4NJ-DVHIMSS-T4-Temple-Kapoor
advertisement

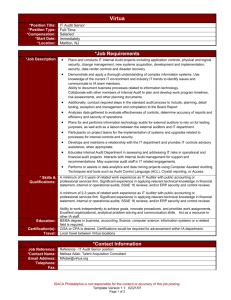
THE AMBULATORY CARE MODEL OF THE FUTURE HAS ARRIVED AT VIRTUA Virtua Medical Group / Richard Temple & Associates, LLC Presented By: Date: Dr. Tarun Kapoor, Vice President/Senior Medical Director, Virtua Medical Group at Virtua Health Rich Temple, Founder/CEO, Richard Temple & Associates, LLC October 29, 2015 Biography Slide for Dr. Tarun Kapoor Tarun Kapoor, MD, SFHM is the Vice President, Senior Medical Director for Virtua Medical Group (VMG), a 300+ clinician multispecialty medical practice. He has been a practicing hospitalist with VMG since its inception in 2008. He joined Virtua’s Medical Informatics team in 2010, helping to develop and implement its inpatient electronic medical record, including full deployment of CPOE and electronic Medication Reconciliation. Prior to joining Virtua, Dr. Kapoor was Regional Director for EmCare’s Mid-Atlantic Hospitalist Division. While at EmCare, Dr. Kapoor developed 16 inpatient care programs for Clinical Staffing Solutions, which was subsequently acquired by EmCare. Dr. Kapoor trained in Internal Medicine at The George Washington University Hospital, where he stayed on an extra year to serve as Chief Resident and Clinical Instructor. He obtained his medical degree from Rutgers Robert Wood Johnson and his undergraduate degree in Government and Chemistry from Cornell University. In his spare time, he is an avid traveler, ice hockey player, golfer and a fly-fishing novice. Biography Slide for Rich Temple Rich Temple has over 25 years of healthcare experience at all levels. He is currently the Founder/CEO of Richard Temple & Associates, a consultancy specializing in healthcare advisory and strategy. In a recent engagement, Rich led numerous strategic projects at the Virtua Medial Group around physician-health system alignment, touching on many current healthcare priorities. Prior to this, Rich was the National Practice Director for IT Strategy for Beacon Partners (now KPMG), an established consulting firm dedicated to serving the healthcare provider community. Before joining Beacon, Rich was a CIO at two different major multi-facility health systems where he led many system implementations, including a major “bigbang” EHR implementation which won multiple awards from the EHR vendor for its overall success. . Rich is a former President, Secretary, and Board Member of NJ HIMSS and has recently relocated to Philadelphia and is becoming more involved with the DV Chapter of HIMSS. About Virtua 3 acute-care hospitals 82 physician office locations 9 ambulatory surgery center locations Virtua Medical Group: A Multi-Specialty Practice (287 Physicians + 87 NP/PA /OB Triage / Midwives) 9.2.15 Family Medicine (84 Physicians, 18 NP, 3 PA) Breast Surgery (4 Physicians, 2 NP, 1 PA) GYN Onc (2 Physicians) Infectious Diseases (11 physicians) Dental (3 Physicians) Female Pelvic (1 Physician) Pulmonary (12 Physicians, 3 NP) Neurology (2 Physicians, 2 NP,) Surgery (34 Physicians, 5 NP, 2 PA) Urgent Care (16 Physicians, 12 NP) Maternal Fetal Medicine (6 Physicians) Internal Medicine (7 Physicians, 2 NP) Hospitalist (59 Physicians 9 NP) Women’s Primary Care (3 Physicians 1 NP) Endocrinology (7 Physicians, 2 NP, 2 PA) Cardiology (19 Physicians, 5 NP, 1 PA) Podiatry (7 Physicians) Occupational Health (4 Physicians, 5 NP) Community 6 Ob-Gyn (7 Physicians,3NP) OB Triage (12) Midwives (2) Women’s Hospital/Specialists Surgery Virtua’s Overarching Vision for Ambulatory “Form Follows Function” Everything revolves around the patient experience Remove Wasteful Processes Easy-in / easy-out – minimize waiting Collaboration among caregivers is emphasized at all points in the care continuum The office visit comprises only a part of the patient’s care experience Care Redesign & Delivery Strategies Access: Streamline Office Operations & functions. Optimize types, number, functions of care team members. Build Access Around the Patient’s Needs, not the Provider’s Patient Activation: Redesign patient encounter to maximize patient activation. Patient activation means the patient self motivates and sustains wellness activities outside of the clinician office Evidence-Based Care: Highest quality care doesn’t necessarily means the greatest amount of resource utilization Care Coordination: Redesign patient encounter to incorporate care across multiple providers and across multiple episodes of care “Wherever you go, we’re there to care for you” Methodologies for Realizing the Vision at the Virtua Medical Group Engaging ALL stakeholders at all points in the process of opening a new ambulatory care center Larger exam rooms to accommodate family members and make it easy for the doctor being able to face the patient throughout the examination Overall office design to optimize the patient’s journey through the entirety of their visit Utilizing the Six-Sigma expertise of Virtua’s “Business Operations Excellence” (BOE) team to understand workflow and overall patient throughput in extremely granular detail Methodologies for Realizing the Vision at the Virtua Medical Group A “welcome center” to provide a warm environment for patients upon their arrival Office layouts that facilitate easy collaboration between physicians and all office staff Providing maximum appointment access to patients through close coordination with Virtua’s Access Center Offering a deep clinical support structure to ensure the EHR is as information-rich as possible and that doctors can have key information about potential care gaps readily pushed to them in the exam room Engaging All Stakeholders When Opening a New Ambulatory Care Center This means ALL stakeholders: • Physician leadership • Physicians in the practice • Office management and staff • VMG management and staff • Virtua leadership • Virtua Facilities department From the initial design session through to the opening of the facility, meet with physicians, office managers, office staff to understand what their current pain points are and how the new center should be configured to address those points Also engaged with Virtua’s Patient Family Advisory Council to get direct “voice of the customer” feedback on our ambulatory care concepts Engaging All Stakeholders When Opening a New Ambulatory Care Center Communicate, communicate, over-communicate We sent out bi-weekly emails about progress on our key projects to everyone involved in any project to create a sense of ownership and skin-in-the-game Make sure the right people are communicating with each other to avoid silos • Physicians • Medical Group leadership • Facilities management • Architects Speak at as many meetings as possible and solicit feedback at these meetings Be prepared to be flexible when scheduling these meetings; physicians often are most accessible very early or very late in the day Providing food helps drive attendance! Engaging All Stakeholders When Opening a New Ambulatory Care Center Having a common liaison to work with all parties to shepherd new construction initiatives through the five key project phases: Test Fit Planning Program Verification and Schematic Design Design Development Construction Documents Bidding and Construction Administration Facilitating direct discussions with all parties – reducing the risk of miscommunication and ensuring the architects clearly understood the needs of the practice in the new locale Going beyond the traditional “Exam” Room Inspired by the Advisory Board’s “Four Zone Exam Room” model, but adjusted to address Virtua’s needs Overall Practice Office Design to Optimize the Patient’s Journey Through the Entirety of Their Visit “Welcome Center” The “gateway” to the (potentially) multiple practices located in the ambulatory care center Warm, inviting The center will have a “greeter” always available to greet patients and immediately answer any questions they may have Check-in occurs here – via either kiosk or via human office assistant – for all practices (exception: Urgent Care, since there are no appointments for Urgent Care Instant communication to medical assistant that patient has arrived and can be roomed Secondary waiting area for family members nearer to the room itself (if they are not going to be in the exam room with the patient) Overall Practice Office Design to Optimize the Patient’s Journey Through the Entirety of Their Visit Strategic placement of functions relevant to the patient encounter Scales / vital-sign collection – right near the entrance to the office suite – on the way to the room. Provide privacy but “keep the flow going” Point of care testing (“POCT”) blood draws or urine samples – lab right next to patient bathroom Clean and soiled utility areas easily accessible but sufficiently far from typical patient paths Placement and angling of exam tables Placement of sinks Set-up of advanced technology to share key information with patients Overall Practice Office Design to Optimize the Patient’s Journey Through the Entirety of Their Visit The team pod: the collaborative area right at the heart of the practice! All caregivers work closely together in a common place with frequent interactions with physicians Full line-of-sight to all exam rooms so everyone can know what is going on and when they are needed Physician “touch down areas” right in the pod and also along the perimeter of the pod Strategic placement of printers and scanners within the pod area Shared physician spaces with very comfortable surroundings – optimize clinical and revenuegenerating areas A Rendition of a Team Pod The “Business Operations Excellence” Team (“BOE”) and Six Sigma Best Practices Virtua has a team of Six Sigma experts who played a hugely valuable role in allowing best practices to be facilitated in the new ambulatory spaces Fleshed out exact processes Identified chokepoints at various points in those processes, along with potential resolutions – • Rigorous attention to "reality" during the design process. Detailed time-and-motion studies to look at patient volumes, calls handled by Medical Assistants per hour, peak periods, potentially uncomfortable high-traffic areas Some Process Areas Examined by BOE Pre-registration process Arriving patients Scanning scripts Providing med lists, ACO packets (where appropriate), new patient welcome kits, collecting copays and other outstanding balances Printing receipts Getting necessary HIPAA and other forms signed Handling walk-ins Handling patients who need to speak to the office staff but don't have an appointment that day (a surprisingly large percentage) Alerting medical assistants to patient arrival Some Process Areas Examined by BOE (continued) Rooming the patient - involves non-obvious things like making the walk from the main Welcome Center to the room and the shared practice waiting area as quick as possible; also need to figure out what types of hardware (e.g., tablets) should be used by the MAs to make this process easy Prepping for medical assistant initial discussion Prepping for the physician visit itself Communicating any next steps / referrals to appropriate staff Printing necessary materials for the patient (referrals, educational collateral, etc.) Check-out (in-room where possible) In-Room Check-Out – New Concept Studies have shown that patients appreciate not having to make an additional stop on their way out after their visit has completed That said, there are circumstances where the check-out process is sufficiently complex and time-consuming that a separate room is necessary Want to balance patient happiness with not locking down a room that could throw off a physician’s schedule Pilot studies showed that patients liked it and it wasn’t unduly cumbersome on physicians, though physicians had – and to some extent, continue to have - concerns Questions: who does the check-out, what types of technology do they need to do it effectively, how to print off additional information for patients while they are in the exam room? A Major Imperative: Providing As Much Access As Possible While Maintaining High Clinician Utilization Virtua maintains a well-staffed “Access Center”, using CRM technology to help patients get appointments and coordinate referrals This Access Center handles a great deal of the scheduling for the Medical Group and reduces this burden for the individual practices The dedicated focus on this with the Access Center allows for a terrific array of metrics showing improvements in patient satisfaction This is one more way that processes are getting streamlined in the new model of ambulatory care at Virtua Clinical Support Services New and revolutionary concept being rolled at Virtua to: Proactively perform outreach to patients prior to an appointment to ensure whatever tests were supposed to be present, in fact, are Aggregating data from a multitude of sources to provide a clear picture to the physician – right in the exam room - of key quality indicators and potential care gaps Relieve the practices of much of the burden of ongoing patient follow-up, medication refill processing, etc. Final Thoughts Key success factors for success in the increasingly ambulatory-centric healthcare provider model: Vision Leadership Communication Collaboration Execution Work closely with your Marketing departments, service-line coordinators, and others to make sure that you are deploying services in a market where those services are needed and that you can do it in a manner that supports organizational strategy Thank you for your time! Questions?