38721
advertisement

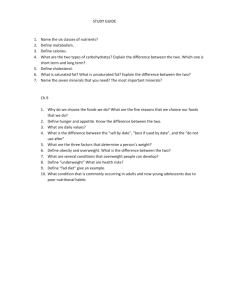
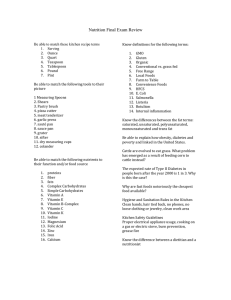
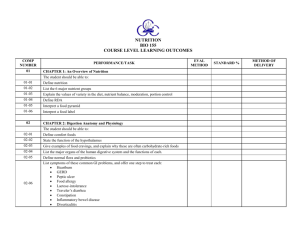
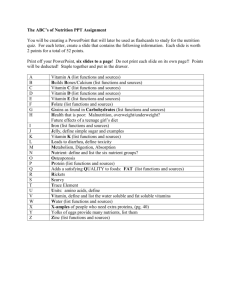
General Nutrition Kathaleen Briggs Early, PhD, RD, CDE Assistant Professor and Registered Dietitian kearly@pnwu.org Learning Objectives o Upon completion of this module, the student will be able to: 1. Define “macronutrients” and identify what the food sources are for the macronutrients 2. Define “micronutrients” and identify what the food sources are for the major micronutrients 3. Identify the components of a healthy diet 4. Identify patients at nutrition risk 5. Identify the causes of malnutrition and those who are malnourished 6. Explain the benefits of breastfeeding during infancy 2 Definitions o A nutrient is any substance in food that the body can use to – obtain energy, – synthesize tissues, or – regulate body processes o Macronutrients – Carbohydrates – Proteins – Lipids o Micronutrients – Vitamins – Minerals o Water 3 Macronutrients: CARBOHYDRATES o Primary source of calories (energy) and glucose (4 kcal/gm) – Glucose is the body’s preferred fuel source – Most people get about half of all their calories from carbohydrates o Food sources – Breads, grains, cereals, rice and pastas are the biggest sources – Dairy/non-dairy alternatives (milk, yogurt, soy and rice milk) – Fruits in any form (fresh, frozen, juice, canned, dehydrated) – Vegetables also have some carbohydrates • Common vegetable-based carbs in Western diet are Peas, Corn and Potatoes – Sweets • Cakes, cookies, ice cream, pastries, etc. o No carbohydrates in meats or cheeses o Carbohydrate-rich foods are also an important source of fiber and antioxidants 4 Macronutrients: FATS o Essential for health – Cellular membrane structure and function – Myelin sheath in nervous system – Fat tissue keeps us warm, provides some protection to our organs o Concentrated source of calories (9 kcal/gm) – Saturated dietary fats • Animal-based – butter, lard, whole and 2% milk, meat, skin • Plant-based – coconut and coconut oil, palm kernel oil, palm oil, cocoa butter 5 Macronutrients: FATS – Unsaturated dietary fat • Monounsaturated fatty acids (MUFA) – Olive and canola oils • Polyunsaturated fatty acids (PUFA) – Corn, safflower, sunflower, fish oils – Trans fats • Very small amount of trans fats are naturally occurring in dairy foods, meat, and darker-meat poultry – Cholesterol from the diet • Only found in animal-based foods • Whole fat dairy products, egg yolks, meat, poultry skin and dark poultry meat 6 Macronutrients: PROTEINS o Primary role is to maintain structural and functional integrity – Muscle tissue, skin, bone, organs, enzymes, hormones, neurotransmitters, fluid and acidbase balance, cellular transport, and blood clotting o Proteins are made up of amino acids o Some amino acids are essential, others are nonessential, and still others are “conditionally” essentially 7 Macronutrients: PROTEINS in Vegetarian Diets o Vegetarian diets can be a very healthy option o Complete vs. Incomplete – Complete proteins contain all 9 essential amino acids (e.g., milk, egg, chicken, meat, fish) – Soy is the only plant-based complete protein – Incomplete proteins are lacking in 1 or more essential amino acids – It is not necessary to combine incomplete proteins at a meal • More important to eat a variety of foods consumed throughout the day to provide the most diverse amino acid and protein sources 8 Micronutrients: Vitamins Water-soluble o Not stored in the body o Deficiencies may develop quickly if inadequate intake occurs – B vitamins • • • • • Folic acid (folate) B12 (cobalamin) Thiamin (B1) Riboflavin (B2) Niacin (B3) Fat-soluble o Stored in liver and fat tissue for long periods of time o Deficiencies develop very slowly – – – – Vitamin A Vitamin D Vitamin E Vitamin K – Vitamin C 9 Micronutrients: Major Minerals and their Common Food Sources o Calcium • dairy products, dark leafy green vegetables, tofu o Phosphorus • Animal proteins, dairy foods, legumes; wide-spread in food supply o Magnesium • Whole grains, “hard” water o Sodium • Processed foods, preserved foods, added salt in cooking and at the table o Potassium • Fruits and vegetables 10 Micronutrients: Trace Minerals and their Common Food Sources o Copper • Liver, shellfish, lentils, mushrooms, cashews, sunflower seeds o Iodine • Iodized salt, seafood o Iron • Most well absorbed: Beef, dark poultry meat, whole eggs, tuna, salmon, legumes, iron fortified cereals, liver • Less well absorbed: prunes, raisins, apricots, dark leafy green vegetables, brown rice o Selenium • Brazil nuts, tuna, beef, brown rice o Zinc • Oysters, meat, poultry, legumes, shellfish, whole grains 11 Micronutrient (vitamin) Deficiency o Pellagra (Niacin deficiency) • The 4 D’s: diarrhea, dermatitis, dementia and death o Pernicious Anemia (B12 deficiency) • Caused from autoimmune destruction for stomach cells needed for intrinsic factor production o Vitamin A deficiency • Leading cause of preventable blindness in children • Increases the risk of disease and death from severe infections 12 Micronutrient (vitamin) Deficiency o Scurvy (vitamin C deficiency) • Collagen breakdown resulting in bleeding gums and petechiae o Rickets and Osteomalacia (vitamin D deficiency) 13 Micronutrient (mineral) Deficiency o Iodine – Regions at greatest risk include countries of the former Soviet Union, south Asia and parts of Africa – Thyroid enlargement (goiter) is an early and visible sign of iodine deficiency o Iron – Iron deficiency anemia – Fatigue, rapid heart rate, and rapid breathing on exertion are the most common signs o Selenium – Kashin disease 14 Dietary History o Questions the nurse can ask the patient directly – Do you eat a wide variety of foods? – Do you have difficulty obtaining adequate food? – Do you have any food allergies/intolerances? – Do you have family? Do you eat alone or with others? o Questions the nurse should consider in their assessment – Is the patient obviously under or overweight? – Does the patient have any obvious warning signs of nutrient deficiencies (see slides 18-27)? 15 Optimizing Nutrition o WHO’s five keys to safer food – Keep clean – Separate raw and cooked – Cook thoroughly – Keep food at safe temperatures – Use safe water and raw materials 16 Assessing Physical Activity o With the world-wide obesity epidemic, addressing physical activity is essential o Use the FITT principle – F: How many times per week does the activity occur? – I: How vigorous is the activity? – T: What is the activity? What is its purpose? – T: How many minutes of the activity are done per session? 17 Anthropometrics o Height • A key indicator of chronic malnutrition is stunted growth o Weight • Recent weight loss is a very sensitive marker of a patient’s nutritional status • Weight loss of more than 5% of usual body weight in 1 month or 10% in 6 months before hospitalization is clinically significant o Weight for height • BMI o Body fat assessment o Activities of Daily Living o Strength – e.g., grip strength 18 Physical Assessment of Nutrition Status o Orbital fat pads • should be present o Triceps skinfold thickness • 1 cm or less = malnourished o Anterior lower ribs • Ribs should not be visible if adequately nourished o Temples • should not be sunken o Clavicle • should not be overtly prominent o Shoulders • Should be rounded or sloped, not squared 19 Physical Assessment of Nutrition Status o Interosseus muscle – Should be bulging when thumb and forefinger pinch together o Scapula – When hand presses against a wall, back should be smooth if adequately nourished o Thigh and Calf – Should be solid – Loose skin upon muscle massage indicates severe deficit 20 Physical Assessment of Nutrition Status o Edema – In ambulatory patients, no impression should remain following pressure application o Ascites – Should not be present in healthy individuals – Degree of fluid accumulation in abdominal cavity can be indicative of nutrition status 21 Malnutrition o When more than 20% of usual body weight is lost, most physiologic body functions become significantly impaired o Malnutrition can also reduce cardiac output, impair wound healing, and depress immune function o Nutritional repletion can often reverse these processes and significantly improve patient outcomes o Difficulty is identifying individuals at risk so that appropriate interventions can be made 22 Protein Energy Malnutrition (PEM) o Most common form of malnutrition o Most often seen in the western hospitalized patient with – – – – – – End-stage liver or renal disease Cancer cachexia HIV/AIDS wasting disease Severe eating disorder Neglect Long-term recovery from multiple trauma o Outside industrialized countries, more often seen in areas of severe drought, infectious disease, and war 23 Kwashiorkor o “Pot Belly” appearance due to hepatic edema and fatty liver o Increased extracellular fluid (edema) and low plasma albumin levels – Increase in extracellular fluid may mask underlying weight loss o Rapid onset; may develop in a few weeks 24 Marasmus o Significant deficit of total body fat and body protein with a slight increase in extracellular water o Obvious body wasting – Skin and bones appearance o Eyes may be sunken o Skull and cheekbones may be prominent o Plasma albumin is often in the low-normal range o Usually takes months or years to develop 25 Comparison of the features of kwashiorkor and marasmus Feature Kwashiorkor Marasmus Growth failure Present Present Wasting Present Present, marked Edema Present (sometimes mild) Absent Hair changes Common Less common Mental changes Very common Uncommon Dermatosis, flaky-paint Common Does not occur Appetite Poor Good Anemia Severe (sometimes) Present, less severe Subcutaneous fat Reduced but present Absent Face May be edematous Drawn in, monkey-like Fatty infiltration of liver Present Absent FAO/WHO 26 Assessing Malnutrition o Temples (temporalis muscles) should be visualized for evidence of wasting o Dull hair, easily plucked = protein energy deficiency o Brittle hair, breaks easily suggests micronutrient deficiencies http://meded.ucsd.edu/clinicalimg/head_temporal_wasting2.htm http://meded.ucsd.edu/clinicalimg/index.htm 27 Causes of Malnutrition o Hunger – Due to poverty and food insecurity o Micronutrient or protein deficiency – More common in elderly o Disease – Infectious disease (e.g., malaria, TB, see next slide) – Chronic disease (e.g., HIV AIDS, cancer, emphysema, etc) 28 29 Defining a Healthy Diet o o o o o o o Aids in maintaining a healthy body weight Promotes general well-being Satisfies hunger and appetite Culturally and age appropriate Suitable to personal preferences Prevents chronic disease Adequate in overall nutrition and balance – High consumption of fruits & vegetables – Low consumption of red meat & fatty foods – Whole and fresh foods are preferred to processed or refined foods – Protein primarily from fish, dairy products, and/or legumes – Limited in added salt, sugar, and alcohol 30 World Health Organization’s Five Keys to a Healthy Diet o Give baby only breast milk for the first six months of life o Eat a variety of foods o Eat plenty of vegetables and fruits o Eat moderate amounts of fat and oils o Eat less salt and sugars 31 Benefits of Breastfeeding For infants o favorable balance of nutrients o improve cognitive development o protects against infections o protect against chronic diseases – Impacts gene expression o protects against food allergies For mothers o contracts the uterus o delays return of regular ovulation (especially in exclusively-breastfeeding moms) o conserves iron stores o protects against breast cancer (especially premenopausal forms) o aids in return of prepregnancy weight 32 Recommendations for Breastfeeding o World Health Organization: – Exclusive breastfeeding for first six months – Introducing age-appropriate and safe complementary foods at six months – Continuing breastfeeding for up to two years or beyond 33 Contact Information Kathaleen Briggs Early, PhD, RD, CDE kearly@pnwu.org 34