Group Project ppt
advertisement

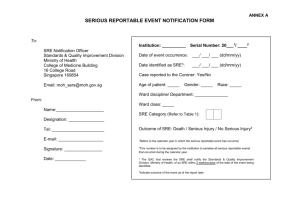
Never Events Board Presentation Lisa Beckman, Connie Egerer, Kerry Heinecke Med Inf 404, Spring 2010 Hospital Background Mid-State University Medical Center is a large midwestern university hospital complex Adult patient hospital is an 11-story, 550-bed, 1.8 Million sq. ft. hospital, opened in 1986 Children’s hospital is a 9-story, 350-bed, 700,000 sq. ft. hospital opened in 2008 Each house diagnostic equipment, clinical laboratories, operating rooms and inpatient and intensive care units 70 percent of patients are admitted from other communities or regional hospitals Never Events Background IOM Reports raised awareness of medical errors CMS lists 17 never events which are nonreimbursable hospital acquired conditions NQF Serious Reportable Event (SRE) list covers 28 types of events grouped in 6 categories Purpose of the SRE’s is to facilitate public accountability for occurrence of medical errors. No federal law mandating reporting; many states have enacted laws requiring reporting of SREs Mid-State University Medical Center Serious Reportable Events Quality Initiative Progress and Recommendations Presenters • Lisa Beckman, Chief Executive Officer • Connie Egerer, Chief Quality and Safety Officer • Kerry Heinecke, Director of Risk Management 5/24/2010 Board Meeting 5 Agenda • Key Objectives • SRE Dashboard • 2008 / 2009 Results for NQF Serious Reportable Events (SRE’s) • Comparison to Similar Institutions • Pareto Analysis • Example SRE • Recommendations • Conclusion 5/24/2010 6 Key Objectives • • • • • • Safe Patient Centered Effective Efficient Timely Equitable 5/24/2010 7 2010 Dashboard Key SRE’s 5/24/2010 8 Serious Reportable Events 16 14 12 10 8 6 4 2 0 5/24/2010 2008 2009 9 Breakdown of Category Product / Device SRE's 1 1 Contaminated drugs, devices, or biologics Device use or function other than intended Intravascular Air Embolism 6 5/24/2010 10 Serious Reportable Events 16 14 12 10 8 6 4 2 0 2008 2009 2009 Similar Institutions 5/24/2010 11 Pareto Analysis 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 2009 % 2009 Cum % 5/24/2010 12 Device Event Example Place Film Plate Take x-ray FILM Move x-ray machine away Retrieve Film Plate Place Tethered Plate Take x-ray DR Retrieve Tethered Plate Move x-ray machine away 5/24/2010 13 Device Event Example • • • • November 2009 Relatively new x-ray technology Experienced x-ray tech Dispatched to PICU for portable x-ray on 2 week old infant POD 1 from open heart surgery to repair complex Congenital Heart Defect – Intubated – Open sternum – Multiple chest tubes, – IV’s, intracardiac lines – Dopamine/Epi to maintain BP 14 SRE Event detail Place Tethered Plate Take x-ray Physician requests to view Retrieve Tethered Plate Move x-ray machine away 5/24/2010 15 Consequences – Extubated – required reintubation – Skeletal series & cranial Ultrasound to Rule Out injury – Family distress – Caregiver distress – No obvious sustained injury – Hospital absorbed extra cost – Hospital paid for family’s meals and lodging in Hotel – $100,000 detector plate shattered 16 Potential Consequences – – – – Severe injury or disability Prolonged hospitalization Death Even more severe family and caregiver distress – Publicity/damage to reputation – Lawsuit 17 Root cause analysis – This was still a new processdetector/(plate) now tethered to machine with cable – Tech was distracted and reverted back to old habit of pulling machine away quickly – Near misses not taken seriously enough – RN and RT not “engaged” in xray taking process – distracted 18 IMPROVEMENT PRINCIPLES • • • • • The safest thing to do is the easiest thing to do Reduce reliance on memory Use fail-safe systems and forcing functions Standardize and simplify processes Design systems to be resistant to psychological and environmental precursors to error – reduce stress in the environment • Enhance access to complete & timely information 19 How did we fix this? – Met with product rep to discuss safety issue • Sensor added to the storage slot for the detector • Activates switch when in detector in place • Switch must be active to move backwards (i.e. plate must be in place, otherwise machine in very slow mode) – 3 “Must do’s” with EVERY portable x-ray • MUST have second assist with plate/detector removal (RN, RT, MD, Tech) • MUST state out loud “Are we ready to remove the detector?” • MUST have OK from second assist: “Lines and tubes secure. It’s OK to remove the detector.” 20 How did we fix this? – Retraining of all techs • Must pass competency in Simulation center • Emphasized 3 “Must do’s” • 2 techs together for portables for the next 3 weeks – Chief safety officer sent memo to all clinicians and managers: • “Do Not Distract X- Ray Technician” • 3 “Must do’s” with EVERY portable x-ray – Near miss log 21 How do we prevent SRE’s? We can benefit from lessons learned from the adoption of an EMR by recognizing the following: – The hospital is becoming a more and more complex environment – New errors result from the use of complex technology in a very complex work environment – Anticipate the unintended and actively look for problems – End users must be encouraged to report problems found, including near misses SRE’s 22 Evaluation • Who are the customers – External – Internal • What is important to them • How do we measure what is important • How are we doing 5/24/2010 23 Recommendations • Continue to promote safety culture • Safety champions throughout the hospital • Develop internal web page for equipment/technology safety issues – Staff can easily submit information • Near misses • New ideas • Safety issues in general – Reward staff for good ideas 5/24/2010 24 Recommendations • Form committee to evaluate new product or device use – – – – – Quality and Safety officer Unit/department Managers Key unit educators Vendor rep Must include users from all relevant departments 25 Recommendations • Committee Agenda: HLPM of current process HLPM of new process Highlight significant differences Encourage end users to “Anticipate the unintended and actively look for problems” – Consider use of a Simulation Center for training – Establish check-off requirements – Consider use of a buddy system for high-risk procedures for defined training period 26 Resources Required • Staff release time for committee work – Membership of committee changes with each new product/device introduced – Requires back-up coverage – Staff time to complete the analysis and to develop new procedures and training • Staff time for training • Developer time for web page • Vendor contracts to include participation 27 Resources Required • Clinical Simulation Center – use existing equipment for training – SimMan – PediaSim – Neonatal simulator • Consultation with Simulation Center Training Staff 28 Conclusion • Safety focus program on SRE’s has been successful in reducing numbers of surgical events • Current priority is reduction of Product or Device SRE’s • Questions 5/24/2010 29 References Anderson, J. (2010, April 5). HEO MED-INF 404- Session 2- Inpatient Care [PowerPoint slides]. Retrieved from Lecture Notes Online Web site: https://courses.northwestern.edu/ Bobb, A. (2010). Incorporating evidence into decision making [PowerPoint slides]. Retrieved from http://www.himssconference.org/docs/sphandouts/PHAR2.p Cook, J., et al. (2009). Understanding national coverage policies: Navigating the maze of HACs, serious reportable events, and wrong surgical sites. Journal of AHIMA 80, (6), 62-64. Executive Office of Health and Human Services. (2009). Serious reportable events in Massachusetts acute care hospitals: January 1, 2008 – December 31, 2008. Retrieved from http://www.mass.gov/Eeohhs2/docs/dph/quality/healthcare/sre_acute_care_hospitals.rtf General Electric Company. (2007). AMX-4+ mobile x-ray system [PDF Document]. Retrieved from http://www.gehealthcare.com/usen/xr/radio/docs/AMX4pls_brochure.pdf General Electric Company. (2010). Definium AMX 700. Retrieved from https://www2.gehealthcare.com/portal/site/usen/ProductDetail?vgnextoid=d025570d21b30210VgnVCM10000024dd1403RCRD&productid=c025570d21 b30210VgnVCM10000024dd1403 Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21 st century. Retrieved from http://books.nap.edu/openbook.php?record_id=10027&page=R1 Kizer, K. W. & Stegun, M. B. (2005). Serious reportable adverse events. Advances in patient safety (4). Retrieved from http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=aps.section.7695 National Quality Forum (NQF). (2006). National quality forum updates endorsement of serious reportable events in healthcare. Retrieved from http://www.qualityforum.org/pdf/news/prSeriousReportableEvents10-15-06.pdf Patterson, E. S., Cook R.I., & Render M.L. (2002, Sep-Oct). Improving patient safety by identifying side effects from introducing bar coding in medication administration. Journal of the American Medical Informatics Association, 9 (5), 540-53. University of Michigan Health Center. (2008). Clinical simulation center. Retrieved from http://www.med.umich.edu/umcsc/index.html 30