M [ research
advertisement

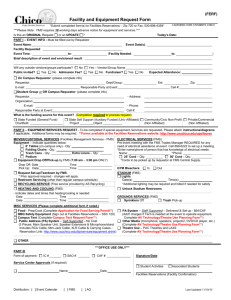
[ ] research report DEYDRE S. TEYHEN, PT, PhD1,2 • SCOTT W. SHAFFER, PT, PhD2 • CHELSEA L. LORENSON, PT3 • JOSHUA P. HALFPAP, PT3 DUSTIN F. DONOFRY, PT3 • MICHAEL J. WALKER, PT, DSc4 • JESSICA L. DUGAN, PT5 • JOHN D. CHILDS, PT, PhD2,6 The Functional Movement Screen: A Reliability Study TTSTUDY DESIGN: Reliability study. TTOBJECTIVES: To determine intrarater test- retest and interrater reliability of the Functional Movement Screen (FMS) among novice raters. TTBACKGROUND: The FMS is used by various examiners to assess movement and predict timeloss injuries in diverse populations (eg, youth to professional athletes, firefighters, military service members) of active participants. Unfortunately, critical analysis of the reliability of the FMS is currently limited to 1 sample of active college-age participants. TTMETHODS: Sixty-four active-duty service members (mean SD age, 25.2 3.8 years; body mass index, 25.1 3.1 kg/m2) without a history of injury were enrolled. Participants completed the 7 component tests of the FMS in a counterbalanced order. Each component test was scored on an ordinal scale (0 to 3 points), resulting in a composite score ranging from 0 to 21 points. Intrarater test-retest reliability was assessed between baseline scores and those obtained with repeated testing performed 48 to 72 hours later. Interrater reliability was based on the assessment from 2 raters, selected from a pool of 8 novice raters, who assessed the same movements on day 2 simultaneously. Descriptive statistics, weighted kappa (κw), and percent agreement were calculated on component scores. Intraclass correlation coefficients (ICCs), standard error of the measurement, minimal detectable change (MDC95), and associated 95% confidence intervals (CIs) were calculated on composite scores. TTRESULTS: The average SD score on the FMS was 15.7 0.2 points, with 15.6% (n = 10) of the participants scoring less than or equal to 14 points, the recommended cutoff for predicting time-loss injuries. The intrarater test-retest and interrater reliability of the FMS composite score resulted in an ICC3,1 of 0.76 (95% CI: 0.63, 0.85) and an ICC2,1 of 0.74 (95% CI: 0.60, 0.83), respectively. The standard error of the measurement of the composite test was within 1 point, and the MDC95 values were 2.1 and 2.5 points on the 21-point scale for interrater and intrarater reliability, respectively. The interrater agreement of the component scores ranged from moderate to excellent (κw = 0.45-0.82). TTCONCLUSION: Among novice raters, the FMS composite score demonstrated moderate to good interrater and intrarater reliability, with acceptable levels of measurement error. The measures of reliability and measurement error were similar for both intrarater reliability that repeated the assessment of the movement patterns over a 48to-72–hour period and interrater reliability that had 2 raters assess the same movement pattern simultaneously. The interrater agreement of the FMS component scores was good to excellent for the push-up, quadruped, shoulder mobility, straight leg raise, squat, hurdle, and lunge. Only 15.6% (n = 10) of the participants were identified to be at risk for injury based on previously published cutoff values. J Orthop Sports Phys Ther 2012;42(6):530-540, Epub 14 May 2012. doi:10.2519/jospt.2012.3838 TTKEY WORDS: injury prediction, injury prevention, injury risk, interrater, intrarater M ore than 10 000 Americans seek medical treatment for sports, recreational activity, and exercise-related injuries on a daily basis.20 Researchers have estimated that 50% to 80% of these injuries are overuse in nature and involve the lower extremity.1,11,25 In the military, physical training and exercise-related injuries account for 30% of hospitalizations and 40% to 60% of all outpatient visits, with 10 to 12 injuries per 100 soldier-months.12 Although the risk of musculoskeletal conditions and injuries is multifactorial,7,9,10,15,17-19 preliminary evidence suggests that neuromuscular and strength training programs may be beneficial for preventing the occurrence of these conditions.7,9,10,15,17-19 However, tools that assess movement to help predict those at highest risk for musculoskeletal conditions and injuries have been lacking for both athletic and military populations. The Functional Movement Screen (FMS) is a relatively new tool that attempts to address multiple movement factors, with the goal of predicting general risk of musculoskeletal Commander, US Army Public Health Command Region-South, Fort Sam Houston, TX. 2Associate Professor, US Army-Baylor University, Fort Sam Houston, TX. 3Physical Therapy Intern, US Army-Baylor University, Fort Sam Houston, TX. 4Assistant Professor, US Army-Baylor University, Fort Sam Houston, TX. 5Researcher, TRUE Research Foundation, San Antonio, TX. 6Director of Musculoskeletal Research, Department of Physical Therapy (MSGS/SGCUY), 81st Medical Group, Keesler Air Force Base, Biloxi, MS. This research study was approved by the Brooke Army Medical Center Institutional Review Board. The views expressed herein are those of the authors and do not reflect the official policy or position of Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Army, Department of the Air Force, Department of Defense, or the US Government. Address correspondence to Dr Deydre S. Teyhen, US Army-Baylor University, 3151 Scott Road, Room 1303 (ATTN: MCCS-HGEPT), Fort Sam Houston, TX 78234. E-mail: dteyhen@gmail.com or Deydre.teyhen@us.army.mil 1 530 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 530 5/22/2012 5:38:56 PM conditions and injuries.3-5,13,14,16 The FMS was designed to identify functional movement deficits and asymmetries that may be predictive of general musculoskeletal conditions and injuries, with an ultimate goal of being able to modify the identified movement deficits through individualized exercise prescription.3,4 The FMS consists of 7 fundamental movement component tests (FIGURE 1) that are scored on a scale of 0 to 3, with the sum creating a composite score ranging from 0 to 21 points.3,4 The 7 movement patterns that are assessed include the deep squat, in-line lunge, hurdle step, shoulder mobility, active straight leg raise, trunk stability push-up, and quadruped rotary stability. Preliminary research by Kiesel et al14 suggests that National Football League (NFL) players (n = 46) who had a composite score less than or equal to 14 on the FMS had an odds ratio of 11.7 (95% confidence interval [CI]: 2.5, 54.5) and a positive likelihood ratio of 5.8 (95% CI: 2.0, 18.4) to sustain a time-loss injury. Although the specificity was relatively high (0.9; 95% CI: 0.8, 1.0), the sensitivity was low (0.5; 95% CI: 0.3, 0.7), indicating that FMS composite scores less than or equal to 14 may suggest higher injury risk but FMS composite scores greater than 14 do not rule out future injury risk. In a separate study on a group of Marines, a composite score less than or equal to 14 on the FMS demonstrated limited ability to predict all future musculoskeletal injuries (traumatic or overuse), with a sensitivity of 0.45 and specificity of 0.71, while the same cutoff value was able to predict a serious injury (any injury that was severe enough to remove the participant from the training program) with a sensitivity of 0.12 and a specificity of 0.94.21 The FMS was also able to predict injury risk in female collegiate athletes.2 Finally, in another study, firefighters with a previous history of injury demonstrated lower FMS composite scores.23 However, it is not clear for which sports or professions the FMS is optimal in predicting injury risk, what types of musculoskel- FIGURE 1. Functional Movement Screen tests. (A) In-line lunge, (B) hurdle step, (C) deep squat, (D) quadruped rotary stability, (E) active straight leg raise, (F) shoulder mobility, and (G) trunk stability push-up. etal injuries are predicted by low FMS composite scores, and whether the original cutoff score of less than or equal to 14 points on the FMS is valid in the different populations. Additionally, researchers have found that FMS composite scores increased in football players,13 firefighters,6 and service members8 following corrective exercises that addressed possible impairments associated with altered movement patterns noted on the FMS component tests. In a group of Marines, 80% of those with a score less than or equal to 14 also demonstrated lower fitness scores on a standardized fitness test compared to those who had an FMS composite score greater than 14.21 However, Okada et al22 found that FMS composite scores were not related to performance or core stability measures among healthy participants. Interpretation of FMS scores is limited by the scant evidence16 regarding the FMS's psychometric properties and, in particular, the reliability of both composite and individual component scores. An initial study by Minick et al16 found acceptable levels of interrater agreement on the FMS component scores among novice and expert raters in a sample of active college-age participants (to include college varsity athletes). However, this study had several limitations: (1) it did not assess test-retest reliability, (2) all raters assessed the same movement pattern via videotaped analysis, and (3) it only assessed agreement of individual FMS component scores and did not assess the overall FMS composite score, which is typically used as the primary indicator of injury risk. Traditionally, the FMS is assessed in real time, without the benefit of video playback. Variability of human movement across trials theoretically should exist; therefore, testretest analysis could lower the reported agreement values. Additionally, the FMS is often assessed in a group setting (eg, preseason physical or preparticipation screening), requiring the use of multiple raters, who may or may not be the same raters to assess the movement at followup testing. Therefore, a more robust reliability study is required to enhance the understanding of the psychometric properties of the FMS. Although these initial FMS studies, which established the validity of the FMS journal of orthopaedic & sports physical therapy | volume 42 | number 6 | june 2012 | 531 42-06 Teyhen.indd 531 5/22/2012 5:38:57 PM [ for predicting musculoskeletal conditions and injuries and the response to training, are encouraging, their data are preliminary and not published in widely accessible journals. Exploring the psychometric properties of the FMS in a large active population would enhance the generalizability of the previous findings beyond a limited subgroup of professional and collegiate athletes and students. The primary purpose of this study was to determine the intrarater (test-retest) and interrater reliability of the FMS component and composite scores in young, healthy service members, when tested by a counterbalance group of novice raters in real time. Specifically, agreement was assessed on the FMS component scores, whereas reliability, response stability, and error threshold measurements were obtained for the FMS composite scores. A secondary purpose of this study was to describe the FMS component and composite scores in this population. METHODS research report TABLE 1 ] Demographics Type Mean SD 95% CI Age, y 25.2 3.8 24.3, 26.2 Height, cm 175.5 9.6 173.1, 177.9 Weight, kg 77.5 12.5 74.4, 80.7 Body mass index, kg/m2 25.1 3.1 24.3, 25.9 Abbreviation: CI, confidence interval. TABLE 2 FMS Descriptive Analysis* FMS Component Score Test 0 1 2 3 Mean SD Trunk stability push-up 0 7 29 27 2.3 0.7 Quadruped rotary stability 0 3 56 5 2.0 0.3 Shoulder mobility 0 2 19 43 2.6 0.6 Active straight leg raise 0 1 36 27 2.4 0.5 Deep squat 0 3 42 19 2.3 0.5 Hurdle step 0 1 51 12 2.2 0.4 In-line lunge 0 1 29 33 2.5 0.5 Abbreviation: FMS, Functional Movement Screen. *The data displayed represent the first analysis of rater 1 on the first day of data collection (n = 64). Participants T he convenience sample included participants who were recruited over an 8-week period from service members in training at Fort Sam Houston, TX. Potential participants were provided a briefing about the study and were given the opportunity to volunteer. Participants were eligible for inclusion if they were between the ages of 18 and 35 years or emancipated minors (17-yearolds who are considered adults and allowed to join the armed services), fluent in English, and had no current or previous complaint of lower extremity pain, spine pain, or medical or neuromusculoskeletal disorders that limited participation in work or exercise in the last 6 months. Participants were excluded if they were currently seeking medical care for lower extremity injuries or had previous medical history that included any surgery for lower extremity injuries. Participants were also excluded if they were unable to participate in physical training due to other musculoskeletal injuries; had a history of fracture (stress or traumatic) in the femur, pelvis, tibia, fibula, talus, or calcaneus; or were known to be pregnant. Potential participants were provided an overview of the research study and specific details of the entrance criteria. After the presentation was completed, those who met the entrance criteria were asked to squat and then hop unilaterally on each leg in the group setting. Individuals who met the entrance criteria and did not have pain on the squat and hop tests were informed about upcoming data collection dates. Those individuals who opted to volunteer returned the following week to sign informed consent forms and were enrolled in the study. Within the military training environment, these procedures allowed potential participants the option to not return if they were not interested in volunteering in the study, and were designed to minimize any potential perception of coercion. All participants signed consent forms approved by the Brooke Army Medical Center Institutional Review Board. Examiners The novice examiners participating in this study consisted of 8 physical therapy students enrolled in their second and third semesters of a doctor of physical therapy training program prior to their 1-year clinical internship. Before testing, all examiners underwent 20 hours of FMS training led by 4 physical therapists and 1 research assistant. Four physical therapy students were randomly assigned to the participants to assess intrarater test-retest reliability by assessing the FMS on day 1 and day 2. The goal of randomly selecting a rater to perform the intrarater test-retest reliability was to increase the variability in the study design. Each rater used for the intrarater test-retest reliability measured between 532 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 532 5/22/2012 5:38:58 PM 14 and 18 participants. There were no differences in outcomes across raters, so aggregate data were analyzed. A second set of 4 physical therapy students were randomly assigned to view the participants’ movement simultaneously with the first set of raters for the interrater reliability assessment on day 2. To minimize bias, raters were randomly assigned, raters for day 2 were blinded to day 1 raters’ measurements, pairs of raters on day 2 were blinded to each other's analysis and scoring, and 48 to 72 hours of time elapsed between intrarater testretest reliability measurements. The goal of having a random set of 2 raters assess each participant was to increase the variability in the study design to more closely mimic field conditions, which often include mass screenings that utilize multiple raters. Procedures The FMS is composed of 7 component tests used to assess different fundamental movement patterns.3-5 Participants completed the component tests in a counterbalanced order, including the deep squat, hurdle step, in-line lunge, shoulder mobility, active straight leg raise, trunk stability push-up, and quadruped rotary stability tests (FIGURE 1). Five of 7 component tests assess asymmetry by measuring the test bilaterally. If discrepancies exist between the left and right sides, asymmetry is noted for that component test and the lower of the 2 scores is included in the FMS composite score. In addition to the 7 component tests, the FMS includes 3 clearing tests that assess for pain: shoulder internal rotation and abduction with the hand placed on the opposite shoulder, lumbar extension performed in the prone press-up position, and end-range lumbar flexion in quadruped. Pain on a clearing test resulted in a score of 0 for the shoulder mobility, trunk stability push-up, or rotary stability test, respectively. Participants performed all tests without a preparticipation warm-up. Each component test was scored on an ordinal scale (0 to 3 points), based on the quality of movement, with 3 being the maximum score.3-5 A score of 2 indicated that the participant required some type of compensation or was unable to complete the entire movement. A score of 1 was given if the individual was unable to remain in the movement position throughout the movement, lost balance during the test, or did not meet the minimum criteria to score a 2. Pain during any of the FMS component tests or during any of the clearing tests indicated a score of 0. All participants were allowed to perform each component test up to 3 times, and the maximal score achieved was recorded. The scores of the component tests were summed, resulting in a composite score from 0 to 21 points, with 21 being the maximum composite score. Additional details on scoring of each of the component tests and the composite score are provided elsewhere3-5 and in the APPENDIX. Statistical Analysis Descriptive statistics and frequency counts were calculated. Agreement of the component tests was analyzed with a weighted kappa statistic. The weighted kappa scores were as follows: 80% and higher, excellent agreement; from 60% to 79.9%, substantial levels of agreement; from 40% to 59.9%, moderate agreement; and below 40%, poor to fair agreement.24 Reliability of the composite test scores was analyzed using intraclass correlation coefficients (ICCs). ICC values of 0.75 and above represent good reliability, those between 0.50 and 0.74 represent moderate reliability, and those below 0.50 indicate poor reliability.24 Intrarater test-retest reliability was assessed using an ICC3,1 model, while interrater reliability was assessed using an ICC2,1 model. Response stability of the intrarater and interrater reliability of the composite scores was calculated using the standard error of the measurement (SEM) at the 95% level of confidence. The minimal detectable change (MDC95) values at the 95% level of confidence were calculated to determine error thresholds. Statistical analyses were conducted using SPSS Version 17.0 (SPSS Inc, Chicago, IL). RESULTS S ixty-four participants (53 males, 11 females) met the inclusion and exclusion criteria and completed the study (TABLE 1). The mean SD age of the participants was 25.2 3.8 years and their body mass index was 25.1 3.1 kg/m2. Overall, the participants included routine exercisers who endorsed a statement that they exercised a minimum of 4 days per week (n = 54, 78.2%). Although the participants were attending training for their military occupation, the majority of the participants were routine exercisers for more than 3 years. Specifically, 29 (45.3%) participants reported performing routine exercise for more than 5 years, 21 (32.8%) for 3 to 5 years, 9 (14.1%) for 1 to 3 years, and 5 (7.8%) for less than 1 year. Descriptive statistics on FMS performance are provided in TABLE 2. None of the participants had pain on the 3 FMS clearing tests. Interrater reliability was calculated on 63 participants, based on an illness of 1 of the raters on day 2 of testing. Only 15.6% (n = 10) of the participants were identified to be at risk for injury, based on an FMS composite score of less than or equal to 14 points. Agreement of the 7 component tests of the FMS (scored 0 to 3) demonstrated moderate to excellent interrater agreement (TABLE 3). Specifically, the novice raters demonstrated excellent interrater agreement on the trunk stability pushup; substantial interrater agreement on the quadruped rotary stability, deep squat, active straight leg raise, hurdle step, and shoulder mobility component tests; and moderate interrater agreement on the in-line lunge. Intrarater (test-retest) agreement scores at 48 to 72 hours demonstrated substantial agreement on the trunk stability push-up, shoulder mobility, active straight leg raise, deep squat, and in-line lunge component tests; moderate agreement on the hurdle step; and poor agreement on the quadruped rotary journal of orthopaedic & sports physical therapy | volume 42 | number 6 | june 2012 | 533 42-06 Teyhen.indd 533 5/22/2012 5:38:59 PM [ TABLE 3 research report Agreement of FMS Component Scores (0-3 points) Percent Agreement κw 95% CI Trunk stability push-up 78 0.82 0.73, 0.90 Quadruped rotary stability 92 0.77 0.57, 0.96 Shoulder mobility 86 0.73 0.57, 0.89 Active straight leg raise 84 0.69 0.51, 0.87 Deep squat 83 0.68 0.51, 0.85 Hurdle step 88 0.67 0.45, 0.88 In-line lunge 68 0.45 0.25, 0.65 Trunk stability push-up 68 0.68 0.55, 0.81 Quadruped rotary stability 83 0.29 0.05, 0.50 Shoulder mobility 81 0.68 0.53, 0.80 Active straight leg raise 80 0.60 0.42, 0.74 Deep squat 88 0.76 0.63, 0.85 Hurdle step 86 0.59 0.42, 0.73 In-line lunge 83 0.69 0.48, 0.77 Type/Test Interrater Intrarater Abbreviations: CI, confidence interval; FMS, Functional Movement Screen. TABLE 4 Reliability of FMS Composite Scores (0-21 points) Type ICC 95% CI SEM MDC95 Interrater 0.76 0.63, 0.85 0.92 2.54 Intrarater (test-retest) 0.74 0.60, 0.83 0.98 2.07 Abbreviations: CI, confidence interval; FMS, Functional Movement Screen; ICC, intraclass correlation coefficient; MDC95, minimal detectable change at the 95% level of confidence; SEM, standard error of measurement. stability component test. The interrater reliability (same day) of the FMS composite score (scored 0-21) resulted in an ICC2,1 of 0.76 (95% CI: 0.63, 0.85) and was considered good (TABLE 4). The SEM for interrater reliability of the composite test was 0.92 points, and the MDC95 was 2.54 points on the 21-point scale. Visual representation of the FMS composite scores between raters is provided in FIGURE 2. The intrarater reliability (test-retest at 48 to 72 hours) of the FMS composite scores resulted in an ICC3,1 of 0.74 (95% CI: 0.60, 0.83) and was considered to be moderate (TABLE 4). Visual representation of the intrarater test-retest FMS composite scores is provided in FIGURE 3. The SEM for intrarater test-retest reliability was 0.98 points and the MDC95 was 2.07 points. DISCUSSION T he FMS has an adequate level of reliability when assessed in healthy service members by novice raters. The interrater agreement of the FMS component scores ranged from moderate to excellent, with 6 of the 7 tests categorized as having substantial agreement (κw60%). The intrarater and interrater point estimates of the FMS composite score reliability ranged from 0.74 to 0.76, with the 95% CIs suggestive of moderate to good reliability. The SEMs for both interrater and intrarater reliability were ] less than 1 point, while the MDC95 ranged from 2.1 to 2.5 points on the 21-point scale. The SEM and MDC values were similar for both intrarater reliability that repeated the assessment of the movement patterns over a 48-to-72–hour period and interrater reliability that had 2 raters assess the same movement pattern simultaneously. Therefore, one can expect the error of measurement to be within 1 point across raters and across time, while a minimum improvement between 2 and 3 points on the 21-point scale would be required to demonstrate a real change over time. These results are consistent with a prior publication on FMS reliability. Minick et al16 reported substantial to excellent interrater agreement on individual FMS component scores when using 2 novice and 2 expert raters assessing videotape performance of active collegeage students and varsity athletes. Adding to the literature, our study provides detailed information on the intrarater and interrater reliability of both FMS component and composite scores by randomly assigned novice raters. Specifically, our study utilized 8 entry-level physical therapy students as raters to collect data prior to their clinical internship. Additionally, these raters measured all movements in real time, without the benefit of being able to replay a videotape (the methodology used by Minick et al16). The increased number of raters and real-time analysis of movement in multiple participants in our study mimic a preparticipation screening environment, thus enhance the generalizability of the results. Further research is needed to assess the stability of the FMS scores over longer periods. Ultimately, the reliability of this group of novice raters was comparable to previously published research and provides further support for the FMS as a reliable tool to screen in a relatively diverse, noncollegiate but physically active population.16 Only 15.6% (n = 10) of the participants in this study had an FMS composite score less than or equal to 14 points. 534 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 534 5/22/2012 5:39:00 PM Rater 2 Rater 1 12 13 14 15 16 17 18 19 Total 12 2 1 1 0 0 0 0 0 4 13 1 0 1 0 0 0 0 0 2 14 1 2 1 0 0 0 0 0 4 15 0 0 3 4 3 0 0 0 10 16 0 1 4 1 6 1 0 0 13 17 0 0 1 3 3 2 3 2 14 18 0 0 0 1 1 6 4 0 12 19 0 0 0 0 0 1 1 1 3 20 0 0 0 0 0 0 0 1 1 Total 4 4 11 9 13 10 8 4 63 FIGURE 2. Comparison of Functional Movement Screen composite scores between rater 1 and rater 2. Green boxes indicate agreement (n = 20), yellow boxes indicate a composite-score difference of only 1 point (n = 27), and orange boxes indicate a composite-score difference of 2 to 3 points (n = 16). FMS Day 2 Composite Score FMS Day 1 Composite Score Although this may not seem surprising, given that the participants were relatively healthy, it supports the suggestion by Cook et al3,4 that FMS scores can identify altered movement patterns in generally healthy and pain-free participants. Our results are similar to those published by O’Connor et al,21 who found that 10% of the 874 Marine officer candidates scored less than or equal to 14 points on the FMS. If the initial research that identified the cutoff value were validated, it would suggest that the FMS would be capable of identifying a subset of individuals at increased risk for time-loss injury within a population of young, healthy service members. Based on the use of the FMS for mass screenings (eg, preseason or annual physical examinations), an injury prediction screening that could identify only 15.6% of the population as having a high injury risk would allow the associated medical staff to prioritize the allocation of limited resources toward the development of individualized injury prevention interventions (eg, corrective exercise prescriptions) for this group. However, the validity of the 14-point cutoff score for this sample cannot be verified in this study, because longitudinal followup was not performed to assess actual injury rates. Based on the SEM of 1 point and the MDC95 value between 2.1 and 2.5 points, it would be more conservative to use a cutoff score of 15 (based on SEM) or 16 to 17 (based on MDC95) to determine those who may benefit from corrective exercise prescription to help mitigate injury risk, until the validity of the 14-point cutoff value can be determined. One of the limitations noted in the FMS component tests was a restriction in the range of scores. Specifically, based on our inclusion/exclusion criteria, no participants scored a 0 on any of the FMS component tests, and only 18 of the 446 scored movement patterns resulted in a score of 1; the remaining movement patterns either received a score of 2 or 3. This restriction in range might have reduced the reliability estimates of the FMS component scores. For example, 12 13 14 15 16 17 18 19 Total 10 1 0 0 0 0 0 0 0 1 11 0 0 0 0 0 0 0 0 0 12 1 1 1 0 0 0 0 0 3 13 2 1 1 1 0 0 0 0 5 14 0 1 1 1 2 1 0 0 6 15 0 1 2 5 3 1 0 0 12 16 0 0 5 0 4 3 1 0 13 17 0 0 0 2 4 1 2 0 9 18 0 0 1 0 1 2 4 4 12 19 0 0 0 0 0 2 0 0 2 20 0 0 0 0 0 0 1 0 1 Total 4 4 11 9 14 10 8 4 64 FIGURE 3. Comparison of FMS composite scores for rater 1 (day 1 to day 2). Green boxes indicate agreement (n = 17), yellow boxes indicate a composite-score difference of only 1 point (n = 26), orange boxes indicate a compositescore difference of 2 to 3 points (n = 20), and the red box indicates a composite-score difference greater than 3 points (n = 1). Abbreviation: FMS, Functional Movement Screen. the in-line lunge was determined to have a weighted kappa of 0.45; for this test, no movements were scored as a 0 or 1. Additionally, only 11 of the 63 paired ratings had a disagreement, with 25 agreements for a score of 2 and 27 agreements for a score of 3. Compared to the other FMS component scores, the in-line lunge and the quadruped rotary stability had the biggest discrepancy between the percent agreement (68% and 83%, respectively) and weighted kappa (0.45 and 0.29, re- journal of orthopaedic & sports physical therapy | volume 42 | number 6 | june 2012 | 535 42-06 Teyhen.indd 535 5/22/2012 7:42:05 PM [ spectively). Interestingly, the lowest levels of agreement between novice raters for both our study and Minick et al16 involved the in-line lunge and quadruped rotary stability tests. Difficulty in performing the quadruped rotary stability test (only 5 of the 64 participants obtained a score of 3 on day 1) also limited variability and potentially intrarater agreement of this measure. Although the restricted range might have influenced statistical calculations, it is important to point out that rater experience and lack of clearly defined scoring criteria, especially mid-range performance, may have also influenced results for these select measures. Future research should determine whether better criteria may help to differentiate levels of performance on the quadruped rotary stability test or to determine the influence of removing the quadruped rotary stability test on the predictive validity of the FMS composite score. Future study designs should assess the reliability of the FMS using novice raters and participants with varying activity levels and sport-specific requirements. Additional longitudinal studies are also required to establish the predictive validity and optimal cut score for various populations. This level of critical investigation would help to enhance the external validity of the FMS and to substantiate its use in the general clinical population, as well as in specific sports settings. Future research should also determine whether there is a ceiling effect in the ability of the FMS to detect change over time. Based on the MDC95 of 2.1 to 2.5 points, positive change may not be able to be noted for individuals who score greater than 18 points at baseline testing. Different scoring criteria or cutoff values may be needed to better differentiate high-end performance on the FMS. CONCLUSIONS A mong novice raters, the FMS composite score demonstrated moderate to good interrater and intrarater reliability, and acceptable lev- research report els of measurement error. The measures of reliability and measurement error were similar for both intrarater reliability that repeated the assessment of the movement patterns over a 48-to-72–hour period and interrater reliability that had 2 raters assess the same movement pattern simultaneously. The interrater agreement of the FMS component scores was good to excellent for the push-up, quadruped, shoulder mobility, straight leg raise, squat, hurdle, and lunge. Only 15.6% (n = 10) of the participants were identified as being at risk for injury based on previously published cutoff values. t ] Warren, and First Lieutenant Sam Wood. Illustrations for the APPENDIX were provided by Elizabeth Holder. KEY POINTS FINDINGS: When using novice raters, the FMS composite scores had moderate to good reliability (ICC = 0.74 and 0.76; SEM, 1.0 points; MDC95, 2.1 and 2.5 points) and the FMS component scores ranged from moderate to excellent agreement (κw = 0.29-0.82). IMPLICATIONS: The FMS has adequate reliability when assessed in young, healthy service members by novice raters over a 48-to-72–hour period. CAUTION: Reliability data must be interpreted within the context of the sample tested and the methods used (ie, time between testing for test-retest reliability estimates). ACKNOWLEDGEMENTS: This study was done in collaboration with research assistants from the University of Texas Health Science Center, Physical Therapy Department, San Antonio, TX: Mark Bauernfeind, Francis Bisagni, Jordan Boldt, Cindy Boyer, Cara Dobbertin, Steve Elliot, Angela Gass, Germaine Herman, Lacey Jung, Jake Mitchess, Teddy Ortiz, Kelly Rabon, Jason Smith, Megan Swint, Joshua Trock, and Jerry Yeung. Additional research assistants from US Army-Baylor University, Department of Physical Therapy, US Army Medical Department Center and School, San Antonio, TX: First Lieutenant Moshe Greenberg, Captain Sarah Hill, First Lieutenant Crystal Straseske, First Lieutenant Sarah Villena, First Lieutenant Christina Yost, First Lieutenant Kristen Zosel, First Lieutenant Rick REFERENCES 1. A lmeida SA, Williams KM, Shaffer RA, Brodine SK. Epidemiological patterns of musculoskeletal injuries and physical training. Med Sci Sports Exerc. 1999;31:1176-1182. 2. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5:47-54. 3. Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function - part 1. N Am J Sports Phys Ther. 2006;1:62-72. 4. Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function - part 2. N Am J Sports Phys Ther. 2006;1:132-139. 5. Cook G, Burton L, Kiesel K, Rose G, Bryant MF. Movement: Functional Movement Systems: Screening—Assessment—Corrective Strategies. Aptos, CA: On Target Publications; 2010. 6. Cowen VS. Functional fitness improvements after a worksite-based yoga initiative. J Bodyw Mov Ther. 2010;14:50-54. http://dx.doi. org/10.1016/j.jbmt.2009.02.006 7. Emery CA, Rose MS, McAllister JR, Meeuwisse WH. A prevention strategy to reduce the incidence of injury in high school basketball: a cluster randomized controlled trial. Clin J Sport Med. 2007;17:17-24. http://dx.doi.org/10.1097/ JSM.0b013e31802e9c05 8. Goss DL, Christopher GE, Faulk RT, Moore J. Functional training program bridges rehabilitation and return to duty. J Spec Oper Med. 2009;9:29-48. 9. Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37:303311. http://dx.doi.org/10.2519/jospt.2007.2322 10. Holm I, Fosdahl MA, Friis A, Risberg MA, Myklebust G, Steen H. Effect of neuromuscular training on proprioception, balance, muscle strength, and lower limb function in female team handball players. Clin J Sport Med. 2004;14:88-94. 11. Jones BH, Cowan DN, Tomlinson JP, Robinson JR, Polly DW, Frykman PN. Epidemiology of injuries associated with physical training among young men in the army. Med Sci Sports Exerc. 1993;25:197-203. 12. Jones BH, Knapik JJ. Physical training and exercise-related injuries. Surveillance, research and injury prevention in military populations. Sports Med. 1999;27:111-125. 13. Kiesel K, Plisky P, Butler R. Functional move- 536 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 536 5/22/2012 5:39:02 PM 14. 15. 16. 17. ment test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports. 2011;21:287-292. http://dx.doi. org/10.1111/j.1600-0838.2009.01038.x Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther. 2007;2:147-158. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003-1010. http://dx.doi. org/10.1177/0363546504272261 Minick KI, Kiesel KB, Burton L, Taylor A, Plisky P, Butler RJ. Interrater reliability of the functional movement screen. J Strength Cond Res. 2010;24:479-486. http://dx.doi.org/10.1519/ JSC.0b013e3181c09c04 Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization 18. 19. 20. 21. and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20:345-353. http://dx.doi. org/10.1519/R-17955.1 Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445-455. http://dx.doi.org/10.1177/0363546505281241 Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51-60. http://dx.doi.org/10.1519/13643.1 National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. CDC Injury Research Agenda. Atlanta, GA: US Department of Health and Human Services; 2002. O’Connor FG, Deuster PA, Davis J, Pappas CG, Knapik JJ. Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011;43:2224-2230. http://dx.doi. org/10.1249/MSS.0b013e318223522d 22. O kada T, Huxel KC, Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25:252-261. http://dx.doi.org/10.1519/ JSC.0b013e3181b22b3e 23. Peate WF, Bates G, Lunda K, Francis S, Bellamy K. Core strength: a new model for injury prediction and prevention. J Occup Med Toxicol. 2007;2:3. http://dx.doi. org/10.1186/1745-6673-2-3 24. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall; 2000. 25. van Mechelen W. Running injuries. A review of the epidemiological literature. Sports Med. 1992;14:320-335. @ MORE INFORMATION WWW.JOSPT.ORG APPENDIX FUNCTIONAL MOVEMENT SCREEN Score Criteria Illustration Deep Squat 3 2 1 0 • Upper torso is parallel with tibia or toward vertical • Femur below horizontal • Knees are aligned over feet • Dowel aligned over feet Performed with heels on 2 × 6-in board • Upper torso is parallel with tibia or toward vertical • Femur below horizontal • Knees are aligned over feet • Dowel aligned over feet Performed with heels on 2 × 6-in board • If any of the 4 criteria are not met when the squat is performed with heels on 2 × 6-in board, the score is 1 • Pain during test journal of orthopaedic & sports physical therapy | volume 42 | number 6 | june 2012 | 537 42-06 Teyhen.indd 537 5/22/2012 5:39:03 PM [ research report ] APPENDIX Score 3 2 1 0 3 2 1 0 3 Criteria • • • • • • • • • Hurdle Step (test both right and left sides)* Foot clears cord (does not touch) and remains dorsiflexed as leg is lifted over hurdle Hips, knees, and ankles remain aligned in the sagittal plane Minimal to no movement is noted in lumbar spine Dowel and hurdle remain parallel Alignment is lost between hips, knees, and ankles Movement is noted in lumbar spine Dowel and hurdle do not remain parallel Contact between foot and hurdle Loss of balance is noted Pain during test • • • • • • • • • • • • • In-line Lunge (test both right and left sides)* nee touches board behind heel K Dowel and feet remain in sagittal plane Dowel contacts remain (head, thoracic spine, sacrum) Dowel remains vertical, no torso movement noted Knee does not touch behind heel Dowel and feet do not remain in sagittal plane Dowel contacts do not remain Dowel remains vertical Movement is noted in torso Loss of balance is noted Inability to achieve start position Inability to touch knee to board Pain during test • • • 2 • • 1 • 0 • Illustration Active Straight Leg Raise (test both right and left sides)* Malleolus of tested lower extremity located in the region between mid-thigh and anterior superior iliac spine of opposite lower extremity (green region) Opposite hip remains neutral (hip does not externally rotate), toes remain pointing up Opposite knee remains in contact with board Malleolus of tested lower extremity located in the region between mid-thigh and knee joint line of opposite lower extremity (yellow region) while other criteria are met Malleolus of tested lower extremity located in the region below knee joint line of opposite lower extremity (red region) while other criteria are met Pain during test 538 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 538 5/22/2012 5:39:05 PM APPENDIX Score Criteria 3 2 1 0 Shoulder Mobility (test both right and left sides)* • Fists are within 1 hand length • Fists are within 1.5 hand lengths • Fists are not within 1.5 hand lengths • Pain during test Shoulder mobility clearing test: if pain is noted as elbow is lifted, shoulder mobility is scored as 0 3 2 1 0 Illustration Trunk Stability Push-up • P erform 1 repetition; the thumbs are aligned with forehead for males and chin for females • Body is lifted as 1 unit (no sag in lumbar spine) • Perform 1 repetition; the thumbs are aligned with chin for males and clavicle for females • Body is lifted as 1 unit (no sag in lumbar spine) • Unable to perform 1 repetition with thumbs aligned with chin for males and clavicle for females • Pain during test Extension clearing test: if pain is noted during a prone press-up, pushup is scored as 0 journal of orthopaedic & sports physical therapy | volume 42 | number 6 | june 2012 | 539 42-06 Teyhen.indd 539 5/22/2012 5:39:06 PM [ research report ] APPENDIX Score 3 2 1 0 Criteria Illustration Quadruped Rotary Stability (test both right and left sides)* • 1 unilateral repetition (lift arm and leg from same side of body) • Keep spine parallel to board • Knee and elbow touch in line over the board and then return to the start position • 1 diagonal repetition (lift arm and leg from opposite sides of body) • Keep spine parallel to board • Knee and elbow touch in line over the board and then return to the start position • Inability to perform diagonal repetition • Pain during test Flexion clearing test: if pain is noted during quadruped flexion, rotary stability is scored as 0 *For component tests that are scored for both the right and left sides, the lower score is used when calculating the Functional Movement Screen composite score. GO GREEN By Opting Out of the Print Journal JOSPT subscribers and APTA members of the Orthopaedic and Sports Physical Therapy Sections can help the environment by “opting out” of receiving the Journal in print each month as follows. If you are: · A JOSPT subscriber: Email your request to jospt@jospt.org or call the Journal office toll-free at 1-877-766-3450 and provide your name and subscriber number. · An APTA Orthopaedic or Sports Section member: Go to www.apta.org and update your preferences in the My Profile area of myAPTA. Select “myAPTA” from the horizontal navigation menu (you’ll be asked to login, if you haven’t already done so), then proceed to “My Profile.” Click on the “Email & Publications” tab, choose your “opt out” preferences and save. Subscribers and members alike will continue to have access to JOSPT online and can retrieve current and archived issues anytime and anywhere you have Internet access. 540 | june 2012 | volume 42 | number 6 | journal of orthopaedic & sports physical therapy 42-06 Teyhen.indd 540 5/22/2012 5:39:07 PM