Presentation - Self
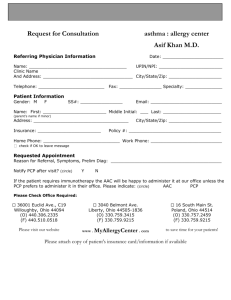
advertisement
IMPACT - Connecting Nursing Facilities and Home Care to the Healthcare System of the Future Massachusetts Care Transitions Forum September 28th, 2012 Drs. Terry O’Malley & Larry Garber Agenda IMPACT – addressing Long Term and PostAcute Care (LTPAC) needs ONC’s S&I Framework - Developing national standards for transitions of care datasets LAND & SEE – software to facilitate integrating LTPAC into electronic health information exchanges (HIE) 2 IMPACT Grant February 2011 – HHS/ONC awarded $1.7M HIE Challenge Grant to state of Massachusetts (MTC/MeHI): Improving Massachusetts Post-Acute Care Transfers (IMPACT) 3 IMPACT Objectives & Strategies • Facilitate developing a national standard of data elements for transitions across the continuum of care • Develop software tools to acquire/view/edit/send these data elements (LAND & SEE) • Integrate and validate tools into Worcester County using Learning Collaborative methodology • Measure outcomes 4 IMPACT Core Project Team • Madeleine Biondolillo, MD - Massachusetts DPH • Amy Boutwell, MD, MPP - Collaborative Healthcare Strategies • Jim Brennan - Massachusetts e-Health Institute • Larry Garber, MD - Reliant Medical Group/SAFEHealth • Paula Griswold, MS - MA Coalition for the Prevention of Medical Errors • Peggy Preusse, RN - Reliant Medical Group/SAFEHealth • Susan Sama, PhD - Reliant Medical Group • Terry O'Malley, MD - Partners HealthCare System • Craig Schneider, PhD - Massachusetts Health Data Consortium • Laurance Stuntz - Massachusetts e-Health Institute • Michele Visconti - Massachusetts DPH 5 IMPACT Advisory Committee • • • • • • • • • • • • • • Leon Barzin - Massachusetts Medical Society Kate Bones - MA Care Transitions Forum Ray Campbell, JD, MPA – Mass. Health Data Consortium Donna Curran - MassPRO James Fuccione - Home Care Alliance of Massachusetts Ellen Hafer, MTS, MBA - Massachusetts League of Community Health Centers Laurie Herndon, MSN, GNP-BC, ANP-BC – Massachusetts Senior Care Association Pat Kelleher - Home Care Alliance of Massachusetts Amy MacNulty, MBA - Community Care Linkages Constance Nichols, MD, MS, FACEP - Massachusetts Emergency Medical Services Pat Noga, PhD, MBA, RN, NEA-BC - Massachusetts Hospital Association John Straus, MD - Mass. Behavioral Health Partnership Laurance Stuntz - Massachusetts e-Health Institute Deborah Wachenheim - Health Care For All 6 Pilot Site Selection Process • 9/2011 – Applications sent to 34 organizations • Selection Criteria: – High volume of patient transfers with other pilot sites – Experience with Transitions of Care tools/initiatives • 16 Winning Pilot Sites: – St Vincent Hospital and UMass Memorial Healthcare – Reliant Medical Group (formerly known as Fallon Clinic) and Family Health Center of Worcester (FQHC) – 2 Home Health agencies (VNA Care Network & Overlook VNA) – 1 Long Term Acute Care Hospital (Kindred Parkview) – 1 Inpatient Rehab Facility (Fairlawn) – 8 Skilled Nursing and Extended Care Facilities 7 IMPACT Pilot Nursing Facilities • Beaumont Rehab & Skilled Nursing Center - Westborough • Christopher House of Worcester • Holy Trinity Nursing and Rehab Center • Jewish Healthcare Center • Life Care Center of Auburn • Millbury Healthcare Center • Notre Dame Long Term Care Center • Radius Healthcare Center - Worcester 8 Developing National Standards to Support LTPAC Needs 9 The “Data Set” Challenge • Multiple customers: – MA UTF – IMPACT Project Requirements – State and National stakeholders • Multiple needs – The Commonwealth – IMPACT participants – Various State and National groups – Consolidate requirements to facilitate standardization through ONC and on to HL7 and then to MU3 Stakeholders/Contributors • State – – – – – UTF work group IMPACT learning collaborative participants MCPME MA Wound Care Committee Home Care Alliance of MA (HCA) • National – – – – – – Substance Abuse, Mental Health Services Agency (SAMSA) Administration for Community Living (ACL) Aging Disability Resource Centers (ADRC) National Council for Community Behavioral Healthcare National Association for Homecare and Hospice (NAHC) Longitudinal Coordination of Care Work Group- ONC Consequences • 200 element UTF • 325 element IMPACT • 450+ LTPAC / LCC elements • +? MA DPH Universal Transfer Form • Started with DPH’s 3-pg Discharge Form • Sought input from LTPAC “receivers” • Reviewed existing forms and datasets: – MDS – OASIS – IRF-PAI – INTERACT • Sought expert opinions • Resulted in 7-page UTF 13 11x11 Sender (left column) to Receiver (top) Transitions to (Receivers) In Patient ED Out patient Transitions From (Senders) Services In patient ED Out patient services LTAC IRF SNF/ECF HHA Hospice Ambulatory Care (PCP) CBOs Patient/Family 14 14 LTAC IRF SNF/ECF HHA Hospice Amb Care (PCP) CBOs Patient/ Family Prioritize Transitions by Volume, Clinical Instability and Time-Value of Information Transitions to (Receivers) In Patient ED Out patient Transitions From (Senders) Services In patient ED Out patient services LTAC IRF SNF/ECF HHA Hospice Ambulatory Care (PCP) CBOs V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=M CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = M TV = H V=H CI = M TV = H IRF SNF/ECF HHA Hospice V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = M TV = H V=M CI = M TV = H V=H CI = M TV = H V=H CI = H TV = H V=H CI = M TV = H V=H CI = M TV = H V=H CI = L TV = H V=L CI = M TV = M V=H CI = M TV = H V=H CI = M TV = H V=H CI = M TV = H V=H CI = M TV = H V=H CI = L TV = H V=H CI = M TV = H V=L CI = L TV = L V=L CI = L TV = M V=M CI = M TV = M V=H CI = L TV = H V=M CI = M TV = H V=L CI = L TV = H V=M CI = M TV = H V=L CI = M TV = H V=M CI = M TV = M V=M CI = L TV = L V=L CI = L TV = M V=L CI = L TV = H V=L CI = H TV = H V=M CI = H TV = M V=L CI = M TV = M V=M CI = M TV = M V=L CI = M TV = H Black circles = highest priority Green circles = high priority Patient/Family 15 V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=H CI = H TV = H V=L CI = H TV = H V=M CI = H TV = H LTAC 15 Amb Care (PCP) V=H CI = M TV = H V=H CI = L TV = H V=H CI = L TV = H V=H CI = M TV = H V=H CI = L TV = H V=H CI = L TV = M V=H CI = L TV = L V=L CI = M TV = L V=L CI = L TV = M CBOs V=H CI = L TV = H V=M CI = L TV = H V=H CI = M TV = H V=H CI = L TV = H V=H CI = M TV = H V=H CI = L TV = L V=M CI = L TV = L V=M CI = L TV = M Patient/ Family V=H CI = M TV = H V=H CI = M TV = H V=H CI = L TV = L V=H CI = M TV = H V=H CI = L TV = H V=H CI = L TV = H V=H CI = L TV = L V=L CI = M TV = M V=L CI = L TV = L UTF Data Element Survey • 46 Organizations completing evaluation • ~300 Data elements evaluated • 1135 Transition surveys completed 16 12 User Roles 17 Findings from UTF Survey • Largest survey of Receivers’ needs • Identified for each transitions which data elements are required, optional, or not needed • Each of the ~300 data elements is valuable to at least one type of Receiver • Many data elements are not valuable in certain care transition • Paper form can’t represent these needs 18 Five Transition Datasets 1. Report from Outpatient testing, treatment, or procedure 2. Referral to Outpatient testing, treatment, or procedure 3. Shared Care Encounter Summary (Office Visit, Consultation Summary, Return from the ED to the referring facility) 4. Consultation Request Clinical Summary (Referral to a consultant or the ED) 5. Permanent or long-term Transfer of Care to a different facility or care team or Home Health Agency 19 Five Transition Datasets Type 3 Dataset: • Office Visit to PHR • Consultant to PCP • ED to PCP, SNF, etc… Type 4 Dataset: • PCP to Consultant • PCP, SNF, etc… to ED Type 5 Dataset: • Hospital to SNF, PCP, HHA, etc… • SNF, PCP, etc… to HHA • PCP to new PCP 20 5 Transition Datasets Transitions to (Receivers) In Patient ED Out patient Transitions From (Senders) Services LTAC IRF SNF/ECF HHA Hospice Amb Care (PCP) 5 3 In patient ED 1 Out patient services 5 LTAC IRF 5 SNF?ECF HHA Hospice Ambulatory Care (PCP) CBOs Patient/Family 21 5 4 2 CBOs Patient/ Family IMPACT Learning Collaborative: Testing the Care Transitions Datasets 16 organization, 40 participants, 6 meetings over 2 months, and several hundred patient transfers… 22 Learning Collaborative Surveys • Surveys directly on envelopes carrying IMPACT packet, filled out by sender as well as receiver. • Online survey at completion of pilot 23 Analyzing data elements helped 24 Senders found the data 25 Receivers got most of their needs 26 Home Care needed even more! 27 Comment from Pilot Site Survey “While we knew what ED's and hospitals required, we didn't realize Home Health Agencies needed much more than what we typically sent.” -Skilled Nursing Facility 28 New World of Standards Development National Coordinator for Health IT (ONC) Office of the Deputy National Coordinator for Programs & Policy Office of the Deputy National Coordinator for Operations Office of Policy & Planning HIT Policy Committee Defines “Meaningful Use” of EHRs Office of Science & Technology (formerly known as the Office of Standards and Interoperability (S&I)) S&I Framework convenes public and private experts, and proposes HIT/HIE standards Office of Provider Adoption Support Office of State & Community Programs 29 Office of the Chief Privacy Officer IMPACT Office of Economic Analysis & Modeling HL7 ballots standards Office of the Chief Scientist Secretary of HHS makes standards part of “Meaningful Use” and EHR Certification S&I’s Longitudinal Coordination of Care WG Longitudinal Coordination of Care Workgroup LTPAC Care Transition SubWorkgroup Patient Assessment Summary SubWorkgroup • Identifying the key business and technical challenges that inhibit long-term care data exchanges • Establishing the standards for the exchange of Patient Assessment Summary (PAS) documents • Defining data elements for LTPAC information exchange using a single standard for LTPAC transfer summaries • Providing consultation to transformation tool being developed by Geisinger to transform the noninteroperable MDSv3 and OASIS-C into an interoperable clinical document (CCD+) 30 • Providing subject matter expertise and coordination of SWGs • Developing systems view to identify interoperability gaps and prioritize activities Longitudinal Care Plan SubWorkgroup • Near-Term: Developing an implementation guide to standardize the exchange of the Home Health Plan of Care (former CMS 485 form) • Long-Term: Identify and develop key functional requirements and data sets that would support a longitudinal care plan Expanded Transfer of Care Dataset • Includes Collaborative Care Plan data elements • Transfer of Care Dataset: ~450 Data Elements • Timeline for standards development: October 2012 November 2012 December 2012 March 2013 May 2013 MA HIway go-live in 10 large sites with CCD Preliminary Implementation Guide completed Pilot full Transfer of Care Dataset in 16 facilities Finish Implementation Guide in S&I Framework HL7 Balloting of Implementation Guide for inclusion in Consolidated CDA 31 Getting Connected: LAND & SEE 32 LAND & SEE • Non-EHR users complete all of the data fields and routing using a web browser to access their “Surrogate EHR Environment” (SEE) • Sites with EHR or electronic assessment tool use these applications to enter data elements – LAND (“Local” Adaptor for Network Distribution) acts as a data courier to gather and securely transfer data if no support for Direct SMTP/SMIME or IHE XDR 33 LTPAC Communication Today – Paper! Home Health Non-standard EHR OASIS PCP Hospital Billing Program MDS Nursing Facility 34 LTPAC Communication with LAND & SEE LAND & SEE fill in gaps Home Health SEE Non-standard EHR OASIS CCD+ OASIS LAND CCD+ Hospital SEE CCD+ MDS Nursing Facility 35 LAND Billing Program MDS CCD+ PCP The Future with LTPAC EHR Standards Home Health EHR OASIS CCD+ CCD+ CCD+ Hospital EHR MDS CCD+ Nursing Facility 36 PCP Next Steps for Pilot Sites Update gap analysis using expanded dataset Catalog which data elements are captured (and by whom using what vocabulary) electronically, on paper, or not at all with current standard process Of those captured electronically (including CCD, MDS & OASIS), identify process (technology & workflow) to make these available to LAND (for Phase 2). Identify workflow to review new documents in SEE Notification by email or text message, and to whom? View online vs. print? Who does it and where? Can any of the data elements received be electronically filed discretely for re-use using LAND? Identify workflow to update and send SEE document with current info when discharging to Home Health or ED transfer How can standard and non-standard data elements be collected and added online using SEE to the documents being sent? How will copies be printed for patient and ambulance? Additional computers, printers, or chairs required? IMPACT Timeline for Next Steps Dates 9/2012 – 12/2012 Activity Integrate pilot sites into state HIE using LAND & SEE 12/2012 – 1/2013 Pilot site Go-lives with state HIE using LAND & SEE (Phase 1) 3/2013 – 4/2013 Upgrade SEE to handle multiple CDA reconciliation (Phase 2) 6/2012 – 5/2013 Ballot updated datasets in S&I Framework and HL7 1/2013 – 9/2013 Evaluate hospital (re)admissions & total cost of care 38 Questions? TOMalley@Partners.org Lawrence.Garber@ReliantMedicalGroup.org