Annual Quality Account 2012-2013 North Tees and Hartlepool Leading Into 2013-14
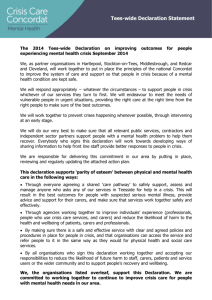
advertisement

North Tees and Hartlepool NHS Foundation Trust Annual Quality Account 2012-2013 Leading Into 2013-14 Annual Quality Account 2012-2013 Leading Into 2013-14 Our approach to Quality: an Introduction to this Annual Quality Account from the Chief Executive The Trust is pleased to present our annual Quality Account to demonstrate our continued commitment to delivering high quality patient care. Whilst there has been continued publicity about the quality of care provided to some patients in hospitals in England and Wales over the last year, I am always pleased to receive excellent feedback from our patients and their relatives across both the community and hospital services we deliver, which demonstrate to me that we strive to ensure that our patients receive high standards of clinical care, delivered by caring, compassionate staff. I am particularly pleased that patients have rated our hospitals as 4.5 to 5 star services on NHS choices (January 2013); the average score across the North East is 3.5. Despite the challenging economic climate during 2012-2013, we remain committed to maintaining quality and protecting frontline teams. We have continued to invest in, and expand our training and development opportunities to provide staff with the skills, technology and knowledge they need to meet the needs of patients and their families. This, our third combined community and hospital service Quality Account, demonstrates some of the actions we have taken during 2012-2013, and highlights actions we will be taking over the forthcoming year to ensure our continued commitment to ensuring and continuing to monitor and improve quality of care and patient experience. Our quality strategy and our Quality Account indicate our priorities for the coming year. These have been developed with patients, carers, staff, governors, commissioners and with key stakeholders including health scrutiny committees, local involvement networks (LINks) and healthcare user groups. We believe and commit to Putting Patients First by making patient safety and experience our number one priority every day. 2 Annual Quality Account 2012-2013 Contents: Part 1: Part 1 Statement on Quality from the Chief Executive Part 2: Part 2A Performance against quality improvements priorities for 2012-2013 Part 2B Quality improvement priorities for 2013-2014 Part 2C Statement of Assurance from the Board Part 3: Part 3A Trust performance against additional Quality Performance Indicators Part 3B Performance from key national priorities from the Department of Health Operating Framework, Appendix B of the Compliance Framework Part 3C Department of Health Core indicator set Annex 1 Third Party Declarations Annex 2 Statement of Directors’ responsibilities in respect of the Quality Account Annex 3 Independent Auditor’s Limited Assurance Report to the Council of Governors Glossary Definition of some of the terms used within this document 3 Annual Quality Account 2012-2013 Part 1: Statement on Quality from the Chief Executive Our quality pledge In 2008, our Board and our staff pledged patient safety and experience as their number one priority supported by our corporate strategy. Our continued commitment to improving the quality of our care and service quality for our patients remains our number one priority. It is prevalent at every level of our organisation and is generating excellent performance results. Our Board of Directors receive and discuss quality, performance and finance at every Board meeting. We use our Patient Safety and Quality Standards (PS & QS) Committee and our Audit Committee to assess and review our systems of internal control and to provide assurance in relation to patient safety, effectiveness of service, quality of patient experience and to ensure compliance with legal duties and requirements. The Patient Safety and Audit Committees are each chaired by non-executive directors with recent and relevant experience, these in turn report directly to the Board of Directors. The Board of Directors seek assurance on the Trust’s performance at all times and recognise that there is no better way to do this than by talking to patients and staff. During 20122013, members of the Board of Directors undertook a night-time review of services. These unannounced visits, at both our hospitals, enabled members of the Board to witness for themselves how well our staff manage patient care during the out-of-hours period. This approach of unannounced visits at varied times will continue during 2013-2014. Quality standards and goals Values, standards and goals The Trust greatly values the contributions made by all members of our organisation, to ensure we can achieve the challenging standards and goals, which we set ourselves in respect of delivering high quality patient care. The Trust also works closely with commissioners of the services we provide to set challenging quality targets. Achievement of these standards, goals and targets form part of the Trust’s four strategic quality aims. Listening to patients and meeting their needs We recognise the importance of understanding patients’ needs and reflecting these in our values and goals. Our patients want and deserve excellent clinical care delivered with dignity, compassion, and professionalism and these remain our key quality goals. Over the last year we have once again spoken with over 1,000 patients. We have spoken to them in their own homes, in community clinics and in our inpatient and outpatient hospital wards and departments. We always ask patients how we are doing and what we could do better. We understand from patients that great healthcare is defined in the way that we treat patients, family members, carers and staff. As a result of this we continue to promote our RESPECT nursing and midwifery strategy, which was developed by staff, patients, governors and stakeholders. 4 Annual Quality Account 2012-2013 The strategy encompasses the fundamental elements of what we believe underpins great patient care. These are: Responsive Timely Equipped Patients Carers Staff Care and Compassion Safe and Secure Evidence Based Person Centred Achievements Unconditional CQC Registration During 2012-2013 the Trust met all standards required for successful and unconditional registration with the Care Quality Commission (CQC) for services across all of our community and hospital services. 5 Annual Quality Account 2012-2013 Finalists for HSJ Awards We were particularly pleased to be the only trust in the country to win two National Nursing Times Awards as well as a regional award in 2012: Winner, 2012 Nursing Times Infection Control Award A health economy approach to reducing Clostridium difficile supporting care homes to reduce environmental contamination. Winner, 2012 Nursing Times Respiratory Nursing Award Chronic Obstructive Pulmonary Disease (COPD) prognostic index to facilitate end of life discussions in primary care; listening to patients. We also won the regional award in 2012 for: Winner, Regional Bright Ideas Award Homeward orthopaedic team Patients who identify a problem with a hip replacement will receive a telephone call and advice or an outpatient’s appointment if clinically appropriate. Governance Ratings All NHS Foundation Trusts are subject to assessment by Monitor against their compliance framework. During 2012-13 we continued to achieve high outcomes for our standards of clinical care; however the Clostridium difficile target remained a significant challenge and we did not achieve this. Section 3 describes actions we have taken to manage this. Our positive patient safety culture, actions and behaviours have continued to deliver results by improving the safety and quality of care we deliver. Working in the spirit of shared learning, by communicating with our colleagues and stakeholders, the benefits of this work have been recognised nationally and internationally. Several of our clinicians and clinical teams have been featured in journals, conferences, or won prestigious awards over the last year. 6 Annual Quality Account 2012-2013 Introduction to Parts 2 and 3 of our Quality Account Part 2 of our Quality Account indicates our priorities for the future and Part 3 demonstrates and reviews our performance over the past year. This Quality Account allows us to demonstrate our commitment to continuous, evidence-based quality improvement; to draw your attention to the standards achieved and the progress we have made; and to describe the approach we intend to continue improving our services to patients. It enables you the opportunity to assess the quality of our performance across the healthcare services we offer. Chief Executive Alan Foster MBE visits the Single Point of Access team. Alan is pictured with (left to right) Amanda Dunn, Tracy Robinson, Carole Storm, Angie Hewitson and (front left to right) Ann Wise and Sam Wharam The areas we have chosen as our quality improvement targets for 2013-2014 have once again been set following consultation with our Council of Governors, local health scrutiny committees, local involvement networks, healthcare user group, our commissioners and importantly, by talking to staff, patients and carers. Progress described within this document is based on data and evidence collected locally and nationally, much of which is presented as part of our performance framework each month and in our public board meetings, Council of Governors meetings and to our commissioners. To the best of my knowledge the information given in this document is accurate. Alan Foster MBE Chief Executive 7 Annual Quality Account 2012-2013 Part 2A: The 2012-2013 quality improvement priorities In our 2011-2012 Quality Account, we identified a number of quality improvement priorities that patients, staff and stakeholders agreed we should focus on over the last year: Priority 1, Patient safety: reduce deaths and prevent deterioration; Priority 2, Effectiveness of Care: clinical documentation and communication; Priority 3, Patient experience: care with compassion. Our progress against the above and the action plans for each of them have been regularly monitored via key quality committees, the Board of Directors and the Council of Governors. Progress is described in this section for each of the 2013 priorities. The outcomes reported in Part 3A are those that were requested and agreed with external and internal stakeholders during consultation. We would like to thank our stakeholders for their continued engagement and involvement in not only setting our quality priorities but also in reviewing progress during the year. We would like to acknowledge the hard work and commitment of our staff, both clinical and non-clinical across all healthcare settings. It is their hard work and dedication to putting patients first that delivers positive results. Priority 1 patient safety: reducing mortality In 2008 the Trust, in partnership with external and internal stakeholders agreed that its first priority should be to reduce mortality. Through our quality strategy, we set out a five year plan to achieve this. Patient safety remains the first priority of every member of staff from ward to board. Our first patient safety priority identified by external and internal stakeholders as well as well as our staff was to reduce the number of patients that die in our hospitals. This year we continued to reduce opportunity for avoidable deterioration at home or in hospital. Some of our ambitions for 2012-2013 were more complex than anticipated and took us longer than expected to achieve. For example, developing an early warning score for use by community nurses took longer than expected because we had to develop and test a new product before we could introduce it for use by community staff. Our community team developed a process for identifying patients at risk of deterioration at home through the use of Telehealth. During the last year we have collected data which identifies the contribution that this assistive technology makes, in conjunction with skilled clinical support, to safely care for patients in their own home. Why/How we chose this as a priority: Reducing mortality has been a key priority since 2008. We have been reporting on our progress to external and internal stakeholders, for example to our commissioners, Council of Governors, to health scrutiny committees and to local involvement networks. During the consultation, Priority 1, everyone agreed that this must remain our number one priority. Stakeholders also asked that we develop a process that can be used in patients' own homes to prevent escalation to hospital for patients with chronic conditions where appropriate. 8 Annual Quality Account 2012-2013 What we said we would do: Reduce deaths and prevent deterioration Monitoring patient safety; mortality Rationale: Staff, patients and key stakeholders agreed that reducing mortality ratio should continue to be our first patient safety objective. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will undertake monthly mortality reviews using the global trigger tool. • Use of the Dr Foster mortality database which predicts the number of deaths that should be expected in our hospital based upon local demographic information and case mix. • Dr Foster mortality data to be presented at every public meeting of the Board of Directors. • Reported at every Public Board of Directors meetings. ✔ • Reported at every Council of Governors meeting. ✔ • Over 961 sets of observation charts reviewed. ✔ • Reported HSMR, SHMI and Crude Mortality Rates. ✔ • Audits of Early Warning Score (EWS) undertaken. ✔ • Senior doctors and nurses will continue to review clinical incidents on a weekly basis. • Mortality data to be presented to the Council of Governors on a quarterly basis. • Monitoring Dr Foster data every month to track our progress against our target. • Review the CHKS data supplied by the North East Quality Observatory System to benchmark mortality in our Trust against other Trusts in the North East. • Monitor management of the deteriorating patient by reviewing observation charts on at least 50 patients every month. As can be seen below, the outcome of Priority 1 was achieved. The following evidence provides more detail to demonstrate / support these trends. The Trust continues to monitor all mortality data including raw mortality data (all actual deaths) weekly as well as looking at monthly and quarterly trends. This data is benchmarked regionally and the overall trend remains positive. Dr Foster reporting period of February 2012 to January 2013 (rolling 12-month period of latest data) - Mortality (in-hospital) measures the Trust as 103.70 against the national average of 100. The following chart details the reporting period of February 2011 to January 2012 against the most recent time period available in Dr Foster (February 2012 to January 2013). Mortality Benchmarking against peer group 120 100 80 60 40 20 0 Northumbria Healthcare NHS Foundation Trust South Tees North Tees and Hospitals NHS Hartlepool NHS Foundation Foundation Trust Trust Feb11-Jan12 Relative Risk Gateshead Health NHS Foundation Trust South Tyneside County Durham City Hospitals The Newcastle Sunderland Upon Tyne NHS Foundation & Darlington NHS Foundation NHS Foundation Hospitals NHS Trust Trust Trust Foundation Trust Feb12-Jan13 Relative Risk National Avergae NB: Data obtained from Dr Foster 9 Annual Quality Account 2012-2013 Dr Foster reporting period of February 2012 to January 2013 (rolling 12 month period of latest data) – Hospital Standardised Mortality Ratio (HSMR) measures the Trust as 102.72 against a national mean of 100. The following chart details the reporting period of February 2011 to January 2012 against the most recent time period available in Dr Foster (February 2012 to January 2013). HSMR Benchmarking against peer group 120 100 80 60 40 20 0 South Tees Hospitals NHS Foundation Trust Northumbria North Tees and Healthcare NHS Hartlepool NHS Foundation Foundation Trust Trust Feb11-Jan12 Relative Risk Gateshead Health NHS Foundation Trust County Durham City Hospitals South Tyneside The Newcastle & Darlington Sunderland Upon Tyne NHS Foundation NHS Foundation NHS Foundation Hospitals NHS Trust Trust Trust Foundation Trust Feb12-Jan13 Relative Risk National Avergae NB: Data obtained from Dr Foster Hospital Standardised Mortality Ratio (HSMR) The following HSMR graph demonstrates the Trusts Relative risk throughout the reporting period (February 2012 to January 2013) (rolling 12 month period of latest data). The Trusts yearly average for Relative Risk is currently 103.00, which is slightly above the national average of 100. The following chart shows the Trusts historical position with the most upto date available data. Relative Risk 150 125 100 75 50 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan 2011/12 2012/13 Trend (Month) Relative Risk *Data taken from Dr Foster 10 Annual Quality Account 2012-2013 National Average Hospital healthcare - evidence in practice Reduced cardiac arrests A cardiac arrest is what happens when a patient’s heart stops. We believe (and the evidence supports) that this reduction is linked to a reduction in the number of patients that deteriorate whilst in our care. During 2012-13 the Trust has experienced unprecedented numbers of very sick patients being admitted to hospital. Although this inevitably results in more patients having a cardiac arrest, we are pleased that we are sustaining very low numbers of patients who show signs of deterioration prior to their cardiac arrest, which is demonstrated in the tables below. Cardiac Arrests Deteriorating Physiology Apr - Jun 2012 Jul - Sept 2012 Oct - Dec 2012 Jan - Mar 2013 Total 34 21 31 34 120 2 5 6 12 25 Number of cardiac arrests Deteriorating physiology prior to cardiac arrest There were 120 cardiac arrests during this period, 25 had signs of deteriorating physiology prior to cardiac arrest, which equates to 20.83%. A full Root Cause Analysis (RCA) has been undertaken in relation these cases to ensure that there was a clear understanding of events that led up to cardiac arrest. Multi-professional teams review RCAs from all patients who have sustained cardiac arrests. Cardiac Arrest Comparisons 45 40 35 30 25 20 15 10 5 0 Apr - Jun Jul - Sept 2010-2011 Quarter/Year Oct - Dec 2011-2012 Jan - Mar 2012-2013 Apr-Jun Jul-Sep Oct-Dec Jan-Mar Totals 2010 - 2011 22 28 38 41 129 2011 - 2012 29 12 28 22 91 2012 - 2013 34 21 31 34 120 11 Annual Quality Account 2012-2013 Infection Control Rationale: Key stakeholders asked us to report on clostridium difficile (C diff) because we did not achieve a reduction in 2012-2013. Trust commissioners and clinicians also asked that we report on e-coli infections. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • Staff training will be monitored. • We will monitor rates of C diff. • The number of e-coli infections will be reported. • Reported at every Public Board of Directors meetings. ✔ • The number of e-coli infections will continue to be reported. • At every public board and council of governors meeting. • At quarterly IPC committee. • Reported at every Council of Governors meeting. ✔ • Discussed in detail at Audit Committee and Directorate meetings. ✔ • Reported in detail to Monitor. ✔ • Two external reviews undertaken at the Trust request. ✔ • Unannounced Prevention Protection Control practices undertaken. ✔ • Did not achieve the 2012-13 C diff target of 44 cases. ✘ • Every hospital acquired C diff and e-coli infection will be investigated to establish cause and actions required. • We will report any trends and actions. • At meetings with our commissioners. Clostridium Difficile (C diff) During 2012-2013 we did not achieve our C diff target. We continued to work hard to control and reduce opportunity for infections to spread when we treat people in our clinical premises or in their own homes. There is no one way in which C diff can be eliminated but a consistent approach across the important areas of cleanliness of the environment; appropriate antibiotic prescribing and strict hygiene at the point of care are vigorously pursued. We continue to invest in new equipment, which is easier to clean, and which is less likely to harbour infections. An independent review of infection prevention and control policy and practice in the Trust was carried out in August 2012, and recommendations were made to further enhance antibiotic prescribing, stewardship, and audit of time to isolate. An action plan was developed in response to the review, and has been presented to both the Board of Directors and Council of Governors. Our hygienists continue with a programme of deep cleaning and fogging with hydrogen peroxide, which has been found to kill the spores responsible for people getting C diff. The work has also been extended to our local care homes as part of a project to reduce recurrent infections and improve patient experience. The Trust won a Nursing Times award for this innovative and collaborative work. The directors responsible for infection prevention and control and for estates and facilities, undertake regular walkabouts to provide support to staff and assurance to the Board of Directors that any environmental issues are dealt with speedily and effectively. 12 The Trust has undertaken a comprehensive review in relation to C diff. Whilst recognising that number of C diff reported by the Trust is higher than other Trusts, it is of interest to note that it also sends a higher proportion of samples for testing. Annual Quality Account 2012-2013 The national Health Protection Agency inclusion criteria for reporting C. difficile infections is as follows: Any of the following defines a C. difficile infection case in patients aged 2 years and above and must be reported to the HPA: 1. Diarrhoeal stools (Bristol Stool types 5-7) where the specimen is C. difficile toxin positive; 2. Toxic megacolon or ileostomy where the specimen is C. difficile toxin positive; 3. Pseudomembranous colitis revealed by lower gastro-intestinal endoscopy or Computed Tomography; 4. Colonic histopathology characteristic of C. difficile infection (with or without diarrhoea or toxin detection) on a specimen obtained during endoscopy or colectomy; 5. Faecal specimens collected post-mortem where the specimen is C. difficile toxin positive or tissue specimens collected post-mortem where pseudomembranou . How did we do? In 2012-2013, we had a challenging C diff target set by our commissioners, which we did not achieve. Over the last few months of the year we were able to bring our rate down, however, the larger numbers in the second quarter of the year resulted in our breaching the end of year target. The following table identifies the numbers of hospital acquired C diff cases reported by the Trust against the target for that period. The table also identifies the number of community acquired cases of clostridium difficile reported by our laboratory. Quarter Q1 Q2 Q3 Q4 Target for hospital acquired cases 15 15 8 6 Number of hospital acquired cases 11 23 13 14 Number of community acquired cases (acquired in people’s own homes) 17 34 23 21 North East Trusts stool specimens examined and tested for C diff. Trust 1 Total No. stool specimens examined C diff toxin tests % of C. diff toxin tests V examined Trust 2 Trust 3 North Tees and Hartlepool NHS Foundation Trust Trust 5 Trust 6 2011 2012 2012 2012 2012 2013 Apr -Jun Jul Sept Oct -Dec Jan Mar Apr -Jun Jul Sept Oct -Dec Jan Mar 1,536 1,666 1,554 1,609 1,582 1,718 1,730 918 842 872 904 896 857 969 59.77 50.54 56.11 56.18 56.64 49.88 56.01 Total No. stool specimens examined 3,329 4,913 6,848 5,664 5,530 5,342 5,563 1,389 1,307 1,829 1,539 1,547 1,276 1,602 % of C. diff toxin tests V examined 41.72 26.60 26.71 27.17 27.97 23.89 28.80 Total No. stool specimens examined 1,299 1,419 1,269 1,263 1,230 1,237 1,518 C diff toxin tests 110 102 91 101 109 91 92 % of C. diff toxin tests V examined 8.47 7.19 7.17 8.00 8.86 7.36 6.06 Total No. stool specimens examined 2,030 2,167 2,218 2,658 2,386 2,627 2,664 C diff toxin tests 1,035 1,053 1,184 1,312 1,108 1,395 1,349 % of C. diff toxin tests V examined 50.99 48.59 53.38 49.36 46.44 53.10 50.64 Total No. stool specimens examined 3,003 3,056 2,581 2,834 2,638 2,659 2,862 C diff toxin tests 1,613 1,501 1,228 1,344 1,268 1,030 1,271 % of C. diff toxin tests V examined 53.71 49.12 47.58 47.42 48.07 38.74 44.41 Total No. stool specimens examined 2,260 2,714 2,358 2,626 3,169 3,132 3,241 706 666 612 741 737 585 664 % of C. diff toxin tests V examined 31.24 24.54 25.95 28.22 23.26 18.68 20.49 Total No. stool specimens examined 1,895 2,048 1,927 2,109 1,973 No Data No Data 270 317 270 253 255 No Data No Data C diff toxin tests Trust 8 2011 C diff toxin tests C diff toxin tests Trust 7 2011 % of C. diff toxin tests V examined 14.25 15.48 14.01 12.00 12.92 - - Total No. stool specimens examined 4,059 5,466 3,746 4,314 4,224 3,792 4,472 C diff toxin tests 1,099 1,068 1,149 1,339 1,498 1,210 1,526 % of C. diff toxin tests V examined 27.08 19.54 30.67 31.04 35.46 31.91 34.12 To note: Quarter 4 (Jan-March 2013) data not available at time of print. Data obtained from Health Care Acquired Infection (HCAI) data capture system administered by Public Health England. Annual Quality Account 2012-2013 13 The following table shows the number of C diff cases that have been confirmed each month for each North East Trust. 2012/13 Apr May Jun Q1 Quarter Jul Aug Total Sep Q2 Quarter Oct Total Nov Dec Q3 Quarter Jan Total Feb Mar Q4 Quarter Year Total Total Trust 1 1 3 6 10 8 3 3 14 4 8 6 18 0 7 8 15 57 Trust 2 5 5 8 18 6 4 4 14 8 6 3 17 3 4 9 16 65 Trust 3 2 1 2 5 3 0 1 4 3 6 2 11 1 0 5 6 26 North Tees and Hartlepool NHS Foundation Trust 0 5 6 11 9 9 5 23 3 6 4 13 7 5 2 14 61 Trust 5 6 8 8 22 0 2 8 10 6 4 3 13 1 2 5 8 53 Trust 6 3 6 7 16 5 1 4 10 2 8 4 14 5 0 3 8 48 Trust 7 1 0 1 2 2 0 1 3 1 1 0 2 0 0 0 0 7 Trust 8 7 8 6 21 7 8 6 21 7 6 3 16 4 8 4 16 74 Monitor, our regulator has reviewed actions taken by the Trust and (at the time of writing) is also satisfied that the Trust has done and continues to do all that we can to reduce opportunity for patients to acquire C diff whilst in hospital. Monitor continues to review the position. The trend in hospital acquired C diff over the last six years can be seen in the following table: Year 2007-2008 Clostridium difficile 210 2008-2009 158 2009-2010 2010-2011 136 53 2011-2012 2012-2013 68 61 The numbers of E-coli reported across the community and our hospitals during the year are presented below. When compared against the 2011-12 figures, it is clear that there needs to be continued engagement with Primary Care. Hospital acquired E-coli Community acquired E-coli Apr 11 to Mar 12 Apr 12 to Dec 13 41 31 149 194 Monitoring patient safety Rationale: stakeholders were pleased that we managed to develop an early warning status tool in the community. They wanted to understand the impact of this over a period of time. Community Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will roll out use of the new community early warning status allied to Telehealth status tool to more areas. • Monitor admissions to hospital. • Quarterly reports to the IPNMB. • Quarterly Reports to IPNMB. ✔ • Number of alerts monitored. ✔ • Number of red alerts from patients on Telehealth use monitored. ✔ • Number of red alerts from patients managed at home. ✔ • Number of patients with red alerts admitted to hospital. ✔ 14 Annual Quality Account 2012-2013 Community healthcare - evidence in practice Development and use of bespoke Telehealth early warning status (EWS) tool for use in community services. We could find no nationally developed early warning status for use in community settings. Our community staff therefore tested the hospital EWS tool for use in the community. The hospital EWS did not work in the community, therefore some staff developed and tested their own system linked to Telehealth. The community EWS track and trigger tool measures patient blood pressure, temperature, pulse and oxygen levels and a trigger (of worsening condition) results in a speedy review of medication and care. The system supports real-time flow of information from patient to clinical staff, supporting continuous evaluation of care needs, risks and appropriately timed interventions. We believe that the system designed by staff will help avoid crisis or deterioration resulting in a need for unscheduled care (unplanned intervention or admission to hospital). The key measurable benefits to patients using this tool include: •Supported early discharge; •Improved confidence because patients know that their condition is being closely monitored; •Rapid response to any change in worsening condition; •Improved clinical risk management for a group of patients known to a service; •Fewer unplanned admissions or readmissions to hospital; •Convenience and comfort of being monitored at home. The Telehealth EWS track and trigger tool was implemented in December 2011, with baseline outcomes being measured and reported in the 2012-2013 Quality Account and Report. Introduction and early success of this ground-breaking work has resulted in our staff aim of developing a virtual ward in the community being achieved. Yes 2 192 Yes ➜ N/A 359 Yes ➜ 58 408 Yes ➜ 30 288 Yes ➜ 15 191 Yes ➜ 119 303 Yes ➜ 68 302 Yes ➜ 44 244 Yes 49 246 Yes ➜ 9 263 Yes ➜ 188 26 25 3 June 22 22 2 July 19 19 0 August 64 ➜ 3 May 64 58 September 45 45 30 October 39 39 15 November 28 28 119 December 0 N/A 68 January 0 ➜ N/A 44 February 7 ➜ ➜ 3 7 49 March 9 ➜ Yes 23 ➜ 201 23 ➜ 3 April ➜ Q4 Green alerts ➜ Q3 Number managed at home ➜ Q2 Amber alerts ➜ Q1 Number managed at home ➜ Red alerts ➜ Summary of community EWS alerts: 9 38 Was the response within 2 hours? 15 Annual Quality Account 2012-2013 Telehealth Case Study The Trust’s telehealth services when used in the right setting, with the right support continues to improve the lives of people with complex long-term conditions, and supports them to manage their health and care. The following case study provided by the specialist heart failure nurse gives insight into both patient and clinician experience of using telehealth. David is a 43 year old gentleman who was admitted to hospital in March 2012. During his stay he was diagnosed with cardiomyopathy and heart failure (cardiomyopathy refers to heart muscle disease). I first met David the following day and found him to be very anxious and distressed regarding his diagnosis. I spent a lengthy visit giving explanations and reassurances regarding his forthcoming management. I called back to see him as agreed and found that he had been back into hospital for an overnight stay after experiencing breathlessness and palpitations. All of his cardiac investigations were stable. In the subsequent days David contacted me about four times each day mainly needing reassurance. He also attended the One-Life Centre (minor injuries unit) on two other occasions. A telehealth unit was installed later that month and David was taught how to use it and how it would be checked. In the first two days he had two red flags due to bradycardia (slow heart rate). David had the telehealth service in place for six weeks. However, after four weeks he felt much better and did not need it. David was able to go out every day walking and is looking forward to returning to work. David had no further admissions to hospital or the One-Life Centre and has since returned to full-time employment with routine six monthly checks from the heart failure team. David stated that using the system had been a very positive experience and that it allowed him to feel assured that he was being checked regularly and that any problems would be acted upon quickly. Community nursing team in Billingham. 16 Annual Quality Account 2012-2013 Priority 2 effectiveness of care; clinical documentation and communication Patients and stakeholders said that they would like us to listen to patients and to provide opportunities for concerns to be heard and acted on in a timely way. In the past year there have been a number of high-profile reports that have drawn attention to examples of poor standards of healthcare. One such report is the Mid-Staffordshire Inquiry, outlining the poor provision in attending to patients’ needs. A copy of the Francis Report can be found on: www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/ digitalasset/dh_113447.pdf The most recent report which includes 290 recommendations can be found at: www.midstaffspublicinquiry.com/report In order to challenge and prevent poor practice, North Tees and Hartlepool NHS Foundation Trust have implemented Intentional Rounding. Intentional Rounding provides an opportunity for our nurses to pick up and address any issues or concerns our patients and visitors have in a timely way. Through communicating with patients and relatives, Intentional Rounding should provide confidence and reassurance in a calm and orderly environment. This is in line with both our Trust RESPECT strategy, and the national 6c’s nursing and midwifery strategy. Patient Stories As part of the Trust commitment to listening to our patients, a number of DVDs have been undertaken and subsequently shared with doctors and nurses during formal and informal teaching sessions. These stories are told by patients who have had experiences they wish to share. As part of this listening experience we have also undertaken a number of written patient stories for those patients who do not want to appear in a DVD but still want their story told. 17 Annual Quality Account 2012-2013 What we said we would do: Improve quality of documentation and communication Communication: Rationale: stakeholders said they would like us to continue to listen to patients and provide improved opportunities for concerns to be heard and acted on. Staff believe that Intentional Rounding will provide an opportunity to understand and act on patient needs in a timely way that is meaningful to them. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will roll out Intentional Rounding to listen to what patients and relatives have to say about standards of care and experience. • We will monitor what we are told and take actions to address any concerns. • Ward/department leaders will feedback daily results of Intentional Rounding to their staff. • Although we have implemented Intentional Rounding across the Trust, we are unable to demonstrate daily feedback happens in all areas. ✘ • Themes of compliments and concerns have been reported to IPNMB, at directorate meetings and at Trust Director Group (TDG). ✔ • There was no method of capturing this data therefore the Trust has developed a way of doing this. ✔ • We continue to report learning from complaints and incident trends locally, regionally and nationally to PS & QS. ✔ • We will continue to ask patients about their experience of clinical care and experience during our PEQS (patient experience and quality standards) reviews. • We will record the results of PEQS reviews. • We will monitor and report the impact of this on complaints relating to nursing. • Themes of compliments and concerns will be reported to the Integrated Nursing and Midwifery Board six-monthly. • Complaints relating to nursing communication will be reported to the Integrated Nursing and Midwifery Board six-monthly. • Complaints and Patient Advice and Liaison (PALS) trends are reported quarterly to the Patient Safety and Quality Standards Committee. Hospital healthcare – evidence in practice Intentional Rounding was introduced to enhance the quality of communication and emotional support to patients and carers. It was initially introduced into Maternity services with excellent results; within three months complaints in relation to Midwifery care had reduced by 55%. Intentional Rounding was subsequently rolled out to all inpatient areas. This is not yet firmly embedded but there are a number of good practices seen, including the fact that a number of clinical areas document Intentional Rounding in the patients contemporaneous notes. The Board of Directors have commenced regular unannounced reviews of care, which is a good example of corporate Intentional Rounding. Our continued success with the PEQS reviews provides additional opportunity for senior nurses to undertake adhoc Intentional Rounding. Over the year, during our scheduled PEQS reviews, our senior nurses, Governors and Directors visited 224 wards and departments in our hospitals, speaking to 961 patients and/or relatives as well as reviewing standards in community clinics and in patients own homes. 18 Annual Quality Account 2012-2013 The following table provides data relating to 2011/2012 and 2012/2013 visits: 2012-13 Wards Visited 209 224 Patients Seen 777 961 Yr on Yr Comparison ➜ ➜ 2011-12 15 184 In 2012 the Trust developed a comprehensive PEQS database, to record all reviews and enable detailed analysis and provide trends for each area and ward. This enables them to monitor and share good practice and provide support where needed. Reports from PEQS reviews are provided to both the Board of Directors and the Council of Governors. The Board of Directors have visited the hospitals at night to review standards of care and to derive assurance that standards remain high no matter what time or day patients are treated in our hospitals. Commissioners have also undertaken an unannounced night time review with positive feedback. The following table reflects the comparisons between 2011-12 and 2012-13 PEQS data for the three key areas in respect of the Trust's hospitals: 2012-13 (%) First Impressions 91 85 Nursing Evidence 90 87 Patient Experience 98 96 Yr on Yr Comparison (%) ➜ ➜ ➜ 2011-12 (%) 6 3 2 Community PEQS The following table reflects the comparisons between 2011-12 and 2012-13 for the Community PEQS Scores. In 2012-13 there were 48 patient homes visited. 2012-13 (%) First Impressions 98 100 Nursing Evidence 77 90 Patient Experience 95 100 Yr on Yr Comparison (%) ➜ ➜ ➜ 2011-12 (%) 2 13 5 19 Annual Quality Account 2012-2013 Detail of the impact of the improvements linked to Priority 2 are demonstrated further below: Hospital healthcare – evidence in practice The way we captured information within the complaints department meant that we were unable to disaggregate nursing complaints. Therefore a nursing dashboard has been developed to support the capture and reporting of this information more effectively. Overall patients tell us that they are satisfied with communication In 2012-13 our Governors and non-executive board members spoke to 961 patients to ask amongst other things, whether our healthcare professionals communicate well with them. They were asked if they understood what the plan of care is and whether they have been involved in decisions about them with staff communicating in a way they understand, using language they understand. Patients and relatives were asked if they knew what their medications are for and if they knew what tests they are having and why. They were also asked if our staff treat them with dignity and respect, with kindness and compassion and whether or not they would recommend our Trust. 94.46% of the 961 patients spoken to reported that they were satisfied with quality of communication and 97.89% reported that they were always treated with dignity and respect. 97.19% of patients interviewed reported that they would recommend the ward or department they were being treated on. These questions continue to be asked on a regular basis and whilst recognising that we don’t get it right every time, we have learned from these reviews as well as from the national survey that patients are satisfied with the following aspects of communication: •We are involving people in decisions about their care; •People can find someone to talk to about their worries and fears; •Patients believe they are given enough privacy when discussing their condition or treatment; •Although we score well when compared to Trusts nationally in relation to telling people about the medication side-effects to watch out for when they go home, there are still improvements we can make; •Our patients gave us a good score when they were asked if they knew who to contact if they were worried about their condition. The National Cancer Patient Survey reported that 72% of patients felt they could discuss worries or fears with staff during visits, placing us in the top 20% nationally. We were also in the top 20% nationally in giving the patient enough emotional support (84% up from 77% in 2010). Trends over three years can be seen in the table below (data taken from the latest national inpatient survey used for CQUIN). 20 Annual Quality Account 2012-2013 82.7 82.6 63.9 71.0 ➜ 79.3 59.1 ➜ ➜ Were you given enough privacy when discussing your condition or treatment? ➜ 59.9 73.6 2012 ➜ ➜ Did you find someone to talk to about worries and fears? 71.2 2011 ➜ 68 2010 ➜ Were you as involved as you wanted to be in decisions about your care and treatment? 2009 ➜ Question 84.00 59.0 Complaints and Compliments From Q3 2011/2012 there were 584 complaints of which 48 were related to communication across all staff groups and services in hospital and the community. In relation to compliments there were 7,985 for the same period. Complaints Quarter Q3 11-12 Q4 11-12 Q1 12-13 Q2 12-13 Q3 12-13 Q4 12-13 91 97 111 91 102 92 Q3 11-12 Q4 11-12 Q1 12-13 Q2 12-13 Q3 12-13 Q4 12-13 1,552 1,455 756 1,157 1,610 1,855 Total Compliments Quarter Total For regional and national benchmarking see section 3. Communication: expand deployment of tough books (mobile working) Rationale: tough books were introduced in 2011-2012, subsequent successful bids will enable the Trust to double the number in use in 2013 Community Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • Training and deployment of initial 40 tough books to be completed within first three-months of 2012 (AprilJune). • The number of units in use will be reported. • Progress will be reported twice yearly to the Patient Safety and Quality Standards Group. • Progress reported to PS & QS. ✔ • Progress reported quarterly to IPNMB. ✔ • Progress reported to Trust executive group. ✔ • 154 additional units to be deployed during the remainder of 20122013. • The impact of mobile working (tough books) on admission to hospital rates and on length of stay in hospital of patients with chronic conditions will be monitored. • The Trust executive management team will receive a progress report twice a year. Community healthcare – evidence in practice The use of the tough books allows staff to electronically and contemporaneously update patient information at the point of care, resulting in timely and accurate documentation and clinical decision-making. This improved access to high quality information has improved staff confidence when working across teams. 339 tough books are currently in use across the directorate. This includes 145 (50 Phase 1 and 95 Phase 2) provided through the Department of Health (DH) pilot, 40 procured through reablement funding and 154 funded locally. There has been further funding approved and we are commencing the procurement of additional mobile devices. The Trust has been involved with the National Mobile Health Worker Project which has recently produced its final report. A number of key improvements were evident during the ongoing evaluation including: Phase 1 (50 units) •Contacts with patients increased by 39% throughout the course of the pilot and showed a consistent increase through the life of the project; •Time spent with patients has increased by 45%; •The report shows an increased efficiency around travel as there has been a smaller increase in the number of journeys when correlated to the increased number of contacts. Annual Quality Account 2012-2013 21 Phase 2 (95 units) •Contacts with patients increased by 33% throughout the course of the pilot and showed a consistent increase through the life of the project; •Time spent on journeys decreased by 5%. All the staff have immediate access to corporate and clinical policies at the point of contact because they are immediately available on the tough-book. The directorate is now undertaking some work with specific teams to enable a standardised approach to the use of the system and the technology. Priority 3 Patient Experience Dementia Rationale: as the population becomes older, dementia is becoming more common. Dementia is a priority for stakeholders, commissioners and staff alike. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will conduct an initial dementia screen on all patients aged 65 and over. • We will undertake a prevalence study on a quarterly basis. • Quarterly to the Integrated Nursing and Midwifery Board. • Progress reported to PS & QS. ✔ • Quarterly to our commissioners. • Progress reported quarterly to IPNMB. ✔ • Progress reported to Trust executive group. ✔ • Where indicated, we will carry out abbreviated mental health tests on patients that fit the dementia criteria. • If required we will refer patients for specialist review. Dementia can have a devastating impact on both the patient and those caring for them. Year on year the total number of people with a confirmed dementia diagnosis is increasing. There are currently over 14,000 people with dementia across County Durham and Darlington, and Tees Acute services area. NHS Hartlepool/Stockton and Tees Clinical Commissioning Group (CCG) has the highest projected increase of dementia by 2025 across the North East (NEQOS, North East Quality Observatory System 2012). Ensuring patients with dementia receive high quality care from staff who are knowledgeable and skilled remains a key objective for the Trust and key stakeholders. Progress against the outcomes agreed with stakeholders last year are included within this section. A prevalence study (snapshot survey over one day across all clinical inpatient departments) has been undertaken monthly from September 2012, and results are shown on the month data collection table that follows: 22 Annual Quality Account 2012-2013 The prevalence study identified a number of measures which are reported in the table below: Dementia Screening - Monthly Data Collection 2012-13 Question Sept Oct Nov Dec Jan Feb Mar a Number of patients 75 and above admitted as emergency inpatients, reported as having been asked the dementia case finding question within 72 hours of admission to hospital or who have a clinical diagnosis of delirium on initial assessment or known diagnosis of dementia. 349 353 386 433 423 390 437 b Number of patients aged 75 and above, admitted as emergency inpatients, minus exclusions. 374 367 412 433 423 390 437 c % of all patients aged 75 and above admitted as emergency inpatients who are asked the dementia case finding question within 72 hours of admission or who have a clinical diagnosis of delirium on initial assessment or known diagnosis of dementia. 93.30% 96.20% 93.70% 100% 100% 100% 100% d Number of admissions of patients aged 75 and above admitted as emergency, inpatients who have scored positively on the case finding question or who have a clinical diagnosis of delirium reported as having had a dementia diagnostic assessment including investigations. 217 58 72 57 112 117 136 e Number of patients aged 75 and above admitted as emergency inpatients who have scored positively on the case finding question or who have a clinical diagnosis of delirium. 217 58 75 57 112 117 136 f % of all patients aged 75 and above admitted as emergency inpatients who have scored positively on the case finding question, or who have a clinical diagnosis of delirium and who do not fall into the exemption categories reported as having had a dementia diagnostic assessment including investigations. 100% 100% 96% 100% 100% 100% 100% g Number of all patients aged 75 and above admitted as an emergency inpatient who have had a diagnostic assessment (in whom the outcome is either positive or inconclusive) who are referred for further diagnostic advice/follow up. 21 19 10 14 28 23 41 h Number of patients aged 75 and above who were admitted as an emergency inpatient who underwent a diagnostic assessment (in whom the outcome is either positive or inconclusive). 21 20 11 14 28 23 41 i % of all patients aged 75 and above, admitted as an emergency inpatient who have had a diagnostic assessment (in whom the outcome is either positive or inconclusive) who are referred for further diagnostic advice/follow up. 100% 95.00% 90.90% 100% 100% 100% 100% 23 Annual Quality Account 2012-2013 Dementia Rationale: district nurses are in a strong position to pick up early signs of dementia. We will develop a dementia screening tool for use by community adult nurses. Community Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • If the Department of Health (DH) recommend a dementia test for use by community nurses, we will adopt it and monitor compliance. • We will evaluate the accuracy of the early warning score by reviewing the number of patients requiring onward referral for further tests and the outcome of the tests. • We will report whether we have adopted the national tests or alternatively, managed to develop a dementia early warning score for use by community nurses. • Progress reported to PS & QS. ✘ • Progress reported quarterly to IPNMB. ✘ • Progress reported to commissioners. ✘ • We will report how many patients we use the early warning scores on, and the outcome. • If not, we will evaluate dementia screening tools in other healthcare sectors. • We will develop and test a dementia early warning score for district nurses. The DH has not provided any guidance/recommendations for dementia screening in the community. This has resulted in an inability to achieve this outcome. The Trust aims to pilot a community trigger tool for dementia screening from March which we aim to rollout in 2013. Priority 3 Patient Experience; Discharge arrangements Discharge Arrangements: Rationale: quality and monitoring of complex discharge arrangements remains a focus for patients, commissioners and key stakeholders. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will develop improved communication processes to GPs. • We will further enhance the current discharge letter format to allow audit of the quality of complex discharge arrangements. • We will report results of the baseline audit data along with any actions that are agreed to the Patient Safety and Quality Standards Committee at the end of the reporting year. • Annual discharge report to PS & QS. ✔ • Audits of simple discharge summaries to commissioners. ✔ • Audits of complex discharge summaries to commissioners. ✔ • Patient satisfaction with discharge arrangements monitored via national inpatient survey. ✔ • Directorates will audit the quality of discharge summaries monthly. • We will collect baseline data about complex nursing discharge. Discharge Arrangements 24 The Trust is required to ensure that at least 95% of electronic discharge summaries are complete and sent to GPs within 24 hours of discharge. Content must be accurate and of a high quality to ensure continuity of care and treatment. In collaboration with primary care colleagues, the Trust has made improvements to the electronic discharge letter, which includes details of new and discontinued medication and reasons for changes. Annual Quality Account 2012-2013 There is a section where specific actions recommended to GPs to provide continuing care and treatment, can be documented. There are also ongoing discussions to include details regarding palliative care arrangements and recommendations. This should help reduce inappropriate admissions to hospital so that care can be provided to patients in their own homes. To monitor the performance, lead clinicians have been identified for each area to oversee the compliance in their teams. End of Life Care Rationale: patients and their carers/families are very vulnerable and can find it difficult to explain what they want. In 2011, the use of carers diaries has been successful in improving quality of care and experience. Monitoring the impact of diaries on quality standards results in better care for patients, better experience for families/carers and better job satisfaction for staff. Stakeholders asked for this to be included in this year’s priorities. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it How did we do? • We will ask families/ carers to score their perception of the quality of care in relation to: • Ward nurses will review the diaries during each visit and respond to the score to ensure we meet the needs of the patient and the families/carers. • Local results will be fed back to every ward and department. • Progress reported to PS & QS. ✔ • Corporate data along with themes, learning and recommendations for training will be reported to the IPNMB on a quarterly basis. • Progress reported quarterly to IPNMB. ✔ • Progress reported to commissioners. ✔ • Pain; • Nausea (sickness); • Dyspnoea (breathlessness); • Diaries will be audited corporately and themes used to inform learning and training needs. • Restlessness; • Nursing care of patient; • Nursing care of families/carers. The Family’s Voice (previously known as the carers diary) - was rolled out in 2010. At time of writing, 446 diaries have been given out. 236 have been given between April 2012 – March 2013, an increase of 43 diaries (22.5%) from the previous reporting year. These results have demonstrated that a high standard of care continues to be provided. The following table demonstrates the overall marks afforded to each ward/department across the Trust. Marks are awarded on a scale of 0 (poor) to 4 (excellent) for each of six key quality indicators, these being; pain, nausea, breathlessness, restlessness, how the nurse is with the patient and how the nurse is with the family or carer. The maximum score that can be achieved is 24. Ward Average score Ward Average score 1 Ward 32/33 - Ortho Trauma NT 24.00 11 Ward 26 Respiratory NT 21.17 2 Crit Care NT (ITU) 23.75 12 Ward 25 Cardio NT 20.93 3 Ward 2 HP 22.56 13 Ward 24 Elderly Care NT 20.71 4 Ward 30 - Womens Health Ward 31 - Surg Level 1 Beds NT 22.00 14 Ward 31 - Surg Level 1 Beds NT 20.57 5 Ward 9 HP 21.97 15 Ward 7 HP 20.50 6 Ward 40/41 Stroke Unit NT 21.72 16 Ward 8 - EAU HP 20.00 7 Ward 11 - Acute Ward HP 21.57 17 Short Stay Unit - NT 19.88 8 Ward 42/43 Rehab NT 21.54 18 Ward 27 Acute Medicine NT 19.61 9 Ward 38 - Heamatology NT 21.50 19 Ward 5 HP 19.15 10 Emergency Assessment Unit NT 21.38 20 Ward 28 Mens Health NT Ward 29 Surg Short Stay NT 15.00 25 Annual Quality Account 2012-2013 Understanding this data helps the Trust to understand how we are doing, and to develop and target training in end of life care for wards where scores are lower. In 2013 we will, once again, send our trainers to work with and support staff in developing knowledge and skills to bring all scores to be equal or exceed the best. The following table highlights how scores (0 being poor and 4 being excellent with a maximum score of 24 showing excellence in every aspect of care) and comments made in one diary helped staff to address issues in a timely way. The improvement in score each day demonstrates how this important feedback can influence quality of care resulting in a peaceful death for a patient and the best possible experience for the next of kin. Day Pain Nausea Calmness Breathing Staff/patient Staff/carer Total score One 2 2 2 2 3 2 13/24 Two 3 3 4 3 4 4 20/24 Three 4 4 4 3 4 4 23/24 Four 4 4 4 4 4 4 24/24 When compared to the national VOICES survey the Family’s Voice demonstrated favourable outcomes especially in relation to pain relief. VOICES Pain relief was excellent (Acute Hospital 1) 53.9% VOICES Pain relief was excellent (Acute Hospital 2) 23.5% NT Family’s Voice Free from pain (all or most of the time - patient days all records) 90.3% NT Family’s Voice Free from pain (all or most of the time - last day only) 89.8% VOICES Pain relieved completely (Acute Hospital 1) 26.0% VOICES Pain relieved completely (Acute Hospital 2) 36.0% VOICES Pain relieved completely (Hospice 1) 50.0% VOICES Pain relieved completely (Hospice 2) 67.0% NT Family’s Voice Free from pain (all of the time - patient days all records) 53.8% NT Family’s Voice Free from pain (all of the time - last day only) 63.5% Senior clinical matron Karen Walker and matron Stuart Harper educate the ward staff on the first World Sepsis Day 26 Annual Quality Account 2012-2013 Comments from the diaries chosen at random: Ward A ‘found staff very caring and attentive and willing to answer all my questions to the best of their ability.’ Ward G ‘Excellent care.’ Ward H ‘Thank you for the care and attention that was given to my aunt. Many thanks to the doctors and all the staff on ward G.’ Ward B ‘Armchairs could be more comfortable if a little higher.’ Ward I ‘Your staff are a huge credit to you. They couldn’t have been a more caring or considerate whilst helping us through a difficult time. They are true diamonds.’ Ward C ‘The care for my mother has been outstanding.’ Ward J ‘Nursing care fantastic. Continuous empathy towards mum and family.’ Ward D ‘It was confusing with the two options. We were getting one off the consultant and another off the ward sister. (Consultant told us just to carry on as normal till the worse happens). Sister told us to be on constant bed watch.’ Ward K ‘We felt excellent care given to mum and ourselves. Couldn’t have expected anything better.’ Ward L ‘Wonderful support and care for my father and my family. Ward E ‘I found it (carers diary) very easy to fill in.’ Ward F ‘There could be more information available on what the next steps are when there is a bereavement.’ 27 Annual Quality Account 2012-2013 This diary has been recommended by NHS Innovations to be considered for roll-out nationally. The impact of treating patients with compassion has a direct link to what patients and relatives/carers think about our organisation. Carers diary Since the research in 2010/11 our carers diary (now known as the ‘Family’s Voice’) was provided to the family or carers of 350 hospital patients placed on the end of life care pathway. The diary provided an opportunity for family/carers to score the quality of end of life care in relation to a number of key quality domains, these being: •pain; •breathlessness; •nausea (sickness); •restlessness; •staff care of the patient; •staff care of the carers. The comments made in these diaries provided staff with a vital opportunity to quickly understand what they are doing well and how they might improve actual and perception of care for each individual patient and their carers. Any score below 25 would indicate that the relative/carer perceived that a suboptimal quality of symptom control or experience of care was provided. Use of the carers diary will enable the Trust to review scores and trends over time. It provides an opportunity for staff to put things right and where appropriate for additional support and training to be put in place to enable Trust staff to influence perception of care so that we continuously meet patient and carer expectations. In almost two years (21 months) we have received only one complaint about end of life care from patients where the carer’s diary has been used. Nutrition: Rationale: good nutrition plays an important contribution to recovery from illness or injury. Our stakeholders and our commissioners are joined by our staff in agreeing that nutrition should be a priority for all patients. We have good standards of nutrition for adult inpatients so we will focus on nutrition for children and in the outpatient setting. Hospital Healthcare Overview of how we said we would do it Overview of how we said we would measure it Overview of how we said we would report it • Introduce the malnutrition universal screening tool (MUST) that we use for adult inpatients into the outpatient setting. • We will train staff to use the MUST and STAMP tools. • Results of audits will be • Progress reported reported to the IPNMB to PS & QS. every 6-months. • Progress reported • To the Nutrition quarterly to Advisory Group (NAG). IPNMB. ✔ • Introduce the screening tool for the assessment of malnutrition in paediatrics (STAMP) into in-patient paediatric wards. • We will collect baseline audit by June 2012. • Progress reported to commissioners. ✔ 28 Annual Quality Account 2012-2013 • We will introduce the tools into outpatient and paediatric inpatient areas. • We will collect baseline audit by June 2012. How did we do? ✔ Nutrition Following patient feedback the catering team has implemented further improvements following the successful introduction of the ward hostess service throughout all wards in our hospitals. Our hostesses have a specific aim of improving the patient enjoyment of food. This ward hostess strategy continues to prove an extremely successful catalyst for improvements in patient experience by ensuring patients always get their meal of choice, well presented and hot. This initiative has also greatly assisted the reduction of food waste averaging by 30% to enable re-investment in improved menu, modified consistency meals and other important patient recommendations. Menu choice is regularly reviewed and is now based on choices familiar with the age of patients on elderly care wards and on children’s wards. Frequent snacks and finger foods are available throughout the day for these patients. For patients with dementia and disability we have introduced coloured, light-weight, easy-to-handle utensils. Feedback from our patients demonstrates that they find it much easier to use these. Picture cards with photographs, drawings and words enable the cognitively impaired to understand and chose what they want. We are also looking to purchase half litre water jugs which are easier to lift and use. Catering assistant Sherry Smith. Therapy assistant Chris Ferguson. 29 Annual Quality Account 2012-2013 2B: Quality improvement priorities for 2013-14 Introduction to 2013-2014 Priorities Key priorities for improvement for 2013-2014 have been agreed through consultation with patients, staff, governors, local involvement networks, commissioners, health scrutiny committees and other key stakeholders. We started the consultation period at the beginning of September 2012, which allowed us to consult widely and provide stakeholders with a significant opportunity to consider and suggest the priorities that they would like to see us address. Feedback and third party declarations have been invited from formal stakeholders. Full details of stakeholder feedback can be found in section 3C. Our governors continue to be actively involved in assisting us in setting our priorities. The Trust continues to develop quality improvement, capacity and capability to deliver our priorities as demonstrated throughout this Quality Account. We would like to thank all of those involved in setting priorities for 2013-14 which are linked to patient safety, effectiveness of care and patient experience. We all agree that our priorities for improvement should continue to reflect three key principles, namely: Don’t harm me Treat me right the first time Be nice to me Stakeholder priorities The quality indicators that our external stakeholders said they would like to see included were: Patient Safety Effectiveness of Care Patient Experience 1. Dementia 1. Discharge Processes Information 1. End of Life Pathway & Family's Voice (Carers Diary) 2. Safeguarding Adults (Learning Disabilities) 2. Discharge Processes Medication 2. Is our care good (Patient Experience Surveys) 3. Infection Control (C diff) 3. Discharge Processes (Safe and Warm) 3. Friends and Family recommendation 4. Nursing Dashboard Rationale for the selection of priorities All of the quality indicators selected by external stakeholders have been incorporated into the quality priorities for 2012-2013 leading into 2013-2014, in addition nursing staff asked that the newly introduced dashboard for nursing outcomes should be reported. The tables over the following pages will describe each priority, the rationale for including it along with a summary of how we aim to achieve the outcome, measure the impact and reporting arrangements. We have incorporated feedback from patients, staff and visitors through our consultation on the Trust’s RESPECT strategy, and through feedback from our dignity day campaign in February 2012. 30 Annual Quality Account 2012-2013 The Chief Nursing Officer launched a consultation document in September 2012 to which we again consulted widely and provided feedback for consideration into the final documents focusing on the six Cs: •Care •Compassion •Competence •Communication •Courage •Commitment We have aligned outcomes where possible to quality indicators requested by commissioners. Patient Safety Priority 1: Improving care for people with dementia Rationale: There are currently 14,000 people with a diagnosis of dementia across County Durham & Darlington and Tees. NHS Hartlepool/Stockton on Tees has the highest projected increase of dementia across the North East by 2025. All stakeholders identified dementia as a key priority. Hospital Healthcare How will we do it How will we measure it How will we report it • We will use the Stirling Environmental Tool to adapt and audit the impact on our hospital environment. • The Stirling Environmental audit assessment tool will be used to monitor the difference pre and post adaptation. • Dementia Strategy Group quarterly. • We will ensure that all patients over 65 receive an Abbreviated Mental Test (AMT) and are, where appropriate referred for further assessment. • The percentage of patients who receive the AMT and, where appropriate, further assessment will be reported quarterly. • Integrated Professional Nursing and Midwifery Board (IPNMB) and PS & QS Quarterly. Patient Safety Priority 2: Safeguarding Adults with Learning Disabilities (LD) All hospital patients will have a named advocate and an individualised plan of care. Rationale: The Winterbourne View Review* identified a number of actions that service commissioners and providers could undertake to prevent the terrible outcome suffered by people with LD at Winterbourne View. The Trust and Commissioners believe that people with LD should not be in hospital unless absolutely necessary. When it is necessary to admit patients with LD, they must have an individualised plan of care and a named advocate. Hospital Healthcare How will we do it How will we measure it How will we report it • All patients with LD will be referred on admission to the LD specialist nurse. • Audits will be carried out and results reported. • Audit results and Action Plans to be reported to IPNMB quarterly. • The LD Specialist nurse will act as the named advocate and will ensure that an individualised plan of care is in place and reasonable adjustments documented. * The national response to The Winterbourne Review report can be accessed on www.wp.dh.gov.uk/publications/files/2012/12/final-report.pdf Annual Quality Account 2012-2013 31 Patient Safety Priority 3: Infection Prevention and Control (IPC): Clostridium Difficile (C diff) To continue to reduce the number of avoidable hospital acquired cases of clostridium difficile. Rationale: C diff remains a burden across the community and hospitals in the Hartlepool and Tees areas. The Trust breached its C diff target in 2012. Stakeholders and the Trust believe that reducing C diff should remain a key priority for 2013-2014. Hospital Healthcare How will we do it How will we measure it How will we report it • We will closely monitor testing regimes, antibiotic management and repeat cases and ensure we understand and manage the root cause wherever possible. • We will monitor the number of hospital and community acquired cases. • Public Board meetings. • We will undertake a multidisciplinary Root Cause Analysis (RCA) within 3 working days. • Infection Control Committee (ICC). • We will define avoidable and unavoidable for internal monitoring. • We will benchmark our progress against previous months and years. • Council of Governor meetings (CoG). • Patient Safety and Quality Standards Committee (PS & QS). • To frontline staff through Chief Executive brief. • Nursing Dashboard. • We will benchmark our position against Trusts in the North East in relation to number of cases reported; number of samples sent for testing and age profile of patients. Patient Safety Priority 4: Dementia All hospital patients will have a named advocate and an individualised plan of care. Rationale: In 2012 the Trust signed up to the Right Care: Creating Dementia Friendly Hospital. Along with key stakeholders, the Trust believes that patients with dementia receive the right treatment in the right place. Community Healthcare How will we do it How will we measure it How will we report it • Patients with dementia will be appropriately assessed and referred on to specialist services. • We will audit the number of patients over 75 admitted as an emergency that are reported as having a known diagnosis of dementia, or have been asked the (Prime Ministers) dementia case finding question. • To the IPNMB. • A monthly audit of the percent of patients who are screened, assessed and referred for specialist review. 32 Annual Quality Account 2012-2013 • To the Board of Directors. Effectiveness of Care Priority 1: Discharge processes – Information/Communication Rationale: Although quality of discharge information has improved considerably over the years, this remains a priority with further improvements recommended by stakeholders. Hospital & Community Healthcare How will we do it How will we measure it How will we report it • All patients discharged to a nursing or care home requiring district nurse review, will receive a written summary of care provided and of ongoing care required. • Audit a number of patients discharged with a letter. • To the IPNMB. • A copy will be provided to the home or district nurse. Effectiveness of Care Priority 2: Discharge processes – Medication Rationale: The latest national patient experience survey identified that the percentage of patients told about medication side-effects to watch out for at home had reduced by 5%. Hospital & Community Healthcare How will we do it How will we measure it How will we report it • All patients will receive information about medication side-effects to watch out for at home. • Via national and local patient surveys. • Local audit reports twice yearly to IPNMB and PS & QS. • National audit report to PS & QS. Effectiveness of Care Priority 3: Discharge and transfer processes – Safe and warm Rationale: Following receipt of a complaint in December 2012, the Trust has included Safe and Warm discharge and transfer as an additional measure for 2013-2014. Hospital & Community Healthcare How will we do it How will we measure it How will we report it • We will deliver a ‘Safe and Warm’ campaign. • Referrals to the ‘Stay Safe and Warm Campaign Scheme' will be monitored. • Annual report to IPNMB from Tees wide Vulnerable Adults Patient Experience Group. • We will review our protocols for transferring and discharging patients to ensure that blankets are always provided and are adequate to maintain warmth throughout the patient journey. • We will liaise with the ambulance services and staff to ensure patients are kept warm until they arrive at their destination. 33 Annual Quality Account 2012-2013 Effectiveness of Care Priority 4: Nursing Dashboard Rationale: The Nursing Dashboard will support close monitoring of nurse sensitive patient outcomes on a day-to-day basis. It will support sharing of best practice and speedy review of any potential areas of concern. Hospital Healthcare How will we do it How will we measure it How will we report it • Training will be completed and each department will evidence that their results have been disseminated and acted upon. • SCMs will monitor ward areas to ensure that data is up to date, accurate and displayed in a public area. • Monthly dashboard analysis to the Director of Nursing • Ward matrons will present their analysis on a public area of the ward for patients and staff to see. The results will be discussed and minuted. • Quarterly to Senior Matron and General Manager meeting and IPNMB To note: For Community, there will be a Community Nursing Dashboard developed and rolled out during 2013-2014. This is dependent on integrated IT systems being in place. Patient Experience Priority 1: End of Life Pathway and Family’s Voice Rationale: The Trust has made excellent progress in rolling out use of the Family’s Voice. Stakeholders and the Trust believe that this needs to remain a priority in 2013-2014 both in hospital and in the community. Hospital Healthcare How will we do it How will we measure it How will we report it • We will continue to embed use of the Family’s Voice in hospital and continue to roll its use out in the community. • We will evaluate feedback in relation to pain, nausea, breathlessness restlessness, care for the patient and care for the family. • Quarterly to IPNMB • Annually to PS & QS Patient Experience Priority 2: Is our care good? Rationale: Trust and key stakeholders believe that it is important to ask this question through internal and external reviews. Hospital Healthcare How will we do it How will we measure it How will we report it • We will ask the question to every patient interviewed in the Patient Experience and Quality Standards (PEQS) reviews. • We will analyse feedback from PEQS and patient experience/ national surveys. • Six monthly reports to IPNMB and to PS & QS. • We will ask the question in all Trust patient experience surveys. • We will monitor patient feedback from national surveys. 34 Annual Quality Account 2012-2013 Patient Experience Priority 3: Friends and Family recommendation. Rationale: The Department of Health require Trusts to ask the Friends and Family recommendation questions from April 2013. Stakeholders agree that this should be implemented and reported in the 2013-2014 Quality Account and Report. Hospital Healthcare How will we do it How will we measure it How will we report it • We will incorporate the Friends and Family test wording into PEQS and patient surveys. • We will analyse feedback from PEQS and patient surveys and discharge questionnaires. • Quarterly to IPNMB and to PS & QS. • We will ask patients to complete a questionnaire on discharge from hospital. Part 2C: Statements of Assurance from the Board Review of Services During 2012-2013 North Tees and Hartlepool NHS Foundation Trust provided and/or subcontracted 64 NHS services. The majority of our services were provided on a direct basis, with a small number under sub-contracting or joint arrangements with others. We have reviewed all of the data available to us on the quality of care in all of these NHS services. The income generated by the NHS services reviewed in 2012-2013 represents 100% of the total income generated from the provision of NHS services by the Trust for 2012-2013. The data reviewed aims to cover the three dimensions of quality: patient safety; clinical effectiveness, and patient experience. In a number of areas there has been no benchmark data available. Where benchmark data has been available, it has been included. Participation in clinical audits All NHS Trusts are audited on the standards of care that they deliver and our Trust participates in all mandatory national audits and national confidential enquiries. The CQC quality risk profile rated the Trust as green in relation to assessing and monitoring the quality of service provision throughout 2012-2013. The CQC quality risk profile is included under the Care Quality Commission section of this report. The Healthcare Quality Improvement Partnership (HQIP) provides a comprehensive list of national audits which collected audit data during 2012-2013 and this can be found on the following link: www.hqip.org.uk/national-clinical-audits-for-inclusion-in-quality-accounts/#QA During 2012-2013, 37 national clinical audits and five national confidential enquiries covered the NHS services that we provide. During that period we participated in all 37 national clinical audits and five national confidential enquiries. This represents 100% of all mandatory national clinical audits and 100% of all mandatory national confidential enquiries. We did not participate in all non-mandatory audits as we have a small audit team. The national clinical audits and national confidential enquiries that we were eligible to participate in during 2012-2013 are listed below. This list also identifies those national clinical audits and national confidential enquiries that the Trust participated in during this period. 35 Annual Quality Account 2012-2013 The national clinical audits and national confidential enquires that the Trust participated in, and for which data collection was completed during 2012-2013, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Audit title Participation M = Mandatory N = Non-Mandatory % cases submitted Adult community acquired pneumonia (British Thoracic Society) Yes (N) Data collection ongoing Adult critical care (Case Mix Programme – ICNARC CMP) Yes (N) Data collection ongoing Emergency Laparotomy (Royal College of Anaesthetists) Yes (M) Audit to commence in 2013 Emergency use of oxygen (British Thoracic Society) Yes (N) 100% National Joint Registry (NJR) Yes (M) Data collection ongoing Non-invasive ventilation – adults (British Thoracic Society) Yes (N) 100% National Confidential Enquiry Patient Outcome and Death (NCEPOD) Yes (M) Data collection ongoing Renal colic (College of Emergency Medicine) Yes (N) 100% Severe trauma (Trauma Audit & Research Network) Yes (N) Data collection ongoing National Comparative Audit of Blood Transfusion - programme contains the following audits, which were previously listed separately in Quality Account: a) O negative blood use (2010/11) b) Medical use of blood (2011/12) c) Bedside transfusion (2011/12) d) Platelet use (2010/11) Yes (N) 100% Potential donor audit (NHS Blood & Transplant) Yes (N) Data collection ongoing Bowel cancer (NBOCAP) Yes (M) 100% Lung cancer (NLCA) Yes (M) 100% Oesophago-gastric cancer (NAOGC) Yes (M) 100% Acute coronary syndrome or Acute myocardial infarction (MINAP) Yes (M) Data collection ongoing Heart failure (HF) Yes (M) Data collection ongoing National Cardiac Arrest Audit (NCAA) Yes (N) Data collection ongoing Adult asthma(British Thoracic Society) Yes (N) 100% Asthma Deaths (NRAD) Yes (M) 100% Bronchiectasis (British Thoracic Society) Yes (N) 100% COPD (Royal College of Physicians) Please note: this is NOT the COPD audit run by the British Thoracic Society) (M) Audit to commence 2013 Diabetes (Adult) ND(A), includes National Diabetes Inpatient Audit (NADIA) Yes (M) 100% Diabetes (Paediatric) (NPDA) Yes (M) 100% Inflammatory bowel disease (IBD) Includes: Paediatric Inflammatory Bowel Disease Services (previously listed separately on 2010/11 quality accounts list) Yes (M) Data collection ongoing Pain database Yes (M) 100% Fractured neck of femur (College of Emergency Medicine) Yes (N) 100% Hip fracture database (NHFD) Yes (M) Data collection ongoing National dementia audit (NAD) Yes (M) 100% Parkinson's disease (National Parkinson's Audit) Yes (N) 100% Sentinel Stroke National Audit Programme (SSNAP) - programme combines the following audits, which were previously listed separately in Quality Account: a) Sentinel stroke audit (2010/11, 2012/13) b) Stroke improvement national audit project (2011/12, 2012/13) Yes (M) Data collection ongoing 36 Annual Quality Account 2012-2013 Audit title Participation M = Mandatory N = Non-Mandatory % cases submitted Elective surgery (National PROMs Programme) Yes (N) 80.3% (based on return rate of patient questionnaires) Child Health (CHR-UK) Yes (M) 100% Epilepsy 12 audit (Childhood Epilepsy) Yes (M) 100% Maternal infant and perinatal (MBRRACE-UK) Yes (M) 100% Neonatal intensive and special care (NNAP) Yes (M) 100% Paediatric asthma (British Thoracic Society) Yes (N) 100% Paediatric fever (College of Emergency Medicine) Yes (N) 100% Paediatric intensive care (PICANet) Yes (M) 100% Paediatric pneumonia (British Thoracic Society) Yes (N) Data collection ongoing Consultant sign-off (College of Emergency Medicine) Yes (N) 100% The Trust participated in all five national confidential enquiries (100%) that it was eligible to participate in, namely: National Confidential Enquiries (NCEPOD) NCEPOD Cardiac Arrest Procedures (Time to Intervene?) NCEPOD Bariatric Surgery Study (Too Lean a Service?) NCEPOD Alcohol Related Liver Disease Study (data collection ongoing) NCEPOD Subarachnoid Haemorrhage Study (data collection ongoing) NCEPOD Tracheostomy Care Study (study just commenced) Confidential Maternal and Child Health Enquiries (CMACE) The Trust provides information to these national enquiries for all maternal, perinatal (the period shortly before and after birth) and child deaths through the Regional Maternity Survey Office (RMSO) and the North East Public Health Observatory (NEPHO). Participation in this audit provides useful benchmarking data across the North East. MBRRACE-UK has been appointed by the Healthcare Quality Improvement Partnership (HQIP) to continue the national programme of work investigating maternal deaths, stillbirths and infant deaths, including the Confidential Enquiry into Maternal Deaths. The aims of MBRRACE-UK are to provide robust information to support the delivery of safe, equitable, high quality, patient-centered maternal, newborn and infant health services. Nationally there are future plans to include a new programme of audit for maternal deaths, late fetal losses, still births and infant deaths. The Trust intends to participate. The maternity, neonatal and paediatric teams will continue to provide information relating to all child deaths from birth to 18 years of age to the RMSO office and the Child Death Overview Panels that review all child deaths on behalf of the Local Safeguarding Children’s Boards. This allows for a multidisciplinary review of data and analysis for any trends and shared learning relating to these deaths. The Trust also provides details to the North East Public Health Observatory (NEPHO) to help collate data including diagnosis and incidences of congenital abnormalities; management and outcome data from multiple pregnancies; and diabetes in pregnancy. This data is analysed regionally and included in national analysis. 37 Annual Quality Account 2012-2013 Commendations on our participation and performance In the latest National Cancer Patient Experience Survey (received 2012), the Trust was rated in the top 20% nationally for over 60% of all responses, with the Trust achieving the highest responses in the country for two questions: •Patients being told to bring a friend when they were first told they had cancer •Providing GPs with enough information about diagnosis and treatment. The Trust was invited to present its work on (NICE50 guideline; reducing deterioration) at the national NICE conference in 2012. National Clinical Audits The Department of Health holds a comprehensive list of National Audits which can be found at: www.dh.gov.uk/health/tag/quality-accounts/ The reports of 13 national clinical audits were reviewed by the Trust in 2012-2013 resulting in the following actions to improve the quality of healthcare provided: Audit title Actions taken National Care of the Dying Audit Introduction of the Family’s Voice to complement the Liverpool End of Life Care Pathway. National Decreased Consciousness Audit (Paediatrics) Local audit between the Paediatric and Accident and Emergency (A&E) departments. UK Inflammatory Bowel Disease Audit Named pharmacist identified. National Inpatient Survey 2011 Reintroduction of red trays in selected wards to alert staff to the patient who may need assistance at meal times. We have introduced a Nurse for the Older Person and Dementia Nurse Specialists to assist. We use Intentional Rounding and PEQS reviews to monitor patient experience. National Outpatient Survey 2011 Detailed patient survey looking at issues such as communication, information provided and privacy and dignity. Specialty specific Customer Care Charters highlight the importance of effective communication, appropriate behaviour and standards of good practice. National Parkinson’s Disease Audit 2011 Communication processes that involve Driver and Vehicle Licensing Agency (DVLA) have been enhanced. NCEPOD report, Time to intervene? A six-monthly audit to monitor quality of medical assessment on admission has been developed. National Epilepsy 12 audit Improvements to documented classification of seizure agreed with visiting neurologists. College of Emergency Medicine National Audit: Consultant sign-off Emergency Department Information System (EDIS) is being adapted to enable an electronic consultant signoff field. College of Emergency Medicine National Audit: Pain Management in Children Audit in A&E department to monitor pain management following initial assessment. College of Emergency Medicine National Audit: Severe Sepsis and Septic Shock Local audits developed to monitor documentation of oxygen therapy and urine output. National Cancer Patient Experience Survey 2011 Task and Finish Group established to improve patient understanding of resources available from local authorities. Information about free prescriptions being provided by Clinical Nurse Specialists. BTS Emergency Oxygen Audit 38 Annual Quality Account 2012-2013 Prescription sheet revised in line with best practice. Further audits. Local Clinical Audits The reports of 42 local clinical audits were reviewed by the Trust in 2012-2013 and the Trust intends to or has commenced the following actions to improve the quality of healthcare provided as follows: Local audit title Actions taken/in progress Fluid Balance Management in Theatres Bespoke staff training. A Standard Operating Procedure (SOP) and audit tool has been developed to monitor compliance. Assessment of Safe Prescribing Safe prescribing training tests developed as part of junior doctor induction Hypertension Audit Assessment and management of hypertension risk in pregnancy. Audit plan agreed. Evaluation of Acute Knee Soft Tissue Injury Clinic Pathway Referral criteria updated. To be audited in 2013 Prescription and Treatment for Postoperative Nausea and Vomiting (PONV) Regular prescription of anti-emetics by anaesthetists to be audited in 2013. Stroke Management in the Emergency Department The ROSIER stroke assessment tool will be used regularly to enable improved stroke diagnosis. In-Patient Medical Management of Anorexia Development of enhanced guidelines and training for staff. The Trust continues to perform well in audit activity and positive points to note include: Local audit title Good practice Neutropenic Sepsis Audit An education programme and posters have been introduced to increase Neutropenic Sepsis awareness. Cardiac Rehabilitation – Clinical Outcomes in the Community Patients have given very positive feedback. Average weight, BMI and alcohol intake have reduced. Diabetes Inpatient Foot Assessment Audit A proforma for foot assessment has been developed and implemented. This ensures that foot assessment is undertaken at the time of admission by the admitting doctor and that there is continuing patient assessment by nursing staff. Vascular Disease Antiplatelet agents are in line with best practice for both Transient Ischaemic Attack (TIA) and Stroke. MUST Nutritional Assessment Tool Bi annual audits undertaken in 2012 to continue in 2013 Thromboprophylaxis Following Normal Vaginal Delivery There is near 100% compliance with guidance. Anaesthetic Techniques for Caesarean Section We achieve high level compliance with Royal College Guidance The Diagnosis & Management of Epididymo-Orchitis New local guidelines have being developed for diagnosis World Health Organisation (WHO) Alcohol Audit Good compliance with the guidance – patients are being correctly referred to an Alcohol Specialist Nurse and are appropriately assessed and supported. All national audit reports are considered by the Audit and Clinical Effectiveness (ACE) Committee which reports to the Patient Safety and Quality Standards (PS & QS) committee, PS & QS reports directly to the Board of Directors. The ACE committee is chaired by an Associate Medical Director and includes patient representatives. The Department of Health’s National Cancer Patient Experience Survey 2011 identified that improvements have been made in relation to patient experience across a number of areas measured, with 62% (up from 59% in 2010) of all results being in the top 20% nationally. The full report can be found at: www.quality-health.co.uk/images/stories/pdfs/2012CancerReports/2011-12cancerpatientexpe riencesurveynationalreport.pdf 39 Annual Quality Account 2012-2013 Participation in Research The Research and Development (R&D) Department continues to embed research into the culture of the Trust through: •More patients being recruited into National Institute for Health Research (NIHR) portfolio studies; •More staff benefiting from the R&D Incentive Funding of higher research degrees and qualifications; •Increased numbers of staff trained in Good Clinical Practice (GCP); •Involvement of new clinical specialisms in research activity. We remain committed to actively encouraging participation into NIHR portfolio research studies as part of our membership agreement with County Durham & Tees Valley Comprehensive Local Research Network (CDTV CLRN). We have 151 active studies registered with the department, 116 of these (77%) are NIHR portfolio studies. The total number of patients receiving NHS services provided or subcontracted by the Trust in 2012-2013, who were recruited during that period to participate in research, approved by a research ethics committee, was 1,663. The table below shows the year on year increases seen in this Trust for portfolio study recruitment (figures correct as at 08/04/2013). Figure 1. NIHR Portfolio recruitment NIHR portfolio Study recruitment 2,000 1,800 1,663 1,600 1,400 1,200 1,147 1,000 800 600 400 200 412 455 2009/10 2010/11 159 0 2008/09 2011/12 2012/13 Other achievements to date are summarised below: •In the Guardian Research League tables 2011/12 our Trust ranked 143rd best nationally in the 'All Trusts' category (397th the previous year). In the 'Acute Trusts - medium sized' category we ranked 16th best in the country 2011/12. Data for 2012/13 was not available at the time of going to print; •The Trust R&D Incentive fund has funded £49,564 of training, research support and course fees within the Trust over the last year. Through the R&D Incentive Fund, we were able to deliver 3 training sessions in Good Clinical Practice for Research (GCP) since the last annual report. In total, 71 members of staff attended GCP training in March and November 2012 and March 2013. 155 members of staff are currently trained in GCP. The course is intended as a refresher every two years for staff who already hold a GCP certificate and an introductory course for those new to research; 40 Annual Quality Account 2012-2013 Clinical respiratory research nurse June Battram and specialist respiratory nurse Karen Galloway. There are 56 members of staff acting as Principal Investigator/Local Collaborators in research within the Trust, some of whom are contributing to 10 studies; •The CLRN funds 17 research nurses within the Trust. These nurses are working a range of whole time equivalents from a few hours a week to full time on research studies. Our bi-monthly research nurses working group continues to be well attended and provides professional support and mentorship; •The 2012 R&D conference was once again a great success with notable interest in the keynote lecture from Professor Alastair Burt. Overall of the 88 people who attended, 98% rated it as either excellent (50%) or good (48%) in terms of overall opinion of the day; •Participation in commercially sponsored portfolio research is an NIHR priority. We have eight commercially sponsored studies active within the Trust with plans for more in 2013. We plan to use the revenue created through overhead fees in these studies to create additional self-funded research posts within the relevant directorates; •The R&D seminar series was held in September 2012 and was attended by 42 members of staff. Evaluation feedback received indicated 94% felt it was relevant to their role, for 97% the seminars met their expectations, 100% found it beneficial, and 97% were likely to recommend it in future, whilst 100% would be likely to attend in the future; •Our staff have presented their research at nine national conferences, eight international conferences and 28 papers have been published in peer reviewed journals; •We have continued to streamline our research governance processes and consistently perform well within the NIHR performance metrics of providing R&D approval for portfolio studies approved within the NIHR Co-ordinated System for gaining NHS Permissions (CSP) within 30 days (median for our Trust nine days); 41 Annual Quality Account 2012-2013 Commissioning for quality and innovation (CQUIN) A proportion of North Tees and Hartlepool NHS Foundation Trusts income in 2012-13 was conditional upon achieving quality improvement and innovation goals with any person or body they entered into a contract, agreement or arrangement with for the provision of relevant health services, through the Commissioning for Quality and Innovation payment framework. The total income received through achievement of CQUIN goals in 2012-2013 is £4,279,015.45* which includes £3,678,332.75* for acute and £600,682.71* for community services. Further details of the agreed goals for 2012/13 for the following 12 month period are available online at: www.monitor-nhsft.gov.uk/sites/all/modules/fckeditor/plugins/ktbrowser/_openTKFile. php?id=3275 To note: 2012-2013 Quarter 4 data not validated at time of print. The total income received through achievement of CQUIN goals in 2011-2012 was £3,168,181 which included £2,793,077 for acute and £375,104 for community services. Care Quality Commission (CQC) Like all NHS Trusts, North Tees and Hartlepool NHS Foundation Trust is required to register with the Care Quality Commission and its current registration status is registered without conditions for all services provided. Results of unannounced CQC inspections During February 2013 the Trust received an unannounced back-to-back visit covering both hospital sites. The following outcomes were reviewed at each site: North Tees Outcome Regulation 4 9 Description Care and welfare of people who use services 10 15 Safety and suitability of premises 13 22 Staffing 17 19 Complaints Hartlepool Outcome Regulation 1 17 Description Respecting and involving people who use services 4 9 Care and welfare of people who use services 12 21 Requirements relating to workers 17 19 Complaints A written report has now been received from CQC assessors and it gave no recommendations and very positive feedback to Trust personnel. The final report will be available from the Trust and on the CQC website. The Trust has undertaken provider compliance assessments against these standards and introduced a shared repository for the collection of supporting evidence. 42 Annual Quality Account 2012-2013 This allows all Trust staff to access the data to facilitate understanding of the requirements within the remit of their particular role or profession. It also enables the CQC to assess the Trust's evidence of compliance more easily. Confirmation of no enforcement action We are happy to confirm that the Care Quality Commission (CQC) has not taken enforcement action against the Trust during 2012/13. Participation in CQC reviews At the time of writing the Trust has not participated in any special review or investigation by the CQC during the reported period. The Trust has received a letter from the CQC in November 2012 regarding the number of hip revision surgery undertaken. The Trust was able to respond, as its surgeons were responsible for finding problems regarding Metal on Metal hip surgery. Trust surgeons alerted the Medicines and Healthcare Authority (MHRA) who subsequently issued a national alert. The Trust was the first in the country to implement a recall programme and offer revision surgery for this group of patients. Trust CQC Quality Risk Profile The CQC provides a Quality Risk Profile (QRP) for all NHS Trusts. The QRPs are updated on a regular basis and take into consideration all information, internal and external, which is collected by them from up to 50 different sources in relation to every Trust. They are used to help monitor compliance against the CQC Essential Standards of Quality and Safety. More information on the essential standards and other CQC assessments can be found on the following link: www.cqc.org.uk. The Trust QRP ratings are shown on the following tables and these demonstrate that the Trust is sustaining very good performing across all essential standards. There are eight ratings that can be assigned to Trusts. The highest possible [best] rating is low green and the lowest [worst] possible rating is high red. An additional two criterion for no data or insufficient data are also used (see CQC diagram overleaf). Birthing centre staff at the University Hospital of Hartlepool. 43 Annual Quality Account 2012-2013 Outcome Descriptions 1. Respecting and involving people who use services 2. Consent to care and treatment 4. Care and welfare of people who use services 5. Meeting nutritional needs 6. Cooperating with other providers 7. Safeguarding people who use services from abuse 8. Cleanliness and infection control 9. Management of medicines 10. Safety and suitability of premises 11. Safety, availability and suitability of equipment 12. Requirements relating to workers 13. Staffing 14. Supporting staff 16. Assessing and monitoring the quality of service provision 17. Complaints 18. Records Risk Estimates Over Time Period Outcome 1 Outcome 2 Outcome 4 Outcome 5 Outcome 6 Outcome 7 Outcome 8 Outcome 9 Mar-12 Low Green High Green Low Green Low Yellow Low Green High Green High Green High Green May-12 Low Green Low Green Low Green Low Yellow High Green Low Green High Green Low Green Jun-12 Low Green Low Green Low Green Low Yellow Low Yellow Low Green Low Green Low Green Jul-12 Low Green Low Green Low Green Low Green Low Yellow Low Green Low Green Low Green Sep-12 Low Green Low Green High Green High Green High Green Low Green High Green Low Green Oct-12 Low Green Low Green High Green High Green High Green Low Green Low Green Low Green Nov-12 Low Green Low Green High Green High Green Low Green Low Green High Green Low Green Jan-13 Low Green Low Green Low Yellow High Green High Green High Green High Green Low Green Feb-13 Low Green Low Green Low Yellow High Green Low Green High Green High Green Low Green Mar-13 Low Green Low Green Low Yellow High Green Low Green High Green Low Yellow Low Green Period Outcome 10 Outcome 11 Outcome 12 Outcome 13 Outcome 14 Outcome 16 Outcome 17 Outcome 21 Mar-12 Low Yellow Low Yellow Low Green Low Green Low Green Low Green Low Green Low Green May-12 High Green Low Yellow Low Green High Green Low Green Low Green Low Green Low Green Jun-12 High Green Low Yellow Low Green High Green Low Green Low Green Low Green Low Green Jul-12 Low Green High Green Low Green Low Green Low Green Low Green Low Green Low Green Sep-12 Low Green High Green Low Green Low Green Low Green Low Green High Green Low Green Oct-12 Low Green High Green Low Green Low Green Low Green Low Green Low Green Low Green Nov-12 Low Green High Green Low Green Low Green Low Green Low Green Low Green Low Green Jan-13 Low Green High Green Low Green Low Green Low Green Low Green Low Green Low Green Feb-13 Low Green Low Yellow Low Green Low Green Low Green Low Green Low Green Low Green Mar-13 Low Green Low Yellow Low Yellow High Green Low Green Low Green Low Green Low Green 44 Annual Quality Account 2012-2013 CQC National Accident and Emergency Survey results 2012 In 2012, the CQC ran a national accident and emergency survey. Thirty-seven questions were asked with the Trust scoring better than other Trusts nationally in 8% of questions. 92% of the questions asked scored about the same as other Trusts, with no questions scoring worse. The Trust scored better nationally for three questions, these being; 1. Were you given enough privacy when being examined or treated? 2. Before you left the A&E Department, did you get the results of your tests? 3. While in the A&E Department, did you ever see any posters or leaflets explaining how to complain about the care you received? The following table shows how the Trust performs in relation to the other Trusts nationally in relation to scores for each section of the national accident and emergency survey. Section heading Score out of 10 for your Trust How this score compares with other Trusts Travelling by ambulance (answered by those who travelled by ambulance only) 9.40 Same Reception and waiting 6.20 Same Doctors and nurses 8.40 Same Care and treatment 8.40 Same Tests 8.70 Same Hospital environment and facilities 8.20 Same Leaving the A&E department (answered only by those who were not admitted to hospital or a nursing home) 6.60 Same Overall views on experience 7.40 Better Quality of Data Good quality information underpins the effective delivery of patient care and helps staff to understand what they do well and where they might improve. The Board of Directors attend regular development sessions and seminars to ensure that every member of the Board is equipped to interpret data, challenge and oversee improvements where necessary. They consider data provided with other intelligence including listening to what patients are saying. Our executive and non-executive directors can often be seen in clinical areas talking to patients and staff to ensure a fully informed and well rounded approach to decision making. The members of the Council of Governors are encouraged to test the data reports they receive through participation in PEQS reviews. This enables governors to speak directly to patients and staff and provides assurance that standards are aligned with information reported. The Trust Board and Council of Governors are presented with a data quality dashboard comparing the benchmark position against other Trusts within the Strategic Health Authority (SHA). Non-executive Directors meet with the Director of Nursing and Clinical Governance personnel on a regular basis to review incident related performance data. They also undertake a quarterly review of complaints related data. This includes monitoring all complaints reported in the previous quarter. A sample is selected for further scrutiny. This provides independent assurance that complaints are dealt with appropriately, in a timely fashion and that lessons are learned and actions taken when we get things wrong. 45 Annual Quality Account 2012-2013 Training staff in critical appraisal is a vital part of ensuring that evidence is considered in an objective and balanced way. We develop clinical staff so that they have the skills and knowledge to use evidence in a way that supports them to make the best clinical decisions. The Deputy Clinical Effectiveness Manager has been training staff in critical appraisal for over ten years. His courses have been recognised and adopted by the British Medical Association (BMA) and the Department of Health (DH). They are now used in the UK, Europe and the United States of America. He remains the highest ranked trainer authorised by the BMA. Additional assurance in relation to data quality is provided independently by Audit North. This provides rigorous and objective testing of data collection and reporting standards. Results of these independent audits are reported to the audit committee and provide the Trust with independent appraisal of clinical, financial and business governance standards. This process of internal audit enables the Trust to test quality assumptions and pursue its philosophy of continual improvement. In order to test and improve quality of data the Trust will continue to commission independent audits of its key business. Smarter Board Reporting Tools The Trust has employed a dedicated Quality Analyst to ensure data quality and to produce clear, concise and accurate reports. The Quality Analyst works and interacts with staff at all levels in the Trust, from ward to board, including community services. During 2012 additional data quality tools and dashboards have been developed by the Quality Analyst to aid the Trust Board reporting system. These analysis tools and dashboards offer a real-time view of the current status of each ward in relation to falls, pressure ulcers, formal complaints, infections and compliments/complaints. The Infection Database and Analysis tool offers a real time analysis of infection data relating to C diff cases. These systems and reports ensure executive and non-executive directors are empowered to challenge, scrutinise and derive appropriate levels of assurance. The data quality tools and Dashboards created during 2012/2013 include: •Nurses Dashboard •Community Dashboard •IPC Dashboard •PEQS Database •Clostridium Difficile Database The tools that have been developed ensure that there are no duplications within the data, the data is valid and that there is tangible analysis undertaken automatically, producing clear, concise and accurate reports tailored to the target audience. Actions to improve data quality going forward. The Trust will be taking the following actions to further improve data quality: •Audits on the data capture within the notes compared to data captured on PAS are carried out for both inpatients and outpatients; •The information team is expanding to provide the same data quality for SystmOne (community IT system) as it currently provides for PAS; •Increase the number of auditors within clinical coding; 46 •Harness full value from new dashboards during 2013. Annual Quality Account 2012-2013 PAS Upgrade The PAS upgrade was a pre-requisite for the upgrade of existing products - the postcoder functionality (QAS) and the clinical coding module (Medicode). Both suppliers upgraded their solutions to change the way the functionality was provided. In order to maintain both these modules for the users, PAS was upgraded to the latest version. Medicode now provides the coders with more functionality including the ability to record the source for the codes e.g. case notes, discharge summaries. NHS number and general medical practice validity The Trust submitted records during 2012-13 to the national Secondary User Service (SUS) for inclusion in the national Hospital Episodes Statistics (HES) for inclusion in the latest published data. The percentage of records in the published data is shown in the following table: Which included the patient’s valid NHS number was: % Which included the patient’s valid general medical practice code was: % Percentage for admitted patient care 99.40 Percentage for admitted patient care 100 Percentage for outpatient care 99.90 Percentage for outpatient care 100 Percentage for accident and emergency care 99.20 Percentage for accident and emergency care 100 *Data period April 12 – February 13 Information governance (IG) Information governance means keeping information safe. This relies on good systems, processes and monitoring. Every year we audit the quality of specific aspects of information governance through the national information governance toolkit report. In 2012-2013 we had to ensure that 95% of all of our staff had received information governance training. This target was challenging, however we have continued to make significant progress with a total of at least 96% of all staff trained during the year for the third year running. The Trust Information Governance Assessment Report score overall for 2012-2013 was 81% and this has been graded as GREEN. A green rating is achieved where Trusts achieve level 2 or above on all requirements (see following table). We continue to provide assurance to the Trust Board that we are constantly assessing and improving our systems and processes to ensure that information is safe. Annual ratings of green (pass) or red (fail) are assigned to Trusts each year. The following table shows progress with ratings when compared to the previous year. Requirement Information Governance Management Corporate Information Assurance Confidentiality and Data Protection Assurance Clinical Information Assurance Secondary Use Assurance Information Security Assurance 2011-2012 rating 2012-2013 rating Green Green 93% 93% Green Green 66% 66% Green Green 83% 79% Green Green 73% 93% Green Green 83% 83% Red Green 75% 75% The IG toolkit is available on connecting for health website. www.igt.connectingforhealth.nhs.uk 47 Annual Quality Account 2012-2013 We receive a number of Freedom of Information (FOI) requests every year. In order to be transparent about information we have been asked to provide, we have developed a virtual reading room on our internet site. Since 1 January 2012, we have been posting responses to Freedom of Information requests on the site and these can be viewed by the public on: www.nth.nhs.uk/foirr Clinical coding Clinical coding translates medical terms written by clinicians about patient diagnosis and treatment into codes that are recognised nationally. The Trust was subject to the Payment by Results clinical coding audit during the reporting period by the Audit Commission and the error rates reported in the latest published audit for that period for diagnosis and treatment coding (clinical coding) were: •Primary diagnoses correct 91.10% •Secondary diagnoses correct 92.20% •Primary procedures correct 84.20% •Secondary procedures correct 84.60% The services reviewed within the sample were 135 finished consultant episodes (FCEs) in general medicine. The primary procedure has only 19 procedure codes to be audited and three were found to have errors. To meet the 90% target there could have been only one error. The results should not be extrapolated further than the actual sample audited. The errors include both coder and documentation errors of which the coding errors will be fed back to the coders as a group and individually. The documentation errors will be taken to directorate meetings. Depth of coding and key metrics is monitored by the Trust in conjunction with mortality data. Monthly coding audits are undertaken to provide assurance that coding reflects clinical management. Our coders organise their work so that they are closer to the clinical teams. This results in sustained improvements to clinical documentation. This supports accurate clinical coding and a reduction in the number of Healthcare Resource Group changes made. This is the methodology which establishes how much we should get paid for the care we deliver. We will continue to work hard to improve quality of information because it will ensure that NHS resources are spent effectively. North Tees and Hartlepool Foundation Trust will be taking the following actions to improve data quality. Specific issues highlighted within the audit have been fedback to individual coders and appropriate training planned where required. Coders currently code from discharge summaries within medicine which does not give them a full detail therefore, in approximately 10 weeks time, coders will share access to paper light records and scanned notes. A lead quality coder will be employed to provide assurance of data quality in 2013-2014. 48 Annual Quality Account 2012-2013 Part 3: Review of Quality Performance Part 3 of this Quality Account provides an opportunity for the Trust to report on progress against additional quality indicators which are not included in part 2 ‘performance against quality improvements priorities’. Where possible we have provided additional sources of external data in section 3A to provide members of the public with as much useful information as possible. Part 3A of this report will describe Trust performance against local quality indicators. Part 3B will describe Trust performance against national priorities from the Department of Health Operating Framework, Appendix B of the Compliance Framework. Part 3C contains the additional Department of Health Core Indicator Set, which includes 9 indicators. The data containted within this section comes from the NHS Information Centre indicator portal (NHS IC). Part 3A: Trust performance against additional Quality Performance Indicators In addition to the three local priorities outlined in part 2, the indicators below further demonstrate that the quality of the services provided by the Trust over 2012-2013 has been positive overall. In keeping with the format of the Quality Account, additional indicators will be presented under the headings of patient safety, effectiveness of care and patient experience. Indicators chosen reflect indicators that have been or remain of interest to key stakeholders as identified through consultation, discussion or enquiries. The indicators that will be reported in this section include: Patient safety Effectiveness of care Patient Experience • MRSA bacteraemia. • Pulmonary embolism (PE) or deep vein thrombosis (DVT). • You're welcome. • SHMI. • Medication Errors. • Post-op Haemorrhage or Haematoma. • Learning disabilities (LD). • Safety Thermometer. • NEQOS effectiveness indicators. • Pressure Ulcers. • Safeguarding (adults and children). • IPNMB. • Complaints and compliments. • Sensory loss. • PROMS. The Quality Account this year reports on the indicators above, the only change from last year's Quality Account is that we have not included delivering same sex accommodation. The reason being is that the Trrust has had no breaches and continues to deliver the highest standards of privacy and dignity for its patients. The reason that these indicators are being reported is because the Trust and/or stakeholders believe that these indicators should remain a focus for improvement for the coming year. Further rationale is provided in relation to the individual outcomes of these indicators and are shared on the following pages. The Trust therefore felt that this indicator will only need to be reported on if this changes in the future. The remaining 2011-2012 Quality Account indicators remain in this section with additional indicators being added. Annual Quality Account 2012-2013 49 Patient Safety 1. Methicillin-Resistant Staphylococcus Aureus (MRSA) bacteraemia The importance of personal hygiene is fully understood by all staff and is visible through the bare below the elbow policy and the presence of alcohol gel dispensers and hand-washing facilities. Further improvements to our environment and practices are constantly being implemented and evaluated. Many patients carry MRSA on their skin, this is called colonisation. It is important that we screen patients when they come in to hospital so that we know if they are carrying MRSA. Screening involves a simple skin swab. If positive, we can provide special skin wash that helps to get rid of MRSA. Our rate of screening for MRSA is very high and we believe that this has helped us to achieve the results reported during the course of the last two years. Screening patients on admission showed that around 200 patients every month bring MRSA into hospital on their skin. This carriage will not harm them unless they become very poorly. How did we do? In 2012-2013, our organisation performed well against regional and national standards in relation to almost all aspects of infection prevention and control and this reflects the hard work of all staff, both clinical and non-clinical, in ensuring that high standards are maintained all of the time. We reported two hospital MRSA bacteraemia during 2012-2013, having had over 560 days without a case. In both cases the patients had MRSA on their skin when they arrived in hospital. Despite our best attempts to decolonise them (treatment to remove skin contamination) we were unable to prevent a bacteraemia. The North East Quality Observatory System benchmark data reports the Trust at 0.00* cases of MRSA bacteraemia per 1,000,000 bed days compared to a national mean of 11.10*. *Data correct as of autumn v6.0 Acute Trust Quality Dashboard – period Q2 2012-13 MRSA Bacteraemia (April 2006 - March 2013) 24 22 20 18 16 14 12 10 8 6 4 2 0 2006/2007 2007/2008 2008/2009 2009/2010 Hospital acquired total Year 2010/2011 2011/2012 2012/2013 Community acquired total 2006/2007 2007/2008 2008/2009 2009/2010 2010/2011 2011/2012 2012/2013 Hospital acquired total 22 16 9 5 4 0 2 Community acquired total 14 12 3 6 4 1 6 Quarter Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Hospital acquired 4 8 7 3 6 2 6 2 5 0 3 1 2 2 1 0 0 0 3 1 0 0 0 0 0 0 2 0 Community acquired 5 4 3 2 3 4 2 3 0 1 2 0 3 2 0 1 1 0 3 0 0 0 0 1 2 3 0 1 The trend over the last seven-years can be seen in the graph and table above. 50 Annual Quality Account 2012-2013 2. Summary Hospital-level Mortality Indicator (SHMI) The SHMI indicator provides an indication on whether the mortality ratio of a provider is as expected, higher than expected or lower than expected when compared to the national baseline in England. SHMI mortality data should be reviewed against other sources of mortality data including Hospital Standardised Mortality Ratio (HSMR). SHMI includes deaths up to 30 days after discharge and does not take into consideration palliative care. Although the Trust SHMI has remained within the as expected range at 110, the Trust has undertaken a comprehensive review of cases to help understand where and why deaths outside of hospital occur. This review demonstrates that there are a high number of patients who have been discharged home to die in accordance with their wishes and this has affected the hospital SHMI score. The Trust is working with commissioners to review pathways of care and support patient choice of residence at end of life wherever possible. The data below has been taken from the Acute Trust Quality Dashboard v6.00. The other Trusts identified are from the north east, and have been anonymised. Summary Hospital-level Mortality Indicator (SHMI) Emergency & Elective RY Q1 1213 National Mean North Tees Trust 1 Trust 2 Trust 3 Trust 4 Trust 5 Trust 6 Trust 7 100 110.50 98.70 108.50 93.60 104.10 104.60 101.30 92.30 Summary Hospital-level Mortality Indicator (SHMI) Emergency & Elective 115.00 110.00 105.00 100.00 95.00 90.00 85.00 80.00 North Tees & Hartlepool Trust 1 Trust 2 Trust 3 Trust 4 Trust 5 Trust 6 Trust 7 Summary Hospital-level Mortality Indicator (SHMI) - Emergency & Elective National Mean 3. Medication errors Between April and February 2013, staff reported 527 medication related incidents across hospital and community services of which 472 originated within the Trust. Some of these will have been actual incidents and some will have been near misses. A near miss is the name for a situation when the error did not actually happen but the circumstances were such that there was potential for an error. In the 2011-2012 Quality Accounts, it was reported that 372 medication related incidents across hospital and community services. Medication errors can happen at a number of steps in the process for example, when the medication is prescribed, when it is dispensed by pharmacy, or when it is administered to the patient. Annual Quality Account 2012-2013 51 There are many thousands of contacts made by our hospital and community teams every day. We estimate there could be around 12 million staff interactions with medications during a year which results in a very low risk of error when the reported incidents are considered against the proportion of: •The number bed days (around 400,000); •The number of drugs a patient might be given, possibly five different drugs three or four times a day; •The steps in the process (prescribing, dispensing and administration). We have a culture of encouraging all staff to report actual medication errors as well as opportunities for error. The figures above show that our staff are doing an excellent job and that patient safety is paramount. The reason for encouraging reporting is not to look for blame; it is very much about understanding why these rare things happen, learning from them and putting in systems which will improve things in the future. Actions taken by the Trust: We have undertaken a number of actions this year to further raise awareness of opportunity for medication errors. The pharmacy department increased the number of ward based pharmacists. It also increased the number of wards operating the system of Patient Orientated Pharmacy (POP). Both of these allow the early identification of drug interactions and dosing errors by pharmacy staff working closely with patients, nursing and medical staff. Additionally the POP service increases patient safety as medication is administered from individual patient lockers reducing the risk of incorrect selection of medication. The Education and Organisation Development Directorate and pharmacy are working together to ensure that all staff involved with the prescribing or administration of medicines receive ongoing, evidence based training to allow them to practice safely. In the last year we have revised the training needs analysis to ensure all staff groups who are involved in medicines management receive appropriate training. We have introduced mandatory training for all new staff involved in preparation, prescribing or administration of injectable medicines. E-learning packages and workbooks have been developed to ensure multiple access points are available for training. In depth audit and training programmes have been introduced to areas such as paediatrics and antibiotic prescribing. The Community Directorate has developed a competency based proficiency tool to support staff involved in medication errors including lessons learnt. Our positive reporting culture enables staff to understand what contributes to actual or potential error and helps them to come up with solutions to continually review and reduce risk. This is the reason why we have checks and balances in place across the Trust to improve patient safety and to help our staff in any situation, whether they are caring for patients in our hospitals or in the community. The latest benchmarking data published by the North East Quality Observatory System demonstrates that the Trust rate of medication errors is 42.5% lower than the national mean rate with 4.12* per 1,000 bed days against a national rate 7.17*. *Data correct as of autumn v6.0 Acute Trust Quality Dashboard – period Oct11- Mar12. 52 Annual Quality Account 2012-2013 4. Safety Thermometer The Trust contributes to the Safety Thermometer which reports on four areas of harm: •Pressure ulcers; •Patient falls; •Catheter acquired urine infection; •VTE. The Trust has been in discussion with the national leads due to problems relating to data upload and accuracy. We continue to submit data for our wards and community services; however we continue to have concerns about the validity of data. The Trust currently triangulates different sources of pressure ulcer data in order to provide an accurate reflection of performance. Safety Thermometer data shows regional benchmarking data for the Trust in relation to new pressure ulcers as follows: as far as we are aware, we are only one of a small number of Trusts nationally who include community data with hospital data, which makes it difficult to accurately compare results. Pressure Ulcers - All Pressure Ulcers - New Falls with harm UTI + Catheter All VTEs *North Tees & Hartlepool (inc. community data) 5.88% 1.71% 1.93% 1.93% 7.34% Trust 1 5.34% 1.07% 0.72% 1.19% 2.34% Trust 2 8.30% 1.54% 1.22% 0.86% 0.30% Trust 3 6.35% 0.96% 1.44% 2.99% 7.57% Trust 4 5.97% 2.42% 0.94% 1.07% 1.53% Trust 5 3.02% 1.28% 0.21% 0.74% 2.15% National Averages 5.34% 1.20% 1.03% 1.12% 2.87% *North Tees and Hartlepool NHS Foundation Trust include hospital and community data. Pressure Ulcers from the Acute Trust Quality Dashboard v6.00 Incidence of patients with pressure ulcers per 1,000 admissions Sep-12 National Mean North Tees & Hartlepool Trust 1 Trust 2 Trust 3 Trust 4 Trust 5 Trust 6 Trust 7 NE SHA 3.65 2.56 1.61 5.24 1.05 8.22 6.89 2.66 2.03 3.08 Data from the Acute Trust Quality Dashboard v6.00 identifies the Trust as a positive outlier against the national mean in relation to pressure ulcers. The reason for the differences in these two data sets is likely to be due to the fact that Safety Thermometer data includes community data as hospital data. The Acute Trust Quality Dashboard measures only hospital data. 53 Annual Quality Account 2012-2013 Venous Thromboembolism VTE Related Readmission Rate The Healthcare Evaluation Data (HED) dataset identifies the Trust as one of the top three performers in the North East, in relation to the number of patients who are readmitted to hospital due to a VTE. The Trust has a consultant led committee that provide leadership and monitoring of VTE. 0.16% 0.14% 0.12% 0.1% 0.083% 0.08% 0.06% 0.04% 0.02% 0% North East Trusts North Tees and Hartlepool NHS Foundation Trust Data taken from 2011-2012 Q3 and Q4, 2012-13 Q1 and Q2 (Year reporting period) 5. Safeguarding Adult Safeguarding The Trust has delivered Passionate about Adult Safeguarding training on a monthly basis during 2012-2013. These are innovative and intensive week long training events that combine workshops covering key topics. This is open to all Trust staff as we recognise that each of us plays a valuable role in Adult Safeguarding. Every member of staff is provided with an Adult Safeguarding card which contains the contact numbers to raise any adult safeguarding alerts and for the independent mental capacity advocate service. The Trust is raising awareness amongst staff and the public through displays and communication campaigns. The following table reflects the number of staff currently trained in the following categories: Mental capacity staff training Deprivation of liberty safeguarding (DOLS) People With Learning Difficulty (PWLD) Adult Safeguarding Individual bespoke training 54 Annual Quality Account 2012-2013 131 staff 71 staff 102 staff 77 staff 265 staff Children’s safeguarding The Trust has continued to deliver on all key performance indicators relating to children’s safeguarding and has received significant assurance from external agencies including Audit North and multi agency OFSTED review in Hartlepool. We have implemented a new in-house safeguarding children training programme, which enables us to deliver targeted training to meet the needs of the organisation and maintain high levels of compliance with standards. Young people who helped the children’s safeguarding team produce e-safety posters. Our Trust has a seat on all three Local Safeguarding Children’s Boards (LSCBs) – Hartlepool, Stockton-on-Tees and County Durham and we continue to provide assurance through Section 11 of the Children’s Act that we are discharging our statutory responsibilities. Section 11 of the Children’s Act provides a statutory framework for arrangements to promote the welfare of children, the Trust's safeguarding for children operation group audits performance in relation to statutory guidance. Safeguarding There are a number of examples of excellent development work being undertaken. One example is the development of an adult risk behaviours assessment tool which has been introduced in A&E/Urgent care. The purpose of this tool is to identify potential safeguarding concerns when an adult presents with a behaviour which may impact on their ability to parent (domestic abuse, substance misuse). The Trust continues to ensure that safeguarding children and adults is a key priority and closely monitors standards. 55 Annual Quality Account 2012-2013 Effectiveness of care 1. Pulmonary embolism (PE) or deep vein thrombosis (DVT) following surgery. Dr Foster reporting period – February 2012 to January 2013 (rolling 12 month period of latest data). The rate of PE or DVT is above the national average value of 100. The expected number of incidents over this time period was 30.90 and the Trust has had 36, giving a Relative Risk (RR) of 116.40. See chart and graph below: Cases of PE or DVT following surgery Observed Expected Relative risk Low High 36 30.90 116.40 81.50 161.10 1,000 Relative Risk 800 600 400 200 0 20 40 60 80 100 120 Expected Deaths *Data taken from Dr Foster 2. Post-op Haemorrhage or Haematoma. Cases of haematoma (bruise) or haemorrhage (bleed) requiring a procedure following surgery, Dr Foster reporting period – February 2012 to January 2013 (rolling 12 month period of latest data). The rate of Post-op haemorrhage or haematoma for the Trust is well below the national average value of 100. The Trust is one of the best performers in the country. The expected number of incidents over this time period was 10.33 and the Trust has had 3, giving a Relative Risk (RR) of 29.05. See following chart and graph: Observed Cases of haematoma or haemorrhage requiring a procedure following surgery 56 Annual Quality Account 2012-2013 Expected 3 10.33 Relative risk 29.05 Low High 5.84 84.49 1,000 Relative Risk 800 600 400 200 0 10 20 Expected Deaths 30 40 *Data taken from Dr Foster 3. Selected quality performance indicators and national benchmarks from the North East Quality Observatory System (NEQOS) NEQOS collects benchmark data on Trusts for a number of clinical indicators. The following indicators provide an indication of Trust performance when compared to other NHS Trusts nationally. 2012/13 2011/12 Effectiveness indicator Date Trust value National Mean Trust Values 95th percentile wait for elective inpatient treatment (weeks) Nov-12 20.80 21.30 18.10 Median wait for elective inpatient treatment (weeks) Nov-12 9.61 8.73 8.77 Delayed transfer of care per 1,000 occupied beds – NHS responsibility Q2 12/13 783.10 669.50 21.20 % of all admissions who have had venous thromboembolism risk assessment Sep-12 91.60% 93.90% 94.40% Medication errors per 1,000 bed days Oct 11Mar 12 4.12 7.17 3.29 Admitted patient care - % valid data (average for all fields) Nov-12 98.80% 98.11% 99.10% Outpatient - % valid data (average for all fields) Nov-12 91.00% 95.87% 91.40% Accident and emergency - % valid data (average for all fields) Nov-12 99.70% 97.44% 99.90% Admitted patient care - % records submitted with valid HRG on first submission Oct-12 99.00% 96.80% 99.80% Staff recommendation of the Trust as a place to work (last CQC survey) 2011 54.60% 52.40% 61.80% Staff recommendation of the Trust as a place to receive treatment (last CQC survey) 2011 63.10% 62.80% 65.60% Overall medical trainees global satisfaction score (last GMC survey) 2012 83.10% 78.60% 78.70% Consultant clinical supervision trainers given to their trainees 2012 91.60% 86.80% 66.40% *Information taken from Release 6.00 Winter 2012-2013. 2011-2012 data taken from the 2011-2012 Quality Report 4. The Integrated Professional Nursing and Midwifery Board (IPNMB) We believe that we are the first hospital and community professional board of this type in the country. The IPNMB is chaired by the Director of Nursing, Patient Safety and Quality. Membership includes senior nursing and midwifery leaders from across both acute and community settings: working collaboratively at a strategic level relating to professional, operational and clinical developments and pathways. This board oversees strategy, standards and assurances in relation to delivery of high quality nursing and midwifery care. Annual Quality Account 2012-2013 57 All graduate profession: The Trust is committed to ensuring that all mentors in practice are prepared for the delivery of the all graduate nurse education programmes. Development of a practice passport, issued to all nurses, midwives and health visitors will enable mentors to record their progress, continuous professional development and provide evidence of meeting the required Nursing and Midwifery Council (NMC) Standards. In September 2012, the Chief Nursing Officer (CNO) for England and the Department of Health Nurse Director provided an opportunity to create a new national strategy for nursing and midwifery by inviting discussion on a consultation to develop a culture of compassionate care, creating a vision for nurses, midwives and caregivers. This vision is underpinned by six fundamental values: (referred to as the six Cs) •Care •Compassion •Competence •Communication •Courage •Commitment There are six areas of action to support professionals to deliver excellent care. Taking a leading edge, these fundamental values will be integrated into both the Trust Nursing and Midwifery Strategy and be adopted by all Trust staff. In 2009, the Trust introduced its modern apprentice scheme; this two year programme delivered in partnership with local further education colleges provides the Trust with an opportunity to ensure that unregistered staff have the skills, knowledge and values acquired to be part of our nursing team. This scheme has been recognised by the CNO for England. Midwifery assistant Ruth Waterman. 58 Annual Quality Account 2012-2013 Patient experience 1. You're welcome You're Welcome is a Department of Health quality criteria for young, people friendly, health services which the Paediatric service are participating in. The service will be assessed by a panel including young people, of their provision within nine topical areas: 6. Accessibility 7. Publicity 8. Confidentiality and consent 9. Environment 10.Staff training, skills, attitudes and values 11.Joined-up working 12.Young people’s involvement in monitoring and evaluation of patient experience 13.Health issues for young people 14.Sexual and reproductive health services 2. People with Learning Disabilities The Trust held successful events in September 2012 and December 2012. These events were focused on the broad issues of protecting those most vulnerable in our communities. Post Winterbourne View Interim Report prompted us to commission the performance Out of Sight, which is an interactive drama which was produced and performed by Operating Theatre. The December 2012 event also promoted the recently adopted 'Deciding Right' approach to advance decisions about end of life choices. Hospital Tours for people with learning disabilities have been introduced in 2012 across both the sites and are proving to be a success. Every ward has been provided with a copy of the Winterbourne View Interim Report as part of their learning resource files. Learning resource files have been developed during 2012 and are in place as a support tool to dealing with people with learning disabilities. MCA, MHA and DoLS codes of practice and posters have been distributed for quick reference. We have updated the Learning Disability Pathways of Care and will continue to refine this in 2013. We have strengthened the Trust's People with Learning Disabilities Strategy Group and this includes people with LD. The Board of Directors have been updated in relation to the Francis Report, Winterbourne View report, Airedale report, Six Lives report, Care Ombudsman report and recently have been briefed on the Savile enquiry. Winterbourne review – Easy Read version www.wp.dh.gov.uk/publications/files/2012/12/easy-read-of-final-report.pdf The Trust hosted multi agency conferences in Hartlepool to highlight its 'Passionate About Safeguarding Work'. Over 300 people attended and provided excellent feedback. 59 Annual Quality Account 2012-2013 3. Pressure ulcers (also known as decubitus ulcer or pressure sores) Reducing opportunity for pressure ulcers has been a high priority for all healthcare staff in the community and in hospital. (See section 3, Patient Safety point 4) Actions taken by the Trust: Over the year, training in the prevention and management of pressure ulcers has been further enhanced. Every pressure ulcer graded as category two, three or four that is acquired whilst in our care is subject to a full investigation to help us to understand whether it was avoidable or not and importantly, whether there is anything that we can learn. At the end of 2011-2012 a new body-mapping process was introduced. This should be completed on admission to hospital or admission onto a district nursing caseload. It is also completed on discharge from hospital for all patients who have a wound and the information passed onto the next care provider. The IPNMB oversee actions to pursue continuous improvement in performance. Bi-annual pressure ulcer prevalence audits are carried out across both the hospital and community services. Our specialist nurses support bespoke training and support clinical teams to maximise treatment options. In 2013-2014, we will continue to focus on the reduction of avoidable pressure ulcers in hospital and in the community setting. At the end of 2012-2013 a new care bundle is to be introduced. The SSKIN (Surface, Skin inspection, Keep moving, Incontinence, and Nutrition) bundle focuses on interventions proven to reduce the risk of pressure ulcers occurring. The Trust participated in a research study ending in 2011 to assist the development and validation of a patient reported outcome measure of health related quality of life for patients with pressure ulcers (PUQOL). This was part of a programme of research and the team have submitted an expression of interest to be a recruiting site for a further two research studies to commence in 2012. The Pressure Ulcer Quality of Life Adjusted Years (PUQALY) is a small sample study of patients with pressure ulcers and involves the completion of a nurse administered questionnaire. The Pressure 2 trial proposes to compare high specification foam mattresses and alternating pressure mattresses for patients at high risk of pressure ulcers in hospital settings. It is anticipated portfolio studies will commence in early 2013 with funding support for research nurse input from the CLRN. 60 Annual Quality Account 2012-2013 How did we do? Dr Foster data for February 2012 to January 2013 (rolling 12 month period of latest data) demonstrates that the Trust is similar when benchmarked nationally in relation to rate of hospital acquired decubitus ulcers in patients discharged from surgical and medical wards/ departments. The relative risk is 104.86, which means that for 100 patients that acquire a pressure ulcer in the average hospital in England, 104.86 patients acquire one in our care. Observed Cases of decubitus ulcer amongst surgical or medical discharges. Expected 252 Relative risk 240.31 Low 104.86 High 92.31 118.64 1,400 1,200 Relative Risk 1,000 800 600 400 200 0 1 201 401 Expected Deaths Dr Foster data for January-December 2011 (reported in the 2011/2012 Quality Report), demonstrates that the Trust performs well nationally. The relative risk of acquiring decubitus ulcers in patients discharged from surgical and medical wards/departments is 84.40; this means that for 100 patients that acquire a pressure ulcer in the average hospital in England, 84.4 patients acquire one in our care. NB: Data obtained from Dr Foster and the 2011/2012 Quality Report. 4. Spiritual and emotional care of patients at the end of their life In November 2011, the National Institute of Health and Clinical Excellence (NICE) published guidance describing the importance of spiritual and religious support to patients approaching end of life. The guidance specifically referred to the role of chaplains in end of life care. We were very pleased to read the guidance because it promotes the approach that our Trust has taken since July 2009 to meet the needs of patients and families when faced with the knowledge that end of life is near. Actions taken by the Trust: Since July 2009, this Trust has routinely referred patients on the end of life care pathway to the chaplaincy team. During 2012-2013, 713 patients were referred by our staff to this pioneering service provided by the Trust chaplains. They provide spiritual, pastoral and emotional support to patients, families and staff. Only 14 patients declined their support during the year. 396 patients welcomed and received multiple visits. This service offers added value to the quality of overall care provided to patients and their loved ones and has highlighted the importance of this aspect of support to the dying patient. This innovative and groundbreaking approach has been recorded for national television and featured in publications. Annual Quality Account 2012-2013 61 This initiative has been so successful that in August 2012, the service was extended into the community. We received funding to run a pilot over 18 months to address the spiritual and pastoral needs of patients in the community. Initially, this was for patients on or near the end of life, but practice has indicated that the service needs to be offered to patients earlier in the palliative care stage, in order to build up a relationship with the patient and offer a meaningful service. Perhaps because of management restructuring in the community, referrals have been less frequent than in the acute trust, but they are now beginning to gather momentum. When this service is allied to the use of the Family’s Voice (carers diary), we believe that our philosophy of care results in a better experience for patients, relatives and carers as well as better job satisfaction for clinical staff and chaplains. The following chart and table provides data relating to chaplain referrals: Chaplain Referrals, Received more than 1 visit and Declined Support 75 70 65 60 55 50 45 40 35 30 25 20 15 10 5 0 Jan-12 Feb-12 Mar-12 Apr-12 May-12 Jun-12 Referrals Jan12 Feb- Mar12 12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Received more than 1 visit Apr- May12 12 Jun12 Jul- Aug12 12 Jan-13 Feb-13 Mar-13 Declined Support Sep12 Oct- Nov12 12 Dec12 Jan13 Feb- Mar13 13 Referrals 52 51 47 62 54 48 64 46 53 64 57 48 68 51 50 Received more than 1 visit 35 34 28 37 33 30 42 4 8 41 43 21 41 25 27 2 2 0 4 1 0 1 0 0 2 1 0 1 1 0 Declined Support 5. Formal complaints and compliments Actions taken by the Trust: The Trust continues to work hard to improve customer satisfaction through patient experience. In 2009-2010 we started to record the number of compliments received. The number of thank you and complimentary comments has increased year on year. Trends in complaints and compliments can be seen in the table below. We do recognise that we don’t always get things right and this is why we have a dedicated patient relations team to listen to and investigate any concerns or complaints. We continue to work hard to provide high standards of clinical care delivered with dignity and compassion for everyone. Feedback from patients is important because it helps us to understand what we do well and what we can improve further. 62 Annual Quality Account 2012-2013 How did we do? The number of formal complaints received over the last four-years is shown in the table below: Year Complaints Compliments 2009 2010 2011 2012 358 341 371 396 2,212 3,786 5,087 5,414 External feedback The North East Quality Observatory System benchmark data reports the Trust at 3.69* written complaints per 1,000 episodes of care, which is significantly lower than the national mean of 4.43*. *Data correct as of autumn v6.0 Acute Trust Quality Dashboard – period Q1 2012-13 In 2013 the CQC undertook an unannounced review of services which included Outcome 16: Assessing and monitoring the quality provision. The full CQC report describes the observations and evidence reviewed. The CQC provided positive feedback regarding the numerous ways the Trust evaluates patient care and reported that any issues raised or complaints made by people had been dealt with promptly and appropriately. North East Quality Observatory System reports (2010-2011), for inpatient experience measure for the Trust as 7.60* against a national mean score of 7.40*. *Data correct as of autumn v6.0 Acute Trust Quality Dashboard – period 2010/11 6. Sensory loss In response to feedback from patients with sensory loss the Trust has delivered a targeted campaign to ensure a focus on quality of experience for people with disability. This work is ongoing. During 2012 progress was made in the following areas: •Scoping all wards and department across both hospital sites to look at the facilities for people with sensory loss and/or impairment; •Work with audiology/ophthalmology to establish best practice and recommend equipment and facilities for use on wards; •Develop a standard range of equipment to be available on all wards in 2013; •Develop sensory loss awareness training; •Re-establish the mobile phone function for people with hearing loss into the Patient Relations department; •Review and renew leaflets and resources in use for supporting patients with sensory loss impairment; •Support and influence the Trust Equality and Diversity Working Group and its action plan; •Work with Teesside Safeguarding Vulnerable Adults in Hospital Group to ensure admission and discharge processes are sensitive to the needs of patients with sensory loss impairment and reasonable adjustments are highlighted; •Involve people with sensory loss in work streams. 63 Annual Quality Account 2012-2013 7. PROMS The Trust participated in the original pilot for PROMS, and as such, this is well embedded into practice with high numbers of returns for our patients admitted via elective pathways for hip, knee replacement, hernia repair and varicose vein surgery. The Trust has been identified as an outlier in relation to hips. In response it has undertaken a comprehensive review of hips PROMS cases and has established that, patients score positively in relation to the outcome of their operation; however patients are scoring less positively in their general health. A review of case notes has identified that the low score relates to overall health and not to the surgery itself in the majority of cases. The following table reflects the four PROMS measures compared with the other North East Trusts: Acute Trust Quality Dashboard (Nov v6.0) Trusts National Mean IH23 IH24 IH25 IH26 Patient Reported Outcome Measure - % Patients reporting an improvement following hip replacement (Apr 11-Mar 12) 1112 Patient Reported Outcome Measure - % Patients reporting an improvement following knee replacement (Apr 11-Mar 12) 1112 Patient Reported Outcome Measure - % Patients reporting an improvement following varicose vein procedure (Apr-Jun 12) 1213 Patient Reported Outcome Measure - % Patients reporting an improvement following hernia procedure (Apr-Jun 12) 1213 Annual Quality Account 2012-2013 Trust 2 Trust 3 Trust 4 Trust 5 Trust 6 Trust 7 87.00% 83.90% 86.90% 87.10% 88.50% 89.50% 78.60% 83.00% 88.00% 78.70% 82.10% 81.00% 58.30% 79.80% 81.00% 78.50% 78.50% 82.00% 39.20% NO DATA NO DATA NO DATA 58.10% NO DATA 0.00% NO DATA 44.40% 46.00% 45.00% 33.30% 54.50% 45.50% 53.80% 39.10% 62.50% 57.10% *Data taken from the Acute Trust Quality Dashboard v 6.0 64 North Tees & Trust 1 Hartlepool Part 3B: Performance from key national priorities from the Department of Health Operating Framework, Appendix B of the Compliance Framework The Trust continued to deliver on key cancer standards throughout the year; two week outpatient appointments, 31 days diagnosis to treatment and 62 day urgent referral to treatment access targets. The Trust demonstrated a positive position with evidence of continuous improvement against the cancer standards introduced in the Going Further with Cancer Waits guidance (2008). www.connectingforhealth.nhs.uk/nhais/cancerwaiting/cwtguide7.pdf The compliance framework forms the basis on which the Trust's Annual Plan and in year reports are presented. Regulation and management of these remain paramount in the Trust to ensure patient safety is considered in all aspects of operational performance and efficiency delivery. The current performance against national priority, existing targets and cancer standards are demonstrated in the table below with comparisons to the previous year. Existing commitments 4 hour emergency care target National Standard Performance 2012-13 Performance 2011-12 Achieved 95% 97% 98.13% √ In patient waiting time 26 weeks 0 0 √ Out patient waiting time 13 weeks 0 0 √ 100% 100% 100% √ Year on year improvement 40% 0.29% √ Readmission within 28 days of non medical cancellation 100% 100% 100% √ Delayed transfers of care 3.50% 2.09% 2.43% √ 18 weeks maximum wait referral to treatment (RTT)- admitted pathways 90% 92.53% 94.07% √ RTT 95th percentile wait – admitted pathways 23 weeks 20.6 weeks 19 weeks √ 95% 99.25% 99.22% √ RTT 95th percentile wait – non admitted pathways 18.3 weeks 11.9 weeks 11.6 weeks √ 18 weeks maximum wait referral to treatment (RTT) – incomplete pathways 92% (Operating Framework 2012-13) 96.75% 97.16% √ 28 weeks 16.94 weeks 16.6 weeks √ MRSA (post 48 hours) 1 2 0 X C dIff (post 48 hours) 44 61 68 X 0 0 0 √ Full Compliance Full Compliance √ Access to rapid access chest pain clinics within 2 weeks of referral from GP Cancelled operations for non medical reasons 18 weeks maximum wait referral to treatment (RTT) - non admitted pathways RTT 95th percentile wait – incomplete pathways Eliminating mixed sex accommodation Compliant with access to healthcare for patients with learning disabilities 65 Annual Quality Account 2012-2013 Cancer standards National Standard Performance 2012-13 Performance 2011-12 Achieved 14 day maximum wait for a first outpatient appointment following urgent GP referral 93% 95.4% 93.58% √ 14 day maximum wait for a first outpatient appointment for breast symptomatic referral 93% 92.6% 94.71% X 31 day maximum wait to decision to treat 96% 99.4% 99.25% √ 31 day maximum wait decision to treat to subsequent treatment (drug therapy) 98% 99.8% 100% √ 31 day maximum wait decision to treat to subsequent treatment (surgery) 94% 98.3% 95.91% √ 62 day maximum wait referral to treatment - all cancers 85% 88.1% 88.20% √ 62 day maximum wait from screening recall to treatment 90% 94.1% 95.76% √ Criteria for 62 day cancer wait: The indicator is expressed as a percentage of patients receiving first definitive treatment for cancer within 62 days of an urgent GP referral for suspected cancer. An urgent GP referral is one which has a two week wait from date that the referral is received to first being seen by a consultant. The indicator only Includes GP referrals for suspected cancer (i.e. excludes consultant upgrade and screening referrals and where the priority type of the referral in National Code 3 - Two week wait). The clock start date is defined as the date that the referral is received by the Trust. The clock stop date is the date the first definitive cancer treatment as defined in the NHS Dataset Set Change Notice (day of the year, not 24 hour periods). To note: Cancer Standards position was not finalised at time of print. Part 3C: Department of Health Core Indicator Set The data for all nine indicators has been taken from the NHIS IC indicator portal. 1. Summary Hospital-level Mortality Indicator (SHMI) - Deaths associated with hospitalisation, England, October 2011-September 2012 The North Tees and Hartlepool NHS Foundation Trust considers that this data is as described for the following reason. SHMI mortality data when reviewed against other sources of mortality data including Hospital Standardised Mortality Ratio (HSMR) and when benchmarked against other NHS organisations will provide a robust overview of overall mortality performance. The North Tees and Hartlepool NHS Foundation Trust has taken actions to improve this score, the quality of its services, by undertaking a comprehensive review of cases to help understand where and why deaths within 30days of discharge occur. Work to understand SHMI is described in public board reports and in Part 2 of this document. The SHMI indicator provides an indication on whether the mortality ratio of a provider is as expected, higher than expected or lower than expected when compared to the national baseline in England. 66 Annual Quality Account 2012-2013 SHMI includes deaths up to 30 days after discharge and does not take into consideration palliative care. Although the Trust SHMI has remained within the as expected range at 1.08 it is higher than HSMR. Provider National Average Trust Value OD Banding 1.00 1.08 2 National Average Trust Value OD Banding Highest SHMI Trust Value in the country 1.00 1.21 1 Lowest SHMI Trust Value in the country 1.00 0.68 3 North Tees and Hartlepool Nhs Foundation Trust Provider NB: Data from the Health and Social Care Information Centre (HSCIC). OD banding descriptions: OD banding 1 - higher than expected OD banding 2 - as expected OD banding 3 - lower than expected 2. Percentage of deaths with palliative care coding, Oct 2011 - Sept 2012 21.60% of patients that die in or within 30 days of discharge from the Trust are coded as patients receiving palliative care. This has been evidenced through the SHMI mortality review and reported to the board. The benchmark data identifies the Trust as having a higher proportion of patients receiving palliative care admitted to hospital than many other organisations in the North East and significantly more than the average across the hospitals in England. Provider Diagnosis Rate Combined Rate North Tees And Hartlepool NHS Foundation Trust 21.60 21.60 South Tees Hospitals NHS Foundation Trust 15.70 15.70 South Tyneside NHS Foundation Trust 20.60 26.90 The Newcastle Upon Tyne Hospitals NHS Foundation Trust 19.40 19.40 Northumbria Healthcare NHS Foundation Trust 24.00 24.30 Gateshead Health NHS Foundation Trust 13.20 13.60 County Durham And Darlington NHS Foundation Trust 13.20 13.20 City Hospitals Sunderland NHS Foundation Trust 11.50 11.50 National Average 19.00 19.20 National Highest and Lowest Trust Diagnosis Rates Provider Diagnosis Rate Combined Rate Highest Trust Diagnosis Rate in the country 43.30 43.30 Lowest Trust Diagnosis Rate in the country 0.20 0.20 NB: Data from the Health and Social Care Information Centre (HSCIC). The latest data available to the Trust for the reporting year (01 April 2012 – 31 March 2013) relating to the palliative care coding is as follows: 14.84% of patients that die in or within 30 days of discharge from the Trust are coded as patients receiving palliative care. 67 Annual Quality Account 2012-2013 3. PROMS; patient reported outcome measures. The North Tees and Hartlepool NHS Foundation Trust considers that this data is as described for the following reasons. The Trust has been identified as an outlier in relation to hips. The North Tees and Hartlepool NHS Foundation Trust has taken the following actions to improve this score, and so the quality of its services, by undertaking a comprehensive review of hips PROMS cases and has established that, patients score positively in relation to the outcome in related to their operation; however patients are scoring less positively in their general health. A review of case notes has identified that the low score relates to overall health and not to the surgery itself in the majority. The Trust participated in the original pilot for PROMS, and as such, this is well embedded into practice with high numbers of returns for our patients admitted via elective pathways for hip, knee replacement hernia repair and varicose vein surgery. North Tees and Hartlepool NHS Foundation Trust PROMS Procedure Group National Average Adjusted average health gain Groin hernia 0.090 0.052 Varicose vein 0.089 No Data Hip replacement 0.429 0.392 Knee replacement 0.321 0.326 Highest and Lowest National health gain Trust scores National Average Highest adjusted average health gain Lowest adjusted average health gain Groin hernia 0.090 0.153 0.017 Varicose vein 0.089 0.138 0.027 Hip replacement 0.429 0.500 0.328 Knee replacement 0.321 0.408 0.201 PROMS Procedure Group NB: Data from the Health and Social Care Information Centre (HSCIC) - April 2011 to December 2012 (published 9th May 2013) – Provisional. For additional information relating to PROMS see section 3A Patient Experience point 7. April 2011 to December 2012 (published 9th May 2013) – Provisional. 4. Patients readmitted to a hospital within 28 days of being discharged. The Trust is reported as having higher than average rates of readmission to hospital within 28 days of being discharged, as shown in the table below. North Tees and Hartlepool NHS Foundation Trust – Medium Acute Trust Age Group Indirectly age, sex, method of admission, diagnosis, procedure standardised percent National Average Percent improvement from 2009-10 to 2010-11 5 Band Comparison against national average 0 to 14 11.45 15 or over 11.48 10.15 6.38 A1 11.42 -2.23 W *Data for 2010-11 standardised to persons 2006-07 (December 2012) NB: Data from the Health and Social Care information Centre (HSCIC). 68 Annual Quality Account 2012-2013 Highest Indirectly age, sex, method of admission, diagnosis, procedure standardised percent scores Trusts Nationally Age Group Indirectly age, sex, method of admission, diagnosis, procedure standardised percent 5 Band Comparison against national average 0 to 14 22.93 A1 15 or over 25.80 A1 Lowest Indirectly age, sex, method of admission, diagnosis, procedure standardised percent scores Trusts Nationally Age Group Indirectly age, sex, method of admission, diagnosis, procedure standardised percent 5 Band Comparison against national average 0 to 14 0.00 B1 15 or over 0.00 B1 5 Band Comparison against national average Note 1: National Comparison, based on 95% and 99.8% confidence intervals of the rate B1 = Significantly better than the national average at the 99.8% level; B5 = Significantly better than the national average at the 95% level but not at the 99.8% level; W = National average lies within expected variation (95% confidence interval); A5 = Significantly poorer than the national average at the 95% level but not at the 99.8% level; A1 = Significantly poorer than the national average at the 99.8% level. Regular audits are undertaken to identify pathways for redesign and other initiatives are being developed, tested and implemented, resulting in a better patient experience whilst maintaining a safe, quality and efficient service. The latest data available has been extracted from Dr Foster (February 2012 – October 2012) which shows the following: Readmisions (28 days) Age Group Actual Expected Difference between actual and expected readmisions 0 to 14 421 428.30 -7.30 15 or over 4528 4415.10 112.90 This demonstrates that the age group of 0-14 has fewer than expected readmissions whilst the age group of 15 or over exceeds its expected readmissions. The North Tees and Hartlepool Foundation Trust has taken the following actions to improve this percentage, and so the quality of its services, by preventing avoidable readmissions within 30 days of discharge has presented a considerable challenge for the Trust and is being addressed by the investment of a significant amount of work and effort. With the required focused clinical leadership and strategic approach there has been a marked improvement to the elective and emergency readmission position. A readmission strategy has been produced, patient pathways have been redesigned and new initiatives implemented including: community integrated assessment teams and teams around practices to ensure that patients receive timely care, at home, by the most appropriate healthcare professional; the introduction of a dedicated cholecystectomy list to provide timely access to surgery for patients who may have had recurrent admissions to hospital with acute cholecystitis whilst awaiting a date for surgery; the implementation of a single telephone access point to direct patients, carers and healthcare professional to the most appropriate service to meet the needs of the patient; and the utilisation of ambulatory care so that patients can be assessed, seen and treated by senior clinicians and return home without the need for admission to hospital. Annual Quality Account 2012-2013 69 5. Responsiveness to the personal needs of its patients, 2003/04 - 2011/12 (Financial year) The Trust has worked hard in order to further enhance its culture of responsiveness to the personal needs of patients. The North Tees and Hartlepool NHS Foundation Trust considers that this data is as described for the following reasons. The Trust has developed its Patients First strategy and understanding patient views in relation to responsiveness, personal needs helps us to understand how well we are performing. The North Tees and Hartlepool NHS Foundation Trust has taken the following actions to improve this score, and so the quality of its services, by delivering accredited programmes that focus on responsiveness of patient and carers for both registered and unregistered nurses. We use human factors training to raise awareness of the impact of individual acts and omissions on patient outcomes and experience. When compared against the national average score the Trust continues to be rated well by patients. Period of Coverage National Average North Tees and Hartlepool NHS Foundation Trust Highest National Trust Average Weighted Score Lowest National Trust Average Weighted Score (out of 100) (out of 100) (out of 100) 2012-13 No Data No Data No Data No Data 2011-12 67.40 71.00 85.00 56.50 2010-11 67.30 70.10 82.60 56.70 2009-10 66.70 65.70 81.90 58.30 2008-09 67.10 68.50 83.40 56.90 2007-08 66.00 66.30 83.10 54.60 2006-07 67.00 72.40 84.00 55.10 2005-06 68.20 72.80 82.60 55.80 2003-04 67.40 73.00 83.30 56.00 NB: Data from the Health and Social Care Information Centre (HSCIC). In 2011-12 the National Average score for England in response to this question was 67.40%. NB: Average weighted score of 5 questions relating to responsiveness to inpatients’ personal needs (Score out of 100). 6. Recommend the Trust as a provider of care to their family or friends The North Tees and Hartlepool NHS Foundation Trust considers that this data is as described for the following reasons. The Family or Friends (F&F) test identifies the percentages of patients who would recommend the Trust as a provider of care to their family or friends. The North Tees and Hartlepool Foundation Trust has taken the following actions to further improve this percentage, and so the quality of its services, by involving patients relatives and staff in developing a strategy for care. Wards and the A&E department are monitored in relation to the F&F test. The Trust believes that the attitude of its staff is the most important factor in the experience of patients. We will continue to work with staff to develop the leadership and role modeling required to further enhance the experience of patients, carers and staff. As part of our commitment to improve the service we provide, the Education & OD department are currently working with patient facing staff to improve customer care. The process starts with reminding staff of the Trust's vision along with the values and behaviors required to achieve it. A customer care charter is then developed by the staff to remind and encourage then to provide the highest care possible. 70 Annual Quality Account 2012-2013 National NHS Staff Survey 2012 Question: If a friend or relative needed treatment, would I be happy with the standard of care provided by this Trust? North Tees and Hartlepool NHS Foundation Trust Score National National NHS Staff Survey 2012 Highest Trust Score Lowest Trust Score 60.619 94.199 35.337 NB: Data from the Health and Social Care Information Centre (HSCIC). This data demonstrates that the Trust results are in line with the national average. The Trust is working to improve this score for the future. 7. Risk assessed for Venous Thromboembolism The North Tees and Hartlepool Foundation Trust considers that this data is as described for the following reasons. Understanding percentage of patients who were admitted to hospital who were risk assessed for VTE helps the Trust to understand and reduce cases of avoidable harm. The North Tees and Hartlepool Foundation Trust has taken the following actions to continue to improve this percentage, and so the quality of its services, by including training on the importance of VTE risks assessment at induction of clinical staff. Consultants monitor performance in relation to VTE risk assessment on a daily basis. The Trust has promoted the importance of doctors undertaking assessment of risk of VTE for all appropriate patients in line with best practice. North Tees and Hartlepool NHS Foundation Trust Quarter Number of VTEassessed Admissions Total Admissions Percentage of admitted patients risk-assessed for VTE National Average Q1 16,957 18,231 93.00% 93.40% Q2 16,813 18,234 92.20% 93.80% Q3 17,316 18,482 93.70% 94.10% Q4 No Data Available No Data Available No Data Available No Data Available NB: Data from the Health and Social Care Information Centre (HSCIC). Highest and Lowest percentage of admitted patients risk-assessed for VTE nationally Quarter Highest percentage of admitted patients risk-assessed for VTE Lowest percentage of admitted patients risk-assessed for VTE Q1 100% 80.80% Q2 100% 80.90% Q3 100% 84.60% Q4 No Data Available No Data Available NB: Quarter 4 data not available at time of print. 71 Annual Quality Account 2012-2013 8. Rate per 100,000 bed days of cases of C diff infection reported within the Trust amongst patients aged 2 or over. Understanding the Trust's benchmark position in relation to C diff is important and informs actions that can be taken to understand and reduce the burden of this infection. The North Tees and Hartlepool Foundation Trust considers that this data is as described for the following reasons. Understanding the Trusts benchmark position in relation to C difficile is important and informs actions that can be taken to understand and reduce the burden of this infection. The North Tees and Hartlepool Foundation Trust has taken the following actions to improve this rate, and so the quality of its services, by undertaking a comprehensive review of all data in relation to C difficile, including not only the number of cases reported, but also the number of samples sent for analysis. This provides evidence that the Trust is proactive in its testing regime when compared to many organisations. When compared to Trusts nationally the organisation is reported as an outlier: April 2011 - March 2012 Rate per 100,000 bed-days for specimens taken from patients aged 2 years and over North Tees and Hartlepool NHS Foundation Trust 35.20 Highest National rate 51.60 Lowest National rate 0.00 National Average rate 21.80 NB: Data from the Health and Social Care Information Centre (HSCIC). For more detail on C difficile see priority 1 patient safety section. The latest position available to the Trust relating to the Rate per 100,000 bed days of cases of C difficile infection reported within the trust amongst patients aged 2 or over is as follows: April 2012 - March 2013 Rate per 100,000 bed-days for specimens taken from patients aged 2 years and over North Tees and Hartlepool NHS Foundation Trust 29.98 *Data not validated at time of print. 9. Patient safety incidents reported within the Trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death. This indicator is expressed as a percentage of Patient Safety Incidents (PSI) reported to the National Reporting and Learning Service (NRLS) that have resulted in severe harm or death. The ‘degree of harm’ for PSIs is defined as follows: •Severe – the patient has been permanently harmed as a result of the PSI; •Death – the PSI has resulted in the death of the patient. Reporting and understanding patient safety incidents is an important indicator of a safety culture within an organisation. 72 The North Tees and Hartlepool Foundation Trust considers that this data is as described for the following reasons. Understanding numbers and rate of incidents reported alongside the percentage of deaths reported enables the organisation to understand whether actions taken are effective. Annual Quality Account 2012-2013 Medium Acute organisations - Organisational incident data by organisation in 6-month period, April 2012 – September 2012. Organisation Name Total Number of Incidents Rate per 100 admissions Severe Harm Incidents Percentage (%) Death Percentage (%) North Tees and Hartlepool NHS Foundation Trust 2,615 6.27 17 0.70 1 0.00 Average across all Medium Acute organisations 2,603 6.87 14.91 0.62 4.53 0.20 Highest and Lowest Trusts rate per 100 admissions Trusts Total Number of Incidents Rate per 100 admissions Severe Harm Incidents Percentage (%) Death Trust A - Highest 4,552 14.44 Trust B - Lowest 1,047 3.11 Percentage (%) 61 1.30 15 0.30 5 0.50 2 0.20 NB: Data from the Health and Social Care Information Centre (HSCIC). The North Tees and Hartlepool Foundation Trust has taken the following actions to improve this reporting rate and so the quality of its services, by weekly monitoring if incidents and actions taken to reduce risk of recurrence. The Trust also undertakes regular mortality reviews and these are described within the Quality Account. The Trust remains proactive in its review of incident reporting and its monitoring of impact of actions taken. This proactive approach to patient safety has supported a reduction in deterioration and serious harm, as is evidenced in part 2. The latest data available to the Trust for the reporting year (1 April 2012 – 31 March 2013) relating to the patient safety incidents that are reported to the National Reporting and Learning Service (NRLS) are as follows: The following incidents total does not include No injury, whilst the tables above reported by the HSCIC does include No injury. Trusts Number of incidents % of incidents Low Minor Moderate Severe Harm Death Total number of incidents 540 707 989 49 1 2,286 23.62 30.93 43.26 2.14 0.04 73 Annual Quality Account 2012-2013 Annex 1 Third Party Declarations from the Annual Quality Account We have invited comments from our key stakeholders. Third party declarations from key groups are outlined below: Council of Governors (third party declaration – 4 March 2013) This statement aims to provide evidence that the Governors of North Tees and Hartlepool NHS Foundation Trust (the Trust) have been involved in the formation of the Trust’s Annual Quality Account 2013-14. Governors were fully appraised regarding the Quality Account at Council of Governors meetings throughout the year, and were provided with a wide range of data and evidence covering all aspects of the Account’s content that was included in regular update and performance reports presented by Directors. Governors are also kept updated regarding service developments, and future visions, and have been able to contribute to discussions regarding the refresh of the Trust’s Corporate Strategy via the Strategy Subcommittee, and development sessions at the Council of Governors meetings. In addition, a working group of Governors assisted by the Assistant Director of Nursing, Quality and Patient and Public Involvement was established, to discuss priority areas to be included in the Quality Account, and to review the draft Account in detail on behalf of the Council of Governors, seeking assurances/providing challenge regarding certain elements that required clarification. The feedback obtained from these sessions helped shape the key priorities within the Quality Account for 2013-14, and the final content. At the Council of Governors development sessions during 2012-13 workshops took place to provide Governors and the Board of Directors with an in depth insight and scrutiny of priority areas from the Quality Account, including Dementia Care, and clostridium difficile. The sessions allowed Governors to provide valuable feedback and suggestions regarding work being undertaken in these areas, and also ensure that they are fully aware of both the challenges being faced by the Trust, and the valuable improvements being made to patient care. The Trust has recently experienced unprecedented levels of activity which has resulted in increasing the North East Escalation Policy (NEEP) to level 3 and on one occasion to level 4. This is the agreed protocol between trusts to manage resilience. It means that the Trust is experiencing service pressures and requires support from staff in all areas, both clinical and non-clinical. The response by staff has been brilliant. The Board thanked staff for their hard work and ensured that provisions were made for staff that were unable to leave clinical areas for a break, and during the spell of bad weather, arrangements were made for staff that were unable to travel home. Patient Safety and Quality continue to be areas of focus for the Trust, and a Quality Report is provided at every Council of Governors and Board of Directors meetings by the Director of Nursing, Patient Safety and Quality. During 2012-13 the programme of Patient Experience Quality Standards continued both at each hospital site and community locations allowing Governors and members of the Board, accompanied by clinicians and senior nursing staff, to witness first hand the level of care and service being provided to our patients. It provides the opportunity to speak with patients and their visitors directly about the experience they have had during their stay at the Trust. The panels seek to establish the privacy and dignity afforded to patients, the level of care given and the standards of the environment around them. The scoring system used during the visits is constantly being updated to reflect new measuring indicators and criteria to ensure they remain as meaningful as possible. Reports from the panels are shared with the Council of Governors to provide assurance. 74 Annual Quality Account 2012-2013 Governors have also been assisting with the recruitment of new members for the Trust, by visiting a wide range of clinical areas and speaking to our patients about their experiences of the Trust and feeding back the comments/suggestions received. Some of the Governors are involved in a number of other groups: the Menu Review Group, Patient Information Evaluation Group and the Hospital User Group which focus on specific service areas. The range of reports that are presented to the Council of Governors highlight the performance and compliance of the Trust against its many performance indicators and particular areas of focus, which this year have included work around hospital acquired infections and clostridium difficile. The meetings are conducted in an open, supportive environment where the opinions and challenges by the Governors are valued and encouraged. As part of the briefings received regarding new service developments, Governors receive updates regarding the momentum: pathways to healthcare programme which aims to transform services and provide care as close to home as possible for our patients. At a development session in January 2013 the new health and social care priorities were discussed, following the publication of the Health and Social Care Act 2012, which aims to provide a seamless pathway of care for patients across health, social care and public health. The interactive session ensured Governors fully understood what the new healthcare landscape would look like, the stakeholders involved, new bodies being established, but more importantly what it would mean for our patients. The Service Development and Quality Committee, a sub-committee of the Council of Governors which met on 7 June 2012, 11 October 2012 and 28 February 2013 was specifically informed regarding initiatives for patients with learning disabilities and dementia, the outcomes of a cancer peer review, operational efficiencies and readmissions. It also provided compliance and service performance data in relation to individual performance indicators, and resilience and emergency preparedness plans. 75 Annual Quality Account 2012-2013 Feedback from NHS County Durham and Darlington Commissioners – 27 February 2013 Many thanks for sending through your Draft Quality Account 2013-14. As a Commissioner of services for the population of Durham we welcome the opportunity to make the comments on your Quality Account, the improvements against 2012-13 priorities and the priorities identified for 2013-14. This plan will support improvements in the quality and safety of care provided to the population of Durham. Durham Dales, Easington and Sedgefield CCG acknowledges the improvements seen in areas of quality identified as priorities for 2012-13. In particular the improvements and achievements of all key performance for patient safety and quality. Regarding the work undertaken to reduce the number of patients that die in your care, we see that this work has impacted positively and although this is not highlighted as a priority for the coming year, will be mainstream to continue the reduction. The ground breaking work in relation to Early Warning Signs (EWS) in the community setting can only be commended and we look forward to seeing further evaluation of this work as it is rolled out and embedded in practice. We acknowledge the sterling work the organisation does in relation to end of life care and being held up as beacon of expertise by colleagues and the satisfaction of patients and carers is testament to this work. The challenges with clostridium difficile cannot go unremarked, we recognise the work being undertaken against reducing the number of cases and as a Commissioner will continue to support your organisation as well as the wider health community. We support all the priorities identified for 2013-14 and look forward to seeing the improvement in the care of patients with Dementia. This programme of work will be supported by the nationally mandated Commission for Quality and Innovation (CQUIN) for Dementia included in this year’s scheme. We support the continued work on reducing the number of avoidable clostridium difficile cases; improvements in discharge processes to support the quality of patient experience and improve safety as well as communication to primary care. Overall we feel you have set out a series of ambitious goals and look forward to working with you. As Commissioners we feel the Quality Account would benefit from further elaboration and more detailed reporting on areas for improvement and development as well as highlighting successes. We will work with you to ensure the recommendations from the Francis report are implemented and we will ask you to report your progress to us as Commissioners mid-year to ensure all actions are being implemented. Yours sincerely Debbie Edwards Nurse Advisor/Clinical Quality Lead 76 Annual Quality Account 2012-2013 Hartlepool LINk response to Annual Quality Account of North Tees and Hartlepool NHS Foundation Trust – 5 February 2013 Following receipt of the draft quality account, Hartlepool LINk wish to make a formal response to the approach taken by the Trust with regards to quality. This response encompasses the views of Hartlepool LINk members, which have been relayed to both the Trust via direct correspondence and also encompassed within our published ‘Enter and View’ statutory reports. Please note this opinion is based on factual ‘Enter and View’ visits undertaken, referrals received into Hartlepool LINk and actual patient experience of LINk members. Our view of future priorities would be of agreement in particular the detail surrounding Patient Safety, Effectiveness of Care and Patient Experience. We firmly believe that key recommendations borne out of our collaborative working with the Trust, fit within the priorities and focus of the quality account. We have carried out a number of visits to Hartlepool and North Tees Hospital Wards and Departments and we have been impressed by what was observed and what we have been told. All visits have been underpinned by what we believe to be openness and honesty with information freely given, which in turn has allowed Hartlepool LINk to produce meaningful and robust reports. At the moment we would welcome the focus on Dementia as this has been a meaningful piece of work by Hartlepool LINk over the last year and our recommendation for dementia training across the Trust staff was welcomed and adopted positively. Whilst it is such an emotive subject regard must also be given to ‘End of Life’ care as it is collectively felt within Hartlepool LINk that the Trust should be applauded for their progress and work in this area. One area Hartlepool LINk is keen for the Trust to reconsider is the issue of Transport. Year on year, as a move towards improving meaningful communication we have formerly requested the Trust adhere to their obligation in notifying patients of the NHS Healthcare Travel Costs Scheme. In this current economic climate we feel some patients are choosing to disengage from treatment purely because they do not have the funds to attend appointments. Hartlepool Link does welcome the collaborative work with the Local Authority in respect of transport. Overall, Hartlepool LINk welcomes the opportunity to respond to the Draft Quality Account and would hope it will continue to reflect the views we present as the sole statutory consultation body for the people of Hartlepool in what will be our transition year as HealthWatch Hartlepool. Yours Faithfully, Christopher Akers-Belcher – LINks Co-ordinator E-mail: c.akersbelcher@hvda.co.uk Website: www.hartlepoollink.co.uk 77 Annual Quality Account 2012-2013 Health Scrutiny Forum, Hartlepool – 1 March 2013 Hartlepool Health Scrutiny Forum welcomes the opportunity to contribute to North Tees and Hartlepool NHS Foundation Trust’s Quality Account for 2013-14. The Forum would like to thank all members of staff who contribute to improving the experience and outcomes for patients accessing services provided by North Tees and Hartlepool NHS Foundation Trust. In relation to communication between the Trust and the Forum, Members feel that communication and timescales have improved significantly this year, which has contributed to an improved Quality Account for 2013-14. Members welcome and support improvements to end of life pathways and are pleased that end of life care has been identified as a key priority for 2013-14. Members congratulate the Trust on the development of the new Oasis Suite and would like the suite to be continued, as it is a facility that will make such a difference to families in difficult times. Even though medication errors remain small when compared to the number of medicines dispensed by the Trust, the Forum emphasises the importance of medicine safety. Members welcome the actions taken by the Trust to reduce medication errors and are supportive of the positive reporting culture that encourages all staff to report actual medication errors as well as opportunities for error. To help minimise medication errors which are as a result of illegible handwriting, Members suggest that a handheld computerised device may be an alternative to a written prescription to ensure that no errors in medication are made because of illegible handwriting. The Forum emphasise the importance of providing nutritional meals to patients and encourage the Trust to continue to provide patients with a meal of their choice and at a time that best suits the patient. The Forum believes that in order to further improve the experiences of patients and visitors, access to Hartlepool and North Tees Hospitals is an area for consideration and improvement by the Trust. Members are of the view that experiences of patients and visitors who travel to the Hospitals are vital and need to be considered to help improve access and patient experience. Councillor Stephen Akers-Belcher Chair of Hartlepool’s Health Scrutiny Forum 78 Annual Quality Account 2012-2013 Third Party Statement from Healthcare User Group (HUG) The main role of the Healthcare User Group (HUG) is to assist the Trust with the Patient and Public Involvement (PPI) agenda. This is achieved through independent visits to inpatient wards and outpatient clinics, talking to staff and patients. HUG is also represented on other Trust committees such as the Quality Standards Steering Group, Patient Environment Action Team, Audit and Clinical Effectiveness Committee and High Impact Action Groups. HUG supports the priorities selected for 2013-14 and has had every opportunity to contribute to the development of these priorities. In relation to the priorities for 2012-13, our visits have shown the desire of staff to push for improvements in service quality and outcomes for patients. In particular, staff are very active in achieving the Dementia strategy and Making the Patient Count with emphasis on dignity, communication and nutrition. They are very aware of research aiming to meet the needs of dementia patients, especially through the use of visual aids and bright colours. We have also observed the desire for improving patient experiences, in particular the further development of the Carers Diary, contributing to better care and experience for patients and families. With regard to infection control, it is disappointing that the target for Clostridium Difficle has been exceeded. We recognise the efforts the Trust has made to prevent and control the spread of infection and this has been observed on our visits. The Trust has presented the correct level of support to allow HUG to perform its independent visits to various wards and clinics. Any concerns or recommendations have been acknowledged and implemented promptly. We view the Quality Accounts as a true and fair reflection of what we have seen on our visits to North Tees and Hartlepool wards and departments. HUG will continue to be an impartial and encouraging party, assisting in developing and monitoring patient services within the Trust. 79 Annual Quality Account 2012-2013 NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group 2 May 2013 NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group (HAST CCG) commission healthcare services for the population of Hartlepool and Stockton-on-Tees and welcome the opportunity to submit a statement on the Annual Quality Account for North Tees and Hartlepool NHS Foundation Trust. NHS Hartlepool and Stockton-on-Tees Clinical Commissioning Group (HAST CCG) can confirm that to the best of its ability, the information provided within the Annual Quality Account is an accurate and fair reflection of the Trust’s performance for 2012-13. During 2012-13 we have continued to provide joint robust challenge through our Clinical Quality Review Groups (CQRGs) to drive improvements in the quality of services and outcomes for patients. The CQRGs involve key stakeholders who focus on a significant range of topics including all aspects of safety, clinical effectiveness and patient experience. North Tees and Hartlepool NHS Foundation Trust have been open and transparent in their approach to working with commissioners and have responded positively to constructive clinical challenge. The key areas of particular challenge have included the reduction of clostridium difficile, MRSA and pressure ulcers, and monitoring of mortality which the Trust has actively engaged with the Commissioner to improve. During 2012-13, clinical members of NHS Hartlepool and Stockton-on-Tees CCG have participated in quality assurance visits, and have continued to attend a number of key working groups and committees in relation to the patient safety agenda. As part of their continued desire to be transparent providers, to improve care and reduce harm, North Tees and Hartlepool NHS Foundation Trust have actively involved the commissioners in the sharing of lessons learned following serious incidents. The Trust have also been proactive in promoting and sharing lessons learned with the wider health economy. The Trust has worked with CCG representatives in agreeing, implementing and delivering a challenging Commissioning for Quality and Innovation (CQUIN) scheme in 2012-13. This approach will be maintained in 2013-14 ensuring active clinical engagement. The CCG have worked with key staff groups during 2012-13 to ensure a seamless transition in the handover of its commissioner responsibilities working with North Tees and Hartlepool NHS Foundation Trust in ensuring that the commissioning, provision and monitoring of safe clinical care for the people of Teesside remains a key priority. The CCG recognises the hard work and dedication of staff across acute and community settings and the overall commitment of the Trust to 'Put Patients First' by making patient safety and experience their number one priority. NHS Hartlepool and Stockton-on-Tees CCG look forward to continuing to work in partnership with North Tees and Hartlepool NHS Foundation Trust during 2013-14 to implement the Francis report and Winterbourne View recommendations and ensure the quality of services that the Trust provides for the people of Teesside continues to improve. Chief Officer Hartlepool and Stockton-on-Tees Clinical Commissioning Group 80 Annual Quality Account 2012-2013 Feedback from the Stockton Council’s Adult Service and Health Select Committee and Stockton LINk Members of both the Select Committee and LINk welcome the opportunity to comment on this year’s Quality Account, and provide a joint statement for inclusion in the published version. Both the LINk and Committee support the priorities that have been selected for 2012-13. There have been great improvements in infection control over the previous few years, and there remains a focus on tackling clostridium difficile (C diff). It is recognised that the target set for the Trust which it must avoid breaching is a testing one, however, irrespective of targets, the total number of cases remains higher than for some other Trusts in the region. It is noted that there are variations in the numbers of C diff toxin tests undertaken on samples by different Trusts in the region; a standard approach to the proportion of sample testing to assist with making comparisons should be considered. Efforts to tackle the issue locally, particularly the investigation of each occurrence and to continually review best practice from elsewhere, are welcomed. Given the number of community-acquired infections, there is also a clear role for community services and partners to play, in order to spread awareness of the need to reduce C diff infections in the community. Discharge should provide a seamless process including the GP, and community services and care homes were relevant, with communication being key. It is pleasing to note the focus given to ensuring that discharged patients are returned home ‘Safe and Warm’. This is in line with the high priority given to the Affordable Warmth agenda by Stockton Council. Continued focus on dementia is necessary and in line with national and other local priorities (including the CCG). In order to fully prepare for the increasing numbers of people with the condition in future years there needs to be an integrated approach across health and social care settings. In the absence of national guidance, it is pleasing to see that the Trust is developing and plan to pilot a dementia screening trigger tool for the community. The introduction of the Nursing Dashboard is welcome and it is pleasing to note the positive reception from staff. Public display of key ward-based nursing indicators (such as falls, pressure sores, compliments, and staff sickness rates) improves transparency, highlights potential issues, and enables comparisons between wards. There has been generally very good performance in achieving the quality priorities for 2012-13. Communication will always be a major priority. From surveys undertaken by non-exec Board members and Governors, there are high levels of patient feedback in relation to being treated with dignity and respect. However it was noticeable that 82.6% of patients responding to the National Inpatient Survey felt that they were given enough privacy; this does mean that 20% felt that they were not. A key concern of the LINk has always been privacy and dignity in health and social care settings, and any effort to improve this score would be welcomed. Intentional Rounding has been introduced across the Trust and the aim is to provide daily feedback to staff. The Trust is not yet able to demonstrate that the feedback occurs in all areas and this should be addressed to ensure that any issues are picked up in a timely manner. 81 Annual Quality Account 2012-2013 End of life care, and particularly communication with patients and carers, continues to be a high priority for the Committee and LINk, and we have supported the development of the Family Voice (carer diary) and are pleased to see that it has been identified as good practice nationally. Support for vulnerable patients has also been a key issue for the Committee and LINk, and so we particularly support the work to provide people with a learning disability with some prior experience of what to expect if admitted to hospital by using an open day event. The proposed accessible version of the Quality Account for people with a learning disability is also welcome. It is understood that Patient Environment Action Team (PEAT) assessments will be replaced by Patient led Assessments in the Care Environment (PLACE) from April 2013 on a national basis. PEAT assessments examine cleanliness, facilities, dignity and privacy, and nutrition. PLACE assessments will formalise the role of patients, family, carers and advocates in the process, together with continued involvement of Trust personnel. This could be an area to include in future Quality Accounts. Following the Francis Report into the Mid-Staffordshire hospital scandal, the Trust was the first to be inspected by the CQC following the publication of the report. It is pleasing to note that no recommendations for improvement were identified during the inspection. No healthcare provider can be complacent and therefore it is good to see that the Trust will be undertaking a gap-analysis of the report’s recommendations and identify any areas for further improvement. Due to the transition to HealthWatch this will be the last joint statement produced by the Committee in conjunction with the LINk. Members and the LINk have welcomed the opportunity to work together with the Trust to discuss the Quality Account over the last few years, and look forward to continued involvement. 82 Annual Quality Account 2012-2013 Annex 2 Statement of directors’ Responsibilities in Respect of the Quality Account The Directors are required under the Health Act 2009 to prepare a Quality Account for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the legal requirements in the Health Act 2009 and the National Health Service (Quality Reports) Regulations 2010 (as amended by the National Health Service (Quality Accounts) Amendments Regulations 2011). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: •The Quality Account presents a balanced picture of the trust’s performance over the period covered; •The performance information reported in the Quality Account is reliable and accurate; •There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; •The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and •The Quality Account has been prepared in accordance with Department of Health guidance. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board Paul Garvin Chairman 24 May 2013 Alan Foster MBE Chief Executive 24 May 2013 83 Annual Quality Account 2012-2013 Annex 3 Independent Auditors' Limited Assurance Report to the Council of Governors of North Tees and Hartlepool NHS Foundation Trust on the Annual Quality Report. We have been engaged by the Council of Governors of North Tees and Hartlepool NHS Foundation Trust to perform an independent assurance engagement in respect of North Tees and Hartlepool NHS Foundation Trust’s Quality Report for the year ended 31 March 2013 (the ‘Quality Report’) and specified performance indicators contained therein. Scope and subject matter The indicators for the year ended 31 March 2013 in the Quality Report that have been subject to limited assurance consist of the following national priority indicators as mandated by Monitor: •Number of Clostridium difficile infections; and •Maximum cancer waiting time of 62 days from urgent GP referral to first treatment for all cancers. We refer to these national priority indicators collectively as the “specified indicators”. Respective responsibilities of the directors and auditors The directors are responsible for the content and the preparation of the Quality Report in accordance with the assessment criteria referred to in the Quality Report (the "Criteria"). The directors are also responsible for the conformity of their Criteria with the assessment criteria set out in the NHS Foundation Trust Annual Reporting Manual (“FT ARM”) issued by the Independent Regulator of NHS Foundation Trusts (“Monitor”). Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: •The Quality Report does not incorporate the matters required to be reported on as specified in Annex 2 to Chapter 7 of the FT ARM; •The Quality Report is not consistent in all material respects with the sources specified below; and •The specified indicators have not been prepared in all material respects in accordance with the Criteria. We read the Quality Report and consider whether it addresses the content requirements of the FT ARM, and consider the implications for our report if we become aware of any material omissions. 84 Annual Quality Account 2012-2013 We read the other information contained in the Quality Report and consider whether it is materially inconsistent with the following documents: •Board minutes for the period April 2012 to the date of signing this limited assurance report (the period); •Papers relating to Quality reported to the Board over the period April 2012 to the date of signing this limited assurance report; •Feedback from the Commissioners NHS Hartlepool & Stockton-on-Tees Clinical Commissioning Group dated 2 May 2013; •Feedback from Governors dated 4 March 2013; •Feedback from Stockton Council’s Adult Service and Health Select Committee and Stockton LINk; •Feedback from Hartlepool LINk dated 5 February 2013; •The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009; •The 2012 national patient survey; •The 2012 national staff survey; •Care Quality Commission quality and risk profiles dated 31 March 2013; and •The Head of Internal Audit’s annual opinion over the Trust’s control environment dated 14 May 2013. We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with those documents (collectively, the “documents”). Our responsibilities do not extend to any other information. We are in compliance with the applicable independence and competency requirements of the Institute of Chartered Accountants in England and Wales (ICAEW) Code of Ethics. Our team comprised assurance practitioners and relevant subject matter experts. This report, including the conclusion, has been prepared solely for the Council of Governors of North Tees and Hartlepool NHS Foundation Trust as a body, to assist the Council of Governors in reporting North Tees and Hartlepool NHS Foundation Trust’s quality agenda, performance and activities. We permit the disclosure of this report within the Annual Report for the year ended 31 March 2013, to enable the Council of Governors to demonstrate they have discharged their governance responsibilities by commissioning an independent assurance report in connection with the indicators. To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Council of Governors as a body and North Tees and Hartlepool NHS Foundation Trust for our work or this report save where terms are expressly agreed and with our prior consent in writing. Assurance work performed We conducted this limited assurance engagement in accordance with International Standard on Assurance Engagements 3000 ‘Assurance Engagements other than Audits or Reviews of Historical Financial Information’ issued by the International Auditing and Assurance Standards Board (‘ISAE 3000’). Our limited assurance procedures included: •Evaluating the design and implementation of the key processes and controls for managing and reporting the indicators; •Making enquiries of management; •Limited testing, on a selective basis, of the data used to calculate the specified indicators back to supporting documentation; •Comparing the content requirements of the FT ARM to the categories reported in the Quality Report; and 85 •reading the documents. Annual Quality Account 2012-2013 A limited assurance engagement is less in scope than a reasonable assurance engagement. The nature, timing and extent of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Limitations Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw allows for the selection of different but acceptable measurement techniques which can result in materially different measurements and can impact comparability. The precision of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precision thereof, may change over time. It is important to read the Quality Report in the context of the assessment criteria set out in the FT ARM and the directors’ interpretation of the Criteria in the Quality Report. The nature, form and content required of Quality Reports are determined by Monitor. This may result in the omission of information relevant to other users, for example for the purpose of comparing the results of different NHS Foundation Trusts. In addition, the scope of our assurance work has not included governance over quality or non-mandated indicators in the Quality Report, which have been determined locally by North Tees and Hartlepool NHS Foundation Trust. Conclusion Based on the results of our procedures, nothing has come to our attention that causes us to believe that for the year ended 31 March 2013; •The Quality Report does not incorporate the matters required to be reported on as specified in annex 2 to Chapter 7 of the FT ARM; •The Quality Report is not consistent in all material respects with the documents specified above; and •The specified indicators have not been prepared in all material respects in accordance with the Criteria. PricewaterhouseCoopers LLP Chartered Accountants Newcastle upon Tyne 24 May 2013 The maintenance and integrity of North Tees and Hartlepool NHS Foundation Trust’s website is the responsibility of the directors; the work carried out by the assurance providers does not involve consideration of these matters and, accordingly, the assurance providers accept no responsibility for any changes that may have occurred to the reported performance indicators or criteria since they were initially presented on the website. 86 Annual Quality Account 2012-2013 Glossary A&E Accident and Emergency ACE Committee Audit and Clinical Effectiveness Committee - the committee that oversees both clinical audit (i.e. monitoring compliance with agreed standards of care) and clinical effectiveness (i.e. ensuring clinical services implement the most up-to-date clinical guidelines). ACL Anterior Cruciate Ligament - one of the four major ligaments of the knee AMT Abbreviated Mental Test CABG Coronary Artery Bypass Graft (or “heart bypass”) CCG Clinical Commissioning Group CHKS Comparative Health Knowledge System Clostridium difficile (infection) An infection sometimes caused as a result of taking certain antibiotics for other health conditions. It is easily spread and can be acquired in the community and in hospital. CLRN Comprehensive Local Research Network COPD Chronic Obstructive Pulmonary Disease CSP Co-ordinated System for gaining NHS Permission CQC The Care Quality Commission - the independent safety and quality regulator of all health and social care services in England. CQRG Clinical Quality Review Group CQUIN Commissioning for Quality and Innovation - a payment framework introduced in 2009 to make a proportion of providers’ income conditional on demonstrating improvements in quality and innovation in specified areas of care. DAHNO Data for Head and Neck Oncology (Head and Neck Cancer) DoLS Deprivation of Liberty Safeguards Dr Foster A major provider of healthcare information and benchmarking DVLA Driver and Vehicle Licensing Agency EAU Emergency Assessment Unit e-coli (infection) An infection sometimes caused as a result of poor hygiene or hand-washing EWS Early Warning Score - a tool used to assess a patient’s health and warn of any deterioration FCE Finished Consultant Episode - the complete period of time a patient has spent under the continuous care of one consultant FOI (act) The Freedom of Information Act - gives you the right to ask any public body for information they have on a particular subject Global trigger tool (GTT) Used to assess rate and level of potential harm. Use of the GTT is led by a medical consultant and involves members of the multiprofessional team. The tool enables clinical teams to identify events through triggers which may have caused, or have potential to cause varying levels of harm and take action to reduce the risk. GCP Good Clinical Practice GM General Manager HCAI Health Care Acquired Infection HES Hospital Episode Statistics HMB Heavy Menstrual Bleeding HQIP Healthcare Quality Improvement Partnership HRG Healthcare Resource Group - a group of clinically similar treatments and care that require similar levels of healthcare resource. HSMR Hospital Standardised Mortality Ratio - an indicator of healthcare quality that measures whether the death rate in a hospital is higher or lower than you would expect. HUG Healthcare User Group IBD Inflammatory Bowel Disease ICNARC Intensive Care National Audit and Research Centre LD Learning Difficulties IG Information Governance Intentional Rounding A formal review of patient satisfaction used in wards at regular points throughout the day IPNMB Integrated Professional Nursing Midwifery Board IPC Infection Prevention and Control Kardex (prescribing kardex) A standard document used by healthcare professionals for recording details of what has been prescribed for a patient during their stay. LD Learning disabilities 87 Annual Quality Account 2012-2013 88 LINks Local Involvement Network - a group established in order to give local people a stronger voice in how their health and social care services are run. Liverpool End of Life Care Pathway Used at the bedside to drive up sustained quality of care of the dying patient in the last hours and days of life. MBRRACE-UK Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries in the UK MCA Mental Capacity Act MHA Mental Health Act MHRA Medicines and Healthcare products Regulatory Agency MINAP The Myocardial Ischaemia National Audit Project Monitor The independent regulator of NHS foundation Trusts MRSA Methicillin-Resistant Staphylococcus Aureus - a type of bacterial infection that is resistant to a number of widely used antibiotics. MUST Malnutrition Universal Screening Tool NCEPOD The National Confidential Enquiry into Patient Outcome and Death NCRN National Cancer Research Network NEPHO North East Public Health Observatory NEQOS North East Quality Observatory System NICE The National Institute of Health and Clinical Excellence NICOR The National Institute for Cardiovascular Outcomes Research NIHR National Institute for Health Research NNAP National Neonatal Audit Programme OFSTED The Office for Standards in Education PALS Patient Advice and Liaison Service PAS Patient Administration System Patient Safety and Quality Standards (Ps&Qs) Committee The committee responsible for ensuring provision of high quality care and identifying areas of risk requiring corrective action. PEQS Patient Experience and Quality Standards PICANet Paediatric Intensive Care Audit Network PROMs Patient Reported Outcome Measures Pseudonymisation A process where patient identifiable information is removed from data held by the Trust Quality Risk Profile (QRP) A CQC tool for monitoring compliance with essential standards of quality and safety that helps to identify where risks lie within an organisation. R&D Research and Development RCA Root Cause Analysis RCOG The Royal College of Obstetricians and Gynaecologists RCPCH The Royal College of Paediatric and Child Health RESPECT “Responsive, Equipped, Safe and secure, Person centred, Evidence based, Care and compassion and Timely” - a nursing and midwifery strategy developed with patients and governors aimed at promoting the importance of involving patients and carers in all aspects of healthcare. RMSO Regional Maternity Survey Office SBAR Situation, Background, Assessment and Recommendation - a tool for promoting consistent and effective communication in relation to patient care. SCM Senior Clinical Matron SHA Strategic Health Authority SHMI Summary Hospital Mortality-level Indicator - a hospital-level indicator which reports inpatient deaths and deaths within 30-days of discharge at Trust level across the NHS. SINAP Stroke Improvement National Audit Programme SSU Short Stay Unit STAMP Screening Tool for the Assessment of Malnutrition in Paediatrics STERLING Environmental Audit Assessment Tool Tough-books Piloted in 2010, these mobile computers aim to ensure that community staff have access to up-to-date clinical information, enabling them to make speedy and appropriate clinical decisions. UHH University Hospital of Hartlepool UHNT University Hospital of North Tees VSGBI The Vascular Society of Great Britain and Ireland VTE Venous Thromboembolism Annual Quality Account 2012-2013 89 Annual Quality Account 2012-2013 North Tees and Hartlepool NHS Foundation Trust Annual Quality Account 2012-2013 www.nth.nhs.uk