8.OesophagusAnat
advertisement

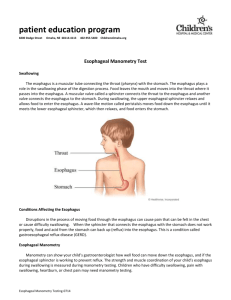
Oesophagus Tony Tiemesmann Diagnostic Radiology Bloemfontein Hospital Complex Key points 1 • The adult human esophagus is an 18- to 25-cm long muscular tube that has cervical, thoracic, and abdominal parts. • The esophagus wall is composed of striated muscle in the upper part, smooth muscle in the lower part, and a mixture of the two in the middle. Key points 2 • Esophagus develops from foregut and by week 10 is lined by ciliated epithelial cells. • Beginning at 4 months, the ciliated epithelium starts to be replaced by squamous epithelium. At either end of the esophagus the ciliated epithelium gives rise to esophageal glands. • The upper esophagus is derived from branchial arches 4, 5, and 6. • Esophageal peristalsis appears in the first trimester, and gastroesophageal reflux can be documented in the second trimester. Introduction • From mouth to stomach, the food conduit consists of the oral cavity, pharynx, and esophagus. • Dynamic tube, pushing food toward the stomach, where digestion and absorption can take place. • Mucus produced by the esophageal mucosa provides lubrication and eases the passage of food. • Active peristaltic contractions propel residual material from the esophagus into the stomach. • During vomiting and reflux, the esophagus also serves as a passageway for gastrointestinal contents traveling retrograde from the stomach or small intestine. Embryology 1 • In the 4th developmental week, a small diverticulum appears at the ventral wall of the foregut - the respiratory (tracheobronchial) diverticulum. • It becomes gradually separated from the foregut by the esophagotracheal septum. • The proliferation of esophageal epithelium almost obliterates the lumen, but the recanalization of the esophagus occurs by the end of the 8th week. Embryology 2 Anatomy 1 • Flattened muscular tube of 18 to 26 cm from the upper sphincter to the lower sphincter. • Between swallows the esophagus is collapsed, canndistend to approximately 2 cm in the anterior-posterior dimension & up to 3 cm laterally. • Connects the pharynx to the stomach - beginning in the neck, at the pharyngoesophageal junction, descends anteriorly to the vertebral column through the superior and posterior mediastinum. • Traverse diaphragm at the diaphragmatic hiatus extends through the gastroesophageal junction to end at the orifice of the cardia of the stomach. Anatomy 2 • Cervical esophagus: pharyngoesophageal junction to the suprasternal notch. • Thoracic esophagus: suprasternal notch to the diaphragmatic hiatus. • Abdominal esophagus: diaphragmatic hiatus to the orifice of the cardia of the stomach. Anatomy 3 • Two high-pressure zones prevent the backflow of food: the upper and lower esophageal sphincter. These functional zones are located at the upper and lower ends of the esophagus but there is not a clear anatomic demarcation of the limits of the sphincters. • Structurally, the esophageal wall is composed of four layers: innermost mucosa, submucosa, muscularis propria, and adventitia. Unlike the remainder of the GIT, the esophagus has no serosa. Blood supply 1 • Rich arterial supply is segmental. • The branches of the inferior thyroid artery provide arterial blood supply to the upper esophageal sphincter and cervical esophagus. • The paired aortic esophageal arteries or terminal branches of bronchial arteries supply the thoracic esophagus. • The left gastric artery and a branch of the left phrenic artery supply the LES and the most distal segment of the esophagus. • The arteries end in an extensive, dense network in the submucosa; rarity of the esophageal infarction. Blood supply 2 Venous drainage 1 • The venous supply is also segmental. • From the dense submucosal plexus the venous blood drains into the superior vena cava. • The veins of the proximal and distal esophagus drain into the azygous system. • Collaterals of the left gastric vein receive venous drainage from the mid-esophagus. • The submucosal connections between the portal and systemic venous systems in the distal esophagus form esophageal varices in portal hypertension. Venous drainage 1 Innervation 1 • The esophagus receives parasympathetic and sympathetic innervation that regulates glandular secretion, blood vessel caliber, and the activity of striated and smooth muscle. • The thin nerve fibers and numerous ganglia of the intramural myenteric (Auerbach) and the submucosal plexi Meissner) provide the intrinsic innervation of the esophagus. Innervation 2 • The spinal afferents have their cell bodies in the dorsal root ganglia and terminate in the spinal column and in the nucleus gracilis and cuneatus in the brainstem. From there, they project, through the thalamus, to primary sensory and insular cortical areas. • The spinal afferents merging from nerve endings in the muscle layer and serosa act as nociceptors for perception of discomfort and pain and are mechanosensitive. Innervation 3 Lymphatics 1 • The lymphatics from the proximal third of the esophagus drain into the deep cervical lymph nodes, and subsequently into the thoracic duct. • The lymphatics from the middle third of esophagus drain into the superior and posterior mediastinal nodes. • Lymphatics of the distal third of the esophageal follow the left gastric artery to the gastric and celiac lymph nodes. • There are considerable interconnections among these three drainage regions; bidirectional lymph flow in this region is responsible for the spread of malignancy from the lower esophagus to the upper esophagus. Lymphatics 2 Musculature 1 • The muscular coat consists of an external layer of longitudinal fibers and an internal layer of circular fibers. • The longitudinal fibers descend in the esophagus and combine to form a uniform layer that covers the outer surface of the esophagus. • The circular muscle layer provides the sequential peristaltic contraction that propels food toward the stomach. • The internal muscular layer is thicker than the external muscular layer. Below the diaphragm, the internal circular muscle layer thickens and the fibers become semicircular and interconnected, constituting the intrinsic component of the LES. Musculature 2 Upper oesophageal sphincter 1 • The upper esophageal sphincter is a high-pressure zone situated between the pharynx and the cervical esophagus. • The UES is a musculocartilaginous structure composed of the posterior surface of the thyroid and cricoid cartilage, the hyoid bone, and three muscles: cricopharyngeus, thyropharyngeus, and cranial cervical esophagus. Upper oesophageal sphincter 2 Lower oesophageal sphincter 1 • The lower esophageal sphincter is a high-pressure zone located where the esophagus merges with the stomach. • The LES is a functional unit composed of an intrinsic and an extrinsic component: intrinsic structure is under neurohormonal influence; extrinsic component consists of the diaphragm muscle. Lower oesophageal sphincter 2 Lower oesophageal sphincter 3 Imaging • • • Endoscopy Rigid Soft PillCam Fluoroscopy Contrast swallow (BaSO4, Iodinated) Nuclear medicine Ba-swallow 1 Ba-swallow 2 Ba-swallow 3 References • Embryo.chronolab.com • Kuo B, Uma D. Oesophagus: Anatomy & development. GI Motility (2006) doi:10.1038/gimo6. 16 May 2006. • Radiologyassistant.nl • Netter FH. Atlas of human anatomy 2nd ed. Hoechstetter. 1999.