O R I G I N A L P A... Abstract This study investigated personality and Introduction
advertisement

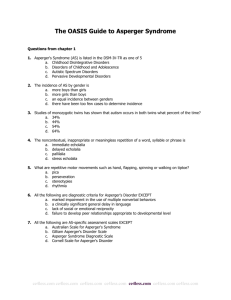
J Autism Dev Disord (2007) 37:847–854 DOI 10.1007/s10803-006-0212-0 ORIGINAL PAPER Psychological and Neurobehavioral Comparisons of Children with Asperger’s Disorder Versus High-Functioning Autism Linda L. Thede Æ Frederick L. Coolidge Published online: 15 September 2006 Ó Springer Science+Business Media, Inc. 2006 Abstract This study investigated personality and neurobehavioral differences between 16 children with Asperger’s Disorder, 15 children with High-Functioning Autism (HFA), and 31 controls, all ranging in age from 5–17 years, M age = 10.7 years, SD = 3.0. Parents rated their children’s behaviors on a 44-item autistic symptoms survey and on the 200-item Coolidge Personality and Neuropsychological Inventory (Coolidge, Thede, Stewart, & Segal (2002a). The Coolidge Personality and Neuropsychological Inventory for Children (CPNI): Preliminary psychometric characteristics. Behavior Modification, 26, 550–566). The results indicated that the two clinical samples were significantly elevated on the Executive Function Deficits scale and Attention-Deficit/Hyperactivity Disorder (ADHD) scale compared to controls. There were more similarities than differences between the two clinical samples on the personality scales, although the Asperger’s group scored significantly on the two scales with anxiety components. Keywords Asperger’s disorder Æ High-functioning autism Æ Coolidge personality and neuropsychological inventory Æ Executive functions deficits scale Æ Autism Æ Personality disorders L. L. Thede Æ F. L. Coolidge (&) Psychology Department, University of Colorado at Colorado Springs, P.O. Box 7150, Colorado Springs, CO 80933-7150, USA e-mail: fcoolidg@uccs.edu Introduction Asperger’s Disorder is categorized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IVTR; American Psychiatric Association, 2000) as a pervasive developmental disorder. Children with Asperger’s Disorder typically exhibit severe and chronic impairments in social interactions, restrictive and repetitive patterns of behaviors, interests, and activities, and significant impairment in social, occupational, and other areas of functioning. Asperger’s Disorder, however, differs from Autistic Disorder in DSM-IV-TR only in that it specifically excludes cognitive and language delays. Asperger’s Disorder is also thought to have a greater prevalence than Autistic Disorder, occurring in 26–36 cases per 10,000 children as opposed to Autistic Disorder which may occur in as few as 4–5 cases per 10,000 (Fombonne, 1999) to as many as 5–16 cases per 10,000 children (Ehlers & Gillberg, 1993; Wing, 1993). High-Functioning Autism (HFA), although it appears frequently in the literature, is not listed as an official DSM-IV-TR diagnosis. The diagnosis of HFA has typically been used to describe individuals with Autistic Disorder that have an IQ above the mentally retarded range (>69), are verbally higher functioning, and presumably require a different treatment approach. Whether HFA and Asperger’s Disorder are the same or different disorders remains controversial (see Schopler & Mesibov, 1998; Tonge, Brereton, Gray, & Einfeld, 1999, for more complete discussions). Currently, most individuals diagnosed with Autistic Disorder are not high functioning. This may, however, be an artifact, because severe cases of autism are more likely to be recognized and diagnosed 123 848 and because of the historical confusion over the validity of HFA and Asperger’s Disorder as separate diagnostic entities. It is estimated that 75% of individuals diagnosed with Autistic Disorder will have IQ’s below 70, and up to 50% of them are mute or severely lacking in communication skills (Pennington, 2002), whereas individuals with Asperger’s Disorder often score high on intelligence tests. Despite the wide range of cognitive abilities among individuals with all these disorders, as noted by Pennington (2002), social impairments may actually be the primary psychological deficit in all autism spectrum disorders. Interestingly, Asperger’s original conception of his eponymous syndrome, which he described as a personality disorder, emphasized the clinical presentation of the children, that is, their well-preserved language skills and intellectual and cognitive abilities, yet coupled with profound social impairments. Wolff (2000) has noted that these impairments often manifest themselves clinically as schizoid personality disorder. Tonge et al. (1999) found that their Asperger’s Disorder group demonstrated elevated levels of disruptive behavior, anxiety, social-relating problems, and antisocial behavior when compared to an HFA group. Obsessive–compulsive features of Asperger’s Disorder have also been noted by Tantam (2000) as well as the comorbidity of Asperger’s Disorder with the anxious (avoidant) personality disorder of ICD-10 (World Health Organization, 1992) and social anxiety. Whenever Asperger’s Disorder is also accompanied by oversensitivity, Tantum suggested a diagnosis of narcissistic personality disorder. Finally, he noted that the paranoid personality disorder, because of its eccentricity and lack of empathy for others, may sometimes be mistaken for Asperger’s Disorder. He noted, however, that all of these personality disorders may occur in the autism spectrum, making the differential diagnosis of Asperger’s Disorder particularly difficult. Gillott, Furniss, and Walter (2001) have also noted high anxiety and obsessive–compulsive features in a group of high-functioning autistic children (with no current language impairments), but it was unclear whether they tested only HFA and omitted individuals with Asperger’s Disorder from their sample. Although children with Asperger’s Disorder do not have glaring deficits in intellect, language, and cognition, there is some evidence (Ozonoff, Pennington, & Rogers, 1991) that Asperger’s Disorder may exhibit symptoms of frontal lobe dysfunction, specifically executive function (EF) deficits on traditional laboratory measures. Because social behavior requires decision-making abilities and the anticipation of 123 J Autism Dev Disord (2007) 37:847–854 consequences, it is highly likely that Asperger’s Disorder would be associated with EF deficits. Deficits in EF in childhood have already been established in some psychological and neuropsychological syndromes, e.g., frontal lobe damage or lesions, attention-deficit/hyperactivity disorder (ADHD), Tourette’s syndrome, and borderline personality disorder features in children (Coolidge, Segal, Stewart, & Ellett, 2000a; Pennington & Ozonoff, 1996). In adults, Raine, Sheard, Reynolds, and Lencz (1992) have found evidence of prefrontal cortical dysfunction associated with schizotypal personality features in a normal population. There is also some evidence of cognitive processing deficits attributable to the frontal lobes in the antisocial personality disorder (e.g., Deckel, Hesselbrock, & Bauer, 1996; Elliott & Gillett, 1992; see Millon & Davis, 1996, for a review of this area). Several studies have also linked EF deficits to autism, but the role of EF deficits specifically in Asperger’s Disorder is unclear. In a review of 14 studies of EF deficits in autism, Pennington and Ozonoff (1996) found that 13 of the studies provided evidence of EF deficits on at least one EF measure. In one of the first studies that attempted to differentiate between Asperger’s Disorder and HFA, Ozonoff et al. (1991) found that both groups showed EF impairments but concluded that HFA and Asperger’s Disorder could be distinguished because only the HFA patients demonstrated deficits in theory of mind and verbal memory. In a more recent review of EF deficits in autism and other disorders, Ozonoff (1997) concluded that there appears to be a converging body of evidence suggesting that the central cognitive deficit in autism may be EF. However, it is unclear whether those deficits are consistent throughout the autism spectrum, whether each disorder embodies deficits in different domains of executive functioning, or whether EF deficits are predominantly associated with the more cognitively impaired individuals with Autistic Disorder. The early behavior problems and socially inappropriate behaviors found in Asperger’s Disorder can also be mistaken for ADHD. It has been established that EF may also be a core deficit in ADHD (e.g., Mattes, 1980; Ozonoff, 1997; Pennington & Ozonoff, 1996; Zametkin & Rapoport, 1986), and therefore, it would not be surprising to see symptoms of ADHD in the autism spectrum. Recently, ADHD and autism have both been linked to a genetic marker on chromosome 16 (locus 16p13; Smalley et al., 2002) indicating a shared genetic association or possible common etiology. The autism spectrum of disorders is already known to be highly heritable (for a review of these studies, see Pennington, 2002), and ADHD has a well-established heritability J Autism Dev Disord (2007) 37:847–854 (e.g., .82, Coolidge, Thede, & Young, 2000b; .76, Stevenson, 1992). There is also preliminary evidence that EF deficits are highly heritable (.77; Coolidge et al., 2000a, b), and a bivariate heritability has also been demonstrated between EF deficits and childhood personality disorder features (Coolidge, Thede, & Jang, 2004). The co-occurrence of EF deficits, ADHD symptoms, and other personality disorder features within autism spectrum disorders warrants further investigation. Therefore, the purpose of the present study was to compare Asperger’s Disorder and HFA children on parent-rated measures of psychological disorders, EF deficits, and ADHD in order to determine patterns of similarities and differences. Ghaziuddin et al. (1994), in a review of the literature of Asperger’s Disorder, found that about 50% of the studies referred to impaired motor functioning such as clumsiness and uncoordinated movement patterns, thus another purpose of the present study was to determine whether there might be impaired motor functioning differences between Asperger’s and HFA children. Method Participants and Procedures Participants were recruited from a registry of the Autism Society of America (www.autism-society.org). The authors requested the names of parents who had children (1) between the ages of 5 and 17 years and (2) that registered their children because they were diagnosed by a clinician as having Asperger’s Disorder or HFA. The authors received contact information for 125 parents who were then contacted by mail. Seventysix parents responded (61% of those originally contacted) and gave their written informed consent, supplied the authors with the child’s official clinical diagnosis, completed a 44-item survey of autistic symptoms created by the authors, and completed the 200-item Coolidge Personality and Neuropsychological Inventory (CPNI; Coolidge, 1998; Coolidge, Thede, Stewart, & Segal, 2002a). Measures The 44-item survey of autistic symptoms (see Appendix) was created from the general literature on autistic, Asperger’s Disorder, and HFA symptomatology, and from DSM-IV-TR criteria for pervasive developmental disorders. The items are broadly clustered into four content areas: socialization (with 849 items measuring interactions with others, friendships, social adeptness), speech (measuring delayed speech development, misinterpretations, inflection, misuse of pronouns), nonverbal communication (gesture use, appropriate facial expressions, body language, eye contact), and repetitive/stereotyped behaviors (single, highly focused interests, repetitive hand or body gestures, intense dislike of change, exceptional sensitivity to sensory stimuli, motor clumsiness). The internal scale reliability (Cronbach’s alpha) of the survey on a normative sample of convenience (n = 88) was .98. The internal scale reliabilities for the four content areas were .89 for socialization, .90 for speech, .95 for nonverbal communication, and .90 for repetitive/stereotyped behaviors. The test-retest reliability (one week interval) on the normative sample was .93. The CPNI is a 200-item parent-as-respondent inventory. It was designed to assess personality and neurobehavioral deficits according to criteria specified in the DSM-IV-TR. The CPNI contains four Axis I scales (Generalized Anxiety Disorder, Major Depressive Disorder, Oppositional Defiant Disorder, and ADHD). It also contains 12 personality disorder scales (10 from Axis II, plus 2 from Appendix B of DSM-IVTR). The CPNI has a 44-item EF Deficits scale that measures three major content areas: decision-making difficulties, metacognitive problems (learning, memory, and language), and social inappropriateness. The CPNI normative sample consists of 780 children, ages 5–17 years old. The CPNI uses a 4-point Likert scale for each item ranging from (1) strongly false to (4) strongly true. The general construct validity of the CPNI scales has been demonstrated in a variety of clinical and non-clinical empirical studies (Coolidge, Aksamit, & Becker, 1994; Coolidge et al., 1992, 2002a, b; Coolidge, Thede, & Jang, 2001), and it has good reliability and validity (see Coolidge et al., 2002a, b, for details). Final Sample Selection Based on the parents’ reports of the children’s clinical diagnoses and the 44-item autistic symptom survey, it was determined that 16 children met criteria for Asperger’s Disorder (which meant that there were no reported language delays and mental retardation, i.e., an IQ < 70). It was determined that 15 children met the authors’ criteria for HFA (i.e., parent reported diagnosis of HFA, all had language delays, but no parent reported that their child had been given a clinical diagnosis of mental retardation). 123 850 J Autism Dev Disord (2007) 37:847–854 The final Asperger’s Disorder group (n = 16) consisted of 13 boys (M age = 11.8 years, SD = 3.0) and 3 girls (M age = 10.3 years, SD = 3.1). The HFA group (n = 15) consisted of 8 boys (M age = 10.4 years, SD = 4.0) and 7 girls (M age = 9.6 years, SD = 2.8). An age and gender matched control sample (n = 31) was selected from the CPNI normative sample (Coolidge et al., 2002a). The final sample (n = 61) consisted of 42 boys and 19 girls who ranged in age from 5 to 17 years, M age = 10.5 years, SD = 3.2. The parents reported their ethnicity as white (n = 49), Hispanic (n = 5), black (n = 3), or other (n = 4). Results Axis I Scales A summary of one factor analyses of variance (ANOVA’s), effect sizes (partial eta squared), Tukey’s post hoc tests, and T score means on the four Axis I disorders appear in Table 1. The table reveals that the Asperger’s and HFA groups differed on only one scale, Generalized Anxiety Disorder. The Asperger’s group was significantly more anxious than the HFA group. The Asperger’s and HFA groups were not significantly different from each other on the ADHD scale (and its two subscales, Inattention and Hyperactivity-Impulsivity), but both groups were significantly more elevated than the control group. Axis II Scales See Table 1 for a summary of these analyses. Of the 12 personality disorder scales, 9 were significantly different among the three groups. The Asperger’s and HFA groups differed significantly on 3. The children in the Asperger’s group were significantly higher than the HFA group on the Obsessive–Compulsive, Avoidant, and Depressive personality disorder scales. Importantly, there were no significant differences between these two groups on the Schizoid and Schizotypal scales, although both groups were significantly more Table 1 ANOVA’s, Tukey’s post hoc test results, and descriptive statistics (T scores) for the Axis I scales, Axis II scales, EF deficits scale and subscale of the CPNI CPNI scale Axis I scales Generalized anxiety dis. Oppositional defiant dis. Major depressive dis. ADHD Inattention Hyperactivity/imp ulsivity Axis II scales Avoidant Borderline Conduct disorder Dependent Depressive Histrionic Narcissistic Obsessive–compulsive Paranoid Passive–aggressive Schizotypal Schizoid Neuropsychological scales EF deficits Decision-making difficulties Metacognitive problems Social inappropriateness Controls n = 31 Mean (SD) Asperger n = 16 Mean (SD) HFA n = 15 Mean (SD) F(2,59) P g2 49.8a (8.8) 48.7 (9.8) 50.0a (11.1) 50.2a (10.4) 50.7a (10.1) 47.3a (10.3) 63.8b (17.5) 55.5 (14.0) 61.5b (12.7) 69.6b (9.8) 67.0b (9.4) 67.8b (11.1) 53.5a (10.7) 53.2 (8.7) 58.5a,b (9.8) 66.1b (10.1) 62.8b (9.1) 65.9b (12.5) 7.27 2.32 6.44 23.80 17.57 18.98 < .002 .107 < .003 < .001 < .001 < .001 .20 .07 .18 .45 .37 .39 49.9a (8.9) 50.5a (9.9) 50.7 (10.7) 51.9a (11.4) 47.7a (8.6) 49.6a (10.3) 46.0a (7.4) 47.9a (9.8) 49.3 (11.1) 49.4 (9.3) 51.8a (11.9) 51.0a (10.4) 60.8b (16.8) 62.6b (10.2) 48.3 (6.3) 62.7b (13.7) 56.1b (15.0) 57.5b (6.4) 53.4b (8.5) 65.5b (10.6) 49.8 (14.6) 54.2 (11.8) 75.2b (15.9) 68.4b (15.8) 50.6a (11.6) 58.8b (10.6) 50.0 (13.2) 54.2a,b (9.6) 44.2a (9.6) 55.5a,b (9.3) 50.2a,b (5.7) 53.8a (11.4) 43.6 (7.4) 47.3 (8.4) 78.4b (16.4) 71.9b (19.1) 4.74 8.42 0.28 4.62 5.21 4.58 5.61 15.13 1.50 2.03 24.40 13.97 .012 .001 .759 .014 .008 .014 .006 < .001 .231 .140 < .001 < .001 .14 .22 .01 .14 .15 .13 .16 .34 .05 .06 .45 .32 46.0a 47.5a 45.9a 46.1a 61.7b 61.1b 60.7b 61.7b 60.5b 60.0b 59.3b 61.3b 34.43 16.74 31.78 32.88 < .001 < .001 < .001 < .001 .54 .36 .52 .53 (7.1) (8.5) (7.2) (6.6) (6.7) (9.7) (6.1) (7.0) (7.8) (8.8) (7.5) (9.5) Note: Different superscripts indicate significant differences; common superscripts indicate no significant difference according to Tukey’s post hoc tests (P < .05). Also, g2 is interpreted as the proportion of variance in the dependent variable that is attributable to the independent variable (.01 = small effect, .06 = moderate effect, .14 = large effect; Cohen, 1988) 123 J Autism Dev Disord (2007) 37:847–854 elevated on the latter two scales than the controls with very large effect sizes. EF Deficit Scales See Table 1 for the results of the analyses for the EF Deficit scales. There were no significant differences between the Asperger’s and HFA groups on the overall EF Deficit scale or on its three subscales. However, in all four comparisons, these two groups were significantly more elevated than the controls, again with substantial effect sizes. Motor Clumsiness The 44-item survey contained two items (#28 and #44) specifically assessing motor clumsiness (see the appendix to view the 44-items). The answers to these two items were first summed to form a continuous scale ranging from 2 to 8. They were also combined to form a dichotomous scale, evidence for motor clumsiness or no evidence for motor clumsiness. A t test for independent groups on the continuous scale revealed no significant differences between the two clinical groups’ means, t (29) = -.378, p > .25. A chi square test on the dichotomous scale revealed no significant differences between the two clinical groups, v2 (1, n = 31) = .11, p > .25. Nonetheless, evidence of motor clumsiness was found in 94% of the Asperger’s children and 80% of the HFA children as reported by their parents. Discussion The results of this study at least partially support the findings in the Tonge et al. (1999) study that found some distinctions between Asperger’s and HFA children. In the present study, as in the Tonge et al. study, the children with Asperger’s Disorder did have higher levels of some types of psychopathology. However, unlike the Tonge et al. findings, the Asperger’s group was not more disruptive or antisocial. The present study did find support for the Tonge et al. finding that Asperger’s children were more anxious than HFA children. Of the four Axis I CPNI scales, the Asperger’s group was significantly higher than the HFA group on the Generalized Anxiety Disorder scale, and their mean T score (64) placed them in a clinically elevated range. Further analysis revealed that 10 of the 16 Asperger’s children (63%) were elevated at least one standard deviation above the normative mean (approximately the 84th percentile or greater) on the Generalized Anxiety Disorder scale; whereas only 4 of 851 the 15 HFA children (27%) were elevated above one standard deviation. In contrast to the findings of the Tonge et al. (1999) study, the Asperger’s children were not more disruptive or antisocial, at least as measured by the CPNI Borderline, Conduct Disorder, and Passive–Aggressive personality disorder scales and the Oppositional Defiant Disorder scale. Of special interest is the finding that the two clinical groups and the control group did not significantly differ on the Conduct Disorder and the Oppositional Defiant Disorder scales. Recently, ADHD and autism have both been linked to a genetic marker on chromosome 16 (loci 16p13; Smalley et al., 2002) indicating a possible shared genetic association or common etiology. The autism spectrum of disorders is already known to be highly heritable (for a review of these studies, see Pennington, 2002), and ADHD has a well-established heritability (e.g., .82, Coolidge et al., 2000b; .76, Stevenson, 1992). In the present study, both clinical groups were significantly elevated on the ADHD scale beyond the control group, but there were no significant differences between the two clinical groups. In fact, with the exception of the Schizotypal and Schizoid personality disorder scale elevations for the two clinical groups, the elevations on the ADHD scale were the third highest in the study. This pattern also held for the Inattention subscale and for the Hyperactivity-Impulsivity subscale. Because recent research (Rinehart, Bradshaw, Brereton, & Tonge, 2002) has found EF differences between Asperger’s and HFA groups and because EF deficits are thought to be a core problem in ADHD (e.g., Pennington, 2002), it was interesting to find that both clinical groups were significantly elevated on the EF Deficits scale as compared to the control group, but there were no differences between the two clinical groups. The latter pattern was true of the overall 44item EF Deficits scale and true, as well, for the Decision-Making Difficulties, the Metacognitive Problems, and Social Inappropriateness subscales. This finding is not necessarily in disagreement with the Rinehart et al. study, as there are many different measures of executive functioning and no single ‘‘gold standard.’’ Furthermore, the CPNI EF Deficits scale focuses primarily on deficits in functioning, while the Rinehart et al. study focused on right and left hemisphere differences in functioning between the two clinical groups. As expected, the Asperger’s and HFA groups were significantly elevated above the control group but not significantly different from one another on the Schizoid and Schizotypal personality disorder scales, and these elevations were the highest observed in this study. This 123 852 pattern was true, as well, for the Borderline personality disorder scale. The Asperger’s group, however, was significantly higher than the HFA group on the Obsessive–Compulsive, Avoidant, and Depressive personality disorder scales. All three of the latter scales do have a component of anxiety, thus they may have been elevated in the Asperger’s group because of that component. Certainly, the latter finding warrants further investigation. With regard to motor clumsiness, a large percentage of parents in both clinical groups reported evidence for clumsy motor movements; however, there were no significant differences between the two groups. This finding would seem to counter arguments that Asperger’s children could be differentiated from HFA children on the basis of greater clumsiness, although the finding supports contentions that motor clumsiness is highly present in the autism spectrum. Limitations of the present study included small sample sizes, using only one parent as the predominant informant, a lack of clinical corroboration as to the diagnoses (although the 44-item survey of autistic symptoms did appear to support the parents’ reports of their children’s diagnoses), and a lack of traditional EF deficits and ADHD measures. The EF Deficits scale of the CPNI was created from contemporary literature and, consequently, includes symptoms of inattention and problems with set shifting. Thus, the ADHD scale and the EF Deficits scale have some overlapping items. Therefore, caution must be urged when interpreting these elevations in the two clinical groups. In summary, it appears that the most fruitful evidence for distinctions between Asperger’s and HFA children exists in their difference in anxiety level. The present study found no evidence for the current hypothesis that the two clinical groups may be distinguishable by greater disruptiveness and motor clumsiness in Asperger’s Disorder. The present study also supports contentions that disorders in the autism spectrum may be associated with EF deficits and ADHD. However, there was no evidence that the two clinical disorders may be distinguished on this basis. Overall, the findings might temper the myth that Asperger’s Disorder is a milder form of autism. The greater anxiety that appeared in the Asperger’s group might indicate that these children have a greater awareness of their problems and the negative consequences of their behaviors than HFA children. Acknowledgment An earlier version of this paper served as a master’s thesis for Linda Thede. The authors wish to thank all of the parents from the registry of the Autism Society of America who participated so graciously in the study. 123 J Autism Dev Disord (2007) 37:847–854 Appendix Survey of Autistic Symptoms Please rate each item on the following scale. Try to answer how your child has behaved for most of his/her life or what appears to be characteristic of how your child acts most of the time. 1 2 3 4 = = = = Strongly False More False Than True More True Than False Strongly True Socialization 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. My child has no close friends. My child tends to avoid activities involving other children. My child is a loner. My child has trouble developing friendships with other children. My child is socially clumsy or awkward. My child has trouble understanding the feelings of others. My child acts inappropriately with other children. My child seems emotionally cold or detached. My child approaches others only when he/she needs something for himself/herself. My child points out things to me that he/she is interested in. My child brings me things that he/she is interested in. _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ Speech & Language 12. 13. 14. 15. 16. 17. 18. 19. 20. My child’s speech development was delayed (e.g., not using single words by age 2 and unable to use simple phrases by age 3). My child misinterprets what other people say. My child has difficulty understanding common expressions such as ‘‘If looks could kill,’’ ‘‘I’m history,’’ or ‘‘Has the cat got your tongue?’’ My child sounds like a ‘‘walking dictionary’’ or encyclopedia. My child talks too much. My child talks too little. My child has trouble following conversations. My child has a strange or unusual rhythm or inflection when he/she speaks. My child repeats over and over exactly what is said to him/her. _____ _____ _____ _____ _____ _____ _____ _____ _____ J Autism Dev Disord (2007) 37:847–854 21. 22. 23. My child misuses pronouns like substituting ‘‘I’’ for ‘‘you,’’ ‘‘him’’ for ‘‘me,’’ or ‘‘her’’ for ‘‘me.’’ My child has trouble starting or maintaining conversations with others. My child has trouble playing like other children his or her age (for example, pretending or make-believe). 853 _____ 41. _____ 42. 43. _____ 44. My child is intensely fascinated with items involving transportation such as trains, planes, ships, cars, or roads. My child has an intense dislike of change. My child is exceptionally sensitive to lights, sounds, tastes, touch, or smells. My child is uncoordinated or clumsy. _____ _____ _____ _____ References Nonverbal Communication 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. My child has limited use of gestures compared to other children. My child has inappropriate or exaggerated facial expressions. When talking to others, my child comes up too close to other people. My child has a limited number of facial expressions compared to other children. My child has large, clumsy or inappropriate body language or gestures. My child is unable to give messages with his/her eyes. My child has difficulty making or maintaining eye contact. My child has a strange or weird handshake (or doesn’t shake hands at all). My child has trouble using his hands to express himself/herself. My child has trouble reading other people’s facial expressions. My child is unaware of what he/she is communicating to others with his/her body language. My child has trouble hugging or kissing people. _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ Repetitive/Stereotyped Behavior 36. 37. 38. 39. 40. My child gets intensely interested or preoccupied with a single subject and doesn’t seem to want to do anything else. My child has to stick to some useless routine and gets angry if it is changed. My child uses some hand or body gestures over and over (for example, hand flapping or finger twisting). My child gets preoccupied or interested with parts of objects or just one aspect of a toy (for example, how it feels or a noise that it might make). My child doesn’t seem to be as interested in as many different things as other children. _____ _____ _____ _____ _____ American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed.-text revised). Washington, DC:Author. Coolidge, F. L. (1998). Coolidge Personality and Neuropsychological Inventory for Children: CPNI. Colorado Springs, CO: Author. Coolidge, F. L., Aksamit, C. R., & Becker, L. A. (1994). Prediction of recidivism in juvenile offenders. Indian Journal of Psychological Issues, 2, 1–6. Coolidge, F. L., Reilman, B. J., Becker, L. A., Cass, V. J., Coolidge, R. L., & Stocker, R. (1992). Emotional problems and neuropsychological symptoms in non-violent juvenile offenders. Journal of Personality and Clinical Studies, 8, 7– 13. Coolidge, F. L., Segal, D. L., Stewart, S. E., & Ellett, J. A. C. (2000). Neuropsychological dysfunction in children with borderline personality disorder features: A preliminary investigation. Journal of Research in Personality, 34, 554– 561. Coolidge, F. L., Thede, L. L., & Jang, K. L. (2001). Heritability of personality disorders in childhood: A preliminary investigation. Journal of Personality Disorders, 15, 33–40. Coolidge, F. L., Thede, L. L., & Jang, K. L. (2004). Are personality disorders psychological manifestations of executive function deficits? Behavior Genetics, 34, 73–82. Coolidge, F. L., Thede, L. L., Stewart, S. E., & Segal, D. L. (2002). The Coolidge Personality and Neuropsychological Inventory for Children (CPNI): Preliminary psychometric characteristics. Behavior Modification, 26, 550–566. Coolidge, F. L., Thede, L. L., & Young, S. E. (2000). Heritability and the comorbidity of attention deficit hyperactivity disorder with behavioral disorders and executive function deficits: A preliminary investigation. Developmental Neuropsychology, 17, 273–287. Coolidge, F. L., Thede, L. L., & Young, S. E. (2002). The heritability of gender identity disorder in a child and adolescent twin sample. Behavior Genetics, 32, 251–257. Deckel, A. W., Hesselbrock, V., & Bauer, L. (1996). Antisocial personality disorder, childhood delinquency, and frontal brain functioning: EEG and neuropsychological findings. Journal of Clinical Psychology, 52, 639–650. Ehlers, S., & Gillberg, C. (1993). The epidemiology of Asperger syndrome: A total population study. Journal of Child and Adolescent Psychiatry, 34, 1327–1350. Elliott, C., & Gillett, G. (1992). Moral insanity and practical reason. Philosophical Psychology, 5, 53–67. Fombonne, E. (1999). The epidemiology of autism: A review. Psychological Medicine, 29, 769–786. Ghaziuddin, M., Butler, E., Tsai, L., & Ghaziuddin, N. (1994). Is clumsiness a marker for Asperger’s syndrome? Journal of Intellectual Disability Research, 38, 519–527. Gillott, A., Furniss, F., & Walter, A. (2001). Anxiety in highfunctioning children with autism. Autism, 5, 277–286. 123 854 Mattes, J. A. (1980). The role of frontal lobe dysfunction in childhood hyperkinesis. Comprehensive Psychiatry, 21, 358– 369. Millon, T., & Davis, R. D. (1996). Disorders of personality DSMIV and beyond. New York: Wiley & Sons. Ozonoff, S. (1997). Components of executive function in autism and other disorders. In J. Russell (Ed.), Autism as an executive disorder (pp. 179–211). New York: Oxford University Press. Ozonoff, S., Pennington, B. F., & Rogers, S. J. (1991). Asperger syndrome: Evidence of an empirical distinction from highfunctioning autism. Journal of Child Psychology and Psychiatry, 32, 1107–1122. Pennington, B. (2002). The development of psychopathology. New York: Guilford Press. Pennington, B. F., & Ozonoff, S. (1996). EF and developmental psychopathology. Journal of Child Psychology & Psychiatry, 37, 51–87. Pennington, B. F., Rogers, S. J., Bennetto, L., Griffith, E. M., Reed, D. T., & Shyu, V. (1997). Validity tests of the executive dysfunction hypothesis of autism. In J. Russell (Ed.), Autism as an executive disorder. New York: Oxford University Press. Raine, A., Sheard, C., Reynolds, G. P., & Lencz, T. (1992). Prefrontal structural and functional deficits associated with individual differences in schizotypal personality. Schizophrenia Research, 7, 237–247. Rinehart, N. J., Bradshaw, J. L., Brereton, A. V., & Tonge, B. J. (2002). Lateralization in individuals with high-functioning autism and Asperger’s disorder: A frontostriatal model. Journal of Autism and Developmental Disorders, 32, 321–332. 123 J Autism Dev Disord (2007) 37:847–854 Schopler, E., & Mesibov, G. B. (1998). Asperger syndrome or high-functioning autism? New York: Plenum Press. Smalley, S. L., Kustanovih, V., Minassian, S. L., Stone, J. L., Ogdie, M. N., McGough, J. J., McCracken, J. T., MacPhie, I. L, Francks, C., Fisher, S. E., Cantor, R. M., Monaco, A. P., & Nelson, S. F. (2002). Genetic linkage of attention-deficit/ hyperactivity disorder on chromosome 16p13, in a region implicated in autism. American Journal of Human Genetics, 71, 959–963. Stevenson, J. (1992). Evidence for a genetic etiology in hyperactivity in children. Behavior Genetics, 22, 337–344. Tantam, D. (2000). Adolescence and adulthood of individuals with Asperger syndrome. In A. Klin, F. R. Volkmar, & S. S. Sparrow, (Eds.), Asperger syndrome (pp. 367–399). New York: The Guilford Press. Tonge, B. J., Brereton, A. V., Gray, K. M., & Einfeld, S. L. (1999). Behavioural and emotional disturbance in highfunctioning autism and Asperger syndrome. Autism, 3, 117– 130. Wing, L. (1993). The definition and prevalence of autism: A review. European Child & Adolescent Psychiatry, 2, 61–74. Wolff, S. (2000). Schizoid personality in childhood and Asperger syndrome. In A. Klin, & F. R. Volkmar, (Eds.), Asperger syndrome (pp. 278–305). New York: The Guilford Press. World Health Organization (1992). ICD: The ICD-10 classification of mental and behavioural disorders—clinical descriptions and diagnostic guidelines. Geneva: WHO. Zametkin, A. J., & Rapoport, J. L. (1986). The pathophysiology of attention deficit disorders. In B.B. Lahey, & A. E. Kadzin, (Eds.), Advances in clinical child psychology. New York: Plenum.