Integumentary System - (www.ramsey.k12.nj.us).
advertisement

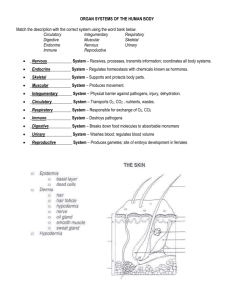
Integumentary System Chapter 5 Overview • Composed of skin and it’s derivatives (sweat & oil glands, hairs and nails) • Primary function is protection The Skin I Two distinct regions 1. Epidermis - outermost protective shield composed of epithelial cells avascularized, obtains nutrients by diffusing through tissue fluid from blood vessels in the dermis 2. Dermis - makes up bulk of skin - tough, leathery layer; fibrous connective tissue - vascularized The Skin II • The dermis and epidermis rest on subcutaneous hypodermis, (superficial fascia) – Not technically part of skin, but shares many of its functions – Mostly adipose tissue w/ some areolar connective – Stores fat – Anchors skin to underlying structures (usually muscle), but allows free sliding – Shock absorber and insulator Epidermis • Avascular, keratinized stratified squamous epithelium • Cells: – Keratinocytes (majority) – Melanocytes – Langerhan’s cells (a.k.a. epidermal dendritic cells) – Merkel cells • Layers/strata (from deep to superficial): – – – – – Stratum basale (basal layer) Stratum spinosum (prickly layer) Stratum granulosum (granular layer) Stratum lucidum (clear layer) *not found in “thin” skin Stratum corneum (horny layer) Dermis - Overview • Dense, irregular connective tissue; Well-supplied with blood vessels, lymphatic vessels & nerves • Cells typical of connective tissue proper: fibroblasts, macrophages, occasional mast cells & WBCs • Semi-fluid matrix heavily embedded with collagen, elastin and reticular fibers • Contains cutaneous receptors, glands & hair follicles Layers of the Dermis • Papillary – superficial & relatively thin – Areolar connective tissue – Dermal papillae that protrude into epidermis – Epidermal ridges that produce fingerprints • Reticular – deep, 80% of dermal thickness – Connective fibers more densely interwoven – Less dense regions between collagen bundles produce cleavage (tension) lines in skin – Points of tight dermal attachment to hypodermis produce dermal folds or flexure lines Skin Color • Skin color reflects the amount of pigments (melanin & carotene) & oxygenation level of hemoglobin in the blood • Melanin production is stimulated by exposure to UV light • Melanin is produced by melanocytes & transferred to keratinocytes where it protects keratinocyte nuclei from damaging effects of UV radiation • Skin color can be affected by emotional state • Alterations in skin color may indicate certain diseases/condition – Ex) Cyanosis, Erythema, Pallor, Jaundice, Bronzing & Bruising Sensory Receptors of the Skin I • Free Nerve Endings: Pain & Temp; cold receptors are more numerous than warm, but there is not obvious structural difference • Hair end plexus: Around base of hair follicle, fires when hair is touched • Meissner’s corpuscle: rapidly adapting mechanoreceptor; perceive light touch; primarily just below epidermis, concentrated in fingertips, palms, lips, tongue, nipples & genitalia • Merkel’s discs: sense pressure & texture; where epidermis meets dermis Sensory Receptors of the Skin II • Ruffini’s organ: slowly adapting mechanoreceptor; senses pressure & temperature; deep in dermis; perceives strecth & touch; monitors slippage & helps gripping mechanism; encapsulated by sheaths of connective tissue, networks of nerve fibers • Pacinian corpuscle: pain & pressure; relatively large, but fewer in number; onion shaped, deep in dermis • Krause’s bulb (bulboid corpuscle): touch; conjuctiva of eye, lips, tongue, genitalia; encapsulated by sheath’s of connective tissue, network of nerve fibers Appendages of the Skin: Sweat Glands • a.k.a “suduriferous” glands • 2 sub-categories – Eccrine (merocrine) sweat glands • Distributed over entire body surface, primary function is thermoregulation • Simple, coiled tubular glands that secrete a salt solution with a few other solutes • Ducts usually empty to skin surface via pores – Apocrine sweat glands • May function as scent glands • Primarily in axillary and anogenital areas • Secretion similar to that of eccrine secretion, but also contains proteins & fatty substances on which bacteria thrive Appendages of the Skin: Sebaceous (oil) Glands • All over body surface, except hands and soles • Simple, aveolar glands, ducts usually empty into hair follicles • Oily secretion, called sebum, lubricates the skin and hair, and acts as a bactericidal agent. • Activated (at puberty) and controlled by androgens Hair • Hair consists of dead, heavily keratinized cells • Hair color reflects amount and kind of melanin present • 2 regions: – Root (embedded in skin) – Shaft (projects from the skin) • Hair structure: – Central medulla (core) – Cortex – Outer cuticle Hair Follicles • Extend from epidermal surface into the dermis, deep end expands forming a bulb • Richly vascularized • Sensory nerve endings, root hair plexus, wraps around each hair bulb. Bending hair stimulates these endings, hair act as sensitive touch receptors • Arrector pili muscles pull follicles into an upright position, producing goose bumps • Components: 1. inner epidermal root sheath, enclosing the matrix (region of hair bulb that produces hair) 2. Outer connective tissue sheath derived from dermis Types & Growth of Hair • Two classifications: – Vellus: body hair of children and adult females – Terminal: coarser, longer hair of eyebrows & scalp • Usually darker • Appear in axillary and pubic regions during puberty • Influences on hair growth and density: – Poor nutrition = poor hair growth – Conditions that increase blood (chronic physical irritation or inflammation) flow generally enhance local hair growth Hair Thinning and Baldness • Hair grows fastest from teen years to 40s, then slows • Hair thinning or alopecia results from hairs are not replaced as fast as they are shed • True baldness (male-pattern baldness) is an x-linked genetic condition Nails • • • • Scale-like modification of the epidermis Correspond to hooves or claws or other animals Composed of keratin, like hair Normally appear pink because of bed of capillaries under nail bed, region over thick nail matix appears as a white crescent, “lunula” Homeostatic Imbalances – Skin Cancer – Most common cause is UV exposure – Basal cell carcinoma is the most common and least deadly. It is slow growing and easily detected prior to metastasis. – Squamous cell carcinoma is faster growing but still usually detected prior to metastasis. – Melanoma (cancer of melanocytes), is the least common but most deadly. However, it is also curable when detected early! – Actinic keratosis are pre-malignant thick, scaly or crusty patches of skin usually found on areas over-exposed to sun; although not cancerous, may develop into a form of skin-cancer Actinic keratosis Basal Cell Carcinoma • Cells of the stratum basale invade the hypodermis • Usually presents as lesions on sun-exposed areas; domeshaped with central pearly ulcer & beaded edge • Slow growing; seldom metastasizes prior to being noticed • Least malignant & most common; (estimated that > 30% of all Caucasians will have it) • 99% of cases can be fully cured by surgical removal Squamous Cell Carcinoma • Arises from keratinocytes of the stratum spinosum • Lesion is a scaly, reddish papule; most often on head or hands • Tends to grow rapidly & will metastasize if not removed • High chance of complete cure, but most be caught early and removed by surgery or treated with radiation Melanoma • Most dangerous; accounts for only ~5% of the cases, but number of cases is on the rise; It is estimated 2% of people will be diagnosed with melanoma in their lifetime • Although the least common, melanoma is responsible for ~75% of all skin-cancer deaths • 99% cure if detected early; when >4mm, probability of metastasis is high and will be at a very rapid rate, probability of cure drops to ~15% • Can occur wherever there is pigment; Approximately 1/3 develop in pre-existing moles, the remaining 2/3 arise “spontaneously” Stages of Melanoma Clark-Beslow System: measurement of depth and thickness T (thickness (1-4); a = no ulceration, b = ulceration N = node involvement M = metastasis • Stage 0: have not grown below the epidermis; surgical removal plus .5cm perimeter of normal skin • Stage I: surgical removal plus margin of normal skin based on thickness of melanoma (1cm per mm of melanoma; stage 1 = 2mm of less • Stage II: wide excision, 2cm perimeter per mm if >2mm; usually lymph biopsy • Stage III: lymph node dissection, wide excision; interferon therapy • Stage IV: metastasis is beyond lymph nodes • Recurrent: risk increases with size of primary melanoma; often second is smaller than 1st; survival varies greatly based on original case, but likelihood less than original “ABCDE” Rule Homeostatic Imbalances – Burns – Initial threat is loss of protein and electrolyte rich body fluids, which may lead to circulation collapse – Bacterial infection is also a significant threat – Rule of Nines to evaluate extent of burn – Classified, in increasing severity, as first-degree, second-degree and third-degree. Third degree requires grafting for recovery Evaluating Burns Developmental Aspects • Epidermis develops from embryonic ectoderm, dermis (and hypodermis) develop from mesoderm. • Fetus exhibits a downy lanugo coat. Fetal sebaceous glands produce vernice caseosa, which helps protects fetal skin from watery environment. • Newborn’s skin is thin. During childhood, skin thickens and more subcutaneous fat is deposited. During puberty, sebaceous glands are activated and terminal hairs appear in greater numbers. • In old age, rate of epidermal declines and skin and hair thin. Skin glands become less active. Loss of collagen, elastin fibers and subcutaneous fat lead to wrinkling. Delayed action genes cause graying and balding. Photodamage is a major cause of skin aging. Functions of the Integumentary System 1. Protection: chemical barrier (antibacterial sebum), physical barrier (hardened keratinized surface), and biological barrier (phagocytes) 2. Temperature regulation: Skin vasculature & sweat glands, regulated by nervous system 3. Cutaneous sensation: sensory receptors respond to temperature, touch, pressure and pain 4. Metabolic functions: Vitamin D synthesized from cholesterol in skin cells 5. Blood reservoir: extensive vascular supply of dermis 6. Excretion: sweat contains small amounts of nitrogen wastes