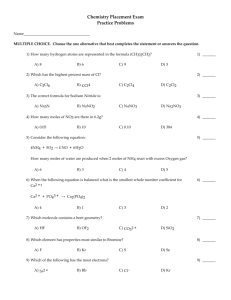
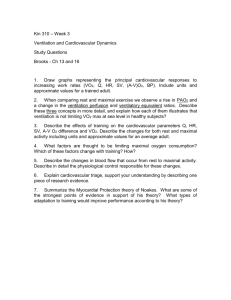
Seminar in Advanced Physiology of Exercise
advertisement
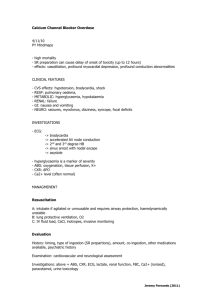
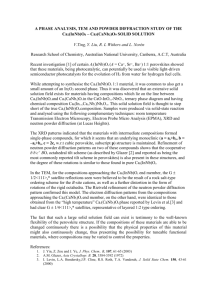
Oxygen Transport Systems Integration of Ventilation, Cardiac, and Circulatory Functions Cardiovascular Function transportation of O2 and CO2 transportation of nutrients/waste products distribution of hormones thermoregulation maintenance of blood pressure Long Refractory Period in Cardiac Muscle Prevents Tetany Cardiac Fibers Develop Graded Tension Frank-Starling Law of the Heart graded Ca2+ release from SR – dependent on Ca2+ influx through DHP channels Autorhythmic cells depolarize spontaneously – leaky membrane – SA and AV node Group III Central command input and output Cardiac output affected by: 1. preload – end diastolic pressure (amount of myocardial stretch) affected by venous return 2. afterload – resistance blood encounters as it leaves ventricles affected by arterial BP 3. contractility – strength of cardiac contraction 4. heart rate Mechanisms affecting HR VO2 = HR SV (a-v O2) Sinoatrial node is pacemaker for heart – spontaneously depolarizes • leakiness to Na+ – influenced by autonomic NS • training down-regulates ß-adrenergic system causing bradycardia Cardiac Output Regulation Extrinsic control autonomic nervous system – sympathetic NS (1 control at HR >100 bpm) – parasympathetic NS (1 control at HR <100 bpm) – stimulates ß-adrenergic receptors on myocardium hormonal – EPI, NE Mechanisms affecting SV VO2 = [HR SV] (a-v O2) amount of Ca2+ influx – APs open Ca2+ channels on ttubules – also stimulates Ca2+ release from SR length-tension relationship – [Ca2+]-tension relationship ß1-adrenergic modulation – activates cAMP phosphorylates L-type Ca2+, SR Ca2+ channels and pumps, troponin – Ca2+ influx and Ca2+ release from SR training LV EDV Intrinsic control Frank-Starling Principle Dotted lines indicate end-systole and end-diastole – Ca2+ influx w/ myocardial stretch – stretched fibers work at optimal lengthtension curve Cardiovascular Response to Exercise Laughlin, M.H. Cardiovascular responses to exercise. Adv. Physiol. Educ. 22(1): S244-S259, 1999. [available on-line] Cardiovascular Response to Exercise Fick principle VO2 = Q (CaO2 – CvO2) VO2 = [HR SV] (CaO2 – CvO2) VO2 = [BP TPR] (CaO2 – CvO2) Exercise Effects on Cardiac Output HR caused by – sympathetic innervation – parasympathetic innervation – release of catecholamines SV, caused by – sympathetic innervation – venous return Myocardial Mechanisms Influencing SV During Exercise SV = EDV – ESV Factors that influence SV – Heart size (LVV) – LV compliance during diastole Progressive in ESV with graded exercise is from contractility – Attributed to sympathetic NS, length-tension changes • Influx of Ca2+ through L-type Ca2+ channels stimulates Ca2+ from SR release channels (Ca2+-induced Ca2+release) Role of Ca2+ in Cardiac Function influx of Ca2+ through L-type Ca2+ channels stimulates Ca2+ from SR release channels (Ca2+induced Ca2+-release) amount of Ca2+ released from SR dependent on sarcomere length SERCA pumps return Ca2+ to sarcoplasmic reticulum sympathetic -adrenergic stimulation contractile force and relaxation time – affects Ca2+ sensitivity through phosphorylation – increases length of diastole to filling time HR and Q responses to exercise intensity SV during graded running Zhou et al., MSSE, 2001 Effect of training and maximal exercise on VO2, Q, and a-v O2 difference VO2 (L·min-1) Q (L·min-1) a-v O2 difference (ml O2·100 ml-1) at rest 0.25 5.0 5.0 at maximal intensity 3.00 20.0 15.0 12 4 3 at rest 0.25 5.0 5.0 at maximal intensity 6.00 37.5 16.0 24 7.5 3.2 Untrained man fold increase Elite endurance male athlete fold increase Effect of training and maximal exercise on VO2, Q, and a-v O2 difference VO2 (L·min-1) HR (bpm) SV (ml·beat-1) a-v O2 difference (ml O2·100 ml-1) at rest 0.25 72 70 5.0 at maximal intensity 3.00 200 100 15.0 12 2.8 0.7 3.0 at rest 0.25 40 125 5.0 at maximal intensity 6.00 195 192 16.0 24 4.9 1.5 3.2 Untrained individual fold increase Elite endurance athlete fold increase Effects of Exercise on Blood Pressure BP = Q TPR Arterioles and Capillaries arterioles terminal arterioles (TA) capillaries collecting venules (CV) arterioles regulate circulation into tissues – under sympathetic and local control precapillary sphincters fine tune circulation within tissue – under local control capillary density 1 determinant of O2 diffusion Regulation of Blood Flow and Pressure Blood flow and pressure determined by: A. Vessel resistance (e.g. diameter) to blood flow B. Pressure difference between two ends A cardiac output A B arterioles B Effects of Exercise Intensity on TPR 25 TPR 20 15 10 5 0 0 50 100 150 200 250 300 Treadmill speed (m/min) 350 400 Effects of Incremental Exercise on BP 250 Blood pressure (mm Hg) 225 200 175 150 125 100 75 Systolic BP Diastolic BP 50 25 0 0 50 100 150 200 Workload (W) 250 300 Effects of Isometric Exercise on BP Blood pressure (mm Hg) 225 200 175 150 125 100 75 Systolic BP Diastolic BP 50 25 0 0 30 60 90 Time (s) 120 150 Control of Blood Flow Blood flow to working muscle increases linearly with muscle VO2 Blood Distribution During Rest Blood Flow Redistribution During Exercise Effect of exercising muscle mass on blood flow (1-adrenergic receptor blocker) 30 s Onset of exercise Local Control of Microcirculation metabolic factors that cause local vasodilation – – – – PO2 PCO2 H+ adenosine endothelial factors that cause local vasodilation – nitric oxide (NO) • released with shear stress and EPI • redistributed from Hb—greater O2 release from Hb induces NO release as well Adenosine metabolism in myocytes and endothelial cells ATP ADP AMP adenosine Adenosine is released in response to hypoxia, ischemia, or increased metabolic work Single layer of endothelial cells line innermost portion of arterioles that releases nitric oxide (NO) causing vasodilation Hemoglobin consists of four O2-binding heme (iron containing) molecules combines reversible w/ O2 (oxy-hemoglobin) Bohr Effect – O2 binding affected by – – – – – PO2 PCO2 pH temperature 2,3-DPG (diphosphoglycerate) CO2 transport Factors affecting Oxygen Extraction Fick principle VO2 = Q (CaO2 – CvO2) O2 extraction during graded exercise Sympathetic stimulation causes spleen to constrict releasing RBC into blood, thus increasing O2-carrying capacity Bohr effect on oxyhemoglobin dissociation PO2, pH and PCO2, temperature, and 2,3 DPG shift curve to left causing greater O2 release Cardiovascular Adaptations to Training HR and Q responses to exercise intensity SV during graded running Zhou et al., MSSE, 2001 Cardiovascular Adaptations to Endurance Training VO2max = HRmax SVmax (a-v O2 diff)max ~50% of VO2max is because of SVmax 1 mechanism is from LV-EDV – compliance (ability to stretch) – myocardial growth (longitudinal and crosssectional) • longitudinal growth doesn’t affect sarcomere length contractility (systolic function) and relaxation (diastolic function) – Ca2+ sensitivity – Ca2+ removal Left ventricular adaptations depend on training type myocardial thickness LV-EDV Endurance trained preload (volume overload) Sedentary Resistance trained afterload (pressure overload) Ventilation PO2 and PCO2 in lungs and blood Humoral Chemoreceptors PAO2 – not normally involved in control PACO2 – central PACO2 chemoreceptors are 1º control factor at rest H+ – peripheral H+ chemoreceptors are important factor during high-intensity exercise – CO2 + H2O H2CO3 H+ + HCO3- Matching of Ventilation and Perfusion 100% of cardiac output flows through lungs – low resistance to flow pulmonary capillaries cover 70-80% of alveolar walls upper alveoli not opened during rest Pulmonary Gas Exchange alveolar thickness is ~ 0.1 µm total alveolar surface area is ~70 m2 at rest, RBCs remain in pulmonary capillaries for 0.75 s (capillary transit time) – 0.4-0.5 s at maximal exercise • adequate to release CO2; marginal to take up O2 O2 and CO2 exchange in alveolar capillaries PO2 = 40 PCO2 = 46 Gas Exchange and Transport Oxygen Transport ~98% of O2 transported bound to hemoglobin Carbon Dioxide Transport dissolved in plasma (~7%) bound to hemoglobin (~20%) as a bicarbonate ion (~75%) CO2 + H2O H2CO3 H+ + HCO3- Hemoglobin consists of four O2-binding heme (iron containing) molecules combines reversible w/ O2 (oxy-hemoglobin) Bohr Effect – O2 binding affected by – – – – – temperature pH PO2 PCO2 2,3-DPG (diphosphoglycerate) Bohr effect on oxyhemoglobin dissociation CO2 transport Ventilatory Control of Blood pH Ventilatory Regulation of AcidBase Balance CO2 + H2O H2CO3 H+ + HCO3 source of these expired carbons is from bicarbonate ions (HCO3-), NOT substrates at low-intensity exercise, source of CO2 is entirely from substrates at high-intensity exercise, bicarbonate ions also contribute to VCO2 Can RER every exceed 1.0? When? Explain Minute Ventilation Minute Ventilation (L/min) 200.0 180.0 160.0 140.0 120.0 100.0 80.0 60.0 40.0 20.0 0.0 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Treadmill Speed (mph) VE and VO2 Response to Incremental Exercise Blood pH 7.45 7.40 7.35 pH 7.30 7.25 7.20 7.15 7.10 7.05 4 5 6 7 8 9 10 11 12 Treadmill Speed (mph) 13 14 15 CO2 Production 90 VCO2 (ml/kg/min) 80 70 60 50 40 30 20 10 0 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Treadmill Speed (mph) Respiratory Exchange Ratio 1.3 RER 1.2 1.1 1.0 0.9 0.8 4 5 6 7 8 9 10 11 12 Treadmill Speed (mph) 13 14 15 35 VE/VO2 30 25 20 15 100 125 150 175 200 225 250 275 300 325 350 375 Treadmill Speed (m/min) Ventilatory equivalents for VO2 (dark blue) and VCO2 (yellow). Arrow indicates occurrence of ventilatory threshold.