Myelomeningocele: Prenatal and Postnatal Treatment and
advertisement
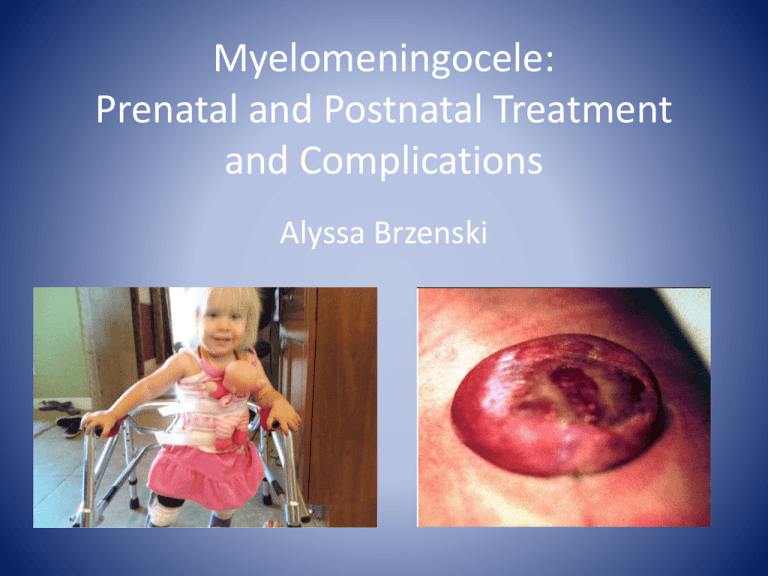
Myelomeningocele: Prenatal and Postnatal Treatment and Complications Alyssa Brzenski Case • A 25 year old G1P0 at 18 weeks gestation, with no previous past medical history, was found during routine screening to have a fetus with T12-S1 myelomeningocele(MMC). The fetus, during a detailed prenatal ultrasound, is found to have Arnold-Chiari malformation but no other congenital abnormalities. What is Spina Bifida? Varying Neural Tube Defects Spina Bifida Basics of MMC • 3.4:10,000 births • Related to low folate levels, anticonvulsants (carbamazepine, valproic acid) • Previous child with same partner is a risk factor Co-morbidities • Sensory motor deficits • Bowel and Bladder Incontinence • Arnold Chiari Type II – Caudal displacement of cerebellar vermis, fourth ventricle, and lower brainstem • Hydrocephalus • Cognitive delay – Lower risk if no VP Shunt needed Co-morbidities Latex Allergies • All patients with MMC are labeled as latex allergic • High rates due to recurrent procedures including urinary catheterization • Cross reaction to avocados, banana, passion fruit, kiwi, banana Management of Myelomeningocele Study • What treatment would you recommend? • How would you anesthetize the mother and fetus for the fetal surgery? • What precautions would you take for a postnatal repair? Anesthetic plan? Mid-gestational Open Fetal Procedures • Significant risk to Mom– Hemorrhage (13% required transfusion) – Infection (9% developed chorioamnionitis) – Pulmonary Edema (28%) – Premature delivery – Uterine Rupture • No direct benefit to Mom Maternal Physiology • Physiology of Pregnancy – Airway/Pulm • Smaller swollen airway • Decreased FRC, Increased Oxygen Consumption • Respiratory Alkalosis – Cardiac • Decreased SVR • Increased CO • Left Uterine Displacement – GI • Full Stomach – MAC • Decreased anesthetic requirements Fetal Physiology • Cardiac– Fetus heart rate dependent – Slowing during the procedure detrimental • Heme– Fetal Blood Volume= 120-160 mL/kg – Hgb = 11.5-12.5 g/dL – Fetal synthesis of clotting factors decreased • Oxygen Delivery – Dependent on placental perfusion • Thermoregulation – Fetus unable to maintain temperature – Must warm any fluid administered to mom and amniotic fluid replacement Mid-gestation Fetal Surgery • Epidural for Mom- post-op pain control • GA for MOM during the procedure with maintence of Uterine-placental perfusion • Must have profound uterine relaxation- Can use high inspired volatile (2MAC) +/- nitroprusside • Fetus paralyzed and monitored during surgery • Minimize fluid administration to avoid pulm edema • Mom must receive tocolysis prior to awakening and will be monitored for pre-term labor Post-natal MMC Repair • Infants repaired early after birth • Must be cautious to not injury the neural tissue during moving or intubation • Routine ASA monitors • Prone position for repair • May or may not receive VP Shunt at the same time • Typically remain intubated as infant should not lie supine for the first day VP Shunts have Complications Sources • • • Adzick S et al. A Randomized Trial of Prenatal vs Postnatal Repair of Myelomeningocele. New England Journal of Medicine 2011; 364: 993-1004. Golombeck K et al. Maternal morbidity after maternal-fetal surgery. AM J Obstet Gynecol 2006; 194: 834-9. Ferschl M et al. Anesthesia for In-utero repair of myelomeningocele. Anesthesiology 2013; 118: 1211-23.