Evidence Demonstrates Rural Public Health Departments Struggle to Meet Demands
advertisement
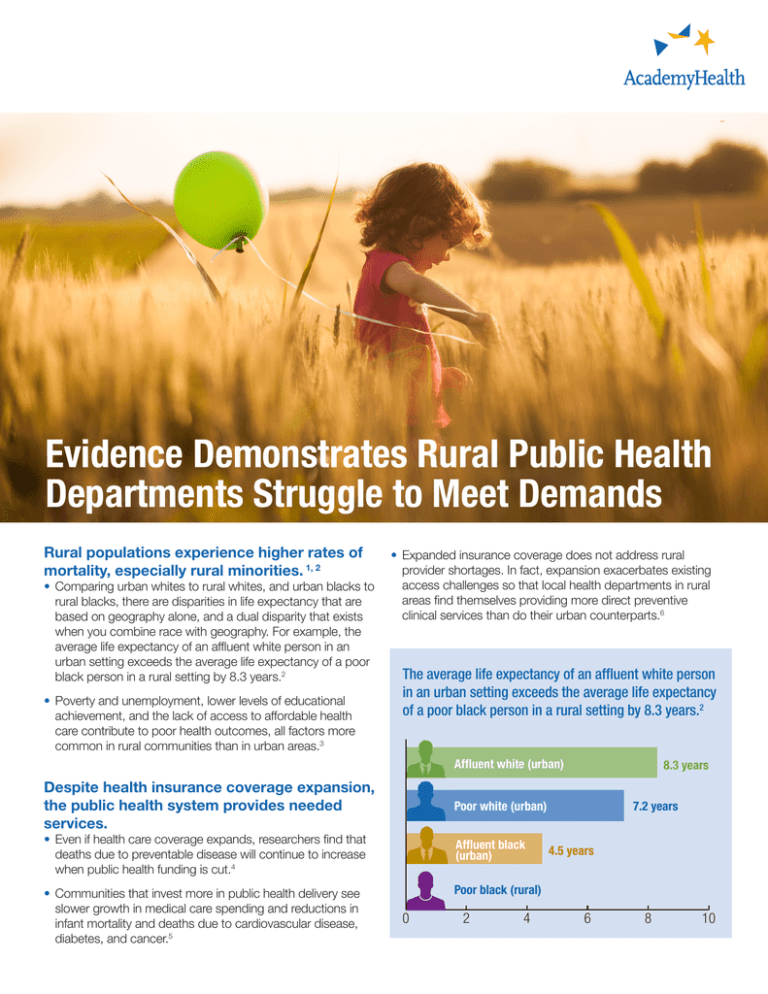
Evidence Demonstrates Rural Public Health Departments Struggle to Meet Demands Rural populations experience higher rates of mortality, especially rural minorities. 1, 2 • Comparing urban whites to rural whites, and urban blacks to rural blacks, there are disparities in life expectancy that are based on geography alone, and a dual disparity that exists when you combine race with geography. For example, the average life expectancy of an affluent white person in an urban setting exceeds the average life expectancy of a poor black person in a rural setting by 8.3 years.2 • Poverty and unemployment, lower levels of educational achievement, and the lack of access to affordable health care contribute to poor health outcomes, all factors more common in rural communities than in urban areas.3 • Expanded insurance coverage does not address rural provider shortages. In fact, expansion exacerbates existing access challenges so that local health departments in rural areas find themselves providing more direct preventive clinical services than do their urban counterparts.6 The average life expectancy of an affluent white person in an urban setting exceeds the average life expectancy of a poor black person in a rural setting by 8.3 years.2 Affluent white (urban) Despite health insurance coverage expansion, the public health system provides needed services. Poor white (urban) • Even if health care coverage expands, researchers find that deaths due to preventable disease will continue to increase when public health funding is cut.4 • Communities that invest more in public health delivery see slower growth in medical care spending and reductions in infant mortality and deaths due to cardiovascular disease, diabetes, and cancer.5 8.3 years Affluent black (urban) 7.2 years 4.5 years Poor black (rural) 0 2 4 6 8 10 Resources are needed to bolster the rural public health system. • Local health departments (LHDs) in rural communities function with lower staffing levels and rely more heavily on part-time public health workers than do their urban counterparts.7, 8 • LHDs in rural communities are proportionally more reliant on state and federal resources; an additional $10 of public health spending per person saves approximately 9.1 lives per 100,000 people—resulting in an annual savings of $2.95 billion.9 • A very small proportion of the evidence focuses on rural health departments—which comprise approximately 60 percent of all LHDs.10 Rural Health in the Numbers11 •Rates of Chronic Obstructive Pulmonary Disease (COPD) are 31 percent higher among our most rural citizens, as compared to our most urban citizens—and it has grown by 25 percent over the past decade, compared to 6% amongst urbanites. • Smoking rates among our most rural youth (age 1217) are double those of our most urban youth; while smoking rates among our most urban adults have decreased 30% over the past decade, rates among rural adults have remained constant. • Mortality rates for heart disease are 80 percent higher for women in the South and more than double the U.S. rate for men in the South. • Mortality rates for suicide are 80 percent higher for men and women in the West. • Mortality rates for cancers are 40 percent higher for men and women in Appalachia. • Mortality rates from unintentional injury are nearly double for men in Appalachia and 2.3 times higher for women in Appalachia. About AcademyHealth AcademyHealth is a leading national organization serving the fields of health services and policy research and the professionals who produce this important work. Together, with our members, we offer programs and services that support the development and use of rigorous, relevant, and timely evidence to increase the quality, accessibility, and value of health care, to reduce disparities, and to improve health. A trusted broker of information, AcademyHealth brings stakeholders together to address the current and future needs of an evolving health system, inform health policy, and translate evidence into action. For additional publications and resources, visit academyhealth.org. Endnotes 1. Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J Urban Heal. 2013;91(2):272-292. doi:10.1007/s11524-013-9847-2. 2. Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):19-29). doi:10.1016/j.amepre.2013.10.017. 3. Crosby R, Monica ML, Vanderpool RC, Casey B. Rural Populations and Health: Determinants, Disparities, and Solutions. San Francisco, CA: John Wiley and Sons; 2012. 4. Mays GP. Does Medicaid crowd out other public health spending? Projecting ACA’s health & economic effects. AcademyHealth Annual Research Meeting. San Diego, CA. Jun. 2014. 5. Mays GP and Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Affairs. 2011; 30(8): 1585-93. doi: 10.1377/ hlthaff.2011.0196 6. Beatty KE, Meit M, Hale N, Khoury A, Masters P. Clinical Service Delivery Disparities along the Urban/Rural Continuum. Paper presented at AcademyHealth PHSR Interest Group Meeting; 2015 June 16-17; Minneapolis, Minnesota. 7. Leep CJ. 2008 national profile of local health departments. J Public Health Manag Pract. 2008;12(5):496-498. http://www.ncbi.nlm.nih.gov/pubmed/22286289. 8. Leider JP, Shah GH, Castrucci BC, Leep CJ, Sellers KSJ. Changes in public health workforce composition: Proportion of part-time workforce and its correlates, 2008–2013. Am J Prev Med. 2014;5 Suppl 3(Nov):S331-S336. doi:10.1016/j.amepre.2014.07.017 9. Brown TT. How effective are public health departments at preventing mortality?. Econ Hum Biol. 2013; 13(1): 34-45. doi: 10.1016/j.ehb.2013.10.001 10.Hale NL. Rural public health systems: challenges and opportunities for improving population health. AcademyHealth. October 2015. 11.Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey.