020112.RVanDyke.LiverPhysiology - Open.Michigan
advertisement

Author(s): Rebecca W. Van Dyke, M.D., 2012
License: Unless otherwise noted, this material is made available under the terms
of the Creative Commons Attribution – Share Alike 3.0 License:
http://creativecommons.org/licenses/by-sa/3.0/
We have reviewed this material in accordance with U.S. Copyright Law and have tried to maximize your ability to use,
share, and adapt it. The citation key on the following slide provides information about how you may share and adapt this
material.
Copyright holders of content included in this material should contact open.michigan@umich.edu with any questions,
corrections, or clarification regarding the use of content.
For more information about how to cite these materials visit http://open.umich.edu/education/about/terms-of-use.
Any medical information in this material is intended to inform and educate and is not a tool for self-diagnosis or a replacement
for medical evaluation, advice, diagnosis or treatment by a healthcare professional. Please speak to your physician if you have
questions about your medical condition.
Viewer discretion is advised: Some medical content is graphic and may not be suitable for all viewers.
Attribution Key
for more information see: http://open.umich.edu/wiki/AttributionPolicy
Use + Share + Adapt
{ Content the copyright holder, author, or law permits you to use, share and adapt. }
Public Domain – Government: Works that are produced by the U.S. Government. (17 USC § 105)
Public Domain – Expired: Works that are no longer protected due to an expired copyright term.
Public Domain – Self Dedicated: Works that a copyright holder has dedicated to the public domain.
Creative Commons – Zero Waiver
Creative Commons – Attribution License
Creative Commons – Attribution Share Alike License
Creative Commons – Attribution Noncommercial License
Creative Commons – Attribution Noncommercial Share Alike License
GNU – Free Documentation License
Make Your Own Assessment
{ Content Open.Michigan believes can be used, shared, and adapted because it is ineligible for copyright. }
Public Domain – Ineligible: Works that are ineligible for copyright protection in the U.S. (17 USC § 102(b)) *laws in
your jurisdiction may differ
{ Content Open.Michigan has used under a Fair Use determination. }
Fair Use: Use of works that is determined to be Fair consistent with the U.S. Copyright Act. (17 USC § 107) *laws in
your jurisdiction may differ
Our determination DOES NOT mean that all uses of this 3rd-party content are Fair Uses and we DO NOT guarantee
that your use of the content is Fair.
To use this content you should do your own independent analysis to determine whether or not your use will be Fair.
M2 GI Sequence
Liver Physiology
Rebecca W. Van Dyke, MD
Winter 2012
Learning Objectives
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
At the end of this presentation students should be able to:
1.
Describe the basic organization of the liver cell plate and its functional
consequences:
a.
Blood supply
b.
Configuration of hepatocytes
c.
Configuration of other liver cells
d.
Concentration gradients in sinusoidal blood.
2.
Describe the basic physiological processes the liver utilizes to accomplish
function:
a.
transport
b.
metabolism
c.
biotransformation
d.
synthesis
e.
secretion
3.
Be able to give examples of the consequences of liver damage on above
processes.
4.
Be able to give examples of possible consequences of liver disease/injury on
liver barrier function and hepatic regeneration.
Industry Relationship Disclosures
Industry Supported Research and
Outside Relationships
• None
Cystic artery
sole supply to bile duct
Anatomy of Liver Acinus
bile duct
hepatic artery
portal vein
blood flow
bile
portal triad
sinusoids
Michigan Histology Collection
central vein
Dual Blood Supply of Liver
liver
Hepatic artery: 20%
Portal vein: 80%
spleen
pancreas
Regents of the University of Michigan
Liver has dual blood
supply:
80% portal vein
20% hepatic artery
What are the Functional
Consequences of….?
• Increased vena caval pressure/hepatic
vein obstruction?
• Decreased hepatic artery blood flow?
and/or
Decreased portal vein blood flow?
• Effects on the bile duct?
Budd-Chiari Syndrome: Obstruction of
the Hepatic Vein(s)
Normal
Budd-Chiari
Hemorrhage in
pericentral area;
hepatic vein
obscured
Dilated upstream
sinusoids;
atrophic/ischemic
hepatocytes
Decreased inflow: ischemic infarction
Bile Duct
• Sole blood supply to the bile duct is through the
hepatic artery via the cystic artery
• Reduced blood flow through the hepatic artery
causes ischemic injury to the extrahepatic bile
ducts
• Ischemia or damage to the bile duct often leads
to injury, fibrosis, stricture
Liver Cell
Anatomy:
Consider
functional
consequences
Image showing relationship between sinusoid,
sinusoid lining cells, and hepatocyte removed.
Scanning Electron micrograph of Liver
Cells in Liver Sinusoid
American Gastroenterological Association
Functional Consequences of
Fenestrated Sinusoidal
Endothelium?
Space of Disse
Other serum
proteins
Albumin
Kupffer Cell
Tissue macrophage
Filtration device
bacteria, endotoxin
Releases inflammatory mediators
that influence hepatocytes
positively or negatively
Looking Down a Sinusoid at a Kupffer Cell
Poised to Grab Passing Bacteria
Kupffer cells (red)
Ito Cell/Fat-storing Cell
Rare cell, located in sinusoids under
endothelium
Stores lipophilic materials such as
Vitamin A
Stimulated by chronic inflammation/alcohol
converts to myofibroblast
produces collagen and extracellular matrix
Responsible for much of the excess fibrotic
material in cirrhosis
Ito Cell (Fat-storing Cell) on a Sinusoid (S)
Hepatic Stellate (Ito) Cell
(arrows)
The Liver:
The Body’s Refinery
Defects in Glucose Metabolism
in Liver Disease
Acute liver failure:
Hypoglycemia
(rapid neuronal death)
Chronic liver disease:
Insulin resistance
and diabetes
(unknown mechanism)
UREA
Fatty acid metabolism within hepatocytes
albumin
FABP
hepatocyte
free fatty acid pool
to mitochondria
for energy
cholin
e
esterification to
TAG
excess
glucose,
amino acids
Apo
B100
VLDL
cholesterol
esters
Regents of the University of Michigan
Greater Role of the Liver in Production
and
Metabolism of Lipoproteins and Lipids
LDL
Cholesterol
Gut
HDL Chol.
Liver
Chylomycrons
TG
CM remnants
TG
VLDL-TG
BILE
Cholesterol
Bile acids
Phospholipids
Fatty Liver with Inflammation
Liver as Protein Synthetic Machine
Vena cava
systemic outflow
Liver synthesizes and secretes:
Lipoproteins
Albumin
Clotting factors
Anti-proteases (1-anti-trypsin)
Fibrinogen
Complement factors
Ceruloplasmin
Transferrin and other binding
proteins
Hepatic artery
carries arterial
blood with blood
proteins
Portal vein carries
venous blood from
intestine, spleen and
pancreas
Protein Secretion Defects in Liver Disease
Example
Clinical Consequence
Albumin
Decreased plasma oncotic pressure/
edema
Decreased binding of hydrophobic
compounds
Clotting factors :
Decreased factors II, VII, IX and X
Increased bleeding
Fibrinogen
Decreased fibrin formation in clotting
Defects in Protein Synthesis/release also cause liver disease:
Alpha1-Anti-trypsin Deficiency
Image of pathophysiology of alpha-1anti-trypsin deficiency removed
PAS Stain Showing Retained Globs of Mutant
Alpha1 Anti-trypsin Protein in Hepatocyte ER
Lipoprotein release: another liver
synthetic function
VLDL: a combination of fat and
protein
The unique position and
blood supply of the liver
also affect liver physiology
Anatomy of Liver Acinus
bile duct
hepatic artery
portal vein
blood flow
bile
portal triad
sinusoids
Michigan Histology Collection
central vein
Consequences of Changes in
Hepatic Blood Flow and/or
Oxygen Delivery?
Peri-central vein (hepatic vein) clotted off with
ischemic damage to hepatocytes
Peri-central
ischemia
HV clot
Peri-portal
normal tissue
Not all liver cells are alike.
Substances found in higher concentrations in the portal vein
•Albumin
•CPS
•FABP
•HMG CoA
Substances found in higher concentrations in the hepatic vein
•P450s
•ADH
•C7H
•Cysteine
•GR
•Gluatamate
2G
•GS
•GLUT-1
-KG
Periportal Necrosis from Allyl Formate
Toxicity
HV
PV
Pericentral Necrosis from Carbon
Tetrachloride Toxicity
Normal cells
PV
HV
Necrosis
Bile Formation
Functions of Bile
• Transports material to the intestine for
excretion
– Drugs, toxins, xenobiotics
– Cholesterol
– Bilirubin
– Copper
• Transports bile acids to the intestine to
aid in fat absorption
Bile Acids
• Organic acid synthesized in liver from
cholesterol
• Conjugated to amino acids
• Secreted in bile - essential for fat
digestion/absorption
• Reabsorbed in distal ileum and
returned to liver via portal vein
Bile Acid
Cholesterol
Cholesterol: Flat (planar) hydrophobic compound
OH
Metamorphosis to a bile acid
OH
Lose the double bond
Metamorphosis to a bile acid
OH
Shorten the side chain
Metamorphosis to a bile acid
COOH
OH
Add a carboxylic acid group
and bend this below the
plane of the rings
Metamorphosis to a bile acid
COOH
OH
Add a hydroxyl group
that is bent down
OH
Metamorphosis to a bile acid
Add another
hydroxyl group
OH
COOH
OH
OH
Metamorphosis to a bile acid
you now have a tri-hydroxy bile acid: cholic acid
OH
COOH
OH
OH
One more change conjugation of an amino acid to the side chain yields
Taurocholate (taurine conjugated cholic acid)
OH
CO NH
OH
COOH
OH
Conjugated tri-OH Bile Acid
Hydrophobic side
OH- OH-
OH-
COOHydrophilic side
Biliary Lipids
Bile acids
from
intestine
To intestine for
fat digestion
Enterohepatic Circulation of Bile Acids: recycling
is efficient Bile acids cycle between
the liver and the small
intestine.
Bile acid
synthesis
Total bile acid pool is
about 3 grams.
Liver
About 90% of bile acids
are reabsorbed in the
terminal ileum.
However about 5-10% of
bile acids are lost daily
into the colon. Effect?
Small bowel
Colon
Liver synthesizes about
5-10% of the total bile acid
pool each day.
Enterohepatic Circulation of Bile Acids: Ilial loss
Resection of 40 cm of
the terminal ileum will
result in what problem?
Bile acid
synthesis
Bile acid loss into the cecum
will increase. What will
this cause?
Liver
Liver upregulates bile
acid synthesis and bile
acid pool remains normal.
Fat absorption remains
the same.
Colon
40 cm resection
of terminal ileum
Enterohepatic Circulation of Bile Acids:
Loss of most of the ileum
Bile acid
synthesis
Resection of >100 cm of
the terminal ileum will
result in what problem?
Liver
Initially, bile acid loss into
the colon will be massive.
What will be the initial
effect of this loss of bile
acids into the colon?
Colon
>100 cm resection
of terminal ileum
Enterohepatic Circulation of Bile Acids: Lost of
Ileum
Resection of > 100 cm of
the terminal ileum will
result in what problem
over time?
Bile acid
synthesis
Liver upregulates bile
acid synthesis but cannot
keep up with loss rate. Bile
acid pool is reduced
Fat is malabsorbed.
Liver
Colon
> 100 cm resection
of terminal ileum
As the bile acid pool falls,
loss into the colon is less
per day and secretory
diarrhea due to bile acids
converts to steatorrhea
(+ secretory diarrhea
from fatty acids).
Enterohepatic Circulation of Bile Acid:
Cholestyramine
Cholestyramine:
bile acid binding resin
that removes bile acids
from the enterohepatic
circulation
Bile acid
synthesis
Liver
Liver upregulates bile acid
synthesis (using up
what compound in the
process?)
If liver cannot keep up,
what happens?
Small bowel
Colon
Less free bile acid in
the colon causes what?
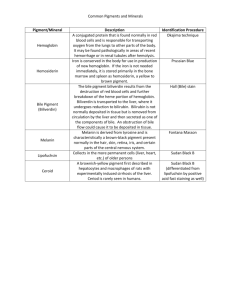
Liver takes up and excretes many other organic compounds:
bilirubin is the classic and historic example
Hepatic Bilirubin Transport
SER
RBC
breakdown
in RES
UDP-glucuronide
+
Unconj BR
Conj
BR
Unconj
Bilirubin
Unconj BR
Bile
Canaliculus
Conj
BR
MRP-2:
Multispecific organic
anion transporter
Conj
BR
ATP
Blood
Hepatocyte
Conjugated bilirubin
Glutathione S-conjugates
other organic anions
Jaundice of the Neonate
•
Newborn infants have poorly
developed bilirubin conjugation
enzymes and jaundice is
common.
•
Premature infants are even
more affected
•
Unconjugated bilirubin in the
brain causes permanent
damage (kernicterus)
•
How to prevent brain damage in
neonates?
Regents of the University of Michigan
Phototherapy for
Unconjugated
Hyperbilirubinemia of the
Neonate
Martybugs, Wikimedia Commons.
Hepatic Bilirubin Transport and Mechanisms
of Hyperbilirubinemia
Gilbert's syndrome (mild)
Crigler-Najjar syndrome (severe)
SER
Hemolysis
Unconj
Bilirubin
Bile
Canaliculus
Unconj BR
Conj
BR
Multispecific organic
anion transporter
Conj
BR
ATP
Conjugated bilirubin
Glutathione S-conjugates
other organic anions
Blood
Hepatocyte
Dubin-Johnson syndrome
Rotor's syndrome
?estrogen/cyclosporin
Consequences of Liver Disease
for Bilirubin Handling?
Bilirubin:
Jaundice
The first liver
disease test
CDC
Liver Biotransformation/Excretion of
Endogenous/Exogenous Compounds
• Bilirubin conjugation is an example
• Many other organic compounds undergo twostep biotransformation
– Example: cholesterol to bile acids
• After biotransformation, metabolites excreted
– Larger, lipophilic molecules excreted in bile
– Smaller (<400 Da) transported to blood and
excreted by kidneys
Step-wise Synthesis of
Bile Acids from Cholesterol
Steps are analogous to Phase I and Phase II
steps of drug/xenobiotic metabolism
Cholesterol
P450- mediated
hydroxylations
OH group
amino acid
Conjugation
of side chain
to glycine or
taurine
Liver and Gut
Barrier Functions
Liver RES/filter
Metabolism
Biliary excretion
Liver helps to remove/eliminate:
Insoluble,
nonabsorbable
compounds
Xenobiotics: metabolism, excretion
Xenobiotics
Drugs
Drugs
Bacteria
(acid,:physical metabolism, excretion
barrier,
gut immune
Bacteria
:
Kupfer cells
system, liver RES)
Intestine
mucosal barrier
Pancreas
Liver’s Magic Trick: Regeneration
Image of liver regeneration process removed
Prometheus
Bound
P.P.Reubens
An early case of
of hepatic regeneration
P. P. Rubens
Functional Consequences of
Losing a Large Amount of Liver
Due to Resection/Necrosis?
•
•
•
•
Hypoglycemia
Poor blood clotting
Cholestasis and jaundice
Increased blood ammonia - affects
cognitive function
• Decreased drug disposition
• Abnormal lipid metabolism
Summary
• Liver exhibits a wide range of functions
• Liver diseases may cause malfunction
of one or more normal function
• Functions regulated separately so any
one liver disease can affect each to a
different extent
• Liver diseases cause:
– Altered liver functions
– Altered tests of liver injury
Additional Source Information
for more information see: http://open.umich.edu/wiki/AttributionPolicy
Slide 73, Image 1 (top): Martybugs, "Jaundice phototherapy," Wikimedia Commons, http://commons.wikimedia.org/wiki/File:Jaundice_phototherapy.jpg,
CC; BY-SA 3.0, http://creativecommons.org/licenses/by-sa/3.0/.