Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente 2015 Annual Meeting
advertisement
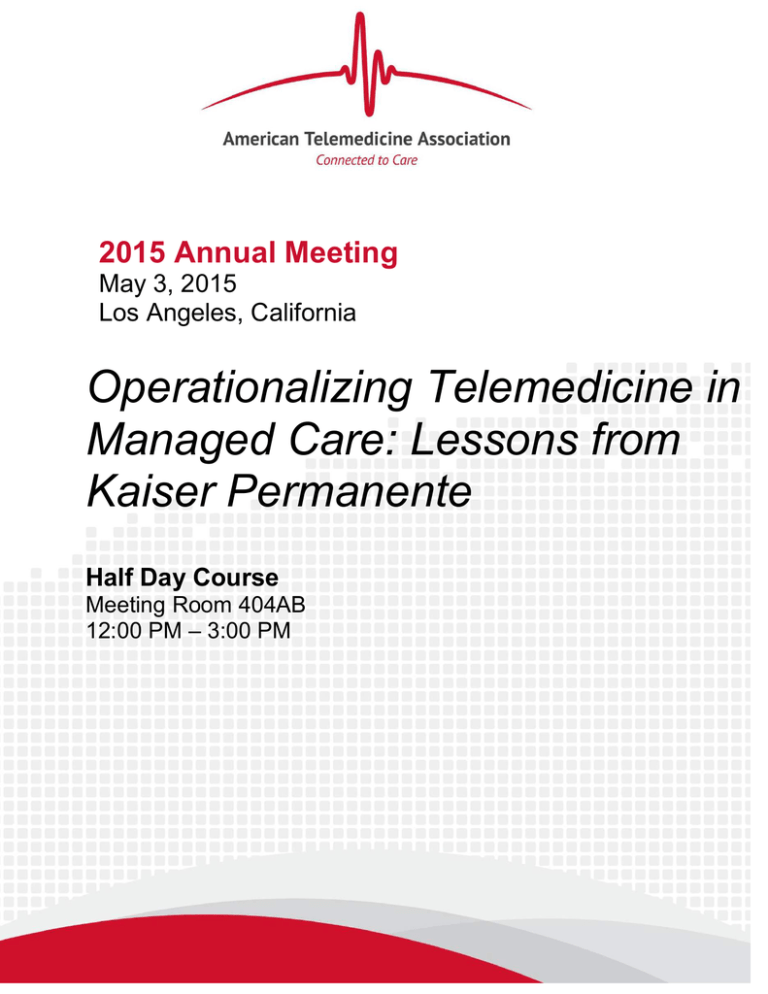
2015 Annual Meeting May 3, 2015 Los Angeles, California Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente Half Day Course Meeting Room 404AB 12:00 PM – 3:00 PM Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente Half Day Course May 3, 2015 –12:00pm – 3:00pm Room 404AB Creating and sustaining an effective, efficient and predictable telehealth program within the already complex care delivery paradigm can be challenging and overwhelming. As the country moves from fee-for-service to value driven reimbursement, Kaiser Permanente will share their strategy and lessons learned for operationalizing telehealth into the managed care delivery model. This course will address how this organization leveraged a variety of telehealth technologies and workflows to enhance and expand quality care, increase consumer engagement and reduce healthcare costs. This course will provide a high level overview of Kaiser Permanente’s Telehealth strategy with detailed learnings from a few select programs. Participants will learn about where and how to incorporate telehealth into an established care delivery model and how to overcome adoption barriers and select the right technology partners. LEARNING OBJECTIVES Understand where and how to incorporate telehealth into an established care delivery model Identify critical success factors and challenges based on the type of program Overcome adoption barriers across key stakeholders Understand how to select the right technology partners Agenda Time Topic Who 12:00 – 12:10 Introduction & Overview of Kaiser Permanente Madhu Narasimhan 12:10 – 12:30 The Landscape of Virtual Care Bill Marsh, MD 12:30 – 12:50 12:50 – 1:10 Video Visits: Outpatient/Home Settings KP Southern California KP Mid-Atlantic States – Leveraging Resources across Departments and State Lines Tadashi Funahashi, MD Dennis Truong, MD 1:10 – 1:35 Break Out Session 1:35 – 1:45 Break 1:45 – 2:15 Video Visits: Inpatient Setting – Telestroke Jo Carol Hiatt, MD, MBA 2:15 – 2:35 Patient-generated Health Data Mark Groshek, MD 2:35 – 3:00 Q&A All Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente Course Faculty Madhu Narasimhan, Vice President, Virtual Care & Analytics, Kaiser Permanente Information Technology (Moderator): Madhu Narasimhan manages teams in the areas of care delivery telehealth, information analytics, health information exchange, clinical informatics, emerging technologies, and clinical contact center systems. Madhu joined Kaiser Permanente in 2002, served in various management positions, and became a vice president in 2010. Madhu has more than 20 years of experience in software development, project/program management and application delivery experience. Tadashi Funahashi, MD, Chief Innovation and Transformation Officer; Assistant Regional Medical Director, Kaiser Permanente Southern California: Tadashi Funahashi, MD joined Kaiser Permanente Southern California Region, Orange County in 1992, and maintains a busy clinical practice in orthopedic surgery. He is the Chief Innovation and Transformation Officer and Assistant Regional Medical Director for Kaiser Permanente Southern California. Dr. Funahashi also founded and chairs the National Implant Registry Committee, and is a clinical professor of orthopedic surgery at University of California Irvine College of Medicine. He earned his medical degree and completed his orthopedic residency at UCLA School of Medicine, and then joined the faculty at the UCLA Department of Orthopedic Surgery prior to joining Kaiser Permanente. Mark Groshek, MD, Medical Director, Digital Services Group, Colorado Permanente Medical Group: Mark Groshek joined the Colorado Permanente Medical Group in 1989. He practices pediatrics in Colorado, and has been part of the Kaiser Permanente Health Connect Team in Colorado since 2004, serving as the Colorado physician lead for kp.org, Kaiser Permanente’s patient web portal. Since June 2013, he has been the Medical Director for Digital Services Group, where he continues to work to ensure that Kaiser Permanente members have easy access to their own information and to their health care teams via kp.org. Communicating with his patients and their families and providing care through kp.org has been an important part of his practice, and he is especially interested in finding more and better ways to gather important member health information outside of Kaiser Permanente offices, to make that information easy to understand and act upon, and to provide more care to our members when and where they need it. He has become an expert on the special challenges with EMRs in honoring teen confidentiality, and published an article in 2012 outlining these issues. Jo Carol Gordon Hiatt, MD, MBA, Chair, National Product Council; Assistant Medical Director, Southern California Permanente Business Administration: Dr. Hiatt is Chair of the National Product Council for Kaiser Permanente and also chairs KP's Inter-Regional New Technologies Committee. She is a partner in Southern California Permanente Medical Group (SCPMG) and is currently Assistant Medical Director, SCPMG Business Management. Dr. Hiatt chairs Southern California's Technology Deployment Strategy Team as well as the Oversight Committee for Integrated Medical Imaging. Dr. Hiatt joined Kaiser Permanente as a general surgeon at Panorama City, later serving as Chief of Surgery at that location and member of the SCPMG Board of Directors. She received her undergraduate degree from Stanford University and her medical degree from Duke University, and trained in general surgery at UCLA. In addition to her clinical degree, Dr. Hiatt received an MBA from UCLA's Anderson School of Management. She was designated an American College of Surgeons Health Policy Scholar in 2013. Bill Marsh, MD, Vice President and Chief of Staff, Colorado Permanente Medical Group: Bill Marsh, MD functions as the VP & Chief of Staff for the senior executive team and the Colorado Permanente Medical Group. He is involved in all areas related to the member experience and service excellence. He also is involved in new technologies, including digital and mobile applications, telemedicine, and telehealth, both locally and nationally. He co-leads the national Kaiser Permanente Virtual Care Workgroup. He graduated from the University of Texas Medical School in San Antonio and completed his pediatric residency in Oklahoma City at Children’s Hospital and a fellowship in both allergy/immunology and pediatric pulmonary medicine at National Jewish Hospital in Denver. He was in private practice for five years before joining Kaiser Permanente. Dennis Truong, MD, FACEP, Emergency Medicine Physician; Telemedicine Director, Physician Lead for HouseCalls, Kaiser Permanente- Mid-Atlantic States: Dr. Truong joined MAPMG as an Emergency Physician in 2010. He helped with the genesis and development of Kaiser Permanente’s 5 regional Clinical Decision Units (CDU) and is a Physician Lead for the Call Center. As the region’s Telemedicine Director since 2014, one of his accomplishments was pioneering the Kaiser Permanente CDU Video Visit program, an innovative 24x7 telemedicine option for low-acuity medical conditions. The accomplishments of this program have been featured in The Washington Post, Modern Healthcare, a Verizon video and news blog, and won The Daily Record “Innovator of the Year” award. Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente Operationalizing Telemedicine in Managed Care: Lessons from Kaiser Permanente As you come in, please find a seat and fill out the worksheet at the middle of each table which will be collected before we begin today’s session. Today’s Agenda Introductions & Overview of Kaiser Permanente Madhu Narasimhan The Landscape of Virtual Care William Marsh MD Video Visits: Outpatient/Home Settings • KP Southern California • KP Mid-Atlantic States – Leveraging Resources Across Departments & State Lines Tadashi Funahashi MD Dennis Truong MD Break Out Session Video Visits: Inpatient Setting : Telestroke Jo Carol Hiatt MD, MBA Patient-Generated Health Data Mark Groshek MD Q&A 3 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Overview of Kaiser Permanente Madhu Narasimhan, Vice President, Virtual Care & Analytics, Care Delivery Business Information Office, KPIT 4 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Kaiser Permanente integrated Northwest 9.6 million members 17,000+ physicians Northern California 49,000+ nurses Colorado Mid-Atlantic Southern California Georgia 192,000+ employees 8 states + District of Columbia 38 hospitals Hawaii 600+ medical offices $56.4 billion operating revenue Nation’s largest not-for-profit health plan Scope includes ambulatory, inpatient, ACS, behavioral health, SNF, home health, hospice, pharmacy, imaging, laboratory, optical, dental, and insurance Telehealth in the (near) future… TELEHEALTH Using digital technologies to deliver medical care, health education, and public health services by connecting multiple users in separate locations. 20% to 30% OF MEMBER APPOINTMENTS COULD HAPPEN IN ALTERNATIVE NON-FACE TO FACE VENUES BENEFITS • • • • • • Timesaving, convenience Decreases CO2 emissions Fewer medical buildings needed Increased consumer satisfaction Expanded access to timely care Increased workplace productivity Kaiser Permanente’s Mission To provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. 7 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. The Landscape of Virtual Care William Marsh MD, Associate Executive Director Government Relations and Care Delivery IT The Permanente Federation 8 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Health Care is Unfrozen: Why Now? What does this mean? 9 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. “Spread health to all… we meet people where they are.” 10 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Virtual Care Work Group: Recommendation for Kaiser Permanente Top Populations Virtual Care Tools to Scale Program Wide Healthy Video Visits Low Utilizing Millennials Acute Respiratory, Minor Injury, Muscular- Skeletal, Dermatology Chronic Diabetes Transitions Hospital to Home End of Life Palliative, Hospice 11 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Web Chat & Text Self Triage w/ Intelligent Routing Member Generated Data; Questionnaires & Remote Monitoring Social Networks Video Visits between clinics & to home 12 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Telestroke 13 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Web Chat 14 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Self Triage, with intelligent routing Intelligent Routing 15 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Member Generated Data Questionnaires 16 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Patient Self-Monitoring Drivers of Health Personal Behaviors 40% Family History and Genetics 30% Environmental and Social Factors 20% Source: McGinnis et al, Health Affairs, 2002 17 10% Medical Care Social Networking Self Managed Health Care Support Social Media Confidence 18 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Knowledge Skills Please note questions on paper and we will collect and review them during the Q&A at the end of today’s session. Video Visits: Outpatient/Home Settings Kaiser Permanente Southern California Tadashi Funahashi MD Chief Innovation & Transformation Officer Asst Regional Medical Director, Health Innovation & Process Transformation Southern California Permanente Medical Group 20 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Integrated Video Visits Background The Integrated Video Visit (IVV) Project enables members to have a scheduled video visit with a Kaiser Permanente physician from their personal computer or mobile smart device (phones/tablets). Benefits Members can receive care without having to go to a Kaiser Permanente Facility Advantages Expanding traditional face to face appt. model. Additional products to meet member’s needs and compete in health care market. 21 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Integrated Video Visits Impact Service – Increase convenience for members and offer alternatives to traditional face-to-face visits. Access – Make virtual appointments more readily available for Primary Care and specialty. Quality – Improve outcomes when members receive more timely care. Affordability – minimize unnecessary ED/UC visits ; maximize use of in-network and specialty resources; reduce travel for patients 22 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Integrated Video Visits Technology Features • A third party platform is used for video visits and has been integrated with the KP EHR, website, and mobile app. • The video visits will be scheduled through the call center or physician’s back office staff. • Providers are able to view video visits on their schedule, launch video visits from their schedule, and document in KP’s EHR while in a video visit. • Members will be able to launch visits from the KP website or the KP flagship app and then review their AVS online. 23 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Integrated Video Visit Members Launch from KP website or mobile app Clinician Schedule & launch from KP’s EHR IVV Interface Screenshots Patient Using PC Our Provider EHR Interface Patient Mobile Device Provider Using PC Provider Mobile Device Key Lessons Learned • Training: Valuable to give demo/training to all providers. All providers need training on video visit functionality, EHR documentation, using new hardware (camera, headset, etc.) • Mobile Devices: Based on preliminary findings, higher success rates when patients use mobile devices (vs patients using a PC) • Readiness: Department Chief go-live before entire department training helps anchor and facilitate leadership to ease use of IVV with potentially anxious department providers. • Local Team: Support structure includes the Chief / Physician-in-Charge, DA/ADA/Supervisor, Project Manager, back office staff, local IT, local EHR support, local Call Center • Weekly Project Manager Meetings: with medical center Project Managers helps communication best practices and share learnings 25 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Please note questions on paper and we will collect and review them during the Q&A at the end of today’s session. Video Visits: Outpatient/Home Settings Leveraging Resources Across Departments & State Lines Dennis Truong MD Telemedicine Director, Physician Lead for HouseCalls, Kaiser Permanente, Mid-Atlantic States 27 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. KPMAS—Three Jurisdictions: Maryland, Virginia, DC Members hailing from Six States 580,395 Members* *As of 2/28/2015 Clinical Decision Units & Urgent Care: After-Hours, Acute Care Services Gaithersburg South Baltimore Tysons Corner Capitol Hill Largo 5 Across the Mid-Atlantic States: 29 KP Medical Office Buildings 109 Miles 29 82 Miles We’re #1!!! In Traffic Congestion …The Beltway Working 9 to 5 Reinventing the “House-Call”: KP Video Visits since August 2013 Electronic Medical Records Emergency Physicians: supporting Call Center dispositions and regional resource utilization Dr. Truong Dr. Becerra Dr. Carney Dr. Do Dr. Johnson Dr. Campbell Dr. Matthews Dr. Nicoll Dr. Patel Dr. Austin Dr. Crismon Dr. Zarrabi KP Call Center: triage and direct patients, guided by Scripts and Protocols Necessity is the Mother of Invention Each Challenge is an Opportunity What If… Delivering on the Triple Aim & Providing an Ideal Patient Care Experience in the Face of Access Constraints …We Could Grow Our Region Virtually, Offering Convenient Solutions to Patients Not Requiring an In-Person Visit Not Reinventing the Wheel Leveraging Existing Resources to Build a Seamless Remote Care Experience for Our Patients Call Center Staff CDU-to-CDU Partnerships “HouseCalls” is Born Call Center Scripts and Protocols KP Emergency Medicine Physicians Integrated Care Delivery and EMR, Leader in Technology Telemedicine: Care Along the Entire Spectrum Chronic Care Adult Primary Care Pediatric SubSpecialties General Pediatrics Behavioral Health Health Maintenance “House Calls”, CDU-toCDU Acute Care Primary Care Specialty Care Virtual Visits Offload the Busiest CDUs Before CDU-to-CDU Telemedicine South Baltimore Largo Patient with straightforward UTI symptoms arrives at Largo CDU—our busiest CDU—at peak hours, anticipating an extended, uncomfortable wait Cart complete with virtual otoscope, stethoscope After CDU-to-CDU Telemedicine • South Baltimore physician is less busy and sees that Largo CDU is very busy via the Wait Time Dashboard • Physician coordinates with Largo RN to activate CDU-2CDU to virtual help Largo volume • Physician reviews patient’s chart, orders UA, and expedites UTI diagnosis and antibiotic for pick up by patient at Largo pharmacy Pilot with Passion and a Purpose Be efficient, leveraging your existing resources Solve a problem without creating bigger problems Play the perspectives Do the right thing Please note down any questions on paper and we will collect and review them during the Q&A at the end of today’s session. Breakout Session Topics for each table will be announced. Tadashi Funahashi MD, Chief Innovation & Transformation Officer, Southern California Permanente Medical Group Mark Groshek MD, Medical Director, Digital Services Group, Colorado Permanente Medical Group Janis Ground, PT, MBA, Project Manager Virtual Care, Colorado Permanente Medical Group Jo Carol Hiatt MD, MBA, Assistant Medical Director, Southern California Permanente Medical Group William Marsh MD, Associate Executive Director, The Permanente Federation Madhu Narasimhan, Vice President, Virtual Care & Analytics Angie Stevens, Telehealth Executive Director, Virtual Care & Analytics Dennis Truong MD, Telemedicine Director, KP-Mid Atlantic States 40 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Video Visits: Inpatient Setting - Telestroke Jo Carol Hiatt MD, MBA Chair, National Product Council, Assistant Medical Director Southern California Permanente Medical Group, Business Administration 41 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Telestroke Care Kaiser Permanente Southern California Background Implementation Data Quality Review Process Recommendations 42 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. What is Telestroke? Provides the ability to rapidly assess individuals with acute neurological deficits for tPA candidacy using a two-way video tele-conferencing system – Proven through clinical trials to allow for more accurate administration of tPA than telephone consult. Program Goals: – Improve acute stroke patient outcomes – Increase appropriate tPA administration rates – Provide timely consults for our patients 24/7 In Scope – patients presenting to the EDs – Any patient with an acute neurological deficit suspicious for stroke, no greater than 4.5 hours since last known to be normal. 43 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Technology Telehealth cart and peripherals in ED Neurologist uses laptop and camera remotely 44 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. Background Received formal approval to launch internal coverage solution (using SCPMG neurologists) region-wide in Dec 2013. – Quality Committee approved pilot for 1 year starting May 2014 KP Telestroke is live in 11 of 14 EDs – Live: Anaheim, Baldwin Park, Downey, Fontana, Irvine, Ontario, Panorama City, South Bay, West LA, Woodland Hills, San Diego Moreno Valley and Riverside are utilizing Specialists On Call (SOC) for this service. Had pre-existing contract prior to regional program launch and Region wanted to stabilize prior to incorporating these sites. Los Angeles neurologists must be available for residency program. Attending neurologists utilize Telestroke to oversee residents. Currently 8 tele-neurologists – Daytime coverage (7a-7p) provided by all vascular neurologists – Evening (7p-7a) and weekend coverage provided by a mixture of vascular and general neurologists (who have met minimum educational requirements to participate in the program) Implementation Prior to go-live, implementation consisted of: – In-person kick-off meeting with all local stakeholders – Equipment training for ED staff – Mock code strokes to allow familiarity with Avizia clinical assistant, as well as train the nursing staff on how to help perform the neurological examination with the tele-neurologist Following go-live – Debrief calls to troubleshoot issues and streamline processes occurred every 2 weeks initially, followed by monthly calls – Follow-up has been demonstrated to improve and maintain shorter door to needle times 46 tPA Data and Door to Needle Time Pre/Post Telestroke Data up to 9/30/2014 for a parallel comparative time period of 13 months (10 medical centers): 47 Pre Telestroke Post Telestroke # pts given tPA 47 84 tPA ≤ 60 minutes 15.9% 52.3%: p <0.05 Mean DTN 91.3 min (SD 30.8) 71.3 min (SD 31.5) Median DTN 82 min (IQR 66.5-115.0 min) 63 min (IQR 54.8-78.3 min) p=0.0006. Abs diff 19 min Quality Review Process Each general neurologist has their first 5 cases reviewed by a vascular neurologist to ensure quality of care. After review of the first 5 cases, each general neurologist has one case per month reviewed. All neurologists participating in telestroke will have one case reviewed at each center by the local center Chief of Neurology. 48 Feedback from our ED Physicians This is a cutting ED MDs highly satisfied with service quality edge program that has established Woodland Hills as a leader in stroke care in the area I would bring my family here The program has been a if they were suffering from a possible stroke game changer … caliber/commitment to quality of the team has improved our Stroke care tremendously. This program has gone above and beyond our every expectation 49 …program has revolutionized how ED's provide critical time-dependent care. Feedback from our ED Physicians (cont.) “The telestroke program has improved the care for stroke patients at WLA tremendously. Similar to a STEMI, early recognition and expediting treatment are keys to improving patient outcomes and decreasing morbidity; however, given the wide ranging presentation of symptoms of CVA patients, recognizing the need and expediting the delivery of tPA for qualified patients had been challenging. Lack of readily available neurology and neurosurgery consultants, differing opinions regarding benefits of tPA, and limitations of telephone consults had further added to treatment delays for CVA patients. The telestroke program has overcome all these factors. Dr. Sangha and Dr. Ajani have been readily available to the WLA ED via the telestroke program – often evaluating patients via tele-medicine within minutes of patients’ arrival to the ED with CVA symptoms. The decision for tPA administration is now appropriately placed with a dedicated group of stroke neurologists, who are intimately familiar with the benefits and risks of such treatment. Lastly, Dr. Sangha and his group have also provided tremendous support for patients who developed hemorrhagic complications after receiving tPA. Overall, the telestroke program have improved the care for CVA patient at WLA tremendously. It has been great to see our organization embrace technological advances, such as telemedicine, for patient care. “ West Los Angeles 50 Please note down any questions on paper and we will collect and review them during the Q&A at the end of today’s session. Patient-Generated Health Data Mark Groshek MD Medical Director, Digital Services Group Colorado Health Connections Physicians Leads Team 52 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only. The Big Idea The Challenge The Gap Key Questions Health conditions could be more effectively co- or self-managed with information and data provided by patients themselves. If we are to improve value to consumers of health care it is critical that we enable them with tools to capture, use and share data pertinent to their health condition. Can we seamlessly integrate patient information into care processes in a way that enables individual treatment decisions and improved outcomes, regardless of where the patient is? What is Patient (Member) Generated Data? Member role in data generation Applicability to patient health Non-transactional health data is considered MGD: ▪ Health history, symptoms, biometric data, treatment history, lifestyle choices, and other information that is ▫ Created, recorded, gathered, or inferred by or from Health related Membergenerated Collected data patients or their designees To help address a health concern1 Clinical transaction data is not MGD: • Data entered as part of a care encounter • Data entered into secure emails with clinicians as free text Not healthrelated Non-member generated ▫ Qualifies as MGD? • MGD does not include: – Health plan data, data entered into forms – Member registration information • Data generated prior to enrollment by non-members is not MGD 1 Office of the National Coordinator (ONC) for HIT, Consumer Empowerment Workgroup. July 2013 How is the data generated? Active – when the member (or their designee) reports it themselves Passive – captured by a remote device (e.g. blood pressure recording, fitness device, etc…) – indirectly captured (e.g. usage patterns or affiliations on social networks) Proactive Assessment of Total Health & Wellness to Add Active Years (PATHWAAY): A comprehensive care delivery strategy for seniors receiving primary care Components: – Total Health Assessment (THA) – KP.org/Clarity + Health Trac results processing and scoring – PATHWAAY MA/RN team outreach calls for identified risks, prior to Annual Wellness Visit – Personalized Prevention Plan (PPP) – Patient-centered office visit A new workflow integrated into existing office workflows 56 PATHWAAY Workflow In Clinic Provider reviews PPP letter and Support Team note, acts on the information and/or encourages follow-up with appropriate health care staff Prior to office visit Initiate THA collection via KP.org or IVR when the visit is scheduled Collaboration: Provider hands member the printed PPP Prior to Office Visit THA responses scored, PPP letter created in EHR, and positive triggers referred to support team In Clinic Staff in clinic see message on schedule to “print PPP” and any other pre-visit needs (Orthostatic BP, PVR, Adv Directive book, etc.) Patient-centered Care Region-wide Implementation July 2012 – February 2015 56,133 Annual Wellness Visits completed 48,482 THAs completed – Roughly 1/3 each via kp.org, IVR, and in office “The PPP provokes conversations that might not happen - like falls, depression, incontinence - because the patients don't normally bring these up on their own.” KPCO Internal Medicine Physician 58 . >23,500 RN outreach calls have been made to patients with risk responses on the THA VALUE of AWV – Increased Identification & Addressing of Risk Factors Nearly everyone who triggered positive for a particular condition reported discussing the health condition with the PCP during the AWV. Many members (one-third to one-half) reported discussing these conditions with the PCP, even when the member did not “trigger” positive, inferring a preventative approach in identifying and addressing possible risk factors. % of Respondents By Positive Trigger and % Discussing Condition with PCP 100% 94% N = 74 92% 90% 80% 80% 78% 75% 60% 40% N = 89 25% 22% 20% 5% 5% 5% 3% 0% Falls Pain Urinary Incontinence % Triggering Positve for Condition on MTHA *Anxiety & Depression were reported as one trigger in the member database 59 April 20, 2015 | © Kaiser Permanente 2010-2015. All Rights Reserved. Anxiety* Depression* Frailty % Positive Trigger Discussing Condition w/ PCP Personalized Prevention Plan (PPP) BOTTOMLINE Most members recall receiving a PPP and found it easy to understand. Members, in general, keep their PPP and half had referred to it after their AWV. Members, in general, believe the PPP is valuable. % “Yes” 78% N = 119 60 April 20, 2015 | © Kaiser Permanente 2010-2015. All Rights Reserved. 14% Ext Val 52% Valuable N = 79 Impact of PATHWAAY Experience on Awareness & Confidence Participating in the PATHWAAY program resulted in an increased awareness of the actions to take to improve health. Participants also reported high confidence in their ability to make changes that would improve their health. N = 254 61 April 20, 2015 | © Kaiser Permanente 2010-2015. All Rights Reserved. Impact of PATHWAAY on Self-Reported Action to Improve Health 62 April 20, 2015 | © Kaiser Permanente 2010-2015. All Rights Reserved. Impact of PATHWAAY on Outcomes Attendance at the balance class and incontinence class increased after the classes were recommended based on the results of the THA - attendance at the classes have been sustained. There has been an increase in diagnosis and treatment of depression and anxiety among seniors since the PATHWAAY program was implemented Performance on the Medicare Health of Seniors (HOS) outcome screening has improved for falls and incontinence More detailed outcomes study is in process 63 April 20, 2015 | © Kaiser Permanente 2010-2015. All Rights Reserved. Keys to Success Patients are offered a choice of ways to complete the questionnaire digitally A new workflow was designed to support existing office workflows A supporting staff infrastructure was built to support the new workflow The information supplied by patients is actively used to engage patients and help improve their health The entire process augments the relationship between the patient and their PCP Still Working On . . . Better integration with the EHR Improved tools to automate production of the Personal Prevention Plan based on patient answers Remote Monitoring enabled by Interchange: Diabetes Management tool-kit Current state: diabetes care managers use regular telephone outreach to help bring patients with out-of-control diabetes into control. Glucose readings are manually transcribed during the call Goal: upload glucometer result digitally into a system to make it available to diabetes care managers and patients at the same time Hypothesis: diabetes care managers will require less time to provide care via telephone and so will be able to serve more patients Remote Monitoring enabled by Interchange: Diabetes Management tool-kit Glucometer Desktop Application – My Link Each member is assigned a glucometer device. A CD to install the My Link desktop application The member uses the glucometer device to take his/her blood glucose readings. The patient installs this My Link desktop application on hi/her personal computer. The patient needs to connect his glucometer to the USB of his PC to be able to automatically send all his readings to the Kaiser physician. Portal for patients Portal for Providers A patient dashboard for member access A provider dashboard for the physicians The patient logs into the patient portal to view all readings sent to Kaiser. The physician views all patients in the pilot. He/she views graphical representation of the readings along with many great features to help them track their diabetes. They can also view the individual reading of the patients thus using that information to help out the patients in a timely and efficient manner. The Nurse and the patient connect every week to go over the readings and the graphs The Nurse at her Desk at a Kaiser facility The Member at his/her home The nurse is able to view the readings of her patients on the web directly. The patient logs in with member id and password and observes his readings. She does not need to manually record the readings anymore. He no longer needs to spend hours narrating the readings to the nurse. Her readings are updated immediately upon the patient uploading their data He also observes the various graphical representations of his progress that highlight his progress and encourage him to keep on track. She can cut and paste the patients readings directly into EHR 68 April 20, 2015 Self-Tracking Affects Outcomes: A1C Pre Vs. Post of Engaged Members (1.6 avg decrease) Figure 1: Graph View We tracked A1C of the 14 most engaged patients over the course of the pilot. Figure 1 (Graph View) shows that A1C of all the patients came down after 3 months as compared to when they started the pilot, and the average A1c for the 14 patients reduced from 9.8 to 8.2 over the duration of the pilot. Remote Monitoring Improves Efficiencies: Average Call Time – Pre v/s Post 31.7% decrease in call time Note – A few users had call time similar to the pre pilot phase, as they now spent more time getting tutored from the providers. Alerts/Data Visualization Changes Behavior: No of Critical and Non-Critical Notifications during pilot The notifications go a long way in letting the diabetic patient know about what is “not right”. Legal Issues What is the expectation of the care team to respond to results that are out of range? – Data upload frequency varies from daily to just before scheduled call—alerts triggered when data is uploaded, so not available in real time – As part of normal practice, patients have been educated about how to respond to out of range values Terms and conditions specified that patients are responsible to contact Diabetes Care Manager when they receive an alert. If not already contacted, DCM does contact patient when they received an alert Legal Issues Data that is used to make or change a medical decision should be part of the electronic medical record For now, this means copying and pasting data and/or curves from the Diabetes Care System into care notes in the EHR Keys to Success It is easy for patients to upload their data Presenting the data back to patients as easily understandable information helped them improve their self care The data flows to the people in the right job role—not everything needs to land with doctors The tool augments the personal relationship patients have with their care manager Patients continue to have responsibility for understanding and managing their data and their health, and this tool helps them do it more effectively Still working on . . . Need an enterprise platform for receiving device generated data, compatible with multiple devices, or with data aggregators Integration into EHR Please note down any questions on paper and we will collect and review them during the Q&A at the end of today’s session. Q&A Please hand in all questions. 77 April 20, 2015 | © 2015 Kaiser Foundation Health Plan, Inc. For internal use only.