Palliative Care in our Region - Department of Family Medicine
advertisement

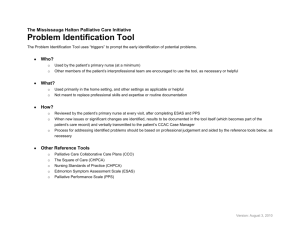
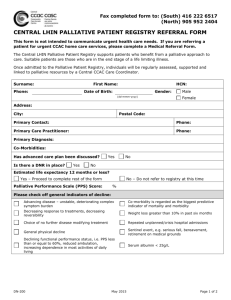
Palliative Care in Kingston and the SE LHIN Dr. Natalie Kondor DFM Grand Rounds Jan 20 2015 Outline What is palliative care? Why is palliative care important? Trends in palliative care provision Regional and local resources for palliative care provision FAQs What is Palliative Care? Palliative care is a philosophy of care that aims to help individuals and families to: Address physical, psychological, social, spiritual and practical issues Prepare for and manage end of life choices and the dying process Cope with loss and grief Treat active issues and manage symptoms Prevent new issues from occurring Promote opportunities for meaningful and valuable experiences Why do we need palliative care? 1900 Average age of death 46 years Usually a rapid death Leading causes: infectious disease, childbirth, accidents Sudden Death High Death Low 2015 Average age of death 85 Only 5% die sudden deaths, 95% decline over time 2-4 years of decline High High Cancer Function Low death Time Dementia/Frailty Function Organ System Failure Function High Time Low death Time death Low Time Our Reality By 2036, seniors will account for 23-25% of the total population 32 % of Canadians suffer from a chronic illness • 39% have a sufferer in their immediate family 74% of seniors have one or more chronic conditions 24% of seniors have three or more chronic conditions Chronic diseases account for 70% of all deaths Palliative Care – Not Just End of Life Care The Need for Palliative Care ESAS symptom profile for cancer patients All Disease Sites, FY 2013/14 80% 70% 12.5% 8.2% 60% 50% 40% 6.6% 14.0% 6.4% 4.9% 14.2% 6.1% 12.8% 39.9% 39.6% Tiredness Wellbeing 5.0% 10.7% 12.1% 1.9% 4.9% 20% 34.3% 27.4% 32.1% 31.2% 22.6% 10% 0% 21.9% 6.3% 11.1% 30% 22.8% Anxiety Depression Drowsiness Lack of Appetite 1 - 3 (Low Severity) 26.8% 17.1% Nausea Pain 4 - 6 (Moderate Severity) Shortness of Breath 7 - 10 (High Severity) Benefits of Earlier and Integrated Palliative Care Leads to better outcomes for Patients & Families: • Reduced symptom burden • Less anxiety and depression • Less caregiver burden • Better quality of life • Less aggressive treatments • More appropriate referral to and use of hospice • Lower health care costs Smith et al., 2012; Temel et al., 2010; Bakitas et al., 2009; Myers et al., 2011; Zimmerman et al 2013 Benefits of Earlier and Integrated Palliative Care - Improved Survival Longer and better survival Better understanding of prognosis Less IV chemo in last 60 days Less aggressive end of life care More and longer use of hospice $2000 per person savings to insurers and society Temel J, et al. NEJM 2010; Temel J, et al, JCO 2011; Greer, et al. Proc ASCO 2012 Current state of Palliative Care in Canada Only 16-30% of Canadians have access to formalized palliative/end-of-life care services At least 25% of the total cost of palliative care is borne by families Approximately 70% of deaths occur in hospital • 40% of terminally ill cancer patients visit the emergency department within the last 2 weeks of life • 41% of long term care home residents have at least one hospital admission in their last 6 months of life 96% of Canadians believe it is important to have conversations with their loved ones about their wishes for care • 34% have actually had a discussion • 13% have completed an Advanced Care Plan CHPCA Fact Sheet – Hospice Palliative Care in Canada (2014) Building capacity for palliative care A palliative approach to care should be practiced by all providers caring for people with life-threatening illnesses o Primary, Secondary and Tertiary care settings o Community settings Not a “one size fits all” approach, but key common elements o Person-centred care o Inter-professional team o Single access point o 24/7 care to ensure continuity & coordination o Building community capacity Regional Implementation – Results in Alberta Edmonton & Calgary: 1993 to 2000 Hospice care Results • Health system costs reduced Costs for last year of life • Acute care costs reduced (from 83% to 63% ) Services Introduced: Hospices Community consult teams • In-hospital days reduced (from 39 to 27 days) Acute care • # of deaths in acute hospitals reduced • # of home deaths increased Fassbender K et al. Utilization and costs of the introduction of system-wide palliative care in Alberta, 1993 to 2000. Palliative Medicine. 2005:19-513-520 Regional Implementation – Results in Ontario Pockets of palliative care excellence in rural & urban areas Community capacity building initiatives across Ontario have created innovative programs A recent analysis of community based, specialist palliative care teams found: o Reduced acute care use o Reduced hospital deaths at the end of life What’s Next in Ontario The Provincial HPC Steering Committee & the Clinical Council are now active HPC now a priority for system transformation in all LHINs All LHINs have committed to: o 10% reduction in one or more of the following areas: Overall palliative-related ALC days Inpatient days per capita among patients that died in hospital; Palliative-related avoidable hospitalizations (repeat ER visits/readmissions) o Implementing regional HPC programs Work underway to develop palliative care indicators Palliative Care In Our Region - SE LHIN Regional Priorities Strengthen capacity of local communities in providing hospice palliative care • Increase capacity in providing palliative care in all care settings especially primary care • Support the uptake of common palliative care plans, guidelines and tools • Promote use of shared information among care settings Create regional mechanisms to enable early identification of patients who would benefit from hospice palliative care • Implement the adapted Gold Standards Framework for Early Identification Increase the understanding and implementation of Health Care Consent and Advance Care Planning Strengthen caregiver support including bereavement Palliative Care in Our Region Resources Inpatient Consult Services Community Palliative Care Services • CCAC – Nursing, PSW, SW, OT, PT, Dietician • Physicians Inpatient Palliative Care Units • SMOL PCU, Brockville PCU Community Hospices • Inpatient, ambulatory Outpatient Ambulatory Clinics • KRCC, Advanced dyspnea management clinic Hospice Palliative Care Nurse Practitioners Community Palliative Care Services For patients with PPS < 50% FamMD makes CCAC referral FamMD +/- colleague follows patient at home and provides 24/7 call coverage FamMD refers to community palliative care physician for concurrent care or transfer of care Patients are seen same day to within 2 weeks depending on urgency On referral, helpful to indicate whether you are requesting community, PCU assessment or clinic visit. If unsure, feel free to phone to suss out which might be most appropriate (548-2485) Helpful to indicate urgency, PPS, decline in PPS, symptom issues, whether want concurrent vs. transfer of care Palliative Care Unit – at SMOL 13 beds – 10 private and 3 semi-private rooms All referrals are to go through the palliative care office and are directed to the intake physician who manages a running list Wait time often less than 2 weeks, can be as soon as same day Patients at home get priority over patients waiting at KGH Prognosis less than 3 months If survive longer, may get transferred to LTC Palliative Care Clinic at KRCC Referrals from specialists (often oncologists), Family MD For symptom management for ambulatory patients (PPS =/>50%) For cancer-related symptoms or symptoms related to cancer therapy Patient continues to receive primary care from Family MD Palliative MD is generally 1st contact regarding symptom management issues Hospice Palliative Care Nurse Practitioners “Would you be surprised if this patient were to die in the next 6-12 months?” No What is your comfort level in providing palliative care at home for this patient? Yes Do not refer at this time I am comfortable and able to provide home palliative care independently I would like to provide home palliative care but lack time and/or comfort/skill level to do so independently I do not wish and /or am not able to provide home palliative care Do not refer at this time Consider referral to either: 1. HPC NPP for shared care where you /your physician group provide(s) call coverage or 2. Queen’s Community Palliative Medicine for consultation or shared care with call coverage to be determined Consider referral to Queen’s Community Palliative Medicine to assume care and provide call coverage Some FAQs What is a PPS and why is it important? Do I have to have CCAC involved to care for my patient at home? Yes – the short answer Why: CCAC is the “umbrella” organization that designates one of the nursing agencies to be the first call to patients/families Coordinate and provide OT/PT/SW support, equipment (hospital beds, nebulizer machines etc) Supplies needles, syringes, dressings, sc sets, catheters, some personal care items, etc. Patient not eligible for CADD pumps or SRKs without CCAC involvement Do I have to have CCAC involved to care for my patient at home? How to get CCAC support: Fill in a CCAC Service Requisition Can simply write: “please see for palliative symptom assessment and management” and the ball will start rolling How many hours of CCAC PSW and nursing support can my patient receive? Not 24/7 bedside care! CCAC’s “End-of-Life” Program PPS less than 30 Life expectancy/need for 30 days or less PSW - Up to 360 hrs allotted for 30 days or 12 hrs per day Nursing – visits as often as needed up to 4 times per day Option of hiring PSW support and nursing privately but lack of manpower and expensive $60-80/hr for nurse $30-40/hr for PSW Compassionate Care Benefits Family member at risk of dying within 26 weeks Doctor completes application form EI program Benefits for up to a maximum of six weeks To be eligible for compassionate care benefits, you must be able to show that: your regular weekly earnings from work have decreased by more than 40 percent; and you have accumulated 600 insured hours of work in the last 52 weeks, or since the start of your last claim (this period is called the qualifying period). The basic benefit rate is 55 percent of your average insurable earnings, up to a yearly maximum insurable amount ($48,600 in 2014). This means that, in 2014, you can receive a maximum payment of $514 per week. Compassionate Care Benefits Do I have to refer my palliative patient at home to the community palliative care team? No! If Dr. You is comfortable with and readily available to provide symptom management and end of life care to your patients at home, you can do it You or a colleague covering for you must be available to be called 24/7 The Queen’s palliative care team has a physician available to call for advice 24/7 (5482485 or ask for the PC doctor on call through the KGH operator if after-hours) Why do referrals to community palliative care need to come from the Family MD? Specialists (eg. CTU resident discharging patient home, oncologist at KRCC) can refer patient to community palliative MD but must get confirmation of agreement (verbal or in writing) from patient’s Family MD To ensure Family MD is aware of situation and give opportunity for Family MD to decide whether prefer they vs. community PC follow pt at home If a patient does not have a Family MD, any MD can refer to community palliative care What is a Symptom Response Kit and how do I order one? What is a Symptom Response Kit and how do I order one? Palliative Care Facilitated Access List Can Bloodwork be done at home? Yes, but not urgent b/w Order on LifeLabs req and write HOME VISIT in the “additional clinical information” area LifeLabs will come to patient’s home usually “within the next week” – may be as soon as next day depending on geography Results available day after b/w is done Costs the patient approximately $35 per visit Occassionally home care nurse can do b/w with an order but only if b/w obtained via a PICC (generally don’t do peripheral venipuncture anymore) and if b/w taken immediately to lifelabs by nurse or family member Can my patient receive IVF or blood transfusions at home? Patients can receive fluid hydration at home – set up by the nurses through CCAC Requires faxed order to CCAC NS is easiest to obtain (vs. 2/3 1/3, NS with KCl, etc) IVF – can order if pt has IV access eg. PICC or Port-aCath. CCAC provides pump for administration Hypodermoclysis – fluids run sc through a sc set by gravity, generally overnight/over 8 hours Blood transfusions cannot be done at home, can be done through ER or KRCC as outpatient (with pre-orders) What is a Yellow Folder? SE LHIN initiative for “expected death at home” Contains information on who/when to call for what situation Contains SRK Rx Contains DNR confirmation form What is a DNR Confirmation Form and does my DNR patient need one? Does an MD need to pronounce and complete the death certificate? In Ontario, in the case of an expected death and the death is caused by the expected cause then a nurse (RN or RPN) may pronounce A physician or NP’s order is required for this to occur and the funeral home should be aware and agreeable Once pronouncement has happened, the funeral home will retrieve the body with or without the death certificate A physician or NP is required to submit an original copy of the death certificate to the funeral home as soon as possible (usually within 24 hours) Summary Palliative care is growing in scope and importance By 2036, 25% of Canadians will be seniors and many of them will need some form of palliative care Tools and resources are readily available for primary care practitioners to provide this care to their patients