14 Periodontium
advertisement

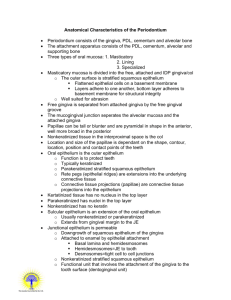
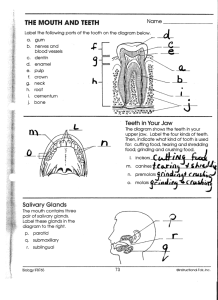
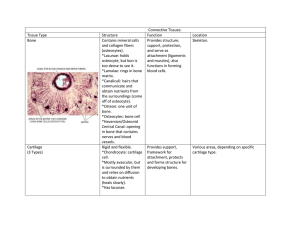
PERIODONTIUM Cementum Pulp cavity Enamel Dentin Gingiva PDL Alveolar bone Cementum Sharpey's fibers Attachment organ Periodontal ligament Root canal Alveolar bone Apical foramen Alveolar vessels & nerves TEETH IN-SITU Periodontium (forms a specialized fibrous joint called Gomphosis) • • • • Cementum Periodontal Ligament Alveolar bone Gingiva facing the tooth Cementum The other bone It is a hard avascular connective tissue that covers the roots of teeth Role of Cementum 1) It covers and protects the root dentin (covers the opening of dentinal tubules) 2) It provides attachment to the periodontal fibers 3) It compensates for tooth resorption Varies in thickness: thickest in the apex and in the inter-radicular areas of multirooted teeth, and thinnest in the cervical area 10 to 15 m in the cervical areas to 50 to 200 m (can exceed > 600 m) apically Cementum simulates bone • Organic fibrous framework, ground substance, crystal type, development • Lacunae • Canaliculi • Cellular component • Incremental lines (also known as “resting” lines; they are produced by continuous but phasic, deposition of cementum) Differences between cementum and bone • Not vascularized – a reason for it being resistant to resorption • Minor ability to remodel • More resistant to resorption compared to bone • Lacks neural component – so no pain • 70% of bone is made by inorganic salts (cementum only 45-50%) • 2 unique cementum molecules: Cementum attachment protein (CAP) and IGF Clinical Correlation Cementum is more resistant to resorption: Important in permitting orthodontic tooth movement Development of Cementum Cementum formation occurs along the entire tooth Hertwig’s epithelial root sheath (HERS) – Extension of the inner and outer dental epithelium HERS sends inductive signal to ectomesenchymal pulp cells to secrete predentin by differentiating into odontoblasts HERS becomes interrupted Ectomesenchymal cells from the inner portion of the dental follicle come in with predentin by differentiating into cementoblasts Cementoblasts lay down cementum How cementoblasts get activated to lay down cementum is not known 3 theories: 1. Infiltrating dental follicle cells receive reciprocal signal from the dentin or the surrounding HERS cells and differentiate into cementoblasts 2. HERS cells directly differentiate into cementoblasts 3. What are the function of epithelial cell rests of Malassez? Cementoblasts • Derive from dental follicle • Transformation of epithelial cells Proteins associated with Cementogenesis • Growth factors – TGF – PDGF – FGF • Adhesion molecules – Bone sialoprotein – Osteopontin Proteins associated with Cementogenesis • Epithelial/enamel-like factors • Collagens • Gla proteins – Matrix – Bone • Collagens • Transcription factors – Cbfa 1 and osterix • Other – Alkaline phosphatase Hyaline layer of Hopewell-Smith (Intermediate Cementum) First layer of cementum is actually formed by the inner cells of the HERS and is deposited on the root’s surface is called intermediate cementum or Hyaline layer of Hopewell-Smith Deposition occurs before the HERS disintegrates. Seals of the dentinal tubules Intermediate cementum is situated between the granular dentin layer of Tomes and the secondary cementum that is formed by the cementoblasts (which arise from the dental follicle) Approximately 10 m thick and mineralizes greater than the adjacent dentin or the secondary cementum Properties of Cementum Physical: Cementum is pale yellow with a dull surface Cementum is more permeable than other dental tissues Relative softness and the thinness at the cervical portion means that cementum is readily removed by the abrasion when gingival recession exposes the root surface to the oral environment Chemical Composition of Cementum Similar to bone 45% to 50% hydroxyapatite (inorganic) 50% to 55% collagenous and noncollagenous matrix proteins (organic) Collagenous component •TYPE I • TYPE III • TYPE XII • TYPE V • TYPE XIV Classification of Cementum • Presence or absence of cells • Origin of collagenous fibers of the matrix • Prefunctional and functional Cellular and Acellular Cementum Acellular cementum: covers the root adjacent to dentin whereas cellular cementum is found in the apical area Cellular: apical area and overlying acellular cementum. Also common in interradicular areas Cementum is more cellular as the thickness increases in order to maintain viability The thin cervical layer requires no cells to maintain viability as the fluids bathe its surface A: Acellular cementum (primary cementum) B: Cellular Cementum (secondary cementum) A: Acellular cementum B: Hyaline layer of Hopwell-Smith C: Granular layer of Tomes D: Root dentin Cellular: Has cells Acellular: No cells and has no structure Cellular cementum usually overlies acellular cementum Acellular Cellular Variations also noted where acellular and cellular reverse in position and also alternate CEMENTUM Canaliculus GT Lacuna of cementocyte Dentin Acellular cementum Cellular cementum Hyaline layer (of Hopewell Smith) Granular layer of tomes Dentin with tubules Cementoblast and cementocyte Cementocytes in lacunae and the channels that their processes extend are called the canaliculi Cementoid: Young matrix that becomes secondarily mineralized Cementum is deposited in increments similar to bone and dentin Are acellular and cellular cementum formed from two different sources? One theory is that the structural differences between acellular and cellular cementum is related to the faster rate of matrix formation for cellular cementum. Cementoblasts gets incorporated and embedded in the tissue as cementocytes. Different rates of cementum formation also reflected in more widely spaced incremental lines in cellular cementum Classification Based on the Nature and Origin of Collagen Fibers Organic matrix derived form 2 sources: 1. Periodontal ligament (Sharpey’s fibers) 2. Cementoblasts Extrinsic fibers if derived from PDL. These are in the same direction of the PDL principal fibers i.e. perpendicular or oblique to the root surface Intrinsic fibers if derived from cementoblasts. Run parallel to the root surface and at right angles to the extrinsic fibers The area where both extrinsic and intrinsic fibers is called mixed fiber cementum Combined classification (see Table 9-2) Acellular Extrinsic Fiber Cementum (AEFC-Primary Cementum) • Located in cervical half of the root and constitutes the bulk of cementum • The collagen fibers derived from Sharpey’s fibers and ground substance from cementoblasts • Covers 2/3rds of root corresponding with the distribution of primary acellular cementum • Principal tissue of attachment • Function in anchoring of tooth • Fibers are well mineralized Primary acellular intrinsic fiber • • • • • • First cementum Primary cementum Acellular Before PDL forms Cementoblasts 15-20μm Cellular intrinsic fiber cementum (CIFCSecondary Cementum ) • Starts forming after the tooth is in occlusion • Incorporated cells with majority of fibers organized parallel to the root surface • Cells have phenotype of bone forming cells • Very minor role in attachment (virtually absent in incisors and canine teeth) • Corresponds to cellular cementum and is seen in middle to apical third and intrerradicular • Adaptation • Repair Secondary cellular mixed fiber cementum • Both intrinsic and extrinsic fibers [Extrinsic (5 – 7 m) and Intrinsic (1 – 2 m)] • Bulk of secondary cementum • Cementocytes • Laminated structure • Cementoid on the surface • Apical portion and intrerradicular • Adaptation Intrinsic fibers are uniformly mineralized but the extrinsic fibers are variably mineralized with some central unmineralized cores Zone of Transition Acellular afibrillar cementum • • • • Limited to enamel surface Close to the CE junction Lacks collagen so plays no role in attachment Developmental anomaly vs. true product of epithelial cells Distribution of Cementum on the Root • Acellular afibrillar: cervical enamel • Acellular extrinsic: Cervix to practically the whole root (incisors, canines) increasing in thickness towards the apical portion 50200μm • Cellular: Apical third, furcations CE junction The “OMG” rule Cementum overlaps enamel 60% Cementum just meets enamel 30% Small gap between cementum and enamel 10% Aging of Cementum 1. 2. 3. 4. Smooth surface becomes irregular due to calcification of ligament fiber bundles where they are attached to cementum Continues deposition of cementum occurs with age in the apical area. [Good: maintains tooth length; bad: obstructs the foramen] Cementum resorption. Active for a period of time and then stops for cementum deposition creating reversal lines Resorption of root dentin occurs with aging which is covered by cemental repair Cementicles • Calcified ovoid or round nodule found in the PDL • Single or multiple near the cemental surface • Free in ligament; attached or embedded in cementum • Aging and at sites of trauma Origin: Nidus of epithelial cell that are composed of calcium phosphate and collagen to the same amount as cementum (45% to 50% inorganic and 50% to 55% organic) Cemental Repair Protective function of cementoblasts after resorption of root dentin or cementum Resorption of dentin and cementum due to trauma (traumatic occlusion, tooth movement, hypereruption) Loss of cementum accompanied by loss of attachment Following reparative cementum deposition attachment is restored Clinical Correlation Cellular cementum is similar to bone but has no nerves. Therefore it is non-sensitive to pain. Scaling produces no pain, but if cementum is removed, dentin is exposed causes sensitivity Cementum is resistant to resorption especially in younger Patients. Thus, orthodontic tooth movement causes alveolar one resorption and not tooth root loss Alveolar Process Gingiva Near the end of the 2nd month of fetal life, mandible and maxilla form a groove that is opened toward the surface of the oral cavity As tooth germs start to develop, bony septa form gradually. The alveolar process starts developing strictly during tooth eruption. a) outer cortical plates b) a central spongiosa c) bone lining the alveolus (bundle bone) Alveolar bone proper: The compact or dense bone that lines the tooth. Contains either perforating fibers from periodontal ligament (Sharpey’s fibers) or just compact bone Sharpey’s fibers embedded into the alveolar bone proper Present at right angles or oblique to the surface of alveolar bone and along the root surface Because alveolar process is regularly penetrated by collagen fiber bundles, it is also called bundle bone. It appears more radiodense than surrounding supporting bone in X-rays called lamina dura Bundle Bone It is perforated by many foramina that transmit nerves and vessels (cribriform plate). Radiographically, the bundle bone is the lamina dura. The lining of the alveolus is fairly smooth in the young but rougher in the adults. Radiodense because increased mineral content around fiber bundles Lamina Dura Supporting Compact Bone Similar to compact bone anywhere else (Haversian bone) Extends both on the lingual (palatal) and buccal side Contains haversian and Volkman’s canals (they both form a continuous channel of nutrient canals) Bundle bone and Trabecular bone Arrows: Sharpey’s fiber The alveolar crest is found 1.5-2.0 mm below the level of the CEJ. If you draw a line connecting the CE junctions of adjacent teeth, this line should be parallel to the alveolar crest. If the line is not parallel, then there is high probability of periodontal disease. Clinical considerations Resorption and regeneration of alveolar bone This process can occur during orthodontic movement of teeth. Bone is resorbed on the side of pressure and opposed on the site of tension. Decreased bone (osteopenia) of alveolar process is noted when there is inactivity of tooth that does not have an antagonist Lack of antagonists Periodontal Ligament PDL is the soft specialized connective tissue situated between cementum and alveolar bone proper Ranges in thickness between 0.15 and 0.38 mm and is thinnest in the middle portion of the root The width decreases with age Tissue with high turnover rate Contains fibers, cells and intercellular substance Embryogenesis The PDL forms from the dental follicle shortly after root development begins FUNCTIONS OF PERIODONTIUM Tooth support Shock absorber: Withstanding the forces of mastication Sensory receptor necessary for proper positioning of the jaw Nutritive: blood vessels provide the essential nutrients to the vitality of the PDL Cells a) Osteoblasts b) Osteoclasts (critical for periodontal disease and tooth movement) c) Fibroblasts (Most abundant) d) Epithelial cells (remnants of Hertwig’s epithelial root sheathepithelial cell rests of Malassez) e) Macrophages (important defense cells) f) Undifferentiated cells (perivascular location) h) Cementoblasts i) Cementoclasts (only in pathologic conditions) Epithelial Cell Rests of Malassez PDL fibers - Collagen fibers: I, III and XII. Groups of fibers that are continually remodeled. (Principal fiber bundles of the PDL). The average diameter of individual fibers are smaller than other areas of the body, due to the shorter half-life of PDL fibers (so they have less time for fibrillar assembly) - Oxytalan fibers: variant of elastic fibers, perpendicular to teeth, adjacent to capillaries - Eluanin: variant of elastic fibers Principal Fibers Run between tooth and bone. Can be classified as dentoalveolar and gingival group Dentoalveolar group a. Alveolar crest group (ACG): below CE junction, downward, outward b. Horizontal group: apical to ACG, right angle to the root surface c. Oblique group: most numerous, oblique direction and attaches coronally to bone d. Apical group: around the apex, base of socket e. Interradicular group: multirooted teeth Runs from cementum and bone , forming the crest of the interradicular septum At each end, fibers embedded in bone and cementum: Sharpey’s fiber Gingival ligament fibers: the principal fibers in the gingival area are referred to as gingival fibers. Not strictly related to periodontium. Present in the lamina propria of the gingiva. a. Dentogingival: most numerous; cervical cementum to f/a gingiva b. Alveologingival: bone of the alveolar crest to f/a gingiva c. Circular: around neck of teeth, free gingiva d. Dentoperiosteal: runs apically from the cementum over the outer cortical plate to alv. process or vestibule (muscle) or floor of mouth e. Transseptal: cementum between adjacent teeth, over the alveolar crest Transeptal Alveolar crest Horizontal Oblique Oxytalan Fibers Type of elastic fibers present as bundes of microfibrils that run oblique from the cementum surface to the blood vessels. Associated with neural elements. Most numerous in the cervical area. Function: Regulate vascular flow in relation to tooth function The PDL gets its blood supply from perforating arteries (from the cribriform plate of the bundle bone). The small capillaries derive from the superior & inferior alveolar arteries. The blood supply is rich because the PDL has a very high turnover as a tissue. The posterior supply is more prominent than the anterior. The mandibular is more prominent than the maxillary. Nerve supply The nerve supply originates from the inferior or the superior alveolar nerves. The fibers enter from the apical region and lateral socket walls. The apical region contains more nerve endings (except Upper Incisors) Interstitial Space Present between each bundle of ligament fibers Contains blood vessels and nerves Designed to withstand the impact of masticatory forces Ground Substance Amorphous background material that binds tissues and fluids A major constituent of the PDL Similar to most connective tissue ground substance Dermatan sulfate is the major glycosaminoglycan 70% water; critical for withstanding forces When function is increased PDL is increased in size and fiber thickens Bone trabeculae also increase in number and thicker However, in reduction of function, PDL narrows and fiber bundles decreases in number and thickness (this reduction in PDL is primarily due to increased cementum deposition)