Document 10591525
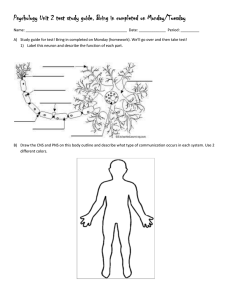
advertisement

REGULATION OF PITUITARY FUNCTION BY la,25-DIHYDROXYVITAMIN D3 by Stanley David Rose B.A. Cornell University (1978) Submitted to the Department of Applied Biological Sciences in Partial Fulfillment of the Requirements of the Degree of DOCTOR OF PHILOSOPHY at the MASSACHUSETTS INSTITUTE OF TECHNOLOGY June 1985 ( Massachusetts Institute of Technology 1985 Signature redacted Signature of Autho r Desartment of Applied Biological Sciences May 3, 1985 This doctoral thesis has been examined by a Committ Applied Biological Sciences as follows:A 'of the Department of Signature redacted Dr. A. North Signature redacted Chairman Dr. M.F. Holick Thesis Supervisor Signature redacted Dr. H. Munro Signature redacted Dr. R. Franceschi Signature redacted Dr. S. Nussbaum Accepted by Signature redacted ;.SA,"HUSFTT3 OFTCNNLOWVn R. MAY 3 11985 Archives Tannenbaum, Chairman, Commi-tee on Graduate Students REGULATION OF PITUITARY FUNCTION BY la,25-DIHYDROXYVITAMIN D3 by STANLEY DAVID ROSE Submitted to the Department of Applied Biological Sciences on May 3, 1985 in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in Neural and Endocrine Regulation ABSTRACT A specific pituitary binding protein for la,25-dihydroxyvitamin D3 (1,25-(OH) 2 D 3 ) has recently been identified and characterized in several species. The physical characteristics of this binding protein indicate that it is similar, if not identical, to the receptor for 1,25-(OH) 2 D3 present in rat intestinal cells. This protein has also been detected in several strains of clonal rat pituitary tumor cells. Although biological responses have been observed in cultures of these transformed rat pituitary cells following administration of 1,25-(OH)2D3, no attempt has been made to determine whether the binding protein present in normal pituitary cells functions as a true receptor. In addition, there is data which suggests that the responses detected in the transformed pituitary cells may be artifactual. . The presence of a 3.5-3.7 S specific binding protein for 1,25-(OH) 2 D3 in both cytosolic and nuclear extracts of rat anterior pituitary was confirmed. The dissociation constant (Kd) for the binding of 1,25-(OH)2D3 to this protein was determined to be 6.0 x 10-10M, with a Bmax of approximately 36 fmol/mg protein. The effects of 1,25-(OH) 2 D 3 on various parameters of the function of non-transformed pituitary cells was examined in primary cultures of enzymatically dispersed rat anterior pituitary cells. These cells in culture were demonstrated to retain both viability and functionality over the time course employed for studies on the effects of 1,25-(OH) D 3 No effects of 1,25-(OH)2D3 were observed on the growth of these cells 2 (in terms of DNA content, protein content, or gross cellular morphology), regardless of the time of the test incubation period, or the dose of 1,25-(OH) 2 D3 used. No sustained significant effects of 1,25-(OH) 2 D 3 were observed on either secretion or synthesis of prolactin. Both secretion and synthesis of thyrotropin, however, were stimulated by treatment with 1,25-(OH) 2 D 3. These observations represent the first demonstration that the specific binding protein for 1,25-(OH) 2 D3 in rat anterior pituitary functions as a receptor, in the classical pharmacological sense. In addition, they are consistent with previous reports in the literature indicative of a biologically significant relationship between the vitamin D and thyrotropin/thyroid hormone endocrine systems. Finally, these results suggest that events which occur in tumor cells (in this case, alterations in prolactin secretion induced by 1,25-(OH) 2 D3 ) may not always mimic the situation observed in their non-transformed counterparts. Thesis Supervisor: Dr. Michael F. Holick, Associate Professor of Nutritional Biochemistry and Endocrinology 2 ACKNOWLEDGEMENTS The contributions of the following individuals and insititutions to this thesis warrant acknowledgement: Dr. Michael F. Holick, for introducing me to vitamin D, for his constant support and guidance, for the respect and independence he gave me, and most of all for the fine example he set for an aspiring scientist; Dr. Alan North, Dr. Sam Nussbaum, Dr. Rene Franceschi, and Dr. Hamish Munro, for their guidance and advice as members of my thesis committee; The NIDA and the NIMH, for granting me the fellowships which enabled me to pursue my doctorate at M.I.T.; The NIADDK, for supplying me with the materials required for the radioimmunoassays I performed; Dr. Fukase, for kindly taking the time to teach me how to grow cells in culture; On a more personal level, I especially thank: Elise, for being with me throughout, and for enhancing my work and my life in countless ways; Dad and Betty, Mom and Jack, Diane and her family, and Audrey, for their constant love and support, and for the lessons they've taught me about life and how to live it; Howard, Brian, and Christina, for being the best friends a person could desire; Maxwell and Nicole, for always being there when I needed them; and My friends at the Muddy Charles Pub, for the intermittent relief they provided from an otherwise grueling pace. 'The object of war is to survive it.' Which struck me as the object of graduate school... Such comparisons struck me hard in those days. - John Irving - Lawrence Berra "It ain't over till it's over." 3 DEDICATION To Elise, for all she's given me. 5 4 TABLE OF CONTENTS page Title Page ........... 1 Abstract .......................... 2 ........... 0 0 Acknowledgements Dedication ........................ ............... ....... 0 ....... * Table of Contents ................. List of Figures ................... ....... 0 ....... 0 ....... 0 List of Tables .................... ...... 0 Introduction ........*0*.. . Literature Survey Metabolism of Vitamin D ...... Function of 1,25-(OH) 2 D3 ----Mechanism of Action .......... Parathyroid Gland as a Target for 1,25-(O)2D3 .................. la-Hydroxylase ..................... . . . . . . . . . . . . . Effects of Anterior Pituitary Hormones on the Renal Pituitary Gland as a Target for 1,25-(OH)2D3 -------------------- Materials and Methods ................. .. . .. .. .. . .. .. . Rationale and Specific Aims ...... Drugs and Chemicals ............................................ Animals ......................................................... Dissection of Rat Anterior Pituitary for Use in Binding Studies Preparation of Cytosolic and Nuclear Extracts of Rat Anterior Pituitary ..................................................... 5 page Sucrose Density Gradient Sedimentation Analysis ................. 46 Determination of Binding Characteristics ........................ 47 Rat Anterior Pituitary Cell Culture ........................... 48 Determination of Cell Number and Viability ..................... 50 Cell Photography .............................................. 51 Determination of Cellular Protein Content ....................... 51 Determination of Cellular DNA Content ........................... 51 Radioimmunoassay for Rat Prolactin .............................. 52 Iodination of rTSH for Use in Radioimmunoassay .................. 55 Radioimmunoassay for Rat Thyroid Stimulating Hormone 60 Double Antibody Immunoprecipitation of ............ 35 s-Methionine Labelled rTSH ............................................... Gel Electrophoresis of Immunoprecipitated Labelled rTSH ..... .. .. .... Double Antibody Immunoprecipitation of Labelled rPRL ......... 62 35 S-Methionine . . .. . . . . .. .. 64 35 S-Methionine . ... ....... .... ........ .. .. .. . 66 Trichloroacetic Acid Precipitation of Proteins .................. Sta t ist ics ...................................................... Results ................ *...........*.. 67 0000000006 7 .................. * 69 Detection of Specific Binding Protein for 1,25-(OH) 2 D 3 in Rat Anterior Pituitary .....000...0000000000............ 69 Determination of Binding Characteristics ........................ 71 Recovery of Viable Cells in Culture ............................. 73 .Viability and Functionality of Cells in Culture 76 6 ................. page Effects of TRH on Secretion of TSH ... .................... 78 Effects of 1,25-(OH)2D3 on the Growth of Rat Anterior Pituitary Cells in Primary Culture ............................ 83 Effects of 1,25-(OH) 2 D3 on Content of rPRL in Cells and in Media ...................................................... 87 Effects of 1,25-(OH)2D3 on Content of rTSH in Cells and in Media .. . . . . . . . . . . . . . . . . . . . . . . . . .. Effects of 1,25-(OH) 2 D3 on Synthesis of rTSH .................... 98 109 . Discussion 88 Summary and Conclusions .......................................... 116 116 Conclusions ................ 119 Suggestions for Future Research ................................ . Summary of Results References ... 121 . .... ................................ .... .. 120 141 Biographical Note........................... 7 LIST OF FIGURES Number Title Page 1. Structures of the D Vitamins ................................. 12 2. Typical Standard Curve for Rat Prolactin Radioimmunoassay 0... 56 3. Sephadex G-50 Gel Chromatographic Purification of Radioiodinated Rat Thyroid Stimulating Hormone 4. ............. Typical Standard Curve for Rat Thyroid Stimulating Hormone Radioimmunoassay ........................................... 5. 59 63 Sucrose Density Gradient Sedimentation Analysis of Rat Anterior Pituitary Cytosolic and Nuclear Extracts 6. 3 H-1,25-(OH)2D3 -.- 00.------ Competitive Binding Assay Employing 70 ...--.-------0 3 H-1,25-(OH) 2 D3 , Incubated with 1,25-(OH) 2 D3, and Rat Anterior Pituitary Cytosol ........... 72 7. Scatchard Analysis of Binding Data ........................... 74 8. Photograph of Cells in Culture 1 Hour Subsequent to Seeding .. 75 9. Basal Secretion of Rat Prolactin from Enzymatically Dispersed Rat Anterior Pituitary Cells in Primary Culture .. 77 10. Effects of Increased Media Potassium Concentration on rPRL Secretion ..... 11. *..................................... 79 Effect of Increased Media Potassium Concentration on rTSH Secretion ................................................. 80 12. Effects of TRH on Secretion of TSH .......................... 81 13. Effects of 1,25-(OH)2D3 on Cellular Protein Content ......... 84 14.- Effects of 1,25-(OH) 2D3 on Cellular DNA Content .............. 85 8 Title Number 15. Effects of 1,25-(OH)2D3 on Gross Cellular Morphology ......... 16. Effects of 1,25-(OH)2 D3 on Cellular rPRL Content (ng/ug protein) ............................................ 17. 95 96 Effects of 1,25-(OH)2D3 on Media rTSH Content (% control) ................................................ 24. 94 Effects of 1,25-(OH) 2 D 3 on Media rTSH Content (ng/ug protein) ............................................ 23. 92 Effects of 1,25-(OH)2D3 on Cellular rTSH Content (% control) ............................................. 22. 91 Effects of 1,25-(OH)2D3 on Cellular rTSH Content (ng/ug protein) ............................................ 21. 90 Effects of 1,25-(OH) 2 D3 on Media rPRL Content (% control) ................................................ 20. 89 Effects of 1,25-(OH) 2 D 3 on Media rPRL Content (ng/ug protein) ............................................ 19. 86 Effects of 1,25-(OH)2D3 on Cellular rPRL Content (% control) ................................................ 18. Page 97 Effects of 48 Hour Treatment with Various Doses of 1,25-(OH)2D3 on Media rTSH Content ........................ 99 25. Effects of 1a,25-(OH) 2 D 3 on Media and Cellular rTSH Content .. 100 26. Gel Electrophoresis of Immunoprecipitated 3 5 S-Methionine-Labelled 27. rTSH ............................... 103 Effects of 10,25-(0H) 2D3 on Incorporation of 3 5 S-Methionine Into Newly Synthesized Immunoprecipitatable rTSH .................................. 108 9 LIST OF TABLES 1. Page Title Number Sedimentation Coefficients of Well-Characterized Proteins Which Specifically Bind 1,25-(OH)2D3 2. 18 Physical Characteristics of Specific Pituitary Binding Sites Detected for 1,25-(OH)2 D3 3. 26 Physical Characteristics of Specific Binding Sites for 1,25-(OH)2D3 Detected in Clonal Pituitary Tumor Cells 29 4. Effects of TRH on Secretion of TSH ............................ 5. Effects of 1,25-(OH)2 D3 on Incorporation of 35 S-Methionine into Newly Synthesized Immunoprecipitatable rTSH 6. .... .............. Effects of 1,25-(OH)2D3 on Incorporation of 102 Effects of 1,25-(OH) 2 D3 on Incorporation of 106 35 S-Methionine into Newly Synthesized TCA-Precipitatable Proteins 10 104 35 S-Methionine into Newly Synthesized Immunoprecipitatable rPRL 8. . Recovery of Counts Added to Gel Following Electrophoresis of 35 S-Methionine-Labelled-rTSH ........... 7. 82 107 LITERATURE SURVEY Introduction The history of vitamin D can be traced back to ancient tales of- bony diseases which may have been due to vitamin D deficiency (1). During the 20th century, from the first assignment of a scientific basis to rickets (2,3), to the eventual demonstration of la,25-dihydroxyvitamin D 3 (1,25-(OH)2D3) as the active hormonal form of vitamin D3 (4,5), consistent progress has been made in elucidating the nature of the vitamin D endocrine system (6-18). As a consequence of this work, and due to the fortification of milk with vitamin D, nutritional rickets and osteomalacia have been virtually eliminated as public health problems in the United States and other complying countries. Metabolism of Vitamin D An important concept in the study of this endocrine system is that there is not a single vitamin D. There exists a family of compounds which exhibit vitamin D activity (see fig.1). The most important of these are vitamin D 2 and vitamin D3 . Vitamin D2 is produced via ultraviolet irradiation of ergosterol (pro-D 2 ), a fungal sterol. Vitamin D3 is produced in skin via ultraviolet irradiation of 7-dehydrocholesterol (pro-D 3 )(19). Pre-vitamin D2 and pre-vitamin D3 are first produced, following photolysis of their respective 5,7-diene sterol precursors (ergosterol and 7-dehydrocholesterol). The pre-vitamin Ds then exist in thermal equilibrium with their respective forms of vi-tamin D (D2 and D3). When consumed in the diet, both forms of vitamin D may be absorbed in the intestine (20-22). 11 Being fat soluble, they are most .N CN 12 C D 1 14 1 N 5 CN2 A D, N H CHI CN2 N 0' N 0e 0O D5 Figure 1. CMN CMH Structures of the D vitamins 12 CHZCHS likely absorbed with other neutral lipids, and thus appear in the lymphatic system as chylomicrons (23,24). Although vitamin D is viewed as an essential dietary factor, the production of vitamin D3 (D3; also known as cholecalciferol) in the skin (following exposure to ultraviolet radiation) requires that it be regarded as a pro-hormone rather than as a vitamin. The majority of vitamin D present in blood is transported bound to a specific a-globulin (24-27). Vitamin D is rapidly taken up by the liver (20,21,23,28, 34), but is not stored specifically in this organ. It appears that the major storage site for vitamin D is actually in the fat depots (30). In the liver, vitamin D is hydroxylated at the 25-C position by specific microsomal enzymes (29,31-33), yielding 25-hydroxyvitamin D (25-OH-D). 25-hydroxylated form of vitamin D3 (25-OH-D3) D3 (34,35). The is 2-5 times more active than Despite this increased activity, it is now clear that 25-OH-D3 is inactive at physiological concentrations, and is not the hormonal form of vitamin D (36-38). 25-OH-D produced in the liver is transported in blood bound to the same vitamin D-transport protein described above, and is the major circulating form of vitamin D (39-41). Although several routes of metabolism have been described for 25-OH-D3, the path of major interest to this thesis involves the formation of 1,25-(OH) 2 D3. la-Hydroxylation of 25-OH-D3 occurs primarily in the kidney (42-44), via the action of a mitochondrial 25-OH-D3-la-hydroxylase (42,49). The placenta has also been reported to possess la-hydroxylase activity (45-48). This dihydroxylated form of cholecalciferol is now recognized as the hormonal 13 form of vitamin D3 (37,51-53). 1,25-(OH)2D3 is transported to target tissues bound to the same vitamin D-transport protein described above. The renal la-hydroxylase has been studied extensively (54-57). Parathyroid honnone (PTH) is the most potent known stimulator of this enzyme (58-62). Low plasma phosphorous concentration is also a major signal for its activation 0 (63,64). The role of calcium as a direct stimulator of this enzyme is unclear, as decreases in plasma calcium concentration lead to increased secretion of PTH. 0 However, there is some evidence indicating that decreased plasma calcium concentration may be a direct signal for activation of the renal la-hydroxylase, independent of PTH (65-67). I There is also evidence suggesting a role for growth hormone (GH) and prolactin (PRL) in the regulation of 25-OH-D3-la-hydroxylase activity. The studies examining effects of these hormones will be described in detail in a separate section below. Estrogens (68,69) and thyroxine (70,71) have also been reported to influence the activity of this renal hydroxylase. * Finally, 1,25-(OH) 2 D3 appears to exert direct negative feedback effects on 2 5 -OH-D3-la-hydroxylase, - in addition to stimulating 24-hydroxylation of 25-OH-D 3 (72). Side-chain cleavage to form calcitroic acid appears to be the major route of inactivation of 1,25-(OH)2D3 (73,74). t However, additional hydroxylations also yield less active metabolites of vitamin D 3 (75-78). All of these vitamin D metabolites eventually appear in the bile and feces (79). The The half life of 1,25-(OH) 2 D3 in plasma has been estimated at between 2 and 6 hours (80). 14 Function of 1,25-(OH)2D3 In a broad sense, the most well-characterized function of 1,25-(OH) 2D3 is to maintain plasma calcium and phosphorous at levels sufficient to support the physiological processes for which they are required. Acting alone, and in conjunction with other hormones, 1,25-(OH) 2 D3 initiates responses at a variety of target tissues. The common factor in all of these actions of 1,25-(OH)2D3 is that they lead to a maintainance of calcium and phosphorous homeostasi s. 1,25-(OH)2D3, via a variety of mechanisms, functions to maintain plasma calcium and phosphorous at levels that support normal mineralization of bone (76,81,82). It is the only known hormone to stimulate active intestinal calcium absorption (83). In addition, 1,25-(OH)2D3 stimulates active intestinal transport of phosphate (76). As dietary intake of calcium varies considerably, intestinal absorption may not always provide sufficient amounts of calcium to support another of its major roles, namely neuromuscular function. In order to maintain normal neuromuscular function, calcium may be mobilized from bone, which acts as a virtual reservoir of this mineral. This mobilization is primarily under the control of PTH, working in concert with 1,25-(OH)2D3 (76). 1,25-(OH) 2 D 3 also acts in the distal renal tubule, again in conjunction with PTH, to cause reabsorption of calcium (76). The kidney normally reabsorbs 99% of the filtered load of calcium, but the residual 1% is under the control of these two hormones. Vitamin D deficiency may produce a variety of clinical disorders. young, growing, terrestrial vertebrate, rickets will ensue. In the In this disease, the collagen fibrils fail to mineralize, the bones become soft, and the stress of weight and muscle operation causes overt structural deformities. 15 Ultimately, death occurs as a result of impairment of internal organ function by the collapse of the bones which protect the internal viscera (76,84). In adults, when normal bone is constantly being remodeled, osteomalacia will result from vitamin D deficiency. In this disease, the entire remodelling process is slowed down, with the mineralization of new organic matrix elaborated by osteoblasts being particularly affected (85). Finally, in the absence of sufficient amounts of extracellular calcium, neuromuscular function will be affected (76,82). A convulsive state of hypocalcemic tetany will be produced, leading to death. In reviewing the current literature concerning 1,25-(OH) 2 -D3, it has become clear that there is yet another important function of this seco-sterol. Although the conception of 1,25-(OH)2-D3 as a calcium homeostatic hormone has been amply justified, several recent reports have provided evidence supporting a more basic biological role for this hormone. These experiments have examined the effects of 1,25-(OH)2-D3 on the replication and differentiation of a variety of cells which possess the classical receptor for this hormone. The reports indicate that 1,25-(OH)2-D3 has potent effects on cell replication and differentiation. These effects have been observed in both normal and transformed receptor-positive cells, including fibroblasts, intestinal cells, bone marrow cells, mammary cancer cells, monocytes, melanoma cells, and ovarian cells (186-196). In most of these studies, the data demonstrates an inhibition of cell proliferation, and a concommitant stimulation of differentiation. The possibility that 1,25-(OH)2-D3 acts as one of many circulating factors which influence the maturation of specific cell types is of major biological significance. It may also provide an explanation as to the 16 relevance of a specific receptor for 1,25-(OH)2-D3 existing in such a wide array of cell types. Mechanism of Action The only significant work performed to date on the mechanism of action of 1,25-(OH)2D3 has been in relation to the hormone's effects on intestinal calcium absorption. Given the structural similarity of vitamin D to steroid hormones, it has been assumed that 1,25-(OH)2D3 might function in a manner similar to the mechanism proposed for steroid action (86). This would involve association with a cytoplasmic receptor, translocation to the nucleus, alteration of transcription of mRNA, and subsequent alteration in the synthesis of specific proteins. Several proteins have been described which specifically bind 1,25-(OH)2D3 (see table 1). The 4.1 S protein is the plasma transport protein for vitamin D and its metabolites, displaying highest affinity for 25-OH-D. The 6.0 S cytosolic protein has been isolated from a large number of tissues (41), and appears to be specific for 25-OH-D (87). Furthermore, this 6.0 S protein is not found in cytosol preparations isolated free of plasma protein (88). It now appears that this 6.0 S cytosolic binding protein is an artifactual product resulting from the interaction of the 4.1 S plasma transport protein and an unidentified nonspecific cytosolic protein (88). The 3.7 S protein isolated from rachitic chick cytosol, and the 3.2 S protein obtained from rat cytosol, appear to be highly specific for 1,25-(OH)2D3 (87,89,90). It is currently believed that the 3.7 S protein is the cytosolic receptor responsible for initiating the effects of 1,25-(OH) 2 D3 on chick intestinal calcium transport. The theory is that 1,25-(OH) 2D3, being transported on 17 Source Sucrose Density Gradient Sedimentation Coefficient 3.7 S chick intestinal cytosol rat intestinal cytosol 3.2-3.3 S rat plasma 4.0-4.1 S rat intestinal cytosol 5.8-6.0 S Table 1. Sedimentation coefficients of well-characterized proteins which specifically bind 1,25-(OH)qDi 18 the 4.1 S plasma protein, is somehow transferred to the villus cell. There is currently no evidence that 1,25-(OH)2D3 is actively transported across the cell membrane. Once inside the cell, 1,25-(OH) 2 D3 binds to the 3.7 S cytosolic protein. This modified receptor then enters the nucleus, interacting with the nuclear chromatin in an unknown fashion. The result is transcription of specific genes that code for the vitamin D-dependent calcium binding protein (91-96). Although synthesis of other proteins may also be induced by 1,25-(OH) 2 D3 , this has yet to be demonstrated. Furthermore, while the vitamin D-dependent calcium binding protein is induced by 1,25-(OH) 2 D3 (97), and its presence has been correlated with active intestinal calcium absorption, its exact role in calcium transport remains unclear (98). Thus, the effect of 1,25-(OH)2D3 on intestinal calcium absorption appears to be due, at least in part, to a nuclear mechanism; The dissociation constant for 1,25-(OH) 2 D3 and the 3.7 S binding protein is 5 x 10-11 M. This binding protein is not found in non-target tissues such as smooth muscle, skeletal muscle, and liver. However, it has been found in tissues previously not considered to be targets for 1,25-(OH) 2 D3, such as skin, parathyroid glands, stomach mucosa, pituitary glands, and mammary glands (99). Recent evidence suggests that 1,25-(OH)2D3 may also cause increased intestinal calcium absorption via a mechanism which does not involve de novo protein synthesis (100,101). In these reports, the primary effect of the sterol was thought to be a modification of membrane phospholipids, leading to an I increased permeability of the brush border membrane to Ca++. Subsequent steps in' the absorption of Ca++ were considered to be secondary to this event (102,103). In line with this theory, it has been reported that the 19 administration of a single dose of 1,25-(OH)2D3 to vitamin D-deficient animals stimulates intestinal calcium absorption prior to the induction of synthesis of the vitamin D-dependent calcium-binding protein (the synthesis of which is induced by the genomic action of 1,25-(OH) 2 D3) (101,104,105). Although others have not observed this temporal discrepancy, it has been reported that when minimal amounts of vitamin D-dependent calcium-binding protein are already present in the intestine, 1,25-(OH) 2 D3 can stimulate calcium absorption prior to the synthesis of additional vitamin D-dependent calcium-binding protein (106). Therefore, it appears that 1,25-(0H)2D3 may exert its effects on intestinal calcium absorption through more than one molecular mechanism. Parathyroid Gland as a Target for 1,25-(OH)2D3 The parathyroid gland produces PTH, a powerful stimulator of the renal 25-OH-D3-la-hydroxylase. In addition, some evidence indicates that the parathyroid gland may be a target tissue for vitamin D. 1,25-(0H) 2 D3 has been shown to associate with nuclei of the parathyroid gland in vivo (107,108). Furthermore, a specific cytosol receptor for 1,25-(OH)2D3 has been characterized in parathyroid glands from several species (109). The parathyroids also contain a calcium-binding protein similar to that induced by 1,25-(OH)2 D3 in the duodenum (110). Of particular interest is the fact that 1,25-(OH)2D3 has been reported to exert feedback inhibition on PTH production in vivo (111) and in vitro (112), causing a decreased response of the parathyroids to low plasma calcium concentrations. Although some investigators havebeen unable to observe such an effect, this evidence has been cited as 20 providing a precedent for feedback effects of vitamin D on endocrine organs which produce regulators of 1,25-(OH)2D3 synthesis (113,114). Effects of Anterior Pituitary Hormones on the Renal la-Hydroxylase Controversy exists over whether GH and/or PRL stimulate, or have no effect on, 25-OH-D3-l-hydroxylase activity. It appears that if these hormones do influence circulating levels of 1,25-(OH) 2 D3, their role is limited to periods of "calcium stress". would stimulate Teleologically, it makes sense that these hormones 2 5 -OH-D3-la-hydroxylase, since pregnancy, lactation, and growth are associated with increased demands for calcium. However, in man it appears that there are either no changes, or only small changes, in plasma 1,25-(OH) 2 D3 levels associated with changes in the levels of GH and PRL. Spencer and Tobiassen showed that in hypophysectomized rats, GH promoted the conversion of 25-OH-[ 3 H]-D 3 to 1,25-(OH)2-[ 3 H]-D3 (115,116). However, GH was ineffective in increasing la-hydroxylase activity in intact rats (115). Spanos, et al. (117) reported that GH produced increased levels of 1,25-(OH)2D3 in hypophysectomized rats which had lower 1,25-(OH)2D3 levels than intact controls. Pahuja and DeLuca (118) confirmed this effect. However, Kumar, et al. (119) found little or no change in plasma 1,25-(OH) 2 D 3 in man during periods of chronically increased or decreased plasma GH. Likewise, Gertner, et al. (120) found that GH administration to GH-deficient dwarfs produced little or no change in plasma levels of 1,25-(OH)2D3. In contrast, Eskildsen, et al. plasma levels of 1,25-(OH) 2 D3 in acromegalics. (121) reported elevated Furthermore, this elevation was normalized following treatment with bromocriptine. 21 In mammals, increased levels of 1,25-(OH)2D3 have been reported during pregnancy and lactation (122-127), periods associated with increased plasma levels of PRL. CB-154, a dopamine agonist used to inhibit PRL secretion, was successful in blocking the rise in 1,25-(OH) 2D3 during lactation (128). In hens, increased levels of 1,25-(OH) 2 D3 have been reported during egg-laying (129). Furthermore, this increase in plasma 1,25-(0H)2D3 has been produced by injecting PRL into non-laying hens (129). PRL has been reported to stimulate production of 1,25-(OH) 2 D3 in a renal tubule preparation (130), and 25-OH-D3-la-hydroxylase activity in kidney homogenates was found to be increased following injection of PRL (131). In contrast, Matsumoto, et al. (132) failed to find a stimulatory effect of PRL on 25-OH-D3-la-hydroxylase activity in vitamin D-deficient rats. In man, an effect of PRL on 25-OH-D3-la-hydroxylase activity has yet to be clearly demonstrated. PRL does not appear to alter plasma levels of 1,25-(OH) 2 D3 in non-pregnant women (133,134). In addition, no significant changes in intestinal calcium absorption have been found in hyperprolactinemic states other than lactation (134). Finally, while levels of 1,25-(OH)2D3 are increased in lactating women during the first few weeks post-partum (135), it is still unclear that PRL is directly responsible for this effect. Although most studies on effects of anterior pituitary hormones on renal la-hydroxylase activity have focused on the effects of GH or PRL, there is also evidence for effects of both thyroid stimulating hormone (TSH), and the thyroid hormones whose secretion is stimulated by TSH. It has recently been reported that TSH has a direct effect on renal 25-OH-D3 metabolism in vitro. Using a perfused rat kidney system, Kano and Jones (197) demonstrated that TSH inhibited 22 synthesis of 1,25-(OH)2D3 from 25-OH-D3. Along with this inhibition of renal 25-(OH)-D3-la-hydroxylase activity, these investigators observed a stimulation of 2 5 -(OH)-D3-24-hydroxylase activity induced by TSH. In addition, the thyroid hormones T 3 and T4 were found to affect renal 25-OH-D 3 metabolism in the same fashion as did TSH. Thyrotropin releasing hormone (TRH), on the other hand, had no effect. Pituitary Gland as a Target for 1,25-(OH)2D3 Prior to 1979, a role for 1,25-(OH)2D3 in the regulation of pituitary function had not been considered. However, results from several lines of experimentation have recently led investigators to speculate that the pituitary gland might be a target organ for the active form of vitamin D. This speculation was based on the following observations: 1. as discussed above, there have been reports in the literature indicating that the anterior pituitary hormones GH, PRL, and TSH may affect the production of 1,25-(OH)2D3; 2. other steroids (e.g., cortisol) whose synthesis is regulated by pituitary hormones have been found to have receptors in the pituitary, and exert feedback effects on the pituitary cells which synthesize these hormones (136); and 3. it has already been reported that 1,25-(OH)2D3 may be involved in a feedback system to regulate the production of PTH by the parathyroid gland (111,112). 23 The first report of a specific pituitary binding protein ("receptor") for 1,25-(OH)2D3 came from Stumpf, et al. (107). Using autoradiographic techniques, these investigators found that when 1,25-(OH) 2 -[3H]-D 3 was injected into vitamin D-deficient rats, the label subsequently appeared in the nuclei of certain anterior pituitary cells (107,138). With combined autoradiography and immunohistochemistry, this group later demonstrated that radioactivity appears in the nuclei of pituitary thyrotropes following injection of 1,25-(OH)2-[3H]-D 3 in the normal rat (140). Furthermore, there was no label apparent in pituitary cells stained by anti-PRL, anti-GH, or anti- LH. The presence of a specific binding protein for 1,25-(OH)2D3 in normal rat pituitary was subsequently confirmed by Haussler, et al. (113). This group characterized a cytosolic binding protein for 1,25-(OH) 2 D3 via sucrose density gradient sedimentation, saturation analysis, and DNA-cellulose chromatography. Non-pregnant female rats were used in this study. investigators looked for specific binding of 1,25-(OH) 2 -[3H]-D 3 The in pituitary sections, dispersed anterior pituitary cells, whole pituitary cytosol, and kidney cytosol. DNA-cellulose chromatography revealed a pituitary cytosolic binding protein which co-eluted with the kidney cytosol receptor. However, this protein represented only a small amount of the bound ligand which eluted from the column. Subsequent analysis of whole pituitary cytosol by sucrose density gradient sedimentation revealed a minor portion of label which migrated at 3.3 S, with the "vast majority" binding to a 5.8 S macromolecule. This 5.8 S protein did not absorb to DNA-cellulose, and the authors concluded that it was an artifactual complex of the serum vitamin D-binding protein with an intracellular protein which is present in all nucleated cells. 24 This 5.8 S species had a higher affinity for 25-OH-D3 than for 1,25-(OH)2D3. When pituitary quarters were assayed in a similar fashion, there was a more selective association of 1,25-(OH)2D3 with the 3.3 S species. still present in sizeable amounts. The 5.8 S protein was It appeared that the 3.3 S protein was specific for 1,25-(OH)2 D3, while 25-OH-D3 bound exclusively to the 5.8 S compound. Finally, when dispersed anterior pituitary cells were examined, 1,25-(OH)2D3 was found to bind uniquely to the 3.3 S binding protein. The 5.8 S species was still present, but not in high enough concentration to compete with the 3.3 S protein for binding of 1,25-(OH)2D3. The dispersed cell preparation was subjected to saturation analysis. Saturation with 1,25-(OH) 2 D3 occurred at approximately 1 nM, with a Kd of 5x10-10M. The concentration of the receptor in cytosol was approximately 4 fmole/ mg protein. No attempt was made to study the functional sequellae of binding of 1,25-(OH) 2D3 to the 3.3 S binding protein. Although specific binding was demonstrated, and the physical characteristics of the binding protein determined, no biological response was shown. This binding protein, therefore, could not yet be characterized unequivocably as a receptor, in the classical pharmacological sense. Similar specific binding sites for 1,25-(OH)2D3 in pituitary preparations have now been demonstrated in several other species. The physical characteristics of these sites are all similar, and are described in table 2. Gelbard, et al. (142,143) have described specific binding of 1,25-(OH)2D3 in crude nuclear and cytosolic fractions of bovine pituitary homogenates. al. .(144) Pike, et injected tritiated 1,25-(OH)203 into vitamin D-deficient chickens, sacrificed them several hours later, and found label in the pituitary. 25 This Animal Preparation Rat cytosol 5 Calf nuclear fr. Chick Eel !1 a Bb Specc SDGd DNAe Reference 4 1,25>25 3.3 + 113 1 104 1,25>25 ND ND 142 cytosol ND ND ND 3.3 + 144 cytosol 1 76 1,25>25 3.7 + 145 Table 2. Physical characteristics of specific pituitary binding sites detected for 1,25-(OH)D a. Dissociation constant (multiply values by 10-10 M). b. Number of binding sites (units = fmol/mg protein). c. Specificity: rank order affinity of vitamin D-metabolites for binding protein (1,25 = 1,25-(OH)2D3; 25 = 25-OH-D3). d. Sucrose density gradient sedimentation coefficient (units = S). e. Affinity for DNA-cellulose (+ if hormone-binding protein complex binds to DNA-cellulose column under low salt conditions and is eluted under high salt conditions). ND. Not done. 26 group also prepared rachitic chick pituitary cytosol and directly labelled it with 10-9M 1,25-(OH)2 -[3 H1-D3- DNA-cellulose chromatography and sucrose density gradient sedimentation revealed a sterol-protein complex with the same characteristics as that obtained from chick intestinal cytosol, and similar to the complex found in normal rat pituitary cytosol. Freake, et al. (145) have recently described a pituitary cytosolic binding protein for 1,25-(OH)2D3 in the common eel (A. arguilla). The characteristics of this protein are similar to those already described in other species. At this point in time, no biological response has been demonstrated as a consequence of 1,25-(OH)2D3 binding to the specific pituitary protein(s) described above. Several groups have attempted to study the interaction between 1,25-(OH)2D3 and the pituitary using clonal cell lines obtained from either rat or mouse pituitary tumors. Cultured cell lines provide an easily manipulated homogeneous cell population in which one may identify and characterize the components of an endocrine response. However, many of the studies performed to date have used different strains of cells and/or different growth conditions. The inconsistencies in cell type, media composition, duration of cell growth, and experimental design (doses of drugs administered, time points for examination, method of assay, method of preparation of cytosol and/or nuclear fractions) make contradictory results difficult to objectively evaluate. Furthermore, the cultured pituitary tumor cells differ from normal pituitary cells in several respects. Some investigators have found that concentrations of 1,25-(OH)2 D3 required for "receptor" occupancy are significantly higher than the in vitro Kd. This may be due to binding of 1,25-(OH) 2 D3 to media proteins, but this has not been confirmed. 27 More importantly, tumor cells in culture show greater fluctuations in phenotypic expression than commonly seen in non-transformed cells. This is a key point to be kept in mind as the results from the following studies are reviewed. In all of these studies, if any biological response was examined, it was synthesis and/or secretion of PRL and/or GH. These parameters were no doubt chosen because of the reported effects of these hormones on the renal 25-(OH)-D-la-hydroxylase. In addition, of the commercially available pituitary tumor cell lines, identification of a specific 1,25-(OH)2D3 binding protein has been reported only in GH cells (which secrete only PRL and GH). The putative receptor was not found in a cell line (AtT20) which secretes metabolites of pro-opiomelanocorticotropin (185). No cell line secreting TSH is currently commercially available, and no attempts have been made to establish a clonal TSH-secreting cell line for the purposes of examining effects of 1,25-(OH)2D3. In spite of their drawbacks, the tumor cell studies are of interest because several of the investigators have attempted to determine the biological response(s) which might result from the interaction of 1,25-(OH)2D3 with its putative receptor. Since the physical characteristics of this protein appear to be identical to those reported for the specific binding protein detected in normal pituitary (see table 3), one might speculate that receptor activation would produce similar effects in both GH cells and normal anterior pituitary. However, such a speculation is risky since the presence of the specific binding protein in these tumor cells may be due to abnormal phenotypic expression of the genome. If this binding protein is not normally expressed in pituitary somatotrophs or lactotrophs, then the responses initiated by 1,25-(OH) D3 2 28 Cell Preparation GH 4 cytosol 1-2 (8-10,000) 1,25>25 GH 3 cytosol 2.9 55,(8500) 1,25>25 AtT20 DNAe f Ref 3.7 ND 114 3.3 + 185 cytosol NO SPECIFIC BINDING PROTEIN DETECTED 185 GH 3 cytosol 0.47 (10,500) 1,25>25 3.3 + 148 GH 1 cytosol 0.31 (10,500) 1,25>25 3.3 + 148 GH 3 nuclear fr. 1.1 59 1,25>25 ND ND 141 Cpecc SDGd Table 3. Physical characteristics of specific binding sites detected for 1,25-(OH)?D3 in clonal pituitary tumor cells a. Dissociation constant (multiply values by 10-10 M). b. Number of binding sites (units = fmol/mg protein, or receptors/cell if displayed in parentheses). c. Specificity: rank order affinity of vitamin D-metabolites for binding protein (1,25 = 1,25-(0H)2D3i 25 = 25-OH-D3). d. Sucrose density gradient sedimentation coefficient (units = S). e. Affinity for DNA-cellulose (+ if hormone-binding protein complex binds to DNA-cellulose column under low salt conditions and is eluted under high salt conditions). ND. Not done. 29 binding to GH cell receptors must be considered artifactual. In light of the evidence obtained by Sar, et al. (140), using autoradiography and immunohistochemistry, this possibility must be seriously considered. Acknowledging that the effects of 1,25-(OH)2 D3 binding to GH cell receptors may not be a true reflection of the sterol's actions in normal pituitary, these tumor cell cultures are still the only preparation in which biological responses to 1,25-(OH)2D3 have been examined. The results obtained to date have been contradictory and difficult to compare. However, they may provide insight into some of the biological responses which would warrant further examination in normal anterior pituitary cells. Murdoch and Rosenfeld (114,146) were the first to report both detection of a specific binding protein for 1,25-(OH)2D3 in a pituitary cell line, and a biological response of these cells following administration of the sterol. In this study, GH 4 cells were grown in Ham's F10 medium, 12.5% horse serum, 2.5% fetal calf serum, and subcultured at 5x10 5 cells/ 30 mm 2 Falcon plate. Four days after subculture, the medium was changed to Ham's F12 plus serum, and supplemented with 0.01 mM Ca++ (their medium contained 0.41 mM Ca++ in the absence of added calcium). 1,25-(OH) 2 D3 and/or TRH was added to the medium to begin an experiment. The medium was removed 48 h later and assayed for PRL. They found that 1,25-(OH) 2 D3 decreased basal PRL secretion, and augmented TRH-stimulated PRL secretion. Both effects varied directly with the concentration of calcium in the medium. Furthermore, they found that in addition to altering PRL synthesis, 1,25-(OH) 2 D3 induced the synthesis of three unidentified cellular proteins. Finally, TRH was found to block basal synthesis of these proteins along with their induction by 1,25-(OH)2D3. 30 The ED50 for the effect of 1,25-(OH)2D3 on PRL secretion was 6x10- 9 M. The authors state that this concentration is higher than they expected, and speculate that this finding is merely a reflection of the medium's capacity to bind 1,25-(OH)2D3. Under these conditions, they claim that only 2.75% of the secosteroid is unbound. If the ED 50 is adjusted for this factor, then it appears to be quite close to the Kd of the receptor. The ED50 for the effect of 1,25-(OH) 2 D3 on protein induction was similar (3 x 10- 9 M). Finally, the ED 50 for TRH-inhibition of this protein induction was the same as the ED 5 0 for induction of PRL by TRH alone. Wark and Tashjian (139) also examined effects of 1,25-(OH)2D3 on PRL secretion using a rat pituitary tumor cell line. However, they used the GH4 C1 strain, and they did not demonstrate that a specific binding protein is expressed by these cells. Furthennore, their experiments. were carried out under serum-free conditions. Consequently, it is difficult to evaluate the discrepancy between the effects they detected and the results reported by Murdoch and Rosenfeld (114,146). F10 medium, 17.5% serum. Wark and Tashjian grew their cells in Ham's Four or five days after subculturing, they replaced the serum-supplemented medium with a serm-free medium (minimal essential medium with non-essential amino acids, Earle's balanced salts without CaCl 2 , and 10% "hormone-free serum substitute"). This serum-free medium contained calcium at a concentration of only 28 + 1 UM (well below physiological levels). Cells were - incubated for 24 h prior to treatment with vitamin D metabolites and/or CaCl 2 Hormone production was then measured at 24 h intervals for up to four days. Concentration of PRL in the medium was determined by RIA, and GH was measured by microcomplement fixation immunoassay. 31 1,25-(OH)2D3 (1x1O-9 M) and CaCl2 (0.15 mM) had no effect on release of GH into the medium at any time point. This combined treatment also failed to alter PRL release during the first 24 h of incubation. However, during the second 24 h period an increase in PRL release was observed (163% of control). Following 96 h of combined treatment, PRL release into the medium was stimulated greater than five-fold, as compared with untreated controls. These investigators next examined hormone release in the presence of various concentrations of CaC1 2 in the medium. Hormone levels were measured only during the second 24 h period subsequent to administration of 1,25-(OH) 2 D3 (1x10-9 M). In the absence of added CaCl 2 , PRL release was unaffected by 1,25-(OH) 2 D3, while GH release diminished to 60% of control (no 1,25-(0H) 2 D3 present). When the medium contained 0.1mM CaCl2, PRL release rose to 300% of control, with GH release remaining at 60% of control. 1,25-(OH)2D3 produced a further increase in PRL release when the medium contained 0.2mM CaCl 2 (to 400% of control), while bringing GH release back to control values. In the presence of 0.4 mM CaCl 2 , the ED50 for the effect of 1,25-(OH)2D3 on PRL release during the second 24 hours of treatment was reported as 2x10-10M. 1-OH-D 3 was found to be 30-fold less potent. 25-OH-D 3 and 24,25-(OH)2D3 were 1000-fold less potent in stimulating PRL release under these conditions. Cell growth in the presence of 1,25-(OH)2D3 was observed following plating at three different densities. No effect of 1,25-(0H) 2 D 3 on cell number was seen, regardless of the initial plating density. 32 Finally, the effect of 1,25-(OH)2D3 on PRL release was also determined to be independent of initial plating density. Thus, in contrast to the results reported by Murdoch and Rosenfeld (114,146), Wark and Tashjian concluded that 1,25-(OH)2D3 stimulates PRL release from cultured pituitary tumor cells, and that this effect is calcium-dependent. Which of the results (if either) represents a physiological effect of the active form of vitamin D in normal pituitary tissue is unclear. Wark and Tashjian, however, have recently extended their studies by examining the effects of 1,25-(OH)2D3 on accumulation of specific rPRL mRNA in GH4 C 1 cells, determined via cytoplasmic dot hybridization (198). Using complementary DNA (cDNA) probes, these authors very elegantly confirmed their earlier findings. Although they state that no consistent effect of 1,25-(OH) 2 D3 could be observed in the first 24 hours of treatment, they found that stimulation of rPRL mRNA accumulation was 163% of control after 48 hours, and 200% of control after 96 hours. The effect was once again determined to be calcium dependent, and no change in growth hormone mRNA accumulation (also measured using a cDNA probe) was observed in response to treatment with 1,25-(OH)2D3. Two other groups have investigated the effects of 1,25-(OH) 2 D3 on the activity of clonal rat pituitary tumor cells, using the GH 3 and GH1 cell lines. These studies further cloud the issue. Haug, et al. (147) report a parallel and dose-dependent decrease in both PRL and GH synthesis induced by 1,25-(OH) 2 D3 in GH3 cells. Ham's F10 medium. These cells were grown in serum-supplemented The effects on hormone production were significant at 10-11M and 10-10M respectively. In this study, hormone production 33 was calculated as the amount released into the medium during the last 24 h of a six day incubation with 1,25-(OH) 2 D3. Although maximal inhibition of hormone release was found following six days of treatment, the effect was detectable after only two days. 25-OH-D3 and la-OH-D3 also inhibited hormone release, but in both cases the ED50 was 1000-fold higher than for 1,25-(OH) 2 D3. No effect of 24,25-(OH)2D3 was observed over a reasonable range of concentrations (o-11M to 10- 6M). affect cell growth (ug protein/ well). 1,25-(OH)2D3 failed to When 1,25-(OH)2D3 was co-administered with either 25-OH-D 3 , la-0H-D3, or 24,25-(OH)2D3 the effect of 1,25-(OH)2D3 on hormone release was only slightly counteracted. TRH and DES (a synthetic analog of estrogen) both were capable of increasing secretion of PRL from GH 3 cells under these incubation conditions. 1,25-(0H) 2 D 3 was found to partially inhibit the effects of these factors on PRL release, without affecting binding of TRH or 170-estradiol to their respective receptors. It was thus concluded that the effect of 1,25-(0H) 2 D3 on PRL release in this cell line was not due to a direct action on receptors for TRH or estrogen. Haussler, et al. (148) also examined the effect of 1,25-(OH) D 2 3 (10-11M to 1o- 7M) on hormone production by GH 3 cells. In contrast to the findings of Haug, et al. (147), no effect was seen on secretion of GH. This group did not measure PRL release, but confirmed the lack of effect of 1,25-(OH)2D3 on GH3 cell growth (in terms of cell number and cellular protein content). They further examined the same parameters in GH 1 cells, and again-found no effect of 1,25-(OH) 2 D 3 on GH release. 34 The studies performed on rat pituitary tumor cell lines have yet to elucidate a consistent effect of 1,25-(OH)2D3 on pituitary function. In light of the autoradiographic evidence for exclusive localization of label from 1,25-(0H) 2 -[3 H]-D3 in nuclei of normal rat pituitary thyrotropes, along with the knowledge of large fluctuations in phenotypic expression of tumor cells in culture, any direct physiological effect of 1,25-(OH) 2 D3 on PRL or GH secretion must, at this point in time, be viewed with skepticism. remains unclear what role, if function. It thus any, 1,25-(OH)2D3 may play in normal pituitary A physiological effect of 1,25-(OH) 2 D3 binding in normal pituitary, whether it be alteration of cell growth, hormone synthesis, or hormone secretion, remains to be clearly demonstrated. In conclusion, some mention must be made of the in vivo evidence which is suggestive of an effect of 1,25-(OH) 20 3 on pituitary function. Stumpf, et al. published an abstract (159) describing effects of 1,25-(OH)2D3 on circulating TSH levels in intact and thyroidectomized vitamin D-deficient rats. In both cases, vitamin D-deficient rats treated with 1,25-(OH) 2 D3 exhibited elevated serum levels of TSH. calcium orally to healthy Czechoslovakian women and measured serum thyroxine, TSH, calcium, and magnesium. treatment, and it Zafkova, et al. (160) administered 25-OH-D 3 and Thyroxine was the only parameter affected by such was elevated. Blumberg, et al. (161) examined several endocrine parameters before and after administration of 1,25-(OH) 2 D3 to patients undergoing maintenance hemodialysis. elevated. Prior to treatment, serum PRL was Following treatment, serum calcium was elevated, serum PTH was decreased, testosterone was slightly elevated in men, and serum PRL was moderately decreased in both men and women. 35 Suzuki, et al. (162) reported effects of la-OH-D3 in a case study of a woman being treated for hypocalcemia due to pseudohypoparathyroidism. Endocrine tests in the hypocalcemic state revealed an exaggerated response of TSH to TRH, and a blunted GH response to arginine-HCl. Both of these abnormalities were rectified following restoration of normocalcemia by giving la-OH-D3. Finally, Tornquist and Lamberg-Allardt recently presented an abstract in which they describe effects of 1,25-(OH) 2 D3 on the regulation of TSH secretion in rats (199). These investigators injected rats with 1,25-(OH)2D3 (5 ug/kg/day) for 3 days, and then injected i.v. TRH 8 hours after the last dose. At various times thereafter, samples of blood were withdrawn from carotic artery cannulae. It was found that 1,25-(OH)2D3 significantly increased the response of TSH to TRH. Although all of these studies demonstrate changes in pituitary function following administration of vitamin D-metabolites, none of them demonstrate conclusively a direct effect of 1,25-(OH) 2 D 3 on pituitary function. 36 RATIONALE AND SPECIFIC AIMS The current conception of 1,25-(OH) 2 D3 as a calcium homeostatic hormone has gained wide acceptance (202,203). This notion is justified by the fact that decreases in plasma calcium concentration stimulate secretion of parathyroid hormone (PTH) (204), and PTH acts as the most potent known stimulator of the renal 25-OH-D3-la-hydroxylase (205-207). Furthermore, at target tissues in which the effects of the hormone have been best characterized (intestine and bone), the ultimate effect is to direct calcium into the circulation (208,209). Given the critical role of calcium in a vast array of biological phenomena (211), any information concerning the overall mechanisms by which the body maintains calcium homeostasis is of potential physiological, pathological, and pharmacological significance. It is clear that calcium is involved in many aspects of pituitary function. These include normal pituitary cell growth (211), basal and stimulated hormone release (200,201), and mediation of many target tissue responses induced by pituitary hormones (212-218). These facts, coupled with the possibility that 1,25-(OH)2D3 may affect intracellular free calcium concentration, suggest that the activation of pituitary receptors for 1,25-(OH) 2 D3 might produce changes in the secretion of specific pituitary hormones. Evidence has been presented indicating that the pituitary may be a target site for 1,25-(OH) 2 D3. Several groups have now demonstrated the existence of a specific pituitary binding protein for 1,25-(OH) 2 D3. A physiological role for this putative receptor in normal pituitary function has yet to be determined. A receptor, by definition, must specifically bind a ligand, with 37 the receptor-ligand interaction initiating a biological response. In the absence of a response, the specific binding protein cannot be classified as a receptor (specific transport proteins and storage proteins are examples of specific binding proteins which are not receptors). The biological -response initiated by the interaction of 1,25-(OH) 2D 3 with a specific binding protein in normal mammalian pituitary cells, and the mechanism underlying such a response, remain unclear. In light of the research already performed concerning effects of 1,25-(OH)2D3 on the activity of neoplastic pituitary cells, it was important to determine how this sterol might affect the activity of non-transformed mammalian anterior pituitary cells which possess the putative receptor. Due to the increased frequency of abnormal genetic expression in pituitary tumor cells, the effects of 1,25-(OH)2D3 receptor activation detected in these cells may be artifactual. It cannot be concluded that the responses observed following binding of 1,25-(OH)2D3 to the expressed receptor are necessarily indicative of the sterol's action(s) in normal pituitary. The variability in responses which have been reported by different groups following administration of 1,25-(OH)2D3 to cultures of transformed pituitary cells is further support for this conclusion. Although dispersed anterior pituitary cells maintained in culture may not be "normal", they are less likely to be expressing abnormal characteristics than are transformed cells. While it is possible that biological responses may be either masked or de-repressed in cultures of dispersed anterior pituitary cells, the information gained from the use of this preparation may provide valuable insights into the responses induced by 1,25-(OH)2D3 in vivo. 38 Given our knowledge of vitamin D and the pituitary, it was possible to speculate several possible roles for 1,25-(OH) 2D 3 in the regulation of pituitary function. Based on the studies with rat pituitary tumor cells, and the reports of alterations in 25-OH-D3-la-hydroxylase activity induced by PRL and GH, one might expect 1,25-(OH) 2 D 3 to alter the synthesis and/or release of these hormones. The autoradiographic evidence for exclusive localization of 1,25-(OH)2D3 in nuclei of pituitary thyrotropes would lead one to suspect an effect of vitamin D on TSH synthesis and/or release. may in some manner alter growth of pituitary cells. Finally, 1,25-(OH)2 D3 Although no effects of 1,25-(OH)2D3 have yet been reported on growth of GH cells, this form of vitamin D has been found to alter the growth of several other types of cells (163-167). The purpose of this thesis work was to examine a variety of biological responses which would be indicative of an effect of 1,25-(OH) 2 D 3 on the activity of non-transformed anterior pituitary cells obtained from normal rats. The general goal of this thesis was to determine whether or not 1,25-(OH)2D3 is capable of affecting the activity of non-transformed mammalian anterior pituitary cells, at least as far as the parameters to be investigated are concerned. If it was to be found that 1,25-(OH)2D3 affects any of these parameters, then it would be apparent that the specific pituitary binding protein present in normal mammalian anterior pituitary is in fact a receptor. If no effects could be demonstrated, then the question of whether or not the specific binding protein detected in non-transformed mammalian anterior pituitary cells is a true receptor would have remained unanswered. case, it could only be concluded that 1,25-(OH) 2 D3 was incapable of 39 In this affecting the specific parameters of pituitary function examined. However, since some of these parameters have been reported to be altered following binding of 1,25-(OH)2D3 to receptors in clonal rat pituitary tumor cells, a negative thesis would raise serious doubts about the physiological relevance of receptor responses detected in transformed cells. It is possible that 1,25-(OH)2D3 may affect neuroendocrine activity either directly, via the putative pituitary receptor, or indirectly, via effects on calcium metabolism in bone, kidney, and intestine. The importance of calcium to neural, endocrine, and muscular function cannot be overstated. The clarification of the relationship between 1,25-(OH)2D3 and the pituitary would further our understanding of the mechanisms by which the body maintains calcium homeostasis. In addition, the speculation of feedback effects of the hormonal form of vitamin D, on an endocrine organ which produces a regulator of 1,25-(OH) 2 D3 synthesis, is of general endocrine interest. The results of these studies would also help to clarify the effects of 1,25-(OH)2D3 on PRL secretion (a response which has been inconsistently affected in tumor cell studies). In the process, they would provide insight into the relevance of receptor responses detected in tumor cells to events which occur in non-transformed cells. In addition, if it is found that 1,25-(OH)2D3 affects the growth of pituitary cells in culture, this would raise the possibility that genesis or progression of specific types of pituitary tumors might be effectively inhibited by 1,25-(OH)2D3. Finally, the results would add to our understanding of the physiological interplay that exists between vitamin D and other endocrine systems, and the regulation of pituitary function. 40 Given this rationale, the specific aims of this thesis work were as follows: 1. Verify the presence of a specific binding protein for 1,25-(OH)2D3 in rat anterior pituitary; 2. Determine the binding characteristics of this putative pituitary receptor for 1,25-(OH)2 D3; 3. Establish primary cultures of viable enzymatically dispersed rat anterior pituitary cells which possess the putative receptor for 1,25-(OH)2D3; 4. Demonstrate the ability to maintain cell viability and functionality in culture for periods of time sufficient to examine the effects of 1,25-(OH) 2 D 3 on the activity of these cells; 5. Determine whether these cells in primary culture retain normal responsiveness to a known secretogogue (TRH) throughout the time period of interest in subsequent studies on the effects of 1,25-(OH)2D3; 6. Examine the effects of treatment with 10- 8 M 1,25-(OH) 2 D3 for various periods of time on several parameters of the function of rat anterior pituitary cells in primary culture, including: A.- synthesis and secretion of rPRL; B.' synthesis and secretion of rTSH; and 41 C. 7. cell growth; Determine whether the responses observed following treatment with 1,25-(OH) 2 D3 are dose-dependent; 8. Determine the structural specificity of 1,25-(OH) 2 D3 required for inducing any observed effects by treating cultures with 10,25-(OH)2D3, a structural analog of 1,25-(OH)2D3. This analog has been shown to be biologically inactive with other well-characterized receptors for 1,25-(OH) 2 D 3 , and does not compete with 1,25-(OH)2D3 for binding to its receptor. 42 MATERIALS AND METHODS Drugs and Chemicals la,25-Dihydroxyvitamin D3 was kindly provided by Dr. M. Uskokovic, Hoffman-LaRoche, Nutley, New Jersey. 25-Hydroxyvitamin D3 was kindly provided by Dr. J. Babcock, Upjohn, Kalamazoo, Michigan. 18,25-Dihydroxyvitamin D3 was kindly provided by Dr. S. Holick, M.I.T., Cambridge, Massachusetts. 1,25-Dihydroxy-[26,27- 3 H]-vitamin D3 (158-170 or 91 Ci/mmol) was purchased from New England Nuclear, Boston, Massachusetts. Thryotropin Releasing Hormone (TRH; p-Glu-His-Pro-NH 2 ) was purchased from United States Biochemical Corporation (catalog #22371; lot #21977), Cleveland, Ohio. 3 5 S-methionine (Methionine, L-[ 3 5S]; 1058 Ci/mmol; 1 mCi/O.1 ml) was purchased from New England Nuclear (catalog #NEG-009T; lot #1013-210), Boston, Massachusetts. 43 Immediately prior to their use, all vitamin D metabolites were re-checked for purity and concentration via ultraviolet spectroscopy and high pressure liquid chromatography. Sources and descriptions of any other chemicals used in these studies, other than standard laboratory reagents, are provided in the sections describing their use. Animals Adult male Sprague Dawley CD-derived rats, weighing 250-300 grams, were obtained from Charles River Breeding Laboratories, Inc. (Wilmington, Massachusetts). Prior to their use, rats were housed in facilities maintained by the M.I.T. Department of Laboratory Animal Medicine. Rats were kept in hanging cages, in pairs, in a climate-controlled room, under a 12:12 light:dark schedule, and fed normal rat chow (Charles River Rat Chow, Charles River Laboratories, Wilmington, Massachusetts). Dissection of Rat Anterior Pituitary for use in Binding Studies Anterior pituitary tissue was obtained from 250-300 g male Sprague Dawley CD-derived rats. Rats were sacrificed by rapid decapitation. opened, and the brain was removed. The calvarium was The membrane covering the pituitary gland was then separated from the underlying tissue, thus exposing the hypophysis. The pituitary was then lifted from the sella turcica, and immediately placed in ice-cold isotonic buffer containing 50 mM Tris-HCl (pH 7.4), 1.5 mM EDTA, and 5 mM dithiothreitol. The posterior pituitary was carefully dissected away from 44 the anterior pituitary and discarded. removed. Any extraneous connective tissue was also The isotonic buffer was then discarded, and the remaining anterior pituitary was washed three times with hypertonic buffer (10 mM Tris-HCl, pH 7.4, 1 mM EDTA, 5 mM dithiothreitol, 300 mM KCl, and 10 mM sodium molybdate) to remove as much plasma as possible. When nuclear extracts of anterior pituitary were to be prepared, this last step was omitted, and the glands were left in isotonic buffer. Preparation of Cytosolic and Nuclear Extracts of Rat Anterior Pituitary Cytosolic and nuclear extracts were prepared from pooled anterior pituitary glands of 20 rats. Isolated anterior pituitary glands were washed in ice-cold hypertonic buffer and minced into 1 mm 2 fragments with sterile razor blades. The tissue fragments were then suspended in 1.0 ml of fresh hypertonic buffer and transferred to a 1.5 ml Eppendorf tube. sonicated for 15 seconds on ice. The tissue suspension was then The resulting homogenate was transferred to a polycarbonate tube, and centrifuged at 100,000 x g for 1 hour, at 40C, in a Beckman 50Ti rotor. This treatment yielded a cytosolic supernatant. The cytosol extract was either used immediately, or kept frozen at -700C prior to assay. Crude nuclear extracts were prepared from isolated rat anterior pituitary glands in isotonic buffer. The anterior pituitaries were minced into 1 mm 2 fragments and suspended in 1.0 ml of fresh isotonic buffer. The tissue suspension was transferred to a 1.5 ml Eppendorf tube and sonicated for 15 seconds on ice. The resulting homogenate was transferred to a polycarbonate 45 tube, and centrifuged at 12,000 x g, for 10 minutes, at 40C, using a Beckman 50Ti rotor. The supernatant was then removed, and the crude nuclear pellet was resuspended in 4 volumes of ice-cold isotonic buffer. This tissue suspension was then transferred to a 1.5 ml Eppendorf tube and washed 4 times With isotonic buffer. Each wash involved addition of ice-cold isotonic buffer, vortexing, centrifugation for 5 minutes in a Beckman Microfuge B at 40C, and removal of the supernatant. After the final wash, the pellet was resuspended in 0.5 ml hypertonic buffer and vortexed vigorously for 2 minutes. The tissue suspension was then transferred to a polycarbonate tube, and centrifuged for 1 hour at 22,000 x g, at 40C, in a Beckman 50Ti rotor. the crude nuclear extract. The resulting supernatant was This nuclear extract was either used immediately, or kept frozen at -700C prior to assay. Sucrose Density Gradient Sedimentation Analysis Sucrose density gradient sedimentation analysis was performed essentially as described by Clemens, et al. (180). 0.2 ml aliquots of either rat anterior pituitary cytosolic or nuclear extracts were incubated on ice for 4 hours in the presence of 4 nM 3 H-1,25-(0H)2D3 (91 Ci/mmol; 80,000 cpm), alone or together with a 50-fold excess of unlabelled 1,25-(OH)2D3. 75 ul of a Dextran-coated charcoal solution was then added to each tube to remove any unbound sterol. The samples were incubated with charcoal for 20 minutes on ice, and then centrifuged at 3,000 x g, for 10 minutes, at 40C. Following centrifugation, 0.2 ml of the supernatant was layered onto 4.8 ml sucrose density gradients (4%-20% sucrose, prepared in hypertonic buffer) in Beckman 46 Ultraclear tubes. The gradients were then centrifuged for 16-18 hours, at 257,000 x g, at 20C, in a Beckman SW50.1 rotor. Gradients were fractionated from the bottom of the tube (5 drops/ fraction) using a peristaltic pump. fraction was placed in a scintillation vial. Each 10 ml of a scintillation cocktail (Instagel; United Technologies/ Packard) was then added to each vial, and the radioactivity in each fraction was determined by liquid scintillation counting in a Packard Tri-Carb 460C liquid scintillation counter. Parallel gradients run on cytosol prepared from intestine of vitamin D-deficient chicks, or from intestine of mice, were used as positive controls. Protein markers (bovine serum albumin, 4.4 S; ovalbumin, 3.7 S) were also used to estimate sedimentation coefficients. Determination of Binding Characteristics Aliquots of rat anterior pituitary cytosol were used in a competitive binding assay in order to determine the receptor equilibrium dissociation constant (Kd) and the number of binding sites (Bmax). The method used was a modification of the method described by Haussler, et al. (113). 0.1 ml aliquots of cytosol were added to duplicate tubes containing various concentrations of 3 H-1,25-(0H) 2D3 (0.25 nM to 4.0 nM), alone or together with a 200-fold excess of unlabelled 1,25-(OH) 2 D3 (to determine non-specific binding). water-bath. The samples were incubated for 30 minutes, at 250C, in a shaking The samples were placed on ice, and 0.15 ml of an ice-cold Dextran-coated charcoal solution was added to remove any unbound sterol. After addition of the charcoal solution, the samples were incubated on ice -for 10 47 minutes, and then centrifuged at 5,000 x g, for 10 minutes, at 40C. 0.2 ml aliquots of the resulting supernatants were transferred to small scintillation vials. 4 ml of a scintillation cocktail (Instagel; United Technologies/ Packard) was added to each vial, and the radioactivity in each sample was determined by liquid scintillation counting in a Packard Tri-Carb 460C liquid scintillation counter. Specific binding was calculated by subtracting the non-specific from the total binding. The data was then subjected to Scatchard analysis (181) to determine the Kd, Bmax, and presence of singular or multiple classes of binding sites (e.g., high affinity and low affinity). Rat Anterior Pituitary Cell Culture Cultures of enzymatically dispersed rat anterior pituitary cells were prepared and maintained essentially as described by Vale, et al. (168). equipment and procedures were used throughout. Sterile Anterior pituitaries were obtained from 250-300 g adult male Sprague Dawley CD-derived rats. Rats were sacrificed via rapid decapitation, the calvarium opened, the brain removed, and the pituitary lifted from the sella turcica. The pituitaries were immediately placed in a HEPES buffer (137 mM NaCl, 5 mM KCl, 0.7 mM Na2HPO4, 25 mM HEPES (n-2-hydroxyethylpiperazine ethanesulfonic acid), 10 mM glucose, 0.36 mM CaCl 2 , pH 7.2) containing 1% (v/v) of an antibiotic solution (penicillin, Sigma PEN-NA, 448 mg/ 100 ml ddH 20; streptomycin, Sigma S-6501, 667 mg/ 100 ml ddH 2 0.). The posterior lobes were then dissected free and discarded. The remaining adenohypophyses were then sliced into 1 mm 2 fragments, and washed three times with HEPES buffer. The washed anterior pituitary fragments were 48 then transferred to a 25 ml Erlenmeyer flask containing a teflon coated magnetic stirring bar, the HEPES buffer was removed, and the tissue fragments were resuspended in 10 ml HEPES buffer supplemented with 3% bovine serum albumin (RIA grade; Sigma), 0.1% hyaluronidase (550 U/mg, ovine testis, type III; Sigma), and 0.35% collogenase (146 U/mg; Worthington). The tissue fragments were then incubated in this enzyme solution at 370C, for 45 minutes, with stirring. Enzymatic dispersion of the cells was assisted by periodic gentle lifting and releasing of the cell suspension with a siliconized Pasteur pipette. Following complete dispersal of the cells, the suspension was transferred to a 15 ml plastic tube and centrifuged at 500 x g for 8 minutes. The supernatant enzyme solution was discarded, and the pelleted cells were resuspended in 10 ml culture medium (85% Ham's F10, M.A. Bioproducts; 12.5% donor horse serum, M.A. Bioproducts; 2.5% fetal bovine serum, M.A. Bioproducts; supplemented with 1% (v/v) of the antibiotic solution described above, filtered through a 0.2 um membrane (Millipore), and heated to 370C). The cells were then washed six times via centrifugation for 2 minutes at 500 x g, removal of the supernatant, and resuspension in fresh culture medium. Following the last wash, 100 ul of the final cell suspension was removed, mixed with an equal volume of a trypan blue dye solution (0.1% trypan blue dye in 0.9% NaCl), and examined microscopically on a hemocytometer to determine the concentration of viable cells present in the suspension. Sufficient culture medium was then added to the cell suspension to achieve a concentration of 3-5 x 105 viable cells/ ml. 1.5 ml of this cell suspension was then added to each of the desired number of 35 mm x 14 mm tissue culture wells (Falcon #3046; approximately 9.6 cm 2 growth area/ well), and the cell cultures were placed in an incubator (NAPCO 6300). 49 Cultures were incubated at 370C, in a humidified atmosphere containing 95% air and 5% C0 2 , for 4 days prior to initiation of experiments. Before beginning an experiment, the serum-supplemented culture medium was removed, and the cells were washed with Ham's F10 (which had been previously filtered through a 0.2 um membrane (Millipore) and heated to 370C). The wash was then discarded, 1.5 ml of fresh Ham's F10 was added to each well, and the cultures were returned to the incubator for a 1 hour pre-incubation period. The desired chemicals were then added to each culture, and the cells were returned to the incubator for the duration of the test period. of each test period. Media and cell samples were collected at the end The media from each culture was removed, placed in an individual 1.5 ml Eppendorf tube, and centrifuged at 1,000 x g for 5 minutes to pellet any floating cells. Each supernatant was then transferred to a new Eppendorf tube, and stored at -200C prior to assay. 1.5 ml of a Tris buffer (50 mM Tris-HCl, pH 7.4, 140 mM NaCl) containing 0.1% Triton X-100 was added to each well, and the attached cells were gently scraped off the dish using a rubber policeman. The scraped cell solution was then combined with the pelleted floating cells, and the total cell sample stored at -200C. Just prior to the initial assay, cell samples were thawed and sonicated for 15 seconds, on ice, using a Tekmar sonic cell disrupter. Determination of Cell Number and Viability The number of viable cells was determined by the trypan blue dye exclusion test '(176). Typically, 100 ul of a cell suspension was mixed with an equal volume of a trypan blue dye solution (0.1% trypan blue dye in 0.9% NaCl). 50 A drop of this mixture was immediately applied to a hemocytometer, and examined microscopically. Duplicate cell counts were performed, each time counting at least 5 regions of the hemocytometer. Concentration of viable cells was calculated as follows: (total number of viable cells counted) / (number of regions examined) x 2 x 104 = (number of viable cells) / ml. Cell Photography Cells in culture were photographed under a variety of treatment conditions using an Olympus microscope coupled with an Olympus camera system. Determination of Cellular Protein Content Protein content of cell samples was determined by the method of Lowry, et al. (178), using bovine serum albumin (RIA grade; Sigma) as standard. Determination of Cellular DNA Content DNA content of cell samples was determined by the method of Burton (179), based on the diphenylamine reaction. Calf thymus DNA (Sigma) was used as standard. 51 Radioimmunoassay for Rat Prolactin The concentration of rPRL in media and cell samples was determined by double-antibody radioimmunoassay, using standards, primary antibodies, and procedures supplied by the NIADDK. Material s: Samples: Samples were typically assayed in either duplicate or triplicate, and occasionally aliquots of different volume fron the same sample were assayed in parallel as a further control for accuracy of results. Assay Buffer: 0.01 M P0 4 , 0.5% bovine serum albumin (RIA grade; Sigma), 0.88% NaCl, 0.05 M EDTA, 0.1% sodium azide, pH 7.6. 1st Antibody Buffer: 0.05% normal rabbit serum (Pel-Freez Biologicals, Rogers, Arkansas) in assay buffer. 1st Antibody: NIADDK-anti-rPRL-S-9 (AFP-131581570), rat prolactin antiserum (rabbit), dissolved in 2% normal rabbit serum in phosphosaline buffer, was diluted 1:10 with 1st Antibody Buffer and stored in 0.5 ml aliquots at -200C. Prior to each assay, an aliquot of this solution was thawed and diluted 1:210 with 1st 52 Antibody Buffer, yielding a final dilution of 1:2100, and a "final tube dilution" of 1:12,600. 2nd Antibody: Goat anti-rabbit IgG (heavy and light chains; Cappel Laboratories, catalog #0112-0081, lot #17808), dissolved in 0.02 M phosphosaline (pH 7.3) containing 0.05% sodium azide, was stored in 500 ul aliquots at -200C. Prior to each assay, an aliquot of this solution was thawed and diluted 1:100 with assay buffer. Tracer: 1251-rPRL (New England Nuclear, catalog #NEX-108; 16.3 uCi total activity; 36.4 uCi/ug specific activity) was diluted with assay buffer to obtain a solution containing approximately 10,000 cpm/100 ul. Standards: NIADDK-rPRL-RP-3 (AFP-4459B) was used as the standard reference preparation. Reconstitution of 1 vial with 1 ml dH 2 0 yielded a solution containing 10 ug rPRL/ml, in 1% BSA in phosphosaline. 100 ul aliquots of this solution were stored in Eppendorf tubes at -200C, and used within 5 months subsequent to solubilization. was used with each assay. A range of standards, prepared in triplicate, This involved diluting an aliquot of the stock reference preparation with assay buffer to achieve a final concentration of 5.0 ng/50 ul, and then serially diluting this solution 1:1 with assay buffer 53 to obtain a series of standards ranging in concentration from 5.0 ng/50 ul to 0.01 ng/50 ul. Procedure: Sufficient assay buffer was added to 12 x 75 mm glass tubes, on ice, such that the combined volume of assay buffer and sample or standard totaled 300 ul. Standards and samples were then added to the appropriate tubes. Six tubes were always prepared containing no sample or standard in order to determine maximum binding and non-specific binding. 100 ul of the 1st antibody was then added to all tubes except for the three tubes used to determine non-specific binding. These three tubes received 100 ul of 1st antibody buffer instead. All tubes were then vortexed gently, and allowed to incubate at room temperature for 24 hours. 100 ul of 125 1-rPRL (10,000 cpm/100 ul) was then added to each tube, followed by gentle vortexing. The tubes were then corked and allowed to incubate for an additional 24 hours at room temperature. During this incubation period, the tubes were pre-counted in a Gamma 4000 gamma counter (Beckman). ul of the 2nd antibody was then added to each tube. and incubated for 24 hours at 40C. 100 The tubes were vortexed, The tubes were then centrifuged for 15 minutes, at 40C, at 6,500 x g, in a Beckman J2-21 centrifuge. The supernatant was aspirated off, and the tubes were counted in a Gamma 4000 gamma counter. The percent bound (%B) in each tube was calculated by comparing the final count (B) with the pre-count (BO). This percentage was then corrected for non-specific binding (NSB) according to the following equation: corrected %B = [(%B-%NSB)/(100-%NSB)] x 100 54 The corrected %B for each standard concentration was then plotted on semi-log paper to obtain a standard curve (see figure 2). The amount of rPRL in each sample aliquot was then determined by comparing each sample's corrected %B with the standard curve. lodination of rTSH for Use in Radioimmunoassay Radioiodination of rTSH was achieved through use of the chloramine T reaction, essentially as described by Greenwood, et al. (218). The radioiodinated rTSH was then purified by Sephadex gel chromatography. Iodination Reaction: Reagents: 0.5 M P04, pH 7.4; Phosphate buffered saline (PBS: 0.05 M P04, 0.88% NaCl, pH 7.4); PBS containing 0.2% sodium azide; rTSH (NIADDK-Rat TSH-I-6, 1 ug/2 ul PBS); Sodium Metabisulfite (12.5 mg/10 ml PBS); 2% Bovine serum albumin (BSA) in PBS; 1% BSA in PBS; Chloramine-T (10.0 mg/10 ml PBS); 125 1-Sodium Iodide (New England Nuclear, catalog :#NEZ-033; 1 mCi/100 ul, in 0.1 N NaOH; specific activity 17.4 Ci/mg). Procedure: The iodination reaction was performed in the vial containing the 12 5I-Sodium iodide, in a glove box authorized for use of high levels of radioactivity. After venting the vial, the following reagents were added via 55 12- zD 0 o. 6- 3- .020 .039 .078 .158 .3125 .625 1.25 2.5 NANOGRAMS RAT PRL- RP-3 Figure 2. Typical Standard Curve for Rat Prolactin Radioimmunoassay Each point is the mean of triplicate determinations. 56 5.0 Hamilton syringes: 10 ul 0.5 M P04, 5 ul rTSH, and 10 ul Chloramine-T (prepared just before use, kept on ice, and protected from exposure to light). The vial was then gently shaken for 30 seconds. The reaction was then stopped by the addition of 10 ul sodium metabisulfite and 200 ul 2% BSA in PBS. The entire reaction mixture was then transferred onto a Sephadex G-50 column for isolation of purified 12 5 1-rTSH. Purification of Radioiodinated rTSH: Preparation of Gel: Sephadex G-50 (Pharmacia) was swelled in PBS containing 0.2% sodium azide, overnight, at room temperature. The gel was then poured into a 20 cm high x 0.7 cm diameter plastic Econocolumn (Beckman). bed was 17.5 cm, and the column volume was 6.75 ml. The height of the gel Five column volumes of PBS containing 0.2% sodium azide were immediately run through the column to settle the gel. A few drops of 10% BSA in PBS were then applied to the gel, followed by elution with another 5 column volumes of PBS containing 0.2% sodium azide. A few drops of a Dextran Blue solution (Dextran Blue 2000, 2 mg/ml PBS; Pharmacia) were then run through the column in order to determine uniformity of flow through the column, and the void volume of the column. gel was then eluted with 5 more column volumes prior to application of the iodination reaction mixture. 57 The Gel Chromatography: The iodination reaction mixture was applied to the column and eluted with PBS containing 0.2% sodium azide. Five drop fractions (approximately 200 ul) were collected in 1.5 ml Eppendorf tubes. 1 ul of each fraction was then counted in a Gamma 4000 gamma counter (Beckman) (see figure 3). The fractions representing the first peak in radioactivity were assumed to be 1251-rTSH, and were subsequently checked for binding activity using antiserum to rTSH. Verification of Binding of Radioactive Fractions to rTSH-anti-serum: Aliquots of each fraction comprising the first peak in radioactivity eluted from the Sephadex gel were diluted to 10,000 cpm/100 ul with the assay buffer used in the rTSH radioimmunoassay. Nine diluted 100 ul samples from each fraction were then assayed for binding activity using the same methodology described below for the rTSH radioimmunoassay. For each fraction, triplicate samples were used to determine maximal binding (no competing standard present), non-specific binding (no competing standard and no 1st antibody present), and displacement by rTSH (co-incubation of 1251-rTSH with 100 ng rTSH standard reference preparation). * The fractions demonstrating high maximal binding, low non-specific binding, and ability to be displaced by non-radioactive rTSH were then pooled and used in the rTSH radioimmunoassay. The pooled 12 5 1-rTSH was stored at 40C, and used within 7 days. 58 30- t: .J 0 25 20 0 () 15- x 10 I- 0-01 5 15 10 20 FRACTION Figure 3. Sephadex G-50 Gel Chromatographic Purification of Radioiodinated Rat Thyraid Stimulating Hormone Each fraction contains 5 drops. 1 ul of each fraction was counted. The first peak represents 12 5 1-labelled-rTSH. Each fraction in this peak was subsequently tested for binding activity to antibodies against rTSH, and for displaceability from binding by non-radioactive rTSH. The most active fractions were then pooled for use in the radioimmunoassay. 59 Radioimmunoassay for Rat Thyroid Stimulating Hormone The concentration of rTSH in media and cell samples was determined by double-antibody radioimmunoassay, using standards, primary antibodies, rTSH for iodination, and procedures supplied by the NIADDK. Materials: Samples: Samples were typically assayed in either duplicate or triplicate, and occasionally aliquots of different volume from the same sample were assayed in parallel as a further control for accuracy of results. Assay Buffer: 0.01 M P0 4 , 0.1% Bovine serum albumin (RIA grade; Sigma), 0.14 M NaCl, 0.025 M EDTA, 0.1% sodium azide, pH 7.5. 1st Antibody Buffer: 0.5% Normal rabbit serum (Pel-Freez Biologicals) in assay buffer. 1st Antibody: NIADDK-anti-rTSH-S-5 (C21381), rat thyroid stimulating hormone antiserum (rabbit), dissolved in 2% normal rabbit serum in phosphosaline buffer, was diluted 1:10 with 1st antibody buffer and stored in 0.5 ml aliquots at -200C. Prior to each assay, an aliquot of this solution was thawed and diluted 1:150 with 1st antibody buffer, yielding a final dilution of 1:1,500, and a "final tube dilution" of 1:10,500. 60 2nd Antibody: Goat anti-rabbit IgG (heavy and light chains; Cappel Laboratories, catalog #9112-0081, lot #17808), dissolved in 0.02 M phosphosaline (pH 7.3) containing 0.05% sodium azide, was stored in 500 ul aliquots at -200C. Prior to each assay, an aliquot of this solution was thawed and diluted 1:40 with assay buffer. Tracer: 125 I-rTSH, prepared from NIADDK-rTSH-I-6 as described above, was diluted with assay buffer to obtain a solution containing approximately 5,000 cpm/100 ul. Standards: NIADDK-rTSH-RP-2 (AFP-5153B) was used as the standard reference preparation. Reconstitution of 1 vial with 1 ml dH2 0 yielded a solution containing 5 ug rTSH/ml, in 1% BSA in phosphosaline. 50 ul aliquots of this solution were stored in Eppendorf tubes at -200C, and used within 5 months subsequent to solubilization. was used with each assay. A range of standards, prepared in triplicate, This involved diluting an aliquot of the stock reference preparation with assay buffer to achieve a final concentration of 25 ng/100 ul, and then serially diluting this solution 1:1 with assay buffer to obtain a series of standards ranging in concentration from 25 ng/100 ul to 0.0.5 ng/100 ul. 61 Procedure: Sufficient assay buffer was added to 12 x 75 mm glass tubes, on ice, such that the combined volume of assay buffer and sample or standard totaled 400 ul. Standards and samples were then added to the appropriate tubes. Six tubes were always prepared containing no sample or standard in order to determine maximal binding and non-specific binding. 100 ul of the 1st antibody was then added to all tubes except for the three tubes used to determine non-specific binding. These three tubes received 100 ul of 1st antibody buffer instead. All tubes were then vortexed gently, and allowed to incubate at 40C for 3 days. of 12 5 1-rTSH 100 ul (5,000 cpm/100 ul) was then added to each tube, followed by gentle vortexing. The tubes were then corked and allowed to incubate for an additional 3 days at 40C. On the last day of this incubation, the tubes were pre-counted in a Gamma 4000 gammma counter (Beckman). antibody was then added to each tube. for 24 hours at 40C. 100 ul of the 2nd The tubes were vortexed, and incubated The tubes were then centrifuged for 15 minutes, at 40C, at 6,500 x g, in a Beckman J2-21 centrifuge. aspirated off, and the tubes were re-counted. The supernatant was then The percent bound in each tube, and the amount of rTSH in each sample, were determined as described above in the procedure for the rPRL radioimmunoassay. A typical standard curve for the rTSH radioimmunoassay is displayed in figure 4. Double Antibody Immunoprecipitation of 35 S-Methionine-Labelled-rTSH 'Other than the exceptions noted below, the methodology and reagents used for the double antibody immunoprecipitation of 35 S-methionine-labelled-rTSH were identical to those employed in the rTSH radioimmunoassay. 62 The z 0 10- .025 .05 .10 .20 .39 .8 .iBs 3.125 NANOGRAMS RAT TSH-RP-2 Figure 4. Typical Standard Curve for Rat Thyroid Stimulating Hormone Radioirmmunoassay Each point is the mean of triplicate determinations. 63 ebs concentrations of both antibodies used in this assay were increased 10-fold over those employed in the corresponding radioimmunoassay. It was unnecessary to use standards in this procedure, and 100 ul of assay buffer were added to each tube instead of 100 ul of 125 1-rTSH. Following aspiration of the final supernatant, the pelleted immunoprecipitated rTSH was resuspended in assay buffer instead of being counted. to glass scintillation vials. Aliquots of each sample were then transferred 10 ml of a scintillation cocktail (Instagel; United Technologies/ Packard) was then added to each vial, and the vials were vortexed. The samples were then allowed to incubate for 24 hours at 40C prior to counting in a Packard Tri-Carb 460C liquid scintillation counter. When samples were to be run on polyacrylamide-SDS gels, the pelleted immunoprecipitated rTSH was resuspended in the gel electrophoresis buffer (described below) instead of the radioimmunoassay buffer. 3 5 S-Methionine-Labelled-rTSH Gel Electrophoresis of Immunoprecipitated Gradient SDS polyacrylamide gel electrophoresis of immunoprecipitated 3 5 S-methionine-labelled-rTSH was performed using a modification of procedures described by Chin, et al. (219). Reagents: 1) 30% Acrylamide, 0.8% Bis (N'N'Methylene-bisacrylamide); 2) 20% SDS (sodium lauryl sulfate/ sodium dodecyl sulfate); 3)10% Ammonium persulfate; 4) TEMED (N' ,N' ,N',N',Tetramethylethylenediamine); 64 80 mM Tris-HCl, pH 6.8, 10% glycerol, 0.0024% bromophenol 5) Sample buffer: blue, 2% SDS, 100 mM dithiothreitol; 6) Running buffer: 0.19 M glycine, 0.025 M Tris-base, 0.1% SDS; 7) Running gels: 20% polyacrylamide 10% polyacrylamide Acrylamide/Bis (30%/0.8%) 3.33 ml 6.67 ml Tris-HCl, pH 8.7 (1.5 M) 2.50 ml 2.50 ml SDS (20%) 0.05 ml 0.05 ml H20 4.12 ml 0.78 ml 8) Stacking gel (5% polyacrylamide): 2.51 ml acrylamide/Bis (30%/0.8%); 1.88 ml Tris-HCl, pH 6.8 (1.0 M); 0.075 ml SDS (20%); 10.5 ml H20; 9) Standards: BRL Pre-stained low molecular weight standards: insulin (3000), bovine trypsin inhibitor (6200), cytochrome C (12300), lysozyme (14300), beta-lactoglobulin (18400), alpha-chymotrypsinogen (25700), and ovalbumin (43000) (Bethesda Research Laboratories). Procedure: Immediately before pouring the running gel and the stacking gel, ammonium persulfate (5 ul/ml of the gel) and TEMED (0.5 ul/ml of the gel) were added to the gel mixtures. The 10%-20% polyacrylamide gradient running gel was poured first and allowed to polymerize, and then the stacking gel was poured. A plastic comb was inserted in the top of the stacking gel, prior to polymerization, in order to form wells for the samples. Following polymerization of the stacking gel, the comb was removed, the gel was attached 65 to a vertical gel box, and running buffer was added to the upper and lower chambers of the box. Samples and standards were prepared in sample buffer, and incubated for 5 minutes in boiling H20 prior to placement into the wells of the gel (via Hamilton syringes). The gel was run at 150 V (constant voltage) until the tracking dye reached approximately 1 cm from the bottom of the gel (usually 4.5-5.0 hours). Evaluation of Gels: Following electrophoresis, the gel was removed from the gel box, and sliced into individual lanes. The positions of the pre-stained standards were recorded, and the sample lanes were cut into 1 mm slices. Each slice was then placed in a scintillation vial, to which 1 ml of 30% hydrogen peroxide was added. The vials were then incubated at 500C, in a shaking water bath, for 24 hours, to dissolve the gel slices. 10 ml of a scintillation cocktail (Instagel) was then added to each vial, and the vials were allowed to incubate for 24 hours at 40C. The vials were then counted in a Packard Tri-Carb 460C liquid scintillation counter. Double Antibody Immunoprecipitation of 3 5S-Methionine-Labelled-rPRL Other than the exceptions noted below, the methodology and reagents used for the double antibody immunoprecipitation of 3 5S-methionine-labelled-rPRL were identical to those employed in the rPRL radioimmunoassay. The concentrations of both antibodies used in this assay were increased 10-fold over those employed in the corresponding radioimmunoassay. 66 It was unnecessary to use standards in this procedure, and 100 ul of assay buffer were added to each tube instead of 100 ul of 125 1-rPRL. The treatment of pelleted immunoprecipitated rPRL following aspiration of the final supernatant was identical to that described above in the procedure for double antibody immunoprecipitation of 3 5 S-methionine-labelled-rTSH. Trichloroacetic Acid Precipitation of Proteins Incorporation of 35S-methionine into newly synthesized proteins was examined through scintillation counting of trichloroacetic acid (TCA) precipitated proteins. tube on ice. 100 ul of each sample was placed in a 1.5 ml Eppendorf 900 ul of ice-cold 5.56% TCA was added to each tube. were then incubated on ice for 30 minutes. The samples The samples were then applied to individual 2.3 cm Whatman 3MM filter papers (or to Schleicher & Schuell# 34 glass fiber filter papers) in a multiple sample filtration device (Millipore). The samples were then washed twice with 5 ml of ice-cold 5% TCA, and twice with 2.5 ml of absolute ethanol. The filters were then removed, allowed to dry overnight, and placed in scintillation vials. 10 ml of a scintillation cocktail (Instagel) was then added to each vial, and the vials were counted in a Packard Tri-Carb 460C liquid scintillation counter. Statistics Statistical significance of differences between treatment groups was determined by either Student's t-test (for differences between 2 groups) or 67 analysis of variance (for differences between more than 2 treatment groups), as described elsewhere (184). 68 RESULTS Detection of Specific Binding Protein for 1,25-(OH)7D3 in Rat Anterior Pituitary Prior to examining the regulation of pituitary function by 1,25-(OH)2D3, it was first necessary to verify the presence of the putative receptor for this hormone in rat anterior pituitary. Detection and preliminary characterization of a specific binding protein for 1,25-(OH)2D3 in rat anterior pituitary was achieved through the use of sucrose density gradient sedimentation analysis. Anterior pituitaries were dissected from 20 male Sprague Dawley CD rats (275-300 g) following rapid decapitation. nuclear extracts were then prepared from the pooled tissue. Cytosolic and Cytosolic extracts of mouse intestine and chick intestine were also prepared for use as positive controls. Aliquots of each extract were incubated with 4 nM 3 H-1,25-(0I) 2 D3, 1,25-(OH) 2D3. either alone or in the presence of 200 nM Subsequent to this incubation, unbound sterols were removed by treatment with dextran-coated charcoal. The solutions containing bound hormone were then subjected to sucrose density gradient sedimentation analysis, as described in the Methods section. The results of sucrose density gradient sedimentation analysis of rat anterior pituitary cytosolic and nuclear extracts incubated with 3H-1,25-(OH) 2D 3 are displayed in figure 5. A 3.5-3.7 S specific binding protein for 1,25-(OH) 2 D3 was detected in both cytosolic and nuclear extracts of rat anterior pituitary. Two peaks of radioactivity (3.5-3.7 S and 6.0 S) 69 logo, K A 3.73 C 1.058 3.73 I I lit 4 433 A 1133' .0 ~0 .0 .0 0 S 1233! 33, 0 411' 0 M.34 zig, 0 * A. 0 V 00 C) & 0 0 * * 4 : 4W q S. 3.33 B - I. D 3.73 1M' 433 33m - 33. 331 43. 0 .0 . .'.!.| .. .... A. 1 I 10 15 20 25 38 S is 15 20 25 31 FRACTION Figure 5. Sucrose Density Gradient Sedimentation Analysis of Rat Anterior Pituitary Cytosolic and Nuclear Extracts Incubated with 3H-1,25-(OHbD3 (A) Chick intestinal cytosol (positive control); (B) mouse intestina cytosol (positive control); (C) rat anterior pituitary cytosolic extract; (D) rat anterior pituitary nuclear extract. In each case (A through D), aliquots from the same sample were incubated with 3H-1,25-(OH) 2 D 3 , alone (solid line) or together with a 50-fold excess of non-radioactive 1,25-(OH) 2 D3 (broken line). Sedimentation coefficients assigned to peaks were estimated from known protein standards (bovine serum albumin, 3.7 S; ovalbumin, 4.4 S) which were run in parallel gradients. 70 were observed in the sedimentation profile of rat anterior pituitary cytosolic extract incubated with 3H-1,25-(OH) 2D3 . The 3.5-3.7 S peak was not apparent when a 50 fold excess of non-radioactive 1,25-(OH) 2 D3 was included in the incubation, thus demonstrating the specificity of this binding protein for 1,25-(OH) 2D3. Binding of 3 H-1,25-(OH) 2 D3 to the 6.0 S protein could not be inhibited by similar treatment with excess 1,25-(OH)2D3. This 6.0 S non-specific binding protein has been detected previously in many receptor positive tissues (41,87,88), and is believed to be a complex of the 4.0 S plasma vitamin D binding protein and some unknown cytosolic protein. Determinination of Binding Characteristics Binding studies were performed in order to determine whether the binding characteristics of the specific binding protein for 1,25-(OH) 2 D3 in rat anterior pituitary were similar to those previously reported for the 1,25-(OH) 2 D3 receptor present in other target tissues. The binding characteristics of the putative rat anterior pituitary cytosolic receptor for 1,25-(OH) 2 D3 were examined via a competitive binding assay. The resulting data was subjected to Scatchard analysis (181) in order to determine the dissociation constant (Kd), number of binding sites (Bmax), and presence of singular or multiple classes of binding sites (e.g., high affinity and low affinity). The results of the competitive binding assay employing 1,25-(OH)2 D3 and its tritiated analog are displayed in figure 6. The curve representing specific binding indicates that binding was saturable. 71 Scatchard analysis of Total - 30 '.4 0 0 25 4J 0 20 '4 '.4 9-4 Non-Specific 15 Specific 10 rn' 5 9 1 2 3 4 2 3 4 2 a TOTAL 3H-1,25-(OH) 2 D 3 (nM) Figure 6. Competitive Binding Assay Employing 3 H-1,25-(OH)D3. 1,25-(H)D3, and Rat Anterior Pituitary Cytosol The curve representing specific binding was determined by subtracting values for non-specific bound from those for total bound at each point in the curve. 72 this data is displayed in figure 7. The observed Kd, calculated as the negative reciprocal of the slope (slope = -1/Kd), was 6.0 x 10-10M. The approximate Bmax, as indicated by the x-intercept, was 37 fmol/mg protein. Linear regression analysis of the data yielded a correlation coefficient of -0.9777, indicating the presence of a single class of receptors. All of this data is in good agreement with previous reports by others concerning the binding characteristics of the rat anterior pituitary receptor for 1,25-(OH)2D3 (113,142,145). Recovery of Viable Cells in Culture The number and percentage of viable cells recovered from the enzymatic dispersion procedure, and subsequently plated in culture, were examined in order to assess the efficacy of this method for obtaining viable enzymatically dispersed rat anterior pituitary cells for use in primary culture. Immediately prior to seeding cultures, an aliquot of the final cell suspension was diluted with a trypan blue dye solution, and examined under a microscope. Cell number was determined using a hemocytometer. Cell viability was determined by the trypan blue dye exclusion test (176). The percentage of viable cells recovered from the enzymatic dispersion procedure was then calculated. The enzymatic dispersion method used to establish primary cultures of rat anterior pituitary cells yielded greater than 95% viable cells. Figure 8 is a photograph of these cells in culture 1 hour subsequent to seeding at a concentration of 3-5 x 105 cells/ml. 73 .24.22- Ken 6.0 x 10', M .20B~8 5' 37 S..l I.meprotein .18 0 .14 8 F 0 .12 q .06 4 .04.021 20 40 60 80 8 100 120 140 180 (pM) Figre 7. Scatchard Analysis of Binding Data The data presented in figure 13 was subjected to Scatchard analysis. B = bound ligand; F = free ligand. Bmax was calculated from the x-intercept, taking into account the protein content of the cytosol used in this assay (as determined by the method of Lowry). Kd was calculated as -1/slope. 74 Figure 8. Photograph of Cells in Culture 1 Hour Subsequent to Seeding Cel s were seeded at a concentration of 3-5 x IOD cells/mi. Greater than 95% of the cells were viable, as determined by the trypan blue dye exclusion test. 75 Viability and Functionality of Cells in Culture The viability and functionality of enzymatically dispersed rat anterior pituitary cells in primary culture was examined in order to determine the efficacy of the cell culture method employed to study regulation of pituitary function by 1,25-(OH) 2 D3. Cell viability under the culture conditions employed in these studies was determined by trypan blue dye exclusion. The number and percentage of viable cells was assayed in triplicate cultures at 24 hour intervals for six days. cell suspension. All cultures were seeded from the same initial Cultures were maintained in serum-supplemented medium for the first four days, and in serum-free medium for the last two days. There was no significant change in the number or percentage of viable cells at any of the time points examined. In addition to being viable, it was important to determine that the cultured cells were functionally intact. This was achieved by examining basal hormone secretion over the first four days in culture, and responsiveness to known secretogogues during the final two day serum-free test period. Radioimmunoassay of media samples from day 0 and day 4 revealed that basal hormone secretory capacity was intact (figure 9). Elevation of media potassium concentration is known to stimulate hormone secretion by functionally intact pituitary cells in culture (168). Enzymatically dispersed rat anterior pituitary cells were therefore maintained for four days in a serum-supplemented medium, and then incubated for 3 hours in either the control serum-free medium (Ham's F10), or a high potassium test medium (Ham's F10 supplemented with sufficient potassium to yield a 10 fold 76 >100 20 ' c5 16 z12 DAY Fligure 9. Basal Secretion of Rat Prolactin From Enzymatically Dispersed Rat Anterior Pituitary ueiis in Primary Culture Aliquots of conditioned media were removed from cultures after 4 days of incubation, and assayed for rPRL content via radioimmunoassay. values were compared with those obtained from aliquots of culture mediumThese taken just prior to addition to cultures (day 0). 77 increase in concentration). The cells incubated in the high potassium medium responded to the treatment by secreting significantly increased amounts of both rPRL (figure 10) and rTSH (figure 11) into the medium. Effects of TRH on Secretion of TSH Since elevation of medium potassium concentration is a relatively non-specific secretory stimulus, and since the function of rat thyrotropes was to be a major focus of this thesis, it was important to determine that the sub-population of TSH-secreting cells present in these primary cultures were capable of responding normally to a more specific secretogogue. This was achieved by examining the effects of thyrotropin-releasing hormone (TRH) on TSH secretion. Cultures of enzymatically dispersed rat anterior pituitary cells were maintained for four days in a serum-supplemented medium, which was then replaced with a serum-free test medium. Sets of cultures were pre-incubated in the test medium for one hour, and then incubated for either 1 hour, 12 hours, 24 hours, or 48 hours. During the last hour of incubation prior to each of the time points, sets of cultures were treated with either TRH (at a final concentration of 0.1 uM) or vehicle. At each of the time points examined, 1 hour of treatment with 0.1 uM TRH resulted in significantly increased concentrations of TSH in the medium, as determined by radioimmunoassay (figure 12, table 4). points. The amplitude of this effect was similar at all of the time These results demonstrated that the sub-population of TSH-secreting cells present in these heterogeneous primary cultures were capable of responding normolly to a well-characterized specific secretogogue. 78 1.4 1.2 S1.0 cc IL 0.8 0.6 0 z 0.4 z 0.2- CONTRSL g.5 V x* n - 3; a:p <0.05 Figure 10. Effect of Increased Media Potassium Concentration on rPRL Secretion Cultures of enzymatically dispersed rat anterior pituitary cells seeded from-ttie same initial cell suspension were maintained for 4 days in a serum-supplemented medi.uni, which was then replaced with a serum-free medium containing. either normal (control) or 10-fold increased (0.5M K+) potassium concentration. Following a 3 hour test incubation period, media samples were removed cultu're and assayed for rPRL content from each by radioimmunoassay. 79 1.41 1.2 1.0 0.8 S0.60- ~0 0 a Q4 O .40.2- 0 -. n - ME 3; a: p < 0.05 Figure 11. Effect of Increased Media Potassium Concentration on rTSH Secretion Cultures of enzymatically dispersed rat anterior pituitary cells seeded from the same initial cell suspension were maintained for 4 days in a serum-supplemented medium, which was then replaced with a serum-free medium normal (control) or 10-fold increased (0.5M K+) potassium containing either Following a 3 hour test incubation period, media samples concentration. culture and assayed for rTSH content by radioimmunoassay. were removed from each 80 0 z0.4- 0.1 uM TRH 0 VEHICLE 0.3. 0.2 0.1- 01 12 24 48 TIME (HOURS) each value is mean + SEM; 2 way ANOVA: effect of TRH: p <.005 effect of time: interaction: p < .005 NS Figure 12. Effects of TRH on Secretion of TSH Following 4 days of incubation in a serum-supplemented medium, sets of cultures were pre-incubated for 1 hour in a serum-free medium, followed by test incubations lasting for the indicated durations. One hour prior to each time point, sets of cultures were treated with either TRH, at a final concentration of 0.1 uM (solid circles), or vehicle (open circles). Media samples were removed at the end of each test period, and subsequently assayed for rTSH content via radioimmunoassay. Cellular protein content was determined by the method of Lowry. 4-6 cultures were examined at each point in the figure. 81 rTSH IN MEDIUM (ng/ug protein) VEHICLE 0.1 uM TRH 0 12 hr 24 hr 48 hr 0.10 + 0.02 0.13 + 0.02 0.20 + 0.03 0.21 + 0.05 (5) (4) (5) (6) 0.18 + 0.04 0.19 + 0.03 0.29 + 0.04 0.30 + 0.03 (5) (6) (6) (5) each value is mean + SEH; 2 way ANOVA: n in parentheses. effect of TRH: effect of time: p < .005 p < .005 interaction NS Table 4.. Effects of TRH on Secretion of TSH FollOwing 4 days of incubation in a serum-supplemented medium, sets of cultures were, pre-incubated for 1 hour in a serum-free medium, followed by test incubations lasting for the indicated durations. One hour prior to each time point, sets of cultures were treated with either TRH, at a final concentration of 0.1 uM, or vehicle. Media samples were removed at the end of each test period, and subsequently assayed for rTSH content via radioimmunoassay. Cellular protein content was determined by the method of Lowry. 82 Effects of 1,25-(OH)2D3 on the Growth of Rat Anterior Pituitary Cells in Primary Culture Given the lack of any previous information concerning the effects of 1,25-(OH) 2 D 3 on the function of non-transformed rat anterior pituitary cells in primary culture, and the numerous recent reports of effects of this seco-steroid on the growth of other receptor-positive cell types in culture (186 -196), it was of interest to determine whether the active hormonal form of vitamin D might similarly affect the growth of receptor-positive rat anterior pituitary cells. Several gross parameters of cell growth were examined. Cultures of enzymatically dispersed rat anterior pituitary cells were maintained for four days in a serum-supplemented medium, which was then replaced with a serum-free test medium (Ham's F10). Following a one hour pre-incubation period, sets of cultures were treated with either 1,25-(OH) 2 D3 (at final concentrations ranging from 1O- 7M to 10-1 3M) or vehicle. The cultures were then incubated for test periods ranging from 6 hours to 48 hours. At various time points, sets of cultures were removed from the incubator, photographed, and separated into cellular and media samples. The samples were kept frozen at -200C prior to being assayed for protein content and DNA content. No generalized quantitative effect of 1,25-(OH)2D3 was observed on cellular protein content (figure 13), cellular DNA content (figure 14), or gross cellular morphology (figure 15), regardless of the dose of 1,25-(OH)2 D3 administered, or the time of incubation. Although these results fail to support the hypothesis that 1,25-(OH)2D3 might affect the growth of 83 o 107% 1,25-() 2-D 0 VEHICLU so 3 46 ~42a 34 a 0 6 9 12 is 24 49 TIME (hours) Figu'e 13. Effects of 1,25-(OH)2D3 on Cellular Protein Content A-time course experiment was performed with sets of cultures being incubated in the presence of either 10- 8 M 1,25-(OH) 2 D3 (open circles) or vehicle (closed circles). Cell samples were assayed for protein content by the method of Lowry. Each point represents the mean + SEM for six cultures. Values for each time point were compared using Student's t-test. No significant differences were observed at any time point. 84 6.812 HOURS 5.2- 4.4 a 6 HOURS 3.6 2.8 C -13 -11 -9 LOG [1,25-(OH) 2-D -8 3 -7 (M) Figure 14. Effects of 1,25-(OH)2D3 on Cellular DNA Content Sets of cultures were incubated for either 6 hours (open circles) or 12 hours (closed circles) in the presence of various doses of 1,25-(OH)2 D3 or vehicle. Cell samples were assayed for DNA content using the diphenylamine method of Burton. Each point represents the mean + SEM for six cultures. Regardless of the dose of 1,25-(OH) 2 D3 employed, no statistically significant difference in cellular DNA content was observed at either time point (as determined by analysis of variance). 85 ............ ..... ....... - - " r _ 8 C E F G I J K A I I a I H Figure 15. Effects of 1,25-(OH)2D3 on Gross Cellular M~rpholog) Sets ot cult-ures were maintained in tne presence of Mom~5 I,5-uH) 2D3 (+) or vehicle (0) for periods of time lasting as long as 24 hours. Photographs of the cells were taken at various time points. No obvious morphological differences were observed in treated vs. control cultures at any time point. (A) Immediately following 1 hour pre-incubation in serum-free medium (to); 6 hours, 0; (C) 6 hours, +; (D) 9 hours, 0; (E) 9 hours, +; (F) 12 hours, 0;(B) (G) 12 hours, +; (H) 18 hours, 0; (I) 18 hours, +; (J) 24 hours, 0; (K) 24 hours, +. 86 receptor-positive rat anterior pituitary cells, neither do they contradict such a possibility. The problem with interpreting these results lies in the fact that the experimental model employed in these studies is poorly suited for observing effects on cell growth which are not gross or generalized.- Most studies of cell growth employ cultures which are homogeneous in nature. The heterogeneous nature of the cell population used in the present studies may have thus seriously confounded the results. Possible effects on the growth of specific sub-populations of cells may have been masked by examining the entire heterogeneous population simultaneously. In addition, the possibility of qualitative changes in either protein synthesis or DNA synthesis induced by treatment of these cells with 1,25-(OH)2D3 cannot be ruled out. Such changes could only be detected, however, by using a homogeneous cell population and assays designed to reveal qualitative changes in DNA or protein content. Similarly, possible effects of 1,25-(OH)2D3 on movement of cells through different phases of the cell cycle could not be examined with a heterogeneous cell population, except in the unlikely event that all sub-populations of cells present were similarly affected. Effects of 1,25-(OH)7D3 on Content of rPRL in Cells and in Media The only previous investigations of responses induced by treatment of rat anterior pituitary cells with 1,25-(OH)2D3 involved use of clonal rat pituitary tumor cells (114,139,146-148,198). As discussed earlier, these transformed cells differ from non-transformed rat anterior pituitary cells in a number of significant ways. It was therefore important to determine whether 87 non-transformed rat anterior pituitary cells in primary culture respond to 1,25-(OH) 2 D3 in a similar fashion as do their transformed counterparts. This issue was of further interest due to the contradictory results reported from various laboratories, which most likely resulted from the use of different strains of clonal rat pituitary tumor cells, and different cell culture conditions. In different laboratories, treatment of rat pituitary tumor cells with 1,25-(OH)2D3 had thus been reported to both stimulate (139) and inhibit (114) secretion of rPRL from different strains of GH cells, under different cell culture conditions. Cultures of enzymatically dispersed rat anterior pituitary cells were maintained for four days in a serum-supplemented medium, which was then replaced with a serum-free test medium (Ham's F10). Following a one hour pre-incubation period, sets of cultures were treated with either 1,25-(OH)2D3 (at a final concentration of 10- 8 M) or vehicle. A time course experiment was then initiated, with sets of treated and control cultures being incubated for either 6,9,12,18,24, or 48 hours. Media and cell samples were collected at each time point, separated, and frozen at -200C prior to determination of rPRL content via radioirnmunoassay. Although some early transient effects were observed, there was no sustained significant effect of 10-8M 1,25-(OH)2D3 on either media or cellular content of rPRL (figures 16-19). Effects of 1,25-(OH)2D3 on Content of rTSH in Cells and in Media . Several reports in the literature suggested that 1,25-(OH) 2 D3 might somehow affect the function of TSH-secreting cells in the rat anterior 88 0 T03 .3 - 10M 1,25-(OH) 2 -D 3 VEHICLE , 0.26-b 0.22a 0.18 0.14- 0.10- 0.06 1 0 6 9 12 7 is 24 49 TIME (hours) a: p < 0.025 b: p < 0.005 Figure 16. Effects of 1,25-(OH)2D3 on Cellular rPRL Content (ng/ug protein) Sets of cultures were incubated for various periods of time in the presence of either 10-8M 1,25-(OH) 2 D3 (open circles) or vehicle (solid circles). The content of rPRL in cell samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. 89 o 10M 0 0.30 1.25-(OH) 2 -D 3 VEHICL3 C 0.25- 0.200 0.15- 0.10- 0.050 6 9 12 01 24 .4 TIME (hours) a: p < 0.05 Figure 18. Effects of 1,25-(OH)203 on Media rPRL Content (ng/ug protein) Sets of cultures were incubated for various periods of time in the presence of either 10- 8M 1,25-(OH) 2D3 (open circles) or vehicle (solid circles). The content of rPRL in media samples from each time point was radieimmunoassay. Cellular protein content was determined by Lowry. Each value represents the mean + SEM of six cultures. treated and control cultures at each time point were compared t-test. 91 determined by the method of Values from using Student's a 1800 1600 140. 8 AVT 120 dP 100 80 60 40 I I 0 6 I 9 I 12 I- 18 24 I 48 TIME (hours) a: p < 0.05 Figure 19. Effects of 1,25-(OH)2D3 on Media rPRL Content (" control) Sets of cultures were incuDated Tor various periods of time in the presence of either 10- 8 M 1,25-(OH) 2 D3 (open circles) or vehicle (solid circles). The content of rPRL in media samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. pituitary. Most notably, a study employing combined autoradiography and immunohistochemistry (140) demonstrated that 3 H-1,25-(OH) 2 D3 localizes exclusively in the nuclei of rat thyrotropes, and not in rat anterior pituitary cells staining positively for PRL, growth hormone, or leutinizing hormone. It was therefore of great interest to determine whether 1,25-(OH)2D3 was capable of altering rTSH secretion in primary cultures of enzymatically dispersed rat anterior pituitary cells. In addition, this was an experiment which could not be performed using commercially available clonal rat pituitary tumor cells, because these cells only secrete PRL and/or growth hormone. Cultures of enzymatically dispersed rat anterior pituitary cells were maintained for four days in a serum-supplemented medium, which was then replaced with a serum-free test medium (Ham's F10). Following a one hour pre-incubation period, sets of cultures were treated with either 1,25-(OH) 2 D 3 (at a final concentration of 10- 8 M) or vehicle. A time course experiment was then initiated, with sets of treated and control cultures being incubated for either 6, 9, 12, 18, 24, or 48 hours. In a separate experiment, sets of cultures were pre-incubated for one hour in the serum-free test medium, and then treated with either vehicle or various doses of 1,25-(OH)2D3, with final concentrations ranging from 10-1 2M to 10- 8 M. for 48 hours. These latter cultures were incubated Media and cell samples were collected at the end of each incubation period, separated, and frozen at -200C prior to determination of rTSH content via radioimmunoassay. Treatment with 10- 8 M 1,25-(0H)2D3 resulted in a sustained significant increase in media rTSH content (figures 20-23). As was the case with' rPRL content, early transient alterations in rTSH content of media and cell 93 W 2.01. C -.4 o 10 * VEHICLE m 1,25-(OH) 2-D3 1. - C6 1.4 1.2.. 1.00.80 0.6 a 0 6 9 12 1I 24 -A U 46 TIME (hours) Figure 20. Effects of 1,25-(OH)2D3 on Cellular rTSH Content (ng/ug protein) Sets 'of cultures were incubated for various periods of time in the presence of either 10- 8 M 1,25-(OH) 2 D3 (open circles) or vehicle (solid circles) The content of rTSH in cell samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. 94 0-4f . 160 140 *1 8 :B 120 100 80 -r TA .I 60 0u 6 9 12 18 TIME Figure 21. 24 4 48 (hours) Effects of 1,25-(OH)2D3 on Cellular rTSH Content (% control) Sets of cultures were incubated Tor various periods of time in the presence of either 10-8M 1,25-(OH) 2 D3 (open circles) or vehicle (solid circles). The content of rTSH in cell samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. 95 a 0 1o-aH 1,2S-(On) -0 2 3 C 3.0 VEHICLZ , b S2.0 0 1.0 0 q 12 is 24 TIME 48 (hours) a: p < 0.0005 b: p < 0.025 Figure 22. Effects of 1,25-(OH)2D3 on Media rTSH Content (ng/ug protein) Sets of cultures were incubated for various periods of time in the presence of either 10- 8 M 1,25-(OH) 2 0 3 (open circles) or vehicle (solid circles). The content of rTSH in media samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. -Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. 96 180. 0 U b a 160 140 120- 8 100 -L E- 8060. I I - 0 6 I 9 12 I U 18 24 - T 48 TIME (hours) a:p < 0.0005 b:p < 0.025 Figure 23. Effects of 1,25-(OH)2D3 on Media rTSH Content (% control) Sets of cultures were incubated for various periods of time in the presence of either 10- 8 M 1,25-(OH) 2 D3 (open circles) or vehicle (solid circles). The content of rTSH in media samples from each time point was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Values from treated and control cultures at each time point were compared using Student's t-test. 97 samples were also observed. Following longer periods of incubation, however, media rTSH content remained significantly elevated, unlike the effects observed for rPRL. The effect of various doses of 1,25-(OH)2D3 on media rTSH content was examined, and no significant effect was observed at doses lower than 10-8M (figure 24). In order to determine the structural specificity of the effect of 1,25-(OH)2D3 on rTSH secretion, sets of cultures prepared according to the same protocol used in the previous experiment were incubated for 24 hours in the presence of either 10- 8 M 1,25-(OH) 2 D3, vehicle, or a variety of concentrations of 10,25-(OH)2D3 (at final concentrations of 10- 8 M, 1o-7M, or 10- 6 M), an analog of 1,25-(0H) 2 D3 which had been demonstrated to be biologically inactive in other target tissues. Media and cell samples were collected, and rTSH content determined via radioimmunoassay. As shown in figure 25, all doses of 1 ,25-(OH)2 D3 failed to alter either cellular or media content of rTSH. These results further supported the hypothesis that 1,25-(OH)2D3 is capable of stimulating rTSH secretion via a direct receptor-mediated effect. Effects of 1,25-(OH)2D3 on Synthesis of rTSH Although cellular content of rTSH was not statistically significantly elevated by treatment with 10- 8 M 1,25-(OH) 2 D3, it remained possible that 98 - 140 120 - :. 100 8 80 .. 19 I C 1 -12 - 60 -11 -10 -9 -8 LOG [1,25-(OH) 2-D3 1 (M) a: p < 0.05 Figure 24. Effects of 48 Hour Treatment with Various Doses of 1,25-(OH)2D3 on Media rTSH Content Sets of cultures were incubated for 48 hours in the presence of a variety of concentrations of 1,25-(OH)2D3 or vehicle (C). The content of rTSH in media samples from each culture was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Content of rTSH was calculated in terms of ng rTSH/ug protein, and then converted into % control. Each value represents the mean + SEM of four cultures. 99 5.0 a .,3 4.0" 0 3.0 @ 2.0" 1.0T V -8 -8 A B -7 B -6 V B -8 A MEDIA -8 B -7 B -6 B CELLS V: Vehicle; A: 1,25-(OH) D ; B: 1,25-(OH)2 2 3 D3 Numbers are -log of the concentration of the compound (M). a: p < 0.005. Figure 25. Effects of 1s,25-(OH)2D3 on Media and Cellular rTSH Content Sets of cultures were incubated for 24 hours in the presence of either_10-8 M 1,25-(OH)2D3, vehicle, or a variety of concentrations of 1$,25-(OH)2D3. The content of rTSH in media and cell samples was determined by radioimmunoassay. Cellular protein content was determined by the method of Lowry. Each value represents the mean + SEM of six cultures. Statistical significance of differences between eaci treatment group and control was determined using Student's t-test. 100 1,25-(OH)2D3 was capable of stimulating synthesis of new rTSH, an effect whose magnitude might be too small to be observed against the background of total cellular rTSH content. To investigate this possibility, the effects of 1,25-(OH) 2 D 3 on incorporation of 3 5S-methionine into newly synthesized rTSH was examined. Cultures of enzymatically dispersed rat anterior pituitary cells were maintained for four days in a serum-supplemented culture medium, which was then replaced with a serum-free test medium (Ham's F10). Following a one hour pre-incubation period, sets of cultures were treated with 35 S-methionine (70 uCi/well) and either 1,25-(OH) 2 D3 (at a final concentration of 10- 8 M) or vehicle. The cultures were then incubated for 24 hours, after which time media and cell samples were collected, separated, and frozen at -200C prior to assays. Cell samples were subsequently assayed for content of 3 5 S-methionine-labelled-rTSH procedure. using a double-antibody immunoprecipitation This assay revealed that 24 hours treatment with 10- 8 M 1,25-(OH) 2 D 3 had resulted in significantly increased incorporation of 3 5 S-methionine into newly synthesized immunoprecipitatable rTSH (table 5). In order to confirm that the immunoprecipitated material was in fact rTSH, both treated and control samples were subjected to gel electrophoresis on 10-20% gradient polyacrylamide gels containing 0.1% SDS. Two peaks of radioactivity were observed in the gels, corresponding to the 18,000 MW alpha and 22,000 MW beta subunits of rTSH. The radioactivity in both of these peaks was increased in samples from cultures which had been treated with 1,25-(OH) 2 D 3 (figure 26,..t'able 6). 101 IMMUNOPRECIPITATED 35S-METHIONINE-rTSH CPM/SAMPLE VEHICLE CPM/ ug PROTEIN 4110 + 197 208 + (7) 10- 8 m 1,25-(OH) 2 -D 3 12 (7) 6041 + 685 a 319 (7) + 44 b (7) each value is mean + SEM; n in parentheses. a) Student's t-test: p <.005 b) Student's t-test: p <.025 Table 5. Effects of 1,25-(OH)2D3 on Incorporation of 35 S-Methionine into'Newly Synthesized Immunoprecipitatable rISH Sets of cultures were incubated for 24 hours in the presence of 3 5 S-methionine (70 uCi/culture) and either 10- 8 M 1,25-(OH) 2 0 3 or vehicle. Cellular content of 35S-methionine-labelled-rTSH was determined by liquid scintillation counting of double-antibody immunoprecipitated material. 102 C 0 I. Sn I 600. - 5000 10-8M 1,25-(OH) 2 -D 0 CONTROL 3 400- 300. 200. 100 5 10 15 20 25 30 35 GEL SLICE (1 mm) Figure 26. Gel Electrophoresis of Immunoprecipitated abJS-MKethionine-Labelled-rTSH Typical profiles of radioactivity observed in 10%-20% gradient polyacrylamide gels containing 0.1% SDS following electrophoresis of double-antibody immunoprecipitated material from cellular samples of cultures treated for 24 hours with either 10-8M 1,25-(OH) 2D3 (solid circles) or vehicle (open circles). 103 CPM ADDED TOTAL CPN IN CEL RECOVERY CPM IN TSH PEAKS 2 OF RECOVERED CPM IN TSH PEAKS CONTROL 4100 1714 41.82 1351 78.82 1,25-(OH) 2-D3 6000 2538 42.3Z 2102 82.82 * cpm in duplicate innunoprecipitates resolubilized in buffer and counted. Table 6. Recovery of Radioactivity Added to Gel Following Electrophoresis of Immunoprecipitated JbS-Methionine- Label led-rTSH Typical profile of recovery and distribution of radioactivity added to gel. 104 In order to determine whether this effect was specific for rTSH, aliquots of the same samples were assayed for content of 35 S-methionine-labelled-rPRL. A similar double-antibody immunoprecipitation procedure was employed for this assay. Treatment with 10- 8 M 1,25-(OH)2D3, in this case, failed to produce any significant difference in incorporation of 35 S-methionine into newly synthesized rPRL (table 7). As an additional check on the specificity of the effect, the incorporation of 35 S-methionine into TCA-precipitatable proteins was examined. Once again, treatment with 10- 8 M 1,25-(OH) 2 D3 failed to produce any significant difference in incorporation of 3 5 S-methionine into newly synthesized TCA-precipitatable protein, thus ruling out any generalized non-specific effect of the seco-steroid on protein synthesis (table 8). Finally, in order to determine the structural specificity of 1,25-(OH)2D3 for stimulation of rTSH synthesis, sets of cultures prepared according to the same protocol described above were incubated for 24 hours with 3 5 S-methionine and either 10- 8 M l,25-(OH) 2 D 3 , vehicle, or a variety of doses of 1,25-(OH)2 D3 (ranging in final concentration from 10- 8 M to . 10- 6 M), a biologically inactive structural analog of 1,25-(OH) 2 D 3 Although this analog differs only slightly in structure from 1,25-(OH) 2 D3 (the 1-hydroxyl group being in the beta position instead of alpha), it has been found to not compete for binding to the 1,25-(OH) 2 D3 receptor, and to lack biological activity in other well-characterized 1,2 5 -(OH)2D3-receptor systems. As shown in figure 27, double-antibody immunoprecipitation of newly synthesized 3 5 S-methionine-labelled-rTSH revealed that all concentrations of 10,25-(OH)2D3 were incapable of stimulating synthesis of rTSH. 105 IMMUNOPRECIPITATED 35S-METHIONINE IABELED rPRL CPM/SAMPLE VEHICLE 107 M 1,25-(OH) 2-D3 each value is mean Student's t-test: CPM/ug PROTEIN 570 + 20 58.4 + 3.6 (6) (6) 625 + 50 64.2 + 6.6 (6) (6) + SEM; n In parentheses. NS Table 7.. Effects of 1,25-(OH) D3 on Incorporation of 35 S-Methionine into Newly Synthesized Immunoprecipitatable rPRL Sets-of cultures were incubated for 24 hours in the presence of 3 5 S-methionine (70 uCi/culture) and either 10-8M 1,25-(0H) 2 D3 or vehicle. Cellular content of 35 S-methionine-labelled-rPRL was determined by liquid scintillation counting of double-antibody immunoprecipitated material. 106 TCA-PRECIPITATED 3SS-METHIONINE LABELED PROTEINS CLASS FIBER FILTERS 3MN FILTERS CPM/SAMPLE 2010 + 200 VEHICLE (6) 2277 + 181 10OH 1,25-(OH)2-D3 (6) CPM/ug PROTEIN CPM/SAMPLE CPM/ug PROTEIN 1048 + 148 808 + 172 397 + 70 (6) (6) (6) 1210 + 142 (6) 918 + (6) 180 498 + 116 (6) each value is mean + SEM; n In parentheses. Student's t-test: HS Table 8. Effects of 1,25-(OH)2D3 on Incorporation of 3 5 S-Methionine into Newly Synthesized TCA-Precipitatable Proteins Sets of cultures were incubated for 24 hours in the presence of 3 5 S-methionine (70 uCi/culture) and either 10- 8 M 1,25-(OH) 2 D 3 or 5 vehicle. Cellular content of 3 S-methionine-labelled-proteins was determined by liquid scintillation counting of TCA-precipitated material. Two different filter systems were used in the precipitation procedure, both producing similar results. 107 4000 a 3500" 3000 2500 V -8 A -8 B -7 B -6 B V: Vehicle; A: 1,25-(OH) 2 D3 ; B: lU,25-(OH) 2 D 3 ; Numbers are -log of the concentration of the compound (M). a:p <0.025. Figure 27. Effects of 10,25-(0H)ZD3 on Incorporation of 35 S-Methionine into Newly Synthesized Immunoprecipitatable rTSH Sets of cultures were incubated for 24 hours in the presence of 3 5 S-methionine (70 uCi/culture) and either 10-8M 1,25-(OH) 2D3, vehicle, or a variety of concentrations of 10,25-(0H) 2 D3. Cellular content of 3 5 S-methionine-labelled-rTSH was determined by liquid scintillation counting of double-antibody immunoprecipitated material. Each value represents the mean + SEM of six cultures. Statistical significance of differences between each treatment group and control was detennined using Student's t-test. 108 DISCUSSION Prior to the studies described in this thesis, no investigations had been performed concerning the direct effects of 1,25-(OH)2D3 on the function of non-transformed anterior pituitary cells. Several in vivo studies had been conducted revealing changes in pituitary hormone secretion following administration of 1,25-(OH)2D3 or other vitamin D metabolites, but none had unequivocably demonstrated a direct receptor-mediated response induced following activation of anterior pituitary receptors for 1,25-(OH) 2 D3 . According to the classical pharmacological definition, a receptor macromolecule must specifically bind a ligand, with this interaction producing a biological response. Although a specific binding protein for 1,25-(OH) 2 D3 had been identified in anterior pituitaries of several species, there had been no reports of responses induced by the ligand-binding protein interaction. Many specific binding proteins have previously been identified which are not receptors. Transport proteins and storage proteins are two examples. receptors are usually tissue-specific. Furthermore, It is thus impossible to conclude that a specific binding protein is a receptor simply because it specifically binds a ligand. The data described in this thesis thus represents the first conclusive evidence that the specific binding protein for 1,25-(OH) 2D3 present in non-transformed rat anterior pituitary cells is a receptor. The existence of a receptor for 1,25-(OH)2D3 had been previously demonstrated in various strains of clonal rat pituitary tumor cells. For several reasons, however, it was not possible to conclude that the specific binding protein for 109 1,25-(OH)2D3 present in non-transformed rat anterior pituitary cells was a receptor on the basis of these reports. Since receptors are often tissue-specific, the existence of a receptor protein in clonal pituitary tumor cells does not necessarily imply that this receptor is expressed in non-transformed cells of similar origin. Neoplastic cells, by nature, express many proteins not seen in their non-transformed counterparts. In addition, the particular tumor cells used in these studies differ from non-transformed rat anterior pituitary cells in several significant respects. The distribution of calcium among intracellular compartments, and the size of the pool of stored intracellular calcium, have been reported to be different in GH cells as compared with non-transformed rat anterior pituitary cells (238). It has also been found that, unlike normal pituitary cells, GH cells do not store hormones following synthesis (239). GH cells. Secretion is thus completely linked to synthesis in Furthermore, while normal pituitary cells only synthesize and secrete individual types of hormones, GH cells are capable of synthesizing several different hormones simultaneously (an indication of inappropriate expression of proteins)(240). Finally, and of particular interest to the work described herein, GH cells do not secrete TSH. Sar, et al. This is significant due to the report by (140), demonstrating through combined autoradiography and immnunohistochemistry that radioactivity from 3 H-1,25-(OH) 2 D3 can only be detected in the nuclei of rat anterior pituitary cells staining positively for rTSH. Even if these significant differences were to be ignored, one must still view any attempts to extend the findings in tumor cells to non-transformed cell physiology with skepticism simply on the basis of the lack of consistency in the 110 responses observed in different laboratories, using different strains of cells and different cell culture conditions. It was therefore reasonable to speculate that although the same receptor protein may have been expressed in both clonal rat pituitary tumor cells and their non-transformed counterparts, the differences in expression of other cellular proteins might lead to significant differences in the responses observed following activation of the receptor in these cells. Activation of the receptor for 1,25-(OH) 2 D3 present in a sub-population of non-transformed rat anterior pituitary cells was observed to result in stimulation of both synthesis and secretion of rTSH. The specific nature of the effect was indicated by the lack of any effect of this seco-steroid on synthesis or secretion of rPRL, and on synthesis of TCA-precipitatable proteins. The fact that a close structural analog of 1,25-(OH)2D3 (1,25-(OH)2D3) was incapable of similarly stimulating rTSH synthesis and/or secretion supported the hypothesis that this effect was not a non-specific effect which might be induced by any seco-sterol, and is probably receptor-mediated. The observed effect of 1,25-(OH)2D3 on the function of cells synthesizing and secreting rTSH was consistent with many previous reports in the literature implying a possible relationship between these two endocrine systems. As mentioned above, the combined autoradiographic and immunohistochemical study of Sar, et al. (140) suggested that 1,25-(OH) 2 D3 might somehow affect the function of TSH-secreting cells in the rat anterior pituitary. Stumpf, et al. published an abstract (159) describing effects of 1,25-(OH)2D3 on circulating TSH levels in intact and thyroidectomized rachi'tic rats. In both cases, vitamin D-deficient rats treated with 111 1,25-(OH)2D3 exhibited elevated serum levels of TSH. administered 25-OH-D 3 and calcium orally to healthy Zafkova, et al. (160) Czechoslovakian women and measured serum thyroxine, TSH, calcium, and magnesium. Thyroxine was the only parameter affected by such treatment, and it was elevated. Suzuki, et al. (162) reported effects of la-OH-D 3 in a case study of a woman being treated for hypocalcemia due to pseudohypoparathyroidism. Endocrine tests in the hypocalcemic state revealed an exaggerated response of TSH to TRH, and a blunted GH response to arginine-HCl. Both of these abnormalities were rectified following restoration of normocalcemia by giving la-OH-D 3 . Finally, Tornquist and Lamberg-Allardt recently presented an abstract in which they describe effects of 1,25-(OH)2D3 on the regulation of TSH secretion in rats (199). These investigators injected rats with 1,25-(OH) 2 D 3 (5 ug/kg/day) for 3 days, and then injected TRH i.v. 8 hours after the last dose. At various times thereafter, samples of blood were withdrawn from carotic artery cannulae. It was found that 1,25-(OH)2 D3 significantly increased the response of TSH to TRH. Although all of these studies suggest changes in the function of pituitary thyrotropes following administration of vitamin D-metabolites, none of them demonstrate conclusively a direct effect of 1,25-(OH)2D3 in the anterior pituitary. In addition, there have been several reports of changes in thyroid status resulting in physiological conditions which might be attributable to alterations in the activity or metabolism of 1,25-(OH) 2D3. For example, it has been well documented that hyperthyroidism results in increased bone turnover, osteoporesis, reduced intestinal calcium absorption, and hypercalciuria (221-226). It has further been shown (227-229) that elevated levels of 112 24,25-dihydroxyvitamin D3 and reduced levels of 1,25-(OH)2D3 are present in hyperthyroidism, and that the opposite effects on vitamin D metabolism are seen in hypothyroidism. Finally, it has been demonstrated that TSH and the thyroid hormones T3 and T4 are potent inhibitors of 25-OH-D3-la -hydroxylase activity in vitro, using a perfused rat kidney system (197). There is thus ample evidence suggesting that a physiologically significant relationship might exist between the vitamin D and thyroid endocrine systems. The present data suggest that 1,25-(OH) 2 D3 may be one of many circulating factors involved in the complex physiological regulation of rTSH secretion in vivo. The implied existence of a feedback system involving effects of 1,25-(OH) 2 D 3 on the activity of cells which produce a factor (rTSH) which is capable of regulating 1,25-(OH) 2D3 synthesis is not unique. Such a system has been suggested for regulation of parathyroid hormone secretion by 1,25-(OH) 2 D3 (111,112). A more general analogy can be seen with the feedback system whereby adrenal corticosteroids inhibit the synthesis of ACTH in the anterior pituitary, with ACTH being involved in the regulation of corticosteroid synthesis in the adrenal cortex (136). The failure to observe any changes in either synthesis or secretion of rPRL is also of significance. As discussed above, the only previous reports concerning effects of 1,25-(OH) 2 D 3 on the activity of pituitary cells demonstrated alterations in rPRL synthesis in clonal rat pituitary tumor cells. The lack of any effects of 1,25-(OH)2D3 on rPRL synthesis or secretion by non-transformed rat anterior pituitary cells in primary culture supports the speculation that the effects observed in tumor cells do not necessarily mimic events occurring in their non-transformed counterparts. 113 While such tumor cell studies are of great value in elucidating the biochemical mechanisms involved in hormone secretion, they may not always be of as much value for determining the ultimate physiological responses induced by receptor activation. In the present case, it is possible to speculate that the anterior pituitary receptor for 1,25-(OH)2D3, like many other cellular proteins, may be inappropriately expressed in these PRL-secreting tumor cells. The various strains of GH cells may, however, still represent a powerful tool for investigating the biochemical mechanism by which 1,2 5 -(OH)2D3-receptor activation results in hormone synthesis. Finally, the studies described herein concerning effects of 1,25-(OH)2D3 on anterior pituitary cell growth deserve further attention. In primary cultures of enzymatically dispersed rat anterior pituitary cells, no generalized quantitative effect of 1,25-(OH)2D3 was observed on protein synthesis, DNA synthesis, or the morphological distribution of cells. the heterogeneous nature of the cell population, however, it Due to is not possible to rule out effects of this seco-steroid on the growth of particular sub-populations of cells. In addition, qualitative changes in DNA synthesis and protein synthesis were not adequately examined. Possible effects on movement of cells through different phases of the cell cycle were also not addressed. Unfortunately, none of these experiments can be performed appropriately using a heterogeneous cell population. A different experimental model would be required. The possibility of such a selective effect of 1,25-(OH) 2 D3 on pituitary cell growth remains of great interest. It appears clear that 1,25-(OH) 2 -D affects its target tissues through a classical steroid mechanism of action 114 3 (86,98). This involves binding of the hormone to a cytosolic receptor, translocation to the nucleus, and interaction of the hormone-receptor complex with the chromatin. In the past, most research in this area has been concerned with the effects of this interaction on the synthesis of proteins which are presumed to be involved in calcium transport (230,231). If one considers that alteration of calcium transport might not be the ultimate effect of 1,25-(OH) 2 -D3, then it is possible to speculate that these same proteins, or other as yet unidentified induced proteins, could be involved in the regulation of target cell maturation. In support of this possibility, there is evidence that intracellular calcium content, or calcium fluxes, may be involved in the commitment of cells towards an end-differentiated state (232-234). There is also evidence for a role of calcium binding proteins in the regulation of cell differentiation (235-237). 1,25-(OH) 2 -D 3 Furthermore, it is possible to speculate that might be capable of affecting cellular development through a mechanism unrelated to induced protein synthesis. It is conceivable, for example, that the mere binding of 10,000 occupied receptors to a cell's chromatin might be sufficient to alter the dynamics of cell replication and differentiation. Such an effect might be dependent upon the particular target tissue, the stage of development of a particular cell, and the stage of the cell cycle during which the binding occurs. An interesting possibility is that the production of specific hormones by pituitary cells in culture could be influenced through changes in the state of differentiation of immature cells, or the rate of replication of proliferating cells. 115 SUMMARY AND CONCLUSIONS Summary of Results 1. The presence of a specific binding protein for 1,25-(OH) 2 D3 in both cytosolic and nuclear extracts of rat anterior pituitary was confirmed. This protein exhibited a sucrose density gradient sedimentation coefficient of 3.5-3.7 S. The dissociation constant (Kd) for the binding of 1,25-(OH)2D3 to this protein was determined to be 6.0 x 10-10M, with a Bmax of approximately 36 fmol/mg protein. 2. A previously described cell culture methodology was employed to study the possible receptor-mediated effects of 1,25-(OH)2D3 on the activity of enzymatically dispersed rat anterior pituitary cells in primary culture. The enzymatic dispersion procedure yielded greater than 95% viable cells at the time of seeding of the cultures. When these cells were incubated for 4 days in a serum-supplemented culture medium, followed by 2 days of incubation in a serum-free medium, the number and percentage of viable cells remained unchanged. 3. Radioimmunoassay of conditioned medium from cultures incubated for the initial 4 day period revealed that basal hormone secretory capacity was intact. These cells were capable of responding normally to both non-specific (increased media potassium concentration) and receptor-mediated (TRH) secretory stimuli. 116 4. Studies were performed to determine the effects of 1,25-(OH)2D3 on several parameters of enzymatically dispersed rat anterior pituitary cell function in primary culture. A. Regardless of the time of incubation or the dose of 1,25-(OH)2D3 administered, no significant effects were observed on any of the indices of cell growth examined. These included cellular protein content, cellular DNA content, cell number, and gross cellular morphology. B. When cultures were incubated with 10- 8 M 1,25-(OH) 2D3 for periods of time ranging from 6 hours to 48 hours, there was no consistent significant alteration in either cellular or media content of rPRL. C. When cultures were incubated with 10-8M 1,25-(OH)2D3 for periods of time ranging from 6 hour to 48 hours, media content of rTSH was found to be significantly elevated at both the 24 hour and 48 hour time points. This effect was found to be dose dependent, with an ED 50 between 10- 8 M and 10- 9 M at 48 hours. Although cellular content of rTSH was not statistically significantly altered during the time course experiment, a trend towards increased cellular rTSH content was observed, suggestive of a possible stimulatory effect on rTSH biosynthesis. 1. The structural specificity of 1,25-(OH)2D3 for stimulating secretion of rTSH was determined by incubating cultures for 24 hours in the presence Qf a variety of concentrations of 10,25-(OH)2D3. 117 The only difference in structure between 1,25-(OH)2D3 and this analog is the sterochemical configuration of the 1-hydroxyl group. This experiment was performed to rule out any non-specific steroid effect of 1,25-(OH) 293 , since it had been previously demonstrated that a change in the sterochemistry of the 1-hydroxyl group from alpha to beta completely abolished its biological activity and its binding to the receptor. All concentrations of this analog failed to have any significant effect on either media or cellular content of rTSH. D. Possible effects of 1,25-(OH)2D3 on rTSH biosynthesis were examined by measuring incorporation of 3 5S-methionine into newly synthesized immunoprecipitatable rTSH following 24 hours of incubation in the presence of 10- 8 M 1,25-(OH)2D3. Using this methodology, it was found that treatment with 1,25-(OH)2D3 resulted in a significant increase in incorporation of 35S-methionine into newly synthesized immunoprecipitatable rTSH, suggesting that 1,25-(OH)2D3 is capable of stimulating synthesis of rTSH. 1. of The specificity of this effect was examined by measuring incorporation 35 S-methionine into both TCA precipitatable proteins and immunoprecipitatable rPRL following 24 hours of incubation in the presence of 10- 8 M 1,25-(OH) 2 D3. Neither of these parameters were significantly affected. 118 2. The structural specificity of 1,25-(OH)2D3 for stimulating rTSH biosynthesis was determined by measuring incorporation of 35 S-methionine into newly synthesized immunoprecipitatable rTSH following 24 hours of incubation in the presence of a variety of concentrations of 10,25-(OH)2D3. All concentrations of this analog failed to significantly alter rTSH biosynthesis. The effect was thus shown to be specific for 1,25-(OH) 2 D3, and not a non-specific effect which might be induced by any seco-sterol. Conclusions 1. A receptor for 1,25-(OH) 2 D3 is present in rat anterior pituitary. 2. 1,25-(OH)2D3 stimulates both synthesis and secretion of rTSH by the sub-population of rat thyrotropes present in primary cultures of enzymatically dispersed rat anterior pituitary cells. 3. 1,25-(OH) 2 D 3 has no sustained effect on either synthesis or secretion of rPRL by the sub-population of rat mammotrophs present in primary cultures of enzymatically dispersed rat anterior pituitary cells. 4. 1,25-(OH) 2 D3 has no effect on the parameters of cell growth examined in this.thesis, although selective effects on the growth of specific sub-populations of cells present in rat anterior pituitary cannot be ruled out. 119 SUGGESTIONS FOR FUTURE RESEARCH Although the work described in this thesis has shed some light on the function of the pituitary receptor for 1,25-(OH) 2 D 3 , it also raises a number of interesting questions which might be studied in the future. Some of these include: 1. What is the molecular mechanism involved in the effects of 1,25-(OH)2 D3 on rTSH biosynthesis and secretion? Is calcium transport involved? Is the vitamin D-dependent calcium binding protein involved? 2. Does 1,25-(OH) 2 D3 affect the growth of specific sub-populations of rat anterior pituitary cells? Is 1,25-(OH) 2 D3 perhaps capable of altering the growth of receptor-positive anterior pituitary cells at certain defined times, such as in the young developing pituitary? 3. Are the effects of 1,25-(OH)2D3 dependent on other aspects of endocrine status, or on the age of the pituitary tissue being studied ? 4. Is there a similar receptor for 1,25-(OH)2D3 present in human pituitary'? If so, does 1,25-(OH) 2 D3 similarly affect the activity of receptor-positive human anterior pituitary cells ? 5. I's 1,25-(OH) 2 D3 capable of altering the growth and/or activity of neoplastic anterior pituitary cells which secrete TSH ? 120 REFERENCES 1. Hess, A. (1929). The history of rickets. In: Rickets, Including Osteomalacia and Tetany, pp.22-37, Lea and Febinger., Philadelphia. 2. Mellanby, E. (1919). 1:407-412. 3. Mellanby, E. (1919). A further demonstration of the part played by accesory food factors in the aetiology of rickets. J. Physiol.(Lond.) 52:liii-liv. 4. Holick, M.F., and M.B. Clark (1978). The photobiogenesis and metabolism of vitamin D. Fed. Proc. Fed. Am. Soc. Exp. Biol. 37:2567-2574. 5. Esvelt, R.P., H.F. DeLuca, and H.K. Schnoes (1978). Vitamin D3 from rat skins irradiated in vitro with ultraviolet light. Arch. Biochem. Biophys. 188:282-286. 6. McCollum, E.V., N. Simmonds, J.E. Becker, and P.G. Shipley (1922). Studies on experimental rickets. XXI. An experimental demonstration of the existence of a vitamin which promotes calcium deposition. J. Biol. Chem. 53:293-312. 7. Huldshinsky, K. (1919). Heilung von Rachitis durch kunstliche Hohensonne. Dtsch. Med. Wochenschr. 45:712-713. 8. Chick, H., E.J. Dalzell and E.M. Hume (1923). Studies of rickets in Vienna 1919-1922. Medical Research Council Special Report No. 77. 9. Steenbock, H., and A. Black (1924). Fat-soluble vitamins. XVII. The induction of growth-promoting and calcifying properties in a ration by exposure to ultraviolet light. J. Biol. Chem. 61:405-422. 10. Hess, A.F., and M. Weinstock (1924). Antirachitic properties imparted to lettuce and to growing wheat by ultraviolet irradiation. Proc. Soc. Exp. Biol. Med. 22:5-6. 11. Askew, F.A., R.B. Bourdillon, H.M. Bruce, R.G.C. Jenkins, and T.A. Webster (1931). The distillation of vitamin D. Proc. R. Soc. Lond. [Biol.] 107:76-90. 12. Windaus, A., 0. Linsert, A. Luttringhaus, and G. Weidlich (1932). das krystallisierte Vitamin D2- Justus Liebigs Ann. Chem. 492:226-241. 13. Windaus, A., F. Schenck, and F. von Werder (1936). Uber das antirachitisch wirksame bestrahlungsprodukt aus 7-dehydro-cholesterin. Hoppe-Seyler's Z. Physiol. Chem. 241:100-103. An experimental investigation of rickets. 121 Lancet Uber 14. Windaus, A., and F. Bock (1937). Uber das provitamin aus dem sterin der schweineschwarte. Hoppe-Seyler's Z. Physiol. Chem. 245:168-170. 15. Nicolaysen, R. (1937). Studies upon the mode of action of vitamin D. II. The influence of vitamin D on the faecal output of endogenous calcium and phosphorus in the rat. Biochem. J. 31:106-121. 16. Nicolaysen, R. (1937). Studies upon the mode of action of vitamin D. III. The infulence of vitamin D on the absorption of calcium and phosphorus in the rat. Biochem. J. 31:122-129. 17. Nicolaysen, R. (1937). Studies upon the mode of action of vitamin D. IV. The absorption of calcium chloride, xylose and sodium sulphate from isolated loops of the small intestine and of calcium chloride from the abdominal cavity in the rat. Biochem. J. 31:323-328. 18. Nicolaysen, R., N. Eeg-Larsen, and O.J. Malm (1953). calcium metabolism. Physiol. Rev. 33:424-444. 19. Holick, M. (1981). The cutaneous photosynthesis of Previtamin D3 : A unique photoendocrine system. J. of Investigative Dermatology 76:51-58. 20. Kodicek, E. (1960). The metabolism of vitamin D. In: Proceedings of the Fourth International Congress of Biochemistry - vol. 11: Vitamin Metabolism. Umbreit, W, and Molitor, H (eds.). pp.198-208. Pergamon Press, London. 21. Norman, A.W., and H.F. DeLuca (1963). The preparation of 3 H-vitamins D2 and D3 and their localization in the rat. Biochemistry 2:1160-1168. 22. Schacter, D., J.D. Finkelstein, and S. Kowarski (1964). Metabolism of vitamin D. I. Preparation of radioactive vitamin D and its intestinal absorption in the rat. J. Clin. Invest. 43:787-796. 23. Avioli, L.V., S.W. Lee, J.E. McDonald, J. Lund, and H.F. DeLuca (1967). Metabolism of vitamin D3- 3 H in human subjects: distribution in blood, bile, feces, and urine. J. Clin. Invest. 46:983-992. 24. Rikkers, H., R. Kletzien, and H.F. DeLuca (1969). Vitamin D binding globulin in the rat: specificity for the vitamins D. Proc. Soc. Exp. Biol. Med. 130:1321-1324. 25. Rikkers, H., and H.F. DeLuca (1967). An in vivo study of the carrier proteins of 3 H-vitamins D3 and D4 in rat serum. Am. J. Physiol. 213:380-386. 26., I'mawari, M., K. Kida, and D.S. Goodman (1976). The transport of vitamin D and its 25-hydroxy metabolite in human plasma. J. Clin. Invest. 58:514-523. 122 Physiology of 27. Haddad, J.G., J. Walgate, C. Min, and T. Hahn (1976). Vitamin D metabolite-binding proteins in human tissue. Biochim. Biophys. Acta 444:921-925. 28. Neville, P.F., and H.F. DeLuca (1966). The synthesis of [1,2- 3 H] vitamin D3 and the tissue localization of a 0.25 ug (10 IU) dose per rat. Biochemistry 5:2201-2207. 29. Ponchon, G., and H.F. DeLuca (1969). The role of the liver in the metabolism of vitamin D. J. Clin. Invest. 48:1273-1279. 30. Rosenstreich, S.J., C. Rich and W. Volwiler (1971). Deposition in and release of vitamin D3 from body fat: evidence for a storage site in the rat. J. Clin. Invest. 50:679-687. 31. Ponchon, G., A.L. Kennan, and H.F. DeLuca (1969). "Activation" of vitamin D by the liver. J. Clin. Invest. 48:2032-2037. 32. Bhattacharyya, M.H., and H.F. DeLuca (1974). Subcellular location of rat liver calciferol-25-hydroxylase. Arch. Biochem. Biophys. 160:58-62. 33. Olson, E.B., Jr., J.C. Knutson, M.H. Bhattacharyya, and H.F. DeLuca (1976). The effect of hepatectomy on the synthesis of 25-hydroxyvitamin D3. J. Clin. Invest. 57:1213-1220. 34. Blunt, J.W., Y. Tanaka, and H.F. DeLuca (1968). The biological activity of 25-hydroxycholecalciferol, a metabolite of vitamin D3. Proc. Natl. Acad. Sci. USA 61:1503-1506. 35. Tanaka, Y., H. Frank, and H.F. DeLuca (1972). Biological activity of 1,25-dihydroxyvitamin D3 in the rat. Endocrinology 92:417-422. 36. Pavlovitch, H., M. Garabedian, and S. Balsan (1973). Calcium-mobilizing effect of large doses of 25-hydroxycholecalciferol in anephric rats. J. Clin. Invest. 52:2656-2660. 37. Boyle, I.T., L. Miravet, R.W. Gray, M.F. Holick, and H.F. DeLuca (1972). The response of intestinal calcium transport to 25-hydroxy and 1,25-dihydroxy vitamin D in nephrectomized rats. Endocrinology 90:605-608. 38. Holick, M.F., M. Garabedian, and H.F. DeLuca (1972). 1,25-Dihydroxycholecalciferol: metabolite of vitamin D3 active on bone in anephric rats. Science 176:1146-1147. 39. -Haddad, J.G., and T.C.B. Stamp (1974). man. Am. J. Med. 57:57-62. Circulating 25-hydroxyvitamin D in 40.- Eisman, J.A., R.M. Shepard, and H.F. DeLuca (1977). Determination of 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 in human plasma using high pressure liquid chromatography. Anal. Biochem. 80 :298-305. 123 41. Haddad, J.G., and S.J. Birge (1975). Widespread, specific binding of 25-hydroxycholecalciferol in rat tissues. J. Biol. Chem. 250:299-303. 42. Fraser, D.R., and E. Kodicek (1970). Unique biosynthesis by kidney of a biologically active vitamin D metabolite. Nature 228:764-766. 43. Gray, R., I. Boyle, and H.F. DeLuca (1971). Vitamin D metabolism: the role of kidney tissue. Science 172:1232-1234. 44. Norman, A.W., R.J. Midgett, J.F. Myrtle, and H.G. Nowicki (1971). Studies on calciferol metabolism. I. Production of vitamin D metabolite 4B from 25-OH-cholecalciferol by kidney homogenates. Biochem. Biophys. Res. Commun. 42:1082-1087. 45. Gray, T.K., G.E. Lester, and R.S. Lorenc (1979). Evidence for extra-renal la-hydroxylation of 25-hydroxyvitamin D3 in pregnancy. Science 204:1311-1313. 46. Whitsett, J.A., M. Ho, R.C. Tsang, E.J. Norman, and K.G. Adams (1981). Synthesis of 1,25-dihydroxyvitamin D3 by human placenta in vitro. J. Clin. Endocrinol. Metab. 53:484-488. 47. Tanaka, Y., B. Halloran, H.K. Schnoes, and H.F. DeLuca (1979). In vitro production of 1,25-dihydroxyvitamin D3 by rat placental tissue. Proc. Natl. Acad. Sci. USA 76:5033-5035. 48. Weisman, Y., A. Harrell, S. Edelstein, M. David, Z. Spirer, and A. Golander (1979). la,25-Dihydroxyvitamin D3 and 24,25-dihydroxyvitamin D3: in vitro synthesis by human decidua and placenta. Nature 281:317-319. 49. Gray, R.W., J.L. Omdahl, J.G. Ghazarian, and H.F. DeLuca (1972). 25-Hydroxy-cholecalciferol-1-hydroxylase: subcellular location and properties. J. Biol. Chem. 247:7528-7532. 50. Holick, M.F., H.K. Schnoes, and H.F. DeLuca (1971). Identification of 1,25-dihydroxycholecalciferol, a form of vitamin D3 metabolically active in the intestine. Proc. Natl. Acad. Sci. USA 68:803-804. 51. Holick, M.F., H.K. Schnoes, H.F. DeLuca, T. Suda, and R.J. Cousins (1971). Isolation and identification of 1,25-dihydroxycholecalciferol. A metabolite of vitamin D active in intestine. Biochemistry 10:2799-2804. 52.. Semmler, E.J., M.F. Holick, H.K. Schnoes, and H.F. DeLuca (1972). The synthesis of la,25-dihydroxycholeciferol - a metabolically active form of vitamin D3. Tetrahedron Lett. 40:4147-4150. 53. Chen, T.C., L. Castillo, M. Korycka-Dahl, and H.F. DeLuca (1974). Role of vitamin D metabolites in phosphate transport of rat intestine. J. Nutr. 104:1056-1060. 124 54. Gray, R.W., J.L. Omdahl, J.G. Ghazarian, and H.F. DeLuca (1972). 25-Hydroxycholecalciferol-1-hydroxylase: subcellular location and properties. J. Biol. Chem. 247:7528-7532. 55. Pedersen, J.I., J.G. Ghazarian, N.R. Orme-Johnson, and H.F. DeLuca (1976). Isolation of chick renal mitochondrial ferredoxin active in the 25-hydroxyvitamin D3-la-hydroxylase system. J. Biol. Chem. 251:3933-3941. 56. Ghazarian, J.G., C.R. Jefcoate, J.C. Knutson, W.H. Orme-Johnson, and H.F. DeLuca (1974). Mitochondrial cytochrome P4 50 : a component of chick kidney 25-hydroxycholecalciferol-la-hydroxylase. J. Biol. Chem. 249:3026-3033. 57. Ghazarian, J.G., and H.F. DeLuca (1974). 25-Hydroxycholecalciferol-la-hydroxylase: a specific requirement for NADPH and a hemoprotein component in chick kidney mitochondria. Arch. Biochem. Biophys. 160:63-72. 58. Garabedian, M., M.F. Holick, H.F. DeLuca, and I.T. Boyle (1972). Control of 25-hydroxycholecalciferol metabolism by the parathyroid glands. Proc. Natl. Acad. Sci. USA 69:1673-1676. 59. Fraser, D.R., and E. Kodicek (1973). Regulation of 25-hydroxycholecalciferol-1-hydroxylase activity in kidney by parathyroid hormone. Nature New Biol. 241:163-166. 60. Boyle, I.T., R.W. Gray, and H.F. DeLuca (1971). Regulation by calcium of in vivo synthesis of 1,25-digydroxycholecalciferol and 21,25-dihydroxycholecalciferol. Proc. Natl. Acad. Sci. USA 68:2131-2134. 61. Bilezikian, J.P., R.E. Canfield, T.P. Jacobs, J.S. Polay, A.P. D'Adamo, J.A. Eisman, and H.F. DeLuca (1978). Response of la,25-dihydroxyvitamin D3 to hypocalcemia in human subjects. N. Engl. J. Med. 299:437-441. 62. Adams, N.D., R.W. Gray, and J. Lemann, Jr. (1979). The effects of oral CaC03 loading and dietary calcium deprivation on plasma 1,25-dihydroxyvitamin D concentrations in healthy adults. J. Clin. Endocrinol. Metab. 48:1008-1016. 63. Tanaka, Y., and H.F. DeLuca (1973). The control of 25-hydroxyvitamin D metabolism by inorganic phosphorus. Arch. Biochem. Biophys. 154:566-574. 64.. Gray, R.W., D.R. Wil z, A.E. Caldas, and J. Lemann, Jr. (1977). The importance of phosphate in regulating plasma 1,25-(OH)2-vitamin D levels in humans: studies in healthy subjects, in calcium-stone formers and in patients with primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 45:299-306. 65. Lund, B.J., 0.H. Sorensen, B.I. Lund, J.E. Bishop, and A.W. Norman (1980). Stimulation of 1,25-dihydroxyvitamin D production by parathyroid hormone and hypocalcemia in man. J. Clin. Endocrinol. Metab. 50:480-484. 125 66. Friedlander, E.J., H.L. Henry, and A.W. Norman (1977). Studies on the mode of action of calciferol XII. Effects of dietary calcium and phosphorus on the relationship between the 25-hydroxyvitamin D5-la-hydroxylase and production of chick intestinal calcium binding protein. J. Biol. Chem. 252:8677-8683. 67. Trechsel, U., J.A. Eisman, J.A. Fischer, J.P. Bonjour, and H. Fleisch (1980). Calcium-dependent parathyroid hormone-dependent regulation of 1,25-dihydroxyvitamin D. Am. J. Physiol. 239:E119-E124. 68. Kenny, A.D. (1976). Vitamin D metabolism: physiological regulation in the egg-laying Japanese quail. Am. J. Physiol. 230:1609-1615. 69. Castillo, L., Y. Tanaka, H.F. DeLuca, and M.L. Sunde (1977). The stimulation of 25-hydroxyvitamin D3-la-hydroxylase by estrogen. Arch. Biochem. Biophys. 179:211-217. 70. Garel , J.M., C. Rebut-Bonneton, and F. Delbarre (1980). Basal bone resorption in the rat fetus related to the hormonal status of the mother. J. Endocrinol. 34:453-458. 71. Weisman, Y., Z. Eisenberg, R. Lubelski, Z. Spirer, S. Edelstein, and A. Harrell (1981). Decreased 1,25-dihydroxycholecalciferol and increased 25-hydroxy- and 24,25-dihydroxycholecalciferol in tissues of rats treated with thyroxine. Calcif. Tissue Int. 33:445-447. 72. Tanaka, Y., R.S. Lorenc, and H.F. DeLuca (1975). The role of 1,25-dihydroxyvitamin D3 and parathyroid hormone in the regulation of chick renal 25-hydroxyvitamin D3-24-hydroxylase. Arch. Biochem. Biophys. 171:521-526. 73. Kumar, R., D. Harnden, and H.F. DeLuca (1976). Metabolism of 1,25-dihydroxyvitamin D3 : Evidence for side-chain oxidation. Biochemistry 15:2420-2423. 74. Esvelt, R.P., H.K. Schnoes, and H.F. DeLuca (1979). Isolation and characterization of la-hydroxy-23-carboxytetranorvitamin D: A major metabolite of 1,25-dihydroxyvitamin D3. Biochemistry 18:3977-3983. 75. Holick, M.F., A. Kleiner-Bossaller, H.K. Schnoes, P.M. Kasten, I.T. Boyle, and H.F. DeLuca (1973). 1,24,25-Trihydroxyvitamin D3: a metabolite of vitamin D3 effective on intestine. J. Biol. Chem. 248:6691-6696. 76. DeLuca, H.F. (1978). Vitamin D. In: The fat-soluble vitamins. Vol. 2: Handbook of lipid research. DeLuca, HF (ed.). pp. 69-132. New York: Plenum Press. 77. DeLuca, H.F., and H.K. Schnoes (1976). Metabolism and mechanism of action of vitamin D. Annu. Rev. Biochem. 45:631-666. 126 Boyle, I.T., J.L. Omdahl, R.W. Gray, and H.F. DeLuca (1973). The biological activity and metabolism of 24,25-dihydroxyvitamin D3 J. Biol. Chem. 248:4174-4180. 79. DeLuca, H.F. (1979). Vitamin D: Metabolism and Function. In: Monographs on Endocrinology. F. Gross, M.M. Grumbach, A. Labhart, M.B. Lipsett, T. Mann, L.T. Samuels, and J. Zander (eds.). Vol. 13. Springer-Verlag Berlin, Heidelberg. 80. Coburn, J.W., G.F. Bryce, B.S. Levine, J.P. Mallon, F. Singer, and 0.N. Miller (1981). In: Osteoporosis: Recent Advances in Pathogenesis and Treatment. H.F. DeLuca, H.M. Frost, W.S.S. Jee, C.C Jognston, Jr., and A.M. Parfitt (eds.). p. 485 (abstract). University Park Press, Baltimore. 81. DeLuca, H.F. (1967). Mechanism of action and metabolic fate of vitamin D. Vitam. Horm. 25:315-367. 82. DeLuca, H.F. (1977). Proc. Annu. Meet. Royal College of Physicians and Surgeons of Canada. pp. 216-225. 83. DeLuca, H.F. (1978). Vitamin D and Calcium Transport. In: Ann. N.Y. Acad. Sci., vol. 307: Calcium Transport and Cell Function. A. Scarpa, and E. Carafoli (eds.). pp. 356-376. New York Academy of Sciences, New York. 84. Sebrell, W.H., Jr., and R.S. Harris (eds.) (1954). Vitamin D Group. The Vitamins. pp. 131-266. Academic Press, New York. 85. Frost, H.M. (1966). Bone dynamics in osteoporosis and osteomalacia. Henry Ford Hospital Surgical Monograph Series. Charles A. Thomas, Springfield. 86. O'Malley, B.W., and W.L. McGuire (1968). Changes in hybridizable nuclear RNA during progesterone induction of a specific oviduct protein. Biochem. Biophys. Res. Commun. 32:595-598. 87. Kream, B.E., M.J.L. Jose, and H.F. DeLuca (1977). The chick intestinal cytosol binding protein for 1,25-dihydroxyvitamin D3: a study of analog binding. Arch. Biochem. Biophys. 179:462-468. 88. van Baelen, H., R. Bouillon, and P. DeMoor (1977). Binding of 25-hydroxycholecalciferol in tissues. J. Biol. Chem. 252:2515-2518. 89. Kream, B.E., S. Yamada, H.K. Schnoes, and H.F. DeLuca (1977). Specific cytosol binding protein for 1,25-dihydroxyvitamin D3 in rat intestine. J. Biol. Chem. 252:4501-4505. . 78. In: 90.. Eisman, J.A., and H.F. DeLuca (1977). Intestinal 1,25-dihydroxyvitamin D3 binding protein: specificity of binding. Steroids 30:245-257. 91. Zerwekh, J.E., M.R. Haussler, and T.J. Lindell (1974). Rapid enhancement of chick intestinal DNA-dependent RNA polymerase II activity by 127 la-25-dihydroxyvitamin D3, in vivo. 71:2337-2341. Proc. Natl. Acad. Sci. USA 92. Brumbaugh, P.F., and M.R. Haussler (1974). la,25-dihydroxycholecalciferol receptors in intestine. I. Association of la,25-dihydroxycholecalciferol with intestinal mucosa chromatin. J. Biol. Chem. 249:1251-1257. 93. Zerwekh, J.E., T.J. Lindell, and M.R. Haussler (1976). Increased intestinal chromatin template activity. Influence of la,25-dihydroxyvitamin D3 and hormone receptor complexes. J. Biol. Chem. 251:2388-2394. 94. Brumbaugh, P.F., and M.R. Haussler (1974). la,25-Dihydroxycholecalciferol receptors in intestine. II. Temperature-dependent transfer of the hormone to chromatin via a specific cytosol receptor. J. Biol. Chem. 249:1258-1262. 95. Pike, J.W., and M.R. Haussler (1979). Purification of chicken intestinal receptor for 1,25-dihydroxyvitamin D. Proc. Natl. Acad. Sci. USA 76:5485-5489. 96. Spencer, R., M. Charman, J.S. Emtage, and D.E.M. Lawson (1976). Production and properties of vitamin-D-induced mRNA for chick calcium-binding protein. Eur. J. Biochem. 71:399-409. 97. Wasserman, R.H., and J.J. Feher (1977). Vitamin D-dependent calcium-binding protein. In: Calcium binding proteins and calcium function. R.H. Wasserman, R.A. Corradino, E. Carafoli, R.H. Kretsinger, D.H. MacLennan, and S.L. Siegel (eds.). pp. 293-302. Elsevier, North Holland. 98. DeLuca, H.F. (1981). Metabolism and molecular mechanism of action of vitamin D: 1981. Biochemical Society Trans. 10:147-158. 99. Franceschi, R.T., R.U. Simpson, and H.F. DeLuca (1981). Binding proteins for vitamin D metabolites: serum carriers and intracellular receptors. Arch. Biochem. Biophys. 210:1-13. 100. Rasmussen, H., 0. Fontaine, E.E. Max, and D.B.P. Goodman (1979). The effect of la-hydroxyvitamin D3 administration on calcium transport in chick intestine brush border membrane vessicles. J. Biol. Chem. 254:2993-2999. 101. - 102. 103. Bickle, D.D., D.T. Zolock, R.L. Morrissey, and R.H. Herman (1978). Independence of 1,25-dihydroxyvitamin D3-mediated calcium transport from de novo RNA and protein synthesis. J. Biol. Chem. 253:484-488. Matsumoto, T., 0. Fontaine, and H. Rasmussen (1981). Effect of 1,25-dihydroxyvitamin D3 on phospholipid metabolism in chick duodenal mucosal cell. Relationship to its mechanism of action. Biol. Chem. 256:3354-3360. Fontaine, 0., T. Matsumoto, D.B.P. Goodman, and H. Rasmussen (1981). Liponomic control of Ca 2+ transport: relationship to mechanism of 128 J. action of 1,25-dihydroxyvitamin D3. 78:1751-1754. Proc. Natl. Acad. Sci. USA 104. Spencer, R., M. Charman, P.N. Wilson, and D.E.M. Lawson (1978). The relationship between vitamin D-stimulated calcium transport and intestinal calcium-binding protein in the chicken. Biochem. J. 170:93-101. 105. Thomasset, M., A. Molla, 0. Parkes, and G. DeMaille (1981). Intestinal calmodulin and calcium-binding protein differ in their distribution and in the effect of vitamin D steroids on their concentration. FEBS Lett. 127:13-16. 106. Wasserman, R.H., M.E. Brindak, S.A. Meyer, and C.S. Fullmer (1982). Evidence for multiple effects of vitamin D3 on calcium absorption: response of rachitic chicks, with or without partial vitamin D3 repletion, to 1,25-dihydroxyvitamin D3. Proc. Natl. Acad. Sci. USA 79:7939-7943. 107. Stumpf, W.E., M. Sar, F.A. Reid, Y. Tanaka, and H.F. DeLuca (1979). Target cells for 1,25-dihydroxyvitamin D3 in intestinal tract, stomach, kidney, skin, pituitary, and parathyroid. Science 206:1188-1190. 108. Henry, H.L., and A.W. Norman (1975). Studies on the mechanism of action of calciferol VII. Localization of 1,25-dihydroxyvitamin D3 in chick parathyroid glands. Biochem. Biophys. Res. Commun. 62:781-788. 109. Hughes, M.R., and M.R. Haussler (1978). 1,25-Dihydroxyvitamin D3 receptors in parathyroid glands. J. Biol. Chem. 253:1065-1073. 110. Oldham, S.A., J.A. Fischer, L.H. Shen, and C.D. Arnaud (1974). Isolation and properties of a calcium-binding protein from porcine parathyroid glands. Biochemistry 13:4790-4796. 111. Chertow, B.S., D.J. Baylink, J.E. Wergedal, M.H.H. Su, and A.W. Norman (1975). Decrease in serum immunoreactive parathyroid hormone in rats and in parathyroid hormone secretion in vitro by 1,25-dihydroxycholecalciferol. J. Clin. Invest. 56:668-678. 112. Dietal, M., G. Dorn, R. Montz, and E. Altenahr (1979). Influence of vitamin D3, 1,25-dihydroxyvitamin D3, and 24,25-dihydroxyvitamin D3 on parathyroid hormone secretion, adenosine 3',5'-monophosphate release, and ultrastructure of parathyroid glands in organ culture. Endocrinology 105:237-245. 113.. Haussler, M.R., S.C. Manolagas, and L.J. Deftos (1980). Evidence for a 1,25-dihydroxyvitamin D3 receptor-like macromolecule in rat pituitary. J. Biol. Chem. 255:5007-5010. 114. Murdoch, G.H., and M.G. Rosenfeld (1981). Regulation of pituitary function and prolactin in the GH 4 cell line by vitamin D. J. Biol. Chem. 256:4050-4055. 129 115. Spencer, E.M, and 0. Tobiassen (1977). The effects of hypophysectomy on 25-Hydroxyvitamin D3 metabolism in the rat. In: Vitamin D: Biochemical, Chemical, and Clinical Aspects Related to Calcium Metabolism. A.W. Norman, K. Schaefer, J.W. Coburn, H.F. DeLuca, D. Fraser, H.G. Grigoleit, and E. von Herrath (eds.). Walter de Gruyter and Co., Berlin. p. 197-199. 116. Spencer, E.M., and 0. Tobiassen (1981). The mechanism of action of growth hormone on vitamin D metabolism in the rat. Endocrinology 108:1064-1070. 117. Spanos, E., D. Barrett, I. MacIntyre, J.W. Pike, E.F. Safilian, and M.R. Haussler (1978). Effect of growth hormone on vitamin D metabolism. Nature 273:246-247. 118. Pahuja, D.N., and H.F. DeLuca (1981). Role of the hypophysis in the regulation of vitamin D metabolism. Mol. Cell. Endocr. 23:345-350. 119. Kumar, R., T.J. Merimee, P. Silva, and F.H. Epstein (1979). The effect of chronic growth hormone excess or deficiency on plasma 1,25-dihydroxyvitamin D levels in man. Proceedings of the Fourth Workshop on Vitamin D. Walter de Gruyter, Elmsford, NY. pp.1005-1009. 120. Gertner, J.M., R.L. Horst, A.E. Broadus, H. Rasmussen, and M. Genel (1979). Parathyroid function and vitamin D metabolism during human growth hormone replacement. J. Clin. Endocrinol. Metab. 49:185-188. 121. Eskildsen, P.C., B.J. Lund, 0.H. Sorensen, B.I. Lund, J.E. Bishop, and A.W. Norman (1979). Acromegaly and vitamin D metabolism: effect of bromocriptine treatment. J. Clin. Endocrinol. Metab. 49:484-486. 122. Pike, J.W., J.B. Parker, M.R. Haussler, A. Boass, and S.U. Toverud (1979). Dynamic changes in circulating 1,25-dihydroxyvitamin D during reproduction in rats. Science 204:1427-1429. 123. Reddy, G.S., A.W. Norman, D.M. Willis, D. Goltzman, H. Guyda, S. Solomon, D.R. Philips, J.E. Bishop, and E. Mayer (1983). Regulation of vitamin D metabolism in normal human pregnancy. J. Clin. Endocrinol. Metab. 56:363-370. 124. Steichen, J.J., R.C. Tsang, T.L. Gratton, A. Hamstra, and H.F. DeLuca (1980). Vitamin D homeostasis in the perinatal period. 1,25-Dihydroxyvitamin D in maternal, cord and neonatal blood. N. Eng. J. Med. 302:315-319. 125.' Kumar, R., W.R. Cohen, P. Silva, and F.H. Epstein (1979). Elevated 1,25-dihydroxyvitamin D plasma levels in normal human pregnancy and lactation. J. Clin. Invest. 63:342-344. 126. Pike, J.W., S. Toverud, A. Boass, T.A. McCain, and M.R. Haussler (1977). Circulating la,25-(OH) 2 D during physiological states of calcium stress. In: Vitamin D: Biochemical, Chemical and Clinical Aspects Related to Calcium Metabolism. A.W. Norman, K. Schaefer, 130 J.W. Coburn, H.F. DeLuca, D. Fraser, H.G. Grigoleit, and E. von Herrath (eds.). Walter de Gruyter and Co., Berlin. p.187-189. 127. Lund, B., and A. Selnes (1979). Plasma 1,25-dihydroxyvitamin D levels in pregnancy and lactation. Acta Endocrinol (Copenh) 92:330-335. 128. MacIntyre, I., K.W. Colston, M. Szelke, and E. Spanos (1978). of the hormonal factors that control calcium metabolism. Acad. Sci. 307:345-354. 129. Spanos, E., J.W. Pike, M.R. Haussler, K.W. Colston, I.M.A. Evans, A.M. Goldner, T.A. McCain, and I. MacIntyre (1976). Circulating la,25-dihydroxyvitamin D in the chicken: enhancement by injection of prolactin and during egg laying. Life Sci. 19:1751-1756. 130. Bickle, D.D., E.M. Spencer, W.H. Burke, and C.R. Rost (1980). Prolactin but not growth hormone stimulates 1,25-dihydroxyvitamin D 3 production by chick renal preparations in vitro. Endocrinology 107:81-84. 131. Spanos, E., K.W. Colston, I.M.S. Evans, L.S. Galante, S.J. Macauley, and I. MacIntyre (1976). Effect of prolactin on vitamin D metabolism. Mol. Cell. Endocr. 5:163-167. 132. Matsumoto, T., N. Horiuchi, T. Suda, H. Takahashi, E. Shimazawa, and E. Ogata (1979). Failure to demonstrate stimulatory effect of prolactin on vitamin D metabolism in vitamin-D-deficient rats. Metabolism 28:925-927. 133. Adams, N.D., T.L. Garthwaite, R.W. Gray, T.C. Hagen, and J. Lemann, Jr. (1979). The interrelationships among prolactin, 1,25-dihydroxyvitamin D, and parathyroid hormone in humans. J. Clin. Endocrinol. Metab. 49:628-630. 134. Kumar, R., C.F. Abboud, and B.L. Riggs (1980). The effect of elevated prolactin levels on plasma 1,25-dihydroxyvitamin D and intestinal absorption of calcium. Mayo Clin. Proc. 55:51-53. 135. Kumar, R., W.R. Cohen, P. Silva, and F.H. Epstein (1979). Elevated 1,25-dihdroxyvitamin D plasma levels in normal human pregnancy and lactation. J. Clin. Invest. 63:342-344. 136. Rasmussen, H. (1974). Organization and control of endocrine systems. In: Textbook of Endocrinology (5th edition). Williams, RH (ed.). W.B. Saunders Co., Philadelphia. pp.1-30. 137. Li.eberberg, J., and B.S. McEwen (1979). In: Biochemical Actions of Hormones. Academic Press, NY. 6:415-459. 138. Stumpf, W.E., M. Sar, S.A. Clark, and H.F. DeLuca (1982). Brain target sites for 1,25-dihydroxyvitamin D3 . Science 215:1403-1405. 131 A survery Ann. N.Y. 139. Wark, J.D., and A.H. Tashjian, Jr. (1982). Vitamin D stimulates prolactin synthesis by GH 4 C1 cells incubated in chemically defined medium. Endocrinology 111:1755-1757. 140. Sar, M., W.E. Stumpf, and H.F. DeLuca (1980). Thyrotropes in the pituitary are target cells for 1,25-dihydroxyvitamin D3- Cell Tissue Res. 209:161-166. 141. Gelbard, H.A., P.H. Stern, and D.C. U'Prichard (1981). Characteristics of [3 H]-1a,25-(OH) 2 D3 binding to nuclear fractions from rat pituitary adenoma GH 3 cells. Life Sci. 29:1051-1056. 142. Gelbard, H.A., P.H. Stern, and D.C. U'Prichard (1980). la,25-Dihydroxyvitamin D3 nuclear receptors in the pituitary. Science 209 :1247-1249. 143. Gelbard, H.A., P.H. Stern, and D.C. U'Prichard, DC (1980). Society 62nd Annual Meeting (abstract). p.80. 144. Pike, J.W., L.L. Gooze, and M.R. Haussler (1980). Biochemical evidence for 1,25-dihydroxyvitamin D receptor macromolecules in parathyroid, pancreatic, pituitary, and placental tissues. Life Sci. 26:407-414. 145. Freake, H.C., C. Marcocci, J. Iwasaki, J.C. Stevenson, and I. MacIntyre (1982). Studies with the 1,25-(OH) 2 D3 binding protein. In: Vitamin D: Chemical, Biochemical, and Clinical Endocrinology of Calcium Metabolism. A.W. Norman, K. Schaefer, D. v. Herrath, and H.G. Grigoleit (eds.). Walter de Gruyter, Berlin. pp.79-81. 146. Murdoch, G.H., and M.G. Rosenfeld (1980). Regulation of pituitary function and prolactin production in the GH 4 cell line by 1,25-diOH Vitamin D. Fed. Proc. 39:560 (abstract A1556). 147. Haug, E., J.I. Pederson, and K. Gautvik (1982). Effects of vitamin D metabolites on prolactin and growth hormone synthesis in cultured rat piuitary cells. In: Vitamin D: Chemical, Biochemical, and Clinical Endocrinology of Calcium Metabolism. A.W. Norman, K. Schaefer, D. v. Herrath, and H.G. Grigoleit (eds.). Walter de Gruyter, Berlin. pp.87-89. 148. Haussler, M.R., J.W. Pike, S. Dokoh, J.S. Chandler, S.K. Chandler, C.A. Donaldson, and S.L. Marion (1982). 1,25-Dihydroxyvitamin D receptor in cultured cell lines: occurrence, subcellular distribution, and relationship to bioresponses. In: Vitamin D: Chemical, Biochemical, and Clinical Endocrinology of Calcium Metabolism. A.W. Norman, K. Schaefer, D. v. Herrath, and H.G. Grigoleit (eds.). Walter de Gruyter, Berlin. pp.109-113. 149. Christakos, S., and A.W. Norman (1979). Studies on the mode of action of calciferol XVIII. Evidence for a specific high affinity binding protein for 1,25-dihydroxyvitamin D3 in chick kidney and pancreas. Biochem. Biophys. Res. Commun. 89:56-63. 132 Endocrine 150. Chandler, J.S., J.W. Pike, and M.R. Haussler (1979). 1,25-Dihydroxyvitamin D3 receptors in rat kidney cytosol. Biophys. Res. Commun. 90:1057-1063. Biochem. 151. Colston, K.W., and D. Feldman (1979). Demonstration of a 1,25-dihydroxycholecalciferol cytoplasmic receptor-like binder in mouse kidney. J. Clin. Endocrinol. Metab. 49:798-800. 152. Chen, T.L., M.A. Hirst, and D. Feldman (1979). A receptor-like binding macromolecule for la,25-dihydroxycholecalciferol in cultured mouse bone cells. J. Biol. Chem. 254:7491-7494. 153. Mellon, W.S, and H.F. DeLuca (1979). An equilibrium and kinetic study of 1,25-dihydroxyvitamin D3 binding to chick intestinal cytosol employing high specific activity 1,25-dihydroxy-[ 3 H-26,27]-vitamin D3 . Arch. Biochem. Biophys. 197:90-95. 154. Hughes, M.R., P.F. Brumbaugh, M.R. Haussler, J.E. Wergedal, and D.J. Baylink (1975). Regulation of serum la,25-dihydroxyvitamin D3 by calcium and phosphate in the rat. Science 190:578-580. 155. Haddad, J.G., and J. Walgate (1976). 25-Hydroxyvitamin D transport in human plasma. J. Biol. Chem. 251:4803-4809. 156. Christakos, S., E.J. Friedlander, B.R. Frandsen, and A.W. Norman (1979). Studies on the mode of action of calciferol XIII. Development of a radioimmunoassay for vitamin D-dependent chick intestinal calcium-binding protein and tissue distribution. Endocrinology 104:1495-1503. 157. Jande, S.S., L. Maler, and D.E.M. Lawson (1981). Immunohistochemical mapping of vitamin D-dependent calcium-binding protein in brain. Nature 294:765-767. 158. Feldman, S.C., and S. Christakos (1983). Vitamin D-dependent calcium-binding protein in rat brain: biochemical and immunocytochemical characterization. Endocrinology 112:290-301. 159. Sar, M., W.L. Miller, and W.E. Stumpf (1981). Effects of 1,25-(OH)2 vitamin D3 on thyrotropin secretion in vitamin D deficient male rats. The Physiologist 24:70 (abstract A372). 160. Zafkova, I., J. Blahos, and J. Bednar (1981). Influence of 25-hydroxyvitamin D3 on thyrotropin and triiodothyronine plasma levels in man. Endokrinologie 78:118-121. 161. Blumberg, A., A. Wildbolz, C. Descoeudres, U. Hennes, M.A. Dambacher, J.A. Fischer, and P. Weidmann (1980). Influence of 1,25-dihydroxycholecalciferol on sexual dysfunction and related endocrine parameters in patients on maintenance hemodialysis. Clin. Nephrol. 13:208-214. 133 162. Suzuki, H., K. Kasai, S. Shimoda, K. Mori, and M. Miyasaka (1982). Improvement in abnormal secretion of thyrotropin and gonadotropin after restoration of serum calcium in pseudohypoparathyroidism. Endocrinol. Jpn. 29:69-75. 163. Honma, Y., M. Hozumi, E. Abe, K. Konno, M. Fukushima, S. Hata, Y. Nishii, H.F. DeLuca, and T. Suda (1983). la,25-Dihydroxyvitamin D3 and la-hydroxyvitamin D3 prolong survival time of mice innoculated with myeloid leukemia cells. Proc. Natl. Acad. Sci. USA 80:201-204. 164. Colston, K., M. Colston, and D. Feldman (1981). 1,25-Dihydroxyvitamin D3 and malignant melanoma: the presence of receptors and inhibition of cell growth in culture. Endocrinology 108:1083-1086. 165. Abe, E., C. Miyaura, H. Sakagami, M. Takeda, K. Konno, T. Yamazaki, S. Yoshiki, and T. Suda (1981). Differentiation of mouse myeloid leukemia cells induced by la,25-dihydroxyvitamin D3. Proc. Natl. Acad. Sci. USA 78:4990-4994. 166. Miyaura, C., E. Abe, T. Kuribayashi, H. Tanaka, K. Konno, Y. Nishii, and T. Suda (1981). la,25-Dihydroxyvitamin D3 induces differentiation of human myeloid leukemia cells. Biochem. Biophys. Res. Commun. 102:937-943. 167. Tanaka, H., E. Abe, C. Miyaura, T. Kuribayashi, K. Konno, Y. Nishii, and T. Suda (1982). la,25-Dihydroxycholecalciferol and a human myeloid leukaemia cell line (HL-60). (The presence of a cytosol receptor and induction of differentiation). Biochem. J. 204:713-719. 168. Vale, W., G. Grant, M. Amoss, R. Blackwell, and R. Guillemin (1972). Culture of enzymatically dispersed anterior pituitary cells: functional validation of a method. Endocrinology 91:562-572. 169. Soll , A.H. (1976). Hormonal regulation of hormone receptor concentration: a possible mechanism for altered sensitivity to hormones. In: Biogenesis and Turnover of Membrane Macromolecules. J.S. Cook (ed.). Raven Press, NY. pp. 179-205. 170. Tell, G.P., F. Haoar, and J.M. Saez (1978). Hormonal regulation of membrane receptors and cell responsiveness: a review. Metabolism 27:1566-1592. 171. 172. Tashjian, A.H., Jr., R. Osborne, D. Maina, and A. Knaian (1977). Hydrocortisone increases the number of receptors for thyroid-releasing hormone on pituitary cells in culture. Biochem. Biophys. Res. Commun. 79:333-340. Hirst, M., and D. Feldman (1982). Glucocorticoid regulation of 1,25 -(OH)2-vitamin D3 receptors: divergent effects on mouse and rat intestine. Endocrinology 111:1400-1402. 134 173. Tashjian, A.H., Jr., Y. Yasumura, L. Levine, G.H. Sato, and M.L. Parker (1968). Establishment of clonal strains of rat pituitary tumor cells that secrete growth hormone. Endocrinology 82:342-352. 174. Hatt, H.D. (managing editor) (1981). Catalogue of Strains II. American Type Tissue Collection (3rd edition). 12301 Parklawn Dr., Rockville, Maryland. 175. Tallo, D., and W.B. Malarkey (1981). Adrenergic and dopaminergic modulation of growth hormone and prolactin secretion in normal and tumor-bearing human pituitaries in monolayer culture. J. Clin. Endocrinol. Metab. 53:1278-1284. 176. Adams, R.L.P. (1980). Cell culture for biochemists. Volume 8 in the series: Laboratory techniques in biochemistry and molecular biology. Elsevier/North Holland Biomedical Press, Amsterdam. 177. Tashjian, A.H., Jr. (1979). Clonal strains of hormone-producing pituitary cells. Meth. Enzym. 58:527-535. 178. Lowry, 0.H., N.J. Rosebrough, A.L. Farr, and R.J. Randall (1951). measurement with the folin phenol reagent. J. Biol. Chem. 193:265-275. 179. Burton, K. (1956). A study of the conditions and mechanism of the diphenylamine reaction for the colorimetric estimation of deoxyribonucleic acid. Biochem. J. 62:315-323. 180. Clemens, T.L., N. Horiuchi, M. Nguyen, and M.F. Holick (1981). Binding of 1,25-dihydroxy-[ 3 H]vitamin D3 in nuclear and cytosol fractions of whole mouse skin in vivo and in vitro. FEBS Lett. 134:203-206. 181. Scatchard, G. (1949). The attractions of proteins for small molecules and ions. Ann. N.Y. Acad. Sci. 51:660-672. 182. Milligan, J.V., and J. Kraicer (1971). 4 5Ca uptake during the in vitro release of hormones from the rat adenohypophysis. Endocrinology 89:766-773. 183. Cheng, Y., and W.H. Prusoff (1973). Relationship between the inhibition constant (Ki) and the concentration of inhibitor which causes fifty percent inhibition (IC5 0 ) of an enzymatic reaction. Biochem. Pharmacol. 22:3099-3108. 184. Brown, B.W., Jr., and M. Hollander (1977). Statistics: A Biomedical Introduction. John Wiley & Sons, N.Y. Protein 185.. Haussler, M.R., S.C. Manolagas, and L.J. Deftos (1982). Receptor for 1,25-dihydroxyvitamin D3 in GH3 pituitary cells. J. Steroid Biochem. 16:15-19. 135 186. Birge, S.J., and D.H. Alpers (1973). Stimulation of intestinal mucosal proliferation by Vitamin D. Gastroenterology 64:977. 187. Bar-Shavit, Z., S.L. Teitelbaum, P. Reitsma, A. Hall, L.E. Pegg, J. Trial, and A.J. Kahn (1983). Induction of monocytic differentiation and bone resorption by 1,25-dihydroxyvitamin D3. Proc. Nat. Acad. Sci. USA 80:5907-5911. 188. McCarthy, D.M., J.F. San Miguel, H.C. Freake, P.M. Green, H. Zola, D. Catovsky, and J.M. Goldman (1983). 1,25-Dihydroxyvitamin D3 inhibits proliferation of human promyelocytic leukaemia (HL-60) cells and induces monocyte-macrophage differentiation in HL-60 and normal human bone marrow cells. Leukemia Res. 7:51-55. 189. Bhalla, A.K., E.P. Amento, T.L. Clemens, M.F. Holick, and S.M. Krane (1983). Specific high-affinity receptors for 1,25-dihydroxyvitamin D3 in human peripheral blood mononuclear cells: presence in monocytes and induction in T lymphocytes following activation. J. Clin. Endo. Metab. 57:1308-1310. 190. Reitsma, P.H., P.G. Rothberg, S.M. Astrin, J. Trial, Z. Bar-Shavit, A. Hall, S.L. Teitelbaum, and A.J. Kahn (1983). Regulation of myc gene expression in HL-60 leukaemia cells by a vitamin D metabolite. Nature 306:492-494. 191. Tanaka, H., E. Abe, C. Miyaura, T. Kuribayashi, K. Konno, Y. Nishii, and T. Suda (1982). la,25-Dihydroxycholecalciferol and a human myeloid leukaemia cell line (HL-60). The presence of a cytosol receptor and induction of differentiation. Biochem. J. 204:713-719. 192. Dodd, R.C., M.S. Cohen, S.L. Newman, and T.K. Gray (1983). Vitamin D metabolites change the phenotype of monoblastic U937 cells. Proc. Nat. Acad. Sci. USA 80:7538-7541. 193. Honma, Y., M. Hozumi, E. Abe, K. Konno, M. Fukushima, S. Hata, Y. Nishii, H.F. DeLuca, and T. Suda (1983). la,25-Dihydroxyvitamin D3 and la-hydroxyvitamin D3 prolong survival time of mice inoculated with myeloid leukemia cells. Proc. Nat. Acad. Sci. USA 80:201-204. 194. Abe, E., C. Niyaura, H. Sakagami, M. Takeda, K. Konno, T. Yamazaki, S. Yoshiki, and T. Suda (1981). Differentiation of mouse myeloid leukemia cells induced by la,25-dihydroxyvitamin D3. Proc. Nat. Acad. Sci. USA 78:4990-4994. 195.. Bar-Shavit, Z., D. Noff, S. Edelstein, M. Meyer, S. Shibolet, and R. Goldman (1981). 1,25-Dihydroxyvitamin D3 and the regulation of macrophage function. Calcif. Tiss. Int. 33:673-676. 196. Dokoh, S., C.A. Donaldson, S.L. Marion, J.W. Pike, and M.R. Haussler (1983). The ovary: A target organ for 1,25 dihydroxyvitamin D3. Endocrinology 112:200-206. 136 197. Kano, K., and G. Jones (1984). Direct in Vitro Effect of Thyroid Hormones on 25-Hydroxyvitamin D3 Metabolism in the Perfused Rat Kidney. Endocrinology 114:330-336. 198. Wark, J.D., and A.H. Tashjian, Jr. (1983). Regulation of Prolactin mRNA by 1,25-Dihydroxyvitamin D3 in GH4C1 Cells. J. Biol. Chem. 258:12118-12121. 199. Tornquist, K., and C. Lamberg-Allardt (1985). Effect of 1,25(OH)2D3, Verapamil, and EDTA-Infusion on the TSH-Response to TRH. In: Abstracts, Sixth Workshop on Vitamin D, Merano, Italy, March 17-22, 1985, pp.122. 200. Moriarty, C.M. (1977). Involvement of intracellular calcium in hormone secretion from rat pituitary cells. Mol. Cell. Endocrinol. 6:349. 201. Rubin, R.P. (1982). 202. DeLuca, H.F. (1979). Vitamin D: Metabolism and Function, In: Monographs on Endocri , F. Gross, M.M. Grumbach, A. Labhart, M.B. Lipsett, T. Mann, L.T. Samuels, and J. Zander (eds.), vol. 13, Springer-Verlag, Berlin & Heidelberg. 203. Norman, A.W. (1979). Vitamin D: The Calcium Homeostatic Steroid Hormone, Academic Press, New York. 204. Rasmussen, H. (1974). Parathyroid Hormone, Calcitonin, and the Calciferols, In: Textbook of Endocrinology, R.H. Williams (ed.), WB Saunders Co., Philadelphia. pp. 660-773. 205. Garabedian, M., M.F. Holick, and H.F. DeLuca (1972). Control of 25-hydroxycholecalciferol metabolism by parathyroid glands. Nat. Acad. Sci. USA 69:1673-1676. Calcium and Cellular Secretion, Plenum Press, N.Y. Proc. 206. Rasmussen, H., M. Wong, D. Bikle, and D.B.P. Goodman (1972). Hormonal control of the renal conversion of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalciferol. J. Clin. Invest. 51:2502-2504. 207. Fraser, D.R., and E. Kodicek (1973). Regulation of 25-hydroxycholecalciferol-1-hydroxylase activity in kidney by parathyroid hormone. Nature New Biol. 241:163-166. 208. Ohmdahl, J., M.F. Holick, T. Suda, Y. Tanaka, and H.F. DeLuca (1971). Biological Activity of 1,25-Dihydroxycholecalciferol. Biochemistry 10:2935-2940. - 209.. DeLuca, H.F. (1978). Vitamin D and calcium transport, In: Calcium Transport and Cell Function, A. Scarpa, and E. Carafoli (eds.), Ann. N.Y. Acad. Sci. 307:356-376. 137 210. Anghileri, L.J., and A.M. Tuffet-Anghileri (eds.) (1982). The Role of Calcium in Biological Systems, vols. 1-3, CRC Press, Boca Raton. 211. Rasmussen, H. (1981). New York. 212. Campbell, A.K. (1983). Intracellular Calcium: Regulator, Wiley, New York. 213. Adelstein, R.S. (1983). Regulation of contractile proteins by phosphorylation. J. Clin. Invest. 72:1863-1866. 214. Rasmussen, H. (1970). Cell communication, calcium ion, and cyclic adenosine monophosphate. Science 170:404-412. 215. Cohen, P. (1979). The hormonal control of glycogen metabolism in mammalian muscle by multivalent phosphorylation. Biochemical Soc. Trans. 7:459-480. 216. Greengard, P. (1978). Phosphorylated Proteins as Physiological Effectors. Science 199:146-151. 217. Liu, A.Y.-C., and P. Greengard (1976). Regulation by steroid hormones of phosphorylation of specific protein common to several target organs. Proc. Nat. Acad. Sci. USA 73:568-572. 218. Greenwood, F.C., W.M. Hunter, and J.S. Glover (1963). The Preparation of 1 3 1I-Labelled Human Growth Hormone of High Specific Radioactivity. Biochem. J. 89:114-123. 219. Chin, W.W., F. Maloof, and J.F. Habener (1981). Thyroid-stimulating Hormone Biosynthesis. J. Biol. Chem. 256:3059-3066. 220. Kruse, P.F., Jr., and M.K. Patterson, Jr. (eds.) (1973). Tissue Culture: Methods and Applications. pp.115-117. New York: Academic Press. 221. Krane, S.M., G.L. Brownell, J.B. Stanbury, and H. Corrigan (1956). The effect of thyroid disease on calcium metabolism in man. J. Clin. Invest. 35:874. 222. Cook, P.B., J.R. Nassim, and J. Collins (1959). The effects of thyrotoxicosis upon the metabolism of calcium, phosphorous, and nitrogen. Q. J. Med. 28:505. 223.. Shafer, R.B., and D.H. Gregory (1972). Calcium malabsorption in hyperthyroidism. Gastroenterology 63:235. 224. Singhelakis, P., C.C. Alevizaki, and D.G. Ikkos (1974). calcium absorption in hyperthyroidism. Metabolism Calcium and cAMP as synarchic messengers, Wiley, 138 Its Universal Role as Intestinal 23:311. 225. Bouillon, R., and P. DeMoor (1974). Parathyroid function in patients with hyper or hypothyroidism. J. Clin. Endocrinol. Metab. 38:999. 226. Mosekilde, L. (1979). Effect of Thyroid Hormone(s) on Bone Remodeling, Bone Mass and Calcium-Phosphorous Homeostasis in Man. Ph.D. Thesis, Aarhus Amtssygehus, Aarhus, Denmark. 227. Bouillon, R., E. Muls, and P. DeMoor (1980). Influence of thyroid function on the serum concentration of 1,25-dihydroxyvitamin D3. J. Clin. Endocrinol. Metab. 51:793. 228. Kano, K., H. Matsutani, N. Sakurada, Y. Iwakawa, A. Nonoda, J. Yata, E. Abe, and T. Suda (1980). Estimation by radioimmunoassay of 25-hydroxyvitamin D and 24,25-dihydroxyvitamin D and its clinical application to childhood disease. Bone Metab. (Tokyo) 13:93. 229. Jastrup, B., L. Mosekilde, F. Melsen, B. Lund, B. Lund, and O.H. Sorensen (1982). Serum levels of vitamin D metabolites and bone remodeling in hyperthyroidism. Metabolism 31:126. 230. Wasserman, R.H. (1980). Vitamin D-induced calcium binding proteins: an overview. In: Calcium-Binding Proteins: Structure and Function. F.L. Siegel (ed.) .pp.357-362. New York: Elsevier/North-Holland. 231. Spencer, R., M. Charman, J.S. Emtage, and D.E.M. Lawson (1976). Production and properties of vitamin-D-induced mRNA for chick calcium binding protein. Eur. J. Biochem. 71:399-409. 232. Bridges, K., R. Levenson, D. Housman, and L. Cantley (1981). Calcium regulates the commitment of murine erythroleukemia cells to terminal erythroid differentiation. J. Cell. Biol. 90:542-544. 233. Hennings, H., D. Michael, C. Cheng, P. Steinert, K. Holbrook, and S.H. Yuspa (1980). Calcium regulation of growth and differentiation of mouse epidermal cells in culture. Cell 19:245-254. 234. Rozengurt, E. (1979). Biochemical basis of the early events stimulated by serum and mitogenic factors in cultures of quiescent cells. In: Hormones and Cell Culture, G. Sato and R. Ross (eds.). pp.773-788. Cold Spring Harbor, New York: Cold Spring Harbor Lab Press. 235. Chafouleas, J.G., L. Lagace, W.E. Bolton, A.E. Boyd III, and A.R. Means (1984). Changes in calmodulin and its mRNA accompany reentry of quiescent (GO) cells into the cell cycle. Cell 36:73-81. 236. Dedman, J.R., T. Lin, J.M. Marcum, B.R. Brinkley, and A.R. Means (1980). Calmodulin: Its role in the mitotic apparatus. In: Calcium-Binding Proteins: Structure and Function, F.L. Siegel (ed.). pp.181-188. New York: Elsevier/North-Holland. 237. Hidaka, H., Y. Sasaki, T. Tanaka, T. Endo, S. Ohno, Y. Fujii, and T. Nagata (1981). N-(6-Aminohexyl)-5-chloro-1-naphthalenesulfonamide, 139 a calmodulin antagonist, inhibits cell proliferation. Acad. Sci. USA 78:4354-4357. Proc. Nat. 238. Delbeke, D., J.G. Scammell, and P.S. Dannies (1984). Difference in Calcium Requirements for Forskolin-Induced Release of Prolactin from Normal Pituitary Cells and GH4C 1 Cells in Culture. Endocrinology 114:1433-1440. 239. Stachura, M.E. (1982). Sequestration of an Early-Release Pool of Growth Hormone and Prolactin in GH 3 Rat Pituitary Tumor Cells. Endocrinology 111:1769-1777. 240. Tashjian, A.H., Jr. (1979). Clonal Strains of Hormone-Producing Pituitary Cells. Methods in Enzymology 58:527-535. 140 BIOGRAPHICAL NOTE Stanley David Rose was born on February 2, 1956, in New York, New York. raised in Greenburgh, New York, and attended Woodlands High School. He was During his senior year, he was awarded his high school's math award, and a New York State Regents Scholarship. In September, 1974, he enrolled at Cornell University. was awarded the Bachelor of Arts degree in psychology in May, 1978. He The following year he worked at Harvard Medical School, as a research assistant for Dr. Peter Dews in the Psychobiology Laboratory. In September, 1979, he enrolled in the graduate program in Neural and Endocrine Regulation at the Massachusetts Institute of Technology. While pursuing his doctorate, he was awarded fellowships by the National Institute of Drug Abuse and the National Institute of Mental Health. He was also a National Institutes of Health graduate trainee. 141