and those in practice for 10+ years were more likely to report plans to remain in a CHC. PCPs who reported being very prepared to practice in this setting at the end of residency training, that the interview process was important, and that the compensation package was not important in their first consideration to join their CHC were also more likely to report remaining in a CHC. Higher levels of satisfaction with their current compensation, however, and increased satisfaction with the CHC’s mission, and the diversity of patients seen were also significantly related to a higher likelihood of remaining in the CHC setting. Finally, a higher likelihood of retention was negatively correlated with opportunities for teaching and research and spousal job assistance. Conclusions: With the nation’s focus on health care reform and results from the reform efforts in Massachusetts and its impact on primary care, our findings provide insights into opportunities to better prepare medical students and residents for careers in CHCs and to recruit and retain this critical workforce. Implications for Policy, Delivery or Practice: For any health care reform effort to succeed, access to a strong and sufficient primary care workforce for underserved populations is needed. PCP compensation is identified as one key strategy; equally important is addressing priorities related to work and personal life that will contribute to the retention of PCPs who plan to remain in a CHC and those currently undecided about their future. Funding Source(s): MassAHEC Network Poster Number: 290 Do Internists and Family Practitioners Have Differing World Views? Variations in the Diagnosis and Management of the Same Patient with Heart Disease Presented by: Rebecca Shackelton, Sc.M., Associate Research Scientist, Health Services and Disparities Research, New England Research Institutes, 9 Galen Street, Watertown, MA 02472; Phone: (617) 972-3119; Email: rshackelton@neriscience.com Co-authors: John McKinlay, Ph.D.; Lisa Marceau, M.P.H.; Carol Link, Ph.D. Research Objective: Variations in the processes and quality of medical care in the U.S have been extensively documented and are a major concern for health services researchers and policy experts. There are documented variations between medical specialties. However, variations within a medical specialty, such as differences between internists and family practitioners within primary care, have received considerably less attention. Internists and family practitioners have been described as having distinct “disease” perspectives with family practitioners having a bio-psychosocial perspective and internists having a patho-physiological perspective of disease. This study aims to answer the following questions: First: are there any differences between internists and family practitioners in their suggested diagnoses and level of diagnostic certainty when encountering exactly the same “patient” with coronary heart disease (CHD)? Second, are there any noteworthy differences in the management of disease between internists and family practitioners? Study Design: In two factorial experiments, primary care providers were shown clinically authentic filmed vignettes with actors portraying “patients” with identical signs and symptoms of CHD. The physician participants were asked how they would diagnose and manage the case. Population Studied: Internists (n=175) and family practitioners (n=192) were randomly sampled from throughout Massachusetts, North Carolina, and South Carolina. Principal Findings: Internists were more certain about the correct diagnosis of CHD than family practitioners and were more likely to act on this diagnosis (order a stress test and prescribe beta blockers). Family practitioners were more likely to diagnose a mental health issue and were more certain about this diagnosis. Conclusions: Clear variations are evident in the way internists and family practitioners would manage the “patient” they encountered. Such variations may reflect fundamental differences in the “disease” model used by the two primary care professional groups (bio-psychosocial vs. pathophysiological). Implications for Policy, Delivery or Practice: The question of training and socialization to a disease model in diagnostic accuracy and certainty is an essential, and often overlooked, element of medical care. Funding Source(s): National Heart, Lung, and Blood Institute Poster Number: 291 Washington State's Oral Health Workforce: Who Provides Services Now and What is Needed for the Future? Presented by: Susan Skillman, M.S., Deputy Director, Center for Health Workforce Studies, University of Washington, 4311 11th Avenue NE, Suite 210, Seattle, WA 98105; Phone: (206)5433557; Email: skillman@u.washington.edu Co-authors: C. Holly Andrilla, M.S.; Joseli AlvesDunkerson, D.D.S., M.P.H., M.B.A.; Wendy Mouradian, M.D., M.S.; Mark Doescher, M.D., M.S.P.H. Research Objective: To describe all components of the oral health workforce in Washington State, the programs by which state residents receive oral health care and preventive services, current and future workforce gaps, and policy options to help ensure an adequate future oral health workforce. Study Design: Using data from surveys, professional licensure records, educational institutions, and a variety of oral health-related organizations and programs in the state, the study provides estimates of the size and distribution of Washington’s oral health workforce; demographic, education and practice characteristics of the workforce; projections of state dental school graduates required to maintain statewide supply to 2027; and discussion of the state’s oral health workforce needs. Population Studied: Providers of oral health care services and oral health improvement programs in Washington State. Principal Findings: There are growing numbers of dentists, dental hygienists, expanded function dental hygienists, dental assistants, denturists, medical providers (physicians, advanced practice nurses and physician assistants), and supporting caregivers who provide oral health services in Washington. There remain, however, underserved populations in much of the state. The size of the workforce appears unlikely to keep pace with state population growth, and some provider types will decline in size as baby boomers retire. Expanding dental school capacity by 25% will contribute to growth of the state's supply of dentists, but not enough to keep pace with the number of dentists needed to maintain Washington’s current dentist:population ratio. Because of projected increases in state population, meeting this benchmark would require having 24% more licensed dentists in Washington in 2027 than were licensed in 2009. Conclusions: More providers will be needed (from in-state educational programs as well as from inmigration) to increase Washington's oral health workforce capacity in the future. There is great need for providers who will care for underserved populations and provide preventive services that will reduce future oral health care demand associated with the growth and aging of Washington’s population. Implications for Policy, Delivery or Practice: Strategies for state health planners, policymakers and educators to improve the distribution and capacity of the oral health workforce include promoting early interest in health careers, improving the capacity of the workforce to care for underserved and special populations, supporting early prevention, supporting collaborative and interprofessional education and practice, and exploring ways to expand the capacity and scope of services provided by oral health care professionals. Funding Source(s): State of Washington Department of Health Poster Number: 292 Projections of Washington State Licensed Practical Nurse Supply and Demand: 2007-2026 Presented by: Susan Skillman, M.S., Deputy Director, Center for Health Workforce Studies, University of Washington, 4311 11th Avenue NE, Suite 210, Seattle, WA 98105; Phone: (206) 5433557; Email: skillman@u.washington.edu Co-authors: C. Holly Andrilla, M.S.; Davis Patterson, Ph.D.; Linda Tieman, R.N., M.N., F.A.C.H.E. Research Objective: This study estimates trends in licensed practical nurse (LPN) supply and demand for Washington State from 2007 through 2026. Study Design: Using available data from state licensing records and a survey of LPNs, the study estimated future in-state LPN graduations, inmigration from other states, re-activation of licensure after license expiration, deaths, agerelated retirements, career changes, and outmigration to other states. Future LPN demand was estimated from state labor department projections. Projections scenarios included estimates of both increases and decreases to the current LPN graduation rates. Population Studied: Licensed and practicing LPNs in Washington State. Principal Findings: The largest single contributor to LPN supply was graduations from in-state education programs. A major factor causing exits from supply was retirement of “baby boomers” from the current workforce. If Washington’s LPN education completion rates increase by 200 LPNs in 2011 (nearly 20% more than the 2007 levels) and this increase is sustained through 2026, the projected supply of practicing LPNs will increase over the next two decades but still be 2,300 LPNs (14%) short of demand in 2026. None of the supply scenarios keep pace with the number of LPNs needed to maintain Washington’s 2008 LPN:population ratio: a benchmark for which increasing numbers of LPNs are needed because of projected increases in state population. Conclusions: Demand for LPNs in Washington will outpace the supply in the state over the next 20 years, even if very large increases to LPN education capacity are implemented. Implications for Policy, Delivery or Practice: Rural locations, including those in Washington, are likely to see greater shortages of LPNs because their populations are older, on average, than urban areas. This growing elderly population has greater need for services, including long-term care, and LPNs are the primary nursing providers in elder care settings. Major changes in health care delivery systems or the economic environment, however, could alter the rate of increase in LPN demand. The registered nurse and LPN workforces are closely related, and growing RN demand may exacerbate the LPN shortage if hiring practices shift to replace RNs with LPNs. LPN education is a critical entry point into the nursing profession, and clear articulation paths between LPN education and other nursing education programs could improve interest in nursing overall. While encouraging LPNs to pursue RN careers may shorten their tenure as LPNs, the potential for professional growth may encourage more people to enter nursing career pathways as LPNs. Funding Source(s): Washington Center for Nursing Poster Number: 293 Hospital RN Job Satisfaction and Nurse Unions Presented by: Joanne Spetz, Ph.D., Professor, Nursing, University of California San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Phone: (415) 502-4443; Email: jojo@thecenter.ucsf.edu Lead Author: Jean Ann Seago, R.N., Ph.D. Co-authors: Michael Ash, Ph.D.; Carolina Herrera, M.A.; Dennis Keane, M.P.H.; Joanne Spetz, Ph.D. Research Objective: Maintaining an adequate nursing workforce has posed an ongoing challenge to policy-makers and hospital managers. While many studies have pursued the determinants of job satisfaction and turnover among hospital-based RNs, none have systematically examined the role of labor unions. Labor unions that represent nurses often argue that their advocacy is central to addressing problems with nurse satisfaction and retention. The broader industrial relations literature suggests unionized workers are more willing to express dissatisfaction and less likely to change employers. This paper addresses this contradiction and considers the role of unions in nurse satisfaction and job seeking in the United States. Study Design: We use data from the 2004 National Sample Survey of Registered Nurses (NSSRN). We limited our sample to RNs who worked in acute care hospitals as their principal nursing environment. We specified nurse satisfaction, jobseeking behavior, and union representation through three NSSRN survey questions. The nursing satisfaction question (“How would you best describe your feelings about your principal nursing position?) offer response options on a five-point Likert scale, while job-seeking and union representation responses were recoded to binary variables. We take three approaches to analyzing the impact of unionization on satisfaction and job seeking. First, we estimate differences in socio-demographic variables by union status and by RN satisfaction, and conduct t-tests and non-parametric tests to determine whether differences are statistically significant. Second, we assess the possibility that unions affect dissatisfaction and job seeking using probit regressions with dichotomized satisfaction (satisfied=1) and job-seeking as the outcome variables. In our third analysis, we examine nursing satisfaction and job seeking in the context of a differentiated attrition model. Differential attrition occurs when job turnover rates differ significantly between two similar cohorts – in this case, between unionized and non-unionized nurses. We stratify those cohorts by age in a probit regression. In all regressions, socio-demographic variables act as controls. Population Studied: United States nurses in 2004. Principal Findings: The population of unionized nurses in the United States in 2004 did not look like the population of non-unionized RNs. Nurses in a union had higher average incomes from their principal nursing positions, worked fewer hours per year and per week, were older, and were more likely to be a minority. They were less likely than non-unionized RNs to be married. They were slightly more likely to report that their highest nursing or nursing-related education was a bachelor’s degree, and less likely to have a graduate degree. RNs reporting higher levels of job satisfaction were more likely to be to be married, female, have higher incomes, and have graduate degrees. T-Testing and non-parametric analysis confirmed a negatively relationship between union status and the distribution of satisfaction. After controlling for other factors in our regression analysis, union representation of all age groups was not a significant predictor of satisfaction. When testing the differentiated attrition model, we find the cohort of older unionized nurses were significantly more likely to be dissatisfied than younger or nonunionized nurses. Preliminary analysis of job seeking suggested it is negatively correlated with unionization; further analysis of job seeking behavior is ongoing. Conclusions: We find evidence that unions are associated with lower nurse satisfaction Implications for Policy, Delivery or Practice: Nurse managers and administrators may find this study useful in that there is no evidence that unions either reconcile nurses to the workplace or foment grumbling. This is in line with expectations about the relationship between unions and satisfaction outside of nursing. Nursing managers may want to note along with intractable demographics such as age and marital status, that lower income and overwork were significantly associated with greater dissatisfaction. This suggests that retention of nurses may devolve to the hospital unit level, where work load, management characteristics, and other environmental factors can be altered by nurse managers. Hospital administrators should evaluate nursing-unit work environments on an individual basis and alter characteristics that dissatisfy their RNs. Funding Source(s): AHRQ Poster Number: 294 Teamwork, Experience and Temporary Registered Nurses Impact on Patient Outcomes and Length of Stay Presented by: Patricia Stone, Ph.D., M.P.H., Professor of Nursing, School of Nursing, Columbia Univeristy, 630 W. 168th Street, New York, NY 10040; Phone: (212) 305-1738; Email: ps2024@columbia.edu Co-authors: Ann Bartel, Ph.D.; Ciaran Phibbs, Ph.D. Research Objective: There is evidence on the importance of registered nurse (RN) staffing in the provision of quality care. However, little evidence exists on the characteristics of the RN needed to provide quality care. To have sufficient staffing some hospitals hire a higher proportion of less experienced and/or temporary RNs (i.e., those from outside agencies). Guided by the theory of human capital, we examined the impact various RN characteristics had on patient outcomes and length of stay (LOS). We chose to measure LOS as it increases with many different adverse events and is a measure of efficiency Study Design: A longitudinal analysis (2003-2006) of administrative data. RN characteristics included the percentage of hours provided by agency nurses, team overlap, unit specific tenure, prior work experience and education. Patient outcomes included the staffing sensitive patient safety indicators (i.e., decubitus ulcer, failure-to-rescue, infections, and post-op deep vein thrombosis) and LOS. All variables were aggregated at the monthly, unit level. Fixed effect, multivariate regressions were conducted for both general and Intensive Care Unit (ICU) settings; we controlled for level of staffing, nursing skillmix (i.e., percentage of RN hours over total nursing hours) and patient severity of illness. Population Studied: Nurses and patients from all Veteran’s Administration (VA) hospitals. Principal Findings: Using 11,637 monthly observations from 266 general wards, the average LOS was 4.9 days (s.d. = 3.7) in general wards and 3.0 days (s.d. = 1.5) in ICUs (7,148 monthly observations from 161 ICUs). On average, in general wards RN unit tenure was 4.0 years (s.d. = 1.3), years of prior experience was 3.4 (s.d. = 1.7) and the percentage of hours of care provided by agency RNs was 2.5 (s.d.= 6.0). In ICUs, RN unit tenure was 5.0 (s.d. = 1.3), years of prior experience was 5.3 (s.d. = 2.3) and the percentage of hours of care provided by agency RNs was 1.6 (s.d. = 5). While some of the RN characteristics were significantly associated with the patient safety outcomes, the results were somewhat inconsistent. We consistently found that lower use of agency nurses, increased length of time RNs have worked on the unit and the larger the overlap of these RNs were all independently associated with decreased LOS in both general wards and ICUs (all p values < 0.05). Conclusions: The characteristics of RNs matter. Implications for Policy, Delivery or Practice: Not only do we need sufficient RNs in the workforce, our findings point to the need for institution specific policies. Hospitals should limit the use of contract nurses and implement strategies to recruit and retain nurses as well as implement exercises designed to encourage RNs to stay with well functioning teams (e.g., team building). A limitation to this study is that it was conducted in VA hospitals; however, because VA RNs have the same credentials and licensing requirements as non-VA nurses and the patient outcomes we are studying are important for all hospitalized patients, it is unlikely that the results would change in non-VA hospitals. Nevertheless, more research is warranted. Funding Source(s): RWJF Poster Number: 295 The Effect of Medical Malpractice Liability on Access to Care Presented by: Daniel Weinberg, Ph.D., Research Associated, IMPAQ International, LLC, 10420 Little Patuxent Parkway, Suite 300, Columbia, MD 21044; Phone: (443) 539-9765; Email: dweinberg@impaqint.com Research Objective: The purpose of this paper is to estimate the effect of medical malpractice liability on access to care measures such as ED utilization, putting off care, having a usual source of care, having unmet health care needs, and others. A primary way in which liability may diminish access is through reductions in provider workforce in highliability markets. Study Design: I employ individual level access to care data from four rounds of the Community Tracking Study (CTS) along with metropolitan statistical area liability measures (a panel at the metro level) to estimate the effect of malpractice liability on access to care. I use a fixed-effects model with a rich set of individual-level covariates to control for metropolitan area unobservables and micro-level factors affecting access. Population Studied: Individuals aged 18-64 living in 47 metropolitan statistical areas in 34 states. National estimates were obtained using the appropriate weighting variables provided by the CTS. Principal Findings: Uninsured individuals experience diminished access to care for some access to care measures (ED utilization, preventive care, mammography, putting off needed care, and travel time) but not for others (flu shot, unmet medical care needs, having a usual source of care, and number of visits with a health care provider). Access measures tend to be more sensitive to the size of medical malpractice claims payments than to the frequency per physician of such payments. Possible explanations for diminished access resulting from liability include reductions in physician workforce and changes in physician behavior such as rejecting high-risk patients, refusing to perform high-risk procedures, and focusing on high-profit patients whose insurers are relatively generous payers. The evidence from this paper suggests that changes in physician supply are not the primary cause of the effect of liability on access. Medicaid patients’ access measures are much less sensitive to changes in malpractice liability. Implications for Policy, Delivery or Practice: Policymakers whose goals include expanding access to care among the uninsured (by, for example, reducing unnecessary ED utilization and increasing preventive care) might consider expanding Medicaid since Medicaid patients’ access measures appear to be less sensitive to changes in malpractice liability. Also, reducing the size of malpractice settlement payments will likely improve access among the uninsured. Caps on noneconomic damage awards may help to accomplish this goal. Poster Number: 296 Certified Nurse Midwives, Nurse Practitioners and Physician Assistants as Abortion Providers: Preliminary Findings from the California Primary Care Initiative Presented by: Tracy Weitz, Ph.D., M.P.A., Associate Professor, ANSIRH, University of California, San Francisco, 1330 Broadway, Suite 1100, Oakland, CA 94612; Phone: (510) 986-8939; Email: weitzt@obgyn.ucsf.edu Lead Author: Diana Taylor, R.N., Ph.D., N.P.; Co-authors: Kristin Nobel, M.P.H.; Molly Battistelli, B.A.; Erin Schultz, J.D.; Tracy Weitz, Ph.D., M.P.A. Research Objective: Early abortion is one of the safest medical procedures, with an average complication rate between 1-5%. The 1.2 million abortion procedures performed in the United States annually are provided by only 178 facilities. Consequently, many women have to travel long distances to access abortion care, resulting in unintended births and abortions at later gestational age. Solutions to this access problem include appropriate training and development of the workforce. Advancing New Standards in Reproductive Health (ANSIRH) initiated a Health Workforce Pilot Project in California in 2007 to train and evaluate whether certified nurse midwives (CNM), nurse practitioners (NP) and physician assistants (PA) as early aspiration abortion providers can help fill the workforce gap. This presentation reports selected findings from data gathered from August 2007 to December 2009. Study Design: This is a multi-site prospective evaluation of CNMs, NPs and PAs trained to competency in early aspiration abortion procedures and followed over time. CNM/PA/NP data are compared with published standards. Data are collected on patient outcomes (safety, satisfaction, access to care) and clinician outcomes (competency, satisfaction) across the peri-abortion care continuum. Population Studied: Women seeking first trimester aspiration abortion in 14 clinical location in California. Principal Findings: Preliminary results from 23 CNMs, NPs and PAs and 2,685 patient procedures indicate that the average rate to date of abortionrelated complications (primarily incomplete abortion, hematometra, mild infection) for CNMs, NPs and PAs is 1.5%. Using an extensive postabortion follow-up protocol, no major complications among CNM/NP/PA patients have been reported, and all minor complications have been resolved without further problems. Patients report a high satisfaction rate of 9.4 (scale 0-10). Conclusions: California CNMs, NPs and PAs provide all aspects of early pregnancy care with the exception of aspiration abortion. Preliminary evidence demonstrates that post-abortion problems can be treated promptly and hospital visits avoided when more abortion-providing clinicians are available. Patients report high satisfaction with the care they receive from CNMs, NPs and PAs. Additional benefits to patients of incorporating aspiration abortion care into CNM/NP/PA practice include: increased continuity of care; ability to receive follow-up care or treatment of com¬plications quickly at local clinics; and reduced stigma by accessing abortion services in primary care and family planning settings. Implications for Policy, Delivery or Practice: Substantial data on abortion provision by CNMs, NPs and PAs are essential to improving patient access to abortion care and to translating evidence into policy, professional education, and clinical practice. Funding Source(s): Private Foundations Poster Number: 297 Tracking the Growth of Hospitalist Medicine in Ontario: Trends in Inpatient Physician Specialty and Continuity-of-Care from 1996 to 2009 Presented by: Heather White, M.Sc., Ph.D. Candidate, Health Policy, Management and Evaluation, University of Toronto, 169 Street George Street, Apartment 506, Toronto, Canada M5R 2M4; Phone: (647) 439-0271; Email: heatherlynn.white@utoronto.ca Co-authors: Dr. Richard Glazier, M.D., M.P.H. Research Objective: Providing high quality, costeffective services within the acute-care setting is becoming increasingly complex and hospitals are seeking to adapt by exploring new delivery models, including the use of hospitalists, which may allow them to improve quality of care while remaining financially sustainable. Defined as physicians specializing in the general medical care of hospitalized patients, hospitalists have emerged as the fastest growing medical specialty in North America with more than 28,000 practitioners and 2,300 programs currently operating across Canada and the United States. Under this discipline, unattached patients and patients whose GP/FPs do not provide inpatient services are transferred to the care of a hospitalist upon admission. Acting as case-manager, the hospitalist’s primary role is to co-ordinate the care of all assigned patients and facilitate their access to post-acute services. Upon discharge, patients are returned to the community and into the care of their GP/FP - if they have one. Although hospitalist medicine has become the dominant model for inpatient care in many Canadian hospitals, data characterizing the prevalence of hospitalists or their influence on inpatient specialty volume and continuity-of-care has not been explored in the Canadian literature to date. This study aims to describe the growth of hospitalist medicine within Ontario hospitals, viewed alongside contemporary changes in inpatient physician specialty and continuity-of-care from 1996 to 2009. Study Design: Using retrospective times-series, this analysis draws on hospitalization abstracts and physician billing claims to examine temporal patterns in inpatient specialty and continuity-of-care for non-elective adult admissions to acute-care hospitals in Ontario from April 1, 1996 to March 31, 2009. Annual service volume and location were extracted from the Ontario Health Insurance Plan database to derive prevalence estimates of hospitalists, GP/FPs, internists and subspecialists providing inpatient services within Ontario hospitals. Clinical information from the Discharge Abstract Database were then linked to billing claims to assess continuity-of-care and hospitalist penetration according to hospital type, size and geographic location. Outcomes were entered into separate univariate regression models, accounting for autocorrelation with a lag set to one. Population Studied: All non-elective, nonobstetrical admissions to Ontario hospitals for adults aged 18 and older from April 1, 1996 to March 31, 2009. Principal Findings: Analyses are currently underway; however results will be available for presentation and discussion in June. Implications for Policy, Delivery or Practice: This study will provide the first descriptive assessment of hospitalist prevalence and penetration within Ontario Hospitals, presented alongside contextual analyses describing overall trends in inpatient service delivery and continuity-ofcare since its inception. This analysis will aid in defining inpatient volume cut-points for identifying hospitalist providers within administrative databases; a necessary first step for future work aimed at evaluating and monitoring hospitalist performance. As hospital CEOs, policy analysts and government agencies continue to explore the viability of these models for improving inpatient care for Canadians, quantitative evidence supporting their penetration and value needs to enter into the policy agenda. Funding Source(s): Canadian Institutes of Health Research Poster Number: 298 The Effects of Data Aggregation on the Link Between Primary Care Workforce and Health Care Utilization Rates Presented by: Brad Wright, M.S., Doctoral Student, Health Policy and Management, University of North Carolina Chapel Hill, 1300 Laurel Springs Drive, Apartment 1301, Durham, NC 27713; Phone: (202) 465-4815; Email: bradwright@unc.edu Co-authors: Thomas Ricketts, III, Ph.D., M.P.H. Research Objective: Most health care workforce studies do not account for data aggregation effects that can significantly affect the direction and magnitude of findings. Building on a 2008 study by Kravet and colleagues (Am J of Med (2008)121: 142-148), which found a higher proportion of primary care physicians to be associated with a decrease in per capita rates of inpatient admissions, emergency room visits, and total surgeries, we sought to re-examine these associations within both metropolitan statistical areas (MSAs) and the counties that compose them to investigate the potential impact of geographic data aggregation on the findings. Study Design: We estimated four distinct crosssectional multivariate regression models to predict health care utilization rates at the county level and the metropolitan statistical area (MSA) level using Area Resource File data from 2007. Our study focused on health care utilization in the United States using inpatient admissions, hospital-based outpatient visits, emergency room visits, and total (inpatient and outpatient) surgeries as dependent variables in separate regressions. These outcomes were selected because we felt that appropriate primary care use would reduce their incidence. The key independent variable was the proportion of primary care physicians out of all active, officebased, non-federal physicians in the area engaged in direct patient care. Controls for regional differences in physician practice patterns were included along with several community-level controls (e.g., physician and population density, percent over age 65, percent female, percent African-American, per capita income, per capita hospital bed supply, and per capita death rate.) Population Studied: We studied county-level and MSA-level relationships between the proportion of primary care physicians in an area and the population’s utilization of health care in that area. For the purposes of this analysis, non-MSA counties were excluded. Principal Findings: We found that a higher proportion of primary care physicians in the area’s physician supply was associated with a decreased number of inpatient admissions at the MSA level, but not the county level, and a decreased number of emergency room visits at the county level, but not the MSA level. Outpatient visits and total surgeries were not associated with the proportion of primary care physicians. Conclusions: There is some evidence that a higher proportion of primary care physicians is associated with a decrease in health care utilization, but these findings depend on the level of aggregation. Implications for Policy, Delivery or Practice: Primary care physicians may help to control health care costs by encouraging more appropriate service use and preventing persons from developing more serious health conditions that require use of more resource-intensive health care services. Further studies are warranted and investigators should be aware of the implications that aggregating data may have on their results, and acknowledge any resultant limitations. Funding Source(s): AHRQ, This research was partially supported by a National Service Research Award Pre-Doctoral Traineeship from the Agency for Health Care Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at C Poster Number: 299 Maintenance of Certification: The Case of Family Medicine Presented by: Imam Xierali, Ph.D., Research Scientist, Robert Graham Center, American Academy of Family Physicians, 1350 Connecticut Avenue Suite 201, Washington, DC 20036; Phone: (202) 331-3360; Email: ixierali@aafp.org Co-authors: Jason Rinaldo, Ph.D.; Andrew Bazemore, M.D.; Bob Phillips, M.D.; Stephen Petterson, Ph.D. Research Objective: Although medical licensure is a state requirement, specialty certification in the U.S. remains a voluntary process. This study tests hypotheses regarding family physicians in direct patient care whose board certification had expired. Study Design: We merged multi-year American Board of Family Medicine Maintenance of Certification (MOC) data with 2009 American Medical Association Master File data, and U.S. census data. We then completed cross-sectional spatial, descriptive, and logistic regression analyses comparing family physicians who are versus who are not maintaining their board certification. Population Studied: Direct patient care family physicians whose board certification expired by the end of 2008 Principal Findings: At the end of 2008, there were 10,759 direct patient care family physicians whose ABFM board certification expired. Physicians younger than 65 years of age whose certification expired were more likely to be male (76.52% vs.62.63%, p<.0001), more likely to be older (p < .0001), more likely working in areas of dense poverty (53.83% vs.47.75%, p < .0001), in Health Professional Shortage Areas (26.17% vs.21.16%, p < .0001), in rural areas (19.95% vs. 19.56%, p <.0001), in Medically Underserved Areas (25.67% vs.21.55%, p < .0001), in Primary Care Service Areas with fewer physicians (5.12% vs.4.12%, p < 0.05). Board certification maintenance is also significantly associated with physician practice type, IMG status, and employment type. Conclusions: Although about 87% of direct patient care family physicians in the United States had maintained their board certification, there were still a substantial number of direct patient care family physicians whose certificate had lapsed by the end of 2008. The study found that family physicians located in poorer and underserved areas would be less likely to have maintained board certification. Implications for Policy, Delivery or Practice: Although the causal relationship between practicing in underserved areas and tendency to lapse board certification is not well established in this analysis, the significant association between them begs for more research into this issue. Also the effect of employment type of physicians show significant association with the likelihood to lapse board certification, indicating policy actions may be needed to reach out to physicians in certain employment setting, especially those in solo practices. Poster Number: 300 Quality Outcomes of Hospital Supplemental Nurse Staffing Presented by: Ying Xue, D.N.Sc., Assistant Professor, School of Nursing, University of Rochester, 601 Elmwood Avenue Box SON, Rochester, NY 14642; Phone: (585) 276-3136; Email: ying_xue@urmc.rochester.edu Co-authors: Linda Aiken, Ph.D.; Deborah Freund, Ph.D.; Katia Noyes, Ph.D. Research Objective: Many hospitals use supplemental nurses (SRNs) hired from agencies to compensate for their shortage of nurses. As the nursing shortage continues, the demand for SRNs may persist or even increase, but little is known about the use and impact of such staff. This study was designed to better determine how one hospital used SRNs and to examine the impact of SRNs on patient and nurse outcomes. Study Design: A retrospective study was conducted using hospital administrative data between 2003 and 2006. Data were collected on discharge patient demographics, primary insurance, principal diagnosis, six secondary diagnosis, nurse staffing characteristics, nursing work environment, and patient and nurse outcomes. Primary patient outcomes included patient satisfaction, patient satisfaction with nurses, inpatient mortality, falls, pressure ulcers, and medication errors. The primary nurse outcome was nurse voluntary turnover. Use of SRNs was defined as the proportion of total nursing hours provided by SRNs. The unit of analysis is unit quarter. Multilevel modeling was employed to model longitudinal effects. False discovery rate was used to adjust multiple procedure comparison and control for type I error. Population Studied: Discharge patient records from 19 adult medical, surgical, and intensive care units in a large urban teaching hospital in the upstate New York during year 2003 and 2006. Principal Findings: The hospital had used SRNs over time with a decreasing trend. Use of SRNs varied widely by units. Of 19 units, 18 units had used SRNs some time during year 2003 to 2006. Use of SRNs ranged from 0.16% to 20.02% of total nursing hours per unit quarter. Units that relied more on SRNs had worse nursing work environments. Higher use of SRNs was associated with lower patient satisfaction and higher RN turnover when only adjusted for patient and nurse staffing characteristics. After controlling nursing work environment, however, use of SRNs didn’t have any negative impact on patient & nurse outcomes. Conclusions: Theses results suggested that heavy use of SRNs might be an indicator of a poor nursing work environment that other literature has linked to poor patient and nurse outcomes. Implications for Policy, Delivery or Practice: Improving working environments could improve patient and nurse outcomes. Future study is needed to further explore the relationship between patterns of using SRNs and nursing work environment. Funding Source(s): RWJF Poster Number: 301 National Trends of Supplemental Nurses’ Characteristics from 1984 to 2004 Presented by: Ying Xue, D.N.Sc., Assistant Professor, School of Nursing, University of Rochester, 601 Elmwood Avenue Box SON, Rochester, NY 14642; Phone: (585) 276-3136; Email: ying_xue@urmc.rochester.edu Co-authors: Joyce Smith, M.S.; Deborah Freund, Ph.D.; Linda Aiken, Ph.D. Research Objective: Use of supplemental nurses (SRNs) as a strategy to address nurse shortages is a long-standing practice. The purposes of this study were to describe patterns of SRNs’ demographics, nursing educational preparation, and nursing work experience; and examine whether these characteristics are different from those of nurses with a permanent position (PRNs). Study Design: A time series cross-sectional analysis of the National Sample Survey of Registered Nurses 1984-2004 was employed. Population Studied: SRNs were defined as nurses who were working in their principal or secondary nursing position in a supplemental role at the time of survey. PRNs were defined as nurses who were working as a facility employee in their principal position with exclusion of those who had secondary positions as SRNs. Principal Findings: SRNs accounted for 3%-5% of RN population during 1988 to 2004. SRNs and PRNs were different in demographics. The proportion of nurses who were older than 40 increased from 41% in 1984 to 58% in 2004 in the SRN group, and from 51% in 1992 to 72% in 2004 in the PRN group. The proportion of nurses who were male increased from 6% in 1984 to 11% in 2004 in the SRN group, and from 4% in 1992 to 6% in 2004 in the PRN group. The proportion of nurses with non-white racial background increased from 15% in 1984 to 21% in 2004 in the SRN group, and from 8% in 1992 to 11% in 2004 in the PRN group. Non-currently married status was about 42-47% in the SRN group, and about 27% in the PRN group over time. SRNs were more likely to receive initial RN education in a foreign country (4% in 1988 to 6% in 2004) than PRNs (about 3% over time). Trend of nurses who had Baccalaureate degree or higher were similar in both groups, it increased from 35% in 1984 to 47% in 2004 in the SRN group, and from 39% in 1992 to 49% in 2004 in the PRN group. Nursing work experience was defined as years since received highest nursing or nursing related degree. SRNs had fewer years of experience (about 13 years in both 2000 and 2004) than PRNs (15 years in 2000 and 16 years in 2004). Conclusions: SRNs are different from PRNs in demographic characteristics. SRNs are characterized by a higher percentage of nurses who are younger, male, non-White, not currently married, and received a basic nursing education in a foreign country. SRNs are equally qualified for work as PRNs in terms of level of nursing educational preparation. Implications for Policy, Delivery or Practice: SRNs are a more very diverse group than PRNs. As the population needing health care in the U.S. becomes more diverse there is urgency to bring more diversity to the PRN population. Future research is needed to explore why some nurses are more likely to work as a SRN and based on further understanding of the SRN population, strategies may be developed to attract these nurses to a permanent position. Funding Source(s): RWJF Poster Number: 302 Physician Perspectives on Electronic Prescribing Using a Locally Developed Versus Commercial Electronic Health Record Presented by: Erika Abramson, M.S., M.S., Assistant Professor, Pediatrics, Weill Cornell Medical College, 402 E. 67th Street, New York, NY 10065; Phone: (646) 962-8058; Email: err9009@med.cornell.edu Co-authors: Vaishali Patel, Ph.D., M.P.H.; Sameer Malhotra, M.D., M.A.; Elizabeth Reynolds, B.A.; S. Nena Osorio, M.D.; Rainu Kaushal, M.D., M.P.H. Research Objective: Federal incentives to adopt interoperable, certified electronic health records (EHRs) with electronic prescribing (e-prescribing) are motivating organizations previously using locally developed systems to transition to commercially developed EHRs. Understanding physicians’ perspectives on the transition and experiences with e-prescribing on these different systems can improve the design and implementation of commercial EHRs. We use the term e-prescribing to describe electronic ordering of medications, regardless of whether prescriptions were printed or electronically transmitted to a pharmacy. Study Design: We conducted a mixed methods study consisting of a closed-ended survey, field observations of prescribing using a new commercial system, and semi-structured interviews with physicians at an academic ambulatory care office practice from January through November 2009. Using these complementary approaches allowed us to develop a rich description of a small group of experienced users. Data collection began nine months after the transition. We analyzed survey data using descriptive statistics and analyzed field notes of observations and transcripts of semistructured interviews using qualitative methods guided by a grounded theory approach. Population Studied: We studied internal medicine faculty (n=19) at an academic-affiliated ambulatory care office practice. Use of the commercial system was mandatory. The information systems (I.S.) team conducted a large-scale, intensive effort to transition physicians from a longstanding locally developed system that had been in place for 15 years to a new commercial system, as well as to transfer and integrate medication data from multiple additional sources. Principal Findings: We identified key themes describing physician experiences transitioning from a locally developed to a commercial EHR and perceptions about the advantages and disadvantages of prescribing with each type of system. Overall, we found that even experienced eprescribers considered the transition difficult. Most physicians did not perceive the commercial system as improving safety, despite having more advanced clinical decision support (CDS). Many physicians were concerned about the potential of CDS to contribute to errors, particularly amongst trainees. Additionally, physicians felt the commercial system was too complex, reducing their efficiency. Conclusions: In spite of the intensive training and effort by I.S. to provide a smooth transition between systems, physicians perceived a negative impact on their productivity. Physicians’ attitudes towards eprescribing using commercial systems appear strongly related to perceived effects on workflow. Designing systems that make prescribing efficient and limiting alerts to those that are clinically relevant may reduce physician resistance to switching to commercial EHRs. Ironically, sophisticated commercial interfaces may need to be simplified to best fit physician workflow. Longitudinal studies should be conducted to examine how physician perspectives evolve over time as physicians become more familiar with new systems and iterative refinements are made. Implications for Policy, Delivery or Practice: Given national focus on increasing the usage of ambulatory interoperable EHRs with e-prescribing, our findings have important implications for the design and widescale implementation of commercial systems. This is amongst the first mixed-method studies to examine physician experiences transitioning between a locally developed EHR with e-prescribing and a commercial one and provides insight on physician preferences for prescribing applications. Developing technical standards to ensure interoperability will also be critically important given the challenges in transferring medication data between systems. Funding Source(s): AHRQ Poster Number: 307 Impact of Information Sharing Through Electric Medical Network Between Pharmacist and Physician on Patient Care in Japan Presented by: Miki Akiyama, Ph.D., Associate professor, Faculty of policy management, Keio University, 5322 Endo Fujisawa, Kanagawa, Japan 2520882; Phone: +81466493448; Email: miki@sfc.keio.ac.jp Co-authors: Takebayashi, Toru, M.D., M.P.H., Ph.D.; Hirai, Aizan, M.D., Ph.D. Research Objective: This study aims to explore influences and effects of use of regional medical information communication network upon doctors and pharmacists communication and their patients’ medication adherence, by conducting clinical epidemiology study of osteoporosis patients and an interview survey with their pharmacists in Sanbu district in Chiba prefecture of Japan where the electronic medical information networking system was implemented in. We conducted cohort study to examined medical adherence of osteoporosis patients in Sanbu district in Chiba prefecture in Japan. The system can be characterized as asynchronous media and store-and-forward techniques liberating users from temporal constraints. Study Design: Triangulation of retrospective cohort study, questionnaire survey and semi-structured interview was carried out. In the cohort study, efficacy of information network use on osteoporosis treatment was evaluated by comparing changes in urinary cross-linked N-telopeptides of type I collagen (NTX), turnover marker of bone, over the study period between patients on the information network and those without the network. A follow-up questionnaire survey was also conducted. In addition, semi-structured interviews with all pharmacists using the network were carried out and transcribed to explore how they perceive the effects of the network. NTX data was compared by MannWhitney U-test, and questionnaire survey data was analyzed by chi-square or Fisher’s exact method. Qualitative data was collected and analyzed according to a modified Grounded Theory approach. Population Studied: The cohort was consisted of 297 female osteoporosis patients in a regional core hospital. Of those, 179 were patients whose records were on the network and 118 were those without the network. There was no difference between the age distributions between two groups (with-network and without-network); 3% /3% for under 40, 40%/41% for 40-64) 58%/56% for over 65. We sent questionnaires to 230 out of 297, who were eligible for questionnaire survey and 136 (82/54) responded (response rate=59.1%). In addition, 21 pharmacists (male 13, female 8) who were using the information network were interviewed. Principal Findings: The born turnover marker NTX was significantly improved among the patients on the network compared to those without network as the medication period got longer. Among patients whose medication period was over 270 days, improvement rate of NTX from baseline was significantly higher (P=0.02) in the network group (69.7%) compared to that of non-network group (48.2%). Patients’ survey indicated that the use of the network enabled better communication, mutual understandings and trusts between pharmacists and patients. Interview data obtained from 21 pharmacists indicated that the network enabled pharmacists to understand physicians’ intentions more clearly and consequently, brings pharmacists well-grounded decisions, effective learning, and motivation as a medical professional. Conclusions: Triangulation of the results obtained from the studies revealed that the medical information network improved patients’ medication adherence. The interviews with pharmacists and the patients’ questionnaire survey explained how the information network ensured better communication between doctors, pharmacists and patients, which lead to better compliance based on mutual understandings and trusts between pharmacists and patients. Implications for Policy, Delivery or Practice: Regional medical information communication network can contribute to good communications between doctors, pharmacists and patients, which would result in good medical practice especially in chronic diseases. Funding Source(s): partly funded by Pfizer Health Research Foundation Japan Poster Number: 308 Impact of Health Information Technology Portfolio on Hospital Quality: A National Study of U.S. Acute Care Facilities Presented by: Ajit Appari, Ph.D., Research Fellow, Center For Digital Strateties, Dartmouth College, 100 Tuck Hall, Hanover, NH 03755; Phone: (603) 646-9017; Email: Ajit.Appari@Tuck.Dartmouth.Edu Co-authors: Denise Anthony, Ph.D.; M. Eric Johnson, Ph.D. Research Objective: This study empirically examines the impact of a portfolio of health information technologies, compared to individual applications, on quality in acute care hospitals. Study Design: We analyze data from the 2006 annual survey of health information technologies (HIT) conducted by Dorenfest Institute-HIMSS Analytics and hospital quality performance data from the 2006 CMS Hospital Compare database. We consider the impact on quality of care of adopting a portfolio of six clinical health IT applications in U.S. acute care hospitals: clinical data repository (CDR), clinical decision support (CDS), computerized physician order entry (CPOE), order entry with communications (OEC), enterprise electronic medical records (EMR), and electronic medication administration record (EMAR) systems. Hospital quality is measured using the eight CMS benchmark care indicators for acute myocardial infarction (AMI). Each AMI quality measure is regressed on the individual HIT applications, and on overall HIT portfolio (controlling for bed size, profit status, academic status, and affiliation with integrated health delivery system). Since the quality measures are bounded within the interval [0,1], we use a generalized linear model (GLM) regression with the logistic function as linking function. To account for potential spatial correlation of errors, we use state-level error clustering. Our approach examines the effect of overall HIT portfolio compared to prior studies examining the relationship between individual HIT applications and quality. Population Studied: 2,624 non-federal acute care hospitals with at least 100 beds. Principal Findings: In our sample, the average HIT portfolio is 3.4 applications (range 0-6). We find limited evidence of an association between individual HIT applications and AMI quality measures. For example, CPOE and EMAR have a positive impact on two of the six medication-based AMI indicators. In analysis of overall HIT portfolio, we find a positive association between size of HIT portfolio and quality. Particularly, hospitals with a larger HIT portfolio are more likely to give patients smoking cessation advice (p-value: 1%), administer aspirin at discharge (p-value: 5%), give PCI intervention within two hours of arrival, (p-value: 5%) and administer beta blocker at arrivals (pvalue: 10%). However, there was no significant relationship between HIT portfolio and the remaining four AMI quality measures. Our findings suggest that the effects of HIT use should not be viewed by individual applications; instead a portfolio view may enable greater quality improvement. Conclusions: We assessed the impact of overall HIT portfolio on the quality of AMI care provided in U.S. hospitals and found statistically significant effects that hospitals with larger HIT portfolios have better process quality measures. Implications for Policy, Delivery or Practice: HIT adoption has become a priority for U.S. policymakers, especially in light of the increasing focus on healthcare cost and quality. Our findings suggest that adoption of a portfolio of key clinical technologies does have a positive impact on quality of care. Developing appropriate policy measures and incentives to enhance the wide-spread diffusion of healthcare technologies, particularly CDR, CDS, CPOE, EMR, and EMAR systems will be critical to realize ulterior goals of improving care quality for all Americans. Poster Number: 309 Physicians’ Eligibility for Medicare and Medicaid EHR Incentives and Current Use Presented by: Brian Bruen, M.S., Lead Research Scientist, Dept. of Health Policy, George Washington University, 2021 K Street NW, Suite 800, Washington, DC 20006; Phone: (202) 9944125; Email: brian.bruen@gwumc.edu Co-authors: Leighton Ku, Ph.D., M.P.H.; Peter Shin, Ph.D., M.P.H.; Patricia MacTaggart, M.B.A., MMA; Sara Rosenbaum, JD; , Research Objective: Under the American Recovery and Reinvestment Act (ARRA), physicians will be eligible for incentive payments to adopt, improve and maintain electronic health records (EHRs). Medicare and Medicaid incentives are available to those who attain “meaningful use.” Medicare physicians who do not use an electronic health record (EHR) system would eventually be penalized through payment reductions. This study estimates the number and characteristics of physicians eligible for Medicare or Medicaid incentives and compares this to their current use of EHRs. Study Design: We analyzed the National Ambulatory Medical Care Survey (NAMCS), which provides data on a nationally representative sample of office-based physicians, including a sample of ambulatory visits and description of physicians’ EHR use. Any physician billing Medicare is eligible for Medicare incentives, while Medicaid incentives require a minimum level of Medicaid volume. A physician must choose whether to receive Medicaid or Medicare incentives; both cannot be received. Since Medicaid incentives tend to be larger, we assume those eligible for both would tend to take the Medicaid payments. Population Studied: Practicing non-federal, officebased physicians Principal Findings: Based on preliminary analyses of the 2007 NAMCS, approximately 257,000 of the nation’s 320,000 physicians (or 80%) could qualify for HIT incentives through either Medicare or Medicaid. Of those physicians who could qualify, about 47,000 physicians (18%) reported having “comprehensive” EHRs already. Another 15% of qualifying physicians have “partial” EHRs and the remaining two-thirds (67%) have no EHRs. Pediatricians, OB/Gyns and psychiatrists were less likely to be eligible for incentives. (Note: "partial" and "comprehensive" do not necessarily correspond to "meaningful use" of EHRs.) Conclusions: Nearly 80% of practicing officebased physicians could be eligible for ARRA incentives. Most did not have comprehensive EHRs as of 2007, so the incentives could spur substantial adoption or improvement of EHR systems. Eligibility for incentive payments does not necessarily mean those physicians will adopt EHRs; that will also depend on factors such as the total cost of EHR systems, perceived difficulty of attaining meaningful use and other factors. Implications for Policy, Delivery or Practice: The ARRA incentives could encourage most officebased physicians to adopt or upgrade EHR systems, which may ultimately improve the quality and cost-effectiveness of care. However, the 20% of physicians who would not be eligible for incentives may represent a special policy challenge to attaining universal deployment of EHRs. Funding Source(s): To Be Determined Poster Number: 310 Assessing the Value of the Veterans' Health Administration Investments in Health Information Technology Presented by: Colene Byrne, Ph.D., Senior Analyst, Center for IT Leadership, Partners Healthcare, One Constitution Center, Charlestown, MA 02119; Phone: (617) 643-4157; Email: cbyrne1@partners.org Co-authors: Blackford Middleton, M.D., M.P.H., M.Sc.; Douglas Johnston, M.T.S; Eric Pan, M.D., M.Sc.; Adam Vincent, M.P.P; Lauren Mercincavage, M.H.S. Research Objective: To assess the value of the Veterans' Health Administration (VHA) investment in the Veterans Health Information Systems and Technology Architecture (VistA) using two complementary methods: benchmarking the VHA against industry norms and modeling the costs and benefits of selected VistA applications/components. Study Design: Two analytic methods were used: 1) comparing the VHA against industry norms on IT spending, adoption, and IT-related quality benchmarks; and 2) stochastic simulation modeling of the monetized costs and benefits of four selected VistA applications/components. Sources of VistA value were categorized: workload reductions; freed space; eliminated redundancy; avoided utilization; and decreased expenses (e.g., supplies, contracted services). Population Studied: The national VHA healthcare system and selected VistA applications were studied - Bar Coding Medication Administration; Computerized Patient Record System (CPRS) including order entry and results reporting; Picture Archiving and Communication System (PACS); and Laboratory Electronic Data Exchange. Principal Findings: Benchmarking: While the VHA historically has spent a higher proportion of its budget on IT, it has achieved a very high level of HIT adoption when compared to industry norms, using several adoption frameworks. The VHA greatly exceeds industry norms in outpatient EHR/EMR adoption and in selected outpatient quality measures that are reflective of the use of automated clinical reminders. Modeling Due to the lack of systematic tracking of costs and benefits of the VistA applications, retrospective, high-level estimates of annual and cumulative costs and benefits were calculated. The total monetized benefit of the 4 selected VistA applications - all first implemented between 1997 and 2001 - was estimated to exceed total costs around 2003. At the end of the evaluation period, when VA had reached full adoption of all the applications studied, the estimated annual net benefit was conservatively estimated at $690 million per year, with a total cumulative estimated benefit during the study period of $3.1 billion. Conclusions: The findings suggest that the VHA investment in IT is associated with increased healthcare value through healthcare cost savings, efficiencies, and improved quality of care from the VistA applications. The VHA spent approximately 1% more than the private sector on IT as a percent of its total budget. This investment has resulted in high inpatient and outpatient adoption of the EHR, and high clinical functionality as compared to the private sector, and likely contributed to better inpatient and outpatient quality measures. The cumulative net benefit from these VistA applications during the study period is estimated at $3.1 billion. The CPRS, which was 100% adopted by 2002, is a major driver of the costs as well as the value. The extent to which the VHA has been able to capture and realize this created value is unknown. Implications for Policy, Delivery or Practice: Cost savings from this investment likely occurred from economies of scale due to in-house software development and support, followed by rapid and high inpatient and outpatient adoption. The VHA is now implementing initiatives to better monitor and track the impact of IT investments, which will ideally add to the body of knowledge about IT cost benefit and value analyses, and IT adoption and evaluation measures. Establishing a framework and methods for evaluating health IT is essential to understanding actual gains and/or consequences from IT use across a system. Public and privatesector policies and programs alike should work towards developing a common set of measures. Funding Source(s): VA Poster Number: 311 The Impact of Health Information Technology Expenditures on Length of Stay and In-hospital Mortality for Acute Myocardial Infarction- Evidence from the Texas Hospital Inpatient Database Presented by: Hsueh-Fen Chen, Ph.D., Assistant Professor, Health Management and Policy, University of North Texas Health Science Center, 3500 Camp Bowie Boulevard., Grapevine, TX 76107; Phone: (817) 735-0311; Email: hschen@hsc.unt.edu Co-authors: Fernando Wilson, Ph.D.; Nuha Lackan, Ph.D.; Abby Kazley, Ph.D. Research Objective: To examine the effect of health information technology (HIT) expenditures by hospitals on the length of stay and in-hospital mortality for acute myocardial infarction (AMI) patients. Study Design: This study uses patient-level, crosssectional data from the 2007 Texas Hospital Inpatient Discharge Public Use Data File (THIDPUDF). The THID-PUDF contains clinical data on all inpatient hospital stays occurring in Texas hospitals. The outcome measures are length of stays and in-hospital mortality for AMI patients. The primary independent variable is the HIT expenditure from the 2006 Texas Hospital Annual Survey. This variable is dichotomized into high expenditure versus low expenditure. A propensity score stratification approach is used with linear regression for length of stay outcome and logit regression for in-hospital mortality. This approach adjusts for possible endogeneity resulting from the possibility that hospitals with high quality of and efficient care are more likely to invest in HIT. The control variables are hospital, market, and patient characteristics from the Texas Hospital Annual Survey, Bureau of Economic Analysis, and THIDPUDF. Population Studied: The study population is individuals aged 18 or older who resided in Texas and were admitted into acute general community hospitals in Texas with a primary diagnosis AMI. Subjects were excluded from the study if they transferred into or out of other acute care hospitals, were admitted into a hospital with less than five admissions, had a length of stay less than two days or more than 30 days, or had missing disposition of the patients at discharge, race, or age information. Additionally, patients with any secondary diagnoses related to HIV or substance abuse were excluded because age information was not available for these patients. The study sample contains data on 18,357 AMI patients admitted to 162 hospitals in Texas in 2007. Principal Findings: After controlling for the lagged effect of HIT expenditure and the endogeneity between HIT expenditures and the two outcome measures, AMI patients admitted to hospitals with above 50 percentile of HIT expenditure significantly experienced shorter length of stay by 3 percent (p<0.01), compared to the ones admitted to hospitals with below 50 percentile of HIT expenditure; however, differences in in-hospital mortality rates between hospitals with high and low HIT expenditures is not statistically significant. Conclusions: Our results suggest that hospitals with high HIT expenditure provide more efficient AMI care, as measured by inpatient length of stay than hospitals with low HIT expenditure. Shortening lengths of stay for AMI inpatients may serve as a plausible mechanism for hospitals to reduce costs without compromising quality of care. Implications for Policy, Delivery or Practice: Investment in HIT by hospitals not only results in benefits to patients, but to the health system as a whole. Given the health sector’s rising proportion of the GDP, any strategies to improve efficiency and reduce costs within the healthcare system should be carefully considered. Although HIT is expected to increase quality of care, our result for the inhospital mortality is not significant. Identifying other quality indicators to measure the HIT effect is needed. Poster Number: 312 A Qualitative Study of Technology Acceptance in Primary Care Practices Presented by: Karen Danna-Lynch, Ph.D., Research Fellow, Family Medicine, UMDNJ-Robert Wood Johnson Medical School, 1 World's Fair Drive, Somerset, NJ 08873; Phone: (609) 2403122; Email: lynchda@umdnj.edu Co-authors: Deborah Cohen, Ph.D.; Rebecca Etz, Ph.D.; Jesse Crosson, Ph.D. Research Objective: Appropriate health information technology (HIT) is needed to deal with the wide level of care provided in the primary care (PC) setting. Yet, despite the expected benefits, there is evidence of numerous implementation failures and low adoption rates. Thus, to optimize HIT adoption in PC settings, it is crucial to better understand the implementation process. This study explores the extent to which a widely used model in the information systems literature (Davis’ 1986 Technology Acceptance Model or TAM) predicts successful implementation. Study Design: This study represents a secondary analysis of 18 qualitative case studies of PC practices in the process of adopting a new HIT. Original data were collected using semi-structured interviews, open-ended questions, and observations. We examined the data with specific reference to TAM, looking at the implementation of 3 different forms of HIT used for the purpose of delivering (direct) patient care: electronic medical records, e-prescribing software, and populationspecific electronic registries. We conducted a content analysis of all data using ATLAS.ti. Population Studied: Eighteen PC practices in 3 states (CA, MI, and NJ) involved in the process of implementing a new HIT. The end-users of the HIT were health-care professionals providing medical care. Principal Findings: Results show that while TAM predicts a portion of factors related to the use and acceptance of HIT (such as ease of use and perceived usefulness), other context-specific factors play an important role in facilitating or hindering HIT adoption in the PC setting, including: 1) personal experience (including prior knowledge of and comfort levels with computers); 2) social support (such as practice-specific champions or team support); 3) social norms (e.g., is HIT use required in the practice? Are computers routinely used for other functions within the practice?); and 4) contextual factors (including government announcements or other outside recommendations). A method for incorporating these additional variables into subsequent theory and research is presented. Conclusions: While TAM has a strong track record in other industries, questions remain concerning its applications to health care. Results show that TAM, used in its generic form, does not capture some of the unique contextual features related to successful HIT implementation in the PC setting. By focusing on end user reactions to the implementation and use of various HIT, this study presents empirical evidence of the subjective norms, personal experiences, and contextual factors that act as actual barriers and/or facilitators to HIT use. We use this evidence to refine and contextualize TAM with respect to the PC context. We tentatively suggest that contextualized TAM measures replace the practice of using generic measures to increase the theory’s compatibility to the health care field. Implications for Policy, Delivery or Practice: This study suggests ways of tailoring TAM so as to help end-users in PC practices prepare for the implementation of various HIT. We present evidence for a contextualized version of TAM that will allow both researchers and practitioners to become aware of PC relevant variables. As such, the results of this study are in line with the growing interest in the concept of “fit” as a critical need for successful HIT design and successful implementation. Funding Source(s): AHRQ, National Institute for Diabetes and Digestive Kidney Diseases Poster Number: 313 IT-Enabled, Non-Invasive Automated Detection of Diabetes Mellitus from a Pulse Morphology Pattern in the Impedance Plethysmographic Pulse Waveform Presented by: Medha Dhurandhar, Ph.D., Head & Program Coordinator, High Performance Computing, Centre for Development of Advanced Computing, Pune University Campus, Ganeshkhind Road, Pune, India 411007; Phone: +2025704222; Email: mdhurandhar@gmail.com Co-authors: Girish Tillu, M.D. Research Objective: To develop IT-enabled tools for detection of metabolic syndromes based on impedance plethysmographic (IPG) pulse signal harnessing low cost, non-invasive technology and mathematical modeling Study Design: Multidisciplinary approach deploying IT-enabled data mining, medical instrumentation and mathematical modeling. Observational, Double-blinded Study. Recording of Clinical Investigations like BP, Lipid profile, Glucose level of the volunteers. Simultaneously capturing IPG-based Pulse signal for a period of 300 seconds from the wrist of the volunteer. Pulse signal analysis based on data mining and mathematical modeling. Multi-centric Study at various hospitals, clinics and institutes. Methodology: Scrubbing of pulse signal data by filtering high frequency noise; Data conversion to ASCII format; Data analysis using numerical methods for identifying a) Proper systolic peaks b) On-set points of the pulse waveform c) Identification of various complexes d) Classification of the complexes into "dominant" and "nondominant" (ectopic) types e) Identification of major deflection points in each of the complexes f) Feature extraction measuring amplitudes and intervals g) Automated pattern recognition based on the correlation amongst the major deflection points h) Determining pattern distribution over the 300 secs. interval i) Finding the most dominant pattern j) Diagnostic classification Population Studied: 557 volunteers: Male & Female; Age Group- 35 to 65. 241 Healthy volunteers. Patients: 91 Diabetic and 225 Nondiabetic but suffering from other diseases Principal Findings: Sufficient condition obtained for a peculiar pulse morphology pattern “MedhaMorph” indicating the volunteer to be diabetic with 98.74% accuracy. The volunteers having MedhaMorph as the dominating pulse pattern were found diabetic with the following exceptions: 1. Only 2 healthy volunteers out of 241 had this pulse pattern (99.17% accuracy), and 2. Only 5 non-diabetic patients out of 225 had pulse pattern MedhaMorph. (97.78% accuracy). Conclusions: Hyperglycemia induced vascular changes in Diabetic patients lead to several complications like retinopathy, nephropathy and neuropathies. It is important to detect these changes early to avoid complications. Proposed method simulates pulse examination and classifies an IPG-based pulse morphology pattern for DM from the pulse signal captured from the peripheral vessel. Even when a patient is under treatment for DM, this pattern can be detected. Follow-up study is being done to see if the exceptions prove to be DMprone. Though currently DM is targeted similar method may be adopted to detect and predict other diseases/disorders especially related with Metabolic Syndrome from a particular pulse morphology pattern. Implications for Policy, Delivery or Practice: Current diagnostic methods for Diabetes detection are invasive. They require blood examination with antiseptic precautions and a laboratory set-up causing venipuncture. Glucometer can be used at home but is expensive and gives approximate blood concentration of glucose. Proposed tool is noninvasive and cost-effective. Also the procedure is not time-consuming and can be carried out at home with a little practice. This minimizes the need for time-consuming visits to pathological laboratories and can help detect DM related medical problems before they become severe or life-threatening. Moreover, such out of medical center testing could reduce unnecessary burden on healthcare professionals and facilities, as well as costs for payers. Funding Source(s): Ministry of ICT, India Poster Number: 314 Reliability and Validity of HIMSS and Leapfrog Data on Computerized Provider Order Entry Presented by: Mark Diana, Ph.D., M.B.A., M.S.I.S., Assistant Professor, Health Systems Management, Tulane University, 1440 Canal Street, Suite 1900, New Orleans, LA 70112-2699; Phone: (504) 988-5359; Email: mdiana@tulane.edu Co-authors: Abby Kazley, Ph.D.; Nir Menachemi, Ph.D. Research Objective: The objective of this research is to assess the reliability, validity, and responsiveness of the HIMSS and Leapfrog dataset measures of computerized physician order entry. Study Design: We created dichotomous measures of the presence of CPOE in hospitals for each data set in each year using the most complete status of CPOE adoption in each survey. We assessed the reliability of the CPOE measure individually for each dataset alone. We tested the validity of the CPOE measure by calculating sensitivity, specificity, positive predictive value, and negative predictive value for each dataset, using the other dataset as the gold standard. We also tested the responsiveness of each dataset by examining the percent increase in complete CPOE adoption from one year to the next in HIMSS and Leapfrog data respectively. Population Studied: We used secondary data on US hospitals collected by HIMSS Analytics, the Leapfrog Group, and the American Hospital Association from 2005 through 2007. We created a dataset from each survey for each year for hospitals that reported CPOE status, a dataset that combined hospitals across all three years for each source, and a dataset that combined hospitals across all three years from both sources. Principal Findings: Hospitals with known CPOE status in both the HIMSS and Leapfrog datasets ranged from 1,053 to 2,355. Reliability was similar, ranging from 76 – 78% in the HIMSS data and 81 – 86% in the Leapfrog data. HIMSS data sensitivity ranged from 48.4 – 71.8%, data specificity ranged from 84 – 89.0%, positive predictive value ranged from 10 – 20%, and negative predictive value was in the range of 98%. Leapfrog data sensitivity ranged from 10 – 20%, specificity was consistently 98%, positive predictive value ranged from 48 – 72%, and negative predictive value ranged from 84 – 89%. Conclusions: Our findings indicate minimal agreement between the two datasets regarding which hospitals have adopted CPOE, but adequate agreement within a given dataset from year to year. The HIMSS data tends to overestimate increases in adoption over time, while the Leapfrog data has more downward trending estimates for year over year increases in CPOE adoption. The Leapfrog data are better suited to for studying outcomes associated with CPOE adoption, while studies whose purpose requires the certain classification of non-adopting hospitals can utilize HIMSS data effectively. Implications for Policy, Delivery or Practice: The disagreement between the HIMSS and Leapfrog datasets regarding hospital CPOE use creates a challenge for researchers, practitioners, and policymakers who wish to understand CPOE use from a national perspective. A possible way to overcome this limitation is for future studies to utilize both datasets and create multiple groups based on agreement or disagreement in the HIMSS and Leapfrog datasets. Specifically, researchers could examine how the results of their study differ when comparing hospitals that reported CPOE use in both datasets to their counterparts that positively reported in only one of the datasets. This sensitivity analyses would be desirable to the presentation of results for only one of the data sources. Poster Number: 315 The Effect of the Implementation of an Electronic Health Record on Nursing-Sensitive Patient Outcomes Presented by: Dawn Dowding, Ph.D., Harkness Fellow, Institute of Health Policy, Kaiser Permanente, One Kaisa Plaza, 22nd Floor, Oakland, CA 94612; Phone: (510) 271-6853; Email: dawn.w.dowding@kp.org Research Objective: To examine the impact of the introduction of an Electronic Health Record (EHR) on nursing sensitive patient outcomes Study Design: An Interrupted Time Series Design. The intervention of interest is the implementation of an EHR in acute clinical areas, specifically acute medical, surgical and critical care units. Data will be collected on the following nursing sensitive patient outcomes and aggregated at facility level; failure to rescue, hospital acquired pressure ulcers, falls and falls with injury, restraint use, peripherally inserted central catheter related blood infections, surgical site infection rates, ventilator associated infections, central line catheter-associated blood stream infection rate for ICU and high risk nursery (HRN) patients. Data will be obtained from three sources; the Collaborative Alliance for Nursing Outcomes (CalNOC), hospital administrative data bases and the national quality, resource and risk management department for Kaiser Permanente. As the implementation of the EHR has been staged, the time point at which the intervention has occurred is different in different facilities. Facilities where the EHR has not been implemented will act as a control group, to assess the potential effect of any external influences on changes in the outcome measures. Population Studied: 33 health care facilities in one Health Care Organisation. Principal Findings: Data will be plotted to examine trends in changes in outcomes over time. Data will also be analyzed using established techniques for the analysis of ITS (analysis of variance, segmented regression analysis, autoregressive integrated moving average models) depending on the number of time points before and after intervention. Data will be corrected for autocorrelation and any seasonal variations in outcome measures. Conclusions: Results of the ITS can identify what impact (if any) the introduction of a comprehensive Electronic Health Record has on patient outcomes associated with the quality of nursing care. Implications for Policy, Delivery or Practice: Many countries, including the U.S. and U.K., are investing in health information technology as a way to improve the quality and safety of care that patients receive. Whilst nurses comprise a significant part of the health care workforce, comparatively little is known about how they use information technology to inform the decisions they make, and the impact this has on the care patients receive. The results of this study will provide valuable evidence to inform how electronic health records can be used to improve nursing care. Funding Source(s): CWF Poster Number: 316 Implementation of Personal Health Records and the Oregon Medicaid Experience: An Evaluation Study Presented by: Oliver Droppers, M.S., M.P.H., Research Assistant, Hatfield School of Government, Portland State University, PO Box 751, Portland, OR 97207-0751; Phone: (503) 24164692; Email: odropper@pdx.edu Co-authors: Sherril Gelmon, Dr.PH.; Jill Rissi, Ph.D. Research Objective: The State of Oregon is implementing a personal health record system (PHR) using a health record bank model for its Medicaid population, supported by a federal Medicaid Transformation Grant. This unique consumer-centric approach could potentially enhance Medicaid clients’ ability to monitor and manage their own health, helping individuals become more active participants in their own wellness and self-care. An evaluation team from Portland State University was contracted by the State to assess the utility of the PHR based on the experiences of Medicaid clients during the initial implementation in 2009-2010. Study Design: The study is quasi-experimental, employing mixed methods through a communityengagement research strategy including use of online surveys, interviews, focus groups, direct observations, and documentation review. Data will be collected during three stages of PHR adoption: design, implementation and optimization. An evaluation conceptual framework of key concepts and indicators will guide the research, helping to illustrate barriers to and facilitators of PHR adoption. Population Studied: Potential participants include all publicly insured individuals within the Oregon Medicaid system who create a personal health record during the study period. As of October 2009, Oregon Medicaid covered approximately 384,000 low-income children, pregnant women, disabled and senior adults. Adults are enrolling in the first phase; followed by children and their associated caregivers, case managers and/or foster parents. All individuals creating a PHR account are eligible to receive the baseline survey. In the first six months (i.e. up to the 2010 ARM), all enrollees are being surveyed. Principal Findings: Preliminary findings from baseline enrollment surveys indicate the following factors are critical in terms of engaging and facilitating consumers in the use of PHRs: environment of trust, privacy and security; consumer choice regarding enrollment; presence of a trusted not-for-profit community organization or state agency as the facilitator of the PHR system; and sharing and accessibility of patient information. Factors likely to influence accessibility and use of PHRs among the study population are limited computer and health literacy, challenges with informed decision-making using their own medical information, and usability of health information accessed through Internet Web sites. Conclusions: PHR systems, particularly those that are consumer-oriented and controlled, are in their infancy. The PHR is intended to facilitate opportunities for Medicaid clients to effectively control and share their personal health information. Findings from this research may inform predictions about the widespread use of PHRs, as we come to appreciate and understand how Medicaid clients interact with PHRs, given fundamental issues related to Internet access and health literacy. Implications for Policy, Delivery or Practice: PHRs must be designed to be accessible to all population groups in order to address existing digital disparities across vulnerable populations. Enhanced understanding of this new technology is a first step. Findings from this study may inform consumers, providers, policymakers, and others, as well as complement the efforts of numerous national, regional, and state health information exchange projects seeking to control health care costs, improve safety, quality, and efficiency, and ultimately achieve better health outcomes through the use of PHRs. Funding Source(s): CMS Poster Number: 317 Measurement of Utilization of an Installed EHR Presented by: Prashila Dullabh, M.D., Health IT Program Manager, Health, National Opinion Research Center, 4350 East-West Highway, Suite 800, Bethesda, MD 20814; Phone: (202) 280-9294; Email: dullabh-prashila@norc.org Co-authors: Elizabeth Babalola, B.A.; Adil Moiduddin, M.P.P.; James Sorace, M.D., M.S. Research Objective: In 2009 the National Opinion Research Center (NORC) conducted a study to assess the feasibility of systematic automated approaches of tracking EHR usage. Study Design: NORC conducted a review of the literature using PubMed to search for peer reviewed publications on national studies of EHR adoption. Internet searches were also conducted to identify government reports and articles relevant to assessing EHR adoption in ambulatory settings. A series of phone discussions were held with stakeholders representing major ambulatory EHR vendors, health center representatives, ambulatory practices and informants involved with quality improvement and EHR adoption. Population Studied: This study included a review of EHR adoption broadly but specific focus was given to federally supported health centers and other safety-net providers. Principal Findings: Limitations in the use of surveys to assess EHR adoption. In a report comparing existing surveys assessing EHR adoption up till the year 2008 it was found that the surveys were of varying quality. EHR Use Limited to Basic Functions. Review of current EHR use suggests that in all practices (small, mid and large) there are certain basic clinical and administrative functions that are commonly used notably encounter notes, medication lists, allergy lists, problems lists, and order entry functions largely focused around lab order entry and results delivery. E-Prescribing (eRX) use is limited but growing rapidly. In addition practices of all sizes report that they support clinical decision support functions related to eRx largely in the form of drug interaction and drug-allergy checking. Tremendous Variability in How EHR Use is Being Monitored. Tracking of EHR utilization data vary in the granularity of tracking, the features being tracked, metrics that are used to assess utilization, the reporting database and the kinds of reports that are being generated. Smaller practices do not appear to have the IT resources and infrastructure to readily support utilization tracking. Feasibility of an Automated Reporting Mechanism. Practices are using different mechanisms of varying degrees of automation to report on quality measures. Some EHR vendors are already providing options for their install base to upload de-identified clinical data on a monthly basis to a centralized research server. The capability of generating automated reports is technically feasible and currently exists. Conclusions: Study findings indicate that there is a common set of EHR functions that all practices are likely to have purchased and that sites would be capable of implementing. Most EHR vendors have capability to track usage of these common functions even though they may not all support the same robust reporting capabilities. By providing tools to health centers and networks to monitor EHR utilization these organizations would be better equipped to promote meaningful use and adoption proactively. These reports can also be used to augment information derived from traditional survey instruments Implications for Policy, Delivery or Practice: “The views expressed in this report/presentation are solely those of the authors, and do not necessarily reflect the views of the Department of Health and Human Services.” Funding Source(s): The Assistant Secretary for Planning and Evaluation (ASPE) Poster Number: 318 Health Information Technology and Physician Career Satisfaction Presented by: Keith Elder, Ph.D., M.P.H., M.P.A., Assistant Professor, Health Services Administration, University of Alabama at Birmingham, LRC 325A 1530 3rd Ave South, Birmingham, AL 35294; Phone: (205) 996-9808; Email: ktelder@uab.edu Co-authors: Nicole Quon, Ph.D.; Ronica Rooks, Ph.D.; Jacqueline Wiltshire, Ph.D.; Rhonda Belue, Ph.D.; Lisa Gary, Ph.D. Research Objective: Health information technology (HIT) and physician career satisfaction are associated with higher quality medical care. However, the link between HIT and physician career satisfaction, which could potentially reduce provider burn-out and attrition, has not been fully examined. This study uses a nationally representative survey to assess the association between key forms of HIT and career satisfaction among primary care physicians (PCP) and specialty physicians. Study Design: We performed a retrospective, cross sectional analysis of physician career satisfaction using the Community Tracking Study Physician Survey, 2004-2005. Nine specific types of HIT as well as the overall adoption of HIT in the practice were examined using multivariate logistic regression. Population Studied: The study sample included 5198 physicians, of which 3016 were primary care physicians and 2182 were specialists. Principal Findings: Physicians who used 5 to 6 (OR=1.46) or 7 to 9 (OR=1.47) types of HIT were more likely than physicians who used 0 to 2 types of HIT to be “very satisfied” with their careers. Information technology usages for communicating with physicians (OR =1.31) and emailing patients (OR=1.35) were positively associated with career satisfaction. PCPs who used technology to write prescriptions were less likely to report career satisfaction (OR=0.67) while specialists who wrote notes using technology were less likely to report career satisfaction (OR=0.75). Physicians who treated chronically ill patients (OR range = 0.570.87) or patients with language barriers (OR range=0.47-0.58) were also less likely to report being “very satisfied” with their careers. Conclusions: Using more information technology was the strongest positive predictor of physicians being very satisfied with their careers. Implications for Policy, Delivery or Practice: Health care organizations working in conjunction with providers should consider exploring ways to integrate various forms of HIT into practice. Funding