The Reproductive System
advertisement

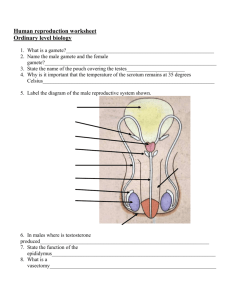
The Reproductive System The reproductive system consists of: 1- The primary sex organs, or gonads are the testes in males and the ovaries in females. The gonads produce sex cells, or gametes and secrete a variety of steroid hormones commonly called sex hormones. 2- The accessory reproductive organs :ducts, glands, and external genitalia . -Although male and female reproductive organs are quite different, their common purpose is to produce offspring. • A sperm and egg may fuse to form a fertilized egg, the first cell of the new individual, from which all body cells will arise. Once fertilization has occurred, the uterus provides the protective environment in which the embryo develops until birth. • Sex hormones–androgens in males and estrogens and progesterone in females–play vital roles both in the development and function of the reproductive organs and in sexual behavior and drives. Anatomy of the Male Reproductive System • The sperm-producing testes or male gonads, lie within the scrotum. • From the testes, the sperm are delivered to the body exterior through a system of ducts including (in order) the epididymis, the ductus deferens, the ejaculatory duct, and finally the urethra, which opens to the outside at the tip of the penis. • The accessory sex glands, which empty their secretions into the ducts during ejaculation, are the seminal vesicles, prostate, and bulbourethral glands. • The Scrotum The scrotum is a sac of skin ,covered with sparse hairs, and contains paired oval testes. A midline septum divides the scrotum, providing a compartment for each testis. Because viable sperm cannot be produced in abundance at core body temperature (37°C), the superficial location of the scrotum, which provides a temperature about 3°C lower, is an essential adaptation. • Furthermore, the scrotum responds to temperature changes: • When it is cold, the testes are pulled closer to the warmth of the body wall, and the scrotum becomes shorter and heavily wrinkled, increasing its thickness to reduce heat loss. • When it is warm, the scrotal skin is flaccid and loose to increase the surface area for cooling (sweating) and the testes hang lower, away from the body trunk. The Testes Each testis is approximately 4 cm (1.5 inches) long and 2.5 cm (1 inch) in width and is surrounded by the tunica albuginea ,the fibrous capsule of the testis. Septa extending from the tunica albuginea divide the testis into 250 to 300 wedge-shaped lobules ,each containing one to four tightly coiled seminiferous tubules, the actual “sperm factories.” Surrounding each seminiferous tubule are smooth muscle cells .By contracting rhythmically, these muscles squeeze sperm and testicular fluids through the tubules and out of the testes. • The seminiferous tubules of testis converge into the rete testis (re′te), a tubular network on the posterior side of the testis. From the rete testis, sperm leave the testis and enter the epididymis. • Lying in the soft connective tissue surrounding the seminiferous tubules are the interstitial cells, also called Leydig cells .These cells produce androgens (testosterone). • Thus, the sperm-producing and hormoneproducing functions of the testis are carried out by completely different cell populations. • testicular arteries, which branch from the abdominal aorta superior to the pelvis supply the testes. • The right testicular vein drains into the inferior vena cava ,the left drains into the left renal vein superiorly. • The testes are served by both divisions of the autonomic nervous system. • Associated sensory nerves transmit impulses that result in agonizing pain and nausea when the testes are hit forcefully. • The nerve fibers are enclosed, along with the blood vessels and lymphatics, in a connective tissue sheath called the spermatic cord which passes through the inguinal canal . The Male Duct System In order (proximal to distal), the accessory ducts are : 1-The Epididymis The cup-shaped epididymis is about 3.8 cm long . Its head caps the superior aspect of the testis. Its body and tail are on the posterolateral area of the testis. It`s an uncoiled length is about 6 m. • The immature, nearly nonmotile sperm as it moves along its tortuous course (a trip that takes about 20 days), the sperm gain the ability to swim. • Sperm are ejaculated as the smooth muscle in the epididymis walls contracts, expelling sperm into the next segment of the duct system, the ductus deferens. • Sperm can be stored in the epididymis for several months, but if held longer, they are eventually phagocytized by epithelial cells of the epididymis. 2-The Ductus Deferens and Ejaculatory Duct The ductus deferens or vas deferens, is about 45 cm long. It runs upward as part of the spermatic cord through the inguinal canal into the pelvis .It then descends along the posterior bladder wall, then it joins with the duct of the seminal vesicle (a gland) to form the short ejaculatory duct. Each ejaculatory duct enters the prostate; there it empties into the urethra. • Its muscular layer is extremely thick and the duct feels like a hard wire when squeezed between the fingertips. At the moment of ejaculation, the thick layers of smooth muscle in its walls create strong peristaltic waves that rapidly squeeze the sperm forward along the tract and into the urethra. • Part of the ductus deferens lies in the scrotal sac. Some men opt to take full responsibility for birth control by having a vasectomy. Sperm are still produced, but they can no longer reach the body exterior. Eventually, they deteriorate and are phagocytized. The Urethra The urethra is the terminal portion of the male duct system. It conveys both urine and semen (at different times), so it serves both the urinary and reproductive systems. Its three regions are (1) the prostatic urethra, the portion surrounded by the prostate; (2) the membranous (or intermediate part of the) urethra in the urogenital diaphragm; and (3) the spongy (penile) urethra, which runs through the penis and opens to the outside at the external urethral orifice(about 15 cm long) . • Accessory Glands The accessory glands produce the bulk of semen (sperm plus accessory gland secretions). 1-The Seminal Vesicles It lie. Two fairly large, hollow glands , about the shape and length (5–7 cm) of a little finger on the posterior bladder surface. • Its secretion is a yellowish viscous alkaline fluid( 60% of the volume of semen) containing fructose sugar, ascorbic acid and prostaglandins, as well as other substances that enhance sperm motility or fertilizing power. • The duct of each seminal vesicle joins that of the ductus deferens on the same side to form the ejaculatory duct. Sperm and seminal fluid mix in the ejaculatory duct and enter the prostatic urethra together during ejaculation. 2-The Prostate The prostate (pros′tāt) is a single doughnutshaped. It encircles the urethra just inferior to the bladder. The prostatic gland secretion enters the prostatic urethra via several ducts when prostatic smooth muscle contracts during ejaculation. It plays a role in activating sperm and accounts for up to one-third of the semen volume. It is a milky, slightly acid fluid that contains citrate (a nutrient source), several enzymes and prostate-specific antigen (PSA). 3-The Bulbourethral Glands The bulbourethral glands are pea-sized glands inferior to the prostate gland .They produce a thick, clear mucus, some of which drains into the spongy urethra when a man becomes sexually excited and neutralizes traces of acidic urine in the urethra. • Semen is a milky white, somewhat sticky mixture of sperm and accessory gland secretions. The liquid provides a transport medium and nutrients. Mature sperm contains little cytoplasm or stored nutrients. Catabolism of the fructose in seminal vesicle secretion provides nearly all the fuel needed for sperm ATP synthesis. -Prostaglandins in semen decrease the viscosity of mucus guarding the entry (cervix) of the uterus and facilitate sperm movement through the female reproductive tract. -The relative alkalinity of semen as a whole (pH 7.2–7.6) helps neutralize the acid environment of the male’s urethra and the female’s vagina, thereby protecting the delicate sperm and enhancing their motility. -Sperms are very sluggish under acidic conditions (below pH 6). - Semen also contains substances that suppress the immune response in the female’s reproductive tract and an antibiotic chemical called seminalplasmin, which destroys certain bacteria. - Clotting factors found in semen coagulate it just after it is ejaculated. Soon, its contained fibrinolysin liquefies the sticky mass, enabling the sperm to swim out and begin their journey through the female duct system. -The amount of semen propelled out of the male duct system during ejaculation is 2–5 ml, but there are between 20 and 150 million sperm per milliliter. Spermatogenesis (sperm formation) -The process begins around the age of 14 years in males, and continues throughout life. Every day, a healthy adult male makes about 400 million sperm. The normal chromosome number in most body cells is referred to as the diploid chromosomal number (dip′loid) of the organism, symbolized as 2n. In humans, this number is 46, and such diploid cells contain 23 pairs of similar chromosomes called homologous chromosomes. One member of each pair is from the male parent (the paternal chromosome); the other is from the female parent (the maternal chromosome). • The number of chromosomes present in human gametes is 23, referred to as the haploid chromosomal number (hap′loid), or n; gametes contain only one member of each homologous pair. When sperm and egg fuse, they form a fertilized egg that reestablishes the typical diploid chromosomal number of human cells. Gamete formation in both sexes involves meiosis, a unique kind of nuclear division that, for the most part, occurs only in the gonads. • Meiosis consists of two consecutive nuclear divisions, and its product is four daughter cells instead of two, each with half as many chromosomes as typical body cells. Thus, meiosis reduces the chromosomal number by half (from 2n to n) in gametes. Mitosis of Spermatogonia: Forming Spermatocytes The outermost tubule cells are stem cells called spermatogonia . -The spermatogonia divide more or less continuously by mitosis and, until puberty, all their daughter cells become spermatogonia. - Spermatogenesis begins during puberty, and from then on, each mitotic division of a spermatogonium results in two distinctive daughter cells–types A and B. The type A daughter cell remains at the basement membrane to maintain the germ cell line. -The type B cell gets pushed toward the lumen, where it becomes a primary spermatocyte destined to produce four sperms. Meiosis: Spermatocytes to Spermatids Each primary spermatocyte generated during the first phase undergoes meiosis I, forming two smaller haploid cells called secondary spermatocytes. The secondary spermatocytes continue on rapidly into meiosis II, and their daughter cells, called spermatids. Spermiogenesis: Spermatids to Sperm Each spermatid has the correct chromosomal number for fertilization (n), but is nonmotile. It still must undergo a process called spermiogenesis, during which it elongates, sheds its excess cytoplasmic baggage, and forms a tail. The resulting sperm, or spermatozoon has a head, a midpiece, and a tail. -The head of a sperm consists almost entirely of its flattened nucleus, which contains the compacted DNA. Adhering to the top of the nucleus is a helmetlike acrosome . -Acrosome contains hydrolytic enzymes that enable the sperm to penetrate and enter an egg. - The sperm midpiece contains mitochondria spiraled tightly around the contractile filaments of the tail. -The long tail is a typical flagellum produced by the centriole near the nucleus. The mitochondria provide the metabolic energy (ATP) needed for the whiplike movements of the tail that will propel the sperm along its way in the female reproductive tract. Hormonal Regulation of Male Reproductive Function The Brain-Testicular Axis Hormonal regulation of spermatogenesis and testicular androgen production involves interactions between the hypothalamus, anterior pituitary gland, and testes, a relationship sometimes called the brain-testicular axis. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which controls the release of the two anterior pituitary gonadotropins: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). (Both FSH and LH were named for their effects on the female gonad). - FSH stimulates spermatogenesis indirectly by making the spermatogenic cells receptive to testosterone’s stimulatory effects. - LH binds to the interstitial cells, prodding them to secrete testosterone (and a small amount of estrogen). - Locally, testosterone serves as the final trigger for spermatogenesis. Testosterone entering the bloodstream exerts a number of effects at other body sites. Male secondary sex characteristics–that is, features induced in the nonreproductive organs by the male sex hormones (mainly testosterone)–make their appearance at puberty. • These include the appearance of pubic, axillary, and facial hair, enhanced hair growth on the chest or other body areas in some men, and a deepening of the voice as the larynx enlarges. The skin thickens and becomes oilier (which predisposes young men to acne), bones grow and increase in density, and skeletal muscles increase in size and mass. -Testosterone also boosts basal metabolic rate and It is the basis of the sex drive (libido) in males and to some extent in females. -The testes are not the only source of androgens; the adrenal glands of both sexes also release androgens. Female Reproductive System The reproductive role of the female is far more complex than that of a male. Not only must she produce gametes, but her body must prepare to nurture a developing embryo for a period of approximately nine months. Ovaries, the female gonads, are the primary reproductive organs of a female, and like the male testes, ovaries serve a dual purpose: They produce the female gametes (ova) and sex hormones, the estrogens and progesterone (pro-ges′tĕ-rōn). The female’s accessory ducts, from the ovary to the body exterior, are the uterine tubes, the uterus, and the vagina. The Ovaries The paired ovaries flank the uterus on each side .Shaped like an almond and about twice as large, each ovary is held in place within the peritoneal cavity by several ligaments. The ovarian ligament anchors the ovary medially to the uterus; the suspensory ligament anchors it laterally to the pelvic . In between , they are enclosed and held in place by a fold of peritoneum, the broad ligament. The ovaries are served by the ovarian arteries, branches of the abdominal aorta and by the ovarian branch of the uterine arteries. • Embedded in the highly vascular connective tissue of the ovary cortex are many tiny saclike structures called ovarian follicles. Each follicle consists of an immature egg, called an oocyte surrounded by one or more layers of very different cells called follicle cells. Follicles at different stages of maturation are distinguished by their structure. • A primordial follicle, one layer of squamouslike follicle cells surrounds the oocyte. • A primary follicle has two or more layers of cuboidal or columnar-type cells enclosing the oocyte; it becomes a secondary follicle when fluidfilled spaces appear and then coalesce to form a central fluid-filled cavity called an antrum. • At the mature vesicular follicle, or Graafian follicle (graf′e-an), stage, the follicle bulges from the surface of the ovary. • Each month in adult women, one of the ripening follicles ejects its oocyte from the ovary, an event called ovulation . • After ovulation, the ruptured follicle is transformed into a very different looking glandular structure called the corpus luteum (lu′te-um; plural: corpora lutea), which eventually degenerates. As a rule, most of these structures can be seen within the same ovary. • In older women, the surfaces of the ovaries are scarred and pitted, revealing that many oocytes have been released. The Female Duct System 1-The Uterine Tubes • The uterine tubes (u′ter-in), also called fallopian tubes or oviducts, form the initial part of the female duct system .They receive the ovulated oocyte and are the site where fertilization generally occurs. • Each uterine tube is about 10 cm (4 inches) long and extends medially from the region of an ovary to empty into the superolateral region of the uterus . • The distal end of each uterine tube expands as funnel-shaped infundibulum bearing ciliated, fingerlike projections called fimbriae that partially surround the ovary. • Unlike the male duct system, which is continuous with the tubules of the testes, the uterine tubes have little or no actual contact with the ovaries. An ovulated oocyte is cast into the peritoneal cavity, and many oocytes are lost there. • The uterine tube performs complex movements to capture oocytes–it bends to drape over the ovary while the fimbriae stiffen and sweep the ovarian surface. The beating cilia on the fimbriae then create currents in the peritoneal fluid that tend to carry an oocyte into the uterine tube, where it begins its journey toward the uterus. HOMEOSTATIC IMBALANCE • The fact that the uterine tubes are not continuous with the ovaries places women at risk for ectopic pregnancy in which a zygote, fertilized in the peritoneal cavity or distal portion of the uterine tube, begins developing there. Because the tube lacks adequate mass and vascularization to support the full term of pregnancy, such pregnancies naturally abort, often with substantial bleeding. HOMEOSTATIC IMBALANCE • Another potential problem is infection spreading into the peritoneal cavity from other parts of the reproductive tract causing an extremely severe inflammation called pelvic inflammatory disease (PID). Unless treated promptly with broad-spectrum antibiotics, PID can cause scarring of the narrow uterine tubes and of the ovaries, causing sterility. Indeed, scarring and closure of the uterine tubes, which have an internal diameter as small as the width of a human hair in some regions, is one of the major causes of female infertility. 2-The Uterus The uterus is located in the pelvis, anterior to the rectum and posterosuperior to the bladder .It is a hollow, thick-walled, muscular organ that functions to receive, retain, and nourish a fertilized ovum. - In a premenopausal woman who has never been pregnant, the uterus is about the size and shape of an inverted pear, but it is usually somewhat larger in women who have borne children. - Normally, the uterus flexes anteriorly where it joins the vagina, causing the uterus as a whole to be inclined forward, or anteverted. However, the organ is frequently turned backward, or retroverted, in older women. -The major portion of the uterus is referred to as the body . -The rounded region superior to the entrance of the uterine tubes is the fundus, and the slightly narrowed region between the body and the cervix is the isthmus. -The cervix of the uterus is its narrow neck, or outlet, which projects into the vagina inferiorly. The cavity of the cervix, called the cervical canal, communicates with the vagina via the external os (os = mouth) and with the cavity of the uterine body via the internal os. The mucosa of the cervical canal contains cervical glands that secrete a mucus that fills the cervical canal and covers the external os, presumably to block the spread of bacteria from the vagina into the uterus. Cervical mucus also blocks the entry of sperm, except at midcycle, when it becomes less viscous and allows sperm to pass through. HOMEOSTATIC IMBALANCE • Cancer of the cervix strikes about 450,000 women worldwide each year, killing about half. • It is most common among women between the ages of 30 and 50. • Risk factors include frequent cervical inflammations, sexually transmitted diseases including genital warts, and multiple pregnancies. • A Pap smear is the most effective way to detect this slow-growing cancer. • Supports of the Uterus The uterus is supported laterally by the broad ligament and anchord anteriorly and posteriorly by the round and uterosacral ligaments respectively. These ligaments allow the uterus a good deal of mobility, and its position changes as the rectum and bladder fill and empty. HOMEOSTATIC IMBALANCE Despite the many anchoring ligaments, the principal support of the uterus is provided by the muscles of the pelvic floor, namely the muscles of the urogenital and pelvic diaphragms .These muscles are sometimes torn during childbirth. Subsequently, the unsupported uterus may sink inferiorly, until the tip of the cervix protrudes through the external vaginal opening. This condition is called prolapse of the uterus. The Uterine Wall Is composed of three layers : • The perimetrium, the incomplete outermost serous layer, is the peritoneum. • The myometrium (mi″o-me′tre-um; “muscle of the uterus”) is the bulky middle layer, composed of interlacing bundles of smooth muscle, that contracts rhythmically during childbirth to expel the baby from the mother’s body. • The endometrium is the mucosal lining of the uterine cavity. If fertilization occurs, the young embryo burrows into the endometrium (implants) and resides there for the rest of its development. • The endometrium has two chief strata (layers): -The functional layer, undergoes cyclic changes in response to blood levels of ovarian hormones and is shed during menstruation (approximately every 28 days). -The thinner, deeper stratum basalis (ba-să′lis), or basal layer, forms a new functional layer after menstruation ends . It is unresponsive to ovarian hormones. -The endometrium has numerous uterine glands that change in length as endometrial thickness changes. The Vagina The vagina is a thin-walled tube, 8–10 cm long. It lies between the bladder and the rectum and extends from the cervix to the body exterior .The urethra is embedded in its anterior wall. • called the birth canal, the vagina provides a passageway for delivery of an infant and for menstrual flow. • The mucosa is a stratified squamous epithelium adapted to stand up to friction. The vaginal mucosa has no glands; it is lubricated by the cervical mucous glands. • The pH of a woman’s vagina is normally quite acidic. This acidity helps keep the vagina healthy and free of infection, but it is also hostile to sperm. • In virgins (those who have never participated in sexual intercourse), the mucosa near the distal vaginal orifice forms an incomplete partition called the hymen (hi′men) . • The hymen is very vascular and tends to bleed when it is ruptured during the first coitus (sexual intercourse). However, its durability varies. In some females, it is ruptured during a sports activity, tampon insertion, or pelvic examination. • ccasionally, it is so tough that it must be breached surgically if intercourse is to occur. • The upper end of the vaginal canal loosely surrounds the cervix of the uterus, producing a vaginal recess called the vaginal fornix. The posterior part of this recess, the posterior fornix, is much deeper than the lateral and anterior fornices . • Generally, the lumen of the vagina is quite small and, except where it is held open by the cervix, its posterior and anterior walls are in contact with one another. The vagina stretches considerably during copulation and childbirth, but its lateral distension is limited by the ischial spines . The External Genitalia The female reproductive structures that lie external to the vagina are called the external genitalia .The external genitalia, also called the vulva . • The mons pubis is a fatty, rounded area overlying the pubic symphysis. After puberty, this area is covered with pubic hair. • Running posteriorly from the mons pubis are two elongated, hair-covered fatty skin folds, the labia majora . The labia majora enclose the labia minora ,two thin, hair-free skin folds. The labia minora enclose a recess called the vestibule (“entrance hall”), which contains the external openings of the urethra and the vagina. • anterior to the vestibule is the clitoris ,a small, protruding structure composed largely of erectile tissue, which is homologous to the penis of the male. • Flanking the vaginal opening are the pea-size greater vestibular glands (Bartholin`s glands), homologous to the bulbourethral glands of males. These glands release mucus into the vestibule and help to keep it moist and lubricated, facilitating intercourse. • The female perineum is a diamond-shaped region located between the pubic arch anteriorly, the coccyx posteriorly, and the ischial tuberosities laterally. The Mammary Glands They are present in both sexes, but they normally function only in females . • They are modified sweat glands that are really part of the skin, or integumentary system. Each mammary gland is contained within a rounded skin-covered breast within the hypodermis (superficial fascia), anterior to the pectoral muscles of the thorax. Slightly below the center of each breast is a ring of pigmented skin, the areola (ahre′o-lah), which surrounds a central protruding nipple. • Internally, each mammary gland consists of 15 to 25 lobes that open at the nipple. Within the lobes are smaller units called lobules, which contain glandular alveoli that produce milk when a woman is lactating. These compound alveolar glands pass the milk into the lactiferous ducts which open to the outside at the nipple. Just deep to the areola, each duct has a dilated region called a lactiferous sinus where milk accumulates during nursing. • In nonpregnant women, the glandular structure of the breast is largely undeveloped and the duct system is rudimentary; hence breast size is largely due to the amount of fat deposits. Breast Cancer Invasive breast cancer is the most common malignancy and the second most common cause of cancer death of U.S. women. Thirteen percent of women in the general population (132 out of 1000 individuals) will develop this condition. Breast cancer usually arises from the epithelial cells of the smallest ducts, not from the alveoli. A small cluster of cancer cells grows into a lump in the breast from which cells eventually metastasize. Known risk factors for developing breast cancer include: (1) early onset menses and late menopause; (2) no pregnancies or first pregnancy later in life and no or short periods of breast feeding. (3) family history of breast cancer (especially in a sister or mother), and (4) postmenopausal estrogen-progesterone replacement. MAMMOGRAPHY Mammography is an x-ray technique that is used to evaluate breast tissue for abnormalities. By far the most frequent usage is to detect breast cancer, which is one of the most common malignancies in women. If detected early, breast cancer may be cured through a combination of surgery, radiation, and chemotherapy. Women should practice breast self-examination monthly , but mammography can detect lumps that are too small to be felt manually. Women in their 30s may have a mammogram done to serve as a comparison for mammograms later in life. Physiology of the Female Reproductive System Oogenesis • Gamete production in males begins at puberty and continues throughout life, but the situation is quite different in females. • It has been assumed that a female’s total supply of eggs is already determined by the time she is born, and the time span during which she releases them extends only from puberty to menopause (about the age of 50). • Meiosis, the specialized nuclear division that occurs in the testes to produce sperm, also occurs in the ovaries. In this case, female sex cells are produced, and the process is called oogenesis .The process of oogenesis takes years to complete. • First, in the fetal period the oogonia, the diploid stem cells of the ovaries, multiply rapidly by mitosis. Gradually, primordial follicles begin to appear as the oogonia are transformed into primary oocytes and become surrounded by a single layer of flattened follicle cells. • By birth, a female has been presumed to have her lifetime supply of primary oocytes; of the original 7 million oocytes approximately 2 million of them escape programmed death and are already in place in the immature ovary. The wait is a long one–10 to 14 years at the very least. • At puberty, perhaps 250,000 oocytes remain and beginning at this time a small number of primary oocytes are activated each month in response to the LH surge midcycle. However, only one is “selected” each time to continue meiosis I, ultimately producing two haploid cells (each with 23 replicated chromosomes) that are quite dissimilar in size. • The smaller cell is called the first polar body. The larger cell, which contains nearly all the cytoplasm of the primary oocyte, is the secondary oocyte. • The first polar body may continue its development and undergo meiosis II, producing two even smaller polar bodies. • The secondary oocyte (not a functional ovum) is ovulated. If an ovulated secondary oocyte is not penetrated by a sperm, it simply deteriorates. But, if sperm penetration does occur, it quickly completes meiosis II, yielding one large ovum and a tiny second polar body . • The union of the egg and sperm nuclei, constitutes fertilization. • The potential end products of oogenesis are three tiny polar bodies, nearly devoid of cytoplasm, and one large ovum. All of these cells are haploid, but only the ovum is a functional gamete. • This is quite different from spermatogenesis, where the product is four viable gametes–spermatozoa. • The unequal cytoplasmic divisions that occur during oogenesis ensure that a fertilized egg has ample nutrients for its six- to seven-day journey to the uterus. Without nutrient-containing cytoplasm the polar bodies degenerate and die. • Since the reproductive life of a female is at most about 40 years (from the age of 11 to approximately 51) and typically only one ovulation occurs each month, fewer than 500 oocytes out of her estimated pubertal potential of 250,000 are released during a woman’s lifetime. The Ovarian Cycle The monthly series of events associated with the maturation of an egg is called the ovarian cycle. The ovarian cycle is best described in terms of two consecutive phases. 1-follicular phase is the period of follicle growth, typically indicated as lasting from the first to the fourteenth day of the cycle. 2-The luteal phase is the period of corpus luteum activity, days 14–28. The so-called typical ovarian cycle repeats at intervals of 28 days, with ovulation occurring midcycle. However, only 10–15% of women naturally have 28-day cycles; cycles as long as 40 days or as short as 21 days are fairly common. In such cases, the length of the follicular phase and timing of ovulation vary, : It is 14 days between the time of ovulation and the end of the cycle. The Follicular Phase It occupies the first half of the cycle and involves several events. • Primordial Follicle Becomes a Primary Follicle When a primordial follicle is activated ,the squamouslike cells surrounding the primary oocyte grow, becoming cuboidal cells, and the oocyte enlarges. The follicle is now called a primary follicle • A Primary Follicle Becomes a Secondary Follicle Next, follicular cells proliferate forming a stratified epithelium around the oocyte . • In the next stage , a layer of connective tissue condenses around the follicle, forming the theca folliculi. As the follicle grows, the surrounding cells cooperate to produce estrogens . • At the same time, the oocyte secretes a glycoprotein-rich substance that forms a thick transparent membrane, called the zona pellucida that encapsulates it . • Clear liquid accumulates between the cells and eventually coalesces to form a fluid-filled cavity called the antrum .The presence of an antrum distinguishes the new secondary follicle from the primary follicle. • A Secondary Follicle Becomes a Vesicular Follicle The antrum continues to expand with fluid until it isolates the oocyte, along with its surrounding capsule of cells called a corona radiata. When a follicle is full size (about 2.5 cm, or 1 inch, in diameter), it becomes a vesicular follicle and bulges from the external ovarian surface like an “angry boil.” This usually occurs by day 14. As one of the final events of follicle maturation, the primary oocyte completes meiosis I to form the secondary oocyte and first polar body. Once this has occurred , the stage is set for ovulation. • Ovulation Ovulation occurs when the ballooning ovary wall ruptures and expels the secondary oocyte (still surrounded by its corona radiata) into the peritoneal cavity . Some women experience a middle pain caused by the intense stretching of the ovarian wall during ovulation. In the ovaries of adult females, there are always several follicles at different stages of maturation. As a rule, one follicle outstrips the others to become the dominant follicle and is at the peak stage of maturation when the hormonal (LH) stimulus is given for ovulation. The others degenerate (undergo programmed cell death, or apoptosis) and are reabsorbed. • In 1–2% of all ovulations, more than one oocyte is ovulated. This phenomenon, which increases with age, can result in multiple births. Since, in such cases, different oocytes are fertilized by different sperm, the siblings are fraternal, or nonidentical, twins. • Identical twins result from the fertilization of a single oocyte by a single sperm, followed by separation of the fertilized egg’s daughter cells in early development. • Additionally, it now appears that in some women, oocytes may be released at times unrelated to the woman’s hormone levels, which may help to explain why a rhythm method of contraception sometimes fails and why some fraternal twins have different conception dates. The Luteal Phase After ovulation, the ruptured follicle collapses, and the antrum fills with clotted blood. The remaining cells increase in size and they form a new, quite different endocrine gland, the corpus luteum (“yellow body”), that begins to secrete progesterone and some estrogen. • If pregnancy does not occur, the corpus luteum starts degenerating in about ten days and its hormonal output ends. In this case, all that ultimately remains is a scar called the corpus albicans . • On the other hand, if the oocyte is fertilized and pregnancy ensues, the corpus luteum persists until the placenta is ready to take over its hormone-producing duties in about three months. Hormonal Regulation of the Ovarian Cycle Gonadotropin-releasing hormone (GnRH) and the pituitary gonadotropins interact to produce the cyclic events occurring in the ovaries. • Establishing the Ovarian Cycle As puberty nears, the hypothalamus begins to release GnRH in a rhythmic manner which stimulates the anterior pituitary to release FSH and LH, which prompt the ovaries to secrete hormones (primarily estrogens). Gonadotropin levels continue to increase for about four years and, during this time, pubertal girls are still not ovulating and thus are incapable of getting pregnant. The young woman’s first menstrual period is referred to as menarche. • Usually, it is not until the third year postmenarche that the cycles become regular and all are ovulatory. • As LH blood levels fall, the stimulus for luteal activity ends, and the corpus luteum degenerates so blood estrogen and progesterone levels drop sharply. The marked decline in ovarian hormones at the end of the cycle (days 26–28) ends their blockade of FSH and LH secretion, and the cycle starts anew. Although the ovarian events are described as if we are following one follicle through the 28-day cycle, this is not really the case. What is happening is that the increase of FSH at the beginning of each cycle activates several follicles to mature. Then, with the midcycle LH surge, one (or more) Graafian follicles undergo ovulation. Uterine (Menstrual) Cycle Although the uterus is where the young embryo implants and develops, it is receptive to implantation for only a short period each month when a developing embryo would normally begin implanting, six to seven days after ovulation. The uterine, or menstrual cycle is a series of cyclic changes that the uterine endometrium goes through each month as it responds to ovarian hormones in the blood. These endometrial changes are coordinated with the phases of the ovarian cycle, which are dictated by gonadotropins released by the anterior pituitary. The events of the uterine cycle, are as follows: 1. Days 1–5, Menstrual phase: In this phase, menstruation ,the uterus sheds all but the deepest part of its endometrium. (At the beginning of this stage, ovarian hormones are at their lowest normal levels and gonadotropins are beginning to rise). The thick, hormone-dependent functional layer of the endometrium detaches from the uterine wall, a process that is accompanied by bleeding for 3–5 days with about 150 ml of blood. The detached tissue and blood pass out through the vagina as the menstrual flow. By day 5, the growing ovarian follicles are starting to produce more estrogen . 2. Days 6–14, Proliferative (preovulatory) phase Under the influence of rising blood levels of estrogens, the basal layer of the endometrium generates a new functional layer. As this new layer thickens, its glands enlarge and its spiral arteries increase in number . Consequently, the endometrium once again becomes velvety, thick, and well vascularized. Normally, cervical mucus is thick and sticky, but rising estrogen levels cause it to thin to facilitate the passage of sperm into the uterus. Ovulation, which takes less than five minutes, occurs in the ovary at the end of the proliferative stage (day 14) in response to the sudden release of LH from the anterior pituitary. LH also converts the ruptured follicle to a corpus luteum. 3. Days 15–28, Secretory (postovulatory) phase: • This 14-day phase is the most constant timewise. Rising levels of progesterone convert the functional layer to a secretory mucosa. The uterine glands enlarge, coil, and begin secreting nutritious glycogen into the uterine cavity. These nutrients sustain the embryo until it has implanted in the blood-rich endometrial lining. • Increasing progesterone levels also cause the cervical mucus to become viscous again, forming the cervical plug, which blocks sperm entry. • Rising progesterone (and estrogen) levels inhibit LH release by the anterior pituitary. • If fertilization has not occurred, the corpus luteum begins to degenerate toward the end of the secretory phase as LH blood levels decline. Progesterone levels fall, and the spiral arteries kink and go into spasms so endometrial cells die, setting the stage for menstruation to begin on day 28. • The spiral arteries then suddenly relax and open wide. As blood gushes into the weakened capillary beds, they fragment, causing the functional layer to slough off. • The menstrual cycle starts over again on this first day of menstrual flow. Developmental Aspects of the Reproductive System • Genetic sex is determined (at the time of fertilization), by the sex chromosomes: an X from the mother, an X or a Y from the father. If the fertilized egg contains XX, it is a female and develops ovaries; if it contains XY, it is a male and develops testes. • The development of male accessory structures and external genitalia depends on the presence of testosterone produced by the embryonic testes. In its absence, female structures develop. • The testes form in the abdominal cavity and descend into the scrotum. • Puberty is the interval when reproductive organs mature and become functional. It begins in males with penile and scrotal growth and in females with breast development. • During menopause, ovarian function declines, and ovulation and menstruation cease. Hot flashes and mood changes may occur. Postmenopausal events include atrophy of the reproductive organs, bone mass loss, and increasing risk for cardiovascular disease. Pregnancy and Human Development • The term pregnancy refers to events that occur from the time of fertilization (conception) until the infant is born. • The time during which development occurs is referred to as the gestation period and extends from the last menstrual period (a date the woman is likely to remember) until birth, approximately 280 days. Thus, at the moment of fertilization, the mother is officially two weeks pregnant! • From fertilization through week 8, the embryonic period, the conceptus is called an embryo, and from week 9 through birth, the fetal period, the conceptus is called a fetus . • At birth, it is an infant. Accomplishing Fertilization • • • • Before fertilization can occur, sperm must reach the ovulated secondary oocyte. The oocyte is viable for 12 to 24 hours after it is cast out of the ovary. Most sperm retain their fertilizing power for 24 to 48 hours after ejaculation. Consequently, for successful fertilization to occur, coitus must occur no more than two days before ovulation and no later than 24 hours after, at which point the oocyte is approximately one-third of the way down the length of the uterine tube. Fertilization occurs when a sperm nucleus fuses with an that of the egg (actually a secondary oocyte) to form a fertilized egg, or zygote ,the first cell of the new individual. • Sperm freshly deposited must first be capacitated over the next 6 to 8 hours; that is, their mobility is enhanced and their membranes must become fragile so that the hydrolytic enzymes in their acrosomes can be released. Thus, even though the sperm may reach the oocyte within a few minutes, they must “wait around” for capacitation to occur. Hundreds of sperms must release their acrosomal enzymes to break down the egg’s corona radiata and zona pellucida. When one sperm binds to receptors on the egg, it triggers the slow block to polyspermy. • Polyspermy (entry of several sperm into an egg) occurs in some animals, but in humans only one sperm is allowed to penetrate the oocyte, ensuring monospermy • Following sperm penetration, the secondary oocyte completes meiosis II. • Then the ovum and sperm pronuclei fuse (fertilization), forming a zygote. Results of fertilization 1- Determination of the sex of the embryo 2-Restoration of chromosomal number (2n) characteristic of the human embryo which is 46. 3-Starting of cleavage. Events of Embryonic Development: Zygote to Blastocyst • Cleavage, a rapid series of mitotic divisions begins with the zygote and ends with a blastocyst. The blastocyst consists of the trophoblast and an inner cell mass. Cleavage produces a large number of cells. • Implantation The trophoblast adheres to, digests, and implants in the endometrium. Implantation is completed when the blastocyst is entirely surrounded by endometrial tissue, about 12 days after ovulation. • hCG released by the blastocyst maintains hormone production by the corpus luteum, preventing menses. hCG levels decline after four months. • Placentation The placenta acts as the respiratory, nutritive, and excretory organ of the fetus and produces the hormones of pregnancy. It is formed from embryonic and maternal tissues. Typically, the placenta is functional as an endocrine organ by the third month. Gastrulation: formation of Germ Layers ultimately the inner cell mass is transformed into a three-layered embryo (gastrula) containing ectoderm, mesoderm, and endoderm. • Ectoderm forms the nervous system and the epidermis of the skin and its derivatives. • Endoderm forms the mucosa of the digestive and respiratory systems, and the epithelial cells of all associated glands (thyroid, parathyroids, thymus, liver, pancreas). It becomes a continuous tube when the embryonic body fuses ventrally. • Mesoderm forms all other organ systems and tissues. Effects of Pregnancy on the Mother • Anatomical Changes 1.Maternal reproductive organs and breasts become increasingly vascularized during pregnancy, and the breasts enlarge. 2. The uterus eventually occupies nearly the entire abdominopelvic cavity. Abdominal organs are pushed superiorly and encroach on the thoracic cavity, causing the ribs to flare. 3. The increased abdominal mass changes the woman’s center of gravity; lordosis and backache are common. A waddling gait occurs as pelvic ligaments and joints are loosened by placental relaxin. 4. A typical weight gain during pregnancy in a woman of normal weight is 28 pounds. • Physiological Changes 1. Many women suffer morning sickness, heartburn, and constipation during pregnancy. 2. The kidneys produce more urine, and pressure on the bladder may cause frequency, urgency, and stress incontinence. 3. Tidal volume and respiratory rate increase, but residual volume decreases. Dyspnea is common. 4. Total body water and blood volume increase dramatically. Heart rate and blood pressure rise, resulting in enhancement of cardiac output in the mother. Parturition (Birth) is giving birth to the baby. It usually occurs within 15 days of the calculated due date (280 days from the last menstrual period). The series of events that expel the infant from the uterus are collectively called labor. Initiation of Labor Fetal cells produce oxytocin, which stimulates prostaglandin production by the placenta. Both hormones stimulate contraction of uterine muscle. Increasing stress activates the hypothalamus, causing oxytocin release from the posterior pituitary; this sets up a positive feedback loop resulting in true labor. Stages of Labor • The dilation stage is from the onset of rhythmic, strong contractions until the cervix is fully dilated. The head of the fetus rotates as it descends through the pelvic outlet. • The expulsion stage extends from full cervical dilation until birth of the infant. • The placental stage is the delivery of the afterbirth (the placenta and attached fetal membranes). Adjustments of the Infant to Extrauterine Life 1. After the umbilical cord is clamped, carbon dioxide accumulates in the infant’s blood, causing respiratory centers in the brain to trigger the first inspiration. 2. Once the lungs are inflated, breathing is eased by the presence of surfactant, which decreases the surface tension of the alveolar fluid. 3. During the first 8 hours after birth, the infant is physiologically unstable and adjusting. After stabilizing, the infant wakes approximately every 3–4 hours in response to hunger. 4. Inflation of the lungs causes pressure changes in the circulation; as a result, the umbilical arteries and vein, ductus venosus, and ductus arteriosus collapse, and the foramen ovale closes. The occluded blood vessels are converted to fibrous cords; the site of the foramen ovale becomes the fossa ovalis. Lactation 1. The breasts are prepared for lactation during pregnancy by high blood levels of estrogen, progesterone, and placental lactogen. 2. Colostrum, a premilk fluid, is a fat-poor fluid that contains more protein, vitamin A, and minerals than true milk. It is produced toward the end of pregnancy and for the first two to three days after birth. 3. True milk is produced around day 3 in response to suckling, which stimulates the hypothalamus to prompt anterior pituitary release of prolactin and posterior pituitary release of oxytocin. Prolactin stimulates milk production and oxytocin triggers milk let-down. Continued breast-feeding is required for continued milk production. 4. At first, ovulation and menses are absent or irregular during nursing, but in most women the ovarian cycle is eventually reestablished while still nursing. • • • • Related Clinical Terms Abortion Premature removal of the embryo or fetus from the uterus; may be spontaneous or induced. Ectopic pregnancy A pregnancy in which the embryo implants in any site other than the uterus; most often the site is a uterine tube (tubal pregnancy). Hydatid (hydatidiform) mole Developmental abnormality of the placenta; the conceptus degenerates and the chorionic villi convert into a mass of vesicles. Signs include vaginal bleeding, which contains some of the grapelike vesicles. Ultrasonography Noninvasive technique that uses sound waves to visualize the position and size of the fetus and placenta . • Physiological jaundice Jaundice sometimes occurring in normal newborns within three to four days after birth. Fetal erythrocytes are short-lived, and they break down rapidly after birth; the infant’s liver may be unable to process the bilirubin (breakdown product of hemoglobin pigment) fast enough to prevent its accumulation in blood and subsequent deposit in body tissues. • Placenta abruptio Premature separation of the placenta from the uterine wall; if this occurs before labor, it can result in fetal death due to anoxia. • Placenta previa Placental formation adjacent to or across the internal os of the uterus. Represents a problem because as the uterus and cervix stretch, tearing of the placenta may occur. Additionally, the placenta precedes the infant during labor.