EBP Paper - Amanda farr
advertisement

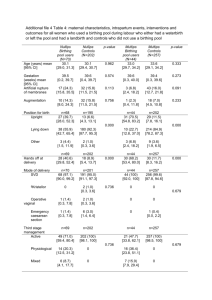
Running head: NON-SUPINE BIRTHING POSITIONS Maternal Non-Supine Birthing Positions Logan Dean, Amy Ellison, Amanda Farr, Meagan Holt, Kate Onion, Abby Rose Auburn University School of Nursing 1 NON-SUPINE BIRTHING POSITIONS 2 Maternal Non-Supine Birthing Positions Pico Question and Significance A PICO question is an integral piece to evidence based practice research. Formation of this clearly defined clinical question leads to organization of related findings in health literature. The clear direction for the evidence based practice project leads to a focused search for research. In this specific investigation, the question of “in women in labor, do non-supine birthing positions result in improved progression of labor and delivery outcomes as compared to supine positions” is addressed as the PICO question. The PICO format is composed of the four components: population, intervention, comparison and outcome. The patient population of interest is women in labor who have a vaginal delivery. The population is comprised of women who gave birth in hospitals, as well as in non-traditional birthing centers. Multiple birthing positions were implemented in both settings. Different types of health care professionals, including physicians and midwives, carried out the birthing process. The intervention of non-supine birthing positions was investigated to test the clinical question. Women in labor assumed various non-traditional positions such as lateral, squatting, or sitting on a birthing seat. In contrast to these non-traditional positions, a traditional position, like lithotomy, is defined as the comparison of interest. The outcome measured is the progression of labor and delivery outcomes. These outcomes include the length of labor, comfort of the mother, degree and incidence of perineal trauma, and prevalence of surgically assisted vaginal deliveries. Different birthing positions led to varying outcomes. The PICO clinical question is significant in the improvement of nursing practice. Nurses in labor and delivery settings will interact with women of childbearing age who have a vaginal delivery. Interactions with this population begin upon admission to the labor and delivery unit NON-SUPINE BIRTHING POSITIONS 3 and continue until discharge instructions post-delivery. Findings stemming from the PICO question will further enhance nursing practice through the latest evidence regarding birthing positions during vaginal labor and delivery. The evidence enhances the ability of nurses to communicate and advocate for the mothers’ wishes regarding birthing positioning. Health care professionals are responsible for carrying out health interventions. In this literature review, health care professionals, including nurses, certified nurse midwives, and physicians, assist mothers into non-supine birthing positions. In particular, nurses may be a mother’s only support system during the labor and delivery process. It is a nurse’s responsibility to assist the mother in assuming different positions throughout delivery. It is integral for nurses to make mothers’ wishes and desires relating to the personal birthing plan a reality. In contrast to the previous knowledge of the traditional supine birthing position, knowledge of nontraditional positions can further improve nursing practice as healthcare professionals care for laboring women. Improved outcomes related to non-supine birthing positions result in better health for the mother. Enhanced maternal health after a vaginal delivery encompasses decreased perineal trauma, increased comfort level, and an overall well being of the mother. Better outcomes may lead to improved patient-nurse relationships, as well as giving the nurse a sense of accomplishment. Traumatic outcomes, such as lacerations and episiotomies, can lead to infection and other postpartum complications. Although it is impossible for nurses to decrease the incidence of perineal lacerations, nurses do have a role in decreasing the risk for lacerations. Research pertaining to non-supine birthing positions provides nurses with the knowledge needed to assist women in planning and executing a birthing plan and improving delivery outcomes. NON-SUPINE BIRTHING POSITIONS The purpose of this paper is to explore the effects of non-supine birthing positions on labor and delivery outcomes and bring about awareness of non-traditional birthing positions. Search Strategies As the group gathered research regarding non-supine birthing positions, the following Auburn University online library databases were included in the searching process: PubMed Clinical Queries, CINAHL, PsychINFO, and Cochrane Library. In narrowing the research process, publications selected fell within the range of the last ten years (2004-2014), were evidence-based and peer-reviewed, and only available in the English language. Specific key words included in the research were, “non-supine,” “birthing positions,” “lateral,” “vaginal delivery,” “non-traditional,” “birth or birthing,” “positions,” “labor,” “maternal,” and “NOT supine.” When limiting the research process, articles that were selected consisted of systematic research, meta-analysis, and primary research. Two of the four articles referenced in the PICO Assignment above are comprised as systematic research review articles from the review database, Cochrane Library. After visiting the National Guideline Clearinghouse (AHRQ) database, there were not any clinical practice guidelines available for the group’s topic, “nonsupine birthing positions.” Synthesis of Findings Literature regarding non-supine birthing positions was reviewed to compare the differences in delivery outcomes among women using various birthing positions. Multiple studies evaluated the traditional supine position in comparison to non-supine positions such as squatting, lateral lying, and use of a birthing stool. Differences in positioning were documented in the first and second stages of labor, each providing positive and negative effects on the laboring process. Different settings for the labor and delivery process were evaluated to 4 NON-SUPINE BIRTHING POSITIONS 5 determine the prevalence of using non-supine birthing positions in both the traditional hospital setting and birthing care centers. A systematic review performed by Lawrence, Lewis, Hofmeyr, and Styles (2013) evaluated ambulation and non-supine positions during the first stage of labor. As a result of upright positions and ambulation, the length of the first stage of labor is shortened and the women are less likely to have an epidural or a Cesarean section. It was also found that these interventions do not have any negative effects on the mother or baby (Lawrence et al., 2013). Findings from Miquelutti, Cecatti, and Makuch (2013) support that the majority of women consider standing up, walking around, and sitting on an exercise ball as the most comfortable positions during the first stage of labor. These women consider horizontal positions less comfortable as these positions hamper the mothers’ mobility and increase the sensation of pain during contractions. Women who attended a Birthing Preparation Program were more likely to feel at ease when assuming these upright positions (Miquelutti et al., 2013). The second stage of labor begins once the mother reaches full cervical dilation and effacement, and signifies that the patient can begin actively pushing (Lowdermilk, Perry, Cashion, & Alden, 2012). Traditionally, health care providers encourage the mother to assume the supine lithotomy position, with feet in stirrups during the second stage of labor (Gupta, Hofmeyr, & Shehmer, 2012). To determine the effects of traditional positioning, researchers studied womens’ labor and delivery experiences and outcomes while clients assume the supine position. Women delivering in the supine lithotomy position show significantly more first and second degree lacerations compared to those delivering in the lateral position (Meyvis et al., 2011). The incidence of episiotomies, as well as lacerations requiring sutures, increases when the mother is in a supine position. There is no conclusive evidence about an increase or decrease NON-SUPINE BIRTHING POSITIONS in estimated blood loss during the postpartum period for a mother giving birth in a supine position (de Jonge, Teunissen, & Lagro-Janssen, 2004). Fewer episiotomies and a decrease in perineal trauma are noted with the lateral birthing position. Delivery in the lateral position, also known as Sims position, is a “hands-off” technique, avoiding unnecessary manipulations while the mother is on her side (Meyvis et al., 2011). Used in conjunction with the lateral birthing position, warm compresses and manual support techniques are shown to decrease perineal trauma (Hastings-Tolsma, Vincent, Emeis, & Francisco, 2007). The use of the upright or lateral position decreases duration of the second stage of labor, as well as decreasing pain, incidence of assisted delivery with forceps, abnormal fetal heart rate patterns, and episiotomies (de Jonge et al., 2004). The birthing stool promotes an upright position that provides comfort for the mother and allows gravity to assist during the delivery. The birth seat does not reduce the number of instrumental vaginal births. Delivering on the birth seat shows no adverse consequences on perineal outcomes and may even protect against episiotomies (Thies-Lagergren, Kvist, Christensson, & Hildingsson, 2011). On a pain scale of 1 to 10, women using the birthing stool ranked pain at a 6.9 whereas women in supine position ranked pain at a 7.6 (De Jonge et al., 2004). De Jonge et al. (2004) found that the lowest rate of postpartum hemorrhage occurred when the mother is in a squatting position with no oxytocin or epidural. However, a study by Hastings-Tolsma et al. (2007) determined an increase in perineal lacerations in primipara mothers who assumed the squatting position. Birthing centers provide increased opportunity for women to assume non-traditional birthing positions as compared to a hospital. Midwives in the birthing centers encourage the 6 NON-SUPINE BIRTHING POSITIONS 7 women to assume the positions that provide the most comfort. Physicians encourage the lithotomy position due to convenience for health care providers, as well as lack of knowledge regarding other non-traditional positions (Waldenstrom & Nisson, 1997). Midwives strive to explore the women’s knowledge of different birthing positions and the patient’s desires during the birthing process. Midwives also help the women assume the desired position and provide personal support (de Jonge, Teunissen, van Diem, Scheepers, & Largo-Janssen, 2008). It is evidenced that there is no discrepancy in quality of care between birthing centers and hospitals (Waldenstrom & Nilsson, 1997). This review of literature determines that the use of alternate positions in both the first and second stages of labor lead to increased progression of labor, as wells as improved delivery outcomes. The use of the supine position is not necessarily the best intervention during labor and delivery for every patient. Better outcomes are found when the mother assumes a lateral or squatting position or uses a birthing stool, especially when these interventions take place in a birthing center with midwives. These outcomes include fewer lacerations and episiotomies, decreased pain, decreased duration of labor, and fewer instrument-assisted births. Appraisal of Evidence The levels of evidence vary among all of the supporting articles. Half are level II, giving those articles much credibility and strength of evidence. The other three articles have lower levels of evidence, ranging from level IV to level VI. The quality of evidence for these articles is slightly lower than that of the level II articles and displays a less thorough design. Of the articles gathered, all of them support the recommendation of utilizing non-supine birthing positions. It is consistently found that the benefits of non-supine positioning greatly outweigh the risks. These articles display the many benefits to applying non-supine positioning in current evidence-based NON-SUPINE BIRTHING POSITIONS 8 practice. The use of non-supine birthing positions during labor is associated with a decrease in perineal damage, including episiotomies and vaginal lacerations, as well as an increase in maternal comfort and control. Findings implied that when given an option to assume alternate positions, new mothers felt more confident while laboring. However, as with any medical recommendation, there are risks involved. It was noted in one of the articles that utilizing a nonsupine birthing position could increase estimated blood loss up to 1000mL. It was also mentioned in a different study that with certain non-supine positions (i.e. squatting), a greater risk of perineal laceration is present in comparison with other non-supine positions. After researching various databases, no recent cost studies were found on the recommended intervention. However, it could be easily inferred that changing birthing positions would not cause a dramatic increase in costs to hospitals or patients. Recommendations Laboring mothers should give birth in the lateral position to decrease the risk for perineal trauma. o Grade: B o Meyvis, I., van Rompaey, B., Goormans, K., Truijen, S., Lambers, S., Mestdagh, E., & Wilhelm, M. (2012). Maternal positions and other variables: Effects on perineal outcomes in 557 births. Birth, 39(2), 115-120. doi:10.1111/j.1523536X.2012.00529.x o Hastings-Tolsma, M., Vincent, D., Emeis, C., & Francisco, T. (2007). Getting through birth in one piece: Protecting the perineum. The American Journal of Maternal/Child Nursing, 32(3), 158-164. doi:10.1097/01.NMC.0000269565.20111.92 NON-SUPINE BIRTHING POSITIONS 9 Nurses should encourage the use of birthing stools to promote comfort among laboring women. o Grade: C o de Jonge, A., Teunissen, T. A., & Lagro-Janssen, A. L. (2004). Supine positions compared to other positions during the second stage of labor: A meta-analytic review. Journal of Psychomatic Obstetrics & Gynecology, 24, 35-45. doi: 10.1080/01674820410001737423 Expectant mothers should participate in a preparation course to increase knowledge on birthing positions, promoting comfort in labor. o Grade: C o Miquelutti, M. A., Cecatti, J. G., & Makuch, M. Y. (2013). Antenatal education and the birthing experience of Brazilian women: A qualitative study. BioMed Central Pregnancy and Childbirth, 13(171), 1-9. doi: 10.1186/1471-2393-13-171 Ambulation and non-supine positioning should be implemented during the first stage of labor. o Grade: A o Miquelutti, M. A., Cecatti, J. G., & Makuch, M. Y. (2013). Antenatal education and the birthing experience of Brazilian women: A qualitative study. BioMed Central Pregnancy and Childbirth, 13(171) 1-9. doi: 10.1186/1471-2393-13-171 o Lawrence, A., Lewis, L., Hofmeyr, G. J., & Styles, C. (2013). Maternal positions and mobility during first stage of labour (Review). Cochrane Database of Systematic Review, 10, Art no. CD003934. doi:10.1002/14651858.CD003934.pub3 NON-SUPINE BIRTHING POSITIONS 10 To women wishing to explore alternative birthing positions, a midwife should be utilized. o Grade: C o de Jonge, A., Teunissen, D. A., van Diem, M. T., Scheepers, P. L., & LagroJanssen, A. L. (2008). Women’s positions during the second stage of labour: Views of primary care midwives. Journal of Advanced Nursing, 63(4), 347-356. doi: 10.1111/j.1365-2648.2008.04703.x To women wishing to explore alternative birthing positions, a birthing center should be considered. o Grade: C o Waldenstrom, L. & Nilsson, C. (1997). A randomized controlled study of birth center care versus standard maternity care: Effects on women’s health. Birth, 24(1), 17-26. Retrieved from http://onlinelibrary.wiley.com/journal/10.1111/(ISSN)1523-536X Non-supine birthing positions should be assumed during the second stage of labor to decrease the risk for episiotomies. o Grade: A o Meyvis, I., van Rompaey, B., Goormans, K., Truijen, S., Lambers, S., Mestdagh, E., & Wilhelm, M. (2012). Maternal positions and other variables: Effects on perineal outcomes in 557 births. Birth, 39(2), 115-120. doi:10.1111/j.1523536X.2012.00529.x o Thies-Lagergren, L., Kvist, L. J., Christensson, K., & Hildingsson, I. (2011). No reduction in instrumental vaginal births and no increased risk for adverse perineal NON-SUPINE BIRTHING POSITIONS 11 outcome in nulliparous women giving birth on a birth seat: Results of a Swedish randomized controlled trial. BioMed Central Pregnancy and Childbirth, 11(1), 22-30. doi:10.1186/1471-2393-11-22 o de Jonge, A., Teunissen, T. A., & Lagro-Janssen, A. L. (2004). Supine positions compared to other positions during the second stage of labor: A meta-analytic review. J Psychosom Obstet Gynecol, 24, 35-45. doi: 10.1080/01674820410001737423 o Gupta, J. K., Hofmeyr, G. J., & Shehmer, M. (2012). Position in the second stage of labour for women without epidural anesthesia. Cochrane Database of Systematic Review, 5, Art no. CD002006. doi:10.1002/14651858.CD002006.pub.3 The supine position should not be used to decrease the incidence of instrumental births. o Grade: A o de Jonge, A., Teunissen, T. A., & Lagro-Janssen, A. L. (2004). Supine positions compared to other positions during the second stage of labor: A meta-analytic review. Journal of Psychosomatic Obstetrics and Gynecology, 24, 35-45. doi: 10.1080/01674820410001737423 o Gupta, J. K., Hofmeyr, G. J., & Shehmer, M. (2012). Position in the second stage of labour for women without epidural anesthesia. Cochrane Database of Systematic Review, 5, Art no. CD002006. doi:10.1002/14651858.CD002006.pub.3 NON-SUPINE BIRTHING POSITIONS 12 References de Jonge, A., Teunissen, D. A., van Diem, M. T., Scheepers, P. L., & Lagro-Janssen, A. L. (2008). Women’s positions during the second stage of labour: Views of primary care midwives. Journal of Advanced Nursing, 63(4), 347-356. doi: 10.1111/j.13652648.2008.04703.x de Jonge, A., Teunissen, T. A., & Lagro-Janssen, A. L. (2004). Supine positions compared to other positions during the second stage of labor: A meta-analytic review. Journal of Psychosomatic Obstetrics & Gynecology, 24, 35-45. doi:10.1080/01674820410001737423 Gupta, J. K., Hofmeyr, G. J., & Shehmer, M. (2012). Position in the second stage of labour for women without epidural anesthesia. Cochrane Database of Systematic Review, 5, Art no. CD002006. doi:10.1002/14651858.CD002006.pub.3 Hastings-Tolsma, M., Vincent, D., Emeis, C., & Francisco, T. (2007). Getting through birth in one piece: Protecting the perineum. The American Journal of Maternal/Child Nursing, 32(3), 158-164. doi:10.1097/01.NMC.0000269565.20111.92 Lawrence, A., Lewis, L., Hofmeyr, G. J., & Styles, C. (2013). Maternal positions and mobility during first stage of labour (Review). Cochrane Database of Systematic Review, 10, Art no. CD003934. doi:10.1002/14651858.CD003934.pub3 Lowdermilk, D. L., Perry, S. E., Cashion, K., & Alden, K. R. (2012). Nursing care of the family during labor and birth. In K. Piotrowski (Ed.), Maternity and women’s health care (p. 457). St. Louis, MO: Elsevier Mosby NON-SUPINE BIRTHING POSITIONS 13 Meyvis, I., van Rompaey, B., Goormans, K., Truijen, S., Lambers, S., Mestdagh, E., & Wilhelm, M. (2012). Maternal positions and other variables: Effects on perineal outcomes in 557 births. Birth, 39(2), 115-120. doi:10.1111/j.1523-536X.2012.00529.x Miquelutti, M. A., Cecatti, J. G., & Makuch, M. Y. (2013). Antenatal education and the birthing experience of Brazilian women: A qualitative study. BioMed Central Pregnancy and Childbirth, 13(171), 1-9. doi: 10.1186/1471-2393-13-171 Thies-Lagergren, L., Kvist, L. J., Christensson, K., & Hildingsson, I. (2011). No reduction in instrumental vaginal births and no increased risk for adverse perineal outcome in nulliparous women giving birth on a birth seat: Results of a Swedish randomized controlled trial. BioMed Central Pregnancy and Childbirth, 11(1), 22-30. doi:10.1186/1471-2393-11-22 Waldenstrom, L. & Nilsson, C. (1997). A randomized controlled study of birth center care versus standard maternity care: Effects on women’s health. Birth, 24(1), 17-26. Retrieved from http://onlinelibrary.wiley.com/journal/10.1111/(ISSN)1523-536X Running head: NON-SUPINE BIRTHING POSITIONS 14 Appendix Evidence Grid: Authors of Article, YR Level of Evidence of article (I – VI) Purpose of study/review and research questions (person who completed this row on grid) Meyvis, I., Rompaey, B., Goormans, K., Truijen, S., Lambers, S., Mestdagh, E., Mistiaen, W. (2012) LOE: IV (Logan Dean) The purpose of this study is to compare the lateral position with the lithotomy position in delivery, with a focus on perineal damage. Research elements: A) Design B)Population C) Sampling method/size D) description of methods/ interventions (if any) E) instruments used F) outcomes measured (not the findings – just what variables were measured as outcomes) A) Correlational B) All women with gestations between 37-42 weeks who were delivering vaginally in a regional hospital in Antwerp, Belgium in a 1 year span C) 557 D) None – retrospective study E) Hospital records F) Perineal damage, lacerations, episiotomies Major findings relevant to project Give strengths and weaknesses of this article for your project related to validity, bias and applicability Women delivering in Strengths: lithotomy position showed 1. Large sample size significantly more lacerations 2. Valid source for me of the first and second degrees to consider in when compared with those planning for my delivering in the lateral project position. 3. All women in the study were around In the lateral position, the same gestational episiotomy was performed age, lending itself to significantly less frequently: consistency this procedure was applied in 4. It gave a lot of 38.2% of the women statistics as to the delivering in lithotomy demographic data of position and in less than 7% the women. of the women delivering in lateral position. Weaknesses: 1. It is noted that NON-SUPINE BIRTHING POSITIONS 15 Including both laceration and episiotomy in the analysis, an intact perineum was significantly more likely in women delivering in the lateral position. In contrast to the lithotomy position, delivery in the lateral position is a “handsoff” technique, avoiding unnecessary manipulations which could explain the low number of episiotomies. Hastings-Tolsma, M., Vincent, D., Emeis, C. & Francisco, T. (2007). LOE: IV (Amy Ellison) The purpose of this study is to determine what interventions can be used in the hospital setting to decrease trauma to the perineum through lacerations or episiotomies A) Retrospective record review/descriptive analysis B) Women having a vaginal birth C) 510 healthy term women whose prenatal and intrapartal information had been entered into the The squatting position in primiparas increases the risk for perineal laceration. The lateral position, upright and hands and knees, decreases the risk for perineal laceration. Birth in a slide-lying position decreases the risk for perineal women in the lateral position were older and less likely to have epidural anesthesia than those who delivered in the lithotomy position, so this could cause a discrepancy. 2. Might not be 100% applicable to the general population because only a specific population from Belgium was looked at. 3. Not everyone was cared for by the same type of birthing caretaker (i.e. midwife, physician) Weaknesses: There is no randomization of individuals, no way to determine the accuracy of the data (besides comparing the electronic charting with paper records), and no way to assess the quality of care given by the nurse midwife. This study was also limited to only healthy term NON-SUPINE BIRTHING POSITIONS 16 Nurse Midwifery Clinical Data Set in 1996-1997 D) There were no methods or interventions in place as this was a retrospective study. However, methods and interventions were recommended in the Clinical Implications portion to provide better nursing care E) No instrumentation was used, as this was a retrospective study. However, hospital records were looked at to gather data. F) 1. Overall spontaneous laceration rate was 49.2%, spontaneous vaginal birth caused some type of laceration in 55.7% of women, but only 36.6% required suturing. A severe laceration was also more likely with a tears for all women, as well as mothers. Little is known protects the perineum. about the impact different interventions have on preterm babies and their mothers. Therefore, it could be difficult to apply to all births. The only major bias that could occur was how the subjects were selected. There was no randomization, which can lead to bias. Strengths: This study had 510 women participate which is significant. It also gave many useful statistics that were determined to be significant (p<.05). NON-SUPINE BIRTHING POSITIONS 17 prolonged second stage of labor, nulliparous women, or if the woman was 30 years or older and insured. 2. Marital status and a baby of 9lbs or more in nulliparous women had an increased risk of an episiotomy. In all women, fetal bradycardia and prolonged second stage of labor increased the risk for episiotomy. 3. Lacerations were more likely to occur in the lithotomy position or prolonged second stage of labor. “Nulliparous women who used lateral positioning, warm compresses, and manual support techniques were less likely to experience a tear” (162). Using NON-SUPINE BIRTHING POSITIONS Thies-Lagergren, L., Kvist, L., Christensson, K., Hildingsson, I. (2011) LOE: II (Kate Onion) The aim of this study was to test through a randomized controlled trial, if using a birthing seat during the second stage of labor, for healthy nulliparous women, decreases the number of instrumentally assisted births and thus may decrease perineal trauma and blood loss. 18 A) B) C) D) perineal care measures lowered the risk of episiotomy. Experimental Women who have a vaginal delivery 1002 women who have a vaginal delivery in Sweden between November 2006 and July 2009; inclusion criteria: normal pregnancy, cephalic presentation and spontaneous onset of labor during 37-41 weeks gestation; BMI less than 30; oral and written information and an invitation to join the study was given by midwives at second trimester ultrasound examination ot at antenatal clinics to eligible women who had reached approximately 28 weeks gestation this sample was randomized to birth The birth seat did not reduce the number of instrumental vaginal births. While the birth seat presented an increased blood loss between 5001000mL, there was no increase in blood loss over 1000mL. Giving birth on the birth seat showed no adverse consequences on perineal outcomes and may be protective against episiotomies. Strengths: 1. This study set good eligibility criteria that could present problems during laboring if not addressed ahead of time 2. This study has a good sample size for an experiment to be able to see trends in the data collected Weaknesses: 1. There were some women included in the study who had BMIs over 30 and women who were under 37 weeks gestation when they began laboring, article believes that since the women were randomized, the inaccuracies may cancel each other out 2. Generally a high rate of non-compliance NON-SUPINE BIRTHING POSITIONS Waldenstrom, L., Nilsson, C. (1997) LOE:II (Amanda Farr) The purpose of this study is to evaluate the effect of birth center care on pregnant women’s health during pregnancy, labor and delivery, and postpartum. 19 on a birth seat (experimental group) or birth in any other position (control group) E) BirthRite birthing seat; or other instrumental devices if the mom’s labor required it (ex: episiotomies) F) Primary outcome measurement: number of instrumental deliveries; Secondary outcome measurements: perineal lacerations, perineal edema, maternal blood loss and hemoglobin A) The study’s population was randomly and equally assigned to either a birthing center or standard care for antenatal, intrapartum, and postpartum care. Clinical records and questionnaires were in intrapartal studies, and some noncompliance seen in this study when women would use the birthing seat briefly then switch to another position for the remainder of labor which may invalidate some of the data collected 3. Prolonged labor or suspected fetal compromise may also lead to noncompliance Women who were assigned to Strengths: the birth center used more 1. The article was alternative birthing positions strong in that is during labor and delivery, followed the which is relevant to our topic participants of non-supine birthing throughout the positions. The article has a whole pregnancy wonderful chart giving process including statistics on 7 birthing antenatal, positions used and the number intrapartum, and of women from each postpartum care. NON-SUPINE BIRTHING POSITIONS 20 used to collect experimental group that used information on the them. health outcomes and medical procedures. B) 1860 pregnant women who did not have a general complicating condition, were not drug abusers or smoker, and who had had a previous VBAC if had history of cesarean delivery. C) Women were randomly assigned to their group during a prenatal visit to the birth center. 928 were assigned the birth center and 932 were assigned standard hospital care. D) Each woman used her assigned care throughout the pregnancy, birth, and postpartum period and data was collected from her medical records and through questionnaires. 2. There is a great chart with valuable information pertaining to nonsupine birthing positions, which is very applicable to our project. 3. The information gathered was directly from the patient’s records or from a survey that they filled out making the data valid. Weaknesses: 1. Blood loss was reported subjectively as an estimate, which could affect validity. 2. Possible bias based on differences midwives’ on breastfeeding support and length of postpartum stay could affect the postpartum survey results. NON-SUPINE BIRTHING POSITIONS Miqueletti, M., Cecatti, J., Makuch, M. (2013) LOE: V The objective of the study was to report the experience of labor as described by nulliparous women who participated 21 E) A mailed questionnaire was used to collect information from the women two months after their delivery. Also, case records were used to gather information from for each woman. F) With the collective data concerning antenatal, intrapartum, and postpartum care Waldenstrom and Nilsson concluded that birth center care is just as effective as standard hospital care for pregnant women and their babies. The birth center is just as safe and effective in identifying complications. A) Qualitative study B) 21 women C) Purposeful (criterion) sampling; 11 women who participated in a BPP and 10 women attending routine All the women, independently of having participated or not in the BPP, said that they had felt more comfortable during labor when they adopted an upright position. The majority considered sitting Strengths: 1. A possible strength of the study lies in the fact that only primiparous women were enrolled as intent to facilitate NON-SUPINE BIRTHING POSITIONS (Abby Rose) and who did not in a systematic Birth Preparation Program (BPP). 22 prenatal care D) The BPP consisted of systematized antenatal group meetings structured to provide physical exercise and information on pain prevention during pregnancy, the role of the pelvic floor muscles, the physiology of labor, and pain relief techniques. E) A digital recorder for the interview F) Control of labor, positions adopted during labor, and satisfaction with labor. and standing up, walking identification of the around, exercising with the effect of antenatal ball on the floor or in the guidance on labor shower as the most and delivery. comfortable positions. On the 2. Another possible other hand these women strength of the study considered horizontal was that the positions less comfortable, interviews were since they hampered their conducted before mobility and increased the discharge from the sensation of pain during maternity hospital; contractions. All of the therefore the women who participated in a birthing experience systematic preparation said was very present for that they had felt at ease to these women. As a assume different upright way to minimize a positions and had changed possible “courtesy positions based on how they bias,” all the were feeling and on what they interviews were had learned during conducted by a preparations. They said they professional that did adopted upright positions to not have contact facilitate cervical dilation and with the participants to help the progression of during BPP labor. The women who did activities or other not participate in a systematic project activities. preparation reported after receiving guidance from the Weaknesses: staff in the labor room they 1. A possible weakness began to use some upright of the present study positions during labor. Some was the fact that women said that adopting spinal anesthesia is vertical positions brought routinely used at the NON-SUPINE BIRTHING POSITIONS 23 comfort and relieved pain, even though they were not at ease to adopt these positions or to change positions without seeking guidance from the staff. maternity ward where the women delivered their babies. The decision about when spinal anesthesia is performed in labor is made by the anesthetic and OBGYN staff and is not a women’s choice. Consequently is was not possible to evaluate women’s autonomy on pain relief only using the alternative of nonpharmacological coping strategies for pain control. 2. Another possible weakness may be the fact that women had the possibility of freely participating in routine educational interventions offered at the institution during prenatal care and for this reason most participants of NON-SUPINE BIRTHING POSITIONS De Jonge, A., Teunissen, D., Van Diem, M., Scheepers, P., Largo-Janssen, A. (2008) LOE: VI (Meagan Holt) The purpose of this study was to explore the views of midwives on different women’s positions during the second stage of labor, and determine when the best time to inform mothers about the benefits of different birthing styles. 24 A.) Qualitative B.) Midwives C.) Purposive sampling of 31 midwives who worked in a practice consisting of one to six midwives, however only one to three of these midwives took part in the study. These midwives assisted women who were having a spontaneous vaginal delivery. D.) There are no methods 31 female participants consisted of various ages and educational backgrounds who worked in a practice of one to six midwives. All but five stated that they used the stool position which is the most common form of upright positioning in the Netherlands. A quarter of the midwives stated that the within the last 10 births had been supine. the present study had taken part in some educational activity. However, some routine activities offered during prenatal care were held outside the medical consultation days, with voluntary participation, were not attended regularly nor systematic educational intervention were performed. Strengths: 1. Increasing the number of midwives that give women an informed choice of different birthing positions may assist them in using a position that is most appropriate and comfortable for them. 2. All midwives conducted practice in the Netherlands. 3. This was a valid NON-SUPINE BIRTHING POSITIONS 25 of interventions used in this study. E.) Interview with midwives F.) Measuring informed consent vs. informed choice. Women expect midwives to source to incorporate give professional opinions on into clinical practice. positions for delivery, and this advice is a stronger influence Weaknesses: than the woman’s personal 1. None of the preference. midwives in this study were opposed By informed choice we mean to non-supine that the midwife explores positioning. what the women think about a 2. Some of the birthing position and actively midwives knew the give them the appropriate interviewers information on various conducting this position options and assist study. them in making their own 3. A quarter of choice. participants stated that of the last ten Only one midwife said that births they assisted she routinely discussed in delivering, the birthing positions with mother was in a women in the antenatal clinic. supine position. 4. Not all of the In most groups, participants midwives had the mentioned that they preferred same type of to perform episiotomy or practice. 87% vaginal examinations in practiced in a group, supine positions and as a while only 7% result of doing this, most practiced mothers would then deliver in individually. a supine position. 5. Bias because of the small sample size used and only allowing midwives NON-SUPINE BIRTHING POSITIONS De Jonge, A., Teunissen, T., Lagro-Janssen, A. (2004) LOE: I (Amanda Farr) The purpose of this review is to determine what the benefits are for women of the routine use of the supine position for the second stage of labor compared to other positions in terms of maternal morbidity and comfort and the morbidity of the baby. 26 A) Meta-analysis of randomized controlled trials, as well as case-control and cohort studies B) Women in the second stage of labor expecting to have a vaginal delivery. C) Nine randomized controlled trials and one cohort study D) The implementation of non-supine birthing positions during the second stage of delivery E) Apgar scale was used to assess babies after vaginal birth. Observation of lacerations and a clock to time the length of the second stage of birth were used to assess the delivery outcomes. F) For the mother: medical interventions for failure to The supine position during vaginal delivery resulted in an increased rate of instrumental deliveries and episiotomies, and a decreased rate of blood loss and postpartum hemorrhage. There were no significant differences found in the newborn’s Apgar score or rate of fetal heart rate abnormalities and neonatal resuscitation between the supine and non-supine birthing positions. Women reported their pain level to be higher while in the supine position compared to when they sat on a birthing stool. who work in practices of six or less midwives. Strengths: A large number of studies were considered in the review leading to large amounts of data gathered for consideration. Weaknesses: In some studies, it was not clear how the second stage of labor was defined. This could cause a lack of validity if not all studies considered the second stage to be at the same point during the labor process. Health care professionals subjectively assessed most outcomes. NON-SUPINE BIRTHING POSITIONS 27 progress, trauma to the birth canal, estimated blood loss, postpartum hemorrhage, hemoglobin levels after delivery, urine or feces incontinence, pelvic pain or instability, and the mother’s satisfaction with the labor and delivery experience, as well as her perception of pain. For the baby: abnormal fetal heart rate patterns, Apgar scores, mean umbilical cord artery pH, and the need for neonatal resuscitation. Lawrence, A., Lewis, L., Hofmeyr, G.J., Styles, C. (2013) LOE: I (Amanda Farr) The purpose of this review is to assess the effects of encouraging women to assume different upright positions versus supine positions during the first A) Systematic Review B) Women in the first stage of labor C) 25 randomized and quasi-randomized trials; total of 5218 women D) The position assumed by the woman during Walking and upright positions during the first stage of labor decreases the length of labor and risk for cesarean birth, the need for an epidural, and does not have any negative effects on the mother or baby. Strengths: There was a very large sample size among the 25 studies. Randomization was utilized in all of the studies. A large number of non-supine positions were used during the women’s first stage of labor, as well as a number of supine NON-SUPINE BIRTHING POSITIONS Gupta, J., Hofmeyr, G., Shehmar, M. (2012) LOE: I (Amanda Farr) 28 stage of labor concerning length of labor, type of birth, and other outcomes for the mother and newborn. the first stage of labor- either upright or supine. E) The Cochrane Handbook for Systematic Reviews of Interventions was used for data collection, assessing study quality, and analyzing results. F) Maternal outcomes: duration of first stage of labor, mode of birth, and maternal satisfaction with positioning and the childbirth experience. Neonatal outcomes: fetal distress requiring immediate birth and use of neonatal mechanical ventilation. The purpose of this review is to assess the benefits and risks of the use of different positions during the second stage of labor. A) Systematic review B) Pregnant women during the second stage of labor without epidural anesthesia C) 22 randomized and quasi-randomized controlled trials; total positions for the control groups. Weaknesses: Quality of studies vary among the 25 reviewed which could affect the validity of the results. There are several possible benefits for upright posture in women without epidural during the second stage of labor but with the possibility of blood loss greater than 500 mL. Women should be allowed to make choices Strengths: A large sample population consisting of 7280 women provided a large quantity of data for assessment. Weaknesses: Random sequence generation, NON-SUPINE BIRTHING POSITIONS 29 of 7280 women D) The use of any upright or lateral position during the second stage of labor compared to the supine or lithotomy position. E) Two review authors assessed and extracted data from the 22 trials. F) Maternal outcomes: pain, use of any analgesia or anesthesia, mod of delivery, trauma to the birth canal that required suturing, blood loss greater than 500 mL, manual removal of placenta, and urinary or fecal incontinence. Newborn outcomes: abnormal fetal heart rate patterns needing intervention, admission to neonatal intensive care unit, and perinatal death. about their birthing positions. allocation concealment, blinding, incomplete outcome data, and selective reporting are weaknesses present in this review that pose a risk for bias. NON-SUPINE BIRTHING POSITIONS 30