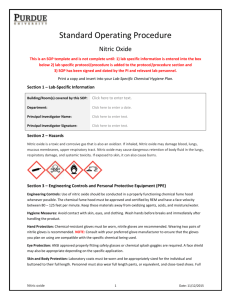
Infection control practices in Respiratory therapy
advertisement
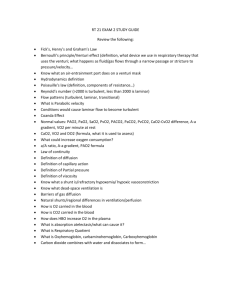
HELIOX AND INHALED NITRIC OXIDEIS IT USEFUL? DR.NANDAKUMAR.V.,M.D.,I.D.C.C.M.,E.D.I.C KMCH Heliox- helium + oxygen • 1 st clinical use – Charles Look 1923 for decompression sickness • 1934 – Barach – grandfather of heliox therapy • Inert/ Non toxic/tasteless/non- flammable gas. • Non carcinogenic, no lasting effect on human organ • Lower in density than in Nitrogen/ O2 Physical properties Composition Density (p) kg/m 3 Viscosity (ή) microPoise Thermal conductivity W/m K Air 1.184 184.33 0.025 CO2 1.81 148.71 0.017 Helium 0.166 197.61 0.14 Nitrogen 1.167 177.82 0.026 oxygen 1.33 205.35 0.026 Physiological issue • To improve ventilation ↑ compliances Resistances airway or Both • Bronchodilator and Steroids used to increase Airway caliber. Heliox = Helium+ Oxygen • No broncho dilating or anti inflammatory properties. • Airway resistance in turbulent flow is directly related to density of gas • Heliox -low density than N2 or O2– lower airway resistances • Low density exert important potential benefits with regards to airway’s dynamic of fluids. Heliox = Helium + Oxygen • Reduces resistances by reducing REYNOLDS number, • the density of mixture is an important determinent of Reynold’s number TURBULENT FLOW LAMINAR FLOW. • Reduces work of breathing and improves Gas exchanges Reynolds Number Reynolds number is a dimensionless number that can used to predict conditions of laminar or turbulences flow depending on the situation Re = pdv ή p=density of gas (kg/L) d= diameter of tube(m) v=linear velocity(m/s) ή= gas viscosity(kg/m/s) Reynolds Number • Re < 2000 - Laminar flow • Re 2000-4000 - Transition flow • Re > 4000 - Turbulent flow Normal physiology: Upper airway & proximal trachea- TURBULENT FLOW Asthma and COPD : Turbulent flow observed more distally. Laminar and Turbulent flow Different type of flow Laminar flow- flow characterized by smooth, parallel layer of fluid Turbulent flow – flow characterized by mixing of adjacent fluid layer Medical Application Upper airway Lower airway Infection Asthma, COPD, Bronchiectasis Bronchiolitis Lung cancer HFOV – croup, epiglottitis, laryngitis, tracheitis. Trauma and Mass effect – foreign body aspiration, post extubation stridor, Tumour. Other – Tracheomalacia, Tracheal stenosis Medical applications • Others Assessment of FRC IABP Operation and Cooling of MRI scanner • Treatment for Decompression sickness Pneumatosis cystoides Hyperammonaemia NEBULIZED DRUG DELIVERY • • Nebulized drug delivery improve gas exchange . Air /O2 vs He-O2 nebulized albuterol in acute severe asthma NO shorten hospital stay NO clinical improvement. (Respiratory care 2013) • In COPD acute exacerbation- (FEF25-75) and (FEV1)– no improvement in FEV1, faster improvementin FEF25-75 (Critical care med 2000) HELIOX DELIVERY Upper airway obstruction B/L Vocal cord palsy, post extubation stridor-compared Heliox vs Adrenaline neb. (PEDIATRICS2001) Asthma Metaanalysis USEFULLNESS IN MORE SEVERE PATIENTS Risk of intubation, while awaiting the effects of standard therapy. (database systemic review 2006) Level of evidences is low. COPD • Multicenter, randomized trial on NIV with heliox mixture vs standard therapy in COPD exacerbation. (critical care 2010 Jan; maggiore SM,) • Complication of NIV and MV, – ET intubation, – Icu and hospital discharge, – 28 days mortality, – Serious adverse effect were recorded– didn’t show any statistical superiority Problem in using • Difficult to obtain • Real benefit - ↓ density, Fio2 < 40% • Thermal conductivity – Heated humdifier • Different function of the valve within the ventilator that controls flow • Expensive Clinically not applicable • Turbulent flow- depends on density of the solution. • Laminar flow- depends on viscosity. • In distal airways laminar flow is maintained in COPD & Asthma due to large cross sectional area. • Poisueille’s law: R = ( 8.1.ń/π.r⁴) Nitric oxide Pathophysiology of ARDS Insult Activation of inflammatory mediators and cellular components Cytokines ( TNF, IL-1, IL-6, IL-8) Neutrophilic infiltartion Damage to capillary endothelial and alveolar epithelial cells Pathophysiology of ARDS • Starling forces fall out of balance - ↑ in capillary hydrostatic pressure ↑ pulmonary capillary - ↓ oncotic pressure gradient. permeability • Exudative fluid in interstitium and alveoli - Impaired gas exchange --- ventilation- perfusion mismatch - Physiological shunting, decreased compliance - Increased pulmonary arterial pressure - Type 2 pneumocyte damage, - Atelectasis • Nitric oxide was formerly known as endothelium-derived relaxing factor (EDRF). • It is one of the nitrogen oxides ("NOx") • Synthesized within cells by an enzyme NO synthase (NOS). • This enzyme catalyses the oxidation of Larginine to L-citrulline, producing NO. METABOLISM NOS is present in two forms • The constitutive form (eNOS) Present in vascular, neuronal, cardiac tissue, skeletal muscle and platelets, producing small quantities of NO continuously. Here NOS is Ca2+/calmodulin dependant-stimulated by cGMP. • The inducible form (iNOS) Present in endothelium, myocytes, macrophages and neutrophils, which produces relatively large quatities of NO after exposure to endotoxins in sepsis. Following induction high levels of NO produced may form cytotoxic radicals and cause capillary leakage. Goal of Inhaled NO • Improve oxygenation • Decrease PVR • Decrease pulmonary edema • Reduction or Prevention of inflammation • Cytoprotection • Protection against infection Respiratory • Basal vasodilatation in pulmonary vessels - reverses hypoxia. • Nitric oxide inhibits – hypoxic pulmonary vasoconstriction – increases blood flow through well ventilated areas of the lung • Improves V/Q relationships. Effect of PO2 in ARDS Benefit of inhaled NO Effect of inhaled NO vs NTP Mechanism of action Inhaled vasodilators • In ARDS • Inhaled vasodilators (green circles) preferentially dilate the pulmonary vessels that perfuse functioning alveoli (white circles), recruiting blood flow away from poorly ventilated units (black circles). • The net effect is improved ventilation/perfusion matching. Basic Concept in using NO • Pulmonary hypertension - one of the hallmark of ARDS • Severe hypoxemia caused by physiologic shunting and V/Q mismatching. • Inhaled vasodilators selectively dilate vessels that has perfuse well ventilated lung zones resulting in – improved V/Q matching – ↓shunting Improves oxygenation Dosing Inhaled NO is typically administered at a dose between 1.25 and 40 parts per million (ppm). • Continuous inhaled NO might become sensitized -Lowerdoses improve oxygenation -Continued higher doses have little or no effect. • When used continuously and weaned, it causes – worsened oxygenation – increased pulmonary artery pressure DELIVERY OF NO IN MV Monitoring Chemiluminescence and electrochemical analysers should be used and are accurate to 1 ppm. Storage • NO is stored in aluminium or stainless steel cylinders which are typically 40 liters. • These contain 100/1000/2000 p.p.m. nitric oxide in nitrogen. • Pure NO is corrosive and toxic. Administration • The drug is injected via the inspiratory circuit of a ventilator. • The delivery system is designed to minimize the oxidation of nitric oxide to nitrogen dioxide. Other Organ Effects-Cardiovascular • • Nitric oxide is a potent vasodilator. Shear stresses in vessels increase NO production and may account for flow dependant vasodilatation. • Endothelial NO inhibits platelet aggregation. • In septic shock the overproduction of NO results in hypotension and capillary leak. • NOS inhibitors have been investigated experimentally in the treatment of sepsis. OTHER ORGAN EFFECTS • GIT – determinant of gastro intestinal motility appears to modulate morphine – induced constipation • GENITOURINARY – play sodium homeostasis in kidney • IMMUNE – macrophage and neutrophils synthesize NO which can be toxic to certain pathogens and may be important in host defence mechanisms Potential harms • Inhaled NO may produce toxic radicals. • However, it is unknown whether the toxic radicals are more harmful than ongoing exposure to high fractions of inspired oxygen. Side effects • Methemoglobin and NO2 concentrations may increase when high doses of NO are given(500-2000 ppm of NO). • Concentration of both should be monitored frequently. Metabolism • Nitric oxide combines with hemoglobin that is 60% to 100% oxygenated. • Nitric oxide combines with oxyhemoglobin to produce methemoglobin and nitrate. • Within the pulmonary system, nitric oxide can combine with oxygen and water to produce nitrogen dioxide and nitrite respectively, which interact with oxyhemoglobin to then produce methemoglobin and nitrate. • At 80 ppm the methemoglobin percent is ~5% after 8 hours of administration. • Methemoglobin levels >7% were attained only in patients receiving 80 ppm. Side effects • Inhaled NO is associated with renal dysfunction. • Inhaled NO has immunosuppressant properties that, in theory, could increase the risk of nosocomial infection. • NO can cause DNA strand breaks and base alterations, which are potentially mutagenic. Other uses • Licensed – persistent Pul.Hypertension • RV failure • Post cardiac surgery • Orthotopic heart and lung transplant • Ventricular assist device • Ischemic- reperfusion injury- no role Thank you!