Active and Retired Non-Medicare Glossary

GLOSSARY OF HEALTH COVERAGE AND MEDICAL TERMS FOR
C&O EMPLOYEES HOSPITAL ASSOCIATION ACTIVE/RETIRED NON-MEDICARE PLANS
This glossary has many commonly used terms, but isn’t a full list. These Glossary terms and definitions are intended to be educational and may be different from the terms and definitions in your plan. Some of these terms also might not have exactly the same meaning when used in your policy or plan, and in any such case, the policy or plan governs. (See your C&O Employees’ Hospital Association Active/Retired Rules &
Regulations Handbook.)
Bold text indicates a term defined in this Glossary.
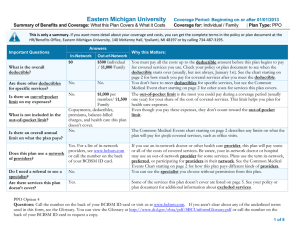
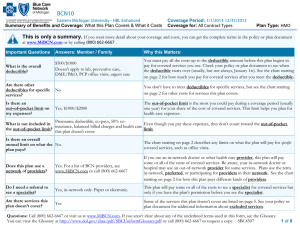
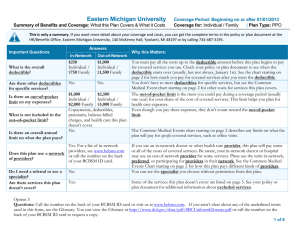
Allowed Amount
Maximum amount on which payment is based for covered health care services. This may be called “eligible expense,” “payment allowance” or “negotiated rate.” If your provider charges more than the allowed amount, you may have to pay the difference under your out-of-network benefits. (See Balance Billing.)
Appeal
A request for your health insurer or plan to review a decision or a grievance again.
Balance Billing
When a provider bills you for the difference between the provider’s charge and the allowed amount. For example, if the provider’s charge is $100 and the allowed amount is $70, the provider may bill you for the remaining $30 under your out-of network benefits.
Co-insurance
Your share of the costs of a covered health care service. You pay the co-insurance and/or any deductibles applicable to your plan of coverage.
Complications of Pregnancy
Conditions due to pregnancy, labor and delivery that require medical care to prevent serious harm to the health of the mother or the fetus, both inpatient and outpatient.
Co-payment
A fixed amount you pay for a covered health care service, ($20 for office visits,
$40 for emergency room visits) usually when you receive the service.
Deductible
The amount you pay for medical health care services, according to your plan of coverage, before your insurance begins to pay. For example, if your deductible is
$100, your plan won’t pay anything until you have met your deductible for health care services.
1
Durable Medical Equipment (DME)
Equipment and supplies ordered by a health care provider for everyday or extended use.
Coverage for DME may include: oxygen equipment, wheelchairs, or crutches, etc., subject to the applicable deductibles.
Emergency Medical Condition
An illness, injury, symptom or condition so serious that it is life-threatening or physically impairing.
Emergency Medical Transportation
Ambulance services for an emergency medical condition.
Emergency Room Care
Services for life-threatening or physically impairing symptoms.
Exceptional Cases
Medical care that is not specified in the
COEHA Active/Retired Non-Medicare Rules and Regulations Handbook.
Exclusions
Health care services that your health insurance plan does not cover.
Grievance
A complaint that you communicate to
COEHA regarding handling of payment for your health care service.
Health Insurance
A contract that requires your health insurer to pay some or all of your health care costs in exchange for a premium.
Home Health Services
Part-time nursing care rendered by or supervised by a registered nurse or licensed practical nurse, prescribed by the attending
2 physician, and subject to the deductible according to your plan.
Hospitalization
Care in a hospital that requires admission as an inpatient and usually requires an overnight stay. An overnight stay for observation could be outpatient care.
Hospital Outpatient Care
Care in a hospital that usually doesn’t require an overnight stay.
Medically Necessary
Health care services or supplies needed to prevent, diagnose or treat an illness, injury condition, disease or its symptoms and that meet accepted standards of medicine.
Network
The facilities, providers and suppliers your health insurer or plan has contracted with to provide health care services.
Orthotics
Items serving to protect, restore or improve function. Coverage for orthotics include: braces, and supports. Not all orthotics are covered.
Out-of –Network
A provider that is not contracted with your insurance to provide health care or services.
Out-of-Network Co-insurance
The allowed amount you pay for out-ofnetwork services.
Out-of-pocket
The amount you pay until you have paid a set amount. Once this amount has been paid by you, our payment reverts to 100% of the allowed amount. Out-of-pocket is yearly.
Plan
A benefit provided to you to pay for your health care services.
Preauthorization
Prior approval by the Administrator of the
C&O Employees’ Hospital Association for a health care service, treatment plan, prescription drug, or for durable medical equipment that is medically necessary.
Your Health insurance or plan may require prior approval for certain services before you receive them, except in an emergency.
The prior approval is not a promise your health insurance or plan will cover the cost.
Premium
The amount that must be paid for your health insurance or plan.
Prescription Drug Coverage
Health insurance or plan that helps pay for prescription drugs and medications.
Prosthetics
Artificial substitutes that replace missing body parts. Your plan covers certain prosthetic devices such as artificial limbs, eyes, breast prosthetics, etc. Not all prosthetic devices are covered. Benefits are administered on a case by case basis.
Provider
A physician or health care professional or health care facility licensed, certified or accredited as required by law.
Reconstructive Surgery
Coverage for surgery in connection with a mastectomy. (See COEHA Rules and
Regulations Handbook)
3
Rehabilitation Services
Health care services that help a person keep, get back, or improve skills and functioning for daily living that have been lost or impaired because a person was sick, hurt ,or disabled. These services may include physical therapy and occupational therapy, speech-language pathology, and psychiatric rehabilitation services in a variety of inpatient and/or outpatient settings.
Skilled Nursing Facility Care
Skilled Nursing Facility (SNF) care is health care given when you need skilled nursing or rehabilitation staff to manage, observe, and evaluate your care. These skilled care services are needed daily on a short-term basis.