antihistamine, treatment of cough
advertisement
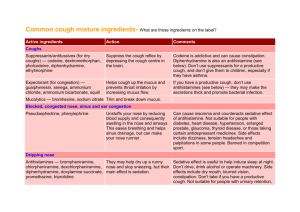
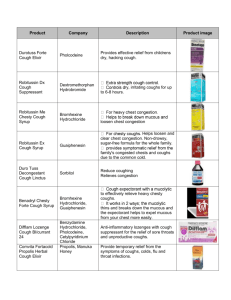
1)ANTI-HISTAMINES 2)ANTI-TUSSIVE MODIFIED BY Israa Classification of antihistamines • • • • • They are classified into H1-blockers & H2-blockers. No currently available antagonist for H3 or H4 Receptors H1-blockers: They block the histamine action on H1 receptors Best work if given before histamine release (prophylactically ) because they only bind to the free receptors • Can be divided in to 1. First Generation: Sedating 2. Second Generation: Non-sedating First Generation Agents • • • • • Ethanol-amines: DIPHEN-HYDRAMINE Ethylene-di-amine: TRI-PELENNAMINE Alkyl-amine: CHLORPHENIRAMINE Phenothiazine: PROMETHAZINE (Phenergan) Piperazines: HYDROXYZINE First Generation Agents uses • In anaphylaxis (serious allergic reaction that is rapid in onset and may cause death.) and other cases where histamine release can occur (epinephrine must also be used) • Anti-allergy (allergic rhinitis, allergic dermatoses, contact dermatitis) • Sedative/sleep aid • To prevent motion sickness • Antiemetic: prophylactic for motion sickness • Antivertigo • Local anesthetic • Antitussive Pharmacokinetics for the first generation • Are absorbed from the GIT. • Can also be given parenterally & topically. • Most of them are widely distributed throughout the body, but some do not penetrate the BBB, • Are most effective when used prophylactically. • Most of the them are metabolized extensively in the liver. additional effects of the first generation • Block H1 receptors in CNS→ sedation, dizziness & fatigue. • Anticholinergic effect → dry mouth, urinary retention, tachycardia • α- blocking effect →postural hypotension, reflex tachycardia. • Antiserotonin effect → ↑appetite Adverse Effects of the first generation • • • • • Sedation (Paradoxical Excitation in children) Dizziness Fatigue Tachydysrhythmias in overdose - rare Peripheral antimuscarinic effects 1. 2. 3. 4. dry Mouth blurred Vision constipation urinary Retention Adverse effects observed with first generation antihistamines The use of first generation H1 antihistamines is contraindicated in treatment of individuals working in jobs where wakefulness is critical Second generation H1-blockers • Examples for this group: loratadine ,fexofinadine, cetirizine, astemazole • Are specific for H1 receptors. • Do not penetrate the BBB so they show less CNS toxicity. Pharmacokinetics for the second generation • Cetirizine (C), loratadine (L), fexofenadine (F) are well absorbed and excreted mainly in unmetabolized form. • C and L are primarily excreted in the urine • F is primarily excreted in the feces • They induce Cyt P450 liver enzymes Adverse Effects of the second generation • in general, these agents have a much lower incidence of adverse effects than the first generation agents. • terfenadine and astemizole were removed from the market due to effects on cardiac K+ channels prolong QT interval (potentially fatal arrhythmia “torsades de pointes”)> is an uncommon variant of ventricular tachycardia that can be the result of lengthening the QT interval.) Treatment of cough Modified By :ISRAA Treatment of Cough • • • • • Antitussives (cough center suppressants) Expectorants Mucolytics Antihistamines Pharyngeal Demulcents (>is an agent that forms a soothing film over a mucous membrane, relieving minor pain and inflammation of the membrane.) 1) Antitussive • Antitussive drugs act by ill defined effect in the brain stem , depressing an even more poorly defined “cough center”. • All opioid narcotic analgesic have antitussive properties in doses lower than those required for pain relief • They have minimum analgesic and addictive properties • Newer agent that only act peripherally on sensory nerves in bronchi are being assessed i) CODIENE • It is the gold standard treatment for cough suppression • It decreases the sensitivity of cough center in the CNS to peripheral stimuli, decrease the mucosal secretion which thicken the sputum, and inhibit ciliary activity • These therapeutic effect occur at doses lower than those required for analgesia but still observed some common side effect like constipation, dysphoria(An emotional state characterized by anxiety, depression, or unease.), and fatigue, in addition to addiction potential ii) DEXTROMETHORPHAN • Is a synthetic derivative of morphine that suppresses the response of the central cough center • It has no analgesic effect, has low addictive profile, but may cause dysphoria at higher doses(An emotional state characterized by anxiety, depression, or unease.) • Has significantly better side effect profile than codeine and has been demonstrated to be equally effective for cough suppression 2) Expectorants (Mucokinetics) • Act peripherally • Increase bronchial secretion OR • Decrease its viscosity and facilitates its removal by coughing • Loose cough ►less tiring &more productive Classification of Expectorants Classified into a) Directly acting E.g., Guaifenesin (glyceryl guaiacolate), Na+ & K+ citrate or acetate, b) Reflexly acting E.g., Ammonium salt Directly acting expectorants i) Sodium & potassium citrate or Acetate • They increase bronchial secretion by salt action ii) Guaifenesin • Expectorant drug usually taken by mouth • Available as single & also in combination • MOA=Increase the volume & reduce the viscosity of secretion in trachea & bronchi • Reflexly acting expectorants: • Ammonium salts:Its expectorant action is caused by irritative action on the bronchial mucosa.It is also a Gastric irritants causing reflex increase in bronchial secretions + sweating 3) Mucolytics • Help in expectoration by liquefying the viscous tracheobronchial secretions • E.g., Bromhexine, Acetyl cysteine, i) Bromhexine • Synthetic derivative of vasicine(*Alkaloid & like Theophylline) MOA of Bromhexine • a) Thinning & fragmentation of mucopolysaccaride fibers • b) ↑ volume & ↓ viscosity of sputum 3) Mucolytics ii) Acetylcysteine • Given directly into respiratory tract • MOA of acetylcysteine: Opens disulfide bond in mucoproteins of sputum =↓ viscosity • Uses: • Cystic fibrosis, Onset of action is quick---used 2-8 hourly • Adverse effects: • Nausea, vomiting, bronchospasm in bronchial asthma 4) Antihistamines • Added to antitussives/expectorant formulation • Due to sedative anticholinergic actions produce relief from cough but lack selectivity for cough center • No expectorant action =▼secretions (anticholinergic effect) • Suitable for allergic cough • E.g., Chlorpheniramine and diphenhydramine 5) Pharyngeal demulcents(>is an agent that forms a soothing film over a mucous membrane, relieving minor pain and inflammation of the membrane.) • Soothe the throat (directly & also by promoting salivation • Reduces afferent impulses from inflamed/irritated pharyngeal mucosa • Provide symptomatic relief in dry cough arising from throat • E.g. lozenges, cough drops, glycerine, liquorice(*Sweet tea), honey Good luck