Tina Munzu, 2010. Nurse Management of Heart Failure in a Hospital
advertisement
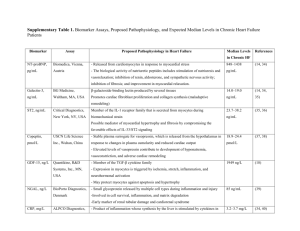
Tina Munzu, RN Alverno College munzutt@alverno.edu home Outcomes By the end of this tutorial the audience will be able to: - Comprehend the basic anatomy and physiology of the heart - Understand and articulate the pathophysiology behind heart failure -Articulate the role of genetics, aging, inflammation and stress on heart failure - Identify the significance of diet, activity, and exercise recommendations and medication therapy in the treatment and management of heart failure - Promote patient adherence to self management of heart failure - Summarize the role of nursing in heart failure management home Before we begin …. This is an interactive Powerpoint. You will with be asked questions and receive feedback with each answer. With the multiple choice questions, select an answer on click on the letter choice for feedback. For the open ended questions click of the slide for the answer. Enjoy learning!!!!! home TABLE OF CONTENTS • Background •Role of aging •The Heart: Anatomy & Physiology •Role of stress • Heart Failure: Definition •Role of inflammation •Left and Right Sided heart failure • Heart Failure Self Management Recommendation: •Medication •Fluid Restriction •Diet •Weight management and exercise •Action plan •Case study •Role of genetics • References home Background -According to the American Heart Association (AHA 2006), nearly 5 million Americans are living with Heart Failure (HF), with 550,000 new cases are diagnosed each year. -HF is the final common pathway for several common illnesses especially hypertension and coronary artery disease. -HF is currently the leading diagnosis and cause of hospitalizations among patients 65 years and older. The costs of healthcare associated with the illness are excessive. (AHA, 2006) home Background: role of nursing … “Stop telling us what to do and teach us how to do it” (anonymous woman with chronic heart failure) Microsoft clip art 2007 -As nurses we have the privilege of being patient educators -Nurses assess a patient’s cognitive function and knowledge of heart failure to help them develop essential skills to manage their disease. -Our goal is to partner with patients for better outcomes. home The Heart: Anatomy and Physiology Blood from lungs Pulmonary Artery Pulmonary Vein Left side of the heart (atrium ventricle) Right side of the heart (atrium ventricle) Aorta Vena Cava Rest of the body (organs and tissues) Retrieved 4/12/10 from http://www.biomaterials.org/SIGS/Cardiovascular/images/cv_anatomy _heart.jpg home PHYSIOLOGY OF THE HEART Microsoft clip art 2007 To increase cardiac output in response to body needs the heart depends on 4 factors: (i) Preload (ventricular filling), (ii) afterload (degree of resistance of blood ejection from the heart), (iii) cardiac contractility, (iv) the heart rate Preload: represents the blood volume in the heart chambers just before a contraction. In ventricular diastolic dysfunction often seen in heart failure, the heart is stiff and thickened from ventricular hypertrophy and cannot relax completely. This reduces preload as the ventricles do not fill adequately with blood volume. Afterload: represents the pressure/tension that the left side of the heart, primarily the left ventricle, must generate in order to contract and force blood into the aorta and the rest of the body. Elevated systemic blood pressure and aortic valve disease increase afterload as the left ventricle must generate a greater tension to pump blood out of its chamber which can lead to heart hypertrophy. All else being equal as afterload increases, cardiac output decreases. (Porth, 2005) home PHYSIOLOGY OF THE HEART Microsoft clip art 2007 Cardiac contractility: refers to the ability of the heart to change its force of contraction. It is heavily determined by factors that mediate actin and myosin interactions in myocardial cells. The concentration of calcium in the cell is one of the most significant biochemicals that affect this interaction. The higher the intracellular calcium, the higher the contractility force. The sympathetic nervous system with the release of epinephrine and norephinephrine promotes increased intracellular calcium and thus increased cardiac contractility. Heart rate: refers to the frequency with which the heart beats/contracts to force blood out to the rest of the body’s tissues. As the heart rate increases, generally so does cardiac output because more blood is being pumped out in a minute. However, if the heart were to continue beating at these higher rates, as seen in ventricular tachycardia, it translates into lesser volume to pump out since the ventricles are not allowed enough time to fill up before they contract again. This could then result in a decreased cardiac output. (Porth, 2005) home Question: Identify the factors that affect the heart’s ability to meet the body’s needs for oxygen and nutrients. 1. Preload Correct! Volume work imposed on the heart before it contracts 2. Afterload Right! The pressure the left ventricle must overcome to force blood into aorta 3. Cardiac contractility Correct! Ability of the heart muscle cells to contract. 4. Heart rate Correct! The frequency with which the heart ejects blood. Affects preload as faster heart rates means less filing time for the ventricles home Question: True or false: Everything else equal there is an inverse relationship between afterload and cardiac output. TRUE FALSE Correct! The higher the afterload, the lower the cardiac output overtime as the heart is overworked and cannot meet body needs. Try again. With increased afterload the heart must work harder to meet body needs. The higher the heart rate the higher the preload. TRUE FALSE Correct! Preload corresponds to the filling time of the heart chambers. The faster the heart beats the less time it has for the ventricle to fill with blood. Wrong! Remember that preload corresponds to the filling time of the heart chambers. home What is Heart Failure? Definition: Heart failure is the inability of the heart to pump blood adequately to the tissues 2 main categories: 1) Systolic dysfunction: Experienced during the pumping/contraction phase, it involves a decrease in cardiac contractility and ejection fraction. Diseases that affect the contractile performance of the heart (MI and cardiomyopathy) or that cause increase pressure overload (hypertension and Valvular stenosis) are most responsible for systolic dysfuntion 2) Diastolic dysfunction: Long standing hypertension is usually the cause of diastolic dysfunction. Over time, the heart muscles stiffen and become less flexible. The heart is no longer able to stretch effectively and fill with blood. (Porth, 2005) home www.med.uc.edu/kranias/heart_failure.htm Systolic and Diastolic Heart Failure Retrieved from www.med.uc.edu/kranias/heart_failure.htm * Evaluated by echocardiogram. Normal ejection fraction is ≥ 50% home Signs and Symptoms of HF Left heart failure Right heart failure Congestion of peripheral tissues Edema and ascites Liver congestion impaired liver function GI tract congestion Pulmonary congestion Cardiac output Activity intolerance Impaired digestion Impaired gas exchange Pulmonary edema Dyspnea cyanosis Cough (w/ frothy sputum) orthopnea Anorexia, Weight loss, cachexia home Question The primary most significant contributing factor to heart failure is: A) Infection Try again! B) Uncontrolled hypertension Correct home C) Mental illness Try again! Question – Click on the screen below each question for answers Take a guess! What percentage of blood is pumped out of the heart with each heart beat? 60% What is the cardiologic diagnostic test used to estimate a patient’s EF? An ECHOCARDIOGRAM home Common Factors that Precipitate HF Hospitalization - Noncompliance with medical regimen, sodium and/or fluid restriction, - Acute myocardial ischemia - Uncorrected high blood pressure - Atrial fibrillation and other arrhythmias - NSAIDS (Nonsteroidal anti-inflammatory drugs) - Excessive alcohol, drug use - Infections (e.g., pneumonia, viral illnesses) home Case Study Ms. M is an 80year woman with a history of hypertension and occasional angina. She presents to the ER with shortness of breath that has gotten worse over the last three days especially with activity. Ms. M reports an inability to sleep at night due to a non productive cough and constantly having to urinate. She sleeps with 2-3 pillows and lately finds herself waking up gasping for air. She presents with severe swelling in her legs. Her admission vitals were: blood pressure 175/75, heart rate 102bpm, respiratory rate 22, temperature 98.5 and pulse oximetry 91% on 2L nasal cannula. Her EKG and chest xray show left ventricular hypertrophy. home Question Identify her significant risk factors plus signs and symptoms of HF -Age (80yrs old) -History of hypertension and angina - Shortness of breath - Activity intolerance - Constant urination (probable side effect of medication) - lower extremity edema -Tachypneic and tachycardia - Cardiac remodeling (left ventricular hypertrophy) home Role of genetics in HF -Researchers are beginning to trace the etiology of HF partly to genetics -The fundamental basis for heart cells are 1) the generation of a contractile force, 2) transmission of this force throughout. -Mutations in the sarcomere proteins of muscle cells have been linked to HF. These mutations - cause uncoordinated heart contractions increased energy consumption - cause changes in calcium homeostasis apoptosis and fiber formation inflammation - However, more research is still on the way to identify exactly the direct role genetics has to play. (Morita et al, 2005) home Modified from Google page http://www.scq.ubc.ca/wpcontent/dna.gif Effects of Aging -HF is a progressive disease and develops over time; hence it is most common with aging. It affects an individual’s quality of life and promotes early mortality. - Aging causes changes in the heart and in the blood vessels: - thickening of the heart’s walls - increased deposits of lipofuscin: heart valves thicken and become stiffer increased workload of the heart - the aorta becomes thicker, stiffer and less flexible increased blood pressure which makes the heart work even harder muscle hypertrophy (Medline Plus, 2008) home Stress Response The body’s systemic response to stress involves baroreceptor reflexes and the reninangiotensin-aldosterone (RAAS) mechanism. Heart failure Decrease cardiac output ( the heart is less capable to pump blood (volume) around to the tissues) HF = Decreased CO Angiotensin II = vasoconstrictor and aldosterone production Sodium and water retention Increased BP Decreased Blood volume to kidneys Converted in the lungs to Angiotensin II by ACE Increased CO and coronary perfusion Kidneys release renin in response to low BP Converts Angiotensinogen Angiotensin I Long term increased workload by the heart worsening EF HF Start here (Angerio, 2005) home stress response cont’d Stress (Decreased Cardiac Output) “Fight-flight” hormones (epinephrine & norepinephrine) are released into bloodstream Increase heart rate. Heart contracts and pumps more forcefully to compensate for low cardiac output Temporary solution. Overtime, if this is sustained, it puts more demand on an already weak heart. Leads to further deterioration of the heart worsening heart failure (Angerio, 2005) home STRESS CONTINUED Prolonged compensatory mechanisms by the RAAS and norepinephrine system lead to deterioration and remodeling of heart muscles Normal Heart MI, HTN etc Compensatory mechanisms Overtime permanent heart remodeling Decreased CO and increased mortality (Angerio, 2005) home Role of Inflammation in HF - One belief is that the progression of HF is heavily influenced by inflammation. -Proinflammatory cytokines ( CRP, TNF, interleukin 6) produce toxins that directly affect the heart and peripheral vasculature. - In response to cardiac stress such as a myocardial infarction (MI), increased pressure or volume overload, myocardial cells produce cytokines especially TNF Secretes more cytokines Tissue Release of Attract monocytes -> Releases damage, cytokines mature into macrophages toxins infection (TNF, IL 6) Decreased CO - HF Increased workload on heart to meet body needs Remodeling (hypertrophy, dilation) home Kills cardiomyocytes TUMOR NECROSIS FACTOR (tnf) -TNF is the most known pro-inflammatory cytokine that contributes to HF: -Elevated levels of TNF in the blood are a good indicator of HF prognosis: - instigates cardiomyocyte hypertrophy thickening and stiffening of heart vessels -triggers apoptosis (cell death) of myocytes less contractile force of the heart decreased cardiac output - blunts adrenergic (epinephrine and norepinephrine) responsiveness prevents initial activation of compensatory mechanism -induces left ventricular dilation cardiac muscle stiffening -promotes progression towards muscle wasting (cachexia) Alcohol and smoking release toxins that induce inflammation!!!!! Copied from http://z.about.com/d/chemistry/1 /0/r/d/flamingdrinks.jpg home The Nursing Impact Focus on Self- Management Education “Stop telling us what to do and teach us how to do it” (anonymous woman with chronic heart failure) - Self care maintenance involves taking all medications as prescribed, following a low salt diet, exercising, watching out for any signs and symptoms such as increased swelling, cognition changes or shortness of breath. -Although knowledge of illness is the basis for self management, it is not sufficient. Patients must develop skill to apply the knowledge. -Our education goal is to transition from an authoritative/prescriptive model of teaching towards a more collaborative skill building model that will promote better selfmanagement by patients home Medication Education and Compliance Microsoft clip art 2007 - Common reasons for medication noncompliance include: - cost - lack of understanding of discharge instructions - not being convinced of the effects and usefulness of the medication. -At discharge only 80% of patients with a prescription for an ACE inhibitor filled their prescription during the 30days after discharge ** NSAIDS: Discourage NSAID use in HF patients (Butler ,2004). Microsoft clip art 2007 home Medication Education and Compliance -Educate on the usefulness of ACE/ARBs and beta blockers in HF management. -For the most part these medications work best when combined with one another. Patients may sometimes be on up to 4 different combinations and must understand their usefulness and mechanism as related to their particular condition to ensure compliance -Encourage patient to use system, such as pill boxes and alarms, to help remind patients when to take their medications Microsoft clip art 2007 home COMMON HEART FAILURE MEDICATIONS Drugs Effects Examples ACE (angiotensin-converting enzyme) Inhibitors Primary drug of choice: block angiotensin II and aldosterone production, dilate vessels, prolong life *cough* Lisinopril, enalapril, captopril Angiotensin II receptor blockers (ARBs) Similar to ACE inhibitors. More tolerable for most patients because has no cough side effects. Usually used together with ACE inhibitors Valsartan, losartan Diuretics Helps kidneys eliminate salt and water decreased fluid volume to relieve the heart’s workload Furosemide, HCTZ Beta-blockers Slows heart rate and blocks excessive heart stimulation such as seen in heart arrhythmias. Usually works well with ACE inhibitors for added benefits Metoprolol , coreg Anticoagulants Helps prevent formation of blood clots especially if blood is pulling in heart chambers such as seen in atrial fibrillation Lovenox, heparin home Question What are the 2 most common drug groups used to manage HF A) ACE inhibitors & NSAIDS B) ACE inhibitors and ARBs Wrong. NSAIDs are contraindicated in HF patients Correct! C) ARBs and nitroglycerin D) Oxygen and diuretics Nitroglycerin is not 1st drug of choice Wrong. Try again home Question On review of Ms M’s (case study) home medications you discover that she was recently started on 5mg lisinopril daily by her primary care physician. She has also been taking 160mg of diovan daily and 40mg of lasix daily. Which medication might be responsible for her cough? A) Lisinopril Correct. Side effect of most ACE inhibitors B) Valsartan Wrong! Pts usually tolerate ARBs better due to lack of coughing side effects home C) Furosemide Try again! Fluid Restriction - General advice to the elderly and public is to maintain hydration especially when ill; thus HF patients often think it helpful to drink loads of fluid. - Some patients on diuretics believe they have to drink to replenish the fluids being lost as urine. - Fluid overload results in increased edema, which increases the workload of an already compensating heart and may lead to difficulty breathing. - United States HF guidelines currently restrict fluid intake to 1.5-2L per day in patients with severe symptoms and hyponatremia. - Encourage patients to weigh themselves daily for early detection of fluid retention. -1 cup = 8 ounces = 240 ml Microsoft clip art 2007 *Importance of daily weight is not for monitoring change in adipose (fat) tissue but instead fluid status* (Riegel et al, 2009) home Question When are HF patients most encouraged to weigh themselves? A) In the Am after breakfast B) At bedtime after taking lasix Try again! Lasix that late will keep them up all night C) On rising in the AM after urinating Correct! home ! Diet - In HF, diet and weight management are very important. Microsoft clip art - HF guidelines recommend 2-3g of sodium per day. Due to its water retaining capabilities excess sodium consumption contributes significantly to HF exacerbation and hospitalization. -Partner up with the nutrition/dietary departments to create learning opportunities for patients where they can learn and understand how to read food labels. - Discourage foods believed to be proinflammatory such as simple sugars, saturated fats and alcohol. - Encourage foods that counteract inflammation such as walnuts, fruits and vegetables, garlic, ginger and sunflower seeds according to patient preferences. (Riegel et al, 2009) home Exercise and Weight Management -The benefits of exercise are extensive. - Exercise is a great way to improve circulation and decrease inflammation. Following an exercise regimen to help maintain ideal body weight helps reduce the workload on the heart. - Exercise: • improves appetite and mood • helps to obtain a more restful sleep • reduces stress • controls blood pressure and cholesterol Microsoft clip art 2007 • eases shortness of breath - The goal is to partner with the patient to develop an exercise plan that fits well into their daily life, budget and their environment. * Weight loss is encouraged if BMI is >40kg/m2. If <30kg/m2 discourage. Encourage patient instead to monitor for loss of appetite, unexpected weight loss and muscle wasting (= symptoms of cachexia). (Riegel et al, 2009) home Question: Ms. M’s echo results come back. She has an EF of 20% and is afraid that her heart will “stop pumping well” and she will get short of breath again. What advice can you give her as to how to manage her heart failure? Weigh yourself daily in the AM Yes. This will help her identify if she is retaining any fluids and how much. Encourage her to keep a journal Raise feet on pillows and wear ted stockings Yes. To help manage any swelling Limit your salt intake. Use spices for food seasoning Take your medications as prescribed. Yes. Salt makes her retain water which increases the workload of the heart Yes. To help manage and prevent exacerbation Drink loads of fluids No. Too much fluids put more pressure on an already struggling heart exacerbation home Stay current on your seasonal vaccines. Follow up with doctor regularly. Yes. Prevents infection which triggers the inflammation process. Action Plan and MD follow up – Use this to help guide you to what action to take! Green • No change in symptoms • No cough or wheeze • Breathing is good • Usual strength and activity • Weight is stable Yellow • Weight gain of more than 3 pounds in 1-2 days • Weight gain of more than 5 pounds in 1 week • Have to sleep sitting up • Start coughing at night • Notice swelling in your ankles or any part of your body • Have pain or bloating in your stomach and lose your appetite • Become tired faster or feel yourself losing energy • Wheezing (noisy breathing) • Have side effects from your pills • Weight loss of more than 5 pounds in 2 days Red • Trouble breathing • Pain or tightness in chest • Dizzy spells or feel faint • Feel anxious or like something bad will happen home Green means GO – You’re doing fine stay on treatment and active 2. Yellow means Caution – Be alert to changes Call your MD within 24 hours Red means Stop – Call for help right away – 911 if emergency * Modified with permission from Aurora HF discharge education packet (2010) References: Riegel B, Moser D, Anker S, et al. AHA state of the science: Promoting self-care in persons with heart failure. Circulation. 2009;120:1141-1163 Dickson, V. V., Riegel B. Are we teaching what patients need to know? Building skills in heart failure self-care. Heart & Lung. 2009;38:253-262 Albert N., Fonarrow G, Abraham W, et al. (2007) Predictors of delivery of hospital-based heart failure patient education: A report from optimize-hf. J Cardiac Failure 13(3) 189-198. Freeman. G, Murray D. Proinflammatory cytokines; predictors of a failing heart? Circulation. 2003;107:1460-1462 Libera L, Vescovo G. (2004) Muscle wastage in chronic heart failure, between apoptosis, catabolism and altered anabolism: a chimaeric view of inflammation? Clinical nutrition and Metabolic Care. 7:435-441 Mueller C, Kilian K, Christ A, et al. (2006) Inflammation and long-term mortality in acute congestive heart failure. American Heart Journal 151:845-850 home References: Angerio A. (2005) The role of endothelin in heart failure. Critical Care Nurse 28(4)335-359 Medical News Today. The genetic background of heart failure and the role of hypertension. Retrieved April 4, 2010 from http://www.medicalnewstoday.com/printerfriendlynews.php?newsid=105716 Medline Plus. Aging changes in the heart and blood vessels. Retrieved April 7, 2010 from http://www.nlm.nih.gov/medlineplus/ency/article/004006.htm Chantier P, Clements R et al. (2006) Congestive heart failure: extent of cardiac functional changes caused by aging and organ dysfunction. Heart 92:686-688 Alexander J, Alexander K, Kong D et al. (1998) Session highlights from the AHA scientific session: november 7-12, 1997. American Heart Journal 135(1) 169-170 Berra K, Miller N. (2009) Inhibiting the renin-angiotensin system: why and in which patients. American Academy of Nurse Practitioners 21:66-75 Morita H, Seidman J, & Seidman C. Genetic causes of human heart failure. Journal of Clinical Investigation. 115:518-526 (2005). home Contact Information Tina Munzu MSN Alverno College Student munzutt@alverno.edu home