Item 6.2a Quality & Performance Report January11
advertisement
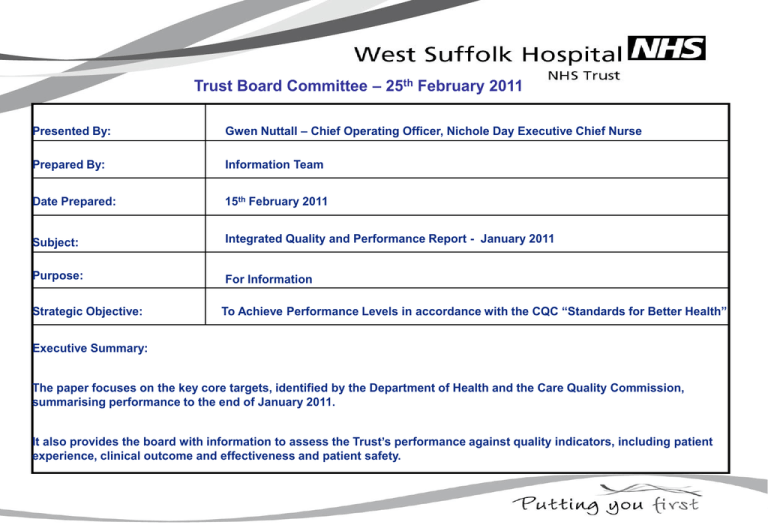
Trust Board Committee – 25th February 2011 Presented By: Gwen Nuttall – Chief Operating Officer, Nichole Day Executive Chief Nurse Prepared By: Information Team Date Prepared: 15th February 2011 Subject: Integrated Quality and Performance Report - January 2011 Purpose: For Information Strategic Objective: To Achieve Performance Levels in accordance with the CQC “Standards for Better Health” Executive Summary: The paper focuses on the key core targets, identified by the Department of Health and the Care Quality Commission, summarising performance to the end of January 2011. It also provides the board with information to assess the Trust’s performance against quality indicators, including patient experience, clinical outcome and effectiveness and patient safety. Matters resulting from recommendations made in this report Financial Implications Present Considered Yes / No Yes / No Workforce Implications Yes / No Yes / No Impact on Equality and Diversity impact Yes / No Yes / No Legislation, Regulations and other external directives Yes / No Yes / No Internal policy or procedural issues Yes / No Yes / No Risk Implications for West Suffolk Hospital (including any clinical and financial consequences): - Failure to deliver the 4 hour core access target for the year. - Failure to achieve C-Difficile target for the year. Mitigating Actions (Controls): • Robust Action Plan developed. • Performance Management and Monitoring. • Improved Escalation • Review of Cohort Unit Level of Assurance that can be given to the Committee from the report based on the evidence [significant, sufficient, limited, none]: SUFFICIENT Recommendation to the Committee: Note the Trust Performance to January 2011 Contents 1. Introduction 2. Emergency Care A&E 3. Cancelled Operations 4. LOS 5. Outcomes & Effectiveness – Clostridium Difficile 6. Patient Safety 7. Risk Assessment 8. Patient Experience 9. Conclusion 1.& 2. Introduction & Emergency Care 1. Introduction: This report provides a briefing to the Board members on the performance against key targets up to January 2011. The paper focuses on the main targets, identified by the Department of Health and the Care Quality Commission. 2. Emergency Care – A&E Target: 95% of patients seen/treated/discharged within 4 hours The Trust did meet the 95% Target for the month of January 2011 (96.14%). Key actions:EAU posts to be advertised in February. Integrated Action Plan agreed and monitored weekly, via weekly A&E departmental meetings. Review of medical commitments in morning and afternoon commenced. Job Plans are being updated. Bed Meetings reviewed and enhanced. Standard operating procedures commenced. Short stay beds introduced on ward G5. Trust will pilot Discharge/Transfer Lounge in March to assist with flow of patients and discharge planning. The updated detailed A&E 4 hour performance action plan is attached as a separate paper. Page 4 3. Cancelled Operations The target was met for January at 0.30% An improvement from last month. Out of theatre time remained the highest reason for cancellation (50%). Bed unavailable (33%). Equipment issues (17%). Target 0.8% Actual 0.85% (YTD) The Productive Operating Theatre project (TPOT) is in progress, and will be reported to the Board in March 2011. Page 5 4. Length of Stay (Spells) The targets are from Dr Foster ‘Expected’ positions using 09/10 as a benchmark. • Non Elective LOS for Medicine is above target – Actions to improve this performance is linked to discharge action plans and implementation of EAU model and short stay beds. •Non Elective LOS for Surgery remains below the expected level, but has seen an increase in 2010/11. This is related to complex elderly patients. •Elective LOS for Surgery is similar to last year. Review of day case and day of surgery activity continues, especially in urology. The productive theatre will also focus on Urology. Page 6 5. Outcomes and Effectiveness Mortality 120 100 80 60 40 20 0 Hospital Standardised Mortality Ratio HSMR has been fairly consistent over recent months and is below the expected level as can be seen by the overall mortality shown in the graphs and the table giving a mortality rate for the five Dr Foster - How Safe is Your Hospital indicators. These tables provide information on relative risk, with red, blue and green traffic lighting. Blue indicates that the score is within the standard deviation. We monitor the HSMR for emergency patients and identify any individual diagnoses that trigger any safety and effectiveness alerts. These are all investigated and reported to the Quality and Risk Committee. Mortality: standardised rate Apr May Jun Rolling 12 Month HSMR-All Admissions 90 85 80 Feb 09 -Mar 10 Mar 09 -Apr 10 Apr 09May 10 May 09 -Jun 10 Oct 09Nov 10 Sep 09Oct 10 Aug 09Sep 10 Jul 09Aug 10 Jun 09Jul 10 May 09Jun 10 Apr 09May 10 Mar 09Apr 10 Feb 09Mar 10 Jan 09 Feb 10 Dec 08 - Jan 10 Oct 08 Nov 09 Sep 08Oct 09 Aug 08Sep 09 Jul 08Aug 09 70 Nov 08 - Dec-… 75 Jan National Rate Jul 08Aug Sep Oct 08 Dec 08 09 – from last Aug 08- 08-Oct - Nov Nov 08 - - Jan Feb reporting 09 Sep 09 09 09 Dec-09 10 10 period Jun 09 -Jul 10 Jul 09Aug 10 Aug 09Sep 10 Sep 09Oct 10 Oct 09Nov 10 - 86.4 85.2 84.5 84.6 82.8 80 80.7 80.2 80.1 76.5 89 89 87.8 86.3 84.6 84.1 86.2 84.9 84.6 84.5 83 80.1 80.8 80.4 80.3 79.6 89.1 89.1 88.1 86.7 84.8 84.2 SMR Stroke (Acute Cerebrovascular Disease) 86.2 85.9 82.6 86.4 82.8 83.3 83.1 82.9 80.9 81.1 79.4 87.8 86.8 88.7 88.6 84.2 84.4 SMR - Heart Attack (AMI) 90 81.6 0.84 100.4 105.1 106.1 94.1 91.8 100.6 96.6 95 92.4 92.1 93.7 94.5 89.4 82.4 78.5 77.9 65 69.4 61.3 64.2 69.5 68.4 64.7 73.3 69.2 60.7 62.9 66.2 66.9 0.65 0.57 0.57 0.44 0.49 0.67 0.62 0.62 0.53 0.49 0.44 0.49 Rolling 12 Month HSMR-All Admissions Rolling 12 Month HSMR-Non Elective SMR - FNOF Mortality from Low Risk Conditions Page 7 Jul Aug Sep Oct Nov Dec Jan Feb Mar 70 65.4 64.9 7 5. Outcomes and Effectiveness Infection Prevention The C. difficile target for 2010/11 is 29 hospital cases although due to the recent C. difficile outbreak the PCT recognised that we would not hit our trajectory and agreed that they would accept no further preventable C. difficile cases. In January there were a further 4 hospital attributed cases, bringing the total to 32 non of which were avoidable. All patients were transferred to the F9 cohort unit within the time frame specified. There have been a further 2 cases in February (as at 17/2/2011), bringing the total to 34. The Trust continues to achieve excellent results in other infection control KPIs. There were no hospital associated MRSA bacteraemia and High Impact Intervention performance has improved. Overall compliance with hand hygiene and the dress code requirements for all directorates in January dropped slightly to 99% and the affected areas are being addressed. Antibiotic Prescribing There has been an improvement in performance to 95%. The revised drug chart which includes a specific antibiotic prescribing section requiring a medical review signature every 3 days is due to be used from the 1st March. Page 8 8 6. Patient Safety Number 20 Pressure Ulcers No of patients with ward acquired pressure sores 15 10 No of patients with ward acquired Grade 3 or 4 pressure sores 5 0 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Falls Number 35 30 25 20 15 10 5 0 Apr No of short RCAs completed for patient falls No of patient falls resulting in harm May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Pressure Ulcers The number of patients with ward acquired pressure ulcers increased this month to 16 however with no Grade 3 or 4 reported. Themes from RCAs: • Lack of continuity of care when patients have been moved around the hospital. • Patient situations that create unavoidable pressure ulcers: patients who choose not to participate in their own pressure ulcer prevention or patients on the Liverpool Care Pathway. Actions: • A pressure ulcer development group has been established to develop, facilitate and review an annual pressure ulcer prevention strategy. • Clinical areas with significant/increased pressure ulcer incidence have been asked to develop action plans concentrating on preventing Grade 2 ulcers, next month themes from Grade 2s will be reported. Patient Falls The number of falls resulting in harm decreased this month to 22, no severe harm was caused. • 16 of these patients had delirium/dementia. Driving forward the dementia strategy by ensuring that patients are more meaningfully occupied may decrease falls in this patient group. The Patient Falls Specialist Group/ Dementia Steering Group have been asked to focus their actions in these areas. • 2 Wards with significant nurse recruitment problems had the highest rates of falls: 41% of total incidences. There are recruitment action plans in place to address these staffing issues. Page 9 9 6. Patient Safety Venous Thrombo-Embolism (VTE) Verbal update to be provided at the meeting by Dermot O’Riordan. Page 10 10 6. Patient Safety Root Cause Analysis (RCA) There were 6 outstanding medical actions and 4 outstanding surgical actions at the month end. The total number of actions demonstrates an on going reduction since September.. Five of the actions reported as outstanding at the last Board have now been completed. 4/6 outstanding actions within Medical Directorate RCAs and 2/4 outstanding actions within Surgical Directorate RCAs have updates indicating progress to achieve completion and evidence is pending. The targeted follow up continues through individual contact with leads as well as presentation of the “outstanding RCA actions” report to the Directorate Performance meetings, Directorate steering groups and the Operational Steering group. Patient Safety Incidents resulting in harm Detail is provided within the SIRI report. Page 12 11 7. Risk Assessments Risk Assessments in date There are currently 108 (as of 15th February) active risks on the Risk Register. Of these, 85 (79%) are in date, while 23 (21%) are late for review. This is a significant improvement as at the start of the year 52% of risk assessments were beyond their review date. The number of risk assessments beyond their review per Directorate are listed below: 1) Medical = 7 2)Trust-Wide = 7 3) Surgical = 6 4) Finance and Information = 2 5) Human Resources = 1 Each directorate receives a monthly report which is discussed at the Directorate Governance Steering Groups. This report details the Directorate’s risk management performance and enables actions to be set on individuals to review/progress risk assessments as necessary. There is also the option to escalate issues where the progression of implementing additional controls is not satisfactory. The Operational Steering Group will be receiving a themed monthly report based on different issues to be addressed from the Risk Register. The Operational Steering Group will deliberate concerns and determine required action with risk management performance accordingly. Page 11 Active risk assessments in date (according to grading Red-3 mths, Amber-6 mths) Additional controls in date Each active risk should identify additional controls which are required to reduce the risk rating to a tolerable level. Currently there are 155 additional controls identified by the active risk assessments. Of these, 124 (80%) are within the agreed timescale, while 31 (20%) have passed their agreed implementation date. This is a significant improvement, as at the start of the year only 51% of the additional controls were in date. The number of additional actions beyond their review date per Directorate are listed below: 1) Medical = 9 2) Trust-Wide = 7 3) Facilities = 6 4) Surgical = 5 5) Finance and Information = 3 6) Human Resources = 1 21% 79% In date Beyond review date 20% The Directorate Governance Performance Meetings and Operational Steering Group reports also detail the actions and status required so that this can be managed/progressed at the Directorate level, and where necessary considered at the Operational Steering Group. 80% In date Beyond im plem entation date 12 8. Patient Experience Patient Satisfaction (Patient Experience Tracker) Overall satisfaction was 95% (see Table 1 for breakdown of clinical areas). (A&E scored 95%+ in all questions with a returns rate of 1350). EAU/ Eye Clinic are developing action plans to increase the volume of patients surveyed. Eye clinic have introduced a volunteer to undertake additional surveys. Main OPD Diabetic Clinic Eye Clinic PAU A&E EAU F4 DSU 1175 returns 650 45 105 1350 5 95 185 93% satisfaction 91% 98% 96% 98% 100% 89% 99% Table 1. Patient Satisfaction Questionnaires (PSQ) (paper) All remaining clinical areas use this method for reporting and overall satisfaction scored 82%. % 100 Patient Satisfaction Questionnaire Enough privacy Call button response time 80 60 The two questions with a red performance rating response was “Has a member of staff told you about medication side effects to watch for when going home?” and “Were you told who to contact if you were worried about your condition after you left hospital?”. Actions: • Matrons to advise ward areas to give PSQ to patients at discharge as patients only receive this information with TTOs. • Discharge leaflets now being used on wards which provide side-effect advice. Page 13 Side effects information 40 20 0 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Contact for worries after discharge Choose hospital again CQUIN Achievement of 2% patients surveyed this month was achieved by all CQUIN reportable areas. 13 8. Patient Experience Same Sex Accommodation Number 300 Same Sex Accommodation 250 200 Same sex accommodation: total breaches 150 100 50 Same sex accommodation: total patients 0 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Environment and Cleanliness % 100 Environmental Audit Environment and Cleanliness Target 80 60 40 20 0 Apr May Jun Page 14 Jul Aug Sep Oct Nov Dec Jan Feb Mar Same Sex Accommodation Same sex accommodation criteria were breached on one occasion during January. This occurred in the assessment area of EAU when two male patients had to be placed in the female assessment bay which contained three female patients. At the time there were no male beds available in the hospital; bed availability and patient movement was being affected by ward closures due to norovirus. Staff apologised to patients and worked with the H@N team to move the female patients to surgical wards as soon as possible. 9. Conclusion The action plan remains in place and performance has improved in January with regard to the 4hr standard. One of the major challenges for the Trust, was in adherence to same sex accommodation , the re-configuration in December has improved performance. Performance with regard to C-Difficile, full RCA’s have been carried out and actions implemented specifically with regard to anti biotic prescribing and monitoring. Progress on other KPI’s is being made. Page 15