Computer Laboratory Worksheet: The Determinants of Cardiac Function
advertisement
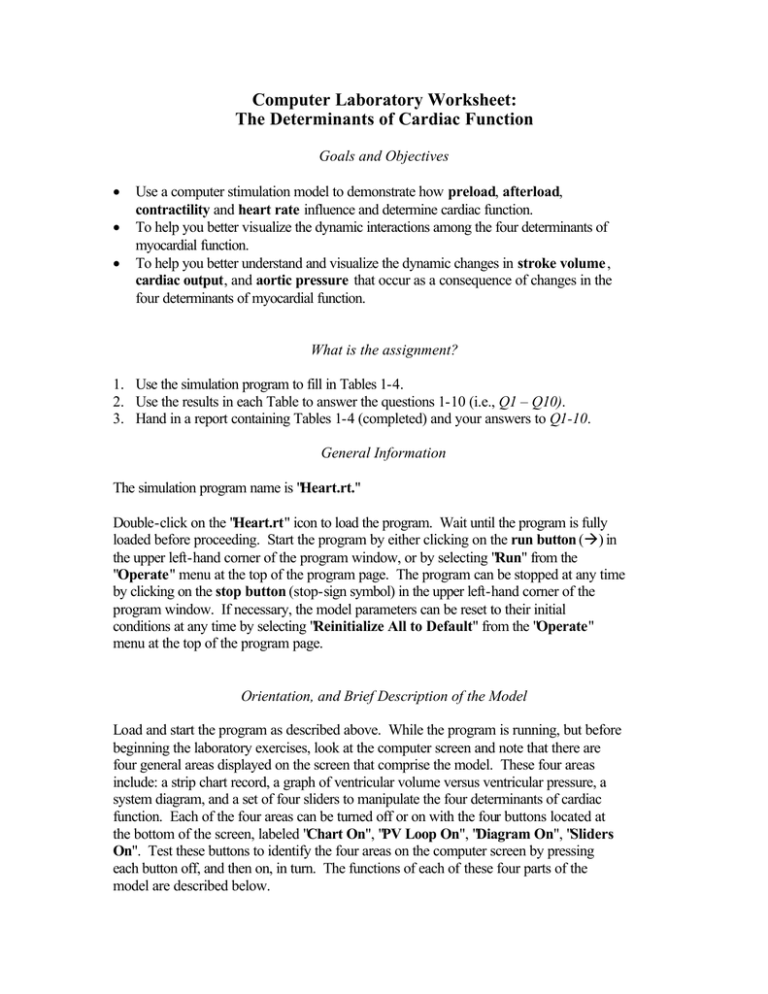
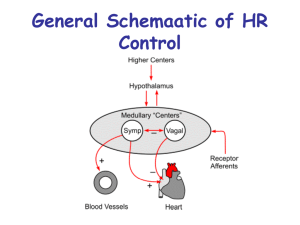
Computer Laboratory Worksheet: The Determinants of Cardiac Function Goals and Objectives • • • Use a computer stimulation model to demonstrate how preload, afterload, contractility and heart rate influence and determine cardiac function. To help you better visualize the dynamic interactions among the four determinants of myocardial function. To help you better understand and visualize the dynamic changes in stroke volume , cardiac output, and aortic pressure that occur as a consequence of changes in the four determinants of myocardial function. What is the assignment? 1. Use the simulation program to fill in Tables 1-4. 2. Use the results in each Table to answer the questions 1-10 (i.e., Q1 – Q10). 3. Hand in a report containing Tables 1-4 (completed) and your answers to Q1-10. General Information The simulation program name is "Heart.rt." Double-click on the "Heart.rt" icon to load the program. Wait until the program is fully loaded before proceeding. Start the program by either clicking on the run button (à) in the upper left-hand corner of the program window, or by selecting "Run" from the "Operate" menu at the top of the program page. The program can be stopped at any time by clicking on the stop button (stop-sign symbol) in the upper left-hand corner of the program window. If necessary, the model parameters can be reset to their initial conditions at any time by selecting "Reinitialize All to Default" from the "Operate" menu at the top of the program page. Orientation, and Brief Description of the Model Load and start the program as described above. While the program is running, but before beginning the laboratory exercises, look at the computer screen and note that there are four general areas displayed on the screen that comprise the model. These four areas include: a strip chart record, a graph of ventricular volume versus ventricular pressure, a system diagram, and a set of four sliders to manipulate the four determinants of cardiac function. Each of the four areas can be turned off or on with the four buttons located at the bottom of the screen, labeled "Chart On", "PV Loop On", "Diagram On", "Sliders On". Test these buttons to identify the four areas on the computer screen by pressing each button off, and then on, in turn. The functions of each of these four parts of the model are described below. Strip chart record (top left quadrant in computer screen) A simulated strip chart recorder is displayed in the top left quadrant of the computer screen and shows time-based records of three basic parameters of a Wiggers' Diagram for the left ventricle. Looking from the top chart down, these include displays of aortic pressure (mmHg) in red, left ventricular pressure (mmHg) in black, and left ventricular volume (ml) in black. Watch the strip chart and consider the following questions. • What is a normal value for Systolic Pressure in the Aorta of a human? • What is a normal value for Diastolic Pressure in the Aorta of a human? • How would you calculate a Mean Arterial Pressure from the Chart Record? What's your answer? • Do you think the Mean Arterial Pressure that you just calculated would be about the same for a Giraffe? Why? Pressure-volume graph (top right quadrant in computer screen) The instantaneous values for left ventricular pressure are plotted as a function of the corresponding values for left ventricular volume and the data are displayed in the top right quadrant of the computer screen. This graph is what physiologists and cardiologists call The Pressure -Volume Loop. At the bottom right corner of the computer screen is a button labeled: "Clear Graph." This button is used to clear the graph when it becomes "cluttered" with accumulated tracings. Test its function by pressing and quickly releasing it. Watch the Pressure-Volume Loop and consider the following questions. • Find the different phases of the cardiac cycle on the Pressure-Volume Loop. What are they called? • Locate the positions on the Pressure-Volume Loop where the aortic valve and mitral valve open and close. What heart sounds are associated with these locations? • Estimate the normal (control) stroke volume from the Pressure-Volume Loop. System diagram of cardiac function (bottom right quadrant of computer screen) A system diagram, which shows the relationships among the different parameters that contribute to the pumping function of the heart, is located in the bottom right quadrant of the computer screen. A continuous display of the numeric values is shown in the small window for each parameter. The parameters associated with the heart are shown in black letters and include: • • • • End-Diastolic Volume (EDV) is the maximum volume of blood that the ventricles hold during a cardiac cycle, and End-Systolic Volume (ESV) is the volume of blood left in the ventricles after a contraction. Stroke Volume (SV) is the difference between EDV and ESV. Cardiac Output (CO) is the product of Heart Rate (HR) and Stroke Volume (SV). Contractility (CONT) is the intrinsic ability of a cardiac muscle fiber to contract at any given fiber length. Contractility determines the rate and magnitude of force generated by the entire heart, and therefore, the magnitude of ESV. The body regulates the contractility of the heart by releasing catecholamines (e.g., norepineprhin) into the bloodstream, which bind to cardiac cells and increase the concentrations of intracelluar calcium. Elevated intracellular calcium levels cause cardiac cells to contract more forcefully. Why? The parameters associated with the peripheral vasculature, external to the heart, are shown in red letters. They include Total Peripheral Resistance (TPR) and Mean Arterial Pressure (Pã). Recall that Pã is proportional to the product of Total Peripheral Resistance and Cardiac Output. Two additional buttons labeled "Act Tension" and "Pause" are also included in the lower right quadrant. They provide the following display enhancements: • Pressing the "Act Tension" button will display a red line on the Pressure-Volume Graph. Do not worry about this feature. • Pressing the "Pause" button causes the strip chart recorder to pause and inserts a new display with a sliding vertical line (blue line) that can be used to identify the elements on the strip chart record (Wiggers' Diagram) that correspond to those same elements in the Pressure -Volume Loop. It is useful for locating the boundaries between the different phases of the cardiac cycle. Press the button to see what happens. To make this feature work properly; first, press the "Clear Graph" button to clear the graph, and the internal buffer. Wait a minimum of 5 cycles while the internal buffer accumulates sufficient data. Next, press the "Pause" button. Finally, manipulate the blue line back-and-forth, or click on the right and left arrowheads to see what happens. This tool is particularly useful if you have trouble visualizing the relationship between left ventricular pressure and volume when displayed as a Wigger's Diagram and as a Pressure -Volume Loop. Controls for manipulating the determinants of cardiac function (bottom left quadrant of computer screen) "Slider" controls for manipulating the four determinants of cardiac function are located in the bottom left quadrant of the computer screen. These are used to manipulate Preload, Total Peripheral Resistance (TPR), Contractility and Heart Rate. In the starting, initial condition, note that three of the variables are grayed out, and only the Preload Slider is operative. • • Preload is the degree of myocardial stretch created by venous return. Total peripheral resistance is the resistance to blood flow through the circulatory system created primarily by the arterioles. The model is designed to operate in one of two different modes: (1) The Isolated Heart (single variable active) mode; and (2) The Intact Heart (all variables active) mode. You will only use the intact heart mode in this exercise. This latter mode illustrates how the pumping function of the heart will behave when one, or more, of the variables is changed, and the other parameters in the system are allowed to reach a new equilibrium. To enable “The Intact Heart” mode, click on the radio button above the Preload Slider to turn it off. All of the grayed out sliders and traces should now be displayed clearly. The label above the sliders should change so it now reads: "Intact Heart (all variables active)." A "feedback" arrow (labeled “afterload”) and a window showing the diastolic pressure in the aorta appear in the system diagram (lower right quadrant). The afterload is the pressure remaining in the left ventricle after it has contracted—it tends to be high in people with high TPR or hypertension. Laboratory Exercise Start the laboratory exercise by first reinitializing everything to the default condition. Then, click the "Clear Graph" button. Effect of varying preload The purpose of this part of the exercise is to observe how changes in preload during the filling phase of the cardiac cycle influence the pumping function of the heart. Make sure the program is in Intact Heart Mode. While performing this part of the exercise, consider the following questions. • • • What is the effect of an increase in preload on the pumping functions of the heart and the mean arterial pressure? Starling’s Law of the Heart states that the tension (or contractile force) generated by cardiac muscle fibers increases as the fibers are stretched (up to an optimum length; see pp. 436-37 in your textbook). What is the physiological significance of this Law to what you observe in the simulation program? What are the underlying molecular mechanisms that account for the length-tension relationship for cardiac muscle? Procedure: To better understand the sequence of events associated with an increase in preload in the intact heart, perform the following procedures. Adjust the Preload Slider back to the control condition (5.0 mmHg) so that the End Diastolic Volume returns to 120 ml. Make certain that the Preload radio button is set so the system is in the Intact Heart Mode . Clear the PV-Loop graph. Let the model run for several cycles, then look at the system diagram and write down the Control Values for the different parameters in Table 1 below. Next, quickly increase the preload to 7.0 mmHg so that the End Diastolic Volume (EDV) increases to 134 ml. Remember that for best results, preload should be increased at the very end of the filling phase or at the beginning of the isovolumetric contraction phase in the cardiac cycle. Watch the changes develop in the PV-Loop and also observe the changes in the system diagram. When a new equilibrium is achieved, record the new values for the different parameters in Table 1 below. If you have trouble seeing the changes, or if you are confused, then simply clear the graph and repeat the procedures until you get a better picture of the sequence of events. Table 1 (Effect of varying preload) Control Preload (5.0) Preload Increased to 7.0 EDV_______________ml ESV_______________ml SV________________ml/beat Heart Rate____72____beats/min CO________________liters/min TPR_________20____arbitrary units Contractility__1.0____arbitrary units Pã_________________mmHg Pdiastolic___________mmHg EDV_______________ml ESV_______________ml SV________________ml/beat Heart Rate____72____beats/min CO________________liters/min TPR_________20____arbitrary units Contractility__1.0____arbitrary units Pã_________________mmHg Pdiastolic___________mmHg Q1. What happened to the End Systolic Volume (ESV) after you increased the preload? Why? Q2. Use the data in Table 1 to calculate values for Systolic Pressure in the Aorta for the control case and following the increase in preload. Q3. How does this change in Pã relate to Starling’s Law of the Heart? Q4. Why is the amount of preload important for normal function? What are the physiological consequences of increasing preload? Effect of varying TPR (Afterload): The purpose of this part of the exercise is to observe how changes in afterload affect the pumping function of the heart. The afterload is manipulated in the model by changing the total peripherial resistance (TPR). Make sure the program is in Intact Heart Mode. Procedure: Click on the radio button over the TPR Slider to set the system to the Intact Heart mode. Make certain that all the sliders are set to the control conditions (red dots). Watch the chart record and the PV-Loop for several cycles and record the control data in the appropriate box in Table 2, below. Calculate the Ejection Fraction for the control condition. The ejection fraction is the percent of the EDV that is ejected with each stroke. It is defined quantitatively as: Ejection fraction = (EDV – ESV) / (EDV) Now, to see the effect of an increase in TPR-afterload when the preload is held constant (Manual Preload On), perform the following manipulations. Make certain the "Act Tension" button is on. Press the "Clear Graph" button to clear the PV-Loop and the internal buffer. Let the model cycle for two or three cycles then suddenly increase TPR to 35 by clicking in the TPR Slider Scale (white column) at the 35 position. Watch what happens. For best results, incre ase TPR at the beginning of the filling phase in the cardiac cycle. Try this procedure several times, if you wish, to get a clear record. Record the new equilibrium data [TPR Increased to 35 (Manual Preload On)] in Table 2 and calculate the new value for the Ejection Fraction. Table 2 (TPR-afterload) Control TPR TPR Increased to 35 (Manual Preload ON) TPR Increased to 35 (Auto Preload ON) EDV______________ml ESV______________ml SV_______________ml/beat Heart Rate___72__beats/min CO_____________liters/min TPR____20___arbitrary units Contractility__1.0_arb. units Pã________________mmHg Pdiastolic__________mmHg Ejection Fraction________% EDV______________ml ESV______________ml SV_______________ml/beat Heart Rate___72__beats/min CO_____________liters/min TPR_________arbitrary units Contractility__1.0_arb. units Pã________________mmHg Pdiastolic__________mmHg Ejection Fraction________% EDV______________ml ESV______________ml SV_______________ml/beat Heart Rate___72__beats/min CO_____________liters/min TPR_________arbitrary units Contractility__1.0_arb. units Pã________________mmHg Pdiastolic__________mmHg Ejection Fraction________% Q5. What changed? What are the physiological consequences of changing TPR? Effect of changing contractility The purpose of this part of the exercise is to observe how changes in contractility affect the pumping function of the heart. Make sure the program is in Intact Heart Mode. Procedure: Make certain that all the sliders are set to the control conditions (red dots). Look at the system diagram and write down the Control Values for the different parameters in Table 3 below. Now, clear the graph and let the PV-Loop run for several cycles. Next, quickly increase the contractility to 1.3 and watch what happens. This is easily done by triple-clicking on the up-arrow above the contractility slider. Remember that for best results, increase the contractility at the end of the isovolumetric relaxation phase and the beginning of the filling phase in the cardiac cycle. Watch the changes develop in the PV-Loop and also observe the changes in the system diagram. When a new equilibrium is achieved, record the new values for the different parameters in Table 3 below. If you have trouble seeing the changes, or if you are confused, then simply clear the graph and repeat the procedures until you get a better picture of the sequence of events. Table 3 (Effect of changing contractility) Control Contractility Contractility Increased to 1.3 (Manual Preload ON) EDV________120____ml ESV_______________ml SV________________ml/beat Heart Rate____72____beats/min CO________________liters/min TPR_________20____arbitrary units Contractility_________arbitrary units Pã_________________mmHg Pdiastolic___________mmHg EDV________120____ml ESV_______________ml SV________________ml/beat Heart Rate____72____beats/min CO________________liters/min TPR_________20____arbitrary units Contractility_________arbitrary units Pã_________________mmHg Pdiastolic___________mmHg Q6. Use the data in Table 3 to calculate the Ejection Fraction when Contractility was set at the control level and when it was elevated to 1.3. Q7. What insights do these results offer into the physiological significance of changing the contractility of the Heart? Effect of varying Heart Rate The purpose of this part of the exercise is to observe how changes in heart rate affect the pumping function of the heart Click on the radio button over the Heart Rate Slider to set the system to the closed loop mode. Make certain that ALL the sliders are set to the control conditions (red dots) and that the "Act Tension" button is pressed. Slowly move the Heart Rate Slider up and down, watch the strip chart recording and the PV-Loop, and see what happens. Depending upon the speed of your computer, you may find it necessary to periodically clear the PV-Loop by briefly holding down the "Clear Graph" button to obtain a more realistic simulation at the higher heart rates. When you have familiarized yourself with the manipulations, then continue with the next procedure to generate a more quantitative picture of the effect of heart rate on the pumping function of the heart. Procedure: Reduce the heart rate to 42 beats / minute by pulling the Heart Rate Slider down to the appropriate level. You may find it easier to click on the "Down Arrow" at the bottom of the Heart Rate Slider. Wait until a steady state is achieved. Again, if the system seems to run too slow, then briefly hold down the "Clear Graph" button. Now, record the values for EDV, ESV and SV in the appropriate columns in Table 4. Next, increase the heart rate in 6 beat / minute steps by clicking once for each step on the "Up Arrow" above the Heart Rate Slider. Watch the PV-Loop and the system diagram at each new heart rate, until steady-state is achieved, then record the new values for EDV, ESV, and SV in Table 4. When you have recorded the data for the range of heart rates, 42 to 180 beats / minute, plot the results in the accompanying graph. Use the results to answer the questions below Table 4. Table 4 (Effect of varying heart rate) Control Contractility Level = 1 Heart Rate (beats/min) 42 48 54 60 66 72 78 84 90 96 102 108 114 120 126 132 138 144 150 156 162 168 174 180 EDV (ml) ESV (ml) SV (ml) 120 55 65 Q8. How does heart rate affect end diastolic volume (EDV) and the filling of the heart? Q9. How does heart rate affect end systolic volume (ESV)? Q10. Stroke Volume decreases almost linearly as Heart Rate increases over a wide range (see your graph in Table 4). Why?