lecture # 18 human development
advertisement
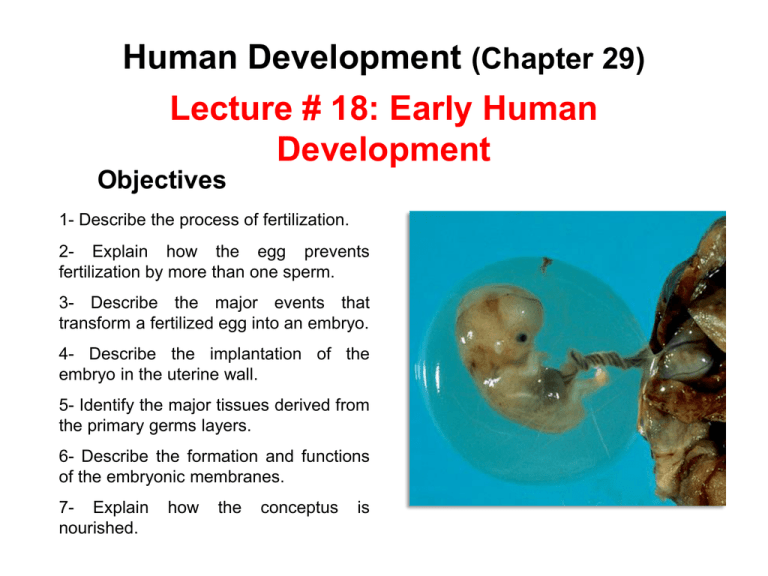
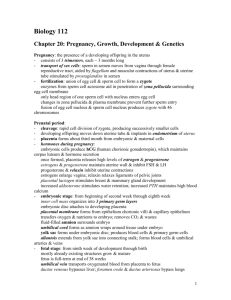
Human Development (Chapter 29) Lecture # 18: Early Human Development Objectives 1- Describe the process of fertilization. 2- Explain how the egg prevents fertilization by more than one sperm. 3- Describe the major events that transform a fertilized egg into an embryo. 4- Describe the implantation of the embryo in the uterine wall. 5- Identify the major tissues derived from the primary germs layers. 6- Describe the formation and functions of the embryonic membranes. 7- Explain nourished. how the conceptus is Oogenesis Oogonia Diploid OOGENESIS MITOSIS Primary oocyte Diploid MEIOSIS I It stops in prophase Before birth MEIOSIS I Completed First polar body After puberty Secondary oocyte Haploid MEIOSIS II It stops in metaphase 1st & 2nd polar body MEIOSIS II Completed Before ovulation After ovulation If fertilization occurs Secondary oocyte Haploid Ovulation of mature (graafian) follicle Oocyte at Ovulation Egg First polar body Secondary oocyte (arrested in metaphase of meiosis II) If not fertilized If fertilized It completes meiosis II Dies Second polar body (dies) Zygote Embryo Zona pellucida It is a layer of glycoprotein gel secreted by granulosa cells around the oocyte. Corona radiata It is composed of several layers of granulosa cells. Mature Spermatozoon Acrosome Head It contains enzymes that break down material surrounding the oocyte. Nucleus It contains one set of 23 chromosomes (haploid). Basal body It is the first part of the flagellum nestled in an indentation in the base of the nucleus. Mitochondrion They provide the ATP needed for the beating of the tail. Axoneme It is the core of the flagellum consisting of microtubules. Midpiece of tail Tail It propels the sperm during migration in the female reproductive system. Principal piece of tail Endpiece of tail Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Fertilization There are two mechanisms to prevention of polyspermy (fertilization by two or more sperm): 1- Fast block: Binding of the sperm to the egg opens Na+ channels in egg membrane. Inflow of Na+ depolarizes the membrane and inhibits the attachment of any more sperm. 4 Rejected sperm 3 Fertilization membrane 2 Cortical reaction 2- Slow block : Sperm penetration releases an inflow of Ca2+, which stimulates the cortical granules to release their secretion beneath the zona pellucida. The secretion swells with water, pushes any remaining sperm away and creates an impenetrable fertilization membrane between the egg and the zona pellucida. 1 Acrosomal reaction It is the exocytosis of the acrosome, releasing the enzymes needed to penetrate the egg. Two acrosomal enzymes are released: Hyaluronidase, which digests the hyaluronic acid that binds granulosa cells together. Acrosin, a protease similar to trypsin. When a path has been cleared, a sperm binds to the zona pellucida. Cortical granules The Preembryogenic Stage 1- Cleavage It comprises the first 16 days of development, culminating with the existence of an embryo. 3- Embryogenesis It refers to the mitotic divisions that occurs 1-Cleavage: in the first 3 days, while the conceptus migrates down the uterine tubes. Zygote Egg pronucleus Morula (72 hours) It is a solid ball of 16 cells that resemble a mulberry. Blastomeres 2-celled stage 4-celled (30 hours) stage 2- Implantation 8-celled stage The morula lies free in uterine cavity for 4-5 days and divides into a 100 cells or so. Blastocyst Sperm pronucleus Fertilization (0 hours) Migration of the Conceptus The zona pellucida disintegrates and releases conceptus: blastocyst. Implanted blastocyst (6 days) 2- Implantation Embryoblast Blastocyst: Blastocoel Trophoblast: Embryoblast Trophoblast Cytotrophoblast Syncytiotrophoblast (6-7 days) Endometrium: Epithelium Endometrial gland The blastocyst attaches to uterine wall 6 days after ovulation, usually on the fundus or the posterior wall of the uterus. 2- Implantation: It is the process of attachment to uterine wall that begins when blastocyst adheres to the endometrium. The trophoblast secrets human chorionic gonadotropin (HCG), which stimulates the corpus luteum to secret estrogen and progesterone (it suppresses menstruation). (8 days) The trophoblast on the attachment side separates into two layers: The superficial layer in contact with the endometrium. The plasma membranes break down and trophoblastic cells fuse into a multinucleate mass called syncytiotrophoblast. The deep layer, close to embryoblast, retains the individual cells divided by membranes and is called cytotrophoblast. 3- Embryogenesis Embryogenesis: It is the arrangement of the embryoblast into three primary germ layers: ectoderm, mesoderm, and endoderm. The embryoblast separates slightly from the trophoblast and creates a narrow space between them: the amniotic cavity. Amniotic cavity Ectoderm Mesoderm Endoderm Once the three primary germ layers are formed, embryogenesis is complete and the individual is considered an embryo. It is about 2 mm long and 16 days old. Zygote Morula Blastocyst Embryo The ectoderm and endoderm are epithelia composed of tightly joined cells. The mesoderm is a more loosely organized tissue which differentiates into a loose fetal connective tissue called mesenchyme. Several accessory organs develop along side the embryo: the placenta, the umbilical cord and four embryonic membranes (amnion, yolk sac, allantois, and chorion) Amniotic cavity Yolk sac Chorion Amnion Allantois They are extensions of Chorionic syncytiotrophoblast into the villi endometrium by digestion and growth of “roots” of tissue. Placental sinus 16 days Uterus Chorionic villus Placental sinus They are lacunae filled with maternal blood that merge and surround villi. Developing placenta Umbilical blood vessels Allantois Yolk sac Amnion Amniotic cavity 28 days Chorion 12 weeks Umbilical cord Placenta It contains two umbilical arteries and one umbilical vein. Allantois It begins as an outpocketing of the yolk sac. It forms the foundation for the umbilical cord becomes part of the urinary bladder. It contributes to formation GI Yolk sac tract, blood cells, and future egg or sperm cells. Amnion It is a transparent sac that grows to completely enclose the embryo and penetrated only by the umbilical cord fills with amniotic fluid. Chorion It is the outermost membrane enclosing all the rest of the membranes and the embryo. The Amniotic Fluid At first, amniotic fluid is formed from filtration of mother’s blood plasma. Beginning at 8 to 9 weeks, the fetus urinates into the amniotic cavity about once per hour contributing substantially to fluid volume. The fetus swallows amniotic fluid at the same rate. At term, the amnions contains about 700 to 1000 mL of fluid. 12 weeks Functions of the Amniotic Fluid: 1- It protects the embryo from trauma, infections, and temperature fluctuations. 2- It allows freedom of movement important to muscle development. 3- It enables the embryo to develop symmetrically. 4- It prevents body parts from adhering to each other. 5- It stimulates lung development as the fetus‘ breathes’ fluid. Amniotic cavity fills with amniotic fluid. Prenatal Nutrition During gestation the conceptus is nourished in three different, overlapping ways: 1- Uterine milk 2- Trophoblastic nutrition 3- Placental nutrition 1- Uterine milk It is a glycogen-rich secretion of the uterine tubes and endometrial glands. The conceptus absorbs this fluid as it travels down the tube and lies free in the uterine cavity before implantation (6, 7 days). 2- Trophoblastic nutrition The conceptus consumes decidual cells of the endometrium. Progesterone from corpus luteum stimulates decidual cells to proliferate and accumulate a store of glycogen, proteins, and lipids. It is the only mode of nutrition for the first week after implantation and remains the dominant source through the end of 8 weeks. 3- Placental nutrition Nutrients diffuse from the mother’s blood through the placenta into the fetal blood. The placental phase is the period beginning the 9th week and it is the sole mode of nutrition from end of 12th week until birth. Placenta and Umbilical Cord As the placenta grows: The villi grow and branch and their surface area increases. The membrane becomes thinner and more permeable. The placental conductivity (the rate at which substances diffuse through the membrane) increases. Materials diffuse from the side of the membrane where they are more concentrated to the side where they are less concentrated. Oxygen and nutrients pass to the fetal blood. Fetal wastes pass the other way and are eliminated by the mother. The placenta is also permeable to nicotine, alcohol, and most other drugs that may be present in the maternal blood stream. Blood Circulation in the Adult Pulmonary trunk Aorta Superior vena cava Right atrium It receives O2 poor blood returning to the heart through the superior and inferior vena cava and the coronary sinus. Left atrium It receives O2 rich blood returning from the lungs through the pulmonary veins. Pulmonary veins Left ventricle It pumps O2 rich blood through the aorta artery to every organ of the body. Inferior vena cava Right ventricle It pumps O2 poor blood to the lungs through the pulmonary arteries. Blood Circulation in the Fetus Pulmonary trunk Aorta Foramen oval Ductus arteriosus 2 Blood bypasses the lungs by flowing directly from the right atrium through the foramen oval into the left atrium. Right atrium 1 It receives O rich blood 2 returning from the placenta, mixed with O2 poor returning through the inferior vena cava. Inferior vena cava 3 2 1 3 Blood also bypasses lungs by flowing from pulmonary trunk through ductus arteriosus to aorta. the the the the