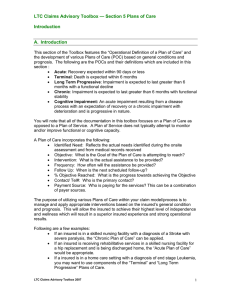
LTC Claims Advisory Toolbox — Section 4 Plans... Chronic Conditions A. Chronic Condition Defined
advertisement

LTC Claims Advisory Toolbox — Section 4 Plans of Care Chronic Conditions A. Chronic Condition Defined A1. A chronic condition is an impairment that is expected to last greater than 6 months. Functional status is stable and progressive decline is not expected in the next 6 months. Examples of diagnoses that fall into the category of Chronic Conditions are cerebral vascular accidents or strokes, coronary artery disease, chronic obstructive pulmonary disease, or spinal stenosis. B1. First consideration is what recent event occurred that caused the insured to develop functional impairment. Often insureds with a chronic condition will initiate a claim due to an acute condition related to the underlying chronic disease. This acute condition has placed them in a weakened state and may have caused some changes in their ability to perform activities of daily living. Examples of this scenario are an insured with coronary artery disease who is hospitalized with congestive heart failure, or a diabetic who is hospitalized due to diabetic coma. These insureds coming on claim would initially have an Acute POC in place to help them regain their pre-morbid level of independent functioning. However there will be claims when the insured will not be able to achieve their prior level of independence or the caregiver can no longer provide the care the insured requires. For these claims the insurer would look to transition the insured from an Acute POC to a Chronic POC with a long term focus. Another reason an insured with a Chronic Condition would come on claim is that co morbid conditions combined with their chronic disease has brought them to a point of were managing ADLs independently is a problem. The chronic disease is stable and physical deterioration related to the disease is not anticipated in the next 6 months. A third reason is the primary care giver is no longer willing or able to care for the insured who has required assistance with activities of daily living prior to filing for benefits. B2. Consider establishing a Chronic POC after all avenues of improvement in condition have been explored through referrals to physical and occupational therapy or a short term stay in a rehabilitation or skilled nursing facility. B3. Conditions that are not stable and are expected to decline in the next six months, should have a Progressive Condition POC developed. B4. Functional and ADL Status should be verified with PCP LTC Claims Advisory Toolbox 2007 1 LTC Claims Advisory Toolbox — Section 4 Plans of Care Chronic Conditions C. Assessment C1. If an Acute POC was in place initially, determine if the highest level of function has been reached. If it is time to transition to a Chronic POC the transition should begin by obtaining another On-Site Assessment (OSA) to establish the insured’s current ADL status, as well as other key findings routinely obtained in the OSA. C2. Review medical records from the treating physician(s), physical and occupational therapist, and rehabilitation or skilled nursing facility as appropriate. These reviews will provide valuable information in assessing insureds with chronic conditions and provide insight into care plan needs. D. Activities of Daily Living D1. Identify what assistive devices and/or home modifications might increase the ability of the insured and their primary caregiver to care for him/her. Providing the insured with some means to participate actively in their self care will promote a sense of well being and may result in requiring a reduction in service levels required to meet their needs. D2. Identify which ADLs insured needs help with and determine: • What type of assistance is required (hands on, cueing, standby)? • How often the assistance is needed and who will provide the assistance e.g. formal or informal caregivers, family etc? • Determine the reasonable amount of time required to complete tasks to meet the insured’s ADL needs. Factor in primary caregiver’s availability to provide ADL assistance throughout the day. E. Instrumental Activities of Daily Living E1. Identify which IADLs the insured needs help with and determine: • Who routinely provided the IADL assistance if other then the insured and is that person still providing assistance? • How often is the assistance needed? • What community resources are available to support the insured’s needs? • Factor in primary caregiver’s availability to provide IADL assistance throughout the day. LTC Claims Advisory Toolbox 2007 2 LTC Claims Advisory Toolbox — Section 4 Plans of Care Chronic Conditions F. Establish and Implement POC F1. Review needs and limitations: • ADL - In planning for ADL needs the challenge is to assist with the insured’s functional limitations while maintaining the greatest level of independence possible. This can be done through such actions as obtaining DME and providing training on its use or referrals to physical and occupational therapy. Also important is in establishing a POC is coordinating care needs and services provided by informal caregivers and community services with formal care provided through the policy’s benefits. And then there’s maximizing, when appropriate, Medicare allowable benefits to augment incurred costs associated with providing services noted in the POC. • Cognitive – If cognition is a problem but does not trigger the LTC policy benefit it is important to accommodate for the challenges this will bring in order to maintain the highest level of function while maintaining safety • IADLS- A cost effective plan is put in place to meet these needs through use of community resources, family, and informal services such as church, neighbors, etc. • Environmental – Review current living arrangements, safety, obtaining equipment or make modifications to the environment so that the insured has the tools to maintain the highest level of independence. • Psychosocial – Identify support systems, family, informal care, services provided by external sources that have been available to the insured and can be used to augment the Chronic POC. F2. Implement a Plan of Care that allows the highest level of Independence: • Maintain highest level of independence while meeting the functional ADL, Cognitive, IADL, Environmental and Psychosocial needs. • Maintain current functional status while maintaining safety. • POC should address respite for informal caregivers. • If DME is identified in OSA that would increase level of function address obtaining and training on its use in the POC. • Facilitate contact with community resources used to augment the POC. G. Home Health Care Considerations G1. A POC should be developed with the insured’s and family wishes known. Usually the goal is to stay home as long as able. • POC should address all needs and services that are required to keep insured at home. • Carrier should communicate POC with MD. LTC Claims Advisory Toolbox 2007 3 LTC Claims Advisory Toolbox — Section 4 Plans of Care Chronic Conditions • • • Duration and frequency of services should be identified on POC. Due to the importance of maintaining stability of a chronic condition follow up should be as follows: • If POC is developed following an Acute POC follow up every 90 days until POC is in a maintenance mode then every 6-12 months. • If this is a new claim follow up every 30 days for 90 days then follow up every 90 days until POC is in a maintenance mode then every 6-12 months. Follow up on POC should include review of services provided and if they continue to be appropriate given current needs/limitations. • Verify needs and limitations with HHC benefits through review of ADL notes, any clinical records related to recent care received, and PT/OT records H. Facility Considerations H1. Is facility equipped to meet the needs of the Insured? • Review facility records and verify the facility provides the services insured needs and that policy is triggered. • ALF services would be outlined in assessment, service plans and/or plan of care. • Skilled nursing facility assessment and POC are outlined in the medical data set (MDS) utilized by Medicare certified facilities or, if not certified by the facility’s care planning as found in the facility’s medical record. • Follow up with the facility could be in 90 days, then in six months and then annually to verify needs are met. LTC Claims Advisory Toolbox 2007 4