Chapter 15 Notes - Castle High School
advertisement
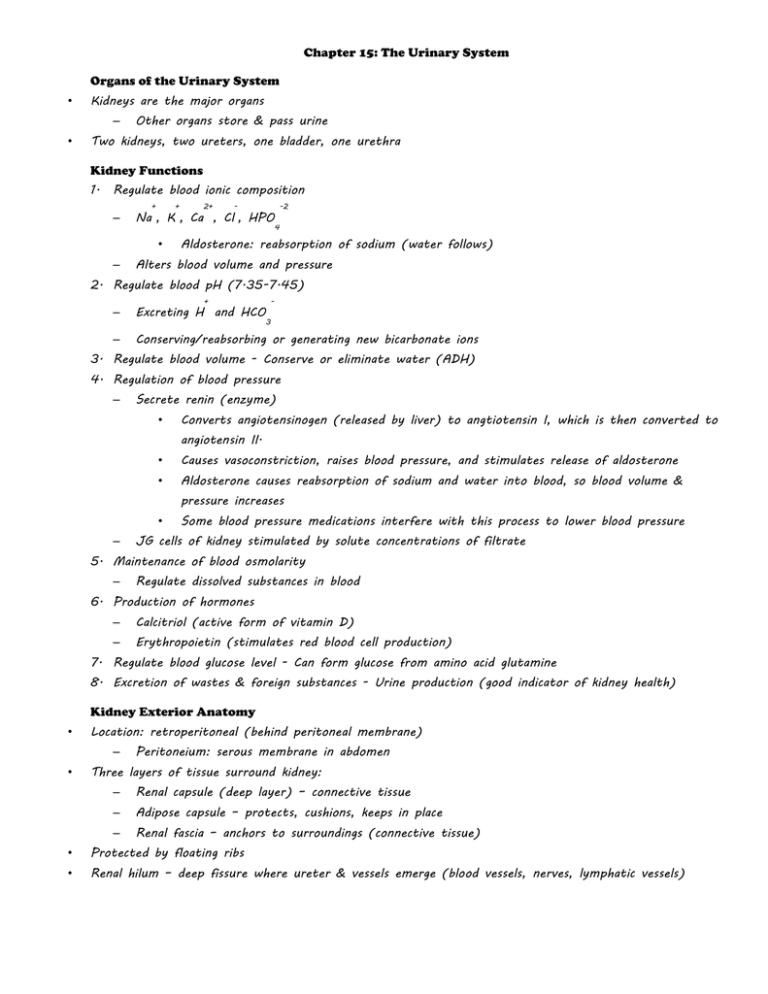
Chapter 15: The Urinary System Organs of the Urinary System • Kidneys are the major organs – • Other organs store & pass urine Two kidneys, two ureters, one bladder, one urethra Kidney Functions 1. Regulate blood ionic composition – + + • – 2+ - Na , K , Ca , Cl , HPO -2 4 Aldosterone: reabsorption of sodium (water follows) Alters blood volume and pressure 2. Regulate blood pH (7.35-7.45) + - – Excreting H and HCO – Conserving/reabsorbing or generating new bicarbonate ions 3 3. Regulate blood volume - Conserve or eliminate water (ADH) 4. Regulation of blood pressure – Secrete renin (enzyme) • Converts angiotensinogen (released by liver) to angtiotensin I, which is then converted to angiotensin II. • Causes vasoconstriction, raises blood pressure, and stimulates release of aldosterone • Aldosterone causes reabsorption of sodium and water into blood, so blood volume & pressure increases • – Some blood pressure medications interfere with this process to lower blood pressure JG cells of kidney stimulated by solute concentrations of filtrate 5. Maintenance of blood osmolarity – Regulate dissolved substances in blood 6. Production of hormones – Calcitriol (active form of vitamin D) – Erythropoietin (stimulates red blood cell production) 7. Regulate blood glucose level - Can form glucose from amino acid glutamine 8. Excretion of wastes & foreign substances - Urine production (good indicator of kidney health) Kidney Exterior Anatomy • Location: retroperitoneal (behind peritoneal membrane) – • Peritoneium: serous membrane in abdomen Three layers of tissue surround kidney: – Renal capsule (deep layer) – connective tissue – Adipose capsule – protects, cushions, keeps in place – Renal fascia – anchors to surroundings (connective tissue) • Protected by floating ribs • Renal hilum – deep fissure where ureter & vessels emerge (blood vessels, nerves, lymphatic vessels) Kidney Interior Anatomy • • Two distinct regions: – Renal cortex (outer) – Renal medulla (inner) – made up of 8-18 cone-shaped pyramids Nephron: functional unit of kidney (mostly in cortex) – • Abundant blood supply (blood filtration) – • About 1,000,000 of them ¼ of blood supply goes through kidneys each minute; supplied by renal arteries Nephrons produce urine – Urine drained into ducts in pyramids to minor calyces • – Calyces enclose tips of pyramids (“cup-shaped”) Then drains to major calyces, then to renal pelvis • Renal pelvis ureter bladder • Nerve supply from renal plexus Nephron Anatomy Page 516 (Figure 15.3) • Two parts: – – Renal corpuscle – blood plasma filtered • Glomerulus: capillary network (knot of capillaries) • Glomerular (Bowman’s) capsule: surrounds glomerulus; contains filtrate from capillaries Renal tubule – passes filtered fluid • Three sections; convoluted (tightly coiled); substances are added or removed from filtrate 1. Proximal convoluted tubule (PCT): renal cortex 2. Loop of Henle (nephron loop): renal medulla 3. Distal convoluted tubule (DCT): renal cortex a. DCT empties into collecting duct that goes down through the pyramid to the calyces • Lined with epithelial tissue of varying types • 80-85% of nephrons are cortical nephrons Renal Physiology Page 518 (Figure 15.4) • Urine formation has three processes – Glomerular filtration (blood to tubule) • Filtration: the use of pressure to force fluids and solutes through a membrane – Nonselective, passive process, Produces “filtrate” – Membrane permits filtration of water and small solutes, but not large solutes » • i.e. blood cells, proteins, etc. (presence indicates a problem) – Afferent artery of glomerulus has higher pressure than efferent artery – Blood pressure very important for process Water and solutes move across capillary wall – More than 99% of what is filtered out of the capillaries returns to the blood stream • GFR: glomerular filtration rate: maintained by kidneys – If too fast, some substances not reabsorbed. If too slow, too much reabsorbed including waste – Regulated by adjusting blood flow and altering surface area of glomerular capillary with contractile cells – Constant GFR promotes health – maintained by kidneys (autoregulation) through feedback loops, nervous system (ANS produces norepinephrine), and endocrine system – Tubular reabsorption (tubule to blood) • 99% of water filtered from glomerulus is returned to the blood • Mostly occurs in the PCT, but DCT & collecting duct also active • Water and solutes (useful substances) reabsorbed by passive and active transport – • Reabsorb amino acids, glucose, urea, ions, small proteins, and peptides Nitrogenous waste is poorly reabsorbed: urea, uric acid, and creatinine (found in high concentrations in urine) • Regulated by hormones – Renin & aldosterone » Both increase reabsorption (increase blood volume) – reinin secreted by glomerular cells which stimulates aldosterone secretion by adrenal cortex – – ADH (pituitary) Tubular secretion (blood & tubule to urine) • Tubular reabsorption in reverse! Blood & tubule cells • Get rid of substances not already in filtrate – urine drugs, creatinine, ions, additional means for regulating pH Hormone Regulation • Tubular reabsorption and secretion are regulated by four hormones – – – Angiotensin II – lowers GFR • Vasoconstriction of afferent arterioles • Increases reabsorption of Na+, Cl-, water • Stimulates release of aldosterone (Na+ reabsorption) ADH – regulates water loss • Released from pituitary gland, increases water permeability of cells by inserting aquaporins • Inhibited by alcohol ANP – atrial natriuretic peptide • Causes increased urine output Urinalysis • Check for normal and abnormal excretions in urine • Reveals kidney health • Normal kidneys produce large volume of dilute urine when fluid intake high and small amount of dilute urine when water intake low – Controlled by ADH – Urinalysis can reveal health of kidneys Dialysis • Used to clean blood if kidneys not functioning • Dialysate: formulated to maintain diffusion gradients to filter out wastes (urea, creatine, uric acid, some ions) & adds needed substances (glucose, bicarbonate) Urine Transportation, Storage, & Elimination • Ureters (pair) – transport urine from kidney to bladder – No valves at opening; pressure in bladder compresses opening and prevents backflow • Bladder – stores urine (approximately 700-800 ml) • Urethra (one) – transports urine from bladder to outside of body – Separate for women; common with reproductive tract for men Kidneys’ Role in Homeostasis • Excretion of nitrogen-containing wastes • Maintaining water balance of blood – ICF is 2/3 of body fluid, ECF is 1/3 of body fluid • • Water gained & lost by ingestion and metabolic synthesis – Hypothalamus: thirst mechanism (most water intake from fluids & foods) – Regulated by hormones (ADH & aldosterone) Maintaining electrolyte balance of blood – Ion concentrations control osmosis, help m aintain pH, carry electrical current, serve as cofactors for enzymes • - + Aldosterone regulates sodium ion content of ECF (and Cl , K , and Mg ) – 80% of sodium reabsorbed from filtrate in PCT – Water follows salt! – Renin-angiotensin mechanism (diagram on next slide) Ensuring proper blood pH – Maintain 7.35-7.45 pH (acidosis or alkalosis if out of balance) – Mechanisms include buffer systems, exhalation of CO , and kidney excretion of H 2 Polycystic Kidney Disease • Degenerative hereditary disease • Kidneys enlarge and have cysts (contain urine) • Eventual outcome: end stage renal failure (transplant needed) Renal Calculi • 2+ – Solutes form crystals that precipitate in the renal pelvis (kidney stones) +