model Familiar Patient Safety in the VA History
advertisement
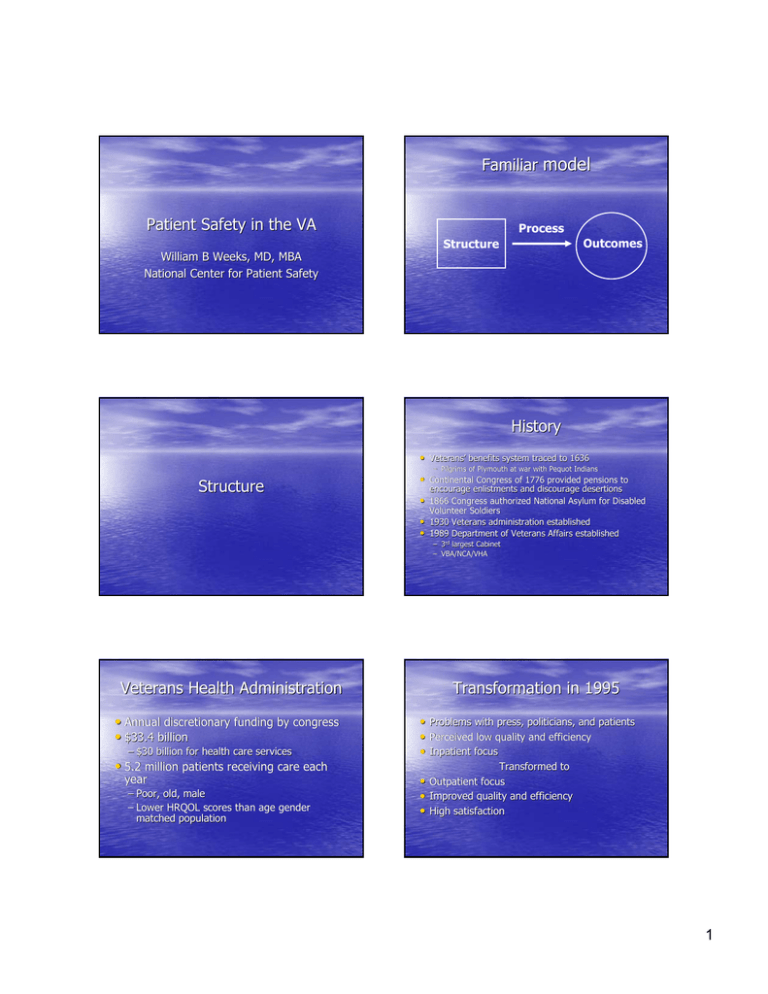
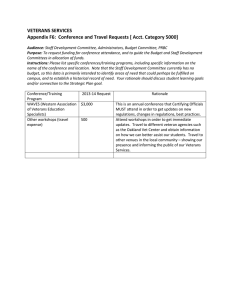
Familiar model Patient Safety in the VA William B Weeks, MD, MBA National Center for Patient Safety Process Outcomes Structure History • Veterans’ Veterans’ benefits system traced to 1636 – Pilgrims of Plymouth at war with Pequot Indians Structure • Continental Congress of 1776 provided pensions to encourage enlistments and discourage desertions • 1866 Congress authorized National Asylum for Disabled Volunteer Soldiers • 1930 Veterans administration established • 1989 Department of Veterans Affairs established – 3rd largest Cabinet – VBA/NCA/VHA Veterans Health Administration • Annual discretionary funding by congress • $33.4 billion – $30 billion for health care services • 5.2 million patients receiving care each year – Poor, old, male – Lower HRQOL scores than age gender matched population Transformation in 1995 • Problems with press, politicians, and patients • Perceived low quality and efficiency • Inpatient focus Transformed to • Outpatient focus • Improved quality and efficiency • High satisfaction 1 Patient Safety Program Structure • National Center for Patient Safety – Established in 1998 Process • Administration – Responsible for policy development, oversite • Operations – Patient safety managers (160 facilities) – Patient safety officers (21 regions) • Investigation – 4 Patient Safety Centers of Inquiry 1. Identification and mitigation of system vulnerabilities Computerized entry – Identification of actual and potential adverse events – Evaluation of severity and frequency – (Aggregate) root cause analysis – Healthcare Failure Mode Effects Analysis – Implementation of corrective actions – Sharing of results Before Reporting Local Incident Report Local Review Possible Local Action Regional Review if Requested Regional National After Local Incident Report Local Review Regional National National Database Analysis and Corrective Action Documented Effectiveness of Action Regional Review Possible Regional Action National Review Possible National Action 2 2. Use of incentives • Performance measures – Widely seen as the key to VA transformation • Safety focus, using results of RCAs – Appropriate use and timeliness of preoperative antibiotics – Timeliness of radiology reporting 4. Technology • Bar Code Medication Administration • Computerized Medical Record • Computerized Order Entry • Critical value alerts • Lab, path, card, and radiology reports Not without their own issues and challenges 3. Support • Program managers who provide guidance and networking • Training, calls, email, alerts, newsletter, web • Toolkits – Falls prevention – Cognitive aids • Patient Safety Improvement Projects – Medical Team Training – Barcode Administration 5. Cooperation with other agencies • JCAHO – Cooperative development of patient safety goals – Pilot and experience in VA can modify – Bagian on review board • AHRQ – Patient safety improvement corps • Modification of training provided to VA PSMs, PSMs, PSOs • DOD – Joint efforts • Breakthrough series • Sessions Current • Internal Outcomes – Facility participation – Reporting quality – Performance measures • External Process measures – JCAHO – NCQA 3 Future • Focus on patient outcomes • Some challenges… challenges…. – Veterans use multiple systems of care – AHRQ indicators may need modification for VA Thanks • Potential opportunities to identify vulnerable subpopulations – NonNon-Medicare enrolled elderly – Patients with psychiatric disorders 4