Overview of the Health Information Protection Act
advertisement
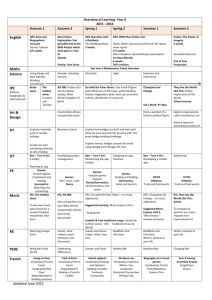
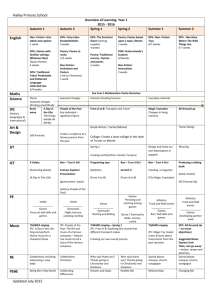
Health Information Protection Act An Overview Ann Cavoukian, Ph.D. Information & Privacy Commissioner/Ontario Ontario Health Records Association www.ipc.on.ca May 7, 2004 Health Privacy is Critical The need for privacy has never been greater: • Extreme sensitivity of personal health information • Patchwork of rules across the health sector; with some areas currently unregulated • Increasing electronic exchanges of health information • Multiple providers involved in health care of an individual – need to integrate services • Development of health networks • Growing emphasis on improved use of technology, including computerized patient records www.ipc.on.ca Slide 2 Unique Characteristics of Personal Health Information Highly sensitive Collected in the context of a publicly-funded health care system Widely shared among a range of health care providers for the benefit of the individual Widely used and disclosed for secondary purposes that are seen to be in the public interest (e.g., research, planning, fraud investigation, quality assurance) www.ipc.on.ca Slide 3 Legislation is Critical The IPC has been calling for legislation to protect health information since its inception in 1987 • Dates back to Justice Krever’s 1980 Report on the Confidentiality of Health Information – The Commission documented many cases of unauthorized access to health files maintained by hospitals and the Ontario Health Insurance Plan – The Report called for comprehensive health privacy legislation at that time www.ipc.on.ca Slide 4 Provincial Health Privacy Laws Alberta • Health Information Act Manitoba • Personal Health Information Act Québec • Act respecting access to documents held by public bodies and the protection of personal information • Act respecting the protection of personal information in the private sector. Saskatchewan • Health Information Protection Act www.ipc.on.ca Slide 5 Ontario Bills of the Past Numerous attempts made over the years to get a bill introduced and passed, but have never succeeded • Bill 159 – Personal Health Information Privacy Act, 2000 • Privacy of Personal Information, 2002 www.ipc.on.ca Slide 6 PHIPA – Bill 159 On December 7, 2000, the government introduced Bill 159 Concerns about the Bill: • Directed Disclosures • Extensive use of Regulations • Lack of full investigation powers www.ipc.on.ca Slide 7 Privacy of Personal Information Act Ontario issued a draft bill in 2002 that applied to all non-public sector organizations Created special rules for health sector MCBS consulted with stakeholders to refine aspects of the draft bill Unfortunately this draft bill was never introduced www.ipc.on.ca Slide 8 If No Provincial Health Legislation? If Ontario fails to enact its own legislation, PIPEDA takes effect: • Only commercial entities covered - ambiguity about who is in and who is out • Not tailored to meet the needs of the health sector • Principle-based approach rather than specifics could result in inconsistent implementation • Oversight left to the federal Privacy Commissioner www.ipc.on.ca Slide 9 Ontario’s Health Information Protection Act, 2003 (HIPA) Ontario government introduced health privacy bill (Bill 31) on December 17, 2003 Referred to the Standing Committee on General Government, which held public hearings and clause-by-clause study Received Second Reading on April 8, 2004 Expected to come into effect January 1, 2005 www.ipc.on.ca Slide 10 Bill 31 – Two parts Schedule A – the Personal Health Information Protection Act (PHIPA) Schedule B – the Quality of Care Information Protection Act (QOCIPA) www.ipc.on.ca Slide 11 Bill 31 – Based on Fair Information Practices Accountability Identifying Purposes Consent Limiting Collection Limiting Use, Disclosure, Retention Accuracy www.ipc.on.ca Safeguards Openness Individual Access Challenging Compliance Slide 12 Scope of PHIPA Health information custodians (HICs) that collect, use and disclose personal health information (PHI) Non-health information custodians where they receive personal health information from a health information custodian (use and disclosure provisions) www.ipc.on.ca Slide 13 Health Information Custodians Definition includes: • • • • • • • Health care practitioners Hospitals and independent health facilities Homes for the aged and nursing homes Pharmacies Laboratories Homes for special care A centre, program or service for community health or mental health www.ipc.on.ca Slide 14 PHIPA Practices Must take reasonable steps to ensure accuracy Must maintain the security of PHI in its custody or control Must have a contact person to ensure compliance with Act, respond to access requests, inquiries and complaints from public Must have information practices in place that comply with the Act Must make available a written statement Must be responsible for actions of agents www.ipc.on.ca Slide 15 PHIPA Consent Consent is required for the collection, use, disclosure of PHI subject to specific exceptions Consent must be a consent of the individual be knowledgeable relate to the information not be obtained through deception or coercion Consent may be express or implied www.ipc.on.ca Slide 16 Collection, Use and Disclosure Without Consent Derogations from the consent principle are allowed in limited circumstances. As required by law To protect the health or safety of the individual or others To identify a deceased person or provide reasonable notice of a person’s death www.ipc.on.ca Slide 17 Patient Access to Records PHIPA Expands and Codifies the Common-Law Right of Access Right of access to all records of personal health information about the individual in the custody or control of any health information custodians Provides right to correct their records of personal health information. Recognizes special factors surrounding health information by allowing for incorrect information to be struck out without obliterating the original record. www.ipc.on.ca Slide 18 Oversight and Enforcement Office of the Information and Privacy Commissioner is the oversight body IPC may appoint an Assistant Commissioner for Personal Health Information IPC may investigate where: A complaint has been received Commissioner has reasonable grounds to believe that a person has contravened or is about to contravene the Act IPC has powers to enter and inspect premises, require access to PHI and compel testimony www.ipc.on.ca Slide 19 Strengths of PHIPA Creation of health data institute to address criticism of “directed disclosures Open regulation-making process to bring public scrutiny to future regulations Implied consent for sharing of personal health information within circle of care Adequate powers of investigation to ensure that complaints are properly reviewed www.ipc.on.ca Slide 20 Role of the IPC IPC currently has oversight of two laws Provincial Freedom of Information and Protection of Privacy Act Municipal Freedom of Information and Protection of Privacy Act IPC may issue orders for access/correction appeals IPC investigates privacy complaints and may issue report with recommendations but not orders www.ipc.on.ca Slide 21 Access and Correction Appeals Appeals under current public sector laws may be dealt with through three stages: IPC will examine situation and may contact individual or organization for more information (Intake) If not dismissed, the appeal proceeds to mediation, the IPC’s preferred method of dispute resolution If mediation is unsuccessful, appeal proceeds to adjudication and an order will be issued. www.ipc.on.ca Slide 22 Privacy Complaints IPC goal in dealing with complaints under public sector legislation is to assist organizations in taking whatever steps are necessary to prevent future occurrences Intake staff attempt to resolve complaints informally, through liaising with organization and complainant If not resolved, complaint goes to the investigation stage and a mediator investigates Mediator prepare a report, including recommendations www.ipc.on.ca Slide 23 Role of IPC under PHIPA Use of mediation and alternative dispute resolution to be stressed Order-making power as a last resort Conducting public and stakeholder education programs Comment on an organization’s information practices www.ipc.on.ca Slide 24 Stressing the 3 C’s Consultation • Opening lines of communication with health community Collaboration • Working together to find solutions Co-operation • Rather than confrontation in resolving complaints www.ipc.on.ca Slide 25 Making Health Privacy Work Think beyond compliance with legislation Use technology to help protect personal health information: • Build privacy right into design specifications • Minimize collection and routine use of personally identifiable information – use aggregate or coded information if possible • Use encryption where practicable • Think about using pseudonymity, coded data • Conduct privacy impact assessments www.ipc.on.ca Slide 26 Lessons from Chatham-Kent Use of encryption to secure databases Investigate privacy-enhancing technologies to shield personal health information from systems administrators Conduct an end-to-end privacy impact assessment (PIA) Conduct independent security audits Privacy Review: Chatham-Kent IT Transition Pilot Project • www.ipc.on.ca/english/pubpres/reports/042202.pdf www.ipc.on.ca Slide 27 Lessons From UHN Privacy Assessment Strong Privacy Policy Real Consequences for Breaches Ongoing Privacy Training • Incorporate privacy training into undergraduate curriculum for medical students Independent Security and Privacy Audits www.ipc.on.ca/english/pubpres/reports/073002.pdf www.ipc.on.ca Slide 28 How to Contact Us Commissioner Ann Cavoukian Information & Privacy Commissioner/Ontario 80 Bloor Street West, Suite 1700 Toronto, Ontario M5S 2V1 www.ipc.on.ca Phone: Web: E-mail: (416) 326-3333 www.ipc.on.ca commissioner@ipc.on.ca Alternatives to Investigation Prior to investigating a complaint, the Commissioner may: Inquire as to other means used by individual to resolve complaint Require the individual to explore a settlement Authorize a mediator to review the complaint and try to settle the issue www.ipc.on.ca Slide 30 Decision Not to Investigate Commissioner may decide not to investigate a complaint where: An adequate response has been provided to the complainant Complaint could have been dealt with through another procedure Complainant does not have sufficient personal interest in issue Complaint is frivolous, vexatious or made in bad faith www.ipc.on.ca Slide 31 Powers of the Commissioner After conducting an investigation, the Commissioner may issue an order To provide access to, or correction of, personal health information To cease collecting, using or disclosing personal health information in contravention of the Act To dispose of records collected in contravention of the Act To change, cease or implement an information practice Orders, other than for access or correction, may be appealed on questions of law www.ipc.on.ca Slide 32 Offences and Penalties Creates offences for contravention of the legislation, including: wilfully collecting, using or disclosing PHI in contravention of the Act; once access request made, disposing of a record of personal information in an attempt to evade the request wilfully failing to comply with an order made by the IPC Maximum penalty of $50,000 for an individual and $250,000 for a corporation www.ipc.on.ca Slide 33 Action for Damages An individual affected by an IPC order may bring an action for damages for actual harm suffered Where the harm suffered was caused by a willful or reckless breach, the compensation may include an award not exceeding $10,000 for mental anguish No action for damages may be instituted against a HIC for anything done in good faith or any alleged neglect or default that was reasonable in the circumstances www.ipc.on.ca Slide 34