Document 10798307
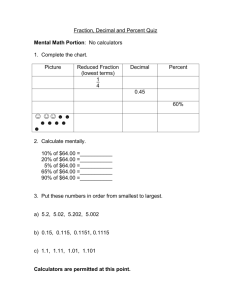
advertisement

Physical & Occupational Therapy in Geriatrics, 29(2):126–135, 2011 C 2011 by Informa Healthcare USA, Inc. Available online at http://informahealthcare.com/potg DOI: 10.3109/02703181.2011.569053 Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. The Effects of the Nintendo Wii Fit on Community-Dwelling Older Adults with Perceived Balance Deficits: A Pilot Study Emily Bainbridge, Sarah Bevans, Brynne Keeley, & Kathryn Oriel Department of Physical Therapy, Lebanon Valley College, Annville, Pennsylvania, USA ABSTRACT. The purpose of this study was to determine if a 6-week intervention program using the Nintendo Wii Fit Balance Board would lead to improvements in balance in community-dwelling older adults over the age of 65 with a perceived balance deficit. Balance, balance confidence, and limits of stability were measured at preintervention and postintervention using the Berg Balance Scale (BBS), Activities-specific Balance Confidence Scale, and the Multi-Directional Reach Test, respectively. The center of pressure excursion was calculated by the Wii Balance Board. The intervention consisted of 30-min sessions, 2×/week using the Balance Board. No statistically significant changes were found for any outcome measure, although 4 of the 6 participants demonstrated clinically significant improvements on the BBS, using established clinical guidelines. These findings suggest that an intervention program including the Wii fit may be an effective rehabilitation option for older adults with perceived balance deficits. KEYWORDS. Nintendo Wii Fit, balance, older adults, fall risk INTRODUCTION According to the 2009 Census Bureau, 12.6% of the United States population is over the age of 64. Of those who are community dwelling, almost one third experiences a fall each year (Centers for Disease Control [CDC], 2005). Fifty-five to sixty percent of those who have fallen are fearful of falling (Howland et al., 1998; Maki, Holliday, & Topper, 1991; Niino, Tsuzuku, Ando, & Shimokata, 2000), while 46% of elderly adults who have never fallen also report a fear of falling (Tinetti, Mendes de Leon, Doucette, & Baker, 1994; Walker & Howland, 1991). This fear of falling may be justified given that falls are one of the leading causes of accidental death in this population (CDC, 2005). While there are many contributing factors to the increased fall risk in older adults (Hughes et al., 2001), impaired balance is a major, Received 2 December 2010; accepted 2 March 2011. Address correspondence to: Dr. Kathryn Oriel, PT, EdD, Department of Physical Therapy, Lebanon Valley College, 101 N. College Avenue, Annville, Pennsylvania 17003, USA (E-mail: oriel@lvc.edu). 126 Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Effects of Nintendo Wii Fit on Older Adults 127 modifiable risk factor that can improve with training (Boyd, Vidoni, & Siengsukon, 2008; Tunney et al., 2003). Historically, interventions for the examination and treatment of balance have included high-cost force plate and virtual reality systems in clinical settings (Gras, Hummer, & Hine, 2009; Shubert, 2010). Recently, owing to its low cost, ease of use, and portability, the Nintendo Wii is being used in physical therapy clinics and skilled nursing facilities as a popular substitute for the expensive and complicated force plates to improve dynamic strength and balance. Despite its growing popularity, the Nintendo Wii’s validity and reliability as an intervention tool is still being investigated. According to Clark et al. (2009), the Wii established excellent test–retest reliability (ICC 0.66) when assessing path length, a measure of deviation from the center of pressure, and demonstrated excellent concurrent validity (ICC 0.77–0.89) when comparing the Wii Balance Board with a laboratory-grade force plate. While the gaming system is commonly used in the clinical setting, little research exists on using the Nintendo Wii Fit as an intervention for improving static and dynamic balance (Bomberger, 2010; Brown, Sugarman, & Burstin, 2009; Pigford & Andrews, 2010; Shih, Shih, & Chiang, 2010; Shih, Shih, & Chu, 2010). Three studies addressed the Wii as a tool to improve balance deficits in older adults (Bomberger, 2010; Brown et al., 2009; Pigford & Andrews, 2010). Brown et al. (2009) described the case of an 86-year-old female following a stroke who used the Wii as part of her rehabilitation program. The patient demonstrated a 10-s improvement in Timed Up and Go, improved anterior–posterior stance symmetry, and a 3-point increase in Berg Balance Score (BBS) with standard physical therapy and four training sessions with the Wii Fit system. A similar case report performed by Pigford and Andrews (2010) with an 87-yearold male with a history of multiple falls showed a 12-point increase in the BBS, a 15-s decrease in Timed Up and Go, a 6% increase in Activities-specific Balance Confidence (ABC) Scale, and a 62% increase in gait speed after 10 sessions of Wii Fit balance games and other therapeutic interventions. Although these case reports described a significant improvement in balance, it is difficult to attribute these changes directly to the Wii Fit since it was not the only intervention performed. A case series by Bomberger (2010) used the Wii Fit balance games as the sole intervention in 14 individuals over 65 years of age with and without balance deficits. Significant improvements in balance between pretesting and posttesting were found in 7 of the 14 outcome measures used. Given the growing trend of virtual reality use in the clinical setting, and its potential importance in improving balance in older adults, the purpose of this pilot study was to investigate the effects of the Nintendo Wii Fit as an intervention in improving balance, balance confidence, and limits of stability in community-dwelling adults over 65 years old. METHOD This study was approved by the institutional review board at Lebanon Valley College. All participants signed an informed consent form prior to the start of the study. 128 Bainbridge et al. Design This prospective, cross-sectional pilot study employed a pretest–posttest design (Jewell, 2008). Participant Recruitment Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Eight participants were recruited through flyers posted in a college sports center in the spring of 2010. In order to participate in the study, individuals had to be community-dwelling older adults over the age of 65 with a perceived decline in balance. Outcome Measures Four outcome measures were used to assess balance, balance confidence, and limits of stability including the BBS, ABC, Multi-Directional Reach Test (MDRT), and center of pressure (COP) excursion measurements. Each test was administered by the same designated examiner with standardized directions. In addition to the balance assessments, all participants completed a health history form. Seated bilateral ankle dorsiflexion passive range of motion measurements with knees flexed and extended were obtained during week 3 of the study secondary to compensatory strategies observed by the researchers. Intervention The intervention consisted of 30-min sessions 2×/week for 6 weeks using the Wii Fit Balance Board. Each treatment session began and ended with 5 min of yoga poses, Half-moon as a warm-up and Warrior as a cooldown [Figures 1(a) and (b)]. Weeks 1–2 included soccer heading, ski jump, ski slalom, and table tilt. Weeks 3–4 included soccer heading, ski slalom, tightrope walk, and table tilt. Weeks 5–6 included penguin slide, ski slalom, tightrope walk, and table tilt. All games were played in the respected order for 5 min per game. Two 1-min seated breaks were allotted at the same time interval in each session. Active training time was measured using a stopwatch to avoid inaccuracy of the Wii timekeeping system. Data Analysis Results were analyzed in IBM SPSS Statistics 17.0 for Windows. The Wilcoxon signed-rank test was used to compare means at pretesting and posttesting for all outcome measures. This nonparametric test was chosen because the parametric assumptions of normality and homogeneity were not met (Jewell, 2008). A significance level of p < 0.05 was established. Results were also compared to established minimal detectable change (MDC) scores for the BBS (Berg, Wood-Dauphine, & Williams, 1995; Stevenson, 2001), ABC (Shumway-Cook, Baldwin, Polissar, & Gruber, 1997), and MDRT (Steffen & Seney, 2008). MDC scores were not available for right and left sidebending and COP excursion. MDC values are used to determine whether change during or after intervention represents meaningful change or are a result of error (Steffen & Seney, 2008). 129 Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Effects of Nintendo Wii Fit on Older Adults FIGURE 1. (a) Ski slolam. (b) Half-moon yoga pose. RESULTS Participant Characteristics Eight participants were initially recruited for this study. The participants in this study, which included 7 females and 1 male, had a mean age of 75 ± 9.7 years. One 130 Bainbridge et al. TABLE 1. Participant Characteristics Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Participant 1 2 3 4 5 6 7 8 Age Gender No. of Prescribed Meds 74 69 68 65 87 87 80 67 M F F F F F F F 1 0 4 8 1 0 3 2 No. of Chronic Health Conditions Assistive Device Falls Within 1 Year 0 2 0 5 3 0 3 2 None None None None SPC None None None None 1 None 5 None None 1 None of the 8 participants used an assistive device, while 2 of the 8 reported a history of falls. Table 1 describes the participant demographics. Of the initial 8 participants, 2 participants withdrew from the study secondary to reports of an exacerbation of preexisting hip osteoarthritis and an increase in preexisting low back pain. Owing to their early withdrawal from the study, these participants were not included in the data analysis. Outcomes Berg Balance Scale Four of the 6 participants improved in the BBS from pretesting to posttesting. These findings were not statistically significant (p = 0.066). The MDC value for the BBS is 5 points (Berg et al., 1995). One participant improved greater than 5 points on the BBS. According to the model established by Shumway-Cook et al. (1997), a 1-point increase in the BBS in individuals with scores between 46 and 54 indicates a 6% decrease in fall risk. Three participants decreased their fall risks by 6%–12%. Activities-specific Balance Confidence Scale Three of the 6 participants improved in the ABC from pretesting to posttesting. These findings were not statistically significant (p = 0.753). None of the participants improved greater than the MDC value for the ABC, which is 18% (Steffen & Seney, 2008). Multi-Directional Reach Test Forward Bending. Three of the 6 participants improved in forward bending from pretesting to posttesting. These findings were not statistically significant (p = 0.588). None of the participants improved by the MDC value for forward bending of the MDRT, a 9-cm change (Lim, van Wegen, & de Goede, 2005; Smithson, Morris, & Iansek, 1998). Backward Bending. Two of the 6 participants improved in backward bending from pretesting to posttesting. These findings were not statistically significant (p = 0.500). None of the participants improved by the MDC value for backward bending of the MDRT, a 7-cm change (Lim et al., 2005; Smithson et al., 1998). Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Effects of Nintendo Wii Fit on Older Adults 131 FIGURE 2. The mean scores of outcome measures at pretesting and posttesting. Right Sidebending. One of the 6 participants improved in right sidebending from pretesting to posttesting. These findings were not statistically significant (p = 0.465). A MDC value does not exist for lateral bending. Left Sidebending. One of the 6 improved in left sidebending from pretesting to posttesting. These findings were not statistically significant (p = 0.465). A MDC value does not exist for lateral bending. COP Excursion Measurement Three of the 6 participants improved in the COP excursion from pretesting to posttesting. These findings were not statistically significant (p = 0.075). There is no MDC value for COP excursion. The mean scores of outcome measures at pretesting and posttesting are displayed in Figure 2, while the Wilcoxon signed-rank test results and p values are displayed in Table 2. DISCUSSION While changes in the BBS scores were not statistically significant from pretesting to posttesting, the results approached significance (p = 0.066). Four of the 6 TABLE 2. Summary of Results Data ABC Berg MDRT forward bending MDRT backward bending MDRT right lateral bending MDRT left lateral bending COP right COP left Wilcoxon Signed-Rank Test Z p −0.314 −1.841 −0.542 −0.674 −0.730 −0.730 −1.782 −1.782 0.753 0.066 0.588 0.500 0.465 0.465 0.075 0.075 Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. 132 Bainbridge et al. participants’ scores demonstrated a decrease in fall risk according to either the MDC value (Berg et al., 1995) or the model established by Shumway-Cook et al. (1997). Five of the 6 participants achieved a posttesting BBS score above the established fall risk cut-off score of 49 (Shumway-Cook et al., 1997). These findings are consistent with the results by Bomberger (2010) who found improvements in the BBS after a 6-week intervention using the Wii Fit. These findings were also consistent with case reports described in the literature (Brown et al., 2009; Clark & Kraemer, 2009; Pigford & Andrews, 2010). The lack of significant BBS improvements may have been due to a ceiling effect on the test, as 4 of the 6 participants’ pretest BBS scores were greater than 49 (Shumway-Cook et al., 1997). Statistical significance was not found with the ABC (p = 0.753), but improvements in balance confidence were noted in 3 of the 6 participants. These findings are similar to the case study results found by Clark and Kraemer (2009) and Pigford and Andrews (2010) who also did not reach MDC values of the ABC with improvements of 2% and 6% respectively. After viewing the pretesting and posttesting ABC scores, it was hypothesized that those participants who decreased in balance confidence may have done so due to recognition of balance limitations that were discovered through the Wii interventions. Cognitive deficits and misunderstandings of the ABC scale may also have led to inaccurate completion of the outcome measures. Statistical significance was not observed with the MDRT in forward bending (p = 0.588), backward bending (p = 0.500), and right and left sidebending (p = 0.465 and 0.465 respectively). Three of the 6 participants improved in forward bending excursion; however, none of the participants met the MDC value of a 9-cm improvement (Lim et al., 2005; Smithson et al., 1998). This is consistent with literature by Brown et al. (2009) whose case study findings reported a forward bending increase by 3 cm after four training sessions with the Wii Fit system accompanied by balance training. Two of the 6 participants improved in backward bending excursion. None of the participants met the MDC value of 7-cm improvement. One participant improved in right sidebending excursion and one in left sidebending excursion. No MDC values exist for lateral bending, although achievement of symmetry is desired (Newton, 2001). One participant achieved equal left and right sidebending symmetry at posttesting. Our results are consistent with Brown et al. who found a 3-cm improvement in right sidebending excursion and a 1-cm improvement in left sidebending excursion. While the COP excursion results were not statistically significant, the results approached significance for left and right COP excursion (p = 0.075 and 0.075 respectively). Three of the 6 participants increased their right and left COP symmetry indicating more equal weight bearing between extremities. Although there is no MDC value for COP excursion, the percentage of weight bearing between extremities should be equal (Nichols, 1997). Throughout the first 3 weeks of the study, researchers observed excessive use of the hip strategy for balance correction (Horak & Nashner, 1986). It was hypothesized that this may be due to decreased ankle dorsiflexion range of motion; therefore, ankle passive range of motion was measured during week 3. These measurements indicated that 4 participants lacked functional bilateral ankle dorsiflexion with knees flexed while 5 lacked functional bilateral dorsiflexion with knees Effects of Nintendo Wii Fit on Older Adults 133 TABLE 3. Dorsiflexion Passive Range of Motion Measurements in Degrees Subjects Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. 1 2 3 4 5 6 Knees Flexed R/L Knees Flexed R/L 8/6 10/13 14/12 4/4 8/12 3/1 2/0 10/13 5/3 −4/−2 2/2 3/0 extended (Root, Orien, & Weed, 1977). These findings are displayed in Table 3. This confirmed our hypothesis that decreased ankle range of motion and absent ankle strategies may have inhibited participant success with the Wii games that require subtle movements more consistent with the ankle strategy. Although this study suggests that the Wii Fit system may be effective in improving balance in older adults, findings should be interpreted within the boundaries of its limitations. The results are limited by the small sample size, which was constrained due to the memory size of the Wii gaming system that only allows 8 participants to be saved. The number of participants was also small due to researchers’ availability, time, and space restrictions. The sample included only one male participant, which also limits the generalizability of results. The results of this study also cannot be isolated to the Wii Fit intervention due to the absence of a control group and the inability to control subject’s physical activity outside of the study. Recommendations for future research include a larger, more representative sample of older adults with more stringent inclusion and exclusion criteria. It is suggested to have a BBS score of less than 48 to prevent a ceiling effect from occurring. A history of falls in the 6 months prior to study initiation may also help to determine the Wii Fit system’s impact on fall risk. To obtain this information, a screening exam may be a useful tool for inclusion in the study. An activity journal is also recommended so that activity outside of the Wii Fit training sessions can be documented. A frequency and duration of 2×/week for 6 weeks was chosen to mimic a typical physical therapy plan of care. A frequency and duration should be considered as this may not be sufficient to improve balance. Also, a greater consistency in games performed by participants during each session should be considered, given that older adults may have deficits in the learning of new motor skills (Boyd et al., 2008; Tunney et al., 2003). CONCLUSION The results of this study suggest that the Wii Fit may be an effective tool for physical therapists to consider when choosing interventions for older adults with balance deficits. While further research is needed, the trends evidenced among our participants indicate that the Wii Fit is a promising, low cost alternative to expensive force plate systems. Declarations of interest: The authors report no declarations of interest. 134 Bainbridge et al. ACKNOWLEDGMENTS The authors wish to acknowledge and thank the following: Lebanon Valley College for providing equipment and space, Alicia Reese and Charissa Nordall for their time and assistance in implementing the interventions, Carol Brashear for her assistance in recruiting and scheduling participants, and all of our participants and their families for their time and effort. Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. ABOUT THE AUTHORS Emily Bainbridge, Sarah Bevans, and Brynne Keeley are doctoral students in the Physical Therapy program at Lebanon Valley College, Annville, Pennsylvania, USA (Note: this study was completed to fulfill requirements for the DPT degree at Lebanon Valley College). Kathryn Oriel, PT, EdD, is an assistant professor in the Department of Physical Therapy at Lebanon Valley College, Annville, Pennsylvania, USA. REFERENCES Berg, K. O., Wood-Dauphine, S., & Williams, J. I. (1995). The Balance Scale: Reliability assessment with elderly residents and patients with an acute stroke. Scandinavian Journal of Rehabilitation Medicine, 27, 27–36. Bomberger, S. A. (2010). The effects of Nintendo Wii Fit on balance of elderly adults. Retrieved March 15, 2010, from William and Mary Digital Archive. http://digitalarchive. wm.edu/bitstream/10288/2018/1/BombergerStephanie2010 Text.pdf Boyd, L. A., Vidoni, E. D., & Siengsukon, C. F. (2008). Multidimensional motor sequence learning is impaired in older but not younger or middle-aged adults. Physical Therapy, 88(3), 351–362. Brown, R., Sugarman, H., & Burstin, A. (2009). Use of the Nintendo Wii Fit for the treatment of balance problems in an elderly patient with stroke: A case report. International Journal of Rehabilitation Research, 32, S109. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2005). Falls among older adults: An overview. Retrieved March 12, 2010, from Web-based Injury Statistics Query and Reporting System (WISQARS). http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html Clark, R., & Kraemer, T. (2009). Clinical use of Nintendo Wii bowling simulation to decrease fall risk in an elderly resident of a nursing home: A case report. Journal of Geriatric Physical Therapy, 32(4), 174–180. Clark, R. A., Bryant, A. L., Pua, Y., McCrory, P., Bennell, K., & Hunt, M. (2009). Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait and Posture, 31, 307–310. Gras, L. Z., Hummer, A. D., & Hine, E. R. (2009). Reliability and validity of the Nintendo Wii Fit. Journal of CyberTherapy and Rehabilitation, 2(4), 329–336. Horak, F. B., & Nashner, L. M. (1986). Central programming of postural movements: Adaptation to altered support surface configurations. Journal of Neurophysiology, 55, 1369–1381. Howland, J., Lachman, M. E., Peterson, E. W., Cote, J., Kasten, L., & Jette, A. (1998).Covariates of fear of falling and associated activity curtailment. Gerontologist, 38, 549–555. Hughes, V. A., Frontera, W. R., Wood, M., Evans, W. J., Dallal, G. E., Roubenoff, R., et al. (2001). Longitudinal muscle strength changes in older adults: Influences of muscle mass, physical activity, and health. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56(6), B209–B217. Phys Occup Ther Geriatr Downloaded from informahealthcare.com by University of Delaware on 10/04/12 For personal use only. Effects of Nintendo Wii Fit on Older Adults 135 Jewell, D. V. (2008). Guide to evidence-based physical therapy practice (pp. 97–100, 206–218). Sudbury, MA: Jones and Bartlett. Lim, L., van Wegen, E., de Goede, C., Jones, C. J., Rochester, D., Hetherington, L., et al. (2005). Measuring gait and gait-related activities in Parkinson’s patients’ own home environment: A reliability, responsiveness, and feasibility study. Parkinsonism & Related Disorders, 11, 19–24. Maki, B. E., Holliday, P. J., & Topper, A. K. (1991). Fear of falling and postural performance in the elderly. Journal of Gerontology, 46, M123–M131. Newton, R. A. (2001).Validity of the Multi-directional Reach Test: A practical measure for limits of stability in older adults. Journal of Gerontology: Medical Sciences, 56(4), M248- M252. Nichols, D. S. (1997). Balance retraining after stroke using force platform biofeedback. PhysicalTherapy, 77(5), 553–558. Niino, N., Tsuzuku, A. F., & Shimokata, H. (2000). Frequencies and circumstances of falls in the National Institute for Longevity Sciences, Longitudinal Study of Aging (NILS-LSA). Journal of Epidemiology, 10, S90–S94. Pigford, T., & Andrews, A. W. (2010). Feasibility and benefit of using the Nintendo Wii Fit for balance rehabilitation in an elderly patient experiencing recurrent falls. Journal of Student Physical Therapy Research, 2(1), 12–20. Root, M. L., Orien, W. P., & Weed, J. H. (1997). Normal and abnormal function of the foot (Vol. 2, pp. 37–38, 41). Los Angeles, CA: Clinical Biomechanics Corp. Shih, C. H., Shih, C. T., & Chiang, M. S. (2010). A new standing posture detector to enable people with multiple disabilities to control environmental stimulation by changing their standing posture through a commercial Wii Balance Board. Research in Developmental Disabilities, 31, 281–286. Shih, C. H., Shih, C. T., & Chu, C. L. (2010). Assisting people with multiple disabilities actively correct abnormal standing posture with a Nintendo Wii Balance Board through controlling environmental stimulation. Research in Developmental Disabilities, 31(4), 936–942. Shubert, T. (2010). The use of commercial health video games to promote physical activity in older adults. Annals of Long Term Care: American Geriatric Society, 18(5), 27–32. Shumway-Cook, A., Baldwin, M., Polissar, N. L., & Gruber, W. (1997). Predicting the probability for falls in community-dwelling older adults. Physical Therapy, 77(8), 812–819. Smithson, F., Morris, M. E., & Iansek, R. (1998). Performance on clinical test of balance in Parkinson’s disease. Physical Therapy, 78, 577–592. Steffen, T., & Seney, M. (2008). Test–retest reliability and minimal detectable change on balance and ambulation tests, the 36-item Short-form Health Survey, and the Unified Parkinson Disease Rating Scale in people with Parkinsonism. Physical Therapy, 88, 733–746. Stevenson, T. J. (2001). Detecting change in patients with stroke using the Berg Balance Scale. Australian Journal of Physiotherapy, 47, 29–38. Tinetti, M. E., Mendes de Leon, C. F., Doucette, J. T., & Baker, D. I. (1994). Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. Journal of Gerontology: Medical Sciences, 49A, M140–M147. Tunney, N., Taylor, L. F., Gaddy, M., Rosenfeld, A., Pearce, N., Tamanini, J., et al. (2003). Aging and motor learning of a functional motor task. Physical & Occupational Therapy in Geriatrics, 21(3), 1–16. US Census Bureau. (2009). United States fact sheet. Retrieved September 27, 2010, from 2006– 2008 American Community Survey. http://factfinder.census.gov/servlet/ACSSAFFFacts? event=&geo id=01000US& geoContext=01000US& street=& county=& cityTown=& state=& zip=& lang=en& sse=on&ActiveGeoDiv=& useEV=&pctxt=fph&pgsl=010& R =null%3Anull submenuId = factsheet 1 & ds name = null & ci nbr = null & qr name = null & keyword=& industry= Walker, J. E., & Howland, J. (1991). Falls and fear of falling among elderly persons living in the community: Occupational therapy interventions. American Journal of Occupational Therapy, 45, 119–122.