GlaxoSmithKline Medal of Merit 2012- Rohan Elliott MEDICATION SAFETY GERIATRIC THERAPEUTICS AWARDS
advertisement

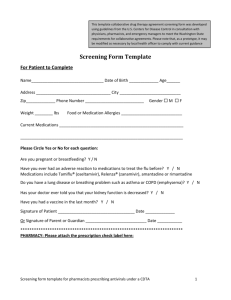
GERIATRIC MEDICATION AWARDS THERAPEUTICS SAFETY GlaxoSmithKline Medal of Merit 2012-Rohan Elliott The GlaxoSmithKline Medal of Merit has been awarded annually since 1962 in recognition of an outstanding contribution to the practice of hospital pharmacy or the professional development of pharmacy. The recipient of the GlaxoSmithKline Medal of Merit 2012 is Rohan Elliott, Senior Aged Care Pharmacist at Austin Health, and Clinical Senior Lecturer and Unit Coordinator in geriatric pharmacy practice at Monash University. Rohan has a long history of collaborative research in aged care highlighted by the recent MedGap project for which he was the principal investigator. The MedGap project was ground breaking as it quantied the impact of using an interim medication chart for patients transferred from hospital to a residential aged-care facility. The project won the Victorian Public Healthcare Award: Excellence in Service Provision 2011. The use of the interim medication chart has transformed the interface between hospital and residential care and is now standard care at Austin Health and some other facilities. The success of this project has prompted the Australian Commission on Safety and Quality in Health Care to commence work on a national interim residential care medication administration chart. Rohan has also been actively involved in SHPA, including serving as treasurer and chair of the Victorian Branch Committee and is currently a member of two reference groups. Rohan also participates in many committees and working groups including the Australian Commission on Safety and Quality in Health Cares National Residential Medication Chart Reference Group and the Victorian Governments Medication Reconciliation Working Party. The GlaxoSmithKline Medal of Merit for 2012 is awarded in recognition of Rohan Elliotts commitment to hospital pharmacy practice through his ongoing work as a clinical practitioner, researcher and educator. Rohan Elliott (C) recipient of the GlaxoSmithKline Medal of Merit 2012 with GSK National Sales Manager Julian Taylor (L) and SHPA Federal Vice President Amber Roberts. Opportunities in Aged Care Rohan A Elliott I would like to thank the Society of Hospital Pharmacists of Australia (SHPA) and GlaxoSmithKline for making this award available. I am also grateful to the Victorian Branch for nominating me and the Federal Council for selecting me. It is a great honour to be recognised by my peers in this way. Of course I would not be standing here today if it were not for the support and assistance of many people that I have been lucky to work with over the years, and in particular a few key individuals who I will mention later. Receiving this award made me re!ect on how and why I came to be doing the work that I have in aged care, and on the role of pharmacists in aged care. I would like to share a few thoughts about my journey into aged care and collaborative research, the aged-care health system, and the opportunities that exist for pharmacists in aged care. It is no secret that Australias population is ageing. Average life expectancy has risen from 60 to more than 80 years over the last century. The number of Australians aged over 65 years is projected to increase from its current level of around 3 million to over 8 million by 2050. Rohan A Elliott, BPharm, BPharmSc (Hons), MClinPharm, CGP, FSHP, Senior Pharmacist, Austin Health, and Clinical Senior Lecturer, Centre for Medicine Use and Safety, Monash University, Parkville, Victoria Corresponding author: Rohan Elliott, Pharmacy Department, Heidelberg Repatriation Hospital, Heidelberg Vic. 3081, Australia. E-mail: rohan.elliott@austin.org.au Journal of Pharmacy Practice and Research Volume 42, No. 4, 2012. The number of people aged over 80 years is expected to quadruple, leading to a huge increase in demand for aged-care services. Given that older people are the biggest users of medicines, the demand for pharmacist services in aged care can only grow.1 Another factor driving demand for pharmacist services is the increasing complexity of medication management for older people. The average number of drugs prescribed for hospitalised older people has doubled over the course of my career, from about 4.5 in the early 1990s to around 9 today.2,3 With evidencebased guidelines supporting multi-drug therapy for most chronic diseases that affect older people, this trend is likely to continue as the population ages. My journey into Aged Care My journey into aged care began in the mid 1990s, when the then Director of Pharmacy at the Austin Hospital, Bill Thomson, encouraged me to apply for a travel grant to visit the USA to explore the role of consultant pharmacists in nursing homes, and to attend the American Society of Hospital Pharmacists clinical conference. This was just prior to the time that residential medication management reviews were funded by the Australian Government, enabling pharmacists to be remunerated for clinical services in aged-care homes. Following this study tour I became accredited to do medication reviews and secured contracts for the Austin pharmacy with four local aged305 care homes and for a number of years we provided a clinical service to these homes. Conducting an evaluation of that service sparked my interest in research and led me to a position as a research pharmacist at the Centre for Applied Gerontology.4 There I managed a multicentre study of prescribing for older hospital inpatients, and assisted with one of the Department of Health and Ageing-sponsored studies that led to the Home Medicines Review program.5,6 These experiences showed me how research and clinical practice can be combined, and how collaborative interdisciplinary research can support and drive the development of clinical pharmacy practice. I thank Bill for sending me down this path and supporting my work in those early years. I then had a few years away from direct involvement in aged care, when I became involved in clinical teaching at Austin Health and then postgraduate teaching at Monash University. This opened my eyes to the potential for combining teaching with clinical practice and research, and in 2006 I moved into my current role in which I have attempted to combine these three areas. I emphasise the word attempted, because it has been a challenge to maintain a balance between these three activities with research and teaching usually taking up most of my time, along with other commitments such as reference groups and committees. At that time, in 2006, I had formed the view that pharmacists were under-utilised in aged care. For example at Austin Health we were providing a basic clinical pharmacy service to our aged-care wards and we had no involvement in the many ambulatory aged-care programs provided by our health service. I also noted that there was little opportunity for postgraduate study for pharmacists in geriatrics and aged care. I proposed the creation of a joint appointment between the university and the hospital with the goal of developing the aged-care pharmacy service at Austin Health and postgraduate units for pharmacists in aged care for the university. I was fortunate to have the support of my two bosses at the time, Professor Roger Nation, then head of the Department of Pharmacy Practice, Monash University, and Kent Garrett, Director of Pharmacy, Austin Health. I would especially like to acknowledge the support of Kent Garrett, who shared my vision for developing and improving aged-care pharmacy services and using collaborative research to facilitate that development. Without Kents tremendous support I would not have been able to do the work that has led to this award, and I would certainly not be standing here today. Aged Care System Australias aged-care system is complex with a wide range of programs funded by all three levels of government. The vast array of programs and different administration and funding arrangements makes it difcult for patients, carers and health professionals to understand and navigate the system. Some reforms of the system have been proposed, but it is likely that the system will remain complex. In my experience few pharmacists, even those practising in aged care, really understand the aged-care system and its many programs, especially those delivered outside the hospital walls such as Aged Care Assessment Teams, Transition Care Programs, Home and Community Care, Community Aged Care Packages, Extended Aged Care Packages (and the list goes on). This is a shame, because there are many opportunities for pharmacists in this space. In my opinion, pharmacists are under-utilised in most of these programs, and I am not alone in that view. 306 Opportunities in Aged Care In recent years I have been involved in a number of projects and committees that have required me to work closely with other health professionals in the aged-care sector, such as doctors, nurses, allied health professionals and managers from hospital, residential care and primary care settings. Two things have become very clear. First, many of the things that pharmacists do are not well understood and we need to do more to market ourselves. For example our contribution to continuity of medication management, such as medication reconciliation, discharge medication planning and clinical handover is poorly understood by other health professionals even within hospitals and is virtually unknown to those outside hospitals and to consumers. Second, despite the scope of our role being poorly understood, there is a lot of support for greater involvement of pharmacists in aged care. This is because the ageing population and increasing intensity and complexity of drug therapy are making medication management a major concern for people working in aged care, and pharmacists are seen as part of the solution. Many aged-care programs are managed, coordinated and/or delivered by allied health professionals, for example case managers in Post-Acute Care, Transition Care and community aged-care programs are usually social workers, occupational therapists, speech therapists, physiotherapists and nurses, most of whom are illequipped to deal with complex medication issues. There is little involvement of pharmacists in these programs. Several times this year I have been at multidisciplinary aged-care meetings and forums, often as the only pharmacist present. The role of pharmacists has come up, and potential to better utilise pharmacists has been raised, without any suggestion from me. There is clearly a perception that we could do more. Proposed areas for greater pharmacist involvement include: assessment of patients medication management, medication review, risk assessment, regimen simplication, screening for cognitive impairment and dementia, staff education and clinical handover. As a profession, we need to nd a way to tap into and capitalise on this demand, and get more involved in aged care. Collaborative research, to develop an evidence-base to underpin expansion of our role within these services, is one way forward. The MedGap project, which was a collaboration between Austin Health, Northern Health and a local division of general practice, demonstrated how pharmacists can contribute to clinical handover and continuity of care in a cost-effective way through the provision of interim residential care medication charts, and has captured the attention of clinicians, governments and hospital managers.7,8 This is just the tip of the iceberg. There is far more we could do in this area. Our role in continuity of care needs to be better marketed to governments and other healthcare funders to ensure that hospital pharmacy departments are adequately resourced to do this work. We also need to increase our use of pharmacy technicians, to enable pharmacists to focus more on direct patient care. If we dont increase our use of technicians to support clinical pharmacy services, our ability to deliver these services, and job satisfaction, will dwindle as the intensity and complexity of medication use continues to rise and length of stay in hospital continues to fall. In a project at Austin Health, sponsored by Health Workforce Australia, we expanded the role of a ward pharmacy technician in subacute aged care, which freed up the Journal of Pharmacy Practice and Research Volume 42, No. 4, 2012. MEDICATION SAFETY pharmacist to spend more time on clinical tasks such as medication review, medication management assessment and discharge planning, and resulted in less unpaid overtime and greater job satisfaction.9 Managing ones own medications is an instrumental activity of daily living an activity a person needs to be able to perform to live independently.10 Assessment of older patients medication management is an area in which I think pharmacists could certainly do more. I was recently talking to a social worker from our Aged Care Assessment Team who assesses inpatients referred to the Transition Care Program. When I asked her how she determined patients level of functioning and post-discharge support needs, she indicated that for mobility she referred to the physiotherapists assessment, and for tasks such as dressing, washing, shopping and cooking she referred to the occupational therapists assessment. However, for medication management there was no reference to the pharmacist, nor any attempt to objectively establish what the patient is likely to be capable of after discharge. Often cognitive function (e.g. Mini-Mental State Examination score) is used as a proxy for medication management ability; but this is a !awed approach. And this is not unusual. I have had similar conversations with a liaison nurse who reviews inpatients referred for Post Acute Care and community nursing services after discharge, and also with community nurses who receive referrals for medication management support in the community. Decisions about medication management are often made in an ad hoc way, without formal or structured assessment. Nobody is routinely assessing and documenting patients medication management capacity as part of care planning. In other projects with colleagues at Austin Health we have identied a range of problems and gaps in medication management for patients referred to aged care outpatient clinics and Aged Care Assessment Teams, again highlighting the under-utilisation and potential roles for pharmacists in these services.11,12 It is this under-utilisation of pharmacists, and potential for pharmacists to contribute more towards improving the care of older people, that has driven me to do the work I have done. I have tried to educate pharmacists about the various aged-care programs and how they can contribute to them and refer people to them, through the postgraduate units that I teach. I have tried to increase pharmacists involvement in these programs through collaborative inter-disciplinary research, by quantifying some of the medication-related problems that exist and demonstrating how pharmacists can address these. Given the need and the opportunities that exist in aged care, I would encourage pharmacists to look for and pursue these opportunities within their organisation and beyond. Based on my experiences, I offer a few tips to those seeking to develop roles or services: Take an evidence-based approach. Describe and quantify the problems using robust methodology, in order to make a strong case for change and to demonstrate that the change once made will improve patient care. For example with the MedGap project, until we collected our baseline data to describe and quantify the gaps in continuity of medication management we had difculty getting the attention and buy-in from some key stakeholders. Collaborate with other disciplines and with consumers. Aged care is a multidisciplinary environment, and it is vital that we work closely with others in the team. Not only will this increase the chances of success but in my experience an invaluable spin-off is that it opens others eyes to what pharmacists do, and what we can do. Look for grant funding opportunities. Developing new service or workforce models and undertaking good quality research to underpin new models are labourintensive endeavours. Access to funding makes it a lot easier to undertake projects in a systematic and evidence-based way, and helps to avoid the project falling over when staff nd that they dont have time to work on it, which I have seen happen many times. Be persistent and patient. These things rarely happen quickly. My projects have all had long lead times, often with failed attempts to obtain funding. It took us almost 2 years, and three attempts before we were able to get the funding for the MedGap project. Some of my projects have just never got off the ground. Take steps to ensure your new service or care model is generalisable and sustainable. Collaborate with another organisation and/or seek input from people outside your organisation to ensure that what you are doing will have wide applicability. I would like to conclude by acknowledging a few people. I have mentioned Bill Thomson, Roger Nation and Kent Garrett, who supported me and were great role models and mentors. Another person who was an important role model and mentor, especially in my early career, is Graeme Vernon. Associate Professor Michael Woodward, Head of Aged Care, Austin Health has been a great supporter of my aged-care research and I thank him for that. There are many others I have worked and collaborated with who I dont have time to mention individually. However, I would like to thank the pharmacy team at Austin Health for being a great bunch of people to work with. We are lucky to have a culture that supports innovation and quality improvement, where staff are willing and supported to try new ways of doing things, to enhance patient care. And last, but not least, I thank my family for their love and support. Journal of Pharmacy Practice and Research Volume 42, No. 4, 2012. 307 References 1. Morgan TK, Williamson M, Pirotta M, Stewart K, Myers SP, Barnes J. A national census of medicines use: a 24-hour snapshot of Australians aged 50 years and older. Med J Aust 2012; 196: 50-3. 2. Turner CD. Drug use in the elderly: results of a multicentre audit [abstract]. Proceedings of the Conference of the Victorian Branch of The Society of Hospital Pharmacists of Australia; 1992 Nov 1315; Lorne, Victoria. 3. Elliott RA. Reducing medication regimen complexity for older patients prior to discharge from hospital: feasibility and barriers. J Clin Pharm Ther 2012; 37: 637-42. Doi:10.1111/j.1365-2710.2012.01356.x. 4. Elliott RA, Thomson WA. Assessment of a nursing home medication review service provided by hospital-based clinical pharmacists. Aust J Hosp Pharm 1999; 29: 255-60. 5. Elliott RA, Woodward MC, Oborne CA. Quality of prescribing for elderly inpatients at nine hospitals in Victoria, Australia. J Pharm Pract Res 2003; 33: 101-5. 6. Sorensen L, Stokes JA, Purdie DM, Woodward M, Elliott R, Roberts MS. Medication reviews in the community: results of a randomized controlled effectiveness trial. Br J Clin Pharmacol 2004; 58: 648-64. 7. Tran T, Elliott RA, Taylor, SE, Garrett K. Development and evaluation of a hospital pharmacy generated interim residential care medication administration chart. J Pharm Pract Res 2012; 42: 100-5. 8. Elliott RA, Tran T, Taylor SE, Harvey PA, Belfrage MK, Jennings JJ, et al. Impact of a pharmacist-prepared interim residential care medication administration chart on gaps in continuity of medication management after discharge from hospital to residential care: a prospective pre- and postintervention study (MedGap Study). BMJ Open 2012; 2: e000918. 9. Elliott R, Perera D, Garrett K, Woodward M, Szysz A, Marriott J, et al. Improving medication safety for subacute aged care patients through expanded pharmacy assistant (technician) support for clinical pharmacy services. Final report. Adelaide: Health Workforce Australia, Workforce Innovation and Reform: Caring for Older People Program; 2011. 10. Elliott RA, Marriott JL. Review of instruments used in clinical practice to assess patients ability to manage medications. J Pharm Pract Res 2010; 40: 36-42. 11. Elliott RA, Woodward MC. Medication-related problems in patients referred to aged care and memory clinics at a tertiary care hospital. Australas J Ageing 2011; 30: 124-9. 12. Elliott RA, Martinac G, Campbell S, Thorn J, Woodward MC. Pharmacistled medication review to identify medication-related problems in patients referred to an Aged Care Assessment Team: a randomised comparative study. Drugs Aging 2012; 29: 593-605. Rohan Elliott delivered his oration on 2 November 2012 at the 38th SHPA National Conference in Canberra. Australian Clinical Pharmacy Award 2012Jason Roberts The Australian Clinical Pharmacy award has been awarded annually since 1997 to a member of SHPA for outstanding contribution to clinical pharmacy practice. The winner of the Australian Clinical Pharmacy Award 2012 is Jason Roberts, consultant pharmacist at the Royal Brisbane and Womens Hospital where he specialises in intensive care medicine and infectious diseases, and an NHMRC Health Practitioner Research Fellow at the School of Medicine, University of Queensland. Jason is internationally recognised and highly regarded by his peers as an expert in antimicrobial use in the critically ill, having completed his PhD in this eld. Jasons contribution to clinical pharmacy practice is exhibited in his clinical expertise, leadership and commitment to the development of clinical pharmacy practice. Despite still being in the early stage of his pharmacy career, Jason has already demonstrated his high standards of clinical research. He has been extensively published, successfully obtained considerable research grants and is regularly invited to national and international meetings. He is also in demand as a reviewer for peer-reviewed journals and ethics committees. Jason is a highly skilled and well regarded clinical educator. He is also known for his generosity of time and effort towards mentoring and encouraging colleagues junior and senior. Jasons leadership and contribution to his profession have also been evident in his involvement with SHPA. He has held an executive position on the Queensland Branch Committee since 2004 and is currently its chair; Jason Roberts recipient of the Australian Clinical Pharmacy Award 2012. during this time he instigated improved access to CPD for Queensland members. Jason is also a member of two SHPA Committees of Specialty Practice Infectious Diseases and Critical Care. Jasons dedication to clinical pharmacy practice as an educator and researcher make him a worthy recipient of the Australian Clinical Pharmacy Award 2012. Australian Clinical Pharmacy Award Oration Jason Roberts It is with great humility that I accept the Australian Clinical Pharmacy Award. I thank the Queensland Branch for their nomination and the Federal Council for their consideration. I also congratulate the high-quality nominees for this award. Like previous awardees, I stand before you grateful for our professions history and excited about our future. Jason Roberts, BPharm (Hons), BAppSc, PhD, FSHP, Pharmacist Consultant, Royal Brisbane and Womens Hospital, NHMRC Research Fellow, Burns Trauma and Critical Care Research Centre, The University of Queensland, and Adjunct Professor and Clinical DirectorAllied Health, Australian Centre for Health Services Innovation, Queensland University of Technology, Brisbane, Queensland Corresponding author: Dr Jason Roberts, Burns Trauma and Critical Care Research Centre, The University of Queensland, Royal Brisbane and Womens Hospital, Brisbane Qld 4029, Australia. E-mail: j.roberts2@uq.edu.au 308 I would like to tell you my story, about how I moved from being a sciencelaw student and pharmacy assistant, to a pharmacist clinicianscientist. The rst part may be obvious. I worked part-time as a storeman in a pharmacy under a strong Queensland pharmacist, Jacqui McInerney. My father who is also a pharmacist researcher, Professor Michael Roberts from The University of Queensland and University of South Australia helped me get this job and unknowingly I had commenced on my future professional pathway. Very quickly, I realised the value of forward pharmacy and how it can assist patient care. So I left my hometown, Brisbane, and headed to James Cook University where John Doonan and Ian Heslop led a new program of pharmacy education in Townsville. Journal of Pharmacy Practice and Research Volume 42, No. 4, 2012.