This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this
material constitutes acceptance of that license and the conditions of use of materials on this site.
Copyright 2012, The Johns Hopkins University and Arik Marcell. All rights reserved. Use of these materials permitted
only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided.
User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for
accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use
from third parties as needed.
Class 5 –
Clinical Interventions
380.720 – Masculinity, Sexual Behavior & Health, 2012 Qtr 2
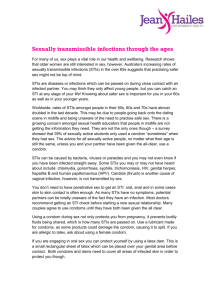
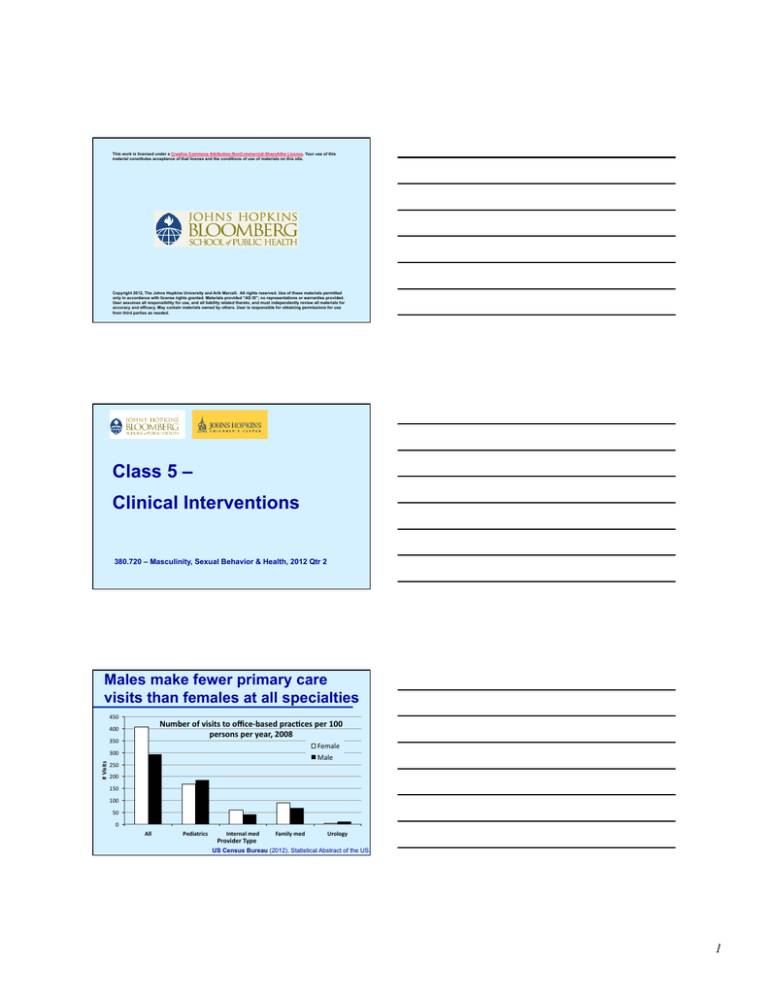
Males make fewer primary care
visits than females at all specialties
450 Number of visits to office-­‐based prac@ces per 100 persons per year, 2008 400 350 Female Male # Visits 300 250 200 150 100 50 0 All Pediatrics Internal med Provider Type Family med Urology US Census Bureau (2012). Statistical Abstract of the US.
1
Males make fewer primary care
visits than females regardless of age
100 % all office visits to primary care generalist physicians by gender & age, 2008 90 80 Female Male 70 60 % 50 40 30 20 10 0 <18 18-­‐44 45-­‐64 Total >65 <18 Peds 18-­‐44 45-­‐64 >65 <18 Internal Medicine 18-­‐44 45-­‐64 >65 Family Medicine US Census Bureau (2012). Statistical Abstract of the US.
Males make fewer number
primary care visits than females
50 Percent distribu@on of number of visits to healthcare professionals, 2007 45 Female Male 40 35 30 25 20 15 10 5 0 None 1–3 4–9 10 or more NAMCS Fact Sheets (2009). http://www.cdc.gov/nchs/ahcd/factsheets.htm#2009
Are sexually active male teens seen
in primary care?
National Longitudinal Study of Adolescent Health
• 9239 adolescents completed a survey at baseline in school
& at follow-up approximately 1.5 years later (retention
rate=71%)
• Asked at both surveys
- Sexual behavior status in past 12 months
- Physical examination receipt in past 12 months
• Study goal
- To examine whether adolescents’ healthcare use increased after
sex onset & how patterns varied by gender adjusting for
sociodemographics & access to care factors
2
Sexual behavior status over time by
teens’ annual visit data (Add Health)
• The majority of sexually
active males reported 2
visits in last year
• Among females,
visits ↑ed among all
sexual behavior
categories (p<.001),
including sexual initiators
(aOR [95%CI]=2.1[1.7-2.6])
FEMALES
MALES
• Among males, visits did not increase especially among males who
initiated sex from baseline to follow-up (aOR=1.3[0.9-1.8])
Marcell (2011). Journal of Adolescent Health. 49:47-52.
Few young men report receipt of
SRH care services
% Female
% Male
Provider report:
Assess for sexual health*
45
Client report:
Counsel on STIs, HIV, pregnancy** 61
Ever HIV test 15-44***
59
HIV test last yr among 15-44
with ≥1 risk behavior***
43
Assess/counsel on contraception
33
Counsel on condoms
18
15
34
42
34
5
7
* Lafferty (2002). American Journal of Public Health.92:1779-83.
** Burstein (2003). Pediatrics. 111:996-1001.
*** NSFG (2006-10). Special tabulations.
Questions for Discussion
• What are men’s barriers to engage in care in
general & SRH care in particular?
3
Do males want to talk about
SRH-related services?
Marcell et al. In process. 2012.
Yes: Majority of males, regardless of age, want to
talk about SRH topics with their healthcare provider
Asked about 11 SRH topics to talk to doctor
• Majority of males (84-98%) report they are willing to talk
about each topic
• Majority of males (45-86%) report they want their doctor
to bring up the topic including…
–
–
–
–
–
Decreasing STI risk
HPV/genital warts vaccine
Emergency contraception
Using condoms correctly
Female birth control methods
Marcell et al. In process. 2012.
Care Use/Seeking
Frameworks
4
Masculinity & Help Seeking
Proposed Model
A man won’t seek care if:
1. Problem is not viewed as “normative”
2. Problem is a central part of him (ego-centric)
3. If there is no opportunity to reciprocate
4. Others react in disparaging ways if help is sought
5. He feels he has much to lose if asking for help
Source: Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. American
Psychologist. 2003; 58(1):5-14.
Andersen’s Behavioral Model of
Health Services Use*
Predisposing
Factors
Enabling
Factors
Males’ Use of
Health Care
Health Behavior
Factors
Need
Factors
*Andersen R. Changing the health care system. 2000.
Positive Health
Outcomes
Predisposing Factors
Individual Level
Predisposing
Factors
- Knowledge about health & health care system
- Health beliefs & concerns
Males’ Use of
- Self efficacy
Health Care
- Skills
Contextual Level
Societal constructs
- Masculinity ideology
5
Enabling Factors
Individual Level
Personal / Family Resources
- Insurance status
- Parental (mother) involvement
Access
- Available
- Accessible (transportation)
- Accommodating (male-friendly)
- Affordable
- Acceptable
- Confidential services
Enabling
Factors
Males’ Use of
Health Care
Contextual Level
Health policies
Financing
Organizations
Other barriers/facilitators
Need Factors
Individual Level
Evaluation of needs
– Flow from an adolescents’ involvement in
health risk behaviors
Males’ Use of
Health Care
Perception of needs
– How a person views his own health state
Need
Factors
Contextual Level
Environmental needs (e.g. based on disease prevalence, etc…)
Population health indices
Stages of Change Model
Pre-contemplation
Contemplation
Maintenance
Relapse
Preparation
Action
Proschaka & DiClemente
6
Stages of Help-Seeking
STAGE 1
STAGE 2
STAGE 3
STAGE 4
Info to
significant
others
Referral
to lay
system
Referral
to medical
care system
• Denial
• Under-evaluation
• Normalization
Symptom
Perception/
Recognition
Self-medication
Self-initiated
Self-initiated
Initiated by others
Moller-Leimkuhler AM. Barriers to help-seeking by men. J Affective Disorders. 2002;71:1-9
Patient side of the equation
• To what extent is men’s health issues related to
disparities in care vs. traditional masculine beliefs?
For example
• No clear message that sexually active males should
have regular sexual/reproductive health visits
vs.
• State requirements for physical examinations to play
sports, school, work
Questions for Discussion
• Are there successful approaches to engage
men in SRH care?
- What approaches to take?
7
Males, Family Planning &
Condom Demonstration
Main question
• Are brief 1-on-1 interventions with males in clinical settings effective
in improving condom skills & SRH outcomes?
Background
• Condoms are males’ main contraceptive method *
– Reported by many young couples as primary contraception method *
• Condom failure is common**
– 31% at least 1 episode of condom breakage in last 3 months ***
– 14% at least 1 episode of condom slippage in last 3 months ***
• What is best use of clinical time?
* NSFG 2006-8
** Reece M et al. J Sex Med. 7(Suppl):266-76
22
*** Crosby RA et al. STI. 2007; 83:71-5
Systematic review
Brief clinical setting condom skill interventions with males
via demonstration/practice
• Searched Pubmed, Cinahl, PsychInfo (from 1980+) plus
hand search
• Goal
– To identify brief (<60 min) interventions involving condom
demonstrations/practice among males in clinical settings
E.g., condom-focused study or embedded within larger intervention
– Examine evidence about intervention effectiveness to
Reduce unintended pregnancy, STI/HIV incidence
Increase condom use behaviors (e.g., last sex, consistency of use)
Increase condom attitudes, knowledge, self-efficacy (e.g., skills)
23
Analytic Framework
(n=3) Clinical Popula@on Teen, adult men Heterosexual MSM SES Race/ethnicity Condom demonstra@on interven@on Q2 (n=4) Condom abtudes (n=3) Condom use self-­‐efficacy (n=5) (n=4) Q3 Other benefits Q4 Harms (n=4) Q1 (n=8) Condom Knowledge Unprotected sex Q5 STI Pregnancy Consistent condom use Condom use last sex Q1 (n=1) 8
Systematic Review
Condom Demonstration/Practice
• Abstracts identified
– From databases:
– From hand search:
8089
59
• Interventions that met inclusion criteria = 11 (12 papers)
25
Systematic Review
Condom Demonstration/Practice
Outcomes Measured
• Condom knowledge, attitudes, self-efficacy
• Condom behavior: % use; use at last sex; % unprotected sex
• Biological outcomes: STIs & pregnancy
26
Systematic Review
Condom Demonstration/Practice
Follow-Up Time Frames
• Immediate term: Same day-1 month
• Short term:
3-4 months
• Medium term: 6-9 months
• Long term:
12 months or longer
27
9
Review Results
Knowledge, Attitudes, Self-Efficacy by Follow-up Period
28
Review Results
Condom Behavior by Follow-up Period
29
Review Results
Biological Outcomes by Follow-up Period
30
10
Systematic Review
Condom Demonstration/Practice
Study limitations
• Studies mainly in STI clinics
• Lack of comparable measures across studies
• When embedded within larger intervention, not able to isolate
impact of condom demonstration from other intervention activities
• Limited assessment of pregnancy outcomes
Overview of study findings among males
• Few studies assessed condom knowledge, attitudes, self-efficacy
– Promising % change in Knowledge in short/medium term
– Mixed results for Condom Attitudes & Self-Efficacy
• Improvement in Condom Behaviors in short/medium term
• Improvement in STI rates in medium/long term
31
Provider Side of the Equation
• Providers see majority of young males during
adolescence & majority are also engaged in
sexual behavior
• Why do providers have such a difficult time
delivering effective services to patients?
Barriers to SRH care delivery
Influences at multiple levels
Individual patient level
• Lack of public health messages that sexually active males should seek care
in general or for SRH
• Access to & use of healthcare
Provider level
• Gender, specialty, year of graduation
• Training, self-efficacy in care delivery (comfort taking sexual history)
Clinic setting level
• Services not designed to meet males’ SRH needs
• Time, competing demands, financial incentives, compensation
• Decision-support tools (reminder systems) & access to internal (e.g. health
educators) or external (e.g. urology) referral resources
System level (HEDIS measures)
• No one professional organization makes recommendations for male
SRH care across lifespan
• But, guidelines alone do not ensure provider compliance*
* Solberg LI, et al. Jt Comm J Qual Improv. 2000; 26:171-88.
11
Care Delivery
Frameworks
Round 1: Key Expert Interviews
Main Goal
• To explore clinical experts’ perceptions of teen
males’ SRH needs
Marcell & Ellen. Core SRHcare to deliver to male
adolescents. Journal of Adolescent Health. 2011.
Characteristics of Key Experts, N=17
12
Clinical Expert Study:
Clinically Relevant Topics (of 237 items)
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Pubertal growth & development
Genital abnormalities, not STIs/ HIV
STI/ HIV risk reduction including testing & treatment
Sexual & gender identity &/or orientation
Sexual basics
Sexuality
Abstinence & condoms (male pregnancy prevention methods)
EC contraception & hormonal methods (female methods)
Sexual partner relationship
Parent/ peer relationship
Substance abuse/ mental health
Physical & sexual abuse
Transition to adulthood including school & work
Follow-Up Question 1.1
• How do key experts’ recommendations change
regarding SRH care delivery if needed to take into
account…
– Time to deliver service?
– Perceived effectiveness in service delivery?
13
Results
Findings – Overview
• Experts screen/assess for issues they do not
necessarily perceive to be effective
• When forced to chose, time alters SRH care
delivery choices
– From 10 of 13 topics 6 of 13 topics
• Split whether SRH care should be provided during
acute visits, with experts recommending only:
– STI/HIV risk reduction including testing/treatment
– Substance/ mental health
Engaging Young Men in SRH Care –
3-Session Study
Purpose
• To retest the effectiveness of a 3-session SRH & care curriculum
designed for young men in GED programs in NYC to increase
their use of condom & SRH care & adapted for use in Baltimore
• Setting: Youth Opportunities East Side
• Design: Quasi-experimental intervention/control (health class)
• Sessions: 3 1-hour sessions on consecutive days
• Intervention content:
- Session 1: STIs & importance to use condoms
- Session 2: Barriers to condom use (pleasure) & pregnancy
prevention; Intro to clinic through case scenario &
pictures of clinic/providers
- Session 3: Other health needs, clinic use, recap
• 99 males assigned to each group
14
Methods: Design
• 2-group quasi-experimental pretest-posttest design
– Health class served as recruitment unit
– Sequential recruitment for intervention & comparison groups
occurred over 1¼ years
• Among 223 students approached,
– 100% agreed to participate &
– 197 were enrolled (88.3% enrollment rate)
• All participants completed a baseline survey
– Intervention then administered to participants in assigned
health class
– 3 months later, participants completed follow-up survey inperson or by telephone (77% retention rate)
Methods: Intervention
• Consisted of 3 1-hour sessions
– Occurred immediately after the GED health class
– Administered on consecutive days
– Led by 2 African American male health educators
• Learning objectives included
Session 1. To identify STI symptoms & modes of transmission, STIs/
HIV can be asymptomatic, methods to avoid STI/HIV acquisition, &
STIs can facilitate HIV transmission
Session 2. To demonstrate proper condom use to prevent STIs &/or
pregnancy, ways to make condoms more pleasurable, & assist partner
use of emergency contraception
Session 3. To increase knowledge about local clinical settings & how
men get examined during a clinical encounter, & tested & treated for
Chlamydia
Methods cont.
• All participants received $15 gift certificates after
completing baseline survey
• Participants who completed the 3-month follow-up survey
received an additional $35 gift certificate
• Taking into account participant incentives & program
staffing & supplies, the cost per participant was ~$271
15
Variables
Demographic characteristics (age; race/ethnicity; grade; health
insurance; last healthcare visit)
SRH knowledge (6 items) about condoms, STIs & HIV
Healthcare knowledge (4 items)
• Awareness of place(s) can get healthcare services confidentially, for
little/no money & specific community clinics
Condom attitudes (3 items)
Sexual behavior (5 items)
• Last 3 months: had sex, # partners, how often use condoms,
lubricant use with condom
• Condom use at last sex
Healthcare behavior (2 items)
• Talk to provider about STIs/HIV, contraception
• Test for STIs/HIV
Data Analysis
• Examined baseline differences between intervention &
comparison participants on key demographic & outcome
characteristics
• Random intercept coefficient regression model accounted for
3-levels (repeated measures, individuals & classroom)
– Allows estimate of individual odds of treatment effect
– E.g., individual odds of change in study outcomes over time
among persons receiving health education curriculum compared
to persons not receiving curriculum
Singer & Willett. 2003. Applied longitudinal data analysis:
Modeling change & event occurrence. NY, NY: Oxford Press.
Results: Demographics
16
Results: Baseline
SRH Knowledge & Attitudes
Scale
Range
0 to 1
0 to 1
1 to 4
1 to 4
1 to 10
Results: Baseline
Sexual Behavior
Scale
Range
1 to 4
Results: Baseline
Healthcare Behavior
*
17
Follow-up Results: Intervention
SRH Knowledge & Attitudes
Follow-up Results: Intervention
Sexual Behavior
Follow-up Results: Intervention
Healthcare Behavior
18
Decision-Making Theory
DOMAIN-SPECIFIC
Patient
risk factors
Setting regulation^
Provider type^^
Condition
Result
Data
gathering
Provider
factors*
Utility
Output
Taking
action
Outcome
• Mortality
• Morbidity
• Cost
Setting
factors**
Tradeoff
Taking
Theory of Planned Behavior
action
Setting
factors**
Tradeoff
Provider Factors
Feeling about behavior
Behavioral beliefs
Others expectations
External
Factors
Others behaviors
Control beliefs
Efficacy beliefs
Attitudes
• Experiential
• Instrumental
Perceived Norm
• Injunctive
• Descriptive
Personal Agency
• Perceived control
• Self efficacy
Knowledge &
skills
Salience
Behavioral
intention
Behavior
• Data gathering
• Taking action
**Setting
constraint
Habit
Tension Inherent in Male SRH Goals
in the Clinical Setting
• SRH guidelines are broad vs.
• Applicability in clinical setting &
• Real world constraints, including…
–
–
–
–
–
–
Time available to spend with a patient
How effective it is to deliver the service
The prevalence of the issue
Provider reimbursement
Training of the provider
How services are organized at the setting (e.g. reminder
systems, etc…)
– Providers do not keep up with clinical guidelines
19